Abstract
The current study is based on the AFM1 contamination of milk determined from April 2013 to December 2018 in the framework of a self-control plan of six milk processing plants in Italy. These data – together with the consumption data of milk consumers – were evaluated and used for the calculation of the Estimated Daily Intake (EDI), the Hazard Index (HI), and the fraction of hepatocarcinoma cases (HCC) due to AFM1 exposure in different population groups. Altogether a total of 31,702 milk samples were analyzed, representing 556,413 tons of milk, which is an outstanding amount compared to published studies. The results indicate the monthly fluctuation of AFM1 levels through a period of nearly 6 years. The EDI of AFM1 in different population groups was in the range of 0.025–0.328 ng kg−1 body weight (bw) per day, based on the average consumption levels and weighted mean contamination of the milk in the study period. Considering average consumptions, in the groups of infants and toddlers, the HI calculation resulted in 1.64 and 1.4, respectively, while for older age groups, it was <1. The estimated fractions of HCC incidences attributable to the AFM1 intakes were 0.005 and 0.004 cases per 100,000 individuals in the 0–0.9 and 1–2.9-year age groups, respectively, and below 0.004 cases in the other age categories. The monthly average AFM1 contamination of tested milk consignments ranged between 7.19 and 22.53 ng kg−1. Although the results of this extensive investigation showed a low risk of HCC, the variability of climatic conditions throughout years that influence AFB1 contamination of feed and consequently AFM1 contamination of milk justifies their continuous monitoring and update of the risk assessment.
Keywords: Aflatoxin M1, enzyme-linked immunosorbent assay, cow’s milk, raw milk, exposure assessment, food safety risk
Introduction
Aflatoxins (AFs) are secondary metabolites produced by Aspergillus flavus, Aspergillus parasiticus, and Aspergillus nominus fungi under certain growing and storage conditions (WHO, 1997; Giorni et al., 2007). The AFs consisted of Aflatoxin B1, B2, G1, and G2 may contaminate food and feed. Maize grains and other feedstuffs such as corn silage, soybean, and press cakes from oil plants can be commonly contaminated by Aspergillus spp. The critical factors facilitating the growth of Aflatoxin-producing molds in corn grains and silage include among others: lack of good agricultural (Kebede et al., 2012), storage practices, and unfavorable climatic conditions (FAO/WHO Codex Alimentarius, 2014; Frazzoli et al., 2017). The risk of Aflatoxin contamination is generally higher in geographical regions with a tropical climate or a subtropical climate (Fakhri et al., 2019a), but an extreme hot and droughty season may promote the growth of Aspergillus spp. in crops and increases their AF contamination as reported in the South and Southwestern regions of Europe (Trevisani et al., 2014; Milićević et al., 2017; Udovicki et al., 2019), the United States (Fakhri et al., 2019a), Turkey (Madali et al., 2018), and in other regions (Rama et al., 2015; Rahmani et al., 2018; Pardakhti and Maleki, 2019). The effects of such conditions on the Aflatoxin contamination of maize prevailed in 2003 and 2012 in the Po valley were evaluated in detail by Canever et al. (2004) and Marchetti et al. (2013).
AFM1 contamination in milk was also reported from a number of countries (EFSA, 2004; Cano-Sancho et al., 2013; Duarte et al., 2013; Tsakiris et al., 2013; Trevisani et al., 2014; Fakhri et al., 2019a,b). In Italy, due to its climatic conditions, the Po valley is considered one of the highest risk areas in this regard, which happens to be the region that produces most of the milk in the country (Frazzoli et al., 2017). Several factors may affect the AFM1 contamination of milk, for example, environmental conditions (Giorni et al., 2007; Prandini et al., 2009; Kebede et al., 2012; Miliĉeviĉ et al., 2019; Fakhri et al., 2019a), different farming and feeding practices, and the quality and safety control system of the food business operators concordant with the different legislations in force.
The mother’s milk may also contain AFM1 in comparable concentrations to the dairy cow’s milk (Kunter et al., 2017; Radonić et al., 2017; Bogalho et al., 2018; Valitutti et al., 2018; Fakhri et al., 2019a,b).
These conditions justify the increased activity in Italy in the field of basic research (Perrone et al., 2014), biological control (e.g., use of non-aflatoxin-producing strains; Mauro et al., 2014, 2018), monitoring of Aflatoxin levels throughout the milk value chain (Anfossi et al., 2011; Kerekes et al., 2016), development and application of different prevention and intervention procedures (Gallo and Masoero, 2010), analytical methods, and validation protocols for the detection of Aflatoxins (Rosi et al., 2007; Bellio et al., 2016).
If ruminants are fed with contaminated feed, the Aflatoxin B1 consumed by the animals is partly degraded by the forestomach before reaching the circulatory system. The remaining part is transformed by the liver into monohydroxy derivative forms: mainly AFM1, and in smaller quantities AFM2, AFM4, and other metabolites such as aflatoxicol. Afterward, it is being secreted into the milk through the mammary glands (Frazzoli et al., 2017). In dairy cows, the excretion takes 12–24 h after AFB1 intake, and the depuration interval is about 2–3 days after the animals are fed with AFB1-free feed. The excreted amount of toxin through milk varies between 1 and 6% of ingested AFB1, depending on the variety of dairy cows and the amount of produced milk. The high-yielding breeds have higher carry-over rate (Tsakiris et al., 2013).
The exposure to Aflatoxins – and other mycotoxins – compromises the health of animals and humans as well (Kunter et al., 2017). The International Agency for Research on Cancer (2002) classified AFB1 to Group 1 of carcinogenic substances for humans. Therefore, no tolerable daily intake (TDI ng AFB1 kg−1 bw day−1) could be set for this substance, and the exposure levels should be kept as low as reasonably achievable. AFM1 has 2–10% of the carcinogenic potency of AFB1 but has the same liver toxicity (Hsieh et al., 1984; Cullen et al., 1987).
Milk is a very important food that provides macro- and micronutrients for the growth and development of the body and for the maintenance of human health, but its AFM1 contamination may impose health risk for the consumers. AFM1 is heat stable and processing, and storage conditions are ineffective in reducing the concentration of AFM1 in milk and milk products (Joint FAO/WHO Expert Committee on Food Additives, 2001; Campagnollo et al., 2016).
The presence of AFM1 in milk and milk products, even in small quantities, represents a concern, mainly because these products are widely consumed by children who are more susceptible to the toxic effects of Aflatoxins, due to their underdeveloped metabolic and immune system (Gonzales-Osnaya et al., 2008; Kunter et al., 2017; Fakhri et al., 2019a).
In view of its hepatotoxicity and potential carcinogenicity, the regulatory agencies established maximum permissible levels for AFM1 in milk ranging from 10 to 500 ng kg−1 (FAO/WHO Codex Alimentarius, 1995; European Community, 2006; USA Guidance levels; Bogalho et al., 2018) following the principle of “As low as reasonably achievable” (ALARA), taking into account the inevitable Aflatoxin contamination of feed.
