Abstract
Background:
Cancer survivors face increased risk of cardiovascular events compared to the general population. Adopting a healthy lifestyle may reduce these risks, and guidelines encourage health promotion counseling for cancer survivors, but the extent of physician adherence is unclear.
Methods:
This mixed method study surveyed 91 physicians: 30 primary care physicians (PCPs), 30 oncologists, and 31 specialists (urologists, dermatologists, and gynecologists). Interviews also were conducted with 12 oncologists.
Results:
Most PCPs (90%) reported recommending health promotion (e.g., weight loss, smoking cessation) to at least some cancer survivors, while few oncologists (26.7%) and specialists (9.7%) said they ever did so (p<.001). While most physicians believed that at least 50% of cancer survivors would be adherent to medication regimens to prevent cancer recurrence, they also believed that if patients were trying to lose weight they would not remain medication adherent. In interviews, oncologists expressed fear that providing health promotion advice would distress or overwhelm patients. Additional health promotion barriers identified by thematic analysis included: identifying cancer as oncologists’ focal concern, time pressure, insufficient behavior change training, and care coordination challenges. Facilitators included perceiving a patient benefit and having health promotion resources integrated into the cancer care system.
Conclusion:
Physicians often do not have the time, expertise, or resources to address health promotion with cancer survivors. Research is needed to evaluate whether health promotion efforts compromise medical regimen adherence, as physicians’ responses suggest.
Keywords: cancer survivors, oncologists, primary health care, health promotion, comorbidity
Precis
Survey responses from primary care physicians (n=30), oncologists (n=30), and other specialists who treat cancer patients (n=31), along with interviews of 12 oncologists, indicate that physicians do not often engage in healthy lifestyle promotion with cancer survivors and fear that providing health promotion advice would distress or overwhelm patients, compromising their medical regimen adherence. Additional health promotion barriers were perceived patient disinterest, cancer as oncologists’ focal concern, time pressure, insufficient behavior change training, and care coordination challenges.
Introduction
Advances in cancer screening and treatments have markedly improved overall cancer survival,1 resulting in 14.5 million cancer survivors in the United States.2 The combination of cardiotoxic cancer treatments and behavioral risk factors (e.g., poor diet and low physical activity) increase cancer survivors’ risk of developing comorbid chronic disease,3 with cardiovascular events constituting the second leading cause of death among cancer survivors diagnosed with early-stage disease.4 Long-term risk of cardiovascular disease is heightened among breast,5,3 colorectal,6 and testicular,7,8 cancer survivors, and many of the same risk behaviors that predispose to cancer also predispose to cardiovascular disease.4,9 Thus, many cancer survivors should be advised to adhere to: 1) medical regimens for treatment of comorbidities, 2) medications to prevent cancer recurrence, and 3) health-promoting behaviors to reduce disease risk.10–13
Current practice guidelines advise physicians, including oncologists, to counsel cancer survivors to adopt healthy lifestyles.13,14 Such physician recommendations are associated with improved health promotion behaviors.15,16 Health promotion advice provided by oncologists may be particularly impactful for cancer survivors because many continue to see their oncologists and report high levels of trust in them.17 Yet, even though 80% of cancer survivors express interest in receiving health promotion advice,18 fewer than half of survivors report having these discussions.19
Physicians and other healthcare providers note several barriers to health promotion, including lack of training,20 time constraints,20,21 and perceiving health promotion counseling as beyond the physician’s role.22 Whether these barriers apply equally to oncologists and other physicians is unknown. In the present study, we focused on primary care provider (PCPs), oncologists, and other specialists who commonly provide care for cancer survivors (i.e., gynecologists for breast cancer, urologists for prostate cancer, and dermatologists for melanoma). All providers have the opportunity and are advised by national guidelines to perform health promotion counseling with cancer survivors,10 but how they perceive this responsibility is poorly understood. Because most cancer survivors see multiple providers, understanding how the various types of providers approach health promotion counseling will guide the development of effective interventions and policy changes. Also unknown is whether physicians perceive a relationship between cancer survivors’ adherence to a medical treatment regimen and adherence to changes to health behaviors. In particular, limited qualitative research exists on oncologists’ perspectives and practices regarding providing health promotion counseling to their patients (qualitative studies in the oncology setting have predominantly examined nurses).20,23
This mixed methods study compared the health promotion practices and beliefs of oncologists, PCPs, and physician specialists. Survey questions were designed to: 1) probe the hypothesis that oncologists and other specialist physicians are less likely than PCPs to provide or refer cancer survivors to health promotion services; 2) examine physician beliefs about their own ability to provide health promotion counseling and about indirect effects on medication adherence when patients are trying to lose weight; and 3) explore barriers to health promotion discussions. Qualitative interviews were conducted with 12 oncologists to identify the unique challenges these physicians face regarding promoting health behavior change among cancer survivors. In this study, we define a cancer survivor as a patient who has completed active treatment and no longer has detectable cancer, and the surveys specified that the health promotion practices of interest included smoking cessation, weight loss, and physical activity.
