ABSTRACT
Nutrition plays an important role in health promotion and disease prevention and treatment across the lifespan. Physicians and other healthcare professionals are expected to counsel patients about nutrition, but recent surveys report minimal to no improvements in medical nutrition education in US medical schools. A workshop sponsored by the National Heart, Lung, and Blood Institute addressed this gap in knowledge by convening experts in clinical and academic health professional schools. Representatives from the National Board of Medical Examiners, the Accreditation Council for Graduate Medical Education, the Liaison Committee on Medical Education, and the American Society for Nutrition provided relevant presentations. Reported is an overview of lessons learned from nutrition education efforts in medical schools and health professional schools including interprofessional domains and competency-based nutrition education. Proposed is a framework for coordinating activities of various entities using a public–private partnership platform. Recommendations for nutrition research and accreditation are provided.
Keywords: medical nutrition education, nutrition competencies, integrative nutrition, culinary medicine, medical board nutrition questions, nutrition coordinating center, academic nutrition medicine
Introduction
Nutrition and dietary behaviors are major contributors to the development and management of chronic diseases including obesity, cardiometabolic disease, and cancer, but healthcare providers remain inadequately trained to initiate or effect patient change (1–3). Adherence to recommended eating patterns can reduce risk and extend quality of life, but consistent and coordinated approaches to assuring the education, training, and competency of healthcare providers remain inconsistent (4, 5).
Physicians are on the frontlines of patient care. Their combined diagnostic and patient counseling skills are vital in initiating and sustaining ongoing follow-up and facilitating patient adherence to prevention and treatment strategies. Health professionals including dietitians and nutritionists, nurse practitioners (NPs), physician assistants (PAs), pharmacists, dentists, and others also play an important role in integrating nutrition and diet interventions in a coordinated interprofessional practice model that can be applied to benefit patients throughout the healthcare spectrum.
To address these topics, the National Heart, Lung, and Blood Institute (NHLBI) of the NIH convened a workshop on the 7–8 September, 2017, that included an interdisciplinary team of over 50 clinicians and educators with expertise in medical nutrition, NIH representatives from other nutrition-related institutes, locally interested graduate and undergraduate medical students, and other healthcare professionals with expertise in academic medicine. This effort followed a 2012 NHLBI workshop that reviewed the contributions of the Nutrition Academic Award (NAA), an initiative conducted among 21 medical schools from 1998 to 2005. Curricular objectives, teaching tools, assessment methodologies, and examination questions for the National Board of Medical Examiners (NBME) were developed through the NAA (1, 2). These accomplishments provided a good start; however, the absence of ongoing infrastructural support limited sustainability and advancements in subsequent years. Manuscripts endorsing the premise and goals of the NAA motivated renewed efforts to proceed with next steps (3–7).
The latest workshop was organized to advance the 2012 workshop goals and identify research gaps and other factors limiting progress towards successful implementation of medical nutrition education. There was further intent to formulate a framework for optimal adaptation of the NAA curriculum guide within the shifting model of education in physician training. Experts in nutrition, metabolism, and lifestyle medicine shared perspectives, deliberated on existing nutrition programs, and considered new culinary medicine interests and emerging priorities. High priorities included updating the curriculum guide, formalizing new and evolving topic areas, developing realistic models for implementing clinical nutrition care, and evaluating competencies and skills. Broader understanding of important integrative educational components and potential strategies to move a multidimensional integrated plan forward were achieved.
This paper summarizes the discussions, case studies, and the coordinated integrated effort needed to achieve workshop goals. The overall goal is to equip trainees with improved nutrition assessment and counseling skills, competencies to make referrals to appropriate providers, and increased awareness of available resources needed to optimize patient care. Research needed to compare outcomes and inform future interprofessional education and training is also summarized.
The Evolving Model of Medical Nutrition Education Then and Now: Historical Perspectives and Lessons Learned
In 1985, based on results of a survey of 45 US medical schools, the National Academy of Sciences recommended at least 25 h of nutrition education in undergraduate medical education (UME) (8). The American Society for Clinical Nutrition's [ASCN; renamed as the American Society for Nutrition (ASN)] Committee on Medical/Dental School and Residency Nutrition Education recommended a minimum of 44 h (9). Consensus on nutrition content in the medical school curriculum remains an ongoing challenge, particularly because of integrated curricula and how hours are counted, more online learning and use of class time for problem solving and discussion (4). In residency and fellowship programs, little medical nutrition education is provided. During the 1980s, the Nutrition in Medicine (NIM) program, a web-based interactive medical nutrition education teaching tool with case studies, was developed at the University of North Carolina, Chapel Hill, and offered free of charge to all US medical schools (10). In 1983, a prototype of a National Nutrition Test Item Bank was developed at the University of Alabama Birmingham in conjunction with the ASCN Committee on Nutrition Education and was deemed viable to address student assessment. Since then, several websites for health professionals have offered links to educational materials including lectures, modules, interactive videos, blogs, and books related to medical nutrition. In addition to nutrition-related societies such as the Academy of Nutrition and Dietetics, ASN, the American Association for Parenteral and Enteral Nutrition (ASPEN), the North American Society for Pediatric Gastroenterology, and The Obesity Society, other societies and institutions such as the American Academy of Pediatrics, the American Academy of Family Physicians, and the American Association of Medical Colleges (AAMC) provide access to peer-reviewed material.
Over the course of the NAA (1998–2005), the 21 funded medical schools developed educational efforts focused on advancing the diet-related guidelines of the National Cholesterol Education Program organized and developed by the NHLBI (2). The NAA schools adopted a variety of approaches (11, 12) and different educational priorities. Common goals included: 1) Establish clear nutrition objectives; 2) Collaborate with the NBME, the AAMC, and the Accreditation Council for Graduate Medical Education (ACGME); 3) Identify how objectives would be nationally standardized and evaluated; and 4) Establish a Coordinating Center to help implement and sustain medical nutrition education.
Evolving models of education and training require a national approach to integrating nutrition across the curriculum supported by teaching faculty and medical school leadership. Pedagogies now emphasize active learning models focused on competencies such as culinary exercises, small group interactions, and hands-on community involvement. In 2006, Boston University School of Medicine (BUSM) created a novel model of medical nutrition education involving students and including student-mentored extracurricular activities to develop, evaluate, and sustain nutrition medicine education (13, 14). Teaching hours in nutrition increased by >5-fold at BUSM, with >108 h of nutrition-related content in the curriculum in 2017–2018. Subsequently, >80% of the NAA curriculum guide was covered across 4 y of UME. Using a medical education database required for full accreditation surveys reviewed by the Liaison Committee on Medical Education (LCME), nutrition was identified in the top 5 out of 32 behavioral and socioeconomic subjects included in required courses at BUSM (13). Subscores on the United States Medical Licensing Examination (USMLE) steps I and II improved. Finally, a cross-sectional electronic survey of first-year to fourth-year medical students including 6 knowledge and 4 self-efficacy nutrition questions showed that students desired more training in counseling and referrals to other healthcare professionals and community resources. Several groups of interested medical students are now involved in extracurricular and curricular nutrition efforts in other universities, including Columbia University, University of North Carolina, Harvard University, Northwestern University, and Tufts University.
Since the 2012 NIH workshop, several professional societies reviewed program practices and provided recommendations. In 2013–2014, 2 bills advocating nutrition education of physicians were introduced into the US Congress (15,16). Legislative progress is limited but interest in culinary medicine, applied nutrition training, competency, and skill development has increased. Several societies and groups approached the LCME to update nutrition questions in the exams, and nutrition champions or advocates have recommended a national medical board for obesity and physician nutrition specialists (4, 17, 18). Needs for interprofessional education to be a component of medical education (18), the development of a coordinating center (4), and the involvement of other government centers, such as Nutrition Obesity Research Centers, in nutrition education and training (7) were also articulated. Nutrition Obesity Research Centers are primarily focused on obesity and nutrition research, but the potential to leverage these resources towards nutrition education and training were identified. The following case studies offer further examples of successful approaches towards providing medical nutrition education.
Case study 1: Brody School of Medicine, East Carolina University
The Brody School of Medicine includes nutrition education in both UME and family medicine curricula. Brody integrated nutrition into the basic science and introductory clinical courses, Family Medicine clerkships, and an elective, as championed by at least 1 physician and a registered dietitian nutritionist and supported by the senior associate dean for curriculum. The current program is under 25 h because of competing priorities, including mandates from the accrediting agency to reduce total curriculum hours. Assessment of clinical nutrition skills occurred within the objective structured clinical examination cases. Curriculum renewal resulted in consensus regarding the requirement for several recommended competencies (19) as follows:
Perform basic nutritional assessment in the inpatient setting and recognize when patient needs to be fed.
Perform basic nutritional assessment in the outpatient setting.
Counsel patients on basic public health nutrition issues (e.g., obesity prevention and treatment, hypertension, cardiovascular disease, and diabetes).
Recognize fads (nonevidence-based diets/supple-ments).
Understand when/how to refer patients to a qualified Registered Dietitian Nutritionist (RDN) or other professional and know the content of that consultation.
Recognize and plan for personal nutrition, physical activity, and wellness.
Case study 2: nutrition education for medical students in rural areas, University of Mississippi
Mississippi is a rural and poor state with multiple health and healthcare challenges, whose residents could benefit from changes in dietary practices and improved access to affordable healthy food. In 2016 the University of Mississippi Medical Center restarted the Department of Preventive Medicine, residing in both the School of Medicine and the John D. Bower School of Population Health. The Department of Preventive Medicine aims to transform health care into a system that values prevention over cure, effectively addresses psychosocial, behavioral, and community factors that influence health, and implements evidence-based interventions for populations as well as individuals. Central to the departmental mission is a commitment to educate medical students and residents regarding nutritional factors that predispose people to chronic diseases, particularly residents in rural, underserved areas.
Led by the Population Health Education Workgroup, nutrition education courses and experiential learning activities were added across all 4 y of UME. The revised curriculum draws from the social science literature in rural health and best practices in competency-based nutrition education, including the NIM program. Nutrition was integrated into organ system education for first-year and second-year students, use of standardized patients was employed during the third year, fourth year students participated in competitions that involved interdisciplinary clinical cases with nutrition content embedded within them. Practice opportunities were designed to increase student awareness of community-based nutrition resources and services.
Medical Education Evolution from Knowledge Acquisition to Knowledge Application: UME to GME—Role and Implementation of Entrustable Professional Activities
Changing paradigms in medical education foster high standards of learner achievement and success. These evolving concepts affect learners across the continuum of medical education and, therefore, it is important to consider the entire continuum from UME to graduate medical education (GME) and continuing medical education (CME). In 1990 Miller (20) described a pyramid of 4 stages of clinical competence showing progressive accomplishments: knows (fact gathering), knows how (interpretation/application), shows (demonstration of learning), does (performance integrated to practice). Miller's pyramid has aided educators in thinking about learner assessment where knowledge is primary in the first 2 levels, and behaviors or skills are embedded in the upper portions of the pyramid.
As the concepts of assessment tied to achievement have progressed, new nomenclature has been identified. The ACGME established 6 competencies (patient care, medical knowledge, systems-based practice, practice-based learning, professionalism, and interpersonal and communication skills). There are additional subcompetencies to further define developmental progression in specific areas.
Entrustable professional activities (EPAs) are those activities or specific tasks that define a profession or specialty related to a particular role (21). EPAs were developed across various disciplines in GME, and the AAMC has established 13 core EPAs related to the completion of UME for those entering residency (22).
