Abstract
Background
Pulmonary arterial hypertension (PAH) is a serious disease exhibiting unspecific symptoms, as a result of which diagnosis is often delayed and prognosis is poor. The underlying pathophysiology includes vasoconstriction and remodelling of small pulmonary arteries. As receptor tyrosine kinases (RTKs) and their ligands have been shown to promote PAH remodelling, our aim was to evaluate if their plasma levels may be utilised to differentiate between various causes of pulmonary hypertension.
Methods
28 biomarkers involved in RTK signalling were measured using proximity extension assays in venous plasma from patients with PAH (n=48), chronic thromboembolic pulmonary hypertension (CTEPH) (n=20), pulmonary hypertension due to diastolic (n=33) or systolic (n=36) heart failure and heart failure patients without pulmonary hypertension (n=15), as well as healthy controls (n=20).
Results
Plasma proto-oncogene tyrosine-protein kinase receptor Ret (RET) was decreased (p<0.04) in PAH compared with all disease groups and controls. RET generated a sensitivity of 64.6% and a specificity of 81.6% for detecting PAH from other disease groups. PAH and the other pulmonary hypertension groups showed elevated plasma tyrosine-protein kinase MER (p<0.01), vascular endothelial growth factor (VEGF)-A (p<0.02), VEGF-D (p<0.01), placental growth factor (p<0.01), amphiregulin (p<0.02), hepatocyte growth factor (p<0.01) and transforming growth factor-α (p<0.05) and decreased VEGF receptor-2 (p<0.04) and epidermal growth factor receptor (p<0.01) levels compared with controls.
Conclusion
Plasma RET differentiates patients with PAH from those with CTEPH, systolic or diastolic heart failure with or without pulmonary hypertension as well as healthy controls. Future studies would be of value to determine the clinical usefulness of RET as a biomarker and its link to PAH pathophysiology.
Short abstract
Receptor tyrosine kinases have been shown to promote PAH remodelling. Plasma RET differentiates PAH from other causes of PH. RET could have the potential to be used as a future diagnostic biomarker. http://bit.ly/2LChPUS
Introduction
Pulmonary hypertension is defined as an elevated mean pulmonary arterial pressure (mPAP) ≥25 mmHg at rest and is classified into five groups, including 1) pulmonary arterial hypertension (PAH), 2) pulmonary hypertension due to left heart disease, 3) pulmonary hypertension due to lung disease and/or chronic hypoxia, 4) chronic thromboembolic pulmonary hypertension (CTEPH) and 5) pulmonary hypertension due to unclear and/or multifactorial mechanisms [1]. At the World Symposium on Pulmonary Hypertension in Nice 2018, a new definition of pulmonary hypertension was suggested [2]. However, the new proposed breakpoint mPAP value of 20 mmHg has not yet been adopted in European guidelines.
PAH is a serious condition where time to diagnosis and introduction of targeted therapy is crucial to improve outcome [1]. However, due to diffuse and unspecific symptoms, such as dyspnoea and fatigue, PAH diagnosis is often set late [1, 3]. Despite current vasoactive therapy, prognosis still remains poor [4, 5]. PAH is related to an imbalance of vasoactive compounds, with pathological changes located to distal pulmonary arteries, comprising vasoconstriction and vessel wall proliferation of the intima, media and adventitia, formation of plexiform lesions, and in situ thrombosis [1, 6, 7]. The precise underlying mechanistic causes of these changes are not completely understood. CTEPH is characterised by organised and fibrotic thromboembolism in the pulmonary arteries, resulting in obstruction and subsequent remodelling [1, 8, 9], partly similar to that seen in PAH. Moreover, pulmonary hypertension due to left heart disease, comprising the largest group of pulmonary hypertension patients [1], may result in endothelial damage and dysfunction, excessive vasoconstriction, followed by vascular remodelling. If such changes become unresponsive to medical vasoactive therapy, it may constitute a contraindication for cardiac transplantation [10, 11].