Method
Recruitment
All participants were attending physicians in the Northwestern Medicine (NM) network. Outreach was made to 40 PCPs who had previously participated in research regarding early detection of cancer. All 47 NM oncologists on the central campus were invited to participate. A subset of 78 other specialists (dermatologists, urologists, and gynecologists) was invited to participate and enrolled sequentially until 10–11 were recruited from each specialist subcategory (Table 1).
Table 1.
Descriptive statistics for physicians completing survey (n=91).
| PCP | Oncologist | Specialist | |
|---|---|---|---|
| n=30 | n=30 | n=31 | |
| no.(%) | no.(%) | no.(%) | |
| Female | 12(40.0%) | 11(36.7%) | 11(36.7%) |
| Age | |||
| Under 30 | 8(26.7%) | 2(6.7%) | 4(12.9%) |
| 31–44 | 5(16.7%) | 9(30.0%) | 9(29.0%) |
| 45–55 | 8(26.7%) | 8(26.7%) | 10(32.3%) |
| 56–65 | 7(23.3%) | 9(30.0%) | 7(22.6%) |
| 66 or older | 2(6.7%) | 2(6.7%) | 1(3.2%) |
| Race | |||
| White | 27(90.0%) | 29(96.7%) | 24(77.4%) |
| Black/African American | 2(6.5%) | ||
| Asian | 2(6.7.%) | 1(3.3%) | 5(16.1%) |
| Multiracial | 1(3.3%) | ||
| Hispanic | 4(13.3%) | 1(3.3%) | 1(3.2%) |
| Years in Practice | |||
| Less than 5 | 9(30.0%) | 3(10.0%) | 8(25.8%) |
| 5–10 | 4(13.3%) | 6(20.0%) | 6(19.4%) |
| 11–15 | 1(3.3%) | 4(13.3%) | 2(6.5%) |
| 16–20 | 6(20.0%) | 6(20.0%) | 6(19.4%) |
| 21–25 | 2(6.7%) | 2(6.7%) | 3(9.7%) |
| 26–30 | 6(20.0%) | 6(20.0%) | 4(12.9%) |
| 31 or more | 2(6.7%) | 3(10.0%) | 2(6.5%) |
| Type of Practice | |||
| Family Medicine | 11(36.7%) | ||
| Internal Medicine | 19(63.3%) | ||
| Medical Oncology | 20(66.7%) | ||
| Surgical Oncology | 10(33.3%) | ||
| Dermatology | 11(35.5%) | ||
| Urology | 10(32.3%) | ||
| Gynecology and/or Obstetrics | 10(32.3%) |
Abbreviation: PCP=Primary Care Physician
Procedures
The Institutional Review Board at Northwestern University determined that the study was “Not Human Subjects Research.” Physicians were emailed a link to a Research Electronic Data Capture (REDCap) survey,24 which included demographic items and 10 questions written by the study authors (see Supplementary File 1). Survey questions were reviewed for clarity by 6 physicians prior to their administration. Items referenced “cancer patients in remission” to avoid ambiguity resulting from differing interpretations of the term “cancer survivor,” which some use to reference any patient following a cancer diagnosis whereas others reference only those who are at least 5 years post-treatment.25
Oncologists who were sent the survey were invited to participate in an in-person structured interview about the study results. The interviewer (BS) used a moderator guide (see Supplementary File 2) to perform one-on-one interviews, while remaining blind to participants’ individual survey responses. Interviews were audio recorded and transcribed. After the eighth interview, two authors with previous qualitative coding experience (TS and BY) created a coding scheme using thematic analysis, adopting a deductive framework.26 After each subsequent interview, they reviewed the coding scheme to accommodate new themes. By interview 11, no new themes emerged; one additional interview was conducted to confirm saturation. TS then coded all interviews and AE served as a consensus coder, with discrepancies resolved by discussion.
Power and Statistical Analysis
Because the primary comparison was between PCPs and the other physicians on a binary outcome (i.e., selecting a health-promoting option versus not), sample size calculations used the statistical test of the difference between two independent proportions. Given evidence that 75% of PCPs practice some level of health promotion counseling,27,28 a difference indicating that fewer than half (45%) of oncologists and specialists do so was considered to have important health care policy and training implications. With α=.05 and allocation ratio=2, to yield a power of .80 to detect this difference, a minimum sample size of 24 was needed for each group; hence, we recruited a sample of 30 for each group.