All of the gastrointestinal societies (the American Association for the Study of Liver Diseases, the American College of Gastroenterology, the American Gastroenterological Association, the American Neurogastroenterology and Motility Society, the American Society for Gastrointestinal Endoscopy, and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition) in a group called the Oversight Working Network, convened to create EPAs for gastroenterology, hepatology, and nutrition. Based on the gastrointestinal Core Curriculum, it accounted for changing paradigms in medical education, health care, and technology (23). In total, 13 EPAs (24) were identified including 1 specific to nutrition: “Assess nutritional status and develop and implement nutritional therapies in health and disease” (25).
Each EPA includes the following: title, detailed description, behaviorally anchored objectives in knowledge, skills, and attitudes, a list of ACGME competencies related to the EPA, the list of reporting milestones to achieve mastery, the time expected to achieve a level of unsupervised practice, suggested assessments, identification of who will make the entrustment decision, and finally, implications of entrustment. A toolbox was created to assist evaluators of trainees to aid in tracking, evaluation, and required reporting.
Program directors can use the Nutrition EPA to tailor educational curricula to fit within a particular program's framework. Flexibility exists to create educational programming that allows trainees to achieve mastery in the patient setting, in simulated exercises, in online training, or in case-based sessions that might include interprofessional partnerships. Similarly, assessments can be designed that conform to the technological capabilities of the educational program and personalized to the program and trainee.
Examples of assessment using curricular elements include:
clinical rotations: direct observations;
standardized patients: 360° evaluations;
case-based conferences: chart-stimulated recall;
online modules: chart audit;
national courses: in-training examination, patient surveys.
EPAs have a great advantage of being competency-based and EPAs promote individualized and personalized education. Creating EPAs across societies provided an opportunity to define the tasks of the profession. Some challenges were identified, particularly embracing change with reflection on new paradigms in education and assessment. The greatest challenge appears to be identifying the ideal assessments to evaluate learner achievement of each EPA's objectives. The ideal assessments are competency-based, and several steps must be considered: 1) Agreeing on what competency is required; 2) Setting milestones that mark progress toward competency; 3) Transitioning from a culture of largely norm-based assessments to criterion-based assessments; and 4) Addressing challenges associated with direct observations of learners (26). This is an opportunity for experts in specific areas, such as nutrition, to contribute to these efforts to ensure that learners and practitioners are skilled and demonstrate competence in these key areas. Figure 1 illustrates these concepts.
FIGURE 1.
A competency-based educational model rather than knowledge alone, competency in application is prioritized. EPA, entrustable professional activity; OSCE, objective structured clinical examination. Adapted and reproduced with permission from (41).
Survey Results in US Medical Schools: What Do Medical Students Need to Know?
In 2012–2013 Adams and colleagues sent a survey to 133 accredited medical schools to identify nutrition content taught across the 4 y of medical school (27). Only 22 (18%) medical schools had a nutrition course. Nutrition taught in UME averaged <20 h, below the 25 h recommended by National Academy of Sciences and 44 h by ASCN (renamed ASN). However, several schools dedicated more time through integrated courses and clinical practice sessions. Eight (6%) medical schools offered >40 h of nutrition education. An average 6.4 h was devoted to clinical practice in only 55 (45%) medical schools that required any clinical practice sessions. Although many schools have nutrition electives, few interested students attend them. Recent unpublished data from the same group has shown no improvement in nutrition education. Thus, “many US medical schools still fail to prepare future physicians for everyday nutrition challenges in clinical practice” (27). Key challenges include the limited number of 1) nutrition providers (e.g., physician nutrition specialists, RDNs) that serve as role models for interprofessional collaboration; and 2) clinics/nutrition services that are accessible to medical students and offer a worthwhile training environment.
In response to these survey findings, the International Association for Medical Science Educators (IAMSE) recognized the need to improve nutrition training and assessment of medical students, and a Nutrition Advocates working group was formed. In 2015 they updated the NAA learning objectives (28) by reorganizing the objectives into 11 categories based on a Core Nutrition Classification proposed at the 2012 NIH workshop and published in 2014 (5). The objectives were revised and simplified, resulting in 92 amended objectives. A survey assessing whether medical students should meet specific learning objectives/outcomes by the end of UME was distributed to IAMSE members and identified nutrition educators. A total of 67 responses from a combination of basic scientists, dietitian/nutritionists, and physicians were returned. Based on these survey results, several objectives were rewritten, and 9 were deleted because of redundancy or lower importance. In addition to the final 83 learning objectives, the IAMSE Nutrition Advocates also identified 1 overarching goal to help focus future efforts: “All graduating medical students will assess nutritional status and manage the clinical encounter to facilitate a personalized nutritional approach for optimal health.” This goal and learning objectives have recently been published in Medical Science Educator (29).
ASN's Nutrition Education in Professional Schools Committee became aware of IAMSE's efforts, and in 2016 a collaboration was formed to conduct a more expansive survey encompassing multiple nutrition interest groups. The ASN survey used the same 11 categories to classify the objectives. Through committee discussion, the initial (NAA) and amended (IAMSE) objectives were reviewed and consensus gained on 101 objectives to include in the survey. Although “nutrition champions” (internal advocates within the existing medical schools) may be teaching in UME, many are not part of the official teaching faculty. In addition, many nutrition champions are members of ASN's Medical Nutrition Council and may be clinicians, educators, and/or advocates. Therefore, the questionnaire was distributed to 153 accredited US medical schools and 41 schools of osteopathic medicine champions (n = 194) via the NIM network of nutrition champions and to members of ASN's Medical Nutrition Council (n = 2046). Nutrition champions from accredited schools were also asked to survey medical students for feedback, including schools with student nutrition clubs. Data collected included individual age, sex, profession, role in the medical school, years in practice, years in curriculum development, and inclusion of nutrition in various years of curriculum and electives. Participants were asked whether all medical students should meet the learning objectives/outcomes within the 11 categories by the end of their UME. Institutional Review Board approval was obtained, and data were analyzed using STATA (version 12.1).
A total of 147 individuals completed the ASN and IAMSE collaborative survey. Not all participants responded to each question. Among 117 respondents, 66% were women. A total of 120 individuals provided information on their professional status (120 of 147) (Table 1). Of 112 respondents, 30% were course directors, 42% were course/curriculum developers, and 82% were faculty (instructor to professor level). About 44% of 118 respondents had >20 y of practice and 33% had 5–20 y of experience with a nutrition curriculum. Only 20% of 114 respondents mentioned that nutrition was included in all years of medical school in their institution, and 17% reported that it was included in the clinical years. For each of the 11 categories used to classify the objectives, respondents recommended dropping an average of 3–7% of the nutrition objectives proposed and rewriting 1–4% of the objectives. Although the number of objectives to be retained without modification was similar between students and faculty, for some objectives, student responses varied from those of faculty. For example, counter to faculty responses, students were supportive of retaining the following objective: “Explain how the physician can be more involved in nutrition in the community.” Thus, student attitudes and opinions must be considered in any effort to modernize the education of the next generation of physicians. Feedback from this survey will inform the final NAA curriculum guide objectives and provide the basis for future competences and assessments of medical trainees. Finalized objectives are expected in 2019–2020 to support the future work of a coordinating center.
TABLE 1.
Professional status in the IAMSE survey (percentage of each survey total sample)1
| Professional affiliation | IAMSE (n = 67) | ASN/IAMSE (n = 147) |
|---|---|---|
| MD | 20 (30%) | 27 (18%) |
| Basic sciences | 29 (43%) | 34 (23%) |
| RDN | 27 (40%) | 47 (32%) |
| Trainees | 0 (0%) | 15 (10%) |
| Other | 10 (15%) | 27 (18%) |
| No response | 4 (6%) | 27 (18%) |
Each of the respondents may have >1 profession. In the other category, respondents included, for example, “faculty who worked together.” ASN, American Society for Nutrition [renamed from American Society for Clinical Nutrition (ASCN)]; IAMSE, International Association for Medical Science Educators; MD, Medical Doctor; RDN, Registered Dietitian Nutritionist.
Learning to Reconcile Old Dogmas with New Concepts?
A major challenge in clinical practice is reconciling the conflict between previously established knowledge and emerging information. Medical nutrition educators teach solid foundations and current guidelines while preparing learners for new concepts just over the horizon. They accomplish this by strengthening critical thinking skills, encouraging questions on both old and new claims, and illustrating the importance of lifelong learning. A key message is that best practice must constantly realign with new scientific insight and clinical evidence. In medicine this “scientific uncertainty” is met with excitement as being at the cutting edge of evidence-informed practice, an approach likewise central to the interface of nutrition and medicine.
For example, precision nutrition acknowledges that each individual has unique dietary needs, requiring the mix of new “omics” technologies (genomics, metabolomics, microbiome, and more) to match specific preventive and therapeutic strategies. There are many opportunities throughout the preclinical and clinical curriculum to better understand nutritionally relevant molecular structures, functional mechanisms, and metabolic pathways, and how they are affected by both nutrition and common genetic variants. Similarly, the community of intestinal microbes is unique in each individual and influences the individual's response to dietary changes. When trainees are introduced to these concepts early on, it simplifies their capacity to keep up with emerging findings and translate them more readily to clinical practice.
This lesson was learned from the NAA experience where medical students increased nutrition knowledge and self-efficacy over the 4 y of the NAA and the strongest predictor of the highest USMLE scores was taking a nutrition course before starting medical school (4, 6, 30). The workshop participants agreed this would undergird a focus on nutrition in pathophysiology, public health, precision medicine, and other specialty areas in medical school.
Developing a Competency-Based Nutrition Curriculum: Examples from the Obesity Curriculum with Local and International Approaches
A competency-based obesity curriculum to prevent and treat obesity was developed by the Bipartisan Policy Institute in collaboration with many stakeholders and partners (31). Major provider competencies include core obesity knowledge, interprofessional obesity care of patients, and patient interactions related to obesity. An analogous process to develop a competency-based nutrition curriculum could include:
define terms, scope, and application;
identify and engage diverse stakeholders;
collect data;
draft nutrition competencies for stakeholder review;
apply the competencies, e.g., Curricular Design, Process Improvement, Program Evaluation;
periodically review and provide updates.
Using these steps, nutrition competencies could include identification of major nutritional deficits in the US population, description of the contribution of diet to chronic diseases in the United States, use of evidence-based care for the delivery of dietary needs of inpatients and outpatients, and development of skills necessary for interprofessional collaboration for nutritional management. Existing examples of schools with UME nutrition competencies include Northwestern University Feinberg School of Medicine and at Deakin University, Australia, in collaboration with other partners.
Case study 3: UME lifestyle medicine thread, Northwestern University
Feinberg School of Medicine
Northwestern University Feinberg School of Medicine underwent curricular renewal in 2012 following the shifting focus promoted by the AAMC towards competency training (22). The traditional 4-y structure of medical education was replaced with 3 competency-based phases organized by 4 elements (science in medicine, clinical medicine, health and society, and professional development) and 5 threads (healthcare quality and patient safety, health equity and advocacy, medical decision-making, teamwork and leadership, and lifestyle medicine) (32). Lifestyle medicine, including assessment/counseling for diet/nutrition, physical activity, smoking, alcohol, stress, and weight management, became a thread as these health behaviors are primary contributors to noncommunicable diseases (NCDs) (33). The practice of lifestyle medicine requires interrelated skills and competencies to address multiple health risk behaviors. Thus, diet/nutrition was integrated throughout the curriculum as 1 component of the lifestyle medicine thread (34).
