Abstract
The ovarian reserve is necessary for female fertility and endocrine health. Commonly used cancer therapies diminish the ovarian reserve, thus, resulting in primary ovarian insufficiency, which clinically presents as infertility and endocrine dysfunction. Prepubertal children who have undergone cancer therapies often experience delayed puberty or cannot initiate puberty and require endocrine support to maintain a normal life. Thus, developing an effective intervention to prevent loss of the ovarian reserve is an unmet need for these cancer patients. The selection of adjuvant therapies to protect the ovarian reserve against cancer therapies underlies the mechanism of loss of primordial follicles (PFs). Several theories have been proposed to explain the loss of PFs. The “burn out” theory postulates that chemotherapeutic agents activate dormant PFs through an activation pathway. Another theory posits that chemotherapeutic agents destroy PFs through an “apoptotic pathway” due to high sensitivity to DNA damage. However, the mechanisms causing loss of the ovarian reserve remains largely speculative. Here, we review current literature in this area and consider the mechanisms of how gonadotoxic therapies deplete PFs in the ovarian reserve.
Keywords: Ovarian follicle, Primary ovarian insufficiency, Fertility, Fertility preservation
Introduction
The ovary is the main female organ that produces critical endocrine steroid hormones such as estrogen and progesterone. These endocrine hormones regulate the development of female sexual characteristics such as timing of reproductive cycles, breast development, and staging the uterus for successful pregnancy.
The ovary is also responsible for the development of mature oocytes capable of fertilization. The number of oocytes present in the ovaries at birth does not increase and determines the female reproductive lifespan [1]. At birth, approximately 1 million oocytes are present in women and approximately 10,000 are present in female mice [2]. The number of oocytes decreases during the development of female gonads and only approximately 400,000 oocytes remain at the puberty. Oocytes in the ovary become arrested in the dictyate stage of prophase in meiosis I before female is born [3]. When a woman's menstrual cycle starts and luteinizing hormone (LH) surge occurs, oocytes that have been arrested in prophase in the ovary enter meiotic resumption [4].
The oocyte is surrounded by pre-granulosa/granulosa cells, which together form the follicle as a functional unit in the ovary [5,6]. The smallest follicles are called primordial follicles (PFs) and their oocytes are surrounded with squamous pre-granulosa cells. They remain dormant inside the ovary until they receive activation signals which recruit them into the growing follicle pool.
Consequences of cancer therapy on ovarian follicles
Cancer therapy is like a 2-sided coin. It often causes many side effects in other organs including the risk of loss of ovarian follicles, while it increases the survival rate in the cancer patients [7,8,9]. As the ovarian follicles are the most sensitive cells, the exposure to the gonadotoxic agents such as chemotherapeutic agents, ionizing radiation, or environmental toxins consequently induce DNA damage and apoptosis in follicles. Thus, gonadotoxic agents eventually reduce the number of ovarian follicles, resulting in primary ovarian insufficiency in females [10]. Even though the follicles might survive the detrimental effects of gonadotoxic agents, the exposure can trigger genomic mutations in surviving follicles, potentially resulting in intergenerational effects [11].
Currently, there are options available for saving the ovarian follicles in cancer patients, which is dependent on their status [12]. Although ovarian tissue freezing is currently used as an option for future fertility for adult women and young girls before puberty, this procedure is not sufficient for long term maintenance of the endocrine system following the removal of the ovaries or depletion of the ovarian reserve [13]. Thus, proposed pharmacological approaches to prevent gonadotoxicity (Table 1) may be beneficial for prepubertal girls as they can protect ovarian follicles without surgery or delayed cancer therapy. However, a thorough understanding of the mechanism of ovarian follicle death by various cancer therapeutic agents is needed to prevent ovotoxicity and preserve fertility.
Table 1. The proposed mechanism of loss of primordial follicles (PFs) induced by chemotherapeutic agents and environmental toxins as well as the suggested fertoprotective adjuvants.
| Proposed mechanism of loss of PFs | Proposed adjuvants | |
|---|---|---|
| Activation | Direct | AS101 [26], everolimus (RAD001) [27], INK128 [27], melatonin [29], ghrelin [29] |
| Indirect | AMH [31] | |
| Apoptosis | Direct | GnRH agonists [40,41], GnRH antagonist [42], LH [46], ATM/ATR inhibitor [21], CHEK2 inhibitor [19,24], and CK1 inhibitor [18], imatinib [48] |
| Indirect | S1P [51,61], ceramide-1-Phosphate [52], zingerone [53], proanthocyanidin [54], gallic acid [55], mangafodipir [56], resveratrol [57], curcumin [58], capsaicin [58], erythropoietin [62], G-CSF [63], tamoxifen [64], dexrazoxane [65,66,67] | |
AMH, anti-Müllerian hormone; GnRH, gonadotropin-releasing hormone; LH, luteinizing hormone; ATM, ataxia-telangiectasia mutated; ATR, ataxia telangiectasia and Rad3-related; CHEK2, checkpoint kinase 2; CK1, casein kinase 1; S1P, sphingosine-1-phosphate; G-CSF, granulocyte-colony stimulating factor.