Four survey items presented scenarios in which physicians were asked to select whether their likely response would be a health promotion option (e.g., agree on a healthy weight loss goal) versus another option (e.g., tell the patient that the physician does not discuss issues outside of his/her area). Responses were dummy-coded (1=health-promoting option) for analysis using logistic regression. The remaining items used ordinal scales; responses were converted into a continuous metric (e.g., “1–25%”=12.5) for analysis using linear regression. In these models, Helmert contrast codes compared 1) PCPs to other physicians, and 2) oncologists to specialists. A paired samples t-test compared physicians’ estimates of the percent of patients who generally adhere to cancer preventive medical treatments to the percent who adhere if also trying to lose weight.
Results
Participants
Thirty PCPs, 30 oncologists, and 31 specialists participated, ranging in age from under 30 to 70. This enrollment represented 75% of PCP’s, 63.8% of oncologists, and 26.9% of specialists contacted. Respondents were predominately white and non-Hispanic and 62.6% were male (Table 1). Of the 12 oncologists interviewed, 5 were male. Cancer specialties included breast (n=3), gastrointestinal (n=2) genitourinary (n=2), head and neck (n=1), lymphoma (n=1) melanoma or skin (n=2), and thoracic (n=1).
Survey Responses
Health Promotion Practices.
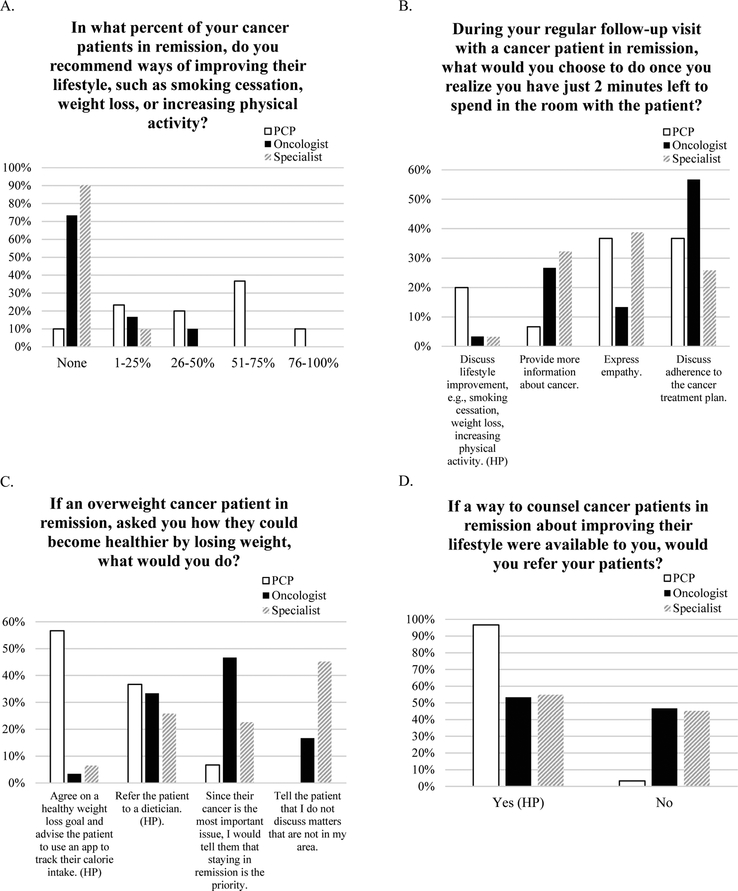
Whereas most PCPs (90%) recommended ways of improving health behaviors to at least some cancer survivors, 26.7% of oncologists and 8.7% of specialists made these recommendations (Figure 1). PCPs recommended health behavior improvements to a significantly higher percentage of cancer survivors than did oncologists and specialists (p<.001). (Table 2) When presented with a scenario in which a physician had two minutes remaining in the visit with a cancer survivor, 8.8% of physicians said they would use that time to discuss topics related to health promotion, with PCPs being significantly more likely to do so than oncologists and specialists (p=.02; Table 3). If an overweight patient asked about weight loss, 93.3% of PCPs indicated they would encourage health behavior change either through a self-help weight loss app or referral to a dietician, but oncologists and specialists were significantly less likely to do so (p<.001), with less than half choosing the health-promoting options. Finally, when asked if they would refer cancer survivors to a service that provided health promotion counseling, 96.7% of PCPs indicated they would make the referral, but oncologists and specialists were significantly less likely to do so (p<.01), with only about half indicating they would.
Figure 1.
Healthy lifestyle promotion practices for cancer survivors (percentage of physicians in each group endorsing each response)
Abbreviation: HP, Health-Promoting Option; PCP, Primary Care Physician
Table 2.