During phase 1, the first 20 mo of medical school, including 13 organ-based modules, diet/nutrition is addressed within 78 different sessions. Using this model, students are sequentially exposed to nutritional concepts that are pertinent to the basic science, clinical care, or population health aspects of the various organ systems. For example, the endocrinology module presents appetite regulation and energy balance, the method for taking a body weight history (35), and the global impact of obesity as a contributor to NCDs. As part of the thread, students also complete a personal behavior change plan, experiencing the process and principles of behavior change while striving to improve their own health (36).
Case study 4: development and future for competency-based nutrition curriculum in Australia
To address the lack of nutrition content in medical courses in Australia (37), an expert group developed a set of 9 nutrition competencies (2009–2011) specifically designed to be easily embedded into draft competency-based Standards for Assessment and Accreditation of Primary Medical Programs by the Australian Medical Council (ratified 2012) (38). These competencies (4 knowledge-based and 5 skills-based) were circulated to educators, the Royal Australian College of General Practitioners, and the Dietitians Association of Australia for feedback. As part of a national teaching award, in collaboration with Monash University, the Universities of Queensland and Tasmania, and the Dietitians Association of Australia, a web-based Nutrition Competency Implementation Toolkit was designed to embed nutrition into the medical curriculum (39). In the Toolkit, competencies were detailed to provide more information on suggested learning objectives, examples of learning activities, and assessment methods, including a bank of appropriate multiple choice examination questions.
The number of competencies was restricted, and simple language was used for easy communication. The nutrition competencies were designed to align with the existing framework required for medical course accreditation and interprofessional competency statements. Feedback indicated that the basic nutrition competencies should not be overly prescriptive and should be readily integrated within a variety of different curricula structures across the learning continuum. They need to be flexible with respect to a range of practice settings and must link to learning activities, and behavioral assessments should be developmentally appropriate for learners at different stages. A future research challenge is to develop and evaluate robust student competency evaluation tools, particularly for practical tasks, with feedback to facilitate the development of nutrition competencies throughout the different stages. Lifestyle medicine has emerged as a systematized approach for the management of chronic disease, encompassing nutrition, physical activity, and mental health. Accordingly, medical schools may be more receptive to embedding nutrition into the curriculum as a component of a cohesive lifestyle medicine program. The student competency domains related to assisting patients to address physical activity and mental health issues are similar to nutrition. There is a research gap to develop common frameworks to evaluate competencies and to assess the impact of producing “lifestyle competent” health professionals on patient lifestyle behaviors and health status. There are significant advantages in linking nutrition competencies with exercise and mental well-being professionals’ education to develop 1 common set of competencies for medical, nursing, and allied health graduates.
The Need for Nutrition Education/Innovation Program, Australia/New Zealand network (NNEdPro NZ) is a collaboration among dietitians, doctors, academics, medical and healthcare educators, researchers, students, and professional associations in the region, linked with the NNEdPro Global Centre in Cambridge, United Kingdom, to build collaborations and initiatives to advance nutrition education. An action plan was developed at a recent workshop (December 2017) (40), encouraging medical schools to map the nutrition competencies of their medical curriculum, and NNEdPro is developing a plan to evaluate the impact of nutrition educational initiatives. Coordinated efforts across the health professions to embed lifestyle competencies during training and evaluation of the impact of increased student lifestyle competencies on patients’ health are necessary to progress this area and ultimately reduce health inequalities (41).
Nutrition in Accreditation and Licensure
The role of the USMLE
Sponsored by the Federation of State Medical Boards and the NBME, the USMLE is a 3-step examination for medical licensure in the United States that assesses a physician's ability to apply knowledge, concepts, and principles, and to demonstrate fundamental patient-centered skills that are important in health and disease and that constitute the basis of safe and effective patient care. Since 2003, “nutrition” has been a reported score category on the USMLE Step I examination and was subsequently included in the subscore domain of “biochemistry” since 2016. Further, nutrition content is represented on the Step II Clinical Knowledge and Step III examinations as a cross-content area within ICD-9 coded diagnoses (e.g., feeding and nutrition issues, nutrition and digestive system disorders, foundations of independent practice domains). Nutrition content is further represented in the Step II Clinical Skills examination in the domain of “health behavior change.”
The inclusion and design of nutrition questions and how they are monitored are primarily driven by the USMLE content outline. This is the basis for the examination material created by the NBME's national faculty of medicine, a representative group of medical educators, practicing physicians, and state medical board members. On a periodic schedule, at least 2 committees critically appraise each test item or case in the USMLE. Material that performs poorly on the examination series or is outdated is discarded. Of note, nutrition-related content is specific to >10 areas of the content outlined across the lifespan and disorders. Periodically, the USMLE program grants requests to review the content of the examination series to external specialty interest groups, including those in the area of nutrition. Similarly, in 2015, the American Board of Obesity Medicine and The Obesity Society reviewed the exams for obesity-related content and made recommendations for improvement to promote more balanced testing of knowledge in obesity. Because of these recommendations and others made over the past 3 decades, the USMLE program responded by enhancing recruitment of additional test committee members with nutrition expertise and attempting to improve cross-content area representation on the exams.
The role of the LCME
The LCME is recognized by the US Department of Education as the reliable authority for the accreditation of US medical education programs leading to the Medical Doctor (MD) degree. As of 1 March, 2018, there were 151 LCME-accredited allopathic medical education programs in the United States that enrolled approximately 81,000 medical students and an additional 17 programs accredited by the LCME in Canada. Allopathic programs must be accredited by the LCME for their graduates to be eligible for postgraduate (residency) training, and medical/osteopathic licensure.
The LCME evaluates an educational program's performance against 93 Elements organized under 12 Accreditation Standards (42). For the most part, the Standards and Elements are nonprescriptive to allow programs flexibility in using resources and expertise, and tailoring the educational program to meet the strengths of the educational environment and the school's mission. The LCME does have expectations that certain topics are covered but does not explicitly specify where in the curriculum or “how much is enough.” Adequacy and effectiveness are determined by outcome measures (such as USMLE) and student satisfaction data.
Standard 7, Element 7.1, requires programs to include content from biomedical, behavioral, and socioeconomic sciences, as applicable to the health of individuals. The data collection instrument for Element 7.3 documents and assesses the location and impact of nutrition as taught in the curriculum. The LCME also queries programs about nutrition curriculum in an annual survey instrument. Data from those surveys document that nutrition content is required within preclinical and clinical courses. Neither the accreditation data collection instrument nor the annual surveys identify or define the actual content, quantity, learning objectives, or assessment measures for nutrition subject matter in the curriculum.
Potential research areas might include 1) student assessment methods used by schools for the nutrition curriculum, 2) granularity on nutrition curriculum content and methods of curriculum delivery, 3) measuring effectiveness of nutrition curriculum on knowledge and skills imparted by nutritional curricula, and 4) GME program satisfaction with postgraduate year 1 resident regarding nutrition education, and how that might relate to medical school curriculum content.
The role of the ACGME
Nutrition, dietary behavior, and societal influences are major contributors to the development of chronic diseases such as obesity. Despite rapidly increasing rates of obesity in both children and adults, many physicians and other healthcare providers do not have the skills necessary to intervene in this epidemic.
The ACGME sets standards for US GME programs and the institutions that sponsor them, and renders accreditation decisions based on compliance with the standards. Accreditation provides assurance that sponsoring institutions and programs meet the quality standards to prepare their graduates and physicians of the future to provide good patient care. The ACGME provides accreditation to 830 sponsoring institutions, including 11,214 programs with 135,326 medical residents and fellows (including fellows whose combined focus can involve clinical practice, research into public health and/or advocacy) and 176,616 faculty members. Although obesity permeates all levels of society and the entire age spectrum, and therefore all specialties, it may be best to direct initial GME training for nutrition dietary behavioral intervention and the treatment of obesity toward the primary specialties including pediatrics, family medicine, and internal medicine. As of December 2018, there were 1350 primary specialty programs, with 48,967 residents and 35,960 faculty (ACGME Data Resource Book Academic Year 2017–2018).
Common and specialty program requirements ensure that medical residents and fellows are provided with a curriculum and clinical environment that ensure sufficient exposure to the diagnostic and therapeutic methods of the specialty. In addition, programs are required to provide clinical experiences and didactic education in preventive health, acute and chronic disease management, and access to longitudinal continuity experiences. Furthermore, medical residents must demonstrate knowledge of established and evolving biomedical, clinical, epidemiological, and social-behavioral sciences, as well as the application of this knowledge to patient care. However, specialty program requirements are written in more general terms without listing every single disease state nor providing a comprehensive list of therapeutic modalities.
The proposed role of ACGME in medical residency and fellowship education in nutrition, dietary behavior and the treatment of obesity is 2-fold.
Dissemination of knowledge through the creation of a “microsite” within the ACGME website. This mechanism successfully provided educational modules for specific topics such as physician wellness, milestones, clinical competency committee, and self-study. In addition, ACGME has a newly established Department of Distance Learning that can create learning modules, video clips and other educational activities for use by medical residents, fellows, and program faculty. This format can provide educational modules in nutrition and obesity to a wide audience.
Creation of a new subspecialty in nutrition and obesity under the primary specialties of pediatrics, family medicine, and internal medicine. ACGME accredits programs in subspecialties that demonstrate that the clinical care of patients and their safety will be improved through accreditation of training in that discipline. Creation of this new subspecialty has several purposes including advanced training that will lead to subspecialists and leaders who will improve the care of patients with obesity, and the education of others who are involved in the care of such patients. Other benefits include focused and standardized care such that medical fellows who complete subspecialty training will share a common foundational knowledge base and skill set in the management of nutrition and obesity.
The panel recommended justification for and benefit derived from a board-certified ACGME-approved subspecialty in nutrition and stated it would advance progress in addressing many of the gaps and limitations in medical nutrition education and training. It further raises awareness regarding the importance of qualified faculty to teach, train, and grow the nutrition focus and develop new career paths. If the leadership and programs are in place, medical students, residents, and other professionals will come. An example is the University of Colorado School of Medicine where fellowship training in Pediatric Nutrition and Obesity/Lifestyle Medicine that follows ACGME guidelines has proven successful with more applicants than positions available.
Interprofessional Nutrition Education
Behavioral science competencies
In 2004, the Institute of Medicine (IOM) summarized how UME curricula should be enhanced to address critical health issues facing the United States today (43). Approximately half of all causes of mortality in the United States are linked to social and behavioral factors such as smoking, diet, alcohol, sedentary lifestyle, and accidents (44), but <5% of the 2 trillion dollars spent on health care annually in the United States is devoted to reducing behavioral and social risk factors (45, 46).
The IOM further reported that most US medical schools do not provide curricula sufficient to teach these behavioral and social risk factors. In response to the IOM report, the NIH awarded grants to 9 medical schools to develop, pilot test, and disseminate behavioral and social sciences integrated curricula across 6 domains: 1) Mind–Body Interactions in Health and Disease, 2) Patient Behavior, 3) Physician Role and Behavior, 4) Physician–Patient Interactions, 5) Social and Cultural Issues in Health Care, and 6) Health Policy and Economics. In all of these areas, nutrition education is vital. Collaborators and curricular innovations are described in detail elsewhere (47).
Briefly, some innovations specific to diet and exercise include: 1) inpatient rounds that include an assessment of nutrient needs and/or interventions associated with discharge care; 2) use of interprofessional teams in student-run health clinics to consistently address nutrition and exercise with every patient seen; 3) involving medical residents in hiking programs with children from local elementary schools and providing a healthy lunch; and 4) having students map neighborhoods’ fast food locations, community gardens, and exercise areas.
Research gaps include: 1) data documenting physician interventions and patient outcomes related to changing diet/exercise behaviors; 2) data comparing educational designs and dose-timing effects to document the importance of nutrition; 3) data resulting from novel strategies to activate physician–patient interactions; and 4) results derived from “collaboratories” among medical schools to study and identify best educational practices for improving patient outcomes.
