Abstract
Alcohol use is highly comorbid with depression, especially among college students whose rates of both phenomena are higher than in the general population. The self-medication hypothesis (i.e., alcohol use is negatively reinforced via the alleviation of negative affect) has dominated explanatory models of comorbidity. However, self-regulation has also demonstrated cross-sectional relationships with both depression and alcohol problems and may contribute to the development of alternative comorbidity models. Self-regulation introduces three alternative models that can be tested empirically: 1) a depressed regulation model; 2) a central nervous system depressant model; and 3) a self-regulatory failure model. The purpose of this study was to test the utility of these models (in addition to the self-medication hypothesis) by examining the temporal precedence in the relations between self-regulation, depressive symptoms, and alcohol problems among heavy drinking college students (N = 393) over five assessment points (baseline, 1-month, 6-month, 12-month, and 16-month) using an autoregressive cross-lagged model. Lower self-regulation, and higher alcohol problems and depressive symptoms, prospectively predicted higher depressive symptoms. Higher alcohol problems and lower self-regulation prospectively predicted higher alcohol problems. Only self-regulation prospectively predicted self-regulation. These results were consistent across multiple time points. Findings are consistent with a self-regulatory failure model of depressive symptoms and alcohol problems. Therefore, self-regulation may be an important etiological variable and potential intervention target to reduce both alcohol problems and depressive symptoms among college students.
Keywords: Emerging adults, alcohol misuse, self-regulation, depression, comorbidity
College students drink at a higher rate than any other demographic group, resulting in a range of problems including hangovers, academic impairment, sexual assault, alcohol-induced blackouts, and death (Hingson, Zha, & Smyth, 2017; White & Hingson, 2013). In 2017, approximately 39% of college students reported a heavy drinking episode (4/5 drinks in one occasion for females/males) within the past month (Hingson et al., 2017). Although alcohol consumption has decreased somewhat among college students in recent years, some alcohol problems may be on the rise, including alcohol-related deaths (Hingson et al., 2017) and alcohol-related cirrhosis (Tapper & Parikh, 2018). Further, alcohol consumption during college is associated with an increased risk for alcohol use disorder post-graduation (Prince, Read, & Colder, 2019). Thus, heavy drinking among this age group is a significant public health problem (Sacks, Gonzales, Bouchery, Tomedi, & Brewer, 2015).
Depression is also more likely among college students than older age groups (American College Health Association, 2015), partially due to a simultaneous increase in stress and decrease in social support associated with the transition to college (Kerr et al., 2004). Greater depressive symptoms are often related to increased alcohol-related problems (Dennhardt & Murphy, 2011; Soltis, McDevitt-Murphy, & Murphy, 2017), but not to greater overall consumption of alcohol (Cranford, Eisenberg, & Serras, 2009; Pauley & Hesse, 2009; Roberts, Glod, Kim, & Hounchell, 2010). This is evident in students with subclinical levels of depressive symptoms, a group that may never seek treatment, yet still experiences significant increases in problems related to use (Acuff, Soltis, et al., 2018; Pedrelli et al., 2016).
Studies examining the relation between depressive symptoms and alcohol problems often use the self-medication hypothesis as the explanatory framework. The self-medication model suggests that alcohol use alleviates negative affect (i.e., negative reinforcement) and therefore increases over time, resulting in a more problematic pattern of use (Khantzian, 1997). Although the self-medication model has received support and has guided research efforts and treatment development for those with comorbid substance misuse and depression (Bolton, Robinson, & Sareen, 2009; Kenney, Merrill, & Barnett, 2017), some phenomena have not been adequately explained by self-medication models. For example, studies consistently report that depressive symptoms are associated with alcohol problems, but not consumption, suggesting that aspects of depression may contribute unique risk towards alcohol problems. Another study found that coping motives explained the relationship between depressive symptoms and alcohol problems among college students, but not among their non-college peers (Kenney, Anderson, & Stein, 2018). Thus, although the self-medication hypothesis does show promise as a model of the association between depressive symptoms and alcohol problems, recent calls for extensions or alternatives to the self-medication model (Lembke, 2012; Levy, 2018; Vujanovic, Wardle, Smith, & Berenz, 2016) highlight the need to explore other mechanisms through which these phenomena are linked over time.
Self-Regulation
Self-regulation may be a risk-factor for both depressive symptoms and alcohol problems. In its simplest form, self-regulation has been defined as the ability to plan, self-monitor, self- evaluate, and implement specific behavior changes in the service of long-term goals or plans (Brown, 1998; Carver & Scheier, 2011). Self-regulation is related to academic/occupational success (Creed, Fallon, & Hood, 2009; Morosanova, Fomina, Kovas, & Bogdanova, 2016; Richardson, Abraham, & Bond, 2012) and is protective against alcohol use (Kuvaas, Dvorak, Pearson, Lamis, & Sargent, 2014), partially because it underlies the ability to navigate new stressors, effectively tolerate stress and delay gratification (Dvorak, Simons, & Wray, 2015), and inhibit maladaptive behaviors in the service of long-term goals.
Strauman (2002) proposed a model of depression focused on deficits in self-regulation in which one or both of two systems, labeled promotion/approach and prevention/avoid, are compromised in such a way that the individual experiences a loss of motivation and is no longer capable of effectively responding to potentially rewarding stimuli. The promotion (approach) system is responsible for motivated behavior towards obtaining positive outcomes, whereas the prevention (avoid) system is responsible for motivated behavior towards minimizing negative outcomes. Strauman (2002) suggested that depression is related to impairment in one or both systems that may manifest in the form of dysfunctional or inaccurate self-monitoring, selfevaluation, and/or behavior implementation to achieve a desired end state. For example, one study found that psychiatric patients with depression used significantly less positive cognitive emotional regulation strategies than a general adult population (Garnefski & Kraaij, 2006). Although emotion regulation is only one part of self-regulation, it seems to be closely connected to general self-regulatory capacities. Indeed, difficulties with emotion regulation among depressed individuals are positively associated with cognitive control difficulties following a negative affective priming task, suggesting that these self-regulatory capacities contribute to depressive symptoms (Joormann & Gotlib, 2010).
Several cross-sectional studies also suggest that lower self-regulation scores are related to higher rates of alcohol problems, and to higher risk-taking more generally among college students (Magar, Phillips, & Hosie, 2008; Pearson, D’Lima, & Kelley, 2013; Pearson, Kite, & Henson, 2013). For example, specific facets of self-regulation (e.g., emotion instability and urgency) differentiate statistically derived drinking classes based on patterns of items from the Alcohol Use Disorder Identification Test (Babor, 2001). Using a person-centered approach, individuals in the “problem drinking class” exhibited significantly greater self-regulatory difficulties than the light, medium, and heavy drinking classes (Kuvaas et al., 2014). This has also been supported in a study that examined within-subject differences in alcohol intoxication and self-regulation over a one-week period among heavy drinking college students (Neal & Carey, 2007). Using event-level analyses, the authors found that self-regulation moderated the association between daily intoxication level and negative consequences such that those with higher self-regulation experienced smaller increases in alcohol problems as intoxication increased compared to those with lower self-regulation.
The above research suggests that individuals higher in self-regulation may consume comparable amounts of alcohol to those with low self-regulation yet experience significantly fewer alcohol-related problems. This may be due to failures in accurate self-monitoring drinking or ones’ level of intoxication, or to implement goal-consistent behaviors (e.g., avoiding alcohol-related harm, attending class, etc.). Further, manifestations of failures or reductions in self-regulation exist in the DSM-5 criteria for alcohol and other substance use disorders. Specifically, failures to stop or control use and continued use despite negative social, occupational, health, or psychological consequences (APA, 2013), represent difficulties in one or more of the aspects of self-regulation outlined by Brown (1998). This is consistent with behavioral models of addiction assuming that effective engagement with substance-free rewards, many of which require prolonged attention and self-regulation (i.e., academic achievement, exercise, developing a hobby), is protective against substance misuse (Acuff, Dennhardt, Correia, & Murphy, 2019; Bickel, Johnson, Koffarnus, MacKillop, & Murphy, 2014). These same self-regulatory difficulties may be present in depressive episodes and may explain some of the variance in the relation between depressive symptoms and alcohol misuse among college students. Behavioral models of depression stress the importance of deficits in positive reinforcement as contributing to depression, and regular patterns of behavior that effectively pursue goals/activities require self-regulation. A few studies have extended these findings prospectively, and the results support self-regulation (Hustad, Carey, Carey, & Maisto, 2009; Quinn & Fromme, 2010) and depressive symptoms (Acuff et al., 2018) as a predictor of alcohol problems over time. However, no study has examined the longitudinal relationship between self-regulation and depressive symptoms.