Differences between physician groups in lifestyle change beliefs and practices for cancer survivors (linear regression analysis).
| % of Patients for Whom You Recommend Healthy Lifestyle Improvements | Estimate of % Patients Adherent to Cancer Tx | Estimate of % of Patients Adherent to Cancer Tx if Trying to Lose Weight | Minutes Discussing Medical Tx for Comorbid Conditions | Minutes Discussing Lifestyle Change for Patients with Comorbid Conditions | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | 95% CI | p | β | 95% CI | p | β | 95% CI | p | β | 95% CI | p | β | 95% CI | p | |
| PCP vs Othersa | 38.56 | 30.84–46.29 | .00 | −5.46 | −15.92–5.01 | .30 | 1.43 | −6.68– 9.54 | .73 | 3.60 | 3.12–4.08 | .00 | .33 | −.01–.66 | .06 |
| Onc vs Spec | 4.62 | −4.25–13.50 | .30 | 2.58 | −14.60–9.44 | .67 | −1.30 | −10.62–8.01 | .78 | .43 | −.12–.98 | .12 | .18 | −.20–.57 | .35 |
Abbreviation: PCP, Primary Care Physician; Onc, Oncologist; Spec, Specialist; Tx=Treatment; β, regression coefficient; CI=Confidence Interval
Oncologists and Specialists
Table 3.
Differences between physician groups in the likelihood of selecting health-promoting option for cancer survivors across three scenarios (logistic regression analysis).
| You realize you have just 2 minutes left to spend in the room with the patient | An overweight cancer patient in remission, asked you how they could become healthier by losing weight | A way to counsel cancer patients in remission about improving their lifestyle is available for referral | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |
| PCP vs Othersa | 7.37 | 1.39–39.14 | .02 | 26.66 | 5.78–123.00 | .00 | 24.62 | 3.15–192.40 | .002 |
| Onc vs Spec | 1.03 | .06–17.33 | .98 | 1.22 | .42–3.50 | .72 | .94 | .34–2.58 | .94 |
Abbreviation: PCP, Primary Care Physician; Onc, Oncologist; Spec, Specialist; Tx=Treatment; β, regression coefficient, CI=Confidence Interval
Oncologists and Specialist
Beliefs about Treatment Adherence and Practices for Those with Comorbidities.
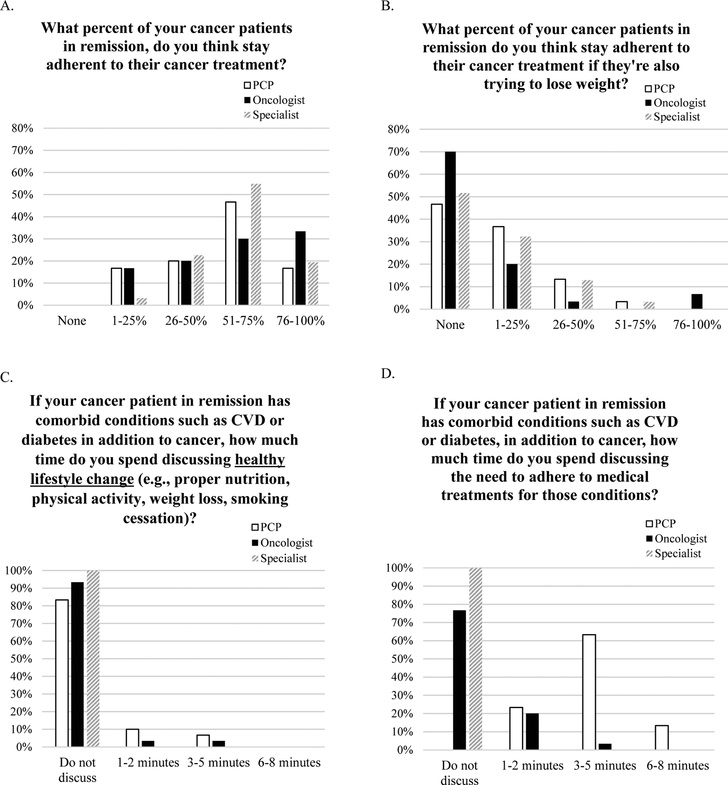
Whereas most physicians believed that at least 50% of cancer survivors would be adherent to medical treatments to prevent cancer recurrence (Figure 2), most also believed that no cancer survivors would remain adherent to cancer preventive medications if they were also trying to lose weight. Indeed, the percentage of physicians who predicted that patients would remain medication adherent decreased from 57.0% (SD=23.5%) to 10.7% (SD=18.12%) if the patient was trying to lose weight, t(90)=17.79, p=.003. Belief that undertaking weight loss undermines adherence to a medical cancer prevention regimen did not differ among physician groups. (Table 2)
Figure 2.
