Abstract
In the glaucoma clinic, patients with normal intraocular pressure (IOP) can sometimes show visual field (VF) progression. Therefore, clarification of relationship between vascular status and glaucomatous VF deterioration is a focus of interest. We used optical coherence tomography angiography (OCTA), with the aim of evaluating the relationship between vessel density (VD) and VF progression in glaucoma patients. We included 104 eyes with open angle glaucoma who were followed up for at least 5 years in this retrospective case-control study. Superficial and deep VD of macula were assessed by OCTA. Regression analysis and Cox proportional hazards model were used to identify factors significantly associated with VF progression. In logistic regression analysis determining VF progression from Guided Progression Analysis (GPA) program, initial IOP and deep macular VD were significantly associated with VF progression in multivariate analysis (P = 0.019 and 0.004). Cox proportional hazards model also identified deep macular VD as significantly related to VF progression (P = 0.035). In conclusion, initial IOP and deep VD were related to VF deterioration in glaucoma. Deep VD might be used as a surrogate of glaucomatous VF progression related with vascular incompetence.
Subject terms: Risk factors, Outcomes research
Introduction
Glaucoma is a progressive disease that involves thinning of the retinal nerve fiber layer (RNFL) and defects in the corresponding areas of the visual field (VF). Uncontrolled intraocular pressure (IOP) has traditionally been considered to be the only modifiable risk factor associated with progression in glaucoma, with the reduction of IOP as the mainstay of treatment1,2. However, there are patients who still show glaucomatous visual field progression even with well controlled IOP3. This indicates that there must be additional factors involved in the progression of glaucoma.
According to the Collaborative Normal-Tension Glaucoma Study (CNTG) and the Early Manifest Glaucoma Trial (EMGT), migraine and disc hemorrhage contributed to the progression of visual field deterioration apart from IOP4,5. Several other studies have also shown that decreased retrobulbar blood flow or impaired systemic circulation was associated with glaucoma progression6,7.
Recently, optical coherence tomography angiography (OCTA) has been used taking the advantage of noninvasiveness and rapid imaging. As an emerging technology that could visualize vascular circulation without dye injection, this machine has become an additional tool for clinical diagnosis and treatment at a rapid rate. For glaucoma specialist, OCTA has major advantages that could afford direct and layer-specific imaging of the circulation of blood in the macula and peripapillary region. Several studies have utilized OCTA to study the relationships between decreased vessel density (VD), incidence of glaucoma, and severity of visual field defects8–10. However, whether low VD is a cause of glaucomatous damage or is merely an epiphenomenon of retinal thinning remains difficult to clarify. The deep retinal microvasculature might be less affected by structural changes due to the occurrence of retinal thinning mainly in the superficial retinal nerve fiber layer (RNFL) and ganglion cell layer (GCL) in glaucoma. A previous study found that deep VD located in the the inner nuclear layer (INL) was an independent risk factor of central visual function in addition to retinal thickness thinning, and it was suggested that deep VD assessed by OCTA might be a biomarker for ocular blood flow11.
The purpose of this study was to evaluate the relationship between retinal VD and glaucomatous VF progression, and to identify an indicator of ocular vascular stress that is associated with VF deterioration.
Results
A total of 151 eyes of patients with open angle glaucoma (OAG) were involved in this study. Five eyes were excluded because of repeated unreliable VF test results, as were 2 eyes of patients who exhibited poor compliance with IOP lowering treatment. In addition, 40 eyes showing inadequate OCTA image quality were excluded, leaving a total of 104 eyes.
Table 1 shows the baseline characteristics of the study participants. All patients had normal IOPs when they were diagnosed with glaucoma. The mean follow-up duration was 110.30 ± 42.76 months, and the SITA 24-2 MD was −4.44 ± 5.68 dB, consistent with mild glaucomatous defect.
Table 1.
Demographic and ocular characteristics of study subjects.
| Total n = 104 | |
|---|---|
| Age, years | 58.21 (±13.11) |
| Sex, male:female | 42:62 |
| Hypertension, n(%) | 34 (32.7%) |
| Diabetes, n(%) | 8 (7.7%) |
| Disc hemorrhage, n(%) | 7 (6.7%) |
| Follow up duration, months | 110.30 (±42.76) |
| Axial length, mm | 24.87 (±1.38) |
| Best corrected visual acuity, decimal | 0.90 (±0.12) |
| Initial intraocular pressure, mmHg | 15.28 (±3.26) |
| Average intraocular pressure, mmHg | 13.64 (±2.81) |
| IOP fluctuation (SD of IOP) | 1.37 (±0.78) |
| Initial RNFL average thickness, μm | 73.35 (±11.89) |
| Last RNFL average thickness, μm | 69.38 (±12.45) |
| Initial SITA 24-2 MD, dB | −4.44 (±5.68) |
| Initial SITA 24-2 PSD, dB | 5.08 (±4.35) |
| Last SITA 24-2 MD, dB | −5.83 (±6.46) |
| Last SITA 24-2 PSD, dB | 6.21 (±4.48) |
| Superficial VD, % | 24.70 (±3.45) |
| Deep VD, % | 31.01 (±2.13) |
IOP: intraocular pressure; MD: mean deviation; PSD: pattern standard deviation; VD: vessel density; RNFL: retinal nerve fiber layer; PPA: peripapillary area.