Quantitative exposure assessment is a methodology developed to evaluate the probable intake of chemical substances via food. Aflatoxins are genotoxic and carcinogenic; therefore, there is no intake level, which can be considered risk free (EFSA Scientific Committee, 2007). The safe dose proposed by Kuiper-Goodman (1990) was derived from the dose causing 50% of the animals developing tumor (TD50) divided by a safety factor of 50,000. The suggested value is 0.2 ng kg−1 of body weight, which was derived from extrapolation to a risk level of 1:100,000. The risk from exposure to genotoxic and carcinogenic substances found in food and feed can be characterized by the margin of exposure (MoE). The MoE provides an indication of the level of safety concern about a contaminant’s presence in food, but it does not quantify the risk as such. As stated by EFSA Scientific Committee (2012), if it is based on the BMDL10 from an animal study, a margin of exposure of 10,000 or higher (in view of uncertainties) considered being of low concern from a public health point of view. Risk characterization, based on the estimated human exposure and available toxicological reference values, provides important information for risk managers on the probability of occurrence and severity of potential adverse health effects to implement appropriate control measures for assuring the safety of food (Leblanc et al., 2005).
The objectives of this study were to evaluate the annual and monthly fluctuation of AFM1 contamination of milk over a period of 5.5 years, the human exposure, and the potential risk of consumers in different age categories based on the vast amount of AFM1 contamination data in milk representing a significant proportion produced and marketed in Italy during the study period, and use these results to justify the need for continuous monitoring of AFM1 contamination in milk.
Materials and Methods
To provide baseline data for future evaluation of the change in AFM1 contamination, the milk collected in six dairy plants from April 2013 to December 2018 in the framework of a self-control plan of the Italian dairy industry is investigated. The milk processing plants, located in Northern, Central, and Southern Italy, collected about 465 million liters of milk per year. Five of them applied the same self-control plan using 40 ng kg−1 AFM1 concentration as action limit (AL), while one plant used a 30 ng kg−1 AL. When the AFM1 concentration of the sample reached the AL, the dairy farms were informed, and corrective measures were applied on the farm level in order to avoid high contamination of the milk. The milk was collected from about 650 dairy farms. The routing of the trucks covering diverse number of dairy farms – depending on the amount of milk produced by each farm – was decided on the basis of logistic optimization. Three types of milk were collected: (1) high quality milk (HQM); (2) normal quality milk (NQM); and (3) organic milk (OM). In case of the truck collected milk from different farms, the milk of the same type was mixed, but the three types of milk (HQM, NQM, and OM) were loaded in different compartments of the truck.
Description of the Self-Control Plan
The self-control plan applied for the control of AFM1 content starts with sampling of the milk of the truck before unloading its content. If trucks contained different types of milk, the personnel of the milk processing plants collected one sample from each type of milk during the discharge of the tanker. All samples were analyzed immediately by a rapid commercial immunochromatographic test (Charm MRLAFMQ® Charm Science INC, Lawrence, MA, USA) utilizing highly specific reactions between antibodies and AFM1. It detects AFM1 at or above 25 ng kg−1 in milk and suitable to indicate the compliance with EU ML of 50 ng kg−1. To obtain quantitative data for the AFM1 as part of a separate program, different milk batches of each collecting zone were also sampled and analyzed at least twice a month with an ELISA kit (Immunoscreen AFM1, Tecna s.r.l., Trieste, Italy), which was validated within the range of 2.5–100 ng L−1 giving linear response up to 80 ng L−1 (Rosi et al., 2007). Note that the AFM1 contamination was reported in some cases from 1 ng kg−1, which is the limit of detection of the ELISA method applied. The ISO (1998) HPLC-FD reference method (LOQ: 8 ng L−1, linearity 3–1,000 ng L−1) was used for confirmation of values higher than 50 ng kg−1. The procedures were performed by the dairy plants as described by Rosi et al. (2007). The performance characteristics of the methods were regularly tested by the plants and periodically verified by the official inspectors according to the HACCP plan of the industries. No further validations of the methods were carried out.
After confirmation that the AFM1 concentration exceeded the legal limit, the competent authority was informed in accordance with the Italian law (Ministero della Salute, 2013). The plants did not process milk with AFM1 content higher than 50 ng kg−1. In view of the inevitable uncertainty of detection with CHARM test and the biweekly frequency of analyses with ELISA tests for obtaining the possible most realistic information on the exposure levels, the AFM1 content higher than 50 ng kg−1 determined with HPLC was used to complement the database obtained with ELISA tests, which did not cover all milk consignments. Data of AFM1 concentration together with the quantity of milk unloaded from each truck were used to calculate the weighted mean AFM1.
Characterization of Data and Exposure Estimation
Descriptive statistical parameters of the AFM1 concentrations [mean, weighted mean (weight was assigned according to the quantity of milk loaded from the sampled trucks), standard deviation, median, percentile values, and their confidence intervals] were calculated for HQM, NQM, and OM. The percentile values were calculated with NIST method (NIST/SEMATECH, 2013). The confidence intervals of the mean and percentile values of the three types of milk were overlapping; hence, there was no significant difference between them.
Dietary Exposure Assessment and Risk Characterization
Food consumption data were obtained from the Comprehensive Food Consumption Database of EFSA1. The database contained data derived from the Italian National Food Consumption Survey (INRAN-SCAI) conducted from October 2005 to December 2006. It involved 3,322 consumers from 1,329 households located in the four main geographical areas of Italy (North-West, North-East, Centre and South, and Islands; Leclercq et al., 2009). The exposure assessment is based on the mean and 95th percentile “Cattle milk” consumption data of “consumers only” of each population groups: infants (0–0.9 years), toddlers (1–2.9 years), other children (3–9.9 years), adolescents (10–17.9 years), adults (18–64.9 years), elderly (65–74.9), and very elderly (>75). The proportion of milk consumers of the respective population groups is presented in Table 1.
Table 1.
Mean body weight and cow milk consumption data used for Estimated Daily Intake (EDI) calculation in different age groups.
| Population Group | Number of consumers | Percentage of milk consumers1 | Mean consumption (g day−1) | 95th percentile consumption (g day−1) | Mean body weight (kg) |
|---|---|---|---|---|---|
| Infants | 2,3962 | 36.61% | 131.522 | 348.132 | 5.00 |
| Toddlers | 333 | 91.67% | 269.013 | 600.003 | 12.00 |
| Other children | 184 | 95.34% | 205.98 | 392.50 | 26.10 |
| Adolescents | 208 | 84.21% | 177.80 | 305.42 | 52.60 |
| Adults | 1,733 | 74.92% | 136.03 | 275.88 | 70.00 |
| Elderly | 223 | 76.90% | 141.10 | 266.25 | 70.10 |
| Very elderly | 188 | 82.46% | 177.13 | 337.19 | 70.10 |
Percentage of population groups consuming milk in Italy. EFSA, The Comprehensive Food Consumption Database (2018).
Because the number of consumption data was low (5), the original data were substituted by the calculated European averages: 132 and 348 g day−1.
Although the number of consumption data was also low in this category, the data were not substituted, because they were the same as the European averages: 270 and 600 g day−1.