Role of TAp63α in follicle death and molecular targets to limit TAp63α action
Oocytes from dormant primordial to early secondary follicle highly express tumor protein p63, TAp63α, an oocyte-specific isoform of p63 [14,15]. TAp63α exists in the nucleus of oocyte as an inactive dimer in postnatal healthy oocytes and controls the fate of small follicles in the ovary [16]. However, DNA damage in oocytes induces the phosphorylation of TAp63α, leading to a conformational switch from an inactive dimer to an active tetrameric structure. This tetramer triggers apoptotic pathways through PUMA (BCL2 binding component 3; BBC3) and NOXA (phorbol-12-myristate-13-acetate-induced protein 1; PMAIP1) resulting in oocyte death [17]. Molecules upstream of TAp63α initiate the phosphorylation of TAp63α to make the tetrameric structure. Checkpoint kinase 2 (CHEK2) is an initiating kinase that phosphorylates dimeric TAp63α and recruits casein kinase 1 (CK1) to completely phosphorylate the primed TAp63α [18,19,20]. The actions of CHEK2 and CK1 promote the formation of TAp63α tetramers, which are kinetically stable and irreversibly activate the apoptotic pathway. The chemotherapeutic agents, cisplatin and doxorubicin, have been shown to phosphorylate TAp63α. Thus, inhibitors of CHEK2 (BML-277 or CHEK2 inhibitor II hydrate) or CK1 (PF670462) block the tetramerization of TAp63α induced by cisplatin and doxorubicin and protect the ovarian reserve [18,19]. Recent reports show that the use of CHEK2 inhibitors also protects the ovarian reserve from ionizing radiation [19,21], suggesting that inhibition of TAp63α tetramerization through pharmacological intervention is a valuable approach to protect the ovarian reserve. These studies are based on understanding the mechanism of oocyte death by the treatment of gonadotoxic cancer therapies.
Loss of primordial follicles
Gonadotoxic therapies deplete PFs in the ovarian reserve. There are two prevailing theories regarding the effect of chemotherapeutic agents on the oocytes of dormant PFs (Table 1). The activation or burnout theory suggests that the chemotherapeutic agents activate dormant PFs into the growing follicle pool and proposes the use of inhibitors against the phosphatidylinositol-3-kinase (PI3K)/protein kinase B (AKT)/mammalian target of rapamycin (mTOR) pathway as an approach to preserve ovarian follicles from chemotherapeutic agents. In contrast, the inactivation or apoptosis theory suggests that chemotherapeutic agents directly destroy the oocytes of dormant PFs through activation of TAp63α and initiation of apoptosis. Thus, further investigation is required to identify and confirm the mechanisms by which chemotherapeutic agents induce death or activation of oocytes in dormant PFs. In order to effectively prevent the loss of oocytes, studies are needed to determine the specific cellular pathways that lead to oocyte/follicle loss based on the type and dose of chemotherapeutic agent as well as the duration of therapy.
Consequences of chemotherapeutic agents on oocytes of dormant primordial follicles: activation or apoptosis?
Intensive research has been conducted in the past decade to better understand how best to protect the ovarian germ cells from gonadotoxic agents such as chemotherapeutic agents or environmental toxins. However, it is unclear how ovarian germ cells die from chemotherapeutic agent insults and which approaches provide the best protection of the germ cells. Thus, this review revisits the current literature with a view towards unveiling the cytotoxic consequences of chemotherapeutic agents on PFs.
Loss of the ovarian reserve: activation
1. Direct activation
Existing literature supports the idea that activation of the PI3K/AKT/mTOR signaling pathway stimulates dormant PFs to enter the pool of growing follicles [22,23,24]. Intriguingly chemotherapeutic agents such as cisplatin and cyclophosphamide are reported to induce PI3K/AKT/mTOR signals in oocytes without promoting the death of oocytes in PFs. Furthermore, Roness et al. [25] and Kalich-Philosoph et al. [26] demonstrated that cyclophosphamide induces PI3K/AKT/mTOR signals in the oocyte of the mouse ovary, causing the initiation of recruitment and growth of all dormant PFs (direct activation). This eventually results in the depletion of the ovarian reserve, and has been labeled as the follicle ‘burnout’ theory. Cyclophosphamide also induces death of growing follicles through apoptosis in granulosa cells, which results in a decrease of Anti-Müllerian hormone (AMH) and paradoxically results in the recruitment of dormant PFs into a cohort of growing follicles (indirect activation). Accordingly, AS101, an immunomodulator, decreased PI3K/AKT/mTOR signaling and eventually prevented the decline of follicles by follicle activation and loss from the treatment of cyclophosphamide. This study suggested that the dormant follicle activation through PI3K/AKT/mTOR signaling is a new mechanism of ovotoxicity underlying the loss of follicles induced by chemotherapeutic agents and environmental carcinogens. Thus, agents that suppress PI3K signaling, such as AS101, may be ideal adjuvants to preserve viability and numbers of dormant PFs when patients are treated with ovotoxins.
A study conducted by Goldman et al. [27] in 8-week-old C57BL/6J female mice supports the findings that cyclophosphamide promotes follicle activation through PI3K/AKT/mTOR signaling. In this report the ooplasm of dormant PFs highly expressed the downstream markers of mTOR signaling after the treatment with cyclophosphamide. Correspondingly, treatment with the mTORC1/2 inhibitors, everolimus (RAD001) or INK128, preserved the ovarian reserve and serum AMH levels. As a consequence, the mTOR inhibitors extended the fertility span in mice treated with cyclophosphamide.