Data are means (±SD) or numbers (%), as appropriate.
The rate of change in the VF was determined by calculating the MD slope of the VF. Table 2 presents the correlation coefficients relating to the MD slope with clinical or ocular parameters, including OCT parameters and VDs derived from OCTA images. Deep VD determined by OCTA was marginally correlated with MD slope (P = 0.058). According to linear regression analysis, the association of deep VD with the MD slope of VF was significant, with the regression line showing a positive gradient (ß = 0.046 and P = 0.018 by multivariate analysis). In other words, the higher the VD, the lower the deterioration rate in the VF. The initial IOP of each study participant was also marginally significant by multivariate analysis (P = 0.051) (Table 3).
Table 2.
Correlation coefficients between the MD slope and clinical or ocular parameters.
| r | R2 | P value | |
|---|---|---|---|
| Age | 0.047 | 0.002 | 0.633 |
| Follow up duration | −0.049 | 0.002 | 0.620 |
| Initial IOP | −0.150 | 0.022 | 0.129 |
| Average IOP | −0.023 | 0.001 | 0.909 |
| IOP fluctuation | −0.012 | 0.000 | 0.950 |
| Initial MD of SITA 24-2 | 0.047 | 0.002 | 0.634 |
| OCT parameters | |||
| RNFL thickness | −0.005 | 0.000 | 0.959 |
| Average CDR | −0.023 | 0.001 | 0.827 |
| Rim area | 0.116 | 0.014 | 0.277 |
| Disc area | 0.094 | 0.009 | 0.380 |
| Cup volume | 0.037 | 0.001 | 0.733 |
| RNFL slope* | 0.073 | 0.005 | 0.552 |
| OCT angiography | |||
| Superficial VD | 0.125 | 0.016 | 0.208 |
| Deep VD | 0.187 | 0.035 | 0.058 |
IOP: intraocular pressure; MD: mean deviation; OCT: optical coherence tomography; RNFL: retinal nerve fiber layer; CDR: cup-disc ratio; VD: vessel density.
*RNFL slope (μm/yr) = (Change in mean RNFL thickness during follow-up period) / (follow-up duration).
Pearson correlation analysis was used.
Table 3.
Univariate and multivariate regression analysis of the MD slope in glaucoma patients.
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| ß | 95% CI | P value | ß | 95% CI | P value | |
| Age | 0.002 | −0.007 to 0.011 | 0.633 | |||
| Follow up duration | 0.001 | −0.002 to 0.001 | 0.620 | |||
| Initial MD of SITA 24-2 | 0.003 | −0.009 to 0.015 | 0.634 | |||
| Initial IOP | −0.016 | −0.037 to 0.005 | 0.129 | −0.024 | −0.048 to 0.000 | 0.051 |
| Average IOP | −0.026 | −0.077 to 0.025 | 0.307 | |||
| IOP fluctuation | −0.006 | −0.195 to 0.184 | 0.950 | |||
| RNFL thickness | 0.000 | −0.006 to 0.006 | 0.959 | |||
| Average CDR | −0.099 | −0.998 to 0.800 | 0.827 | |||
| Rim area | 0.214 | −0.175 to 0.603 | 0.277 | 0.274 | −0.152 to 0.700 | 0.204 |
| Disc area | 0.088 | −0.110 to 0.287 | 0.380 | |||
| Cup volume | 0.054 | −0.257 to 0.365 | 0.733 | |||
| RNFL slope | 0.017 | −0.039 to 0.073 | 0.552 | |||
| Superficial VD | 0.013 | −0.007 to 0.033 | 0.208 | −0.003 | −0.027 to 0.022 | 0.836 |
| Deep VD | 0.031 | −0.001 to 0.063 | 0.058 | 0.046 | 0.008 to 0.084 | 0.018 |
CI: confidence interval; MD: mean deviation; IOP: intraocular pressure; RNFL: retinal nerve fiber layer; CDR: cup-disc ratio; VD: vessel density
Multivariate regression analysis included factors of P values lower than 0.3 in univariate analysis.
According to guided progression analysis (GPA) program, 55 eyes showed significant progression of VF loss during the follow-up period, while 49 eyes had not progressed. As shown in Table 4, the differences in age, gender, frequency of disc hemorrhage, axial length, visual acuity, and RNFL thickness between the progressors and nonprogressors were not significant. The initial MD values of SITA 24-2 were comparable between the two group, however, the final MD and MD slope were significantly worse for the progressors (−7.38 ± 6.75 dB of last MD and −0.34 ± 0.35 dB/yr of MD slope in progressor; −4.08 ± 5.69 dB of last MD and −0.02 ± 0.27 dB/yr of MD slope in non-progressor; all P < 0.001). As expected, the RNFL change slope was steeper (−1.05 ± 1.05 μm/yr) and initial IOP was higher (16.08 ± 3.21 mmHg) in the progressor group compared to non-progressor group (−0.16 ± 1.411 μm/yr and 14.81 ± 3.17 mmHg, P = 0.010 and 0.017, respectively). Interestingly, deep VD was significantly lower in the progressor group (30.40 ± 2.11% in progressor and 31.68 ± 1.96% in non-progressor; P = 0.002).