Data used for EDI calculation are summarized in Table 1. Since the number of consumers (5) in the infant category was low, these consumption data were substituted by the cattle milk consumption of all available (infant) consumers in the EFSA database in order to provide an approximate estimate for the mean consumption values for the Italian population. The 95th percentile exposure calculations were carried out only on a monthly basis because it is not realistic that such high quantity of milk is consumed over the year.
The estimated daily intakes (EDI: ng kg−1 bw day−1) of the population groups were calculated as:
Monthly, yearly, and four-year average EDI values were calculated from the corresponding weighted mean (WM) AFM1 concentrations unloaded from the tankers in the given period of time and the average (AC) and large portion size (95th percentile – as worst-case scenario calculation) consumption data (kg/day).
In order to calculate hazard indices (HI), the monthly, yearly, and four-year average estimated daily intakes were divided with 0.2 (Kuiper-Goodman, 1990). The same approach was also used in other studies (Shundo et al., 2009; Duarte et al., 2013; Tsakiris et al., 2013; Kerekes et al., 2016).
Because BMDL10 value is not available for AFM1, the BMDL10 of AFB1 (870 ng kg−1 bw day−1) was used as a conservative value. MoE was calculated by dividing the benchmark dose for a 10% increase in hepatocellular carcinoma (HCC) incidence (BMDL10) by the human exposure (EDI) values. The MoE then was divided by the mean or 95th percentile EDI values for each population groups. The calculation was carried out for each month from April 2013 to December 2018.
The prevalence of carriers of hepatitis B (HBV) in the Italian population is between 1.2 and 2% (Serraino et al., 2003). The risk potency was calculated assuming that 2% of population is HBV+ and using the cancer potencies for AFB1, which was estimated by JECFA to be 0.01 for hepatitis B surface antigen negative (HBsAg–) individuals and 0.3 for HBsAg+ individuals (JECFA, 1998). Based on the given cancer potencies, the risk potency can be calculated as follows = 0.01 × 98% + 0.3 × 2% = 0.016 HCC/year per 100,000 persons (Cano-Sancho et al., 2013). The proportion of population at risk was estimated by multiplying the risk potency with the BMDL10 and then dividing with the MoE considering the mean and 95th percentile of exposure estimation:
Results
Aflatoxin M1 Results
A total of 31,702 milk samples were analyzed for AFM1, representing 556,413 tons of milk, which comprised 16,107 (304,625,633 kg), 13,726 (222,189,472 kg), and 1,869 (29,598,042 kg) trucks (batches) of HQM, NQM, and OM, respectively, during 2013–2018.
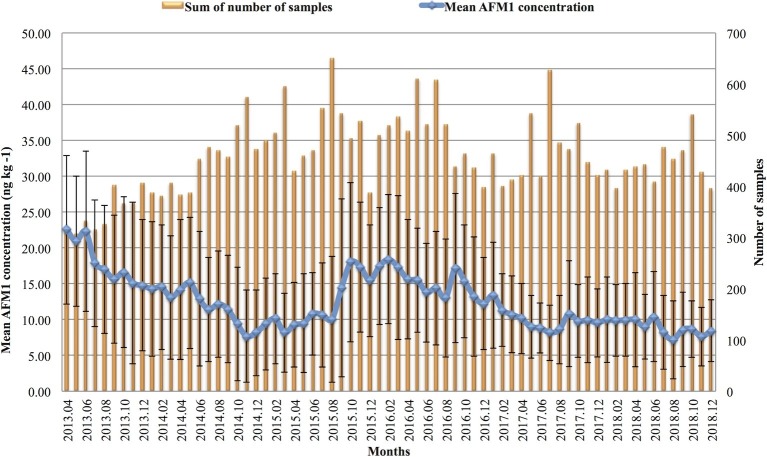
As the confidence intervals of the median values of the AFM1 contamination in HQM and NQM overlapped, these data were merged into one subset (AQM – average quality milk). The difference between the Northern, Central, and Southern regions was negligible, however, the median values of AQM were statistically different from that of organic milk (OM 8 ng kg−1) collected only in the Northern region. Details of the descriptive statistics of the AFM1 levels for AQM and OM are reported in Table 2. The differences between the number of samples taken in each region should be noted. Figure 1 demonstrates the changes occurring throughout the years. In 2017 and 2018, the levels of contamination were about the same as it was observed from December 2014 through August 2015. However, between September 2015 and December 2016, the AFM1 contamination was nearly as high as in 2013 during the Aflatoxin crisis.
Table 2.
Distribution of Aflatoxin M1 concentration (ng kg−1) in different milk types and in various geographical areas of Italy during the 5.5-year period.
| OM1 Northern Italy | AQM2 Northern Italy | AQM2 Central Italy | AQM2 Southern Italy | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of samples | 1,869 | 20,574 | 2,438 | 6,821 | ||||||||
| Confidence intervals | 95% CI | (LCL-UCL) | 95% CI | (LCL-UCL) | 95% CI | (LCL-UCL) | 95% CI | (LCL-UCL) | ||||
| Mean concentration | 10.3 | 9.9 | 10.6 | 12.6 | 12.5 | 12.7 | 13.3 | 12.9 | 13.6 | 11.4 | 11.3 | 11.6 |
| SD | 7.7 | 8.5 | 8.6 | 7.5 | ||||||||
| Median | 8 | 8 | 9 | 10 | 10 | 11 | 11 | 11 | 11 | 9 | 9 | 10 |
| P0.90 | 18 | 17 | 20 | 23 | 23 | 23 | 24 | 24 | 26 | 21 | 20 | 21 |
| P0.95 | 24 | 23 | 27 | 28 | 28 | 29 | 30 | 29 | 33 | 26 | 25 | 27 |
| P0.975 | 30 | 29 | 33 | 34 | 34 | 35 | 38 | 35 | 40 | 32 | 30 | 33 |
| P0.99 | 41 | 36 | 49 | 41 | 40 | 41 | 43 | 41 | 46 | 40 | 38 | 40 |
| Weighted mean concentration | 10.8 | 10.4 | 11.1 | 12.6 | 12.5 | 12.6 | 13.4 | 13.0 | 13.7 | 11.7 | 11.6 | 11.9 |
The percentile values (P0.90–P0.99) were calculated with the NIST method; LCL and UCL are the lower and upper 95% confidence intervals (CI).
Organic milk.
Average quality milk.
Figure 1.
Monthly summary of the total number of samples analyzed and the mean Aflatoxin M1 (AFM1) concentration and standard deviation of milk samples in the given month.