Nutrition and dietetics professionals; RD/RDNs: competencies in team-based care, an interprofessional approach
Identifying potential gaps
The Academy of Nutrition and Dietetics is the largest association of food and nutrition professionals in the United States, representing more than 100,000 RDNs, registered nutrition and dietetic technicians, and advanced-degree nutritionists, and is committed to improving the nation's health through food and nutrition across the lifecycle (48). The Academy's position is that RDNs should play a significant role in educating medical students, residents, fellows, and physicians in practice (30). Training of medical students involving interaction with RDNs develops competencies in addressing the preventive and therapeutic role of nutrition throughout the lifecycle and recognizing the importance of the MD/RDN collaborative effort. Addressing the following gaps in competencies may support interprofessional practice and better meet the nutrition needs of patients served:
Underuse of RDNs' interprofessional education and care: despite strong evidence documenting the value of nutrition interventions/counseling provided by an RDN as part of the healthcare team in improving patient outcomes (49), RDNs remain highly underused in both interprofessional education and interprofessional care. Medical students benefit from opportunities to interact with RDNs and nutrition and dietetics students as part of their education to practice interprofessionally on graduation. The goal is not to become nutrition experts, rather, to understand the value of referral to RDNs and best to leverage their expertise as part of the healthcare team and augment the physician's care of the patient.
Payer coverage of nutrition services provided by RDNs: medical providers often operate under an outdated, incorrect assumption that payment for nutrition services does not exist. On the contrary, Medicare coverage for patients with diabetes, nonend stage renal disease and postrenal transplant has existed since 2001, yet only 5% of the >12 million Medicare beneficiaries with diabetes are provided (30).
Medical Nutrition Therapy: benefits of nutrition counseling have evolved, especially in the private payer world. Competency in applying these fundable and essential referrals to RDNs is a crucial skill for achieving best patient outcomes (30).
Skills in making referrals and activating patients towards seeking RDNs: medical providers benefit from understanding the full range of RDN services to effectively prescribe for their patients the benefit and need to follow-up on referrals (50).
Coding for nutrition services: medical providers need basic knowledge about coding for nutrition services as part of their practice management competencies.
The role of RDNs and nutrition services in value-based payment models: medical providers who learn how to apply these models to support and pay for RDN nutrition services benefit patients. Data show financial viability in having an RDN on the team, especially in category 2, 3, and 4 payment models (51).
Nutrition services advocacy: medical education should advocate strategies for nutrition services coverage at the patient, practice, and/or healthcare system level.
Finding an RDN: medical education starts with recognizing the value of the RDN on the team and how best to recruit the appropriate RDN expert for the team.
Other interprofessional organizations have developed their own goals and objectives as well.
Oral health
Relations between nutrition and oral health are abundant and relevant to overall health. Oral problems including dental caries, tooth loss, and oral soft tissue and oral bone infections are major risk factors for malnutrition, choking risk, and even potentially fatal systemic infection. Research provides clear, irrefutable evidence that dietary and nutritional factors, in conjunction with oral flora, are the essential etiologic factors in dental caries (the most prevalent disease of children to age 19). New evidence of relations between systemic nutrition and oral soft tissue and bone health and disease is continuously emerging (52).
Consequently, schools of dental medicine and dental hygiene have taught nutrition in some form since the earliest recognition of relations among nutrition, oral health, and disease (53). The importance of these relations is formalized through position/policy statements from both dental and nutrition professional organizations, and through related accreditation standards. Nevertheless, ensuring that nutrition is included in dental curricula in a meaningful way has been a consistent challenge (53). Many system-wide issues contribute to this difficulty:
Nutrition is not a traditional core subject in dental education, which now favors more general outcomes/competencies. Few practice models and curricular road maps exist. Accreditation guidelines for dental hygiene schools are more prescriptive than for dental schools, whereas guidelines for dental school outcomes relate only to basic science education requiring that the “graduate must be competent in oral health promotion and disease prevention for all age groups.” Nutrition is implied but not named.
Faculty available and qualified to teach nutrition in dental and dental hygiene schools are rare or nonexistent. Various faculty including biochemists, oral biologists, general dentists with an interest in nutrition, and on-site dental hygiene faculty typically fill these roles, but nutrition knowledge and skills vary widely and may conflict. Ideally, an RDN with core skills in direct patient care is best suited to this role, but few nutrition professionals have training in oral health.
For nutrition teaching to be meaningful in dental education, graduates must be able to apply their knowledge. Students need to be as “comfortable” discussing nutrition as they are discussing oral hygiene or fluoride (54).
Incorporating nutrition into patient care requires an “applied nutrition” curriculum, including interviewing and counseling skills, as well as nutrition science (55).
Interprofessional education offers effective training in applied nutrition and an integrated curriculum including nutrition science, dental science, communication skills, applied nutrition, and clinical practice.
Physical activity
In addition to nutrition training, educating health professionals in the clinical knowledge, skills, and attitudes regarding physical activity for health benefits, a key component of Lifestyle Medicine, is essential for decreasing lifestyle-related chronic disease morbidity, mortality, and economic burden. The definition of physical activity is “any bodily movement that increases energy expenditure”; structured exercise, a subcategory of physical activity, is “planned, structured, repetitive and intentional movement intended to improve or maintain physical fitness” (56). Both physical activity and exercise may be used to maintain wellness and reduce the risk of chronic diseases.
Physical activity competencies for medical professionals should include: 1) physical activity assessment; 2) exercise prescription and implementation, 3) exercise counseling and behavioral strategies; and 4) self-care for the physician.
Physical activity assessment
To provide health benefits and lower risk of NCDs, the 2008 Physical Activity Guidelines for Americans (57) recommendation is for all adults to perform at least 150 min/wk of moderate-intensity or 75 min/wk of vigorous-intensity, aerobic activity, and moderate-intensity or high-intensity muscle-strengthening activities involving all major muscle groups on ≥2 d/wk. In addition to encouraging patients to follow these guidelines, screening for physical activity behaviors should be implemented at every patient visit through a physical activity vital sign (58).
Exercise prescription and implementation
The “FITT” Principle (frequency, intensity, time and type) is the most common and acknowledged method to effectively prescribe exercise and implement into a patient's lifestyle. Frequency: How many times per week; Intensity: low, moderate, or vigorous, Time: how long every session; and Type: walking, jogging, bicycling, etc., are ways to prescribe and implement exercise for optimal results.
Exercise counseling and behavioral strategies
Tools to implement physical activity and exercise into patients’ lifestyles include using the Transtheoretical Model Stages of Change, Motivational Interviewing, and Shared Decision-Making for both the healthy ambulatory patients and especially for patients with or at risk for chronic disease. Special conditions and populations (e.g., children and adolescents, older adults, disabled individuals, pregnancy, obesity, cancer) must be taken into consideration.
Self-care for the physician
Physician burnout is prevalent in health care, with >50% of physicians reporting symptoms of burnout. The Healthy Doc-Healthy Patient study also demonstrated that physicians who have a healthy lifestyle are also more likely to counsel their patients on adopting and maintaining a healthy lifestyle. Therefore, physical activity and exercise should be promoted by physicians and to physicians alike (59).
The University of South Carolina School of Medicine Greenville was the first medical school to require all undergraduate medical students to obtain training in nutrition, clinical exercise physiology, sleep hygiene, self-care/stress management, behavior change, and other lifestyle medicine components as part of their curriculum (59). For medical schools wishing to adopt and implement lifestyle medicine training in their schools, the Lifestyle Medicine Education Collaborative (60) offers leadership, guidance, and resources in medical schools throughout the United States and internationally.
Nursing/NPs
Nutrition is an important practice component for nurses and NPs. The present state, challenges, and opportunities in terms of nutrition education and training for nurses and NPs is well-documented (6). A socioecological framework is used to identify education and training opportunities related to nutrition for nurses and NPs, review current nutrition-related practice initiatives that impact nurses and NPs, and identify areas for further research (61).
Individual level
Knowledge, attitudes, and beliefs are key individual level factors in any socioecological model. Standalone nutrition courses are “not mandated” by accrediting bodies for nurse training at the prelicensure level, but nutrition content is integrated into the curriculum as it is testable knowledge on the National Council Licensure Examination (6). An educational action item centers on development of a standardized nutrition curriculum for the varied NP specialty programs as formal nutrition courses are not taught at the graduate level. NP programs could enhance content on nutritional assessment, the integration of nutrition with acute and chronic disease management, the diagnosis of nutritional alterations, and the prescription of appropriate nutritional therapies. Standards of nutrition care practice and professional performance for nurses and NPs were recently published by the ASPEN Nurse Standards Revision Task Force (62). These standards differentiate competencies for nurses and NPs for the nutrition support nurse specialist and nonspecialist (generalist), and could serve as a framework for updated NP curricular threads. Finally, improving one's personal attitudes and beliefs toward nutrition and a healthy lifestyle could potentially impact patient care. In 2017 the American Nurses Association initiated the Healthy Nurse, Healthy Nation Grand Challenge to empower the 3.6 million American nurses to increase their personal wellness and that of their family, community, patients, and, ultimately, the nation. Components of the program include choosing nutritious foods and maintaining an active lifestyle. Future research could identify nutrition-related knowledge, attitudes, and practice patterns of the Healthy Nurse program participants.
Interprofessional level
Hospitals are the only healthcare settings where the majority of the interprofessional healthcare team provides care, including dietitians, nurses, NPs, pharmacists, physicians, PAs, and physical therapists (PTs). Nutrition is an important component of the care delivered in the hospital setting. The Joint Commission mandates that all patients receive a nutrition screen within 24 h of admission (63). In most hospitals, the initial screen is performed by nurses (64), and dietitians conduct in-depth nutritional assessment and recommend appropriate medical nutrition therapy. Healthcare professionals have numerous opportunities to integrate nutrition into care and services across the care continuum including wellness and fitness centers, retail pharmacy, physician offices and clinics, urgent care, diagnostic imaging centers, ambulatory procedure centers, emergency departments, inpatient rehabilitation, outpatient rehabilitation, extended care facilities, skilled nursing facilities, home health, and hospices. They should incorporate essential nutrition principles into health promotion and wellness activities, as well as acute and chronic disease management. Nurses/NPs should also know when referral to RDNs is necessary (64).
Organizational level
Professional organizations play a key role in developing and implementing nutrition practice standards in alignment with their missions. For example, ASPEN focuses on reducing the incidence of hospital malnutrition; their Malnutrition Solution Center houses important interprofessional resources (65).
Community level
The transition from hospital to home represents a gap in nutrition care. Patients undergo a nutrition screen at hospital admission, but there is no mandated requirement to conduct a nutrition screen upon discharge, nor a mandated requirement for home care nurses to perform a nutrition screening in the home care setting. Postdischarge malnutrition impacts hospital readmission rates (66, 67), but the true prevalence of malnutrition during the transition between hospital and home in the United States is unknown. Further compounding the issue is the limited number of dietitians who work in home care settings. At a recent National Academies of Science, Engineering, and Medicine workshop (68), DiMaria-Ghalili recommended that research should focus on integrating nutrition risk assessment into predictive models to determine the level of nutritional care postdischarge. Nutritional interventions in the postdischarge, community, or home care setting could be prioritized into 3 levels: high-risk nutritional interventions delivered by a registered dietitian, medium-risk interventions delivered by nurses, and low-risk nutrition interventions delivered by social workers or lay health community or home care workers. Some hospitals collaborate with home-delivered meal options to provide food postdischarge. Evaluative data are urgently needed.