Table 4.
Comparisons between glaucoma patients with or without visual field progression.
| Progressor (n = 55) | Non-progressor (n = 49) | P value | |
|---|---|---|---|
| Age, years | 58.91 (±12.21) | 57.43 (±14.21) | 0.500 |
| Sex, male:female | 24:31 | 18:31 | 0.474 |
| Hypertension, n(%) | 18 (32.7%) | 16 (32.7%) | 0.994 |
| Diabetes, n(%) | 5 (10.2%) | 3 (5.5%) | 0.364 |
| Disc hemorrhage, n(%) | 5 (9.1%) | 2 (4.1%) | 0.309 |
| Axial length, mm | 24.78 (±1.51) | 24.99 (±1.20) | 0.583 |
| Best corrected visual acuity, decimal | 0.91 (±0.13) | 0.89 (±0.12) | 0.366 |
| Initial IOP, mmHg | 16.08 (±3.21) | 14.81 (±3.17) | 0.017 |
| Average IOP, mmHg | 14.35 (±3.04) | 12.64 (±2.24) | 0.120 |
| IOP fluctuation (SD of IOP) | 1.42 (±0.85) | 1.30 (±0.68) | 0.691 |
| Initial RNFL average thickness, μm | 73.69 (±12.47) | 72.96 (±11.32) | 0.756 |
| Last RNFL average thickness, μm | 68.04 (±13.01) | 70.88 (±11.74) | 0.247 |
| RNFL slope, μm/yr | −1.05 (±1.05) | −0.16 (±1.41) | 0.010 |
| Initial SITA 24-2 MD, dB | −4.81 (±5.83) | −4.01 (±5.54) | 0.476 |
| Initial SITA 24-2 PSD, dB | 5.37 (±4.37) | 4.75 (±4.35) | 0.470 |
| Last SITA 24-2 MD, dB | −7.38 (±6.75) | −4.08 (±5.69) | 0.009 |
| Last SITA 24-2 PSD, dB | 7.48 (±4.29) | 4.77 (±4.29) | 0.002 |
| MD slope, dB/year | −0.34 (±0.35) | −0.02 (±0.27) | <0.001 |
| PSD slope, dB/year | 0.30 (±0.39) | −0.01 (±0.22) | <0.001 |
| Superficial VD, % | 24.62 (±3.58) | 24.78 (±3.32) | 0.810 |
| Deep VD, % | 30.40 (±2.11) | 31.68 (±1.96) | 0.002 |
IOP: intraocular pressure; SD: standard deviation; RNFL: retinal nerve fiber layer; MD: mean deviation; PSD: pattern standard deviation; VD: vessel density.
Data are means (±SD) or numbers (%), as appropriate.
Student’s t test and Chi-square test were used.
Table 5 shows the results of logistic regression analysis, which was used to identify those factors that were related to the glaucomatous progression of VF loss as determined by GPA. Follow-up duration, initial IOP, cup volume from initial OCT and deep VD from OCTA showed significant or marginal significance by univariate analysis (P values ranging from 0.003 to 0.106). By multivariate analysis, initial IOP and deep VD were significantly associated with VF progression (P = 0.019 and 0.004, respectively).
Table 5.
Logistic regression analysis of visual field progression in glaucoma patients.
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| Exp(ß) | 95% CI | P value | Exp(ß) | 95% CI | P value | |
| Age | 0.985 | 0.938 to 1.035 | 0.554 | |||
| Follow up duration | 1.008 | 0.998 to 1.018 | 0.106 | 1.009 | 0.992 to 1.026 | 0.318 |
| Initial IOP | 1.110 | 0.981 to 1.256 | 0.099 | 1.575 | 1.131 to 2.195 | 0.019 |
| Average IOP | 0.084 | 0.815 to 1.451 | 0.570 | |||
| IOP fluctuation | 1.235 | 0.456 to 3.347 | 0.678 | |||
| Initial MD of SITA 24-2 | 0.975 | 0.909 to 1.045 | 0.473 | |||
| RNFL thickness | 1.005 | 0.973 to 1.039 | 0.753 | |||
| Average CDR | 15.864 | 0.118 to 2136.641 | 0.269 | |||
| Rim area | 0.815 | 0.099 to 6.697 | 0.849 | |||
| Disc area | 2.091 | 0.690 to 6.334 | 0.192 | 4.186 | 0.295 to 59.378 | 0.290 |
| Cup volume | 4.357 | 0.742 to 25.589 | 0.103 | 0.125 | 0.002 to 8.957 | 0.340 |
| Superficial VD | 0.986 | 0.881 to 1.103 | 0.807 | |||
| Deep VD | 0.735 | 0.600 to 0.901 | 0.003 | 0.548 | 0.374 to 0.803 | 0.004 |
CI: confidence interval; MD: mean deviation; IOP: intraocular pressure; RNFL: retinal nerve fiber layer; CDR: cup-disc ratio; VD: vessel density
Multivariate regression analysis included factors of P values lower than 0.2 in univariate analysis.