Beliefs about treatment adherence and practices for those with comorbidities (percentage of physicians in each group endorsing each response option)
Abbreviation: PCP, Primary Care Physician
If a cancer survivor also had cardiometabolic comorbidities, 92.3% of physicians said they would not discuss health promotion; average minutes (.09) devoted to discussing health behavior change during the clinical visit did not differ between physician groups. In contrast, all PCPs indicated they would spend at least some time discussing adherence to medical treatments for comorbid conditions, estimating that they would spend an average of 3.82 minutes on this topic. Specialists and oncologists indicated they would spend less time (M=.21 minutes) than PCPs discussing adherence to medical treatments for comorbid conditions (p<.01), with the vast majority indicating they would not discuss this topic at all.
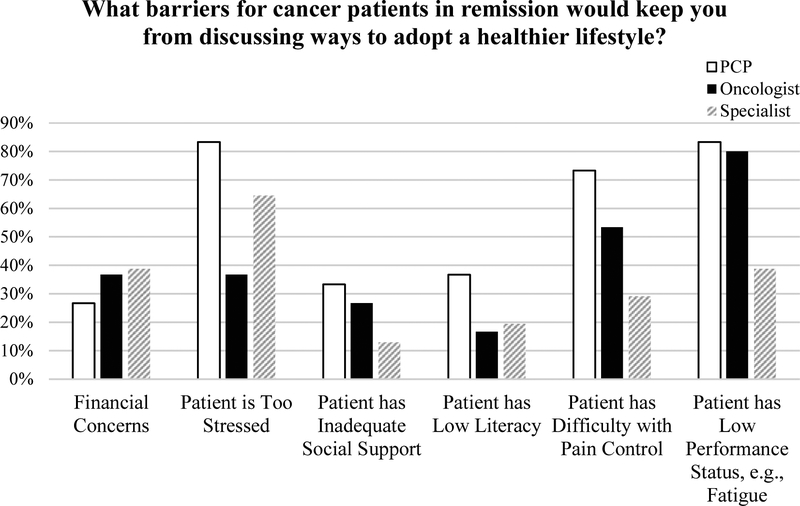
Barriers and Confidence in Addressing Health Promotion.
Physicians rated their confidence as low: M=1.34 (SD=1.46), with oncologists and specialists reporting lower confidence than PCPs (p<.001). The most common barriers for PCPs were the patient having distress, pain, and low performance status. For oncologists, low performance status was the most-endorsed barrier; and for specialists, patient distress the most-endorsed barrier (Figure 3).
Figure 3.
Barriers to healthy lifestyle discussions with cancer survivors (percentage of physicians in each group endorsing each response option)
Qualitative Interview Responses
Patient Factors.
The most commonly-mentioned patient factor that influenced health promotion conversations was the patient’s expressed interest in making changes. (Table 4) Oncologists said that health promotion conversations were “often more so triggered by the patient than us” and that they refrained from providing health promotion advice when patients presented with psychosocial challenges, such as financial stress.
Table 4.
Themes and subcodes about barriers and facilitators to health promotion counseling emerging from interviews with 12 oncologists.
| Example | n | |
|---|---|---|
| Patient Factors | ||
| Non-cancer issues makes lifestyle change lower priority (B) | “[I]f they have lots of comorbidities, because there are obese women who have very severe arthritis or very severe heart disease or whatever. If they’re sick from other reasons and they’re really obese it seems besides [sic] the point.” (ID 8) |
2 |
| Interested in lifestyle changes (F) | “for someone who’s had surgery and is being followed actively… they always ask, “What else can I do?” They ask about diet, they ask about vitamins” (ID 4) | 7 |
| Oncologist Factors | ||
| Primary concern is cancer care (B) | “[T]his may be tunnel vision… we’re so focused on the cancer that it’s like almost as if you made it this far, it should be a switch to now let’s maintain your longevity by augmenting the rest of your life, but it almost feels like ‘phew.’ ” (ID 5) | 12 |
| Lack of training on lifestyle change, evidence of its benefits (B) | “[Oncologists are] not necessarily maintaining their internal medicine boards and don’t feel necessarily comfortable that they’re keeping up with that literature and keeping up with what might be the state of the art.” (ID 1) |
8 |
| Fear of causing distress or overwhelming patient (B) |
“they’re stressed out about their scan results, bad lab results, we talked about a million and a half things, am I going to add weight loss to their issue? No.” (ID 10) |
4 |
| Perceives patient benefit to addressing healthy lifestyle (F) | “I see this as giving the patient some power of taking control over a situation that is out of their control.” (ID 6) | 9 |
| System-Related Factors | ||
| Billing/Time (B) | “[T]here is stress to produce, stress to generate revenue, see as many patients, increase access, increase billing, you can’t have half hour conversations with people about weight loss.” (ID 1) | 11 |
| Issue related to primary care (B) | “[I]t’s almost like primary care people in general [are] deferring to the oncologists… and I think part of it is, the bulk of it is, discomfort.” (ID 6) | 7 |
| Effective Integration between cancer care and lifestyle change resources (F) | “I think that if you are trying to care in a holistic way for say a breast cancer patient, it would be nice to have all the services very seamlessly integrated.” (ID 4) | 11 |
Abbreviation: B, Barrier, F, Facilitator
Oncologist Factors.