A recent in vitro study by Lande et al. [28] that examined PFs in human ovarian tissues supports the activation theory. These investigators observed a statistically significant increase in the number of growing follicles in the human ovarian tissues following the treatment with high concentrations of 4-hydroperoxy cyclophosphamide (4-HC) or phosphamide mustard, which are cyclophosphamide metabolites, as compared with untreated ovarian tissues. Although there was no proposed mechanism in this report, the results correlate with others showing more developing follicles after the treatment with cyclophosphamide as compared to the untreated controls [26].
Jang et al. [29] supported the concept that cisplatin activates the PI3K/AKT/mTOR signaling pathway and stimulates dormant PFs. This study also provided evidence for melatonin and ghrelin being fertoprotective against cisplatin-induced ovarian damage by decreasing PI3K signaling. In the ovary, dormant PFs highly express Forkhead box O3a (FOXO3a) in the nuclei of oocytes [30]. A wave of follicle activation signals initiates PI3K/AKT signaling resulting in the phosphorylation of FOXO3a inside the oocyte nucleus. Phosphorylated FOXO3a shuttles out of the nucleus, stimulating activation of dormant PFs and converting the squamous pregranulosa cells into cuboidal granulosa cells (direct activation). In this report, the authors demonstrated that the treatment of mice with low doses of cisplatin (2.5 mg/kg) for 12 days activated dormant PFs through phosphorylation of FOXO3a. They also found that the treatment with melatonin and ghrelin synergistically suppressed the phosphorylation of FOXO3a by cisplatin and retained FOXO3a in the nucleus of oocytes of PFs. They further showed that the ovarian follicles express receptors for melatonin (MT1 and MT2) and ghrelin (GHSR1) in PFs [29]. These findings suggest that the dormant PFs may be protected from ovotoxins like cisplatin through high nuclear expression of FOXO3a. Furthermore, the combination of melatonin and ghrelin may serve as ovoprotectants/fertoprotectants to mitigate the adverse effects of cisplatin treatment.
2. Indirect activation
The indirect activation concept for loss of the ovarian reserve was recently highlighted by Kano et al. [31] demonstrating that AMH/Müllerian inhibiting substance (MIS) produced by granulosa cells protects the ovarian reserve from chemotherapeutic agents like carboplatin, doxorubicin or cyclophosphamide [32]. AMH/MIS plays an important role in the development of male and female gonads and the differentiation of the urogenital ridge. In females, AMH/MIS is mainly produced by granulosa cells from primary to medium sized antral follicles [33] and thus it is considered by the fertility clinics to be a biomarker for the ovarian reserve [34,35,36,37]. It serves an important role as a negative regulator of PF activation [38,39]. The study by Kano et al. [31] demonstrated that co-treatment of AMH/MIS with chemotherapeutic agents protects PFs through suppression of PFs. According to this concept, chemotherapeutic agents destroy the growing follicles and thus reduce the production of AMH/MIS from them. Consequently, the lack of AMH/MIS production removes the suppressive effects allowing the PFs to be recruited into the pool of growing follicles (indirect activation). They also demonstrated that the treatment of AMH/MIS is reversible, showing that the cessation of treatment allows dormant PFs to resume ovarian folliculogenesis. Thus, co-treatment of AMH/MIS with chemotherapeutic agents is a therapeutic option for protecting the ovarian reserve.
Loss of the ovarian reserve: apoptosis
1. Direct apoptosis
Gonadotropin-releasing hormone (GnRH) agonists/antagonists are clinically used as ovoprotectants/fertoprotectants [40,41,42]. Several reports show that the loss of ovarian cyclicity is prevented by co-treatment of GnRH agonist/antagonists with chemotherapeutic agents as compared with the chemotherapeutic agents alone [43]. Although the use of GnRH agonist has been promising, its usefulness has been debated due to the inconsistency of results in protection of ovarian follicles [12,44]. A proposed mechanism indicates an increase in cAMP levels by GnRH agonist in oocytes leading to the suppression of oocyte apoptosis, although this finding was not confirmed in studies using mice and human [45]. This is thought to occur as a result of the passage of cAMP between oocytes and granulosa cells through gap junctions, eventually resulting in the survival of the ovarian follicles. The critical role of cAMP in ovoprotection is also supported by studies showing that treatment with LH provides protection against cisplatin. Research from Dr. Klinger's group showed that LH protects oocytes against cisplatin through the activation of the LH/choriogonadotropin receptor in ovarian cells [46]. In postnatal day 8 and adult mouse ovary, the LHCGR is expressed in cells surrounding follicles. Accordingly, exogenous 8-Bromo-cAMP and forskolin, factors mimicking the signaling pathway activated by LH, protect the ovarian follicles against cisplatin and initiate DNA repair kinetics in oocytes. Furthermore, LH stimulated the expression of KIT-ligand (Stem cell factor, SCF, KL, steel factor) and KIT (receptor), and protected oocytes against cisplatin-induced death in, both, oocytes and granulosa cells of the ovarian tissues in vitro. They proposed that protein kinase A activity, downstream of KL/KIT, protects oocytes from ovotoxicity by cisplatin followed by the activation of PI3K/AKT pathway to promote oocyte survival. However, it is not known whether the activation of PI3K/AKT pathway induced by LH treatment is necessary for protecting oocytes in PFs; in the case that it is needed, it must be on the level of threshold to promote oocyte survival.