Considering the varied follow-up periods of participants and the marginal significance of the association of follow-up period with VF progression by logistic analysis, we used Cox proportional-hazards models to identify meaningful factors affecting VF deterioration. By univariate analysis, age at last follow-up and deep VD had marginal significance (P = 0.082 and 0.085, respectively), and multivariate analysis showed that the previous two factors were significantly associated with VF progression (P = 0.005 and 0.007, respectively, Table 6). The hazard ratio of deep VD was 0.548, indicating that a higher VD value was less related to VF progression (Table 6).
Table 6.
Risk factors affecting visual field progression using Cox proportional-hazards models.
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P value | HR | 95% CI | P value | |
| Age | 0.969 | 0.947 to 0.992 | 0.082 | 1.541 | 1.138 to 2.088 | 0.005 |
| Initial IOP | 1.070 | 0.982 to 1.166 | 0.122 | 1.261 | 0.978 to 1.627 | 0.073 |
| Average IOP | 1.128 | 0.967 to 1.316 | 0.125 | |||
| IOP fluctuation | 1.657 | 0.824 to 3.332 | 0.156 | |||
| Initial MD of SITA 24-2 | 1.000 | 0.958 to 1.044 | 0.987 | |||
| RNFL thickness | 1.007 | 0.984 to 1.030 | 0.555 | |||
| Average CDR | 0.798 | 0.026 to 24.205 | 0.897 | |||
| Rim area | 1.063 | 0.264 to 4.287 | 0.931 | |||
| Disc area | 0.870 | 0.392 to 1.929 | 0.731 | |||
| Cup volume | 1.011 | 0.348 to 2.933 | 0.985 | |||
| Superficial VD | 1.037 | 0.950 to 1.132 | 0.421 | 1.308 | 0.975 to 1.753 | 0.073 |
| Deep VD | 0.886 | 0.772 to 1.017 | 0.085 | 0.586 | 0.396 to 0.865 | 0.007 |
CI: confidence interval; MD: mean deviation; IOP: intraocular pressure; RNFL: retinal nerve fiber layer; CDR: cup-disc ratio; VD: vessel density.
Multivariate analysis used the backward elimination method.
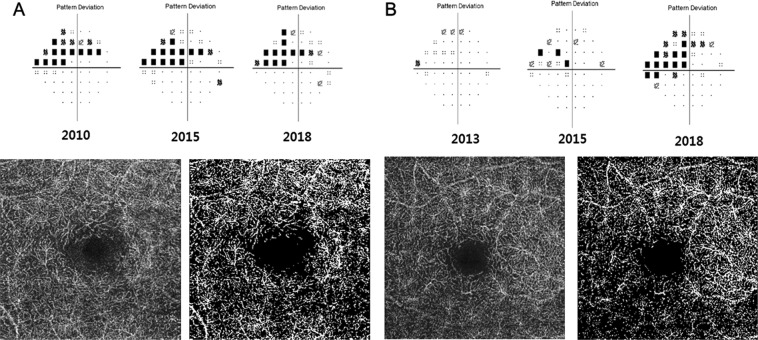
Representative cases are shown in Fig. 1. An 81-year-old woman and a 50-year-old woman without any systemic cardiovascular disease had well controlled normal IOP. The 50-year-old woman showed glaucomatous progression of VF loss even with a lower initial MD than that of the 81-year-old woman. The calculated deep VD of the 50-year-old progressor was lower than that of the 81-year-old nonprogressor (31.20% vs 34.02%, respectively).
Figure 1.
Two representative cases with contrasting features. The lower left image from each case is the original OCT angiography image of deep retinal layer, and the lower right image is the binarized result to calculate vessel density. (A) An 81-year-old woman with stable visual field (VF) results; (B) a 50-year-old woman with progressed VF. During the follow-up period, case B showed VF progression and lower deep retinal vessel density than that of case A.
Discussion
Ocular blood flow is known to play a critical role in the development and progression of glaucoma12–14. However, the direct assessment and identification of ocular blood circulation are difficult. Laser Doppler flowmetry (LDF), laser speckle contrast imaging (LSCI), and magnetic resonance imaging (MRI) have all been used to study ocular blood flow15. However, there are several limitations to these approaches, including penetration depth of the laser into ocular tissue16, difficulty in quantifying blood flow17, the time-consuming nature of the procedures, and the significant cost burden, especially in the outpatient setting. OCTA has come into widespread use in more recent years as a direct indicator of local ocular blood flow. Because OCTA allows higher imaging speeds and obtains volumetric scans that can be segmented by retinal layer to improve image quality and allow for quantitative analysis, it is an important, useful, and practical tool18,19.
The vascular plexus of the retinal deep layer is located mainly within INL of retina20,21. The INL undergoes little structural change in glaucoma; thus, blood circulation in the INL might help to minimize the effect of resulting decrease of VD due to RNFL and GCL thinning. This point accounts for our continued interest in the deep vascular plexus of the retina. We previously showed that deep VD was not correlated with retinal thickness, even in the INL, where the deep vascular plexus is located11. Shin et al. focused on the decreased peripapillary VD segmented into superficial and deep retina in glaucoma patients22. Lommatzsch et al. evaluated macular VD by dividing the retina into superficial and deep layers, and found that the VD in each layer was decreased in glaucoma23.