Current Study
These findings support the general proposition that depressive symptoms, self-regulation, and alcohol problems are related over time, although tests of relations have been unidirectional, and these variables have not been examined in a simultaneous model that accounts for the other variables. Temporal precedence (also known as priority) is a critical criterion in establishing causal relationships among variables (Hume, Norton, & Norton, 2005; Rosenthal & Rosnow, 2008), but precedence of one of these variables over the others has yet to be established. Although a number of possible configurations of temporal order exist, four different models seem to be the most likely based on previous support and are presented conceptually in Figure 1. The first model suggests that depressive symptoms precede alcohol problems, and that self-regulation does not play a central role (i.e., self-medication model). The second model suggests that depressive symptoms temporarily impair executive functioning, which diminishes self- regulatory capacity and leads to an increase in overall problems (i.e., depressed regulation model). The third model suggests that the depressant effects of alcohol on the central nervous system (potentially in combination with the negative effects of increases in alcohol problems) lead to diminished self-regulatory capacity and subsequent increases in depressive episodes (i.e., CNS depressant model). Finally, the fourth model suggests that self-regulatory deficits exist as a stable trait that precedes and contributes to the development of depressive symptoms and alcohol problems (i.e., self-regulatory failure model). Without explicit a priori hypotheses, the current exploratory study investigates these models of depressive symptoms, self-regulation, and alcohol problems over 16-months among heavy drinking college students. This research is an important step in developing a more complete understanding of the potential role of self-regulation in the comorbidity between depressive symptoms and alcohol problems. The results could guide more comprehensive etiological models and inform prevention and treatment efforts for high-risk young adults.
Figure 1.
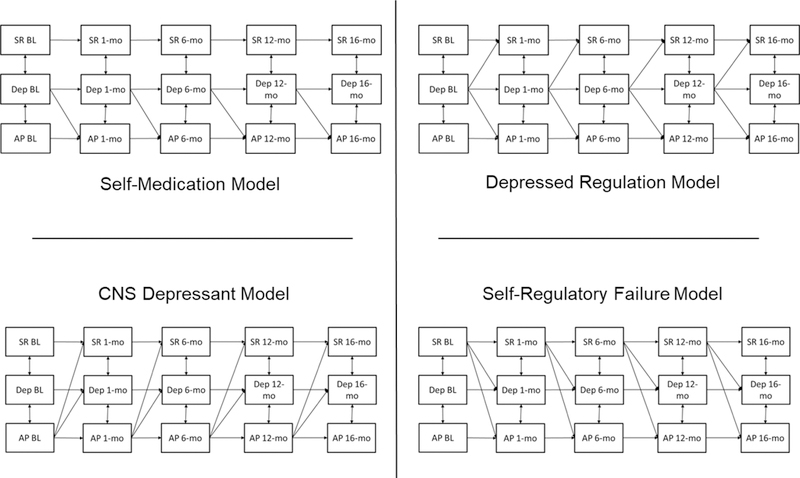
Representations of expected relations between self-regulation (SR), depressive symptoms (Dep), and alcohol problems (AP) for each model. College students (N = 393) were measured at five timepoints (i.e., baseline, 1-month, 6-month, 12-month, and 16-month). Support for the self-medication model would result in relations between depressive symptoms at one time point and alcohol problems at the next prospective timepoint, without positing any effect from self-regulation. Support for the depressed regulation model would result in relations between depressive symptoms at one time point and both alcohol problems and self-regulation at the next prospective timepoint. Support for the CNS depressant model would result in relations between alcohol problems at one time point and both depressive symptoms and self-regulation at the next prospective timepoint. Support for the self-regulatory failure model would result in relations between self-regulation at one time point and both depressive symptoms and alcohol problems at the next prospective timepoint.
Method
Participants
Participants were 393 undergraduate college students recruited from two large public universities in the United States. Students were eligible to participate in the study if they were enrolled as either a freshman or sophomore, were at least 18 years old, and had reported 2 or more heavy episodic-drinking episodes in the past month (4/5 or more standard drinks on one occasion for women/men, respectively). Most participants were freshmen (n = 244, 62.1%). The sample identified as 78.9% White, 10.9% Black or African American, 1.8% Asian, 1.8% American Indian, and 0.5% Hawaiian/Pacific Islander. Further, 5.9% of the sample identified their ethnicity as Hispanic. This study uses the same sample as a recent study that examined the longitudinal associations between depressive symptoms and alcohol problems (Acuff et al., 2018), although this study uses the full sample while the previous study used only the control group (n = 138).
Procedure
The current study is a secondary analysis from a larger project that evaluated brief alcohol interventions (Murphy et al., 2019). This was a sample of non-treatment seeking college students who were selected on the basis of self-reports of two or more past-month heavy drinking episodes (4/5 drinks for women/men). Participants were recruited via mass email research participation screening surveys at two large public universities. This study was described to them as a research study that would entail questionnaires about alcohol use and other activity engagement, and that some would also participate in an interview related to lifestyle, consumption of alcohol, and perception of others’ alcohol consumption. These individuals would also participate in a second session that would involve either having a discussion about college and career goals or learning about various relaxation techniques. If the student was eligible, study personnel described the study in more detail and scheduled the initial study appointment. At the initial appointment, participants completed measures on a private lab computer for 1 hour. During this visit, they were randomized to either an assessment-only control condition or to a brief motivational intervention (BMI) condition. Those randomized to the BMI completed another 1-hour session and were further randomized to complete either the substance-free activity session (intervention described in Murphy et al., 2019) or a relaxation training session one week later. All participants then returned to the lab to complete follow-up surveys 1-, 6-, 12-, and 16-months after completion of their initial session. Follow-up rates were high: 1-month (N = 366, 93% follow-up rate), 6-month (N =344, 88% follow-up rate), 12-month (N =342, 87% follow-up rate), and 16-month (N =311, 79% follow-up rate) post-intervention. The universities’ Institutional Review Boards approved all study procedures.
Measures
Self-Regulation.
The Short Self-Regulation Questionnaire (SSRQ; Carey, Neal, & Collins, 2004) is a 31-item measure used to assess behavioral regulation and ability to delay gratification. Items include “I have trouble making up my mind about things” and “I have trouble following through with things once I’ve made up my mind to do something.” Participants rated each item from 1 (strongly disagree) to 5 (strongly agree). Several items are reverse scored, and all items are summed to create a total self-regulation score, with higher scores indicating greater self-regulatory capacity. Previous work has established two subscales of the SSRQ, measuring impulse control and goal-setting behavior (Neal & Carey, 2005), although the current study focuses on the total score as an index of general self-regulatory capacities. Internal consistency for the SSRQ in the current sample exceeded a > .93 at all time-points.
Depressive Symptoms.
The Depression, Anxiety, and Stress Scale (DASS-21; Antony, Bieling, Cox, Enns, & Swinson, 1998; Lovibond & Lovibond, 1995) is a 21-item measures that assesses past week symptoms of depression, anxiety, and stress. Examples items include “I was unable to become enthusiastic about anything” and “I couldn’t seem to experience any positive feeling at all.” Participants rated how much each item applied to them from 0 (Didnot apply to me at all) to 3 (Applied to me very much, or most of the time). Items on the DASS are separated by subscale, summed, and multiplied by two to generate subscale scores. Only the depression subscale was used for the present analyses. This measure has demonstrated good internal consistency and concurrent validity (Antony et al., 1998). Internal consistency for the DASS depression subscale in the current sample exceeded a > .88 at all time-points.
Alcohol Consumption.
Participants were asked to estimate the total number of standard drinks they consumed each day during a typical week in the past month on the Daily Drinking Questionnaire (DDQ; Collins, Parks, & Marlatt, 1985). The number estimated for each day is summed to produce an estimate of typical drinks per week. The DDQ is a reliable measure used frequently to assess college student drinking (Carey et al., 2018).
Alcohol Problems.
The 48-item Young Adult Alcohol Consequences Questionnaire (YAACQ) is a Yes/No self-report measure of alcohol-related problems or consequences experienced over the past 1 month. The YAACQ has demonstrated good predictive validity and test-retest reliability (Read, Kahler, Strong, & Colder, 2006). Internal consistency exceeded α > .90 at all time-points.