Recent studies from our laboratory indicate that the chemotherapeutic agents directly destroy oocytes of dormant PFs and supports the inactivation concept. In support of the notion, cyclophosphamide treatment in three different mouse strains (C57BL/6J, CD-1 and BALB/cJ) did not promote any increase in the total number of primary and secondary follicles [47]. Our findings showed that the oocytes within the PFs are the most sensitive cells to DNA damage induced by cyclophosphamide treatment; this is in accordance with the previous data with cisplatin and X-rays [16]. Accordingly, oocytes of PFs were destroyed prior to damage to other ovarian cells without the activation of oocytes of dormant PFs, preserving the quiescent pregranulosa cells surrounding the oocytes of PFs. However, granulosa cells in growing follicles were also damaged. In addition, our results showed that the damaged granulosa cells are replaced within 3 days, if the follicles keep a portion of healthy granulosa cells, supported by proliferation of Ki67 markers and a subsequent increase in AMH production [47]. This suggests that the elevation of AMH does not represent the recruitment of dormant follicles into the pool of growing follicles. Furthermore, we found that the oocytes within the PFs presented temporal expression of phosphorylated-AKT as well as considerably prolonged expression of cleaved poly (ADP-ribose) polymerase (PARP) inside of the same PFs upon the treatment with cyclophosphamide or 4-HC, the active metabolite of cyclophosphamide in vivo. Moreover, cyclophosphamide induced time-dependent increases in apoptosis of oocytes of PFs as was evident by elevated expression of BAX and cleaved PARP. The oocytes expressed additional markers of apoptosis including γH2AX and phosphorylated TAp63α. Additional studies have demonstrated that cyclophosphamide-induced damage in oocytes of dormant PFs occurs via the p-ataxia telangiectasia and Rad3-related (ATR)>p-CHEK1/p-CHEK2>p-p63 apoptotic pathway [47], while cisplatin induces the p-ATR>p-CHEK2>p63/p73>PUMA/NOXA apoptotic pathway [17,21,48]. The apoptotic pathway induced by cyclophosphamide eventually leads to the formation of TAp63α tetramers in the nucleus of oocytes, resulting in the induction of an irreversible apoptotic pathway. As shown in another report, ataxia-telangiectasia mutated (ATM), CHEK2, and CK1 inhibitors inhibit the tetramerization of TAp63α induced by cisplatin and doxorubicin [18], suggesting that the apoptotic inhibitors can block oocyte death at the molecular level [21,48,49]. This suggests that PFs are destined to die rather than activate upon cyclophosphamide treatment, even though oocytes in PFs temporally present phosphorylated-AKT signals in response to chemotherapeutic agents. We assume that those follicles may contain genomic mutations or damaged DNA if the follicles with both the signals manage to survive. Taken together, these findings suggest that the apoptotic inhibitors instead of inhibitors of PI3K pathway should be used to protect dormant PFs from ovotoxins such as cisplatin, cyclophosphamide and X-ray [16,21,47].
2. Indirect apoptosis by reactive oxygen species
Oxidative stress affects reproductive health in females through the production of reactive oxygen species (ROS). Although ROS play an important role in signal transduction during folliculogenesis, oocyte maturation, and embryogenesis [50], excessive ROS can induce damage to the ovary through the induction of granulosa cell death [51], follicle atresia or oocyte damage. In addition, it adversely affects the production of ovarian hormones and mature oocytes from healthy follicles. Of relevance to the preservation of fertility, reports suggest that the antioxidants such as S1P [51], ceramide-1-phosphate [52], zingerone [53], proanthocyanidin [54], gallic acid [55], mangafodipir [56], resveratrol [57], curcumin [58], and capsaicin [58] protect the ovary from ovotoxins including chemotherapeutic agents. Thus, oxidative stress-induced damage can be prevented by antioxidants through attenuating the free radical induced ovarian damages. However, there are only few reports that show direct evidences of ROS in oocytes of PFs. Thus, the effect of ROS on mitochondria in oocytes or granulosa cells should be further investigated [59,60].
Conclusion
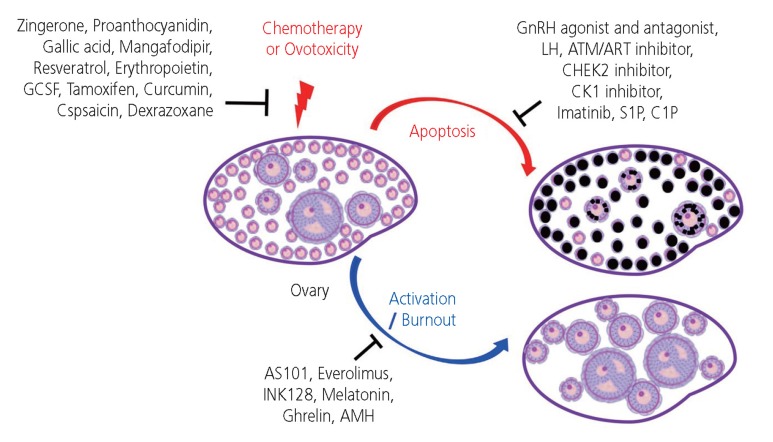
Understanding the exact mechanisms responsible for the disruption of the ovarian reserve induced by different classes of chemotherapeutic agents and environmental ovotoxins will allow for a rational approach to identify drug targets that protect oocytes and germ line integrity, select specific adjuvants and protect the ovarian reserve following cancer treatments (Fig. 1).
Fig. 1.