Moghimi et al. recently reported that macular VD was related to the rate of RNFL thinning and might be a predictors of the risk of glaucoma progression24. However, they considered the vascular plexus of the superficial retina that could be confused with resulting GCL thinning of glaucoma. To strive to overcome these shortcoming, we investigated the VD of deep retinal layer. According to our results, it is suggested that the lower the deep VD, the more progressed VF result. In addition, deep VD was identified as a factor determining the MD slope. During the period of follow-up, the presence of VF deterioration was affected by decreased deep VD, and progressed patients had lower deep VD than non-progressors. Although the causal relationship between these factors is not clear, it is thought that compromised ocular blood circulation underlies VF progression in glaucoma patients with well controlled IOP, and deep VD might reflect the status of the local ocular blood circulation.
In our study, the superficial VD was not associated with VF progression and it is contrasting with the aforementioned study of Moghimi et al. However, the OCTA of Moghimi’s study was performed at baseline and ours was performed at different timing. The superficial VD of our study may be affectd by RGC structure of current status – not baseline. According to several studies, glaucoma progression is affected by the baseline state of disease, not by the current state when the patient is treated25–27. This difference could make this contradictory results, but the future study with large subjects is required to clarify it.
We had concerns about the effects of topical IOP-lowering medication on retinal VD. Supplementary Table 1 showed the relationships of VDs between different medication groups. Topical prostaglandin did not affect VDs significantly, but patients with topical beta blocker (BB) showed lower superficial VD. The difference might be caused by the different initial IOP and MD for topical BB as shown in Supplementary Table 1. In our subjects, PG eyedrops are often prescribed as the primary choice, and topical BBs tend to be added when trying to strengthen the treatment. The patients with worse glaucoma state or higher IOP were often prescribed the BB and these patients might have thinner GCL thickness – this difference could affect superficial VD. Though, the deep VD located in the INL and not affected by GCL thinning, was not decreased even in the topical BB group. In other words, the deep VD seems not to be significantly affected by topical vasoactive BB.
Our findings incorporated initial IOP as a variable associated with occurrence of VF deterioration. According to several studies including EMGT, higher baseline IOP is consistently found to be a predictive factor for VF progression28,29. However, average IOP and IOP fluctuation were not associated with VF progression in this study. Heiji A et al30. reported that higher mean IOP was associated with more rapid progression, and the study of Matlach31 showed the IOP fluctuation as the meaningful factor of glaucoma progression. This controversial results might be due to the different subjects of glaucoma between studies. Our data included examinations from NTG patients but previous studies included mainly POAG patients. In CNTG study, the IOP was not associated with VF progression32. Also, in the previous study of our group, mean IOP and IOP fluctuation were not associated with VF progression in NTG patients33. However, this controversy should be investigated further with larger study subjects.
There are also many other factors to consider regarding glaucoma progression. We found that when taking into consideration the follow-up period, age was associated with the progression of deterioration in VF. This result in our study was consistent with previous studies asserting that older patients experience greater progression5,34. Worse baseline MD was associated with VF progression in several previous studies25,35, but this study did not show significant association. Severity of glaucoma in our study subjects was better than −12dB of MD corresponding with mild to moderate glaucoma. Including only patients with limited range of severity could make limitation and a study including with various severity and large number of subjects should be conducted.
Disc hemorrhage is widely known to be related to glaucoma progression36. However, in our results, the presence of disc hemorrhage did not show significant relationship with VF progression. There was possibility of undervalued incidence of disc hemorrhage since it can only be confirmed when the patient visits the clinic and this matter could be a limitation of our study.
There are some more limitations in this study. First, OCTA is a recent technology, and obtaining baseline OCTA information on patients is difficult. Patient data collected over the long term is required for evaluating disease progression; therefore, we had to utilize OCT and OCTA data collected from different points in time. However, as we mentioned previously in the discussion, the deep retinal layer is relatively unaffected by glaucoma progression, and under well controlled IOP, there might be minimal compression of blood vessels in the lamina. Thus, deep VD could be used as a surrogate of baseline ocular blood flow. In addition, the retrospective profile of this study could be another limitation. In future study, prospective research that incorporates baseline OCTA data might be more valuable for predicting glaucoma progression. A second limitation of our study was that VF test could have fluctuation of accuracy. To minimize this weakness, both automated GPA program and MD slope were evaluated to assess progression of VF. Also, strict reliability assessment was performed when including subjects. Third, our study was limited because it could not evaluate the effect of systemic vasoactive medication such as BB for hypertension medication on VD. According to chart review, we identified that only two patients took systemic beta-blocker as hypertension medication, but if the patients were prescribed drugs at other hospitals, there must be missed information. A larger number of study participants might be needed for assessing the relationship between systemic vasoactive medication and VD. Fourth, we could not totally exclude the patients with cataract or multifocal intraocular lens insertion that could affect the quality of OCTA image. So, we tried to minimize the interference by restricting the collected OCTA with image quality over 70.
In conclusion, the status of the deep retinal vascular circulation might be a useful and direct indicator of local ocular blood circulation, and OCTA could be used to assess it. Indeed, deep VD values, as measured by OCTA, might be predictive of the risk of deterioration of visual function in glaucoma.