Data Analysis
Data was analyzed using Mplus v7.4 (Muthen & Muthen, 2015). Outliers were winsorized by changing values outside of 3.29 standard deviations above the mean to one unit higher than the largest non-outlier, as recommended by Tabachnick and Fidell (2013). Due to modest nonnormality in data distributions, data were analyzed using robust maximum likelihood estimation (Yuan & Bentler, 1998). Missing data were handled using Full Information Maximum Likelihood estimation. All tested models were overidentified. We tested our hypotheses using autoregressive cross-lagged models examining the associations between depressive symptoms, self-regulation, and alcohol problems at 5-time points. Contemporaneous associations were modeled by correlating each construct at each time-point (e.g., 12-month depressive symptoms associated with 12-month alcohol problems and 12-month self-regulation). Autoregressive associations were modeled by regressing each variable onto the same variable measured at the previous time-point (e.g., 16-month depressive symptoms regressed onto 12-month depressive symptoms; 12-month depressive symptoms regressed onto 6-month regressive symptoms). Cross-lagged associations were modeled by regressing each variable onto different variables measured at previous time-points (e.g., 16-month depressive symptoms regressed onto 12-month self-regulation and alcohol problems; 12-month depressive symptoms regressed onto 6-month self-regulation and alcohol problems). Shared variance between different variables measured at common time-points was modeled in all analyses. Due to known relationships with primary study variables (Nolen-Hoeksema & Corte, 2004; Soltis et al., 2018), we controlled for condition, gender, and baseline alcohol consumption in all models.
Model fit indices for six different models were examined. Conceptual representations of each statistically tested model are included in the supplementary materials. In model 1, all relations at all time-points were unconstrained (i.e., not forced to be equal). In model 2, autoregressive relations were constrained to be equal. In model 3, cross-lagged relations, in addition to autoregressive relations, were constrained to be equal. In model 4, covariate effects were constrained to be equal in addition to autoregressive and cross-lagged relations. In model 5, within variable covariance (i.e., relations between same variables across time) were constrained to be equal in addition to model constraints described for model 4. This model suggests that, in addition to the true effects, the residual correlation due to multiple measurement (i.e., same measurement at different time points) should not vary across time. Finally, between variable covariances (i.e., relations between different variables at the same time point) were constrained to be equal in model 6, in addition to the model constraints described for all previous models. This model suggests that, in addition to the true cross-lagged effects, the residual variance between variables should not vary across time.
Model selection was determined by a balance of parsimony, interpretability, and statistical model fit. To assess model fit, six model fit indices were examined and reported, per the suggestion of Kline (2016): the model Chi-square, the root mean square error of approximation (RMSEA), the comparative fit index (CFI), the standardized root mean square residual (SRMR), the Akaike Information Criterion (AIC) and the Bayesian Information Criterion (BIC). The model Chi-square is an indicator of model fit, with nonsignificant values indicating the model is not rejected and significant values indicating the model fails to fit the data. Chi-square difference tests accounting for scaling correction were used to compare more restricted and parsimonious models with less restricted and parsimonious models (Satorra, 2000). The goal is to obtain a balance of parsimony and model fit, so we were interested in a more constrained model that does not fit significantly worse than a less constrained model. Significant Chi-square difference tests indicate whether a more restricted model fits significantly worse than a less restricted model (Werner & Schermelleh-Engel, 2010). RMSEA is a model fit index favoring parsimony, and values with confidence intervals below .08 suggest adequate model fit (Hu & Bentler, 1999). The CFI represents incremental improvement over a base model with no variables, and values greater than or equal to .90 are considered to represent acceptable fit (Hu & Bentler, 1999). The SRMR is another index of good fit, with values under .08 representing good fit (Hu & Bentler, 1999). Lastly, we reported two indices of parsimony, the AIC and the BIC, with smaller numbers representing more parsimonious fit. For all significant results, we report both unstandardized (Figure 2) and standardized estimates (in text).
Figure 2.
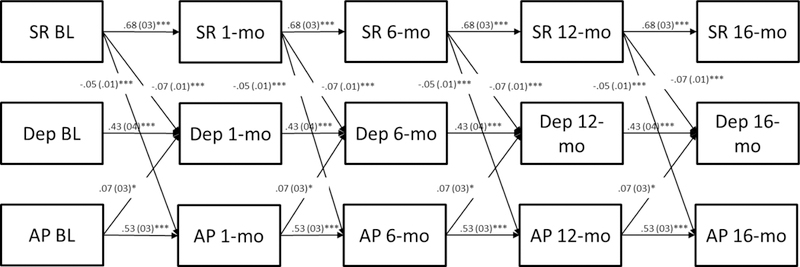
Relationships between self-regulation (SR), depressive symptoms (Dep), and alcohol problems (AP) among college students (N = 393) measured at five timepoints (i.e., baseline, 1-month, 6-month, 12-month, and 16-month). Only significant relations are presented in this figure; full conceptual models can be found in the supplementary materials. Unstandardized beta estimates are reported in this figure. Autoregressive and cross-lagged relations were held constant across timepoints; contemporaneous relationships between variables were allowed to vary freely. Lower self-regulation, and higher alcohol problems and depressive symptoms, prospectively predicted higher depressive symptoms. Higher alcohol problems and lower self-regulation prospectively predicted higher alcohol problems. Only higher self-regulation prospectively predicted higher self-regulation. Lines represent significant cross-lagged or autoregressive relationships identified in the model. Contemporaneous relations were also significant but are not reported in this figure. *p < .05, ** p < .01, *** p < .001.
Results
Descriptive Statistics and Correlations among Variables
Descriptive statistics are reported in Table 1. At baseline, participants reported consuming 16.76 alcoholic drinks per week in the last month (SD = 11.97) and experiencing 13.05 alcohol-related problems over the past month (SD = 7.89). The mean level of depressive symptoms at baseline was 7.42 (SD = 8.85) and 19.3% of the sample reported at least moderate depressive symptoms; 7.4% scored above the clinical cutoff for severe symptoms. Correlations among all study variables at all time-points are reported in Table 2. At baseline, higher levels of self-regulation were significantly associated with lower depressive symptoms and alcohol problems, but not typical drinks per week. Similarly, higher depressive symptoms were significantly associated with higher levels of alcohol problems, but not typical drinks per week. Finally, higher levels of alcohol problems were associated with greater typical drinks per week. These relations were generally consistent at each subsequent time-point.
Table 1.
Demographics and Mean, Standard Deviation, Skewness, and Kurtosis for Primary Study Variables
| Variable | N | Percent | M | SD | Skewness | Kurtosis | ||
|---|---|---|---|---|---|---|---|---|
| Statistic | S. E. | Statistic | S. E. | |||||
| Gender (% female) | 393 | 60.8 | ||||||
| Year in school at BL | 392 | |||||||
| Freshmen | 244 | 62.1 | ||||||
| Sophomore | 148 | 37.7 | ||||||
| Race | ||||||||
| White | 79.9 | |||||||
| Black | 10.7 | |||||||
| Other | 9.4 | |||||||
| Age | 381 | 18.77 | 1.07 | 2.46 | 13 | 8.93 | .25 | |
| BL SSRQ | 393 | 114.68 | 16.67 | −.34 | 12 | .27 | .25 | |
| 1-mo. SSRQ | 363 | 116.88 | 16.57 | −.01 | 13 | −.17 | .26 | |
| 6-mo. SSRQ | 338 | 117.62 | 16.31 | −.09 | 13 | −.02 | .26 | |
| 12-mo. SSRQ | 340 | 117.41 | 17.46 | −.24 | 13 | −.07 | .26 | |
| 16-mo. SSRQ | 304 | 117.54 | 17.27 | −.19 | 14 | −.15 | .28 | |
| BL DASS | 393 | 7.42 | 8.85 | 1.83 | 12 | 3.22 | .25 | |
| 1-mo. DASS | 364 | 5.16 | 7.63 | 2.87 | 13 | 10.77 | .26 | |
| 6-mo. DASS | 342 | 4.84 | 7.31 | 2.48 | 13 | 6.78 | .26 | |
| 12-mo. DASS | 340 | 5.96 | 8.83 | 2.57 | 13 | 7.87 | .26 | |
| 16-mo. DASS | 308 | 5.55 | 8.16 | 2.22 | 14 | 4.85 | .28 | |
| BL DDQ | 393 | 16.76 | 11.97 | 1.50 | 12 | 2.39 | .25 | |
| BL YAACQ | 393 | 13.05 | 7.89 | .62 | 12 | .02 | .25 | |
| 1-mo. YAACQ | 365 | 8.88 | 7.96 | 1.10 | 13 | .66 | .25 | |
| 6-mo. YAACQ | 343 | 8.01 | 8.11 | 1.16 | 13 | .66 | .26 | |
| 12-mo. YAACQ | 343 | 8.52 | 8.79 | 1.17 | 13 | .63 | .26 | |
| 16-mo. YAACQ | 311 | 8.40 | 9.35 | 1.48 | 14 | 1.60 | .28 | |
Note. BL = Baseline; DDQ = Daily Drinking Questionnaire; SSRQ = Short-Self-regulation Questionnaire; DASS = Depression subscale of the Depression, Anxiety, and Stress Scale; YAACQ = Young Adult Alcohol Consequences Questionnaire.