Policy level
Strategic policy initiatives, such as educational program accreditation standards, credentialing or licensure standards, healthcare accreditation standards, or reimbursement regulations are badly needed. A 2015 commentary published by the ASPEN Malnutrition Committee in The Joint Commission Journal on Quality and Patient Safety called for a malnutrition-focused national goal to address the issue of disease-related malnutrition (69). Targeted messaging to key stakeholders of the importance of integrating nutrition principles in education and practice can help raise awareness, eventually impacting policy.
Osteopathic medicine, PAs, and PTs
Nutrition education in osteopathic medical schools
Nutrition education is integral to the distinct osteopathic philosophy and osteopathic physician (DO) training even more than in allopathic medical schools. There are 33 osteopathic medical schools and more than 108,000 practicing DOs in the United States, reflecting a 68% increase in the last 10 y according to the 2017 Osteopathic Medical Profession MP Report (70). DOs are licensed in all 50 states to practice the full scope of medicine. Graduate medical education doctors from both allopathic (MD) and osteopathic (DO) schools of medicine have merged and now compete for the same residency training programs and take the same national medical licensing examination (71). DOs may choose any medical specialty and often become primary care physicians, providing much-needed health care in underserved regions (70, 71).
The osteopathic curriculum is a 4-y postbaccalaureate program. Students learn preventive medicine, pharmacology, and surgery, with added training (>200 h) in osteopathic manipulative medicine. Nutrition education averages 25 h of lectures for allopathic preclinical curricula (72). DO nutrition curricula include strong biochemical and clinical components, reinforcing the role of nutrients in metabolism. Additional instruction includes nutritional assessment, patient education, and collaboration with credentialed RDNs.
In 2017, the Journal of the American Osteopathic Association published results of a survey of DOs (often the sole providers of patient nutrition education and counseling) stating that nutrition is often overlooked during office visits, with <10% of primary care providers offering weight loss counseling to their patients (73). Allopathic medicine has long recognized this problem and dedicated training in providing patients with nutrition awareness, especially as a component of preventive medicine. The MD and DO single graduate medical education accreditation systems provide new opportunities for curricular reform.
Nutrition education for PAs and PTs
The number of PAs graduating from 173 accredited programs is expected to increase in the United States. PAs, taught to treat the whole patient, value the importance of health promotion and disease prevention. PAs serve as partners to advocate for patient nutrition education. They receive graduate-level education in the basic sciences, and clinical skills, including initiation of nutritional assessment and diet counseling. Similar to nurses, NPs, and nursing assistants, PAs can make referrals to RDNs.
Surveys of PA students initially found that nutrition knowledge and attitudes were lower than expected (74, 75); however, this improved progressively with each year of PA education.
There are no specified requirements for nutrition education in PA programs as set by the Accreditation Standards for Physician Assistant Education; however, 10% of the national certification examination relates to gastrointestinal and nutrition questions (74). PA training programs are typically based in academic medical centers where establishment of a medical subspecialty in Nutrition and Obesity would support multiple Advance Practice Training programs including those for PAs.
PTs complete a doctoral degree program, and nutrition is a component of their professional scope of practice. Nutrition was included as an element of PT education in 2012 and added to the guidelines of the Commission on Accreditation for Physical Therapy Education. The American Physical Therapy Association (APTA) states, “the role of the physical therapist is to screen for and provide information on diet and nutritional issues to patients, clients, and the community within the scope of physical therapist practice.” The PT profession supports helping patients understand how nutrition affects function. However, each state has its own laws and regulations regarding how PTs can fulfill that role and who can legally provide nutrition counseling. Some states permit them to give nutrition advice, but only RDNs can charge or bill insurance. Other states require licensed RDNs to give nutrition advice.
The APTA web page, Nutrition and Physical Therapy, provides resources and links to state regulations and laws and states APTA's position that it is the role of PTs to “screen for and provide information on diet and nutritional issues…within the scope of practice for PT” (76).
Culinary medicine
The nutrition-related chronic disease epidemic requires enhanced education of healthcare professionals in assisting patients with nutrition. Pilot studies demonstrate efficacy of nutrition education interventions aimed at improving competencies among medical students. Yet their generalizability is limited by a lack of control comparison (77–85), validated survey metrics (77, 78, 82, 84), multiyear longitudinal follow-up (77, 79, 80, 82–84), and large sample size (77–81, 83, 84). Past studies (77–84) also fail to incorporate the most extensively supported diet for patients, including the Dietary Approaches to Stop Hypertension (DASH) and Mediterranean diets (85–87).
Simulation-based medical education with deliberate practice (SBME-DP) has been shown to be superior for skill acquisition in mastery learning (88). Culinary medicine programming addresses this disparity using SBME-DP through hands-on cooking classes as a platform for teaching healthcare providers positive food-related messaging that they can incorporate into their patient encounters. In a large sample of medical students, a multiyear prospective observational cohort study showed superiority of SBME-DP-style hands-on cooking and nutrition education elective over traditional clinical education for preventive medicine (89).
Culinary medicine SBME-DP programming extends to multiple educational and clinical settings for students including:
required hands-on culinary medicine programming offered at 3 medical schools;
multiple-module hands-on culinary medicine programming offered as electives;
standalone condition and disease-specific programming offered as optional programming;
medical student involvement and delivery of hands-on community cooking classes.
Growth has accelerated over the last 5 y with more than 35 medical schools, 3 nursing schools, and 9 graduate medical education programs offering Culinary Medicine programs nationwide. More than 40 of these sites are using courseware focused on the Mediterranean diet with translation for the American kitchen, as well as teaching healthcare providers practical strategies to effect change in their patients.
Nutrition Research and Training Needs and the Road to Sustainability
A major NIH goal is to develop, diversify, and sustain the scientific workforce. Research training of health professionals is an integral component of its mission. Within the various NIH institutes, training through career development and fellowships has been the hallmark of their mission, and many institutes have implemented strategies to enhance their training efforts. One example of such training is the previously discussed NAA program.
To examine federal funding of training of medical professionals in nutrition as a follow-up to the NAA, we reviewed the NIH portfolios from 2006 through 2017 using the search terms “nutrition and medical school,” “nutrition and primary care,” and “nutrition and residency training,” and then manually screened grants for relevance. We excluded training awards that were awarded to individuals (e.g., K awards) or training programs that trained scientists for research careers. We found 9 NIH-funded projects over the 12-y period that addressed the topic of nutrition training for medical students and health professionals. Four of the 9 NIH-funded projects used training mechanisms. This includes 2 T35 short-term research training projects that added an optional summer course to medical students’ curricula. The NIH also funded 1 T32 institutional national research service award on nutrition and obesity research training and 1 D43 international research training grant for a training program on nutrition and metabolism in HIV. These grants, while adding important nutrition-related topics that reached a portion of medical students, did not create permanent changes in the medical training of their recipient institutions.
Three of the 9 NIH-funded relevant projects were R25 short-term education projects to increase diversity in health-related research. Two of these R25 awards aimed to provide education in nutrition and cancer to medical students, residents, and preceptors and the remaining R25 award aimed to foster opportunities for nutrition and global health. The NIH also funded 2 R13 conference grants in this time frame. These conference grants provided funds to support scientific conferences. While scientific conferences have a large potential reach because of the number of participants, a major limitation of these grants is that they are funded for only 1 y and do not provide funds to sustain a training program. These results demonstrate that nutrition research training in the health professions represents an important need and an opportunity for investigators to address.
The T32 postdoctoral training fellowship offers an important opportunity for physicians to receive research training and preparation for future careers in academic medicine with a specific focus on nutrition/obesity/metabolism. Areas of nutrition research range from basic (T1) to translational (T4) research that offer outstanding faculty development opportunities for growth.
Recently, the NIH established a Nutrition Research Task Force to coordinate and accelerate progress in nutrition research and to develop a nutrition strategic research plan to be implemented within 10 y across NIH Institutes and Centers. Through crowdsourcing across NIH and the extramural community and meetings with thought leaders across the United States, 7 research themes emerged:
Investigate nutritional biochemistry, physiology, behavior, and the microbiome.
Assess the role of nutrition and dietary patterns in development, health, and disease across life stages.
Explore individual variability in response to diet to inform nutrition science, improve health, and prevent disease.
Enhance clinical nutrition to improve treatment outcomes in patients.
Advance research on implementation of nutrition-related programs, practices, and behaviors.
Develop and refine research methods and tools.
Support training to build an outstanding nutrition research workforce.
These themes have the potential to provide a strong foundation to train the next generation of researchers including medical and other health professionals in nutrition.
The following are examples of nutrition research and training interests identified by NIH staff who attended the workshop.
The National Institute on Aging's nutrition research and training agenda focuses on dietary interventions that have the potential to modulate aging changes, delay or prevent the occurrence of chronic conditions, and promote healthy aging. The National Institute on Aging's GEMSSTAR program supports training of early career physician-/dentist-scientists in aging research and/or clinical care of older adults (including diet and nutrition) using the R03 grant mechanism. The Butler-Williams Scholars Program provides training opportunities for junior faculty and researchers to gain insight about research on aging from different perspectives, including health disparities and nutrition.
The National Cancer Institute (NCI) supports preclinical and clinical research and training that covers the full range of the cancer continuum, from prevention to end of life. In fiscal year 2017 the NCI funded 377 grants and cooperative agreements involving nutrition research totaling $117 million. There are currently no targeted nutrition training solicitation programs; however, the portfolio of projects includes several grants that provide support to investigators at different stages in their careers including educational (R25) and training grants (T32) and career awards (K). Nutrition training may be provided via other mechanisms within larger research center grants (e.g., P01s, P30s, P50s). Funding opportunity announcements are available through the NCI's Division of Cancer Prevention (90).
The NHLBI is the second largest NIH funder of nutrition research. It supports basic and mechanistic nutrition research, nutrition epidemiology and population science, clinical trials, and translational research. NHLBI support of nutrition research has ranged from $221 million/y to $239 million/y over the past 10 y. The NHLBI supports academic and professional training in nutrition research as well as the development of innovative nutrition education programs for medical students, residents, attending physicians, and other healthcare professionals. Nutrition research topics of interest to the NHLBI that could form the basis for training health professionals include research that identifies the mechanisms and risk factors associated with cardiovascular-related, pulmonary-related, and blood-related diseases, nutritional assessment, nutrition interventions, and translational research (91). Applicants may use any of the existing grant mechanisms, including Educational (R25), Training (T32, T35), or Research Project Grant (R01). It is important to talk with a program officer about current funding opportunities before applying for funds.
Other organizations such as the US Preventive Services Task Force recommend that primary care physicians intervene or refer patients for intensive behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease (CVD) prevention, specifically for adults who are overweight or obese and have additional CVD risk factors. They reviewed evidence that demonstrated the effectiveness of intensive behavioral counseling interventions that often combined diet and exercise and took from 2 to 10 h in helping patients make small but important changes in health behavior and improvements in other intermediate outcomes over 1–2 y. The Task Force noted gaps in the delivery of these counseling interventions in the real world and commented that many such programs require resources that are not yet available. They suggested additional dissemination and implementation research to put these recommendations into current primary care practice. These resources are needed at all levels of primary care training from undergraduate to fellowship level (92).
Ongoing Sustainability
Nutrition education, training, and research (basic, clinical epidemiological) is a dynamic process and the need to refine mechanisms, address validated assessment methods, and formulate new guidelines is ever evolving. Achievement of this major effort requires collaboration among existing governmental and nongovernmental organizations and institutions that include strong nutrition committees/working groups specializing in specific topic areas and who publish in those areas. A few examples included in this workshop are noted below.