Materials and Methods
Subjects
This study was approved by the Institutional Review and Ethics Boards of Seoul St. Mary’s Hospital, South Korea. Informed consent was obtained from every subject. All work was performed according to the tenets of the Declaration of Helsinki. The subjects of the current study were enrolled from the ongoing Catholic Medical Center Glaucoma Progression Study (CMC-GPS), which was initiated in 2009 at Seoul St. Mary’s Hospital. The collected data in this study was accumulated from 2009 to 2018.
A total of 104 eyes from 104 OAG patients with IOP under 21 mmHg was included. Only patients with at least 5 years of follow-up were included in this study and all subjects visited our clinic every 3 months with fundus photography. VF test and OCT evaluation were performed at 6-month intervals for the first 3 years after diagnosis of glaucoma and annually thereafter.
The inclusion criteria for the study were as follows: (1) age between 20 and 79 years, (2) IOP ≤ 21 mmHg with IOP-lowering medication, (3) best corrected visual acuity of 20/40 or better, (4) open angle on gonioscopy, (5) spherical equivalent within ±5.0 diopters, and (6) no history of disease affecting visual pathways, retinal disease, or optic neuritis. If both eyes satisfied the inclusion criteria, the right eye was selected. Patients with a history of incisional glaucoma surgery or laser trabeculoplasty were excluded.
All subjects underwent comprehensive ophthalmic examinations, which included the following: report of systemic disease, best-corrected visual acuity, slit-lamp examination, Goldmann applanation tonometry, gonioscopy, and dilated stereoscopic examination of the optic disc. Red-free fundus photography (Canon, Tokyo, Japan), Cirrus OCT (Carl Zeiss Meditec), and Humphrey VF examination using the Swedish interactive threshold standard algorithm (SITA) 24-2 (Carl Zeiss Meditec) were also performed.
Glaucomatous VF defects satisfied following the following conditions: (1) glaucoma hemifield test results were outside normal limits (2) ≥3 adjacent points with a probability of <5% of the normal population, with one of these points having a probability of <1%, or (3) a pattern standard deviation (PSD) with a P value < 5%. Two glaucoma specialists confirmed the glaucomatous field defects (SJJ and HYP). We considered the VF results to be reliable as follows: when fixation loss was <20%, the false-positive rate was <15%, and the false-negative rate was <15%.
Vessel density evaluation using OCT angiography
The vascular status of the macula was imaged using swept-source OCTA device (DRI OCT Triton; Topcon). The central wavelength of 1050 nm and scan speed of 100,000 A-scans per second were applied. A 3 × 3 mm macular scan was obtained and active eye tracker system was used to reduce motion artifacts during imaging. En face images via automated layer segmentation were acquired. The superficial retinal vascular plexus corresponds to the region starting from 2.6 μm below the internal limiting membrane to 15.6 μm below the junction of the inner plexiform layer (IPL) and INL (IPL/INL). The deep retinal vascular plexus reach from 15.6 μm below IPL/INL to 70.2 μm below IPL/INL.
To calculate macular VD, a binary slab image was created by ImageJ software (National Institutes of Health, Bethesda, MD, USA) as described by our group and others11,37,38. The binarized image was converted to a red-green-blue (RGB) color model and then split into three channels corresponding to red, green, and blue. The red channel was chosen as the reference. After using the “adjust threshold” tool, which automatically sets lower and upper threshold values, images were segmented into an area of interest and background. The white pixels were designated “vessel” and black pixels designated “background”, and the VD was calculated as a percentage from the total area of the white pixels divided by the total area of the image.
To reduce image quality fluctuation, the examinations were performed by one trained examiner. Only images with image quality scores greater than 70 were selected. OCTA images containing motion artifacts or blurred vessel contours that interfered with the clarity of vascular status were excluded. In the case of deep retinal angiogram images with projection artifacts from superficial retinal vessel, those images were also excluded. The quality of en face image was independently evaluated by three glaucoma specialists (SJJ, HYP, and CKP).
Definition of VF progression
The presence of glaucomatous VF progression was assessed by trend-based analysis using Guided Progression Analysis (GPA) software. In trend-based analysis, eyes with a significant negative regression slope with a probability value less than 0.05 were defined as having glaucomatous VF progression. In addition, the rate of VF progression was calculated as the mean deviation (MD) slope and recorded as decibels per year (dB/yr). To minimize the effect of subjectivity in VF testing, all patients were required to produce at least 5 reliable VF tests, and the first result was excluded from the calculation of the MD slope.
Statistical analysis
All descriptive results were calculated as the value of mean and standard deviation. All OCT parameters used for analysis were measurements from the initial examination. Correlation coefficients were calculated to evaluate the relationship between the MD slope and clinical or ocular parameters by Pearson correlation analysis. Linear regression analysis was applied to assess meaningful factors affecting the MD slope. After categorizing subjects as progressors or non-progressors according to GPA analysis, we used the Student’s t test and chi-square test to compare continuous or categorical variables between progressors and non-progressors. Logistic regression analysis was used to identify factors associated with glaucomatous VF progression, and the Cox proportional hazards model was applied to reflect different follow-up periods between subjects. All statistical analyses were performed with SPSS version 24.0 (SPSS Inc., Chicago, IL, USA) and P < 0.05 was considered to be statistically significant.