Mechanism of primordial follicle (PF) loss by chemotherapeutics and ovotoxicity along with proposed fertoprotective agents to maintain the ovarian reserve. PFs consist of oocytes and squamous pregranulosa cells, while growing follicles are surrounded by cuboidal granulosa cells in the ovary. Fertoprotective agents have been proposed against the cytotoxic consequences of chemotherapeutic agents or ovotoxicity on PFs.
G-CSF, granulocyte-colony stimulating factor; GnRH, gonadotropin-releasing hormone; LH, luteinizing hormone; ATM, ataxia-telangiectasia mutated; ATR, ataxia telangiectasia and Rad3-related; CHEK2, checkpoint kinase 2; CK1, casein kinase 1; S1P, sphingosine-1-phosphate; C1P, ceramide-1-phosphate; AMH, anti-Müllerian hormone.
Footnotes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
Ethical approval: The study is not applicable to Institutional Review Board (IRB).
Patient consent: There is no need for patient consent in this review article.
References
- 1.Wilkosz P, Greggains GD, Tanbo TG, Fedorcsak P. Female reproductive decline is determined by remaining ovarian reserve and age. PLoS One. 2014;9:e108343. doi: 10.1371/journal.pone.0108343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Findlay JK, Hutt KJ, Hickey M, Anderson RA. How is the number of primordial follicles in the ovarian reserve established? Biol Reprod. 2015;93:111. doi: 10.1095/biolreprod.115.133652. [DOI] [PubMed] [Google Scholar]
- 3.Eppig JJ. Coordination of nuclear and cytoplasmic oocyte maturation in eutherian mammals. Reprod Fertil Dev. 1996;8:485–489. doi: 10.1071/rd9960485. [DOI] [PubMed] [Google Scholar]
- 4.Sen A, Caiazza F. Oocyte maturation: a story of arrest and release. Front Biosci (Schol Ed) 2013;5:451–477. doi: 10.2741/s383. [DOI] [PubMed] [Google Scholar]
- 5.Picton HM. Activation of follicle development: the primordial follicle. Theriogenology. 2001;55:1193–1210. doi: 10.1016/s0093-691x(01)00478-2. [DOI] [PubMed] [Google Scholar]
- 6.Pepling ME. Follicular assembly: mechanisms of action. Reproduction. 2012;143:139–149. doi: 10.1530/REP-11-0299. [DOI] [PubMed] [Google Scholar]
- 7.Rose SR, Horne VE, Howell J, Lawson SA, Rutter MM, Trotman GE, et al. Late endocrine effects of childhood cancer. Nat Rev Endocrinol. 2016;12:319–336. doi: 10.1038/nrendo.2016.45. [DOI] [PubMed] [Google Scholar]
- 8.Chemaitilly W, Sklar CA. Childhood cancer treatments and associated endocrine late effects: a concise guide for the pediatric endocrinologist. Horm Res Paediatr. 2019;91:74–82. doi: 10.1159/000493943. [DOI] [PubMed] [Google Scholar]
- 9.Livinalli A, Silva MT, Lopes LC. Late adverse effects related to treatment in a cohort of survivors of childhood and adolescent cancer. Medicine (Baltimore) 2019;98:e14921. doi: 10.1097/MD.0000000000014921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bedoschi G, Navarro PA, Oktay K. Chemotherapy-induced damage to ovary: mechanisms and clinical impact. Future Oncol. 2016;12:2333–2344. doi: 10.2217/fon-2016-0176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Madanat-Harjuoja LM, Malila N, Lähteenmäki P, Pukkala E, Mulvihill JJ, Boice JD, Jr, et al. Risk of cancer among children of cancer patients - a nationwide study in Finland. Int J Cancer. 2010;126:1196–1205. doi: 10.1002/ijc.24856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim SY, Kim SK, Lee JR, Woodruff TK. Toward precision medicine for preserving fertility in cancer patients: existing and emerging fertility preservation options for women. J Gynecol Oncol. 2016;27:e22. doi: 10.3802/jgo.2016.27.e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jeruss JS, Woodruff TK. Preservation of fertility in patients with cancer. N Engl J Med. 2009;360:902–911. doi: 10.1056/NEJMra0801454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suh EK, Yang A, Kettenbach A, Bamberger C, Michaelis AH, Zhu Z, et al. p63 protects the female germ line during meiotic arrest. Nature. 2006;444:624–628. doi: 10.1038/nature05337. [DOI] [PubMed] [Google Scholar]
- 15.Livera G, Petre-Lazar B, Guerquin MJ, Trautmann E, Coffigny H, Habert R. p63 null mutation protects mouse oocytes from radio-induced apoptosis. Reproduction. 2008;135:3–12. doi: 10.1530/REP-07-0054. [DOI] [PubMed] [Google Scholar]
- 16.Kim SY, Cordeiro MH, Serna VA, Ebbert K, Butler LM, Sinha S, et al. Rescue of platinum-damaged oocytes from programmed cell death through inactivation of the p53 family signaling network. Cell Death Differ. 2013;20:987–997. doi: 10.1038/cdd.2013.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kerr JB, Hutt KJ, Michalak EM, Cook M, Vandenberg CJ, Liew SH, et al. DNA damage-induced primordial follicle oocyte apoptosis and loss of fertility require TAp63-mediated induction of PUMA and NOXA. Mol Cell. 2012;48:343–352. doi: 10.1016/j.molcel.2012.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tuppi M, Kehrloesser S, Coutandin DW, Rossi V, Luh LM, Strubel A, et al. Oocyte DNA damage quality control requires consecutive interplay of CHK2 and CK1 to activate p63. Nat Struct Mol Biol. 2018;25:261–269. doi: 10.1038/s41594-018-0035-7. [DOI] [PubMed] [Google Scholar]