Exposure Assessment
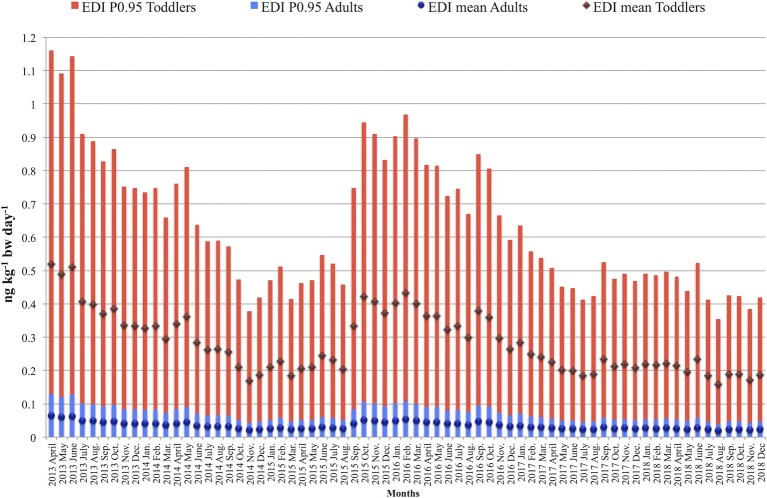
The monthly and yearly averages of EDI, HI, and liver cancer incidence (LCI) values were calculated together with their average values for the whole study period. In Figure 2, the results of monthly EDI calculations, based on mean and large portion size consumption (95th percentile) data, are shown for two different age categories: toddlers and the adult population. Among adults, the mean EDI values varied between 0.02 and 0.08 ng kg−1 bw day−1 during the study period, and for the large portion size consumers, the results were between 0.04 and 0.13 ng kg−1 bw day−1. In the population of infants, mean EDI of AFM1 resulted in the monthly range of 0.19–0.61 ng kg−1 bw day−1, and in the range of 0.49–1.62 ng kg−1 bw day−1 considering the 95th percentile consumption values. Similarly, among toddlers, the mean EDI values varied between 0.16 and 0.52 ng kg−1 bw day−1. In case of large portion size consumers, the results ranged between 0.35 and 1.16 ng kg−1 bw day−1. Naturally, the EDI patterns throughout the years follow the same pattern as the weighted mean AFM1 concentrations presented in Figure 1.
Figure 2.
Monthly variation of Estimated Daily Intake (EDI) values of adults and toddlers during the 2013–2018 study period.
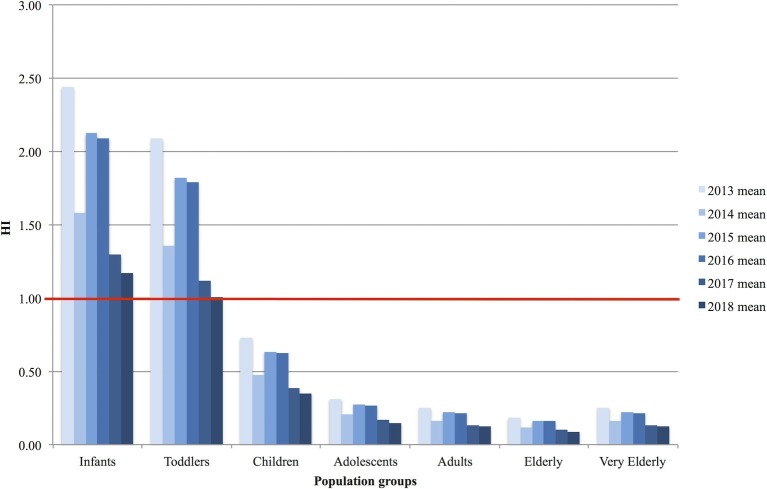
To facilitate the interpretation of EDI values, the corresponding hazard indices (HIs) were calculated by dividing the (monthly, yearly, or four-year average) EDI with 0.2 (the “safe dose”). The calculation shows the amount of AFM1 of concern (HI value >1). The results of yearly mean hazard index calculations for each population groups are presented in Figure 3.
Figure 3.
Yearly variation of mean Hazard Index (HI) values in the population groups throughout the 2013–2018 study period.
Over the age of 3 years, the HI was <1 considering mean intake values. However, for infants and toddlers, the observed intake levels resulted in HI values higher than 1 in each year during the study period.
The fraction of incidence of HCC or liver cancer incidence (LCI) attributable to the intake of AFM1 was taken into account on the basis of MoE considering the estimated mean exposure. The yearly average LCI values for the whole study period are reported for the population groups in Table 3. The calculation predicted a low additional number of cases in the examined age categories.
Table 3.
“Heat map” (scale: green-yellow-red) of the estimated yearly average liver cancer incidence (LCI) (cases per 100,000 people) in the Italian population by age groups during 2013–2018.
| Year/Age group | Infants | Toddlers | Children | Adolescents | Adults | Elderly | Very Elderly |
|---|---|---|---|---|---|---|---|
| 2013 | 0.0078 | 0.0067 | 0.0023 | 0.0010 | 0.0008 | 0.0006 | 0.0008 |
| 2014 | 0.0051 | 0.0043 | 0.0015 | 0.0006 | 0.0005 | 0.0004 | 0.0005 |
| 2015 | 0.0068 | 0.0058 | 0.0020 | 0.0009 | 0.0007 | 0.0005 | 0.0007 |
| 2016 | 0.0067 | 0.0057 | 0.0020 | 0.0009 | 0.0007 | 0.0005 | 0.0007 |
| 2017 | 0.0042 | 0.0036 | 0.0012 | 0.0005 | 0.0004 | 0.0003 | 0.0004 |
| 2018 | 0.0038 | 0.0032 | 0.0011 | 0.0005 | 0.0004 | 0.0003 | 0.0004 |
Based on the mean consumption and yearly weighted mean AFM1 concentration, the HCC incidence cases were between 0.0004 and 0.0008, 0.0032 and 0.0067, and 0.0038 and 0.0078 per 100,000 people for adults, toddlers, and infants, respectively. The highest risk group is the infants.
Discussion
The reported concentration of AFM1 in milk varied widely in recent years worldwide, ranging from non-detects to values up to 48,000 ng kg−1 (Shundo et al., 2009; Duarte et al., 2013; Tsakiris et al., 2013; Oluwafemi et al., 2014; Scaglioni et al., 2014; Temamogullari and Kanici, 2014; Flores-Flores et al., 2015; Rahmani et al., 2018; Fakhri et al., 2019a).
In our study, 63 (0.20%) raw milk samples collected from trucks contained AFM1 higher than 50 ng kg−1. These batches were discarded. The raw milk complying with EC regulation was processed to pasteurize and UHT milk as well as for cheese and other milk-based products. The mean AFM1 concentrations were between 10.3 ng kg−1 in OM and 12.4 ng kg−1 in AQM with a weighted mean of 10.9 and 12.5 ng kg−1, respectively. These data are comparable with the mean contamination levels previously reported in other European countries such as Spain (n = 603, mean = 9.69 ng L−1 in UHT milk; Cano-Sancho et al., 2013), France (n = 264, mean = 14.3 ng kg−1 in raw milk; Boudra et al., 2007), and Portugal (n = 40, mean = 23.4 ng L−1 in pasteurized milk; Duarte et al., 2013) except in Serbia (ranging from 5 to 1,260 ng kg−1; mean 71 ± 130; Milićević et al., 2017). The percentages of non-compliant samples were in the lower range of the results (0 and 9.1% in raw milk) reported in previous studies (Roussi et al., 2002; Rodríguez-Velasco et al., 2003; Martins et al., 2005; Boudra et al., 2007; Milićević et al., 2017).