Supplementary information
Acknowledgements
None of the authors has any proprietary interests in any device or drug mentioned in the article.
Author contributions
Soo Ji Jeon wrote the main manuscript text. Soo Ji Jeon, Da-Young Shin and Hae-Young Lopilly Park performed the data review and analysis. The critical revision of the manuscript was done by Chan Kee Park. All authors reviewed the manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
is available for this paper at 10.1038/s41598-019-53354-4.
References
- 1.Weinreb RN, Khaw PT. Primary open-angle glaucoma. Lancet (London, England) 2004;363:1711–1720. doi: 10.1016/S0140-6736(04)16257-0. [DOI] [PubMed] [Google Scholar]
- 2.Hazin R, Hendrick AM, Kahook MY. Primary open-angle glaucoma: diagnostic approaches and management. Journal of the National Medical Association. 2009;101:46–50. doi: 10.1016/S0027-9684(15)30811-7. [DOI] [PubMed] [Google Scholar]
- 3.Choi J, Kook MS. Systemic and Ocular Hemodynamic Risk Factors in Glaucoma. BioMed research international. 2015;2015:141905. doi: 10.1155/2015/141905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Drance S, Anderson DR, Schulzer M. Risk factors for progression of visual field abnormalities in normal-tension glaucoma. American journal of ophthalmology. 2001;131:699–708. doi: 10.1016/S0002-9394(01)00964-3. [DOI] [PubMed] [Google Scholar]
- 5.Bengtsson B, Leske MC, Yang Z, Heijl A, Group E. Disc hemorrhages and treatment in the early manifest glaucoma trial. Ophthalmology. 2008;115:2044–2048. doi: 10.1016/j.ophtha.2008.05.031. [DOI] [PubMed] [Google Scholar]
- 6.Moore NA, et al. Baseline retrobulbar blood flow is associated with both functional and structural glaucomatous progression after 4 years. The British journal of ophthalmology. 2017;101:305–308. doi: 10.1136/bjophthalmol-2016-308460. [DOI] [PubMed] [Google Scholar]
- 7.Shoshani Y, et al. Impaired ocular blood flow regulation in patients with open-angle glaucoma and diabetes. Clinical & experimental ophthalmology. 2012;40:697–705. doi: 10.1111/j.1442-9071.2012.02778.x. [DOI] [PubMed] [Google Scholar]
- 8.Yarmohammadi A, et al. Relationship between Optical Coherence Tomography Angiography Vessel Density and Severity of Visual Field Loss in Glaucoma. Ophthalmology. 2016;123:2498–2508. doi: 10.1016/j.ophtha.2016.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen HS, Liu CH, Wu WC, Tseng HJ, Lee YS. Optical Coherence Tomography Angiography of the Superficial Microvasculature in the Macular and Peripapillary Areas in Glaucomatous and Healthy Eyes. Investigative ophthalmology & visual science. 2017;58:3637–3645. doi: 10.1167/iovs.17-21846. [DOI] [PubMed] [Google Scholar]
- 10.Yarmohammadi A, et al. Peripapillary and Macular Vessel Density in Patients with Glaucoma and Single-Hemifield Visual Field Defect. Ophthalmology. 2017;124:709–719. doi: 10.1016/j.ophtha.2017.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jeon SJ, Park HL, Park CK. Effect of Macular Vascular Density on Central Visual Function and Macular Structure in Glaucoma Patients. Scientific reports. 2018;8:16009. doi: 10.1038/s41598-018-34417-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abegao Pinto L, et al. Ocular blood flow in glaucoma - the Leuven Eye Study. Acta Ophthalmol. 2016;94:592–598. doi: 10.1111/aos.12962. [DOI] [PubMed] [Google Scholar]
- 13.Caprioli J, Coleman AL. Blood pressure, perfusion pressure, and glaucoma. American journal of ophthalmology. 2010;149:704–712. doi: 10.1016/j.ajo.2010.01.018. [DOI] [PubMed] [Google Scholar]
- 14.Costa VP, et al. Ocular perfusion pressure in glaucoma. Acta Ophthalmol. 2014;92:e252–266. doi: 10.1111/aos.12298. [DOI] [PubMed] [Google Scholar]
- 15.Grudzinska E, Modrzejewska M. Modern Diagnostic Techniques for the Assessment of Ocular Blood Flow in Myopia: Current State of Knowledge. Journal of ophthalmology. 2018;2018:4694789. doi: 10.1155/2018/4694789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Riva CE, Geiser M, Petrig BL. Ocular blood flow assessment using continuous laser Doppler flowmetry. Acta Ophthalmol. 2010;88:622–629. doi: 10.1111/j.1755-3768.2009.01621.x. [DOI] [PubMed] [Google Scholar]
- 17.Briers D, et al. Laser speckle contrast imaging: theoretical and practical limitations. Journal of biomedical optics. 2013;18:066018. doi: 10.1117/1.JBO.18.6.066018. [DOI] [PubMed] [Google Scholar]