Table 2.
Correlations Among Variables at all Timepoints
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gender (% female) | - | |||||||||||||||
| 2. BL SSRQ | −17** | - | ||||||||||||||
| 3. 1-mo. SSRQ | −.11* | 77** | - | |||||||||||||
| 4. 6-mo. SSRQ | −.08 | 73** | .77** | - | ||||||||||||
| 5. 12-mo. SSRQ | −.05 | 69** | 73** | 74** | - | |||||||||||
| 6. 16-mo. SSRQ | −.06 | .66** | 73** | 71** | .82** | - | ||||||||||
| 7. BL DASS | .15** | −.47** | − 37** | −.31** | −.35** | − 34** | - | |||||||||
| 8. 1-mo. DASS | .10 | −.39** | − 42** | − 32** | −.34** | −.36** | .61** | - | ||||||||
| 9. 6-mo. DASS | .14* | −.34** | −.29** | − 43** | −.37** | −.35** | .50** | .48** | - | |||||||
| 10. 12-mo. DASS | .05 | −.39** | − 34** | −.36** | −.43** | −.36** | .53** | .47** | .52** | - | ||||||
| 11. 16-mo. DASS | .04 | −.32** | −.31** | −.33** | − 47** | −.45** | 44** | .45** | .47** | .63** | - | |||||
| 12. BL YAACQ | .13** | −.36** | −.30** | −.25** | −.26** | − 29** | 34** | .26** | .29** | .26** | .24** | - | ||||
| 13. 1-mo. YAACQ | −.05 | −.19** | −.28** | −.20** | −.23** | −.28** | .18** | .26** | 23** | .22** | 23** | .60** | - | |||
| 14. 6-mo. YAACQ | −.04 | −.20** | −.27** | − 32** | −.28** | −.26** | .12* | .24** | .35** | .26** | .29** | .49** | 64** | - | ||
| 15. 12-mo. YAACQ | −.02 | −.22** | − 19** | −.26** | −.30** | −.28** | 14** | .18** | .22** | .25** | .24** | .49** | .51** | .56** | - | |
| 16. 16-mo. YAACQ | −.07 | −.22** | −.26** | − 32** | −.37** | −.38** | .14* | .16** | .24** | .27** | .38** | .43** | .45** | .53** | .72** | - |
| 17. BL DDQ | − 29** | −.02 | −.05 | −.07 | −.08 | −.09 | .00 | .05 | .01 | .05 | .00 | .36** | .38** | .36** | 27** | 25** |
Note. BL = baseline; SSRQ = Short Self-Regulation Questionnaire total score; DASS = Depression subscale of the Depression Anxiety, and Stress Scale; YAACQ = Young Adult Alcohol Consequences Questionnaire total score; DDQ; typical drinks per week calculated from the Daily Drinking Questionnaire.
p < .05
p < .01.
Cross-lagged Model Selection and Results
Model Selection.
Model fit results are presented in Table 3. Fit indices for all models provided mixed results. All model chi-square tests were significant, although the chi-square test is known to be sensitive to minor model misspecifications and sample size (Hu & Bentler, 1999). Models 1, 2, and 3 demonstrated the strongest model fit with regards to the CFI and SRMR indices; however, the RMSEA confidence interval for Models 1 and 2 were slightly above acceptable limits. Models 4, 5, and 6 demonstrated slightly worse CFI and SRMR indices, but with RMSEA values within acceptable limits. The Chi-square difference tests indicated that Model 2, which added autoregressive equality constraints, did not fit the data significantly worse than Model 1, and that Model 3, which added cross-lagged equality constraints to the autoregressive equality constraints, did not fit the data significantly worse than Model 2. However, Model 4, which added the constraints of equivalent covariate effects, did fit the data significantly worse than Model 3. Thus, adding equivalent covariate effects to Model 4 resulted in significantly worse model fit and Model 3, with autoregressive and cross-lagged equality constraints, provides the best balance of parsimony and model fit. Results for the final model (Model 3) are displayed in Figure 2.
Table 3.
Model Fit Indices
| X2 (df), p-value | X2 Diff. Test |
RMSEA | CFI | SRMR | AIC | BIC | |
|---|---|---|---|---|---|---|---|
| Model 1 | 167.80 (48,)<.001 | - | .08 (.07 & .09) | .95 | .08 | 36507.99 | 37092.14 |
| Model 2 | 179.22 (56), < .001 | 8.63, > .05 | .08 (.06 & .09) | .95 | .08 | 36525.77 | 37078.129 |
| Model 3 | 197.79 (75), <.001 | 19.09, > .05 | .07 (.05 & .08) | .95 | .08 | 36513.89 | 36990.75 |
| Model 4 | 272.00 (111), <.001 | 78.22, < .05 | .06 (.05& .07) | .93 | .09 | 36507.79 | 36841.59 |
| Model 5 | 320.08 (126), <.001 | 48.39, < .05 | .06 (.05 & .07) | .91 | .10 | 36549.44 | 36823.63 |
| Model 6 | 379.61 (138), <.001 | 58.58, < .05 | .07 (.06 & .08) | .89 | .15 | 36608.03 | 36834.54 |
Note. Due to the use of MLR estimation in analyses, Chi-square difference tests accounted for scaling correction. Chi-square difference test results for each model were compared to the previous model in the Table. Significant Chi-square indicates significantly worse fit for the more constrained model. Bold text indicates the strongest fit for each index. Model 1 = All relationships (autoregressive, cross-lagged, and covariances) unconstrained; Model 2 = autoregressive effects constrained; Model 3 = autoregressive and cross-lagged effects constrained; Model 4 = autoregressive, cross-lagged, and covariate effects constrained; Model 5 = autoregressive, cross-lagged, covariate, and across-time covariance effects constrained; Model 6 = autoregressive, cross-lagged, covariate, across-time covariance, and within time covariance effects constrained. Df = degrees of freedom; RMSEA = Root Mean Square Error of Approximation; CFI = Comparative Fit Index; SRMR = Standardized Root Mean Squared Residual; AIC =Akaike Information Criterion; BIC = Bayesian Information Criterion.
Model-based Contemporaneous Associations.
We examined model-based correlations between variables at each time-point accounting for covariate effects and residual variance from relations at previous timepoints. At baseline, higher depressive symptoms were significantly associated with lower self-regulation (standardized estimate (β)=−.36; unstandardized estimate (B) (SE) = −49.46 (9.23),p < 0.001) and higher alcohol problems (β=30; B (SE) = −20.21 (4.21), p < 0.001); higher self-regulation was associated with lower alcohol problems (β=−.33; B (SE) = −41.90 (6.62), p < 0.001). At 1-month, higher depressive symptoms were significantly associated with lower self-regulation (β=−.22; B (SE) = −13.61 (3.45),p < 0.001) and higher alcohol problems (β=.19; B (SE) = 6.49 (2.20), p = .003); higher self-regulation was associated with lower alcohol problems (β=−.19; B (SE) = −11.64 (3.19),p < 0.001). At 6-months, higher depressive symptoms were significantly associated with lower self-regulation (β=−.30; B (SE) = − 19.28 (4.72),p < 0.001) and higher alcohol problems (β=.24; B (SE) = 9.06 (3.10),p = 0.003); higher self-regulation was associated with lower alcohol problems (β=−.20; B (SE) = −12.04 (4.07), p = 0.003). At 12-months, higher depressive symptoms were significantly associated with lower self-regulation (β=−.18; B (SE) = −15.10 (5.76), p = 0.009), but not with alcohol problems (β=.08; B (SE) = 4.24 (3.64), p = 0.24); higher self-regulation was associated with lower alcohol problems (β=−.13; B (SE) = −11.20 (5.11), p = 0.03). At 16-months, higher depressive symptoms were significantly associated with lower self-regulation (β=−.17; B (SE) = −10.56 (4.05), p = 0.009) and higher alcohol problems (β=.23; B (SE) = 8.79 (3.34), p = 0.009); higher self-regulation was significantly associated with lower alcohol problems (β=−.13; B (SE) = −8.35 (3.42), p = 0.015).