- 19.Rinaldi VD, Hsieh K, Munroe R, Bolcun-Filas E, Schimenti JC. Pharmacological inhibition of the DNA damage checkpoint prevents radiation-induced oocyte death. Genetics. 2017;206:1823–1828. doi: 10.1534/genetics.117.203455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bolcun-Filas E, Rinaldi VD, White ME, Schimenti JC. Reversal of female infertility by Chk2 ablation reveals the oocyte DNA damage checkpoint pathway. Science. 2014;343:533–536. doi: 10.1126/science.1247671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim SY, Nair DM, Romero M, Serna VA, Koleske AJ, Woodruff TK, et al. Transient inhibition of p53 homologs protects ovarian function from two distinct apoptotic pathways triggered by anticancer therapies. Cell Death Differ. 2019;26:502–515. doi: 10.1038/s41418-018-0151-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu K, Rajareddy S, Liu L, Jagarlamudi K, Boman K, Selstam G, et al. Control of mammalian oocyte growth and early follicular development by the oocyte PI3 kinase pathway: new roles for an old timer. Dev Biol. 2006;299:1–11. doi: 10.1016/j.ydbio.2006.07.038. [DOI] [PubMed] [Google Scholar]
- 23.Jagarlamudi K, Liu L, Adhikari D, Reddy P, Idahl A, Ottander U, et al. Oocyte-specific deletion of Pten in mice reveals a stage-specific function of PTEN/PI3K signaling in oocytes in controlling follicular activation. PLoS One. 2009;4:e6186. doi: 10.1371/journal.pone.0006186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zheng W, Nagaraju G, Liu Z, Liu K. Functional roles of the phosphatidylinositol 3-kinases (PI3Ks) signaling in the mammalian ovary. Mol Cell Endocrinol. 2012;356:24–30. doi: 10.1016/j.mce.2011.05.027. [DOI] [PubMed] [Google Scholar]
- 25.Roness H, Gavish Z, Cohen Y, Meirow D. Ovarian follicle burnout: a universal phenomenon? Cell Cycle. 2013;12:3245–3246. doi: 10.4161/cc.26358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kalich-Philosoph L, Roness H, Carmely A, Fishel-Bartal M, Ligumsky H, Paglin S, et al. Cyclophosphamide triggers follicle activation and “burnout”; AS101 prevents follicle loss and preserves fertility. Sci Transl Med. 2013;5:185ra62. doi: 10.1126/scitranslmed.3005402. [DOI] [PubMed] [Google Scholar]
- 27.Goldman KN, Chenette D, Arju R, Duncan FE, Keefe DL, Grifo JA, et al. mTORC1/2 inhibition preserves ovarian function and fertility during genotoxic chemotherapy. Proc Natl Acad Sci U S A. 2017;114:3186–3191. doi: 10.1073/pnas.1617233114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lande Y, Fisch B, Tsur A, Farhi J, Prag-Rosenberg R, Ben-Haroush A, et al. Short-term exposure of human ovarian follicles to cyclophosphamide metabolites seems to promote follicular activation in vitro. Reprod Biomed Online. 2017;34:104–114. doi: 10.1016/j.rbmo.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 29.Jang H, Na Y, Hong K, Lee S, Moon S, Cho M, et al. Synergistic effect of melatonin and ghrelin in preventing cisplatin-induced ovarian damage via regulation of FOXO3a phosphorylation and binding to the p27Kip1 promoter in primordial follicles. J Pineal Res. 2017;63:e12432. doi: 10.1111/jpi.12432. [DOI] [PubMed] [Google Scholar]
- 30.John GB, Gallardo TD, Shirley LJ, Castrillon DH. Foxo3 is a PI3K-dependent molecular switch controlling the initiation of oocyte growth. Dev Biol. 2008;321:197–204. doi: 10.1016/j.ydbio.2008.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kano M, Sosulski AE, Zhang L, Saatcioglu HD, Wang D, Nagykery N, et al. AMH/MIS as a contraceptive that protects the ovarian reserve during chemotherapy. Proc Natl Acad Sci U S A. 2017;114:E1688–97. doi: 10.1073/pnas.1620729114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pépin D, Sabatini ME, Donahoe PK. Müllerian inhibiting substance/anti-Müllerian hormone as a fertility preservation agent. Curr Opin Endocrinol Diabetes Obes. 2018;25:399–405. doi: 10.1097/MED.0000000000000442. [DOI] [PubMed] [Google Scholar]
- 33.Xu J, Xu F, Letaw JH, Park BS, Searles RP, Ferguson BM. Anti-Müllerian hormone is produced heterogeneously in primate preantral follicles and is a potential biomarker for follicle growth and oocyte maturation in vitro. J Assist Reprod Genet. 2016;33:1665–1675. doi: 10.1007/s10815-016-0804-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dewailly D, Andersen CY, Balen A, Broekmans F, Dilaver N, Fanchin R, et al. The physiology and clinical utility of anti-Müllerian hormone in women. Hum Reprod Update. 2014;20:370–385. doi: 10.1093/humupd/dmt062. [DOI] [PubMed] [Google Scholar]