- 18.de Carlo TE, Romano A, Waheed NK, Duker JS. A review of optical coherence tomography angiography (OCTA) International journal of retina and vitreous. 2015;1:5. doi: 10.1186/s40942-015-0005-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spaide RF, Fujimoto JG, Waheed NK, Sadda SR, Staurenghi G. Optical coherence tomography angiography. Progress in retinal and eye research. 2018;64:1–55. doi: 10.1016/j.preteyeres.2017.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nemiroff J, Phasukkijwatana N, Sarraf D. Optical Coherence Tomography Angiography of Deep Capillary Ischemia. Developments in ophthalmology. 2016;56:139–145. doi: 10.1159/000442806. [DOI] [PubMed] [Google Scholar]
- 21.Campbell JP, et al. Detailed Vascular Anatomy of the Human Retina by Projection-Resolved Optical Coherence Tomography Angiography. Scientific reports. 2017;7:42201. doi: 10.1038/srep42201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shin JW, Sung KR, Lee JY, Kwon J, Seong M. Optical coherence tomography angiography vessel density mapping at various retinal layers in healthy and normal tension glaucoma eyes. Graefe’s archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2017;255:1193–1202. doi: 10.1007/s00417-017-3671-4. [DOI] [PubMed] [Google Scholar]
- 23.Lommatzsch C, Rothaus K, Koch JM, Heinz C, Grisanti S. OCTA vessel density changes in the macular zone in glaucomatous eyes. Graefe’s archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2018;256:1499–1508. doi: 10.1007/s00417-018-3965-1. [DOI] [PubMed] [Google Scholar]
- 24.Moghimi S, et al. Macular and Optic Nerve Head Vessel Density and Progressive Retinal Nerve Fiber Layer Loss in Glaucoma. Ophthalmology. 2018;125:1720–1728. doi: 10.1016/j.ophtha.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 25.Leske MC, et al. Archives of ophthalmology (Chicago, Ill.: 1960) 2003. Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial; pp. 48–56. [DOI] [PubMed] [Google Scholar]
- 26.Coleman AL, Miglior S. Risk factors for glaucoma onset and progression. Surv Ophthalmol. 2008;53(Suppl1):S3–10. doi: 10.1016/j.survophthal.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 27.Nitta K, et al. Prediction of Visual Field Progression in Patients with Primary Open-Angle Glaucoma, Mainly Including Normal Tension Glaucoma. Scientific reports. 2017;7:15048. doi: 10.1038/s41598-017-15267-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leske MC, et al. Predictors of long-term progression in the early manifest glaucoma trial. Ophthalmology. 2007;114:1965–1972. doi: 10.1016/j.ophtha.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 29.Leske MC, Heijl A, Hyman L, Bengtsson B, Komaroff E. Factors for progression and glaucoma treatment: the Early Manifest Glaucoma Trial. Current opinion in ophthalmology. 2004;15:102–106. doi: 10.1097/00055735-200404000-00008. [DOI] [PubMed] [Google Scholar]
- 30.Heijl A, Buchholz P, Norrgren G, Bengtsson B. Rates of visual field progression in clinical glaucoma care. Acta Ophthalmol. 2013;91:406–412. doi: 10.1111/j.1755-3768.2012.02492.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Matlach J, et al. Investigation of intraocular pressure fluctuation as a risk factor of glaucoma progression. Clin Ophthalmol. 2019;13:9–16. doi: 10.2147/OPTH.S186526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Drance S, Anderson DR, Schulzer M. & Collaborative Normal-Tension Glaucoma Study, G. Risk factors for progression of visual field abnormalities in normal-tension glaucoma. American journal of ophthalmology. 2001;131:699–708. doi: 10.1016/S0002-9394(01)00964-3. [DOI] [PubMed] [Google Scholar]
- 33.Park HY, Park SH, Park CK. Central visual field progression in normal-tension glaucoma patients with autonomic dysfunction. Investigative ophthalmology & visual science. 2014;55:2557–2563. doi: 10.1167/iovs.13-13742. [DOI] [PubMed] [Google Scholar]
- 34.Verma S, et al. Visual Field Progression in Patients with Primary Angle-Closure Glaucoma Using Pointwise Linear Regression Analysis. Ophthalmology. 2017;124:1065–1071. doi: 10.1016/j.ophtha.2017.02.027. [DOI] [PubMed] [Google Scholar]
- 35.Kim, J. H. et al. Risk Factors For Fast Visual Field Progression In Glaucoma. American journal of ophthalmology (2019). [DOI] [PubMed]
- 36.Heijl A, et al. Archives of ophthalmology (Chicago, Ill.: 1960) 2002. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial; pp. 1268–1279. [DOI] [PubMed] [Google Scholar]
- 37.Battaglia Parodi M, et al. Vascular abnormalities in patients with Stargardt disease assessed with optical coherence tomography angiography. The British journal of ophthalmology. 2017;101:780–785. doi: 10.1136/bjophthalmol-2016-308869. [DOI] [PubMed] [Google Scholar]
- 38.Ting DSW, et al. Optical Coherence Tomographic Angiography in Type 2 Diabetes and Diabetic Retinopathy. JAMA Ophthalmol. 2017;135:306–312. doi: 10.1001/jamaophthalmol.2016.5877. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.