Comparison of the results reported in this study (2013–2018) with data obtained during the mycotoxin crisis (1999–2004) by the same industry shows a clear reduction in AFM1 concentration. Both the percentage of milk batches containing AFM1 above the EU limit and the mean AFM1 concentration decreased (see Table 4). The investigations performed during 2005–2010 showed a higher percentage of non-compliant batches than the present investigation. The notable reduction of the ratio of samples over the legal limit is attributed to the regular monitoring of raw milk, and timely advice is given to the dairy farms for corrective measures.
Table 4.
AFM1 concentration and the ratio of non-compliant samples of raw milk collected in Italy by the same milk processing plants during a 17-year period.
| Year(s) | Number of samples | Mean AFM1 concentration (ng kg−1) | 95th percentile | Number of samples >50 ppt (%) | Reference |
|---|---|---|---|---|---|
| 2000–2001 | 791 | 27–30** | NA* | 23.5 | Serraino et al. (2003) |
| Jan. 2001-July 2004 | 2,512 | 29–34 | 80 | NA* | Trevisani et al. (2006) |
| Sep. 2003-July 2004 | 4,190 | 35 | 80 | NA* | Trevisani et al. (2006) |
| 2005 | 4,886 | 12–19** | 30–40** | 0.7–3.1** | Trevisani et al. (2014) |
| 2006 | 4,718 | 13–15** | 33–40** | 0.6–1.7** | Trevisani et al. (2014) |
| 2007 | 4,354 | 11–13** | 27–29** | 0.3–1.1** | Trevisani et al. (2014) |
| 2008 | 4,195 | 15–18** | 30–38** | 1.7–2.5** | Trevisani et al. (2014) |
| 2010 | 3,740 | 11–12** | 25–28** | 0.5–0.7** | Trevisani et al. (2014) |
| 2013–2014 | 9,017 | 13–17** | 29–35** | 0.24 | Kerekes et al. (2016) |
| 2013–2018 | 31,702 | 10–13** | 24–30** | 0.20 | Present study |
NA, data not available.
Range of AFM1 contamination detected in different types of milk (i.e. HQM, NQM, AQM, or OM) or in samples collected in different Italian regions.
In view of the similar mean AFM1 concentrations and the lack of data on the different consumption levels of HQM, NQM, or OM among the Italian population groups, the exposure assessment was performed using the combined database of all types of milk and the average daily milk consumption.
The EDI and HI results indicate that – due to the relatively large milk intake compared to their body weights – infants and toddlers are the two most exposed groups of the population to AFM1. As demonstrated in Figure 2, the EDI of the other population groups (adolescents-adults-elderly-very elderly) resulted in a significantly lower range of 0.01–0.18 ng kg−1 bw day−1, while infants and toddlers are exposed to 0.35–1.16 ng kg−1 bw day−1 daily intake levels. The latter data are in line with previously reported mean EDIs of 0.08 ng kg−1 bw day−1 (n = 40) in Portugal (Duarte et al., 2013), 0.09 ng kg−1 bw day−1 (n = 16) in France (Leblanc et al., 2005), and 0.18–0.20 ng kg−1 bw day−1 (n = 1,233) in Serbia (Milićević et al., 2017). The calculated monthly and yearly mean HI values were < 1 in the age groups of adolescents, adults, elderly, and very elderly, but for infants, toddlers, and children, the results are close to or well over 1, which means that the amount of AFM1 consumed with milk (Figure 3) might be a considerable risk. The higher HI values for younger consumers compared to older age groups are in agreement with the results of Tsakiris et al. (2013); however, the results of this study show a higher exposure level. The slight differences in the outcome of the two studies can be explained by the different calculation methods – considering “consumers only” in this study – and the number of samples.
The LCI estimated in other population groups is significantly lower (Table 3). The estimated fraction of incidence of HCC in the Italian population that predicted a slight increase in cases due to milk consumption is in line with those reported previously by Trevisani et al. (2006; 0.011–0.057 cases/100,000 people in different age categories).
The results of the current study represent the exposure of people consuming milk. Therefore, the estimates cannot be extrapolated to the whole age groups including non-consumers.
Comparison of our results with the previously reported ones should be made with caution, because the latter ones are based on much fewer samples taken within a short period of time compared to our database. Even the comprehensive review on the presence of mycotoxins in animal milk (Flores-Flores et al., 2015) covering 38 countries during the period of 1991–2012 includes results obtained based on 3–6,537 samples taken within 1 or 2 years. Our study is the first, which evaluates the monthly variation of AFM1 exposure, based on 300–650 samples per month totaling 31,702 samples during the period of almost 6 years (69 months), enabling the reliable estimation of the mean AFM1 concentrations, and the corresponding EDI values, and demonstrates their fluctuations over the years.
Conclusions
Although the results of this investigation showed a low risk of HCC for the adolescent and adult population attributable to intake of AFM1 via milk consumption during the study period (2013–2018), it should be considered that the present study does not include the AFM1 intake due to other milk-based products, e.g., cheese and yoghurt, which could add a notable amount to the estimated quantity consumed. Furthermore, it should be taken into account that our EDI calculations could not include the exposure derived from the consumption of mother’s milk either, because we had no data on the combined intake of breast milk and cow milk. Breast milk may also contain AFM1 derived from cow milk as well as from the mother’s food contaminated with AFB1 (Galvano et al., 2008; Radonić et al., 2017). In Italy, the AFM1 contamination was found in four (5%) breast milk samples [ranging from <7 to 140 ng L−1; mean = 55.35 ng L−1 (Galvano et al., 2008)]. Another Italian study revealed that AFM1 was detected in 37% of samples (mean = 12 ng L−1 ± SD = 11 ng ml−1; range = 3–340 ng L−1) taken from patients (n = 30) with celiac disease, while in the healthy control group, the mean AFM1 concentration levels (9 ± 07 ng L−1; range = 3–67 ng L−1) were lower (Valitutti et al., 2018). The latter results indicate that the exposure of infants can be substantially higher than our estimate depending on the dietary pattern of the mothers. Further investigation is needed to evaluate the total exposure for this contaminant for all population groups.
The previous Aflatoxin crisis due to high AFB1 contamination of maize has increased the awareness of the food safety risk managers; induced regulatory measures, research, and innovation activities; and reinforced the consciousness of the food business operators. Consequently, they have implemented strict monitoring and regular control along the feed and food chain utilizing the availability of rapid and less expensive detection kits. This self-control and corrective measures at dairy farms resulted in the slow decrease of AFM1 contamination.
Nevertheless, the variability of climatic conditions throughout years and the number of other factors that may influence AFB1 contamination of crops and consequently AFM1 contamination of milk underline the need of continuous monitoring of milk contamination and regular update of the exposure assessments.
Data Availability Statement
The datasets generated for this study will not be made publicly available. The dataset is based on confidential private industry data.