Oncologists noted both physical and psychological benefits that cancer survivors might derive from adopting health behavior changes: improved health and “taking control over a situation that is out of their control.” Yet, all oncologists noted that cancer control is their primary concern, which reduced the priority of providing health promotion advice. As one oncologist stated, “We’re so focused on the life or death aspect of cancer, everything falls through the cracks.” Another oncologist suggested, “[W]hen you’re a hammer, the whole world’s a nail. From an oncologist’s standpoint, if the patient becomes obese and their cancer is cured, they’ve successfully treated the patient.” Oncologists perceived weight gain ambivalently: “Our goal is often don’t lose weight, because losing weight is the first bad sign that we’re heading towards progression of disease. We definitely jump on weight loss and we aren’t so jumpy on weight gain. I often use the phrase, ‘In my world I’m not too unhappy about gaining weight.’ ”
Some oncologists noted that training in health promotion had not been included in their medical curriculum, decreasing their comfort with counseling patients: “The appreciation for lifestyle change is relatively recent…There is much greater awareness, even in the last 5 years, but it is relatively recent.” Some expressed a degree of skepticism about the evidence base and practicality of health promotion interventions: “You know, I don’t even know what the impact is…I’m skeptical sometimes about some of the data.” This oncologist elaborated that “[f]or many of us, the interpretation of lifestyle data is more nebulous and oftentimes very difficult or perceived as very difficult to adhere to the recommendation…”
Several oncologists expressed fear that providing health promotion advice would distress or overwhelm patients. Their expressed fear was consistent with survey responses suggesting physicians feared a zero-sum game in which cancer survivors would not remain adherent to medical treatment if also trying to lose weight. As one oncologist put it, “Most people are saying that patients cannot do both… like chewing gum and walking.”
Systems Factors.
Oncologists emphasized that they lack time and resources to perform health promotion during regular visits, necessitating that health promotion advice be provided to cancer survivors elsewhere in the healthcare system. Even though oncologists viewed health promotion counseling as falling more within the PCP’s purview than their own, they acknowledged that cancer survivors were probably not having these conversations with PCPs. Oncologists stated that “a general practitioner is intimidated by a cancer patient and therefore doesn’t want to do anything wrong.” Accordingly, PCPs were perceived as feeling uncomfortable treating and recommending health behavior changes to cancer survivors. Several suggested that “a well-established survivorship clinic is the best way to [provide health promotion advice] … because then all [oncologists] would have to do is say, ‘I’d like to refer you to the survivorship clinic.’ ”
Another suggested health system improvement by placing an automatic alert in the electronic medical record to trigger referral of cancer survivors who could benefit from health promotion services. However, oncologists worried that those providing health promotion would lack adequate understanding of what cancer patients face – “[O]ne of the biggest fears… is what are they going to say to the patient? Are they going to have the knowledge to be able to separate the nuances between melanoma and breast and lung? … . . Are they going to give conflicting information to the patient?” Hence, providing health promotion counseling via a survivorship clinic led by staff well-versed in cancer was preferable to having PCPs counsel cancer survivors.
Discussion
This mixed method study centeracterized the practices and beliefs of PCPs, oncologists, and other physician specialists regarding providing health promotion counseling to cancer survivors. We identified several differences between PCPs and other providers, including that oncologists and other specialists were less likely than PCPs to recommend health promotion to cancer survivors and to make referrals for health promotion counseling. All physicians were unlikely to advise health behavior change when cancer survivors exhibited comorbid cardiometabolic disease, even though these patients may have the greatest need to improve health behaviors.
Whereas most physicians were optimistic that at least 50% of cancer survivors stay adherent to medical treatments, they appeared to perceive competition between patients’ adherence to the pharmacologic components of cancer prevention and efforts to improve health behaviors. Most physicians believed that cancer survivors would not remain adherent to an anti-cancer medical regimen if they were also trying to lose weight. Several factors may contribute to physicians’ doubt that patients can accomplish healthy lifestyle change and medical adherence simultaneously. First, physicians may delimit patients’ health goals out of a genuine fear of overwhelming them (which may also explain failure to provide health promotion counseling when survivors have comorbidities). Second, to the extent that oncologists remain skeptical about the benefits of health behavior change, health promotion efforts can be construed as an unproductive distraction. Third, oncologists may be uniquely ambivalent about patients’ obesity treatment efforts because they are accustomed to seeing weight loss signify cancer progression.