The AHA model: CVD diet competencies with tools, training, assessment, and applications to AHA “Simple 7” goals
The AHA routinely updates reviews of nutrition research to formulate guidelines that can be used in patient care and public health efforts (93–95). The AHA has also developed and validated the “Life's Simple 7” goals that include interprofessional efforts to facilitate adherence to a healthy diet as well as nonsmoking, physical activity behaviors, and meeting risk factor goals for blood pressure and blood cholesterol (96). The AHA has also included medical and integrative nutrition education efforts to facilitate training at the UME, GME, and CME levels (97). Taking full advantage of these activities and leveraging them to help spread the word interprofessionally can augment and strengthen the updated efforts to standardize nutrition messages across all medical specialty areas.
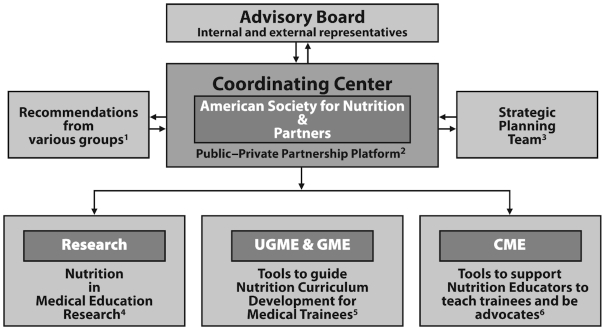
ASN: development of a coordinating center
For >3 decades, ASN has been advocating and publishing, as an organization and in partnership with governmental and nongovernmental organizations, on the topic of medical nutrition, metabolism, and lifestyle education and training as well as the ethics of public–private partnerships. Although there are multiple efforts in the United States and abroad to educate and train healthcare professionals in nutrition and physical activity, these efforts vary in focus and quality, are largely uncoordinated and partially redundant, and in some cases, compete. In 2014 the ASN and the NHLBI published recommendations for remodeling nutrition education (4, 5, 7, 98). Establishing a mechanism to coordinate the multiple stakeholders was identified as critical to advancing the medical nutrition education agenda.
Recently, the ASN Board approved an effort to seek funding to establish a coordinating center to guide the nutrition education of healthcare professionals. A planning committee defined the effort's scope, governance structure, and timeline, and completed a gap analysis. Over the past year, meetings have been held with key stakeholders including the AAMC, the LCME, governmental agencies, the National Board of Physician Nutrition Specialists, and groups that have successfully impacted medical education. Critical to advancing medical school education are:
Coordination of resources to collect, centralize, and distribute multidisciplinary educational resources, credentialing resources, and practice and reimbursement resources.
Community building to establish a network of key contacts at medical schools and medical and scientific organizations to increase organization of already available educational data, educational materials, examination questions, etc.
Confirmation of objectives with stakeholders to define provider competencies for medical schools and EPAs for residence programs.
Development of a career path through a recognized subspecialty in nutrition.
Capacity building to train “nutrition ambassadors” to conduct and consult on educational programs for healthcare professionals within and outside of the United States.
Research to identify and disseminate funding opportunities.
Advocacy for education, legislation, and/or research funding.
The September 2017 NHLBI workshop attendees acknowledged the need for improved coordination to advance a broad-based educational effort including identifying strategies to assess improvements in patient care and outcomes from coordinated activities.
Throughout the United States and abroad, interprofessional education has become an important approach advocated by various leading medical groups. Registered dietitians, nurses, NPs, PAs, pharmacists, dental hygienists, exercise physiologists, and others can positively affect patient care by providing and/or reinforcing nutrition metabolism and lifestyle education (6, 99). An effort to establish a coordinating center on medical nutrition, metabolism, and lifestyle education training and research is a precursor to a broader effort to collaborate on the education and training of all health professionals engaged in improving nutrition-related patient outcomes.
The proposed coordinating center will be directed by a leadership structure using multidisciplinary volunteers representing various medical and scientific societies. Optimally, all medical organizations concerned with nutrition (e.g., AHA, American Diabetes Association, American Academy of Pediatrics, American Gastroenterological Association, ASPEN, Academy of Nutrition and Dietetics, AAMC, IAMSE, and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition) will be engaged. The National Board of Physician Nutrition Specialists maintains credentialing standards for assessment and certification of physicians seeking recognition as a nutrition specialist. This group is committed to the education and training of nutrition faculty in medical schools and a critical partner in this effort. A proposed structure is displayed in Figure 2.
FIGURE 2.
Proposed leadership framework for an ASN-led coordinating center. 1Recommendations from groups such as USMLE, AAMC, societies, etc. 2Partners (e.g., foundations, nongovernmental organizations, government, scientific and medical societies, industry, individual donors). 3Strategic planning team includes education leaders familiar with EPAs and nutrition curriculum, administrative personnel, etc. 4Medical education research is overseen by ASN and partners. 5With its partners, ASN coordinates committees to develop tools to guide medical curriculum development for undergraduate and graduate medical education (e.g., EPA competencies, objectives), which are critical for interprofessional nutrition education and practice. 6ASN coordinates CME, mentoring, and implementation phase of projects with partners (e.g., CME, train-of-trainer, media, material links, mentoring, blog). AAMC, American Association of Medical Colleges; ASN, American Society for Nutrition; CME, continuing medical education; EPA, entrustable professional activity; GME, graduate medical education; UGME, undergraduate medical education; USMLE, US Medical Licensing Examination. Created by C.M. Lenders in cooperation with the ASN Nutrition Education in Professional Schools Committee.
Funding to establish this coordinating center is being sought from government, industry, and other public and private entities. ASN developed best practices for public–private partnerships involving governmental, nongovernmental, industry, and academic partners to address food and nutrition-related research challenges (100). Grant funding from governmental and nongovernmental organizations is proposed for outcomes-based research, education, and training in nutrition, metabolism, and lifestyles.
Conclusions and Next Steps
The workshop identified major avenues to advance the implementation of medical nutrition education in the United States and abroad, and to promote interprofessional nutrition education and better achieve a collaborative and complementary outcome. Consensus among workshop participants included the need for competency-based nutrition curricula, accreditation boards, integrative nutrition education across the health professions, and focus on selected NIH institutes’ interested in funding nutrition training. A collaborative leadership framework is proposed to guide the coordination of nutrition training within the United States.
The workshop underscored the need to develop, diversify, and sustain the scientific workforce by developing curricula and educational resources for healthcare providers. To achieve these efforts, the construct of a career path in nutrition that includes a board-approved medical subspecialty in nutrition is key to attracting faculty members who will build high-quality programs and trainees who want to follow their lead. This document is a resource for organizations with representation across various disciplines, including allopathic medicine, bioinformatics, dietetics/nutrition, family medicine, internal medicine, nursing, obesity and metabolic health, oral health, pediatrics, physical activity, population health, and surgery among others (101). Leaders from the NBME, the ACGME, the LCME, and other organizations are encouraged to collaborate in support for implementation of the proposed framework to enhance medical nutrition education, training, and research.
Acknowledgments
The authors’ responsibilities were as follows—LVH, CAP, CML: decided on content and wrote the manuscript; GT: supplied the figures; and all authors: contributed summaries of their workshop presentations and read and approved the final manuscript.
Notes
Presented at the Workshop, “Advancing Nutrition Training, and Research for Medical Students, Residents, Fellows, Attending Physicians and other Clinicians” held in Bethesda, Maryland, 7–8 September, 2017.
Supported by National Institutes of Health, National Heart, Lung, and Blood Institute, National Institutes of Health, Office of Dietary Supplements, National Institutes of Health, Office of Disease Prevention, American Society for Nutrition.
Author disclosures: CML: educational/research support at the time of this activity includes the New Balance Foundation, a public–private partnership (BUSM, BioQuest Global Solutions Pvt. Ltd, & Nutrition Nestle Institute–NNI), the Robert Wood Johnson Foundation, and the Boston Nutrition Obesity Research Center (P30 DK40561); RFK: currently on the Scientific Advisory Board for WW (formally Weight Watchers); EP: Co-Director of the Lifestyle Medicine Education Collaborative (LMEd), which has received program support from Ardmore Institute of Health, American Council on Exercise, Physicians Committee for Responsible Medicine, and Josiah Macy Jr Foundation; JLT: Co-Director of the Lifestyle Medicine Education Collaborative (LMEd), which has received program support from Ardmore Institute of Health, American Council on Exercise, Physicians Committee for Responsible Medicine, and Josiah Macy Jr Foundation. All other authors report no conflicts of interest.
Disclaimer: The content expressed in this paper is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, And Blood Institute, the National Institute of Aging, the National Cancer Institute, the National Institutes of Health, or the US Department of Health and Human Services.
Published in a supplement to Advances in Nutrition. The Guest Editors for this supplement were LVH, CML, and CAP, and each has no disclosures. Publication costs for this supplement were defrayed in part by the payment of page charges by the National Institutes of Health, Office of Disease Prevention, and the American Society for Nutrition. The opinions expressed in this publication are those of the authors and are not attributable to the sponsors or the publisher, Editor, or Editorial Board of Advances in Nutrition.
The Supplement Coordinators for the supplement publication were Charlotte A Pratt, National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD 20892, USA, and Gwen Twillman, American Society for Nutrition, Rockville, MD 20850, USA. Both Supplement Coordinators have no disclosures.
Abbreviations used: AAMC, American Association of Medical Colleges; ACGME, Accreditation Council for Graduate Medical Education; APTA, American Physical Therapy Association; ASCN, American Society for Clinical Nutrition; ASN, American Society for Nutrition [renamed from American Society for Clinical Nutrition (ASCN)]; ASPEN, American Association for Parenteral and Enteral Nutrition; BUSM, Boston University School of Medicine; CME, continuing medical education; CVD, cardiovascular disease; DO, osteopathic physician; EPA, entrustable professional activity; GME, graduate medical education; IAMSE, International Association for Medical Science Educators; IOM, Institute of Medicine (now called the National Academy of Medicine); LCME, Liaison Committee on Medical Education; MD, Medical Doctor; NAA, Nutrition Academic Award; NBME, National Board of Medical Examiners; NCD, noncommunicable disease; NCI, National Cancer Institute; NHLBI, National Heart, Lung, and Blood Institute; NIM, Nutrition in Medicine; NNEdPro, Need for Nutrition Education/Innovation Program; NP, nurse practitioner; PA, physician assistant; PT, physical therapist; RD, Registered Dietitian; RDN, Registered Dietitian Nutritionist; SBME-DP, simulation-based medical education with deliberate practice; UME, undergraduate medical education; USMLE, United States Medical Licensing Examination.