- 35.Josso N, Picard JY, Rey R, di Clemente N. Testicular anti-Müllerian hormone: history, genetics, regulation and clinical applications. Pediatr Endocrinol Rev. 2006;3:347–358. [PubMed] [Google Scholar]
- 36.Josso N, Legeai L, Forest MG, Chaussain JL, Brauner R. An enzyme linked immunoassay for anti-Müllerian hormone: a new tool for the evaluation of testicular function in infants and children. J Clin Endocrinol Metab. 1990;70:23–27. doi: 10.1210/jcem-70-1-23. [DOI] [PubMed] [Google Scholar]
- 37.Hudson PL, Dougas I, Donahoe PK, Cate RL, Epstein J, Pepinsky RB, et al. An immunoassay to detect human Müllerian inhibiting substance in males and females during normal development. J Clin Endocrinol Metab. 1990;70:16–22. doi: 10.1210/jcem-70-1-16. [DOI] [PubMed] [Google Scholar]
- 38.Nilsson EE, Schindler R, Savenkova MI, Skinner MK. Inhibitory actions of anti-Müllerian hormone (AMH) on ovarian primordial follicle assembly. PLoS One. 2011;6:e20087. doi: 10.1371/journal.pone.0020087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang MY, Cushman RA, Fortune JE. Anti-Müllerian hormone inhibits activation and growth of bovine ovarian follicles in vitro and is localized to growing follicles. Mol Hum Reprod. 2017;23:282–291. doi: 10.1093/molehr/gax010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Leonard RCF, Adamson DJA, Bertelli G, Mansi J, Yellowlees A, Dunlop J, et al. GnRH agonist for protection against ovarian toxicity during chemotherapy for early breast cancer: the Anglo Celtic Group OPTION trial. Ann Oncol. 2017;28:1811–1816. doi: 10.1093/annonc/mdx184. [DOI] [PubMed] [Google Scholar]
- 41.Munhoz RR, Pereira AA, Sasse AD, Hoff PM, Traina TA, Hudis CA, et al. Gonadotropin-releasing hormone agonists for ovarian function preservation in premenopausal women undergoing chemotherapy for early-stage breast cancer: a systematic review and meta-analysis. JAMA Oncol. 2016;2:65–73. doi: 10.1001/jamaoncol.2015.3251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Meirow D, Assad G, Dor J, Rabinovici J. The GnRH antagonist cetrorelix reduces cyclophosphamide-induced ovarian follicular destruction in mice. Hum Reprod. 2004;19:1294–1299. doi: 10.1093/humrep/deh257. [DOI] [PubMed] [Google Scholar]
- 43.Ataya K, Rao LV, Lawrence E, Kimmel R. Luteinizing hormone-releasing hormone agonist inhibits cyclophosphamide-induced ovarian follicular depletion in rhesus monkeys. Biol Reprod. 1995;52:365–372. doi: 10.1095/biolreprod52.2.365. [DOI] [PubMed] [Google Scholar]
- 44.Lambertini M, Ceppi M, Poggio F, Peccatori FA, Azim HA, Jr, Ugolini D, et al. Ovarian suppression using luteinizing hormone-releasing hormone agonists during chemotherapy to preserve ovarian function and fertility of breast cancer patients: a meta-analysis of randomized studies. Ann Oncol. 2015;26:2408–2419. doi: 10.1093/annonc/mdv374. [DOI] [PubMed] [Google Scholar]
- 45.Horicks F, Van Den Steen G, Gervy C, Clarke HJ, Demeestere I. Both in vivo FSH depletion and follicular exposure to Gonadotrophin-releasing hormone analogues in vitro are not effective to prevent follicular depletion during chemotherapy in mice. Mol Hum Reprod. 2018;24:221–232. doi: 10.1093/molehr/gay005. [DOI] [PubMed] [Google Scholar]
- 46.Rossi V, Lispi M, Longobardi S, Mattei M, Di Rella F, Salustri A, et al. LH prevents cisplatin-induced apoptosis in oocytes and preserves female fertility in mouse. Cell Death Differ. 2017;24:72–82. doi: 10.1038/cdd.2016.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Luan Y, Edmonds ME, Woodruff TK, Kim SY. Inhibitors of apoptosis protect the ovarian reserve from cyclophosphamide. J Endocrinol. 2019;240:243–256. doi: 10.1530/JOE-18-0370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gonfloni S, Di Tella L, Caldarola S, Cannata SM, Klinger FG, Di Bartolomeo C, et al. Inhibition of the c-Abl-TAp63 pathway protects mouse oocytes from chemotherapy-induced death. Nat Med. 2009;15:1179–1185. doi: 10.1038/nm.2033. [DOI] [PubMed] [Google Scholar]
- 49.Perez GI, Knudson CM, Leykin L, Korsmeyer SJ, Tilly JL. Apoptosis-associated signaling pathways are required for chemotherapy-mediated female germ cell destruction. Nat Med. 1997;3:1228–1232. doi: 10.1038/nm1197-1228. [DOI] [PubMed] [Google Scholar]
- 50.Agarwal A, Gupta S, Sekhon L, Shah R. Redox considerations in female reproductive function and assisted reproduction: from molecular mechanisms to health implications. Antioxid Redox Signal. 2008;10:1375–1403. doi: 10.1089/ars.2007.1964. [DOI] [PubMed] [Google Scholar]