Autoregressive Associations.
We also examined the relationships between the same variables at different time points (e.g., depressive symptoms at baseline with depressive symptoms at follow-ups) after controlling for covariates and other variables of interest in the model. Unstandardized estimates for all significant relationships are reported in Figure 2. As expected, greater levels of depressive symptoms significantly predicted greater levels of depressive symptoms at subsequent timepoints (β = .50 p < .001). Similarly, greater levels of self-regulation significantly predicted greater levels of self-regulation at subsequent time-points (β = .71 p < .001). Finally, greater levels of alcohol problems significantly predicted greater levels of alcohol problems at subsequent time-points (β = .53, p < .001).
Cross-lagged Associations.
Next, we examined relations between variables at a single time-point with different variables at subsequent time points (e.g., baseline predicting 1-month, 1-month predicting 6-month) while controlling for covariates and all other variables of interest. Higher alcohol problems (β = .07, p = .02) prospectively predicted higher depressive symptoms, lending partial support for the CNS depressant model. Lower self-regulation prospectively predicted higher alcohol problems (β = −.10, p < .001) and higher depressive symptoms (β = −.15, p < .001), lending support for the self-regulatory failure model. However, depressive symptoms did not predict alcohol problems or self-regulation, explicitly ruling out the self-medication and depressed regulation models. No other cross-lagged associations were significant.1 Resulting R2 values for dependent variables in the model can be found in Table 4.
Table 4.
R2 for each predicted variable in the model
| Variable |
R2 for the Final Model |
All cross- lagged relations removed |
Change in R2 for a model with all autoregressive relations and cross-lagged relations only for: |
||
|---|---|---|---|---|---|
| SSRQ | DASS | YAACQ | |||
| 1-mo. SSRQ |
.537 | .507 | .030 | .003 | .004 |
| 6-mo. SSRQ |
.609 | .580 | .029 | .000 | .002 |
| 12-mo. SSRQ |
.579 | .539 | .043 | −.004 | −.001 |
| 16-mo. SSRQ |
.654 | .614 | .045 | −.008 | −.003 |
| 1-mo. DASS |
.364 | .333 | .021 | .019 | .006 |
| 6-mo. DASS |
.328 | .295 | .016 | .020 | .011 |
| 12-mo. DASS |
.285 | .266 | .050 | .022 | .000 |
| 16-mo. DASS |
.407 | .380 | .016 | .026 | −.003 |
| 1-mo. YAACQ |
.455 | .430 | .016 | .006 | .014 |
| 6-mo. YAACQ |
.451 | .412 | .027 | .008 | .017 |
| 12-mo. YAACQ |
.351 | .319 | .017 | .003 | .022 |
| 16-mo. YAACQ |
.466 | .433 | .015 | −.001 | .030 |
Note. R2 for all variables demonstrated p-values < .001. SSRQ = Short Self-Regulation Questionnaire total score; DASS = Depression subscale of the Depression Anxiety, and Stress Scale; YAACQ = Young Adult Alcohol Consequences Questionnaire total score.
Discussion
Self-regulation, depressive symptoms, and alcohol problems have all demonstrated significant associations in samples of heavy drinking college students, yet these variables have never been studied prospectively in a single model. This study explicates the temporal order of these variables and highlights differential pathways to comorbidity between depressive symptoms and alcohol problems. Our results provide initial support for the self-regulatory failure model of comorbidity among heavy drinking college students, in which self-regulation is a stable trait that prospectively predicts both depressive symptoms and alcohol problems. This is consistent with previous research demonstrating that self-regulation is a prospective predictor of alcohol problems (Hustad et al., 2009; Soltis et al., 2018) and extends these findings by controlling for autoregressive relations. Further, our findings support self-regulation as a stable, transdiagnostic factor associated with depressive symptoms and alcohol problems, at least among college student heavy drinkers.
In contrast, the three alternative explanatory models for self-medication, depressed regulation, and CNS depressant model were not supported. Although contemporaneously correlated with both alcohol problems and self-regulation, depressive symptoms did not predict either variable prospectively. In previous studies examining the self-medication hypothesis, alcohol problems have typically been modeled as the dependent variable to understand how a depressive state can increase engagement in alcohol problems (Acuff et al., 2018; Dennhardt & Murphy, 2011; Kenney et al., 2018, 2017). Previous studies have not controlled for autoregressive relations (i.e., controlling for the same variable measured over time, such as later alcohol problems predicted from prior alcohol problems) or self-regulation, missing important shared variance that may better account for relations and change results. Indeed, the current study suggests that greater alcohol problems prospectively predict depressive symptoms rather than the other way around, at least among college students. Thus, neither the self-medication model nor the depressed regulation model was ultimately supported when controlling for each variable over time in addition to self-regulation. The third model (i.e., CNS depressant model) was partially supported, with alcohol problems prospectively predicting depressive symptoms across time points. However, the pathway for this relationship was not through any change in self-regulation, suggesting that the impact of the alcohol problems may have a direct effect on subsequent depressive symptoms (e.g., alcohol may impact inhibitory control, mood, health, and social functioning thereby increasing depressive symptoms; Finn, Justus, Mazas, & Steinmetz, 1999; Singleton & Wolfson, 2009).
The present findings most adequately fit within a contextual model of self-regulation change mechanisms, which emphasizes the compounding effect of self-regulatory capacity and context in understanding addictive behaviors (Roos & Witkiewitz, 2017). Under this model, self-regulatory behavior is considered within both the immediate situational (e.g., internal states and external cues) and broader (e.g., major life events, environmental conditions) context. Some individuals may have lower rates of self-regulation overall that are stable over time, which increases the likelihood of alcohol problems. However, not all people with low self-regulation are experiencing high levels of alcohol problems, a phenomenon that may be accounted for by protective contextual factors within the individual environment (e.g., effective prohibitions against underage drinking, effective harm reduction strategies and policies). Our findings suggest that this model may generally apply to psychopathology other than alcohol misuse as well, as depressive symptoms were also predicted by low levels of self-regulation. In fact, environments that are conducive to alcohol problems (e.g., many college environments), may be one context in which depressive symptoms are more likely to develop (American College Health Association, 2015). Although our study does not elucidate the mechanisms driving this relationship, several processes may exist. College students may develop a pattern of problematic drinking that is, to some degree, uncontrollable due to impaired attentional processes (inadequate or inaccurate informational input) and/or inability to detect a problem/discrepancy which may lead to a sense of helplessness and other depressive symptoms. Alternatively, college students may have general levels of self-regulation that, under the influence of alcohol, are further dampened to result in more severe alcohol problems and a depressive reaction (Finn et al., 1999). Poor self-regulation could also impact sleep, diet, physical activity and social relationships which could in turn impact both alcohol problems and depressive symptoms (Singleton & Wolfson, 2009; Sudhinaraset, Wigglesworth, & Takeuchi, 2015). Self-regulation may also influence engagement in substance-free activities (e.g., academic activity, exercise) that are often less immediately gratifying but hold greater long-term future value. Diminished engagement in rewarding activities is a known risk factor for alcohol problems (Acuff et al., 2019; Correia, Carey, Simons, & Borsari, 2003; Leventhal et al., 2015) and depression (Lewinsohn, Sullivan, & Grosscup, Sally, 1980) and may operate as a mechanism explaining this relationship.
More broadly, our study also provides the first examination of longitudinal relations between self-regulation and depressive symptoms, and the results have implications for theories of self-regulation and depressive symptoms. The results are only partially consistent with models of depressive symptoms and self-regulation suggesting that a decrease in self-regulatory capacity precedes the onset of depressive symptoms (Strauman, 2002, 2017). Although it does seem that self-regulation deficits precede depressive symptoms as this model suggests, it also appears that self-regulatory capacity is relatively stable over time and may not necessarily shift prior to the onset of the depressive symptoms. It is important to note, however, that this sample contained individuals with low levels of depressive symptoms, and these variables may interact differently in samples with clinical levels of depression. Further, our measurement approach was not sensitive to changes that may occur just before the onset of depressive symptoms, given that we included only 5 assessment points over 16 months.