References
- 1. Pearson TA, Stone EJ, Grundy SM, McBride PE, Van Horn L, Tobin BW. Translation of nutritional sciences into medical education: the Nutrition Academic Award Program. Am J Clin Nutr. 2001;74(2):164–70. [DOI] [PubMed] [Google Scholar]
- 2. Van Horn L. The Nutrition Academic Award: brief history, overview, and legacy. Am J Clin Nutr. 2006;83(4):936s–40s. [DOI] [PubMed] [Google Scholar]
- 3. Kris-Etherton PM, Pratt CA, Saltzman E, Van Horn L. Introduction to nutrition education in training medical and other health care professionals. Am J Clin Nutr. 2014;99(5 Suppl):1151s–2s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kris-Etherton PM, Akabas SR, Bales CW, Bistrian B, Braun L, Edwards MS, Laur C, Lenders CM, Levy MD, Palmer CA et al.. The need to advance nutrition education in the training of health care professionals and recommended research to evaluate implementation and effectiveness. Am J Clin Nutr. 2014;99(5 Suppl):1153s–66s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kushner RF, Van Horn L, Rock CL, Edwards MS, Bales CW, Kohlmeier M, Akabas SR. Nutrition education in medical school: a time of opportunity. Am J Clin Nutr. 2014;99(5 Suppl):1167s–73s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. DiMaria-Ghalili RA, Mirtallo JM, Tobin BW, Hark L, Van Horn L, Palmer CA. Challenges and opportunities for nutrition education and training in the health care professions: intraprofessional and interprofessional call to action. Am J Clin Nutr. 2014;99(5 Suppl):1184s–93s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lenders CM, Deen DD, Bistrian B, Edwards MS, Seidner DL, McMahon MM, Kohlmeier M, Krebs NF. Residency and specialties training in nutrition: a call for action. Am J Clin Nutr. 2014;99(5 Suppl):1174s–83s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. National Research Council. Nutrition Education in U.S. Medical Schools. Washington, DC: National Academies Press; 1985. [PubMed] [Google Scholar]
- 9. Weinsier RL, Boker JR, Brooks CM, Kushner RF, Visek WJ, Mark DA, Lopez SA, Anderson MS, Block K. Priorities for nutrition content in a medical school curriculum: a national consensus of medical educators. Am J Clin Nutr. 1989;50(4):707–12. [DOI] [PubMed] [Google Scholar]
- 10. Adams KM, Kohlmeier M, Powell M, Zeisel SH. Nutrition in medicine: nutrition education for medical students and residents. Nutr Clin Pract. 2010;25(5):471–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hark LA. Lessons learned from nutrition curricular enhancements. Am J Clin Nutr. 2006;83(4):968S–70S. [DOI] [PubMed] [Google Scholar]
- 12. Krebs NF, Primak LE.. Comprehensive integration of nutrition into medical training. Am J Clin Nutr. 2006;83(4):945S–50S. [DOI] [PubMed] [Google Scholar]
- 13. Lenders C, Gorman K, Milch H, Decker A, Harvey N, Stanfield L, Lim-Miller A, Salge-Blake J, Judd L, Levine S. A novel nutrition medicine education model: the Boston University experience. Adv Nutr. 2013;4(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Schoettler CL, Lee JN, Ireland KA, Lenders CM. A novel method of increasing medical student nutrition awareness and education. J Biomed Educ. 2015;2015:8. [Google Scholar]
- 15. Education and Training for Health Act of 2017, 115th Congress, 1st session. 2017. [Google Scholar]
- 16. Expanding Nutrition's Role in Curricula and Healthcare Act, 113th Congress, 2nd session. 2014. [Google Scholar]
- 17. Kiraly LN, McClave SA, Neel D, Evans DC, Martindale RG, Hurt RT. Physician nutrition education. Nutr Clin Pract. 2014;29(3):332–7. [DOI] [PubMed] [Google Scholar]
- 18. Hark LA, Iwamoto C, Melnick DE, Young EA, Morgan SL, Kushner R, Hensrud DD. Nutrition coverage on medical licensing examinations in the United States. Am J Clin Nutr. 1997;65(2):568–71. [DOI] [PubMed] [Google Scholar]
- 19. Englander R, Cameron T, Ballard AJ, Dodge J, Bull J, Aschenbrener CA. Toward a common taxonomy of competency domains for the health professions and competencies for physicians. Acad Med. 2013;88(8):1088–94. [DOI] [PubMed] [Google Scholar]
- 20. Miller GE. The assessment of clinical skills/competence/performance. Acad Med. 1990;65(9 Suppl):S63–7. [DOI] [PubMed] [Google Scholar]
- 21. ten Cate O, Scheele F. Competency-based postgraduate training: can we bridge the gap between theory and clinical practice?. Acad Me. 2007;82(6):542–7. [DOI] [PubMed] [Google Scholar]
- 22. Association of American Medical Colleges. Core Entrustable Professional Activities for Entering Residency: Curriculum Deve-lopers' Guide. Association of American Medical Colleges. [Internet] 2014. Available from: https://store.aamc.org/downloadable/download/sample/sample_id/63/. [Google Scholar]
- 23. Pershing S, Fuchs VR. Restructuring medical education to meet current and future health care needs. Acad Med. 2013;88(12):1798–801. [DOI] [PubMed] [Google Scholar]
- 24. Rose S, Fix OK, Shah BJ, Jones TN, Szyjkowski RD. Entrustable professional activities for gastroenterology fellowship training. Gastroenterology. 2014;147(1):233–42. [DOI] [PubMed] [Google Scholar]
- 25. EPA Toolbox: Oversight Working Network. [Internet]. 2014. Available from: http://webfiles.gi.org/docs/Supplementary_EPA_Toolbox.pdf.
- 26. Pereira AG, Woods M, Olson APJ, van den Hoogenhof S, Duffy BL, Englander R. Criterion-based assessment in a norm-based world: how can we move past grades?. Acad Med. 2018;93(4):560–4. [DOI] [PubMed] [Google Scholar]
- 27. Adams KM, Butsch WS, Kohlmeier M. The state of nutrition education at US medical schools. J Biomed Educ. 2015;2015:7. [Google Scholar]
- 28. Curriculum Committee of the Nutrition Academic Award Program. Nutrition Education for Health Professionals. [Internet]. 2012. Available from: https://www.nhlbi.nih.gov/research/training/naa/products/curr_gde/index.htm. [Google Scholar]
- 29. Lindsley JE, Abali EE, Bikman BT, Cline S, Fulton T, Lopez B, Rosenthal OD, Uhley VE, Weintraut RJ, Williams DP et al.. What nutrition-related knowledge, skills, and attitudes should medical students develop?. Med Sci Educ. 2017;27(4):579–83. [Google Scholar]
- 30. Hark LA, Deen D. Position of the academy of nutrition and dietetics: interprofessional education in nutrition as an essential component of medical education. J Acad Nutr Diet. 2017;117(7):1104–13. [DOI] [PubMed] [Google Scholar]
- 31. Bradley DW, Dietz WH, and the Provider Training and Education Workgroup. Provider Competencies for the Prevention and Management of Obesity. [Internet]. 2017. Available from: https://bipartisanpolicy.org/report/provider-competencies-for-the-prevention-and-management-of-obesity/. [Google Scholar]
- 32. Heiman HL, O'Brien CL, Curry RH, Green MM, Baker JF, Kushner RF, Thomas JX, Corbridge TC, Corcoran JF, Hauser JM et al.. Description and early outcomes of a comprehensive curriculum redesign at the Northwestern University Feinberg School of Medicine. Acad Med. 2018; 93(4):593–9. [DOI] [PubMed] [Google Scholar]
- 33. Kushner RF, Mechanick JI. Lifestyle medicine – an emerging new discipline. US Endocrinology. 2015;11(1):36–40. [Google Scholar]
- 34. Kushner RF, Van Horn L. Teaching nutrition in the context for lifestyle medicine. Med Sci Educ. 2018;18:9–12. [Google Scholar]
- 35. Kushner RF. Taking a weight history – using mnemonics to learn a missing skill in medical education. MedEdPublish. 2017;6(4):46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kushner RF, Kessler S, McGaghie WC. Using behavior change plans to improve medical student self-care. Acad Med. 2011;86(7):901–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Nowson C, Roshier-Taks M, Crotty B. Nutrition competencies for the prevention and treatment of disease in Australian medical courses. Med J Aust. 2012;197(3):147. [DOI] [PubMed] [Google Scholar]
- 38. Medical School Accreditation Committee. Standards for Assessment and Accreditation of Primary Medical Programs by the Australian Medical Council. 2012. [Google Scholar]
- 39. Nowson C. A web-based nutrition competency implementation toolkit for entry-level medical courses. Final report. [Internet]. Deakin University, 2015. Available from: http://www.deakin.edu.au.
- 40. Crowley J, Perlstein R, Blackburn, Martin SM, McCaffrey T, Charlton K, Nowson C, Beck E. Turning a Terrific Two. Complete Nutrition. [Internet]. 2018.; Available from: www.nnedpro.org.uk/articles-and-newsletters/4592621766.
- 41. Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N, Evans T, Fineberg H, Garcia P, Ke Y, Kelley P et al.. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376(9756):1923–58. [DOI] [PubMed] [Google Scholar]
- 42. Liaison Committee on Medical Education. Function and Structure of a Medical School: Standards for Accreditation of Medical Education Programs Leading to the MD degree. 2017:39. [Google Scholar]
- 43. Institute of Medicine Committee on Behavioral, Social Sciences in Medical School Curricula. The National Academies Collection: reports funded by National Institutes of Health. In: Cuff PA, Vanselow NA, editors. Improving Medical Education: Enhancing the Behavioral and Social Science Content of Medical School Curricula. Washington (DC): National Academies Press (US) National Academy of Sciences; 2004. [PubMed] [Google Scholar]
- 44. McGinnis JM, Foege WH.. Actual causes of death in the United States. JAMA. 1993;270(18):2207–12. [PubMed] [Google Scholar]
- 45. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System (BRFSS). [Internet]. 1998. Available from: https://www.cdc.gov/brfss/index.html. [Google Scholar]
- 46. Health Care Financing and Administration. Department of Health and Human Services Fiscal Year 2000 Freedom of Information Annual Report. 2000. [Google Scholar]
- 47. Hollar D, Carney P, Swiderski D, Dewey C, Stuber M, Cross A, Wimmers P, Satterfield J, Graham M, Skochelak S et al.. The National Institutes of Health Social and Behavioral Sciences Consortium: An Introduction and Progress Report on Undergraduate Medical Education Curricular Innovations. 2007. 60–8.p. [Google Scholar]
- 48. U.S. Department of Labor, Bureau of Labor Statistics. Occupational Outlook Handbook, Dietitians and Nutritionists. [Internet]. 2018. Available from: https://www.bls.gov/ooh/healthcare/dietitians-and-nutritionists.htm. [Google Scholar]
- 49. Academy of Nutrition and Dietetics Evidence Analysis Library. Medical Nutrition Therapy Evidence Analysis Project 2013–2015. [Google Scholar]
- 50. Liebhart J, Cook SR, Schofield M, Peterson LE, Radecki L. The Childhood Obesity Performance Improvement (COPI) Collaborative: A Pilot to Improve Practice Systems for Children with Overweight or Obesity through Enhanced Care Coordination, Evidence-Based Practice, and Use of the Healthier Generation Benefit. 2016. 147A–A.p. [Google Scholar]
- 51. Rajkumar R, Conway PH, Tavenner M. CMS–engaging multiple payers in payment reform. JAMA. 2014;311(19):1967–8. [DOI] [PubMed] [Google Scholar]
- 52. Stanski R, Palmer C. Oral health and nutrition as gatekeepers to overall health: We are all in this together. Eur J Gen Dentistry. 2015;4(3):99–105. [Google Scholar]
- 53. Khan SY, Holt K, Tinanoff N. Nutrition education for oral health professionals: a must, yet still neglected. J Dent Educ. 2017;81(1):3–4. [PubMed] [Google Scholar]
- 54. Palmer CA, Dwyer J, Clark RE. Expert opinions on nutrition issues in clinical dentistry. J Dent Educ. 1990;54(10):612–8. [PubMed] [Google Scholar]
- 55. Taylor GW, Stumpos ML, Kerschbaum W, Inglehart MR. Educating dental students about diet-related behavior change: does experiential learning work?. J Dent Educ. 2014;78(1):64–74. [PubMed] [Google Scholar]
- 56. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–31. [PMC free article] [PubMed] [Google Scholar]
- 57. Offices of Disease Prevention and Health Promotion. 2008 Physical Activity Guidelines for Americans. [Internet]. Health.gov, 2008 Available from: https://health.gov/paguidelines/2008/pdf/paguide.