Our results are consistent with prior findings of physicians’ low rates of health promotion counseling. We build upon prior research by investigating the reasons underlying physicians’ decisions regarding provision of health promotion counseling. Qualitative results indicate that oncologists may not be aware of or concur with findings that engaging in healthy behaviors can improve quality of life, minimize cancer reoccurrence, and reduce the risk of cardiovascular disease.4,29 This finding suggests a need for improved training on tertiary and quaternary prevention (i.e., actions aimed at alleviating adverse consequences of illness and medical treatment).30 Confidence with providing health promotion advice was low among all physician groups and particularly so among oncologists and other specialists. Despite oncologists’ lack of confidence in their own ability to address health promotion and despite guidelines advising collaboration with PCPs,10 the present findings indicate that oncologists doubt that PCPs understand the nuances of cancer sufficiently to council survivors appropriately. On the other hand, oncologists have expressed a willingness to refer to a survivorship clinic with staff trained to provide health promotion services tailored to the needs of the cancer survivor.
One strength of this mixed methods study was its direct comparison between the health promotion practices and beliefs of three different types of physicians who treat cancer survivors. Another strength was its examination, for the first time, of physicians’ beliefs about whether survivors’ adherence to medication and to healthvbehavior change are related. The addition of qualitative data from oncologists deepened and contextualized understanding of the survey findings.
This research is not without limitations. Only one urban/suburban health care system was studied. Generalizability to other health care systems, including rural and federally-qualified centers, remains unknown and is an important future direction. Physicians who chose to participate in this study may have differed systematically from those who declined the invitation. PCPs, who were selected from a pool of physicians who participated in prior research may have been atypically interested in health promotion. The limited number of physician subspecialties were chosen because they treat cancer types with a high survival rate. Further, recruitment rates were lower among specialists than other physician groups, which may reflect less interest in health promotion among specialists. Finally, both survey and qualitative data relied upon self-report, which may bias responses in a socially desirable direction.
Conclusions
The gap in providing health promotion counseling to cancer survivors will impair the long-term health of many cancer survivors. As the health care system currently configures survivorship care, it is unlikely that well-meaning physicians have the time, ability, or resources to provide the needed behavioral counseling. Evidence is needed to evaluate oncologists’ worry that health promotion efforts are either not feasible or undermine medical regimen adherence and to determine the optimal methods and timeframe for providing health promotion advice to cancer survivors. Systems-level solutions, such as providing health promotion through survivorship clinics, could help to ameliorate the barriers identified in this study and close the gap in delivery of needed behavior change services to cancer survivors.
Supplementary Material
Acknowledgments
We acknowledge administrative support from Alejandra Povedano, Elyse Daly, and Frankie Granata IV. TKS acknowledges salary support by NIH/NCI training grant T32 CA193193. The authors express thanks to Drs. Angela Pfammatter, Kara Gavin, Annie Lin, Laura Finch, Sharon Baik, and Karly Murphy for their feedback, and to Drs. Juned Siddique and Don Hedeker for advice on statistical analyses. We additionally acknowledge use of REDCap, supported at FSM by the Northwestern University Clinical and Translational Science (NUCATS) Institute. Research reported in this publication was supported, in part, by the National Institutes of Health’s National Center for Advancing Translational Sciences, Grant Number UL1TR001422. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The authors report no conflicts of interest.
References
- 1.de Moor JS, Mariotto AB, Parry C, et al. Cancer survivors in the United States: prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev. 2013;22(4):561–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DeSantis CE, Lin CC, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin. 2014;64(4):252–271. [DOI] [PubMed] [Google Scholar]
- 3.Mehta LS, Watson KE, Barac A, et al. Cardiovascular Disease and Breast Cancer: Where These Entities Intersect: A Scientific Statement From the American Heart Association. Circulation. 2018;137(8):e30–e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koene RJ, Prizment AE, Blaes A, Konety SH. Shared Risk Factors in Cardiovascular Disease and Cancer. Circulation. 2016;133(11):1104–1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hooning MJ, Botma A, Aleman BM, et al. Long-term risk of cardiovascular disease in 10-year survivors of breast cancer. J Natl Cancer Inst. 2007;99(5):365–375. [DOI] [PubMed] [Google Scholar]
- 6.Baraghoshi D, Hawkins ML, Abdelaziz S, et al. Long-term risk of cardiovascular disease among colorectal cancer survivors in a population-based cohort study. J Clin Oncol. 2018;36(7_suppl):113–113. [Google Scholar]
- 7.van den Belt-Dusebout AW, Nuver J, de Wit R, et al. Long-term risk of cardiovascular disease in 5-year survivors of testicular cancer. J Clin Oncol. 2006;24(3):467–475. [DOI] [PubMed] [Google Scholar]
- 8.Weaver KE, Foraker RE, Alfano CM, et al. Cardiovascular risk factors among long-term survivors of breast, prostate, colorectal, and gynecologic cancers: a gap in survivorship care? J Cancer Surviv. 2013;7(2):253–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spring B, King AC, Pagoto SL, Van Horn L, Fisher JD. Fostering multiple healthy lifestyle behaviors for primary prevention of cancer. Am Psychol. 2015;70(2):75–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bluethmann SM, Mariotto AB, Rowland JH. Anticipating the “Silver Tsunami”: Prevalence Trajectories and Comorbidity Burden among Older Cancer Survivors in the United States. Cancer Epidemiol Biomarkers Prev. 2016;25(7):1029–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharifi N, Gulley JL, Dahut WLJJ. Androgen deprivation therapy for prostate cancer. JAMA. 2005;294(2):238–244. [DOI] [PubMed] [Google Scholar]
- 12.Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: An overview of the randomised trials. Lancet. 2005;365(9472):1687–717. [DOI] [PubMed] [Google Scholar]
- 13.National Comprehensive Cancer Network. Survivorship (Version 2.2018). 2018 Accessed October 25, 2018, 2018. [Google Scholar]
- 14.American Society of Clinical Oncology. Survivorship Care Planning Tools. 2019; https://www.asco.org/practice-guidelines/cancer-care-initiatives/prevention-survivorship/survivorship-compendium.