The specific self-regulatory deficits that confer greatest risk for depressive symptoms or alcohol problems remain unclear. Self-regulation is a multi-faceted construct consisting of information processing and self-monitoring skills in both cognitive and emotional domains. Specific self-regulatory deficits may be more associated with a depressive episode compared to alcohol problems. Alternatively, the same self-regulatory concerns may be associated with both depressive symptoms and alcohol problems. This is important because certain self-regulatory domains may be more amenable to change (e.g., goal setting) than others (e.g., impulse control). Although our study does not address this question, it does provide the groundwork for selfregulation as a transdiagnostic mechanism and further justification to examine different facets of self-regulation as predictors of depressive symptoms and alcohol problems.
Strengths, Limitations and Future Directions
The study had several strengths, including the inclusion of a relatively large sample collected at two sites with five follow-ups over a 16-month period. Follow-up retention was also high. The analytic approach improved upon previous research in this area by controlling for residual variances from previous timepoints and relationships. However, several limitations should also be noted. First, our sample included 19–21-year-old heavy drinkers with relatively low levels of depressive symptoms (26.7% reported elevated levels of depressive symptoms). The results may be different in clinical samples. Severe depressive symptoms may significantly impair self-regulatory capacity, which could lead to an increase in alcohol problems. Second, our examination focused on heavy drinkers who were already in the young adult developmental period. Self-regulation may have already been influenced by depressive episodes or alcohol use earlier in life for some individuals. Third, these results might be different in a study that examined differences between chronic heavy drinkers and abstainers/light drinkers. Chronic heavy drinking is associated with long-term neurological deficits (Kroenke et al., 2014; Pitel, Segobin, Ritz, Eustache, & Beaunieux, 2015), and the effects of heavy alcohol use on self-regulation may not manifest until late into adulthood. This heavy use may affect executive functioning, which is necessary but not sufficient for effective self-regulation. Limits to these processes, however, may more significantly impair self-regulatory strategies. Fourth, college students represent a population selected due to variables that require reasonably high levels of self-regulation (e.g., high school GPA, achievement tests), resulting in restricted range in this variable. Fifth, future research should attempt to examine different facets of self-regulation (i.e., goal setting and impulse control) using a more comprehensive measurement approach, including with measures that have more items and that are not highly multicollinear. Sixth, contemporaneous associations represent residual associations that account for covariates and all autoregressive and cross-lagged relations modeled in the analyses. Thus, it important to acknowledge that these correlations do not represent simple bivariate relations between variables, but instead represent what remains in a bivariate relation after controlling for all other variables. Finally, although our findings support a stable, transdiagnostic model of self-regulation, they do not explicitly rule out the other posited models (i.e., depressive symptoms or heavy alcohol use damaging self-regulatory capacity) or the role of other unmeasured variables. Reward functioning deficits, for example, have been implicated as a candidate alternative mechanism of comorbidity (i.e., depressed individuals have blunted reward response or lack of access of alternatively available activities; Acuff et al., 2018; Vujanovic, Wardle, Smith, & Berenz, 2016), opening the door for inquiry into other alternative mechanisms. Further, protective behavioral strategies, elsewhere called “alcohol-specific self-regulation” (D’Lima, Pearson, & Kelley, 2012; Pearson, D’Lima, et al., 2013), may be a manifestation of these self- regulatory processes, and indeed, have shown significant associations with both depressive symptoms and alcohol-related problems (Martens et al. 2008). Models that include these variables could further explicate a comprehensive transdiagnostic model.
Implications for Theory and Practice
Our results provide an alternative mechanism to self-medication models, namely selfregulation, which prospectively predicts depressive symptoms and alcohol problems and may explain additional variance in this comorbidity. Low self-regulation may be a common risk factor for both depressive symptoms and alcohol problems, a “prerequisite” through which both develop possibly within the context of environmental risk factors like socioeconomic status or other forms of trauma or deprivation in childhood (Roos & Witkiewitz, 2017; Tripp, Mcdevitt-Murphy, Avery, & Bracken, 2015). These factors may influence initial deficits in self-regulation by emerging adulthood (e.g., inability to plan and implement behavior towards a long-term goal) which in turn increases personal risk of depressive symptoms and alcohol problems (see Roos & Witkiewitz, 2017), although our study was not designed to test this. The study also found that alcohol problems predicts depressive symptoms among college students when controlling for autoregressive relations, suggesting that targeting alcohol problems may be an effective way to also reduce depression (Murphy et al., 2019, 2012).
Our results also highlight self-regulation as a promising target for intervention. Research has found that emerging adults with low self-regulation or depressive symptoms are less likely to respond to alcohol interventions (Carey, Henson, Carey, & Maisto, 2007; Murphy et al., 2012), and that increases in self-regulation following an intervention mediates the effect of a brief motivation intervention on changes in alcohol misuse among heavy drinking college students (Soltis et al., 2018), suggesting that self-regulation may be malleable. Interventions focusing on increasing goal-setting behaviors, tracking behavior over time, and increasing orientation toward future activities may be mechanisms through which self-regulation is affected, and this may also be the case for interventions targeting depressive symptoms and may be an effective transdiagnostic mechanisms for interventions focused on treating the specific population with comorbidity (Daughters, Magidson, Lejuez, & Chen, 2016). Further, brief motivational interventions targeting alcohol misuse that include either relaxation training or enhancing substance-free activities and future goals demonstrate reductions in alcohol problems and depressive symptoms, and increases in protective behavioral strategies and substance-free activities, supporting the functional association among these variables (see Murphy et al., 2019, which examined treatment outcomes using the same sample included in the present study).
Conclusion
Our results suggest that self-regulation may be a transdiagnostic risk-factor for increases in depressive symptoms and alcohol problems over a 16-month period in heavy drinking college students. These findings provide support for the self-regulatory failure model as an explanation of the comorbidity between depressive symptoms and alcohol problems. Interventions that enhance self-regulation may have salutary effects on both depressive symptoms and alcohol problems.
Supplementary Material
Acknowledgments
This work was supported by National Institute of Health grants R01 AA020829 (PI: James G. Murphy), F31 AA027140 (PI: Samuel F. Acuff), and F31 AA026486 (PI: Kathryn E. Soltis). The funding source had no role other than financial support. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism or the National Institutes of Health. The authors declare no conflict of interest. Some of the data presented in this article were presented in the form of a poster at the 2019 Collaborative Perspectives on Addiction conference.
Footnotes
We also tested two alternative models, each replacing the SSRQ total score with one of the SSRQ subscales (i.e., goal setting and impulse control) first derived by Neal and Carey (2005). The autoregressive results remained the same for both models. Neither the goal setting or impulse control scale predicted either depressive symptoms or alcohol problems. High correlations between the subscales (rs > .67 at all timepoints) precluded further simultaneous analyses.
Contributor Information
Samuel F. Acuff, Department of Psychology, University of Memphis, Memphis, Tennessee, USA
Kathryn E. Soltis, Department of Psychology, University of Memphis, Memphis, Tennessee, USA
Ashley A. Dennhardt, Department of Psychology, University of Memphis, Memphis, Tennessee, USA
Brian Borsari, Mental Health Service (116B) San Francisco VA Medical Center, San Francisco, California, USA.
Matthew P. Martens, Department of Educational, School, and Counseling Psychology, University of Missouri, Columbia, Missouri, 65211, USA
Katie Witkiewitz, Department of Psychology and Center on Alcoholism, Substance Abuse, and Addictions, University of New Mexico, Albuquerque, New Mexico, USA.