Author Contributions
ÁA, AS, and FG contributed to the conception and design of the study. AC and AZ organized the database. PB and KK performed the statistical analysis. AS wrote the first draft of the manuscript. KK, ZF, and ÁA finalized the manuscript and prepared for publication. All authors contributed to manuscript revision, read and approved the submitted version.
Conflict of Interest
AC and AZ were employed by company Granarolo S.p.A., Bologna, Italy.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The current study contributes to the Ph.D. research of KK being carried out in the Food Science Doctoral School, Faculty of Food Sciences, Szent Istvan University, Hungary.
Glossary
Abbreviations
- AFB1
Aflatoxin B1
- 95% CI
95% confidence intervals
- AFM1
Aflatoxin M1
- AQM
Average quality milk (normal and high quality altogether)
- BMDL10
Benchmark dose lower confidence limit for a 10% response
- bw
Body weight
- EC
European Commission
- EDI
Estimated Daily Intake
- EFTA
European Free Trade Association
- EFSA
European Food Safety Authority
- ELISA
Enzyme-linked immunosorbent assay
- EU
European Union
- FAO
Food and Agriculture Organization of the United Nations
- HBV
Hepatitis B virus
- HCC
Hepatocellular carcinoma
- HI
Hazard Index
- HPLC
High Performance Liquid Chromatography
- HQM
High quality milk
- JECFA
Joint FAO/WHO Expert Committee on Food Additives
- LCI
Liver cancer incidence
- LCL
Lower confidence limit
- MoE
Margin of Exposure
- NIST
National Institute of Standards and Technology
- NQM
Normal quality milk
- OM
Organic milk
- SD
Standard deviation
- TD50
Dose causing 50% of the animals developing tumor
- TDI
Tolerable daily intake
- UCL
Upper confidence limit
- WHO
World Health Organization
- WM
Weighted mean
Funding. Project no. 2018-1.2.1-NKP-2018-00002 (to KK, ZF, and ÁA) has been implemented with the support provided from the National Research, Development and Innovation Fund of Hungary, financed under the 2018-1.2.1-NKP funding scheme.
1EFSA, The Comprehensive Food Consumption Database (2018). https://www.efsa.europa.eu/en/food-consumption/comprehensive-database
References
- Anfossi L., Baggiani C., Giovannoli C., D’Arco G., Passini C., Giraudi G. (2011). Occurrence of aflatoxin M1 in Italian cheese: results of a survey conducted in 2010 and correlation with manufacturing, production season, milking animals, and maturation of cheese. Food Control 25, 125–130. 10.1016/j.foodcont.2011.10.027 [DOI] [Google Scholar]
- Bellio A., Bianchi D. M., Gramaglia M., Loria A., Nucera D., Gallina S., et al. (2016). Aflatoxin M1 in cow’s milk: method validation for milk sampled in Northern Italy. Toxins 8, 57. 10.3390/toxins8030057, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogalho F., Duarte S., Cardoso M., Almeida A., Cabeças R., Lino C., et al. (2018). Exposure assessment of Portuguese infants to aflatoxin M1 in breast milk and maternal social-demographical and food consumption determinants. Food Control 90, 140–145. 10.1016/j.foodcont.2018.02.043 [DOI] [Google Scholar]
- Boudra H., Barnouin J., Dragacci S., Morgavi D. P. (2007). Aflatoxin M1 and ochratoxin A in raw bulk milk from French dairy herds. J. Dairy Sci. 90, 3197–3201. 10.3168/jds.2006-565, PMID: [DOI] [PubMed] [Google Scholar]
- Campagnollo F. B., Ganev K. C., Khaneghah A. M., Portela J. B., Cruz A. G., Granato D., et al. (2016). The occurrence and effect of unit operations for dairy products processing on the fate of aflatoxin M1: a review. Food Control 68, 310–329. 10.1016/j.foodcont.2016.04.007 [DOI] [Google Scholar]
- Canever A., Serraino A., Rosmini R. (2004). “Presenza di aflatossine nei mangimi desti- nati all’alimentazione animale” in Proceedings of the 14th National Congress of AIVI, Santuario di Vicoforte (CN), Italy. ed. Associazione Italiana Veterinari Igienisti (AIVI) (Italy: Associazione Italiana Veterinari Igienisti (AIVI), Ozzano dell’Emilia (Bologna)), 451–455. [Google Scholar]
- Cano-Sancho G., Sanchis V., Marín S., Ramos A. J. (2013). Occurrence and exposure assessment of aflatoxins in Catalonia (Spain). Food Chem. Toxicol. 51, 188–193. 10.1016/j.fct.2012.09.032, PMID: [DOI] [PubMed] [Google Scholar]
- Cullen J. M., Reubner B. H., Hsieh L. S., Hyde D. M., Hsieh D. P. (1987). Carcinogenicity of dietary Aflatoxin M1 in male fisher rats compared to aflatoxin B1. Cancer Res. 47, 1913–1917. PMID: [PubMed] [Google Scholar]
- Duarte S. C., Almeida A. M., Teixeria A. S., Pereira A. L., Falcão A. C., Pena A., et al. (2013). Aflatoxin M1 in marketed milk in Portugal: assessment of human and animal exposure. Food Control 30, 411–417. 10.1016/j.foodcont.2012.08.002 [DOI] [Google Scholar]
- EFSA (2004). Opinion of the scientific panel on contaminants in the food chain on a request from the commission related to Aflatoxin B1 as undesirable substance in animal feed. EFSA J. 39, 1–27. 10.2903/j.efsa.2004.39 [DOI] [Google Scholar]
- EFSA Scientific Committee (2007). Opinion of the scientific panel on contaminants in the food chain on a request from the commission related to the potential increase of consumer health risk by a possible increase of the existing maximum levels for aflatoxins in almonds, hazelnuts and pistachios and derived products. EFSA J. 446, 1–127. 10.2903/j.efsa.2007.446 [DOI] [Google Scholar]
- EFSA Scientific Committee (2012). Scientific opinion on the applicability of the margin of exposure approach for the safety assessment of impurities, which are both genotoxic and carcinogenic in substances added to food/feed. EFSA J. 10:2578. 10.2903/j.efsa.2012.2578 [DOI] [Google Scholar]
- European Community (2006). Commission Regulation (EC) No 1881/2006 of 19 December 2006 setting maximum levels for certain contaminants in foodstuffs. Offic. J. Eur. Union L364/5.
- Fakhri Y., Ghorbani R., Taghavi M., Keramati H., Amanidaz N., Moradi B., et al. (2019b). Concentration and prevalence of Aflatoxin M-1 in human breast Milk in Iran: systematic review, meta-analysis, and carcinogenic risk assessment: a review. J. Food. Protect. 82, 785–795. 10.4315/0362-028X.JFP-18-367 [DOI] [PubMed] [Google Scholar]
- Fakhri Y., Rahmani J., Oliveira C. A. F., Franco L. T., Corassin C. H., Saba S., et al. (2019a). Aflatoxin M1 in human breast milk: a global systematic review, metaanalysis, and risk assessment study (Monte Carlo simulation). Trends Food Sci. Tech. 88, 333–342. 10.1016/j.tifs.2019.03.013 [DOI] [Google Scholar]
- FAO/WHO Codex Alimentarius (2014). Code of practice for the prevention and reduction of mycotoxin contamination in cereals (CAC/RCP 51-2003). Adopted 2003. Revised 2014.