- 51.Tilly JL, Tilly KI. Inhibitors of oxidative stress mimic the ability of follicle-stimulating hormone to suppress apoptosis in cultured rat ovarian follicles. Endocrinology. 1995;136:242–252. doi: 10.1210/endo.136.1.7828537. [DOI] [PubMed] [Google Scholar]
- 52.Pascuali N, Scotti L, Di Pietro M, Oubiña G, Bas D, May M, et al. Ceramide-1-phosphate has protective properties against cyclophosphamide-induced ovarian damage in a mice model of premature ovarian failure. Hum Reprod. 2018;33:844–859. doi: 10.1093/humrep/dey045. [DOI] [PubMed] [Google Scholar]
- 53.Kaygusuzoglu E, Caglayan C, Kandemir FM, Yıldırım S, Kucukler S, Kılınc MA, et al. Zingerone ameliorates cisplatin-induced ovarian and uterine toxicity via suppression of sex hormone imbalances, oxidative stress, inflammation and apoptosis in female wistar rats. Biomed Pharmacother. 2018;102:517–530. doi: 10.1016/j.biopha.2018.03.119. [DOI] [PubMed] [Google Scholar]
- 54.Zhang JQ, Xing BS, Zhu CC, Shen M, Yu FX, Liu HL. Protective effect of proanthocyanidin against oxidative ovarian damage induced by 3-nitropropionic acid in mice. Genet Mol Res. 2015;14:2484–2494. doi: 10.4238/2015.March.30.6. [DOI] [PubMed] [Google Scholar]
- 55.Li B, Weng Q, Liu Z, Shen M, Zhang J, Wu W, et al. Selection of antioxidants against ovarian oxidative stress in mouse model. J Biochem Mol Toxicol. 2017;31:e21997. doi: 10.1002/jbt.21997. [DOI] [PubMed] [Google Scholar]
- 56.Qin Y, Iwase A, Murase T, Bayasula, Ishida C, Kato N, et al. Protective effects of mangafodipir against chemotherapy-induced ovarian damage in mice. Reprod Biol Endocrinol. 2018;16:106. doi: 10.1186/s12958-018-0426-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Banu SK, Stanley JA, Sivakumar KK, Arosh JA, Burghardt RC. Resveratrol protects the ovary against chromium-toxicity by enhancing endogenous antioxidant enzymes and inhibiting metabolic clearance of estradiol. Toxicol Appl Pharmacol. 2016;303:65–78. doi: 10.1016/j.taap.2016.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Melekoglu R, Ciftci O, Eraslan S, Cetin A, Basak N. Beneficial effects of curcumin and capsaicin on cyclophosphamide-induced premature ovarian failure in a rat model. J Ovarian Res. 2018;11:33. doi: 10.1186/s13048-018-0409-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Li XH, Wang HP, Tan J, Wu YD, Yang M, Mao CZ, et al. Loss of pigment epithelium-derived factor leads to ovarian oxidative damage accompanied by diminished ovarian reserve in mice. Life Sci. 2019;216:129–139. doi: 10.1016/j.lfs.2018.11.015. [DOI] [PubMed] [Google Scholar]
- 60.Luderer U. Ovarian toxicity from reactive oxygen species. Vitam Horm. 2014;94:99–127. doi: 10.1016/B978-0-12-800095-3.00004-3. [DOI] [PubMed] [Google Scholar]
- 61.Morita Y, Perez GI, Paris F, Miranda SR, Ehleiter D, Haimovitz-Friedman A, et al. Oocyte apoptosis is suppressed by disruption of the acid sphingomyelinase gene or by sphingosine-1-phosphate therapy. Nat Med. 2000;6:1109–1114. doi: 10.1038/80442. [DOI] [PubMed] [Google Scholar]
- 62.Dayangan Sayan C, Tulmac OB, Karaca G, Ozkan ZS, Yalcin S, Devrim T, et al. Could erythropoietin reduce the ovarian damage of cisplatin in female rats? Gynecol Endocrinol. 2018;34:309–313. doi: 10.1080/09513590.2017.1395836. [DOI] [PubMed] [Google Scholar]
- 63.Akdemir A, Zeybek B, Akman L, Ergenoglu AM, Yeniel AO, Erbas O, et al. Granulocyte-colony stimulating factor decreases the extent of ovarian damage caused by cisplatin in an experimental rat model. J Gynecol Oncol. 2014;25:328–333. doi: 10.3802/jgo.2014.25.4.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ting AY, Petroff BK. Tamoxifen decreases ovarian follicular loss from experimental toxicant DMBA and chemotherapy agents cyclophosphamide and doxorubicin in the rat. J Assist Reprod Genet. 2010;27:591–597. doi: 10.1007/s10815-010-9463-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kropp J, Roti Roti EC, Ringelstetter A, Khatib H, Abbott DH, Salih SM. Dexrazoxane diminishes doxorubicin-induced acute ovarian damage and preserves ovarian function and fecundity in mice. PLoS One. 2015;10:e0142588. doi: 10.1371/journal.pone.0142588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Roti Roti EC, Salih SM. Dexrazoxane ameliorates doxorubicin-induced injury in mouse ovarian cells. Biol Reprod. 2012;86:96. doi: 10.1095/biolreprod.111.097030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Salih SM, Ringelstetter AK, Elsarrag MZ, Abbott DH, Roti EC. Dexrazoxane abrogates acute doxorubicin toxicity in marmoset ovary. Biol Reprod. 2015;92:73. doi: 10.1095/biolreprod.114.119495. [DOI] [PMC free article] [PubMed] [Google Scholar]