At present, there is no curative medical treatment available for PAH or for other causes of pulmonary hypertension. Medical vasoactive therapies are, however, well established in PAH and may decrease morbidity as well as mortality. As pulmonary hypertension is a negative prognostic factor in both left heart and pulmonary diseases [1, 11–13], it is of great importance to develop new diagnostic methods to identify and differentiate pulmonary hypertension, and especially PAH, patients at an earlier stage, to enable earlier treatment initiation that may stabilise or move the patient's “risk strata” into the low-risk zone.
Receptor tyrosine kinases (RTKs) and their ligands are involved in cell cycle regulation and of great interest in PAH development, since cellular changes involving their signalling pathways have been shown to be affected [14–16]. Such changes are suggested to be involved in PAH remodelling, including characteristics that are shared with cancer pathology, with dysregulated proliferation, apoptosis resistance and abnormal metabolism [15]. Antineoplastic drugs have therefore become of great interest. The tyrosine kinase inhibitor imatinib, a platelet-derived growth factor (PDGF) receptor inhibitor, was evaluated in the Imatinib in Pulmonary Arterial Hypertension, a Randomised, Efficacy Study (IMPRES), where patients showed improved physical capacity and haemodynamics. However, serious adverse events occurred [17].
Moreover, the vascular endothelial growth factor (VEGF) family is an intriguing group of tyrosine kinases that have been widely investigated in pulmonary hypertension. The VEGF ligands and their receptors have been shown to be altered in earlier studies, indicating dysregulated angiogenesis in pulmonary hypertension pathology [18–21]. In a rat model, monocrotaline-induced pulmonary hypertension was shown to be associated with reduced VEGF expression [22]. Overexpression of the angiogenic factor VEGF-A has furthermore been suggested to be protective in pulmonary hypertension [23]. PDGF has additionally been reported to mediate smooth muscle proliferation in pulmonary vascular remodelling in rats [24] and to be upregulated in PAH patients [25]. These findings indicate the complexity in pulmonary hypertension pathophysiology and the value of further research to characterise the specific roles of tyrosine kinases in pulmonary hypertension development.
New circulating plasma biomarkers, such as tyrosine kinases, could have the potential to be used for earlier diagnosis and differentiation of pulmonary hypertension aetiologies, for risk stratification, as well as in decisions for listing patients for lung and/or heart transplantation. We therefore investigated a broad range of blood-borne plasma biomarkers related to RTKs and associated proteins, in relation to different causes of pulmonary hypertension.
Methods
Study design and population
28 circulating plasma biomarkers related to RTK signalling were analysed from mixed venous blood plasma samples of 152 patients, separated into PAH (n=48), CTEPH (n=20), pulmonary hypertension due to diastolic heart failure (preserved ejection fraction, n=33), pulmonary hypertension due to systolic heart failure (reduced ejection fraction, n=36) and heart failure without pulmonary hypertension (n=15), as well as from peripheral venous plasma samples from healthy control subjects (n=20). All samples from the patient groups were obtained from the same location of venous introducers during standard right heart catheterisation (RHC) procedures between September 2011 and March 2017 at diagnosis, before initiation of any disease-specific treatments in PAH patients. The samples were stored in and retrieved from the Lund Cardio Pulmonary Register (LCPR), a cohort in the Biobank of Region Skåne (Sweden). Data on patient characteristics, medications, haemodynamics and clinical parameters, including World Health Organization Functional Classification (WHO FC) and 6-min walk distance (6MWD), assessed in connection with blood sampling, were retrieved retrospectively from medical records. All patients and controls gave written informed consent for storage and analysis of their blood samples in the LCPR. The study was approved by the local ethics board in Lund (2010/114, 2010/442, 2011/368, 2011/777 and 2015/270) and performed in accordance with the Declaration of Helsinki.