- FAO/WHO Codex Alimentarius (1995). General Standard for Contaminants and Toxins in Food and Feed. Adopted in 1995. (CXS 193-1995) Revised in 1997, 2006, 2008, 2009. Amended in 2010, 2012, 2013, 2014, 2015, 2016, 2017, 2018, 2019.
- Flores-Flores M. E., Lizarraga E., Lopez de Cerain A., Gonza lez-Penas E. (2015). Presence of mycotoxins in animal milk: a review. Food Control 53, 163–176. 10.1016/j.foodcont.2015.01.020 [DOI] [Google Scholar]
- Frazzoli C., Gherardi P., Saxena N., Belluzzi G., Mantovani A. (2017). The hotspot for (global) one health in primary food production: Aflatoxin M1 in dairy products. Front. Public Health 4:294. 10.3389/fpubh.2016.00294, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo A., Masoero F. (2010). In vitro models to evaluate the capacity of different sequestering agents to adsorb aflatoxins. Ital. J. Anim. Sci. 9:e21. 10.4081/ijas.2010.e21 [DOI] [Google Scholar]
- Galvano F., Pietri A., Bertuzzi T., Gagliardi L., Ciotti S., Luisi S., et al. (2008). Maternal dietary habits and mycotoxin occurrence in human mature milk. Mol. Nutr. Food Res. 52, 496–501. 10.1002/mnfr.200700266, PMID: [DOI] [PubMed] [Google Scholar]
- Giorni P., Magan N., Pietri A., Bertuzzi T., Battilani P. (2007). Studies on Aspergillus flavi isolated from maize in northern Italy. Int. J. Food Microbiol. 113, 330–338. 10.1016/j.ijfoodmicro.2006.09.007, PMID: [DOI] [PubMed] [Google Scholar]
- Gonzales-Osnaya L., Soriano J. M., Moltò J. C., Manez J. (2008). Simple liquid chromatography assay for analyzing ochratoxin in bovine milk. Food Chem. 108, 272–276. 10.1016/j.foodchem.2007.10.013 [DOI] [Google Scholar]
- Hsieh D. P., Cullen J. M., Ruebner B. H. (1984). Comparative hepatocarcinogenicity of aflatoxins B1 and M1 in the rat. Food Chem. Toxicol. 22, 1027–1028. 10.1016/0278-6915(84)90160-1, PMID: [DOI] [PubMed] [Google Scholar]
- Joint FAO/WHO Expert Committee on Food Additives (2001). Safety evaluation of certain mycotoxins in food. Available at: http://www.inchem.org/documents/jecfa/jecmono/v47je01.htm (Accessed September 10, 2018).
- Kebede H., Abbas H. K., Fisher D. K., Bellaloui N. (2012). Relation between aflatoxin contamination and physiological response of corn plants under drought and heat stress. Toxins 4, 1385–1403. 10.3390/toxins4111385, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerekes K., Bonilauri P., Serraino A., Giacometti F., Piva S., Zambrini V., et al. (2016). An effective self-control strategy for the reduction of aflatoxin M1 content in milk and to decrease the exposure of consumers. Food Addit. Contam. A 33, 1840–1849. 10.1080/19440049.2016.1241895, PMID: [DOI] [PubMed] [Google Scholar]
- Kuiper-Goodman T. (1990). Uncertainties in the risk assessment of three mycotoxins: aflatoxin, ochratoxin, and zearalenone. Can. J. Physiol. Pharmacol. 68, 1017–1024. 10.1139/y90-155, PMID: [DOI] [PubMed] [Google Scholar]
- Kunter I., Hürer N., Gülcan H. O., Öztürk B., Dogan I., Sahin G. (2017). Assessment of Aflatoxin M1 and heavy metal levels in mothers breast milk in Famagusta. Cyprus. Biol. Trace Elem. Res. 175, 42–49. 10.1007/s12011-016-0750-z, PMID: [DOI] [PubMed] [Google Scholar]
- Leblanc J. C., Tard A., Volatier J. L., Verger P. (2005). Estimated dietary exposure to principal food mycotoxins from the first French Total Diet Study. Food Addit. Contam. 22, 652–672. 10.1080/02652030500159938, PMID: [DOI] [PubMed] [Google Scholar]
- Leclercq C., Arcella D., Piccinelli R., Sette S., Le Donne C., Turrini A. (2009). The Italian National Food Consumption Survey INRAN-SCAI 2005–06: main results in terms of food consumption. Public Health Nutr. 12, 2504–2532. 10.1017/S1368980009005035 [DOI] [PubMed] [Google Scholar]
- Madali B., Gulec A., Ayaz A. (2018). A survey of Aflatoxin M1 in different milk types in Turkey: risk assessment of children’s exposure. Prog. Nutr. 20, 659–664. 10.23751/pn.v20i4.6889 [DOI] [Google Scholar]
- Marchetti G., Serraino A., Giacometti F., Bonfante E., Rosmini R. (2013). Rassegna sulle aflatossine negli alimenti e nei mangimi: fonti di contaminazione per l’uomo e controllo. Ind. Aliment 52, 7–19. Avilable at: https://www.chiriottieditori.it/it/industrie-alimentari/883 [Google Scholar]
- Martins H. M., Guerra M. M., Bernardo F. (2005). A six year survey (1999-2004) of the occurrence of aflatoxin M1 in daily products produced in Portugal. Mycotoxin Res. 21, 192–195. 10.1007/BF02959261, PMID: [DOI] [PubMed] [Google Scholar]
- Mauro A., Battilani P., Cotty P. J. (2014). Atoxigenic Aspergillus flavus endemic to Italy for biocontrol of aflatoxins in maize. BioControl 60, 125–134. 10.1007/s10526-014-9624-5 [DOI] [Google Scholar]
- Mauro A., Garcia-Cela E., Pietri A., Cotty P. J., Battilani P. (2018). Biological control products for Aflatoxin prevention in Italy: commercial field evaluation of Atoxigenic Aspergillus flavus active ingredients. Toxins 10:30. 10.3390/toxins10010030, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miliĉeviĉ D., Petronijeviĉ R., Petroviĉ Z., Đjinoviĉ-Stojanoviĉ J., Jovanoviĉ J., Baltiĉ T., et al. (2019). Impact of climate change on aflatoxin M1 contamination of raw milk with special focus on climate conditions in Serbia. J. Sci. Food Agric. 99, 5202–5210. 10.1002/jsfa.9768, PMID: [DOI] [PubMed] [Google Scholar]
- Milićević D. R., Spirić D., Radičević T., Velebit B., Stefanović S., Milojević L., et al. (2017). A review of the current situation of aflatoxin M1 in cow’s milk in Serbia: risk assessment and regulatory aspects. Food Addit. Contam. Part A. 34, 1617–1631. 10.1080/19440049.2017.1363414, PMID: [DOI] [PubMed] [Google Scholar]
- Ministero della Salute. Nota del Ministero della Salute prot. n. 855 del 16/1/2013—Aflatossine (2013). Extraordinary operating procedures for the prevention and management of the risk of aflatoxin contamination in the dairy supply chain and in the production of maize destined for human and animal nutrition, following extreme weather conditions. Available at: http://www.unionalimentari.com/website/law.aspx?id=1287&key=&fl= (Accessed December 2018).