James G. Murphy, Department of Psychology, University of Memphis, Memphis, Tennessee, USA
References
- Acuff SF, Dennhardt AA, Correia CJ, & Murphy JG (2019). Measurement of substance-free reinforcement in addiction: A systematic review. Clinical Psychology Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acuff SF, Soltis KE, Luciano MT, Meshesha LZ, Dennhardt AA, Pedrelli P, & Murphy JG (2018). Depressive symptoms as predictors of alcohol problem domains and reinforcement among heavy drinking college students. Psychology of Addictive Behaviors, 32(7), 792–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College Health Association. (2015). American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2015. Hanover, MD: American College Health Association; 2015. [Google Scholar]
- Antony MM, Bieling PJ, Cox BJ, Enns MW, & Swinson RP (1998). Psychometric Properties of the 42-Item and 21-Item Versions of the Depression Anxiety Stress Scales in Clinical Groups and a Community Sample. Psychological Assessment, 10(2), 176–181. [Google Scholar]
- Babor T (2001). The Alohol Use Disorders Identification Test. Who, (07), 1–40. Retrieved from http://whqlibdoc.who.int/hq/2001/who_msd_msb_01.6a.pdf [Google Scholar]
- Bickel WK, Johnson MW, Koffarnus MN, MacKillop J, & Murphy JG (2014). The behavioral economics of substance use disorders: Reinforcement pathologies and their repair. Annual Review of Clinical Psychology, 10, 641–677. 10.1146/annurev-clinpsy-032813-153724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton JM, Robinson J, & Sareen J (2009). Self-medication of mood disorders with alcohol and drugs in the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Affective Disorders, 115(3), 367–375. 10.1016/jjad.2008.10.003 [DOI] [PubMed] [Google Scholar]
- Brown JM (1998). Self-regulation and the addictive behaviors. In Treating addictive behaviors (2nded.). [Google Scholar]
- Carey KB, Henson JM, Carey MP, & Maisto SA (2007). Which Heavy Drinking College Students Benefit From a Brief Motivational Intervention? Journal of Consulting and Clinical Psychology, 75(4), 663–669. Retrieved from http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed8&NEWS=N&AN=2007462603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Neal DJ, & Collins SE (2004). A psychometric analysis of the self-regulation questionnaire. Addictive Behaviors, 29(2), 253–260. 10.1016/j.addbeh.2003.08.001 [DOI] [PubMed] [Google Scholar]
- Carey KB, Walsh JL, Merrill JE, Lust SA, Reid AE, Scott-Sheldon JLA, ... Carey MP (2018). Using e-mail boosters to maintain change after brief alcohol interventions for mandated college students: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 86(9), 787–798. 10.1037/ccp0000339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, & Scheier MF (2011). Self-regulation of action and affect In Vohs KD & Baumeister RF (Eds.), Handbook of self-regulation: Research, theory, and applications (pp. 3–21). New York, NY: Guilford Press. [Google Scholar]
- Collins RL, Parks GA, & Marlatt GA (1985). Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology, 53(2), 189–200. 10.1037/0022-006X.53.2.189 [DOI] [PubMed] [Google Scholar]
- Correia CJ, Carey KB, Simons JS, & Borsari BE (2003). Relationships between binge drinking and substance-free reinforcement in a sample of college students: A preliminary investigation. Addictive Behaviors, 28(2), 361–368. 10.1016/S0306-4603(01)00229-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cranford JA, Eisenberg D, & Serras AM (2009). Substance use behaviors, mental health problems, and use of mental health services in a probability sample of college students. Addictive Behaviors, 34(2), 134–145. 10.1016/_j.addbeh.2008.09.004 [DOI] [PubMed] [Google Scholar]
- Creed PA, Fallon T, & Hood M (2009). The relationship between career adaptability, person and situation variables, and career concerns in young adults. Journal of Vocational Behavior. 10.1016/_j.jvb.2008.12.004 [DOI] [Google Scholar]
- D’Lima GM, Pearson MR, & Kelley ML (2012). Protective behavioral strategies as a mediator and moderator of the relationship between self-regulation and alcohol-related consequences in first-year college students. Psychology of Addictive Behaviors, 26(2), 330–337. 10.1037/a0026942 [DOI] [PubMed] [Google Scholar]
- Daughters SB, Magidson JF, Lejuez CW, & Chen Y (2016). LETS ACT: A behavioral activation treatment for substance use and depression. Journal of Dual Diagnosis, 9(2/3), 74–84. [Google Scholar]
- Dennhardt AA, & Murphy JG (2011). Associations between depression, distress tolerance, delay discounting, and alcohol-related problems in European American and African American college students. Psychology of Addictive Behaviors, 25(4), 595–604. 10.1037/a0025807 [DOI] [PubMed] [Google Scholar]
- Dvorak RD, Simons JS, & Wray TB (2015). Alcohol Use and Problem Severity: Associations With Dual Systems of Self-Control*. Journal of Studies on Alcohol and Drugs. 10.15288/jsad.2011.72.678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finn PR, Justus A, Mazas C, & Steinmetz JE (1999). Working memory, executive processes and the effects of alcohol on Go/No- Go learning: Testing a model of behavioral regulation and impulsivity. Psychopharmacology, 146(4), 465–472. 10.1007/PL00005492 [DOI] [PubMed] [Google Scholar]
- Garnefski N, & Kraaij V (2006). Relationships between cognitive emotion regulation strategies and depressive symptoms: A comparative study of five specific samples. Personality and Individual Differences, 40(8), 1659–1669. https://doi.org/10.1016Zj.paid.2005.12.009 [Google Scholar]
- Hingson RW, Zha W, & Smyth D (2017). Magnitude and Trends in Heavy Episodic Drinking, Alcohol-Impaired Driving, and Alcohol-Related Mortality and Overdose Hospitalizations Among Emerging Adults of College Ages 18 – 24 in the United States, 1998–2014. Journal of Studies on Alcohol and Drugs, 78, 540–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Hume D, Norton DF, & Norton MJ (2005). A treatise of human nature. Oxford philosophical texts series. 10.2307/2216614 [DOI] [Google Scholar]
- Hustad JTP, Carey KB, Carey MP, & Maisto SA (2009). Self-Regulation, Alcohol Consumption, and Consequences in College Student Heavy Drinkers : A Simultaneous Latent Growth Analysis. Journal of Studies on Alcohol and Drugs, 70, 373–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joormann J, & Gotlib IH (2010). Emotion regulation in depression: Relation to cognitive inhibition, 24(2), 281–298. 10.1080/02699930903407948.Emotion [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney SR, Anderson BJ, & Stein MD (2018). Drinking to cope mediates the relationship between depression and alcohol risk: Different pathways for college and non-college young adults. Addictive Behaviors, SO(January), 116–123. 10.1016/_j.addbeh.2018.01.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney SR, Merrill JE, & Barnett NP (2017). Effects of depressive symptoms and coping motives on naturalistic trends in negative and positive alcohol-related consequences. Addictive Behaviors, 64, 129–136. 10.1016/_j.addbeh.2016.08.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr S, Johnson VK, Gans SE, Krumrine J, Johnson VK, & Gans SE (2004). Predicting Adjustment During the Transition to College: Alexithymia, Perceived Stress, and Psychological Symptoms, 45(6), 593–611. 10.1353/csd.2004.0068 [DOI] [Google Scholar]
- Khantzian EJ (1997). The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry, 4(5), 231–244. 10.3109/10673229709030550 [DOI] [PubMed] [Google Scholar]
- Kline RB (2016). Principles and Practice of Structural Equation Modeling (Fourth). New York: The Guilford Press. [Google Scholar]
- Kroenke CD, Rohlfing T, Park B, Sullivan EV, Pfefferbaum A, & Grant KA (2014). Monkeys that voluntarily and chronically drink alcohol damage their brains: A longitudinal MRI study. Neuropsychopharmacology, 39(4), 823–830. 10.1038/npp.2013.259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuvaas NJ, Dvorak RD, Pearson MR, Lamis DA, & Sargent EM (2014). Selfregulation and alcohol use involvement: A latent class analysis. Addictive Behaviors, 39(1), 146–152. https://doi.org/10.10167j.addbeh.2013.09.020.Self-regulation [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lembke A (2012). Time to Abandon the Self-Medication Hypothesis in Patients with Psychiatric Disorders. The American Journal of Drug and Alcohol Abuse, 38(6), 524–529. 10.3109/00952990.2012.694532 [DOI] [PubMed] [Google Scholar]
- Leventhal AM, Bello MS, Unger JB, Strong DR, Kirkpatrick MG, & Audrain- McGovern JE (2015). Diminished Alternative Reinforcement as a Mechanism Underlying Socioeconomic Disparities in Adolescent Substance Use. Preventative Medicine, 80, 75–81. https://doi.org/10.1016Zj.ypmed.2015.05.021.Diminished [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy M (2018). The Many Faces (and Potential Dangers) of Self-Medication as an Explanatory Concept for Substance Use. International Journal for the Advancement of Counselling, 1–10. 10.1007/s10447-018-9341-3 [DOI] [Google Scholar]