- 58. Sallis RE, Baggish AL, Franklin BA, Whitehead JR. The call for a physical activity vital sign in clinical practice. Am J Med. 2016;129(9):903–5. [DOI] [PubMed] [Google Scholar]
- 59. School of Medicine Greenville. Lifestyle Medicine Curriculum. University of South Carolina; 2013. [Google Scholar]
- 60. Lifestyle Medicine Education Collaborative. Home page 2016.. Available from: lifestylemedicineeducation.org.
- 61. Dimaria-Ghalili RA, Edwards M, Friedman G, Jaferi A, Kohlmeier M, Kris-Etherton P, Lenders C, Palmer C, Wylie-Rosett J. Capacity building in nutrition science: revisiting the curricula for medical professionals. Ann N Y Acad Sci. 2013;1306:21–40. [DOI] [PubMed] [Google Scholar]
- 62. DiMaria-Ghalili RA, Gilbert K, Lord L, Neal T, Richardson D, Tyler R, Guenter P. Standards of nutrition care practice and professional performance for nutrition support and generalist nurses. Nutr Clin Pract. 2016;31(4):527–47. [DOI] [PubMed] [Google Scholar]
- 63. The Joint Commission 2015 Comprehensive Accreditation Manual for Hospitals. Oak Brook, IL; 2014. [Google Scholar]
- 64. Patel V, Romano M, Corkins MR, DiMaria-Ghalili RA, Earthman C, Malone A, Miller S, Sabino K, Wooley J, Guenter P. Nutrition screening and assessment in hospitalized patients: a survey of current practice in the United States. Nutr Clin Pract. 2014;29(4):483–90. [DOI] [PubMed] [Google Scholar]
- 65. American Society for Parenteral and Enteral Nutrition. Malnutrition Solution Center. [Internet]. 2019. Available from: http://www.nutritioncare.org/guidelines_and_clinical_resources/Malnutrition_Solution_Center/.
- 66. Kassin MT, Owen RM, Perez SD, Leeds I, Cox JC, Schnier K, Sadiraj V, Sweeney JF. Risk factors for 30-day hospital readmission among general surgery patients. J Am Coll Surg. 2012;215(3):322–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Mudge AM, Kasper K, Clair A, Redfern H, Bell JJ, Barras MA, Dip G, Pachana NA. Recurrent readmissions in medical patients: a prospective study. J Hosp Med. 2011;6(2):61–7. [DOI] [PubMed] [Google Scholar]
- 68. Food and Nutrition Board; Health and Medicine Division; National Academies of Sciences Engineering and Medicine. Meeting the Dietary Needs of Older Adults: Exploring the Impact of the Physical, Social, and Cultural Environment: Workshop Summary. Washington (DC): National Academies Press; 2016. [PubMed] [Google Scholar]
- 69. Guenter P, Jensen G, Patel V, Miller S, Mogensen KM, Malone A, Corkins M, Hamilton C, DiMaria-Ghalili RA. Addressing Disease-Related Malnutrition in Hospitalized Patients: A Call for a National Goal. Jt Comm J Qual Patient Saf. 2015;41(10):469–73. [DOI] [PubMed] [Google Scholar]
- 70. American Osteopathic Association. OMP Report: 2017. 2017. [Google Scholar]
- 71. American Osteopathic Association. The Single GME Accreditation System. 2018. [Google Scholar]
- 72. Briggs Early K, Adams KM, Kohlmeier M. Analysis of nutrition education in osteopathic medical schools. J Biomed Educ. 2015;2015:6. [Google Scholar]
- 73. Hargrove EJ, Berryman DE, Yoder JM, Beverly EA. Assessment of nutrition knowledge and attitudes in preclinical osteopathic medical students. J Am Osteopath Assoc. 2017;117(10):622–33. [DOI] [PubMed] [Google Scholar]
- 74. Favia M, Moore A, Kelly P, Werner C. What do physician assistant students know about nutrition? A survey of attitudes, self-perceived proficiency, and knowledge during three stages of physician assistant education. J Physician Assist Educ. 2016;27:131–5. [DOI] [PubMed] [Google Scholar]
- 75. Sullivan SY. Nutrition education in physician assistant programs: a national survey. J Physician Assist Educ. 2000;11(1):18–24. [Google Scholar]
- 76. American Physical Therapy Association. Nutrition and Physical Therapy. [Internet]. 2018. Available from: http://www.apta.org/PatientCare/Nutrition/.
- 77. Afaghi A, Mohamadi AAHA, Sarchami R, Ziaee A. Effect of an integrated case-based nutrition curriculum on medical education at Qazvin university of medical sciences, Iran. Global J Health Sci. 2012;4(1):112–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Barss P, Grivna M, Al-Maskari F, Kershaw G. Strengthening public health medicine training for medical students: development and evaluation of a lifestyle curriculum. Med Teach. 2008;30(9-10):e196–218. [DOI] [PubMed] [Google Scholar]
- 79. Conroy MB, Delichatsios HK, Hafler JP, Rigotti NA. Impact of a preventive medicine and nutrition curriculum for medical students. Am J Prev Med. 2004;27(1):77–80. [DOI] [PubMed] [Google Scholar]
- 80. Kohlmeier M, McConathy WJ, Cooksey Lindell K, Zeisel SH. Adapting the contents of computer-based instruction based on knowledge tests maintains effectiveness of nutrition education. Am J Clin Nutr. 2003;77(4 Suppl):1025s–7s. [DOI] [PubMed] [Google Scholar]
- 81. Lebensohn P, Kligler B, Dodds S, Schneider C, Sroka S, Benn R, Cook P, Guerrera M, Low Dog T, Sierpina V et al.. Integrative medicine in residency education: developing competency through online curriculum training. J Grad Med Educ. 2012;4(1):76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Lewis KO, Frank GR, Nagel R, Turner TL, Ferrell CL, Sangvai SG, Donthi R, Mahan JD. Pediatric trainees’ engagement in the online nutrition curriculum: preliminary results. BMC Med Educ. 2014;14(1):190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Schlair S, Hanley K, Gillespie C, Disney L, Kalet A, Darby PC, Frank E, Spencer E, Harris J, Jay M. How medical students' behaviors and attitudes affect the impact of a brief curriculum on nutrition counseling. J Nutr Educ Behav. 2012;44(6):653–7. [DOI] [PubMed] [Google Scholar]
- 84. Ray S, Udumyan R, Rajput-Ray M, Thompson B, Lodge K-M, Douglas P, Sharma P, Broughton R, Smart S, Wilson R et al.. Evaluation of a novel nutrition education intervention for medical students from across England. BMJ Open. 2012;2(1):e000417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Estruch R, Ros E, Salas-Salvado J, Covas MI, Corella D, Aros F, Gomez-Gracia E, Ruiz-Gutierrez V, Fiol M, Lapetra J et al.. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368(14):1279–90. [DOI] [PubMed] [Google Scholar]
- 86. Ajala O, English P, Pinkney J. Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am J Clin Nutr. 2013;97(3):505–16. [DOI] [PubMed] [Google Scholar]
- 87. Esposito K, Maiorino MI, Bellastella G, Chiodini P, Panagiotakos D, Giugliano D. A journey into a Mediterranean diet and type 2 diabetes: a systematic review with meta-analyses. BMJ Open. 2015;5(8). doi: 10.1136/bmjopen-2015-008222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. McGaghie WC, Issenberg SB, Cohen ER, Barsuk JH, Wayne DB. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med. 2011;86(6):706–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Monlezun D, Leong B, Joo E, Birkhead A, Sarris L, Harlan T. Novel Longitudinal and Propensity Score Matched Analysis of Hands-On Cooking and Nutrition Education versus Traditional Clinical Education among 627 Medical Students. Adv Prev Med. 2015;656780. doi: 1155/2015/656780 [Epub 2015 Sep 8]. [DOI] [PMC free article] [PubMed]
- 90. Nutritional Science Funding Opportunities: National Cancer Institute, Division of Cancer Prevention. [Internet]. 2019. Available from: https://prevention.cancer.gov/research-groups/nutritional-sci-ence/funding.
- 91. NIH Nutrition Research Report 2015 & 2016: National Institute of Diabetes and Digestive and Kidney Diseases. [Internet]. 2017. Available from: https://www.niddk.nih.gov/about-niddk/strategic-plans-reports/nih-nutrition-report.
- 92. Lin JS, O'Connor EA, Evans CV, Senger CA, Rowland MG, Groom HC. U.S. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews. Behavioral Counseling to Promote a Healthy Lifestyle for Cardiovascular Disease Prevention in Persons With Cardiovascular Risk Factors: An Updated Systematic Evidence Review for the US Preventive Services Task Force. Rockville (MD): Agency for Healthcare Research and Quality (US); 2014. [PubMed] [Google Scholar]
- 93. Van Horn L, Carson JA, Appel LJ, Burke LE, Economos C, Karmally W, Lancaster K, Lichtenstein AH, Johnson RK, Thomas RJ et al.. Recommended dietary pattern to achieve adherence to the American Heart Association/American College of Cardiology (AHA/ACC) guidelines: a scientific statement from the American Heart Association. Circulation. 2016;134(22):e505–29. [DOI] [PubMed] [Google Scholar]
- 94. Sacks FM, Lichtenstein AH, Wu JHY, Appel LJ, Creager MA, Kris-Etherton PM, Miller M, Rimm EB, Rudel LL, Robinson JG et al.. Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Circulation. 2017;136(3):e1–23. [DOI] [PubMed] [Google Scholar]
- 95. Hivert MF, Arena R, Forman DE, Kris-Etherton PM, McBride PE, Pate RR, Spring B, Trilk J, Van Horn LV, Kraus WE. Medical training to achieve competency in lifestyle counseling: an essential foundation for prevention and treatment of cardiovascular diseases and other chronic medical conditions: a scientific statement from the American Heart Association. Circulation. 2016;134(15):e308–27. [DOI] [PubMed] [Google Scholar]
- 96. Aspry KE, Van Horn L, Carson JAS, Wylie-Rosett J, Kushner RF, Lichtenstein AH, Devries S, Freeman AM, Crawford A, Kris-Etherton P. Medical nutrition education, training, and competencies to advance guideline-based diet counseling by physicians: a science advisory from the American Heart Association. Circulation. 2018;137(23):e821–41. [DOI] [PubMed] [Google Scholar]
- 97. Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF et al.. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic impact goal through 2020 and beyond. Circulation. 2010;121(4):586–613. [DOI] [PubMed] [Google Scholar]
- 98. Levy MD, Loy L, Zatz LY. Policy approach to nutrition and physical activity education in health care professional training. Am J Clin Nutr. 2014;99(5 Suppl):1194s–201s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Schmitt M, Blue A, Aschenbrener CA, Viggiano TR. Core competencies for interprofessional collaborative practice: reforming health care by transforming health professionals' education. Acad Med. 2011;86(11):1351. [DOI] [PubMed] [Google Scholar]
- 100. Alexander N, Rowe S, Burton-Freeman B, Brackett RE, Kretser A, Hentges EJ, Klurfeld DM, Meyers LD, Ohlhorst S, Mukherjea R. Achieving a transparent, actionable framework for public-private partnerships for food and nutrition research. Am J Clin Nutr. 2015;101(6):1359–63. [DOI] [PubMed] [Google Scholar]
- 101. Advancing Nutrition Training, and Research for Medical Students, Residents, Fellows, Attending Physicians and other Clinicians: National Heart, Lung, and Blood Institute. [Internet]. 2017. Available from: https://www.nhlbi.nih.gov/events/2017/advancing-nutrition-training-and-research-medical-students-residents-fellows-attending.