- NIST/SEMATECH (2013). E-Handbook of statistical methods. Available at: http://www.itl.nist.gov/div898/handbook (Accessed August 2018).
- Oluwafemi F., Badmos A. O., Kareem S. O., Ademuyiwa O., Kolapo A. L. (2014). Survey of aflatoxin M1 in cows’ milk from free-grazing cows in Abeokuta, Nigeria. Mycotoxin Res. 30, 207–211. 10.1007/s12550-014-0204-4, PMID: [DOI] [PubMed] [Google Scholar]
- Pardakhti A., Maleki S. (2019). Risk assessment of Aflatoxin M1 contamination of milk in Iran. Int. J. Environ. Res. 13, 265–271. 10.1007/s41742-019-00172-1 [DOI] [Google Scholar]
- Perrone G., Gallo A., Logrieco A. F. (2014). Biodiversity of Aspergillus section Flavi in Europe in relation to the management of aflatoxin risk. Front. Microbiol. 5:377. 10.3389/fmicb.2014.00377, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prandini A., Tansini G., Sigolo S., Filippi L., Laporta M., Piva G. (2009). On the occurrence of aflatoxin M1 in milk and dairy products. Food Chem. Toxicol. 47, 984–991. 10.1016/j.fct.2007.10.005, PMID: [DOI] [PubMed] [Google Scholar]
- Radonić J. R., Kocić Tanackov S. D., Mihajlović I. J., Grujić Z. S., Vojinović Miloradov M. B., Škrinjar M. M., et al. (2017). Occurrence of aflatoxin M1 in human milk samples in Vojvodina, Serbia: estimation of average daily intake by babies. J. Environ. Sci. Heal. Part B 52, 59–63. 10.1080/03601234.2016.1229454 [DOI] [PubMed] [Google Scholar]
- Rahmani J., Alipour S., Miri A., Fakhri Y., Riahi S. M., Keramati H., et al. (2018). The prevalence of aflatoxin M1 in milk of Middle East region: a systematic review, meta-analysis and probabilistic health risk assessment. Food Chem. Toxicol. 118, 653–666. 10.1016/j.fct.2018.06.016, PMID: [DOI] [PubMed] [Google Scholar]
- Rama A., Latifi F., Bajraktari D., Ramadani N. (2015). Assessment of aflatoxin M1 levels in pasteurized and UHT milk consumed in Prishtina, Kosovo. Food Control 57, 351–354. 10.1016/j.foodcont.2015.04.021 [DOI] [Google Scholar]
- Rodríguez-Velasco M. L., Calonge Delso M. M., Ordónez Escudero D. (2003). ELISA and HPLC determination of the occurrence of aflatoxin M(1) in raw cow’s milk. Food Addit. Contam. 20, 276–280. 10.1080/0265203021000045208, PMID: [DOI] [PubMed] [Google Scholar]
- Rosi P., Borsari A., Lasi G., Lodi S., Galanti A., Fava A., et al. (2007). Aflatoxin M1 in milk: reliability of the immunoenzymatic assay. Int. Dairy J. 17, 429–435. 10.1016/j.idairyj.2006.05.003 [DOI] [Google Scholar]
- Roussi V., Govaris A., Varagouli A., Botsoglou N. A. (2002). Occurrence of aflatoxin M(1) in raw and market milk commercialized in Greece. Food Addit. Contam. 19, 863–868. 10.1080/02652030210146864, PMID: [DOI] [PubMed] [Google Scholar]
- Scaglioni P. T., Becker-Algeri T., Drunkler D., Badiale-Furlong E. (2014). Aflatoxin B1 and M1 in milk. Anal. Chim. Acta 829, 68–74. 10.1016/j.aca.2014.04.036, PMID: [DOI] [PubMed] [Google Scholar]
- Serraino A., Trevisani M., Boscolo D., Rosmini R. (2003). AFM1 pollution in Italian raw milk: quantitative risk assessment for consumer. Ind. Aliment-Ital. 42, 1113–1119. 10.4315/0362-028X.JFP-12-163 [DOI] [Google Scholar]
- Shundo L., Navas S. A., Conceiçăo L., Lamardo A., Ruvieri V., Sabino M. (2009). Estimate of aflatoxin M1 exposure in milk and occurrence in Brazil. Food Control 20, 655–657. 10.1016/j.foodcont.2008.09.019 [DOI] [Google Scholar]
- Temamogullari F., Kanici A. (2014). Short communication: Aflatoxin M1 in dairy products sold in Şanlıurfa, Turkey. J. Dairy Sci. 97, 162–165. 10.3168/jds.2012-6184, PMID: [DOI] [PubMed] [Google Scholar]
- Trevisani M., Farkas Z., Serraino A., Zambrini V. A., Pizzomiglio V., Giacometti F., et al. (2014). Analysis of industry generated data part I. a baseline for the development of a tool to assist milk industry in the design of sampling plans for controlling aflatoxin M1 in milk. Food Addit. Contam. A 31, 1246–1256. 10.1080/19440049.2014.925587 [DOI] [PubMed] [Google Scholar]
- Trevisani M., Serraino A., Canever A., Varisco G., Boni P. (2006). “Quantitative risk assessment of aflatoxicosis associated with milk consumption in Italy (2000-2004)” in Towards a risk-based chain control. eds. Smulders F. J. M., Collins J. D. (The Netherlands: Wageningen Academic Publisher; ), 91–114. [Google Scholar]
- Tsakiris I. N., Tzatzarakis M. N., Athanasios K., Alegakis A. K., Vlachou M. I., Renieri E. A., et al. (2013). Risk assessment scenarios of children’s exposure to aflatoxin M1 residues in different milk types from the Greek market. Food Chem. Toxicol. 56, 261–265. 10.1016/j.fct.2013.02.024, PMID: [DOI] [PubMed] [Google Scholar]
- Udovicki B., Djekic I., Eleni P., Kalogianni E. P., Rajkovic A. (2019). Exposure assessment and risk characterization of Aflatoxin M1 intake through consumption of milk and yoghurt by student population in Serbia and Greece. Toxins 11, 205–216. 10.3390/toxins11040205, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valitutti F., De Santis B., Trovato C. M., Montuori M., Gatti S., Oliva S., et al. (2018). Assessment of mycotoxin exposure in breastfeeding mothers with celiac disease. Nutrients. 10:336. 10.3390/nu10030336, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (1997). Evaluation of certain food additives and contaminants, Fourty-ninth report of the Joint FAO/WHO Expert Committee on Food Additives, WHO Technical Report Series, 884, 69–77. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated for this study will not be made publicly available. The dataset is based on confidential private industry data.