- 15.Jones LW, Sinclair RC, Rhodes RE, Courneya KS. Promoting exercise behaviour: an integration of persuasion theories and the theory of planned behaviour. Br J Health Psychol. 2004;9(Pt 4):505–521. [DOI] [PubMed] [Google Scholar]
- 16.Park JH, Lee J, Oh M, et al. The effect of oncologists’ exercise recommendations on the level of exercise and quality of life in survivors of breast and colorectal cancer: A randomized controlled trial. Cancer. 2015;121(16):2740–2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hillen MA, Onderwater AT, van Zwieten MC, de Haes HC, Smets EM. Disentangling cancer patients’ trust in their oncologist: a qualitative study. Psycho-Oncol. 2012;21(4):392–399. [DOI] [PubMed] [Google Scholar]
- 18.Demark-Wahnefried W, Peterson B, McBride C, Lipkus I, Clipp E. Current health behaviors and readiness to pursue life-style changes among men and women diagnosed with early stage prostate and breast carcinomas. Cancer. 2000;88(3):674–684. [PubMed] [Google Scholar]
- 19.Kenzik K, Pisu M, Fouad MN, Martin MY. Are long-term cancer survivors and physicians discussing health promotion and healthy behaviors? J Cancer Surviv. 2016;10(2):271–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anderson AS, Caswell S, Wells M, Steele RJ. Obesity and lifestyle advice in colorectal cancer survivors - how well are clinicians prepared? Colorectal Dis. 2013;15(8):949–957. [DOI] [PubMed] [Google Scholar]
- 21.Karvinen KH, DuBose KD, Carney B, Allison RR. Promotion of physical activity among oncologists in the United States. J Support Oncol. 2010;8(1):35–41. [PubMed] [Google Scholar]
- 22.Spellman C, Craike M, Livingston P. Knowledge, attitudes and practices of clinicians in promoting physical activity to prostate cancer survivors. Health Educ J. 2014;73(5):566–575. [Google Scholar]
- 23.O’Hanlon É, Kennedy N. Exercise in cancer care in I reland: a survey of oncology nurses and physiotherapists. Eur J Cancer Care. 2014;23(5):630–639. [DOI] [PubMed] [Google Scholar]
- 24.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bell K, Ristovski-Slijepcevic S. Cancer survivorship: Why labels matter. J Clin Oncol. 2013;31(4):409–411. [DOI] [PubMed] [Google Scholar]
- 26.Braun V, Clarke V. Using thematic analysis in psychology. Qualitative research in psychology. 2006;3(2):77–101. [Google Scholar]
- 27.Kruger J, O’Halloran A, Rosenthal AC, Babb SD, Fiore MC. Receipt of evidence-based brief cessation interventions by health professionals and use of cessation assisted treatments among current adult cigarette-only smokers: National Adult Tobacco Survey, 2009–2010. BMC public health. 2016;16:141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pollak KI, Tulsky JA, Bravender T, et al. Teaching primary care physicians the 5 A’s for discussing weight with overweight and obese adolescents. Patient Educ Couns. 2016;99(10):1620–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baker AM, Smith KC, Coa KI, et al. Clinical care providers’ perspectives on body size and weight management among long-term cancer survivors. Integr Cancer Ther. 2015;14(3):240–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Norman AH, Tesser CD. Quaternary prevention: A balanced approach to demedicalisation. Br J Gen Pract. 2019;69(678):28–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.