Right heart catheterisation
RHCs were performed as a part of the routine clinical investigation for all patients, using a Swan–Ganz catheter (Baxter Health Care, Santa Ana, CA, USA), inserted predominantly via an introducer in the right internal jugular vein, at The Hemodynamic Lab, The Section for Heart Failure and Valvular Disease, Skåne University Hospital (Lund, Sweden). Haemodynamic parameters including mPAP, mean right atrial pressure (mRAP), pulmonary arterial wedge pressure (PAWP), diastolic pulmonary arterial pressure, systolic pulmonary arterial pressure and mean arterial pressure (mAP) were measured during the procedure. Cardiac output (CO) was estimated using thermodilution.
Cardiac index (CI), pulmonary vascular resistance (PVR), left ventricular stroke work index (LVSWI) and right ventricular stroke work index (RVSWI) were calculated using the following formulae: CI=CO/body surface area (BSA), PVR=(mPAP−PAWP)/CO, LVSWI=(mAP−PAWP)×stroke volume (SV)/BSA and RVSWI=(mPAP−mRAP)×SV/BSA.
Biomarker analyses
Blood samples were centrifuged and stored at −80°C in the LCPR. Biomarkers were analysed using the proximity extension assay (PEA) technique followed by PCR (Olink Bioscience, Uppsala, Sweden), as previously described [26]. A subgroup of biomarkers involved in RTK signalling was analysed using Proseek Multiplex CVD II, CVD III and Oncology II 96-plex immunoassay panels (Olink Bioscience), including members of 1) TAM receptor kinase family (tyrosine-protein kinase MER (MERTK) and tyrosine-protein kinase receptor UFO (AXL)); 2) VEGF family (VEGF receptor (VEGFR)-2 and -3, VEGF-A and -D, and placental growth factor (PlGF)); 3) epidermal growth factor (EGF) family (EGF receptor (EGFR), human EGFR (HER) 2, HER3, HER4, pro-EGF, amphiregulin, heparin-binding EGF-like growth factor (HB-EGF) and transforming growth factor (TGF)-α); 4) TIE family of angiopoietin receptors (angiopoietin receptor TEK tyrosine kinase (Tie2) and angiopoietin 1 (Ang-1)); 5) PDGF family (PDGF subunit A and B); 6) non-RTK family (proto-oncogene tyrosine-protein kinase Src (SRC), tyrosine-protein kinase Lyn (LYN) and tyrosine-protein kinase ABL1 (ABL-1)); 7) ephrin receptor family (ephrin type A receptor 2 (EPHA2), ephrin type B receptor 4 (EPHB4)) and 8) other tyrosine kinases (proto-oncogene tyrosine-protein kinase receptor Ret (RET), stem cell factor (SCF), hepatocyte growth factor (HGF) and fibroblast growth factor-binding protein 1 (FGF-BP1)). N-terminal pro-brain natriuretic peptide (NT-proBNP) levels were analysed using the same technique. Plasma levels of these biomarkers were measured in normalised protein expression values, which is an arbitrary unit on a log2 scale. Validation documents of the Olink PEA and PCR analyses can be found at: www.olink.com/resources-support/document-download-center.
Statistics
Statistical analyses as well as figures were made using Prism version 7.00 for Mac (www.graphpad.com) or R version 3.5.1 (www.r-project.org). Comparisons of plasma biomarker level differences between PAH, CTEPH, pulmonary hypertension due to diastolic heart failure (preserved ejection fraction), pulmonary hypertension due to systolic heart failure (reduced ejection fraction) with pulmonary hypertension and heart failure patients without pulmonary hypertension, as well as controls, were analysed using the Kruskal–Wallis test. False discovery rates (FDRs) were determined for all Kruskal–Wallis tests comparing biomarkers in the studied groups. FDR was set to 5%. The number of statistical tests was 273 based on the biomarkers included in all three panels. Post hoc analyses using Dunn's multiple comparison test was performed for tests with significant adjusted Kruskal–Wallis p-values.
To assess the performance of RET as a predictor of PAH