- Lewinsohn PM, Sullivan JM, & Grosscup, Sally J (1980). Changing reinforcing events: An approach to the treatment of depression. Psychotherapy: Theory, Research, & Practice, 77(3), 322–334. [Google Scholar]
- Lovibond PF, & Lovibond SH (1995). The Structure of Negative Emotional States: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behavioral Research and Therapy, 33(3), 335–343. [DOI] [PubMed] [Google Scholar]
- Magar ECE, Phillips LH, & Hosie JA (2008). Self-regulation and risk-taking. Personality and Individual Differences, 45(2), 153–159. 10.1016/j.paid.2008.03.014 [DOI] [Google Scholar]
- Morosanova VI, Fomina TG, Kovas Y, & Bogdanova OY (2016). Cognitive and regulatory characteristics and mathematical performance in high school students. Personality and Individual Differences. 10.1016/j.paid.2015.10.034 [DOI] [Google Scholar]
- Murphy JG, Dennhardt AA, Martens MP, Borsari BE, Witkiewitz K, & Meshesha LZ (2019). A randomized clinical trial evaluating the efficacy of a brief alcohol intervention supplemented with a substance-free activity session or relaxation training. Journal of Consulting and Clinical Psychology. 10.1037/ccp0000412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Skidmore JR, Borsari BE, Barnett NP, Colby SM, & Martens MP (2012). A randomized controlled trial of a behavioral economic supplement to brief motivational interventions for college drinking. Journal of Consulting and Clinical Psychology, 80(5), 876–886. 10.1037/a0028763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L, & Muthén BO (2015). Mplus. Seventh edition Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Neal DJ, & Carey KB (2005). A follow-up psychometric nalysis of the self-regulation questionniare. Psychology of Addictive Behaviors, 19(4), 414–422. 10.1007/s00198-018-4526-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neal DJ, & Carey KB (2007). Association between alcohol intoxication and alcohol-related problems: An event-level analysis. Psychology of Addictive Behaviors, 21(2), 194–204. 10.1037/0893-164X.2L2.194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, & Corte C (2004). Gender and self-regulation In Baumeister RF & Vohs KD (Eds.), Handbook of self-regulation: Research, theory, and applications (pp. 411–421). New York, NY: Guilford Press. [Google Scholar]
- Pauley PM, & Hesse C (2009). The Effects of Social Support, Depression, and Stress on Drinking Behaviors in a College Student Sample. Communication Studies, 60(5), 493–508. 10.1080/10510970903260335 [DOI] [Google Scholar]
- Pearson MR, D’Lima GM, & Kelley ML (2013). Daily use of protective behavioral strategies and alcohol-related outcomes among college students. Psychology of Addictive Behaviors, 27(3), 826–831. 10.1037/a0032516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson MR, Kite BA, & Henson JM (2013). Predictive effects of good self-control and poor regulation on alcohol-related outcomes: do protective behavioral strategies mediate? Psychology of Addictive Behaviors, 27(1), 81–89. 10.1037/a0028818\r2012-14757-001[pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedrelli P, Shapero B, Archibald A, & Dale C (2016). Alcohol use and depression during adolescence and young adulthood: a summary and interpretation of mixed findings. Current Addiction Reports, 3(1), 91–97. 10.1007/s40429-016-0084-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitel AL, Segobin SH, Ritz L, Eustache F, & Beaunieux H (2015). Thalamic abnormalities are a cardinal feature of alcohol-related brain dysfunction. Neuroscience and BiobehavioralReviews, 54, 38–45. 10.1016/_j.neubiorev.2014.07.023 [DOI] [PubMed] [Google Scholar]
- Prince MA, Read JP, & Colder CR (2019). Trajectories of college alcohol involvement and their associations with later alcohol use disorder symptoms. Prevention Science. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn PD, & Fromme K (2010). Self-Regulation as a Protective Factor Against Risky Drinking and Sexual Behavior. Psychology of Addictive Behaviors, 24(3), 376–385. 10.1037/a0018547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Kahler CW, Strong DR, & Colder CR (2006). Development and preliminary validation of the young adult alcohol consequences questionnaire. Journal of Studies on Alcohol, 67(1), 169–177. 10.15288/jsa.2006.67.169 [DOI] [PubMed] [Google Scholar]
- Richardson M, Abraham C, & Bond R (2012). Psychological correlates of university students’ academic performance: A systematic review and meta-analysis. Psychological Bulletin. 10.1037/a0026838 [DOI] [PubMed] [Google Scholar]
- Roberts SJ, Glod CA, Kim R, & Hounchell J (2010). Relationships between aggression, depression, and alcohol, tobacco: Implications for healthcare providers in student health. Journal of the American Academy of Nurse Practitioners, 22(7), 369–375. 10.1111/j.1745-7599.2010.00521.x [DOI] [PubMed] [Google Scholar]
- Roos CR, & Witkiewitz K (2017). A contextual model of self-regulation change mechanisms among individuals with addictive disorders. Clinical Psychology Review. https://doi.org/10.1016Zj.cpr.2017.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal R, & Rosnow RL (2008). Essentials of Behavioral Research: Methods and Data Analysis McGraw-Hill Series in Psychology (3rd ed.). New York, NY: : McGraw Hill; [Google Scholar]
- Sacks JJ, Gonzales KR, Bouchery EE, Tomedi LE, & Brewer RD (2015). 2010 National and State Costs of Excessive Alcohol Consumption. American Journal of Preventive Medicine, 49(5), e73–e79. 10.1016/j.amepre.2015.05.031 [DOI] [PubMed] [Google Scholar]
- Satorra A (2000). Scaled and Adjusted Restricted Tests in Multi-Sample Analysis of Moment Structures BT - Innovations in Multivariate Statistical Analysis. In Innovations in Multivariate Statistical Analysis. 10.1007/978-1-4615-4603-0 [DOI] [Google Scholar]
- Singleton RA, & Wolfson AR (2009). Alcohol consumption, sleep, and academic performance among college students. Journal of Studies on Alcohol and Drugs, 70(3), 355–363. 10.15288/jsad.2009.70.355 [DOI] [PubMed] [Google Scholar]
- Soltis KE, Acuff SF, Dennhardt AA, Borsari BE, Martens MP, & Murphy JG (2018). Self-regulation as a mediator of the effects of a brief behavioral economic intervention on alcohol related outcomes: A preliminary analysis. Experimental and Clinical Psychopharmacology, 26(4), 347–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soltis KE, McDevitt-Murphy ME, & Murphy JG (2017). Alcohol demand, future orientation, and craving mediate the relation between depressive and stress symptoms and alcohol problems. Alcoholism: Clinical and Experimental Research, 41(6), 1191–1200. 10.1111/acer.13395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauman TJ (2002). Self-Regulation and Depression. Self and Identity, 1(2), 151–157. 10.1080/152988602317319339 [DOI] [Google Scholar]
- Strauman TJ (2017). Self-Regulation and Psychopathology : Toward an Integrative Translational Research Paradigm, (December). 10.1146/annurev-clinpsy-032816-045012 [DOI] [PubMed] [Google Scholar]
- Sudhinaraset M, Wigglesworth C, & Takeuchi DT (2015). Social and cultural contexts of alcohol use: Influences in a social-ecological framework. Alcohol Research: Current Reviews. https://doi.org/10.1016Zj.foodhyd.2016.07.022 [PMC free article] [PubMed] [Google Scholar]
- Tabachnick BG, & Fidell LS (2013). Using multivariate statistics (6th ed.). Boston, MA: Pearson. [Google Scholar]
- Tapper EB, & Parikh ND (2018). Mortality due to cirrhosis and liver cancer in the United States, 1999–2016: observational study. BMJ, 362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tripp JC, Mcdevitt-Murphy ME, Avery ML, & Bracken KL (2015). PTSD Symptoms, Emotion Dysregulation, and Alcohol-Related Consequences Among College Students With a Trauma History. Journal of Dual Diagnosis, 11(2), 107–117. 10.1080/15504263.2015.1025013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vujanovic AA, Wardle MC, Smith LJ, & Berenz EC (2016). Reward Functioning in Posttraumatic Stress and Substance Use Disorders. Current Opinion in Psychology, 49–55. 10.1016/j.copsyc.2016.11.004 [DOI] [PubMed] [Google Scholar]
- Werner C, & Schermelleh-Engel K (2010). Deciding Between Competing Models: Chi-Square Difference Tests. Introduction to Structural Equation Modeling with LISREL. [Google Scholar]
- White AM, & Hingson RW (2013). The burden of alcohol use: Excessive alcohol consumption and related consequences among college students. Alcohol Research: Current Reviews, 35(2), 201–218. 10.1136/emermed-2015-205295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan KH, & Bentler PM (1998). Structural Equation Modeling with Robust Covariances. Sociological Methodology, 28(1), 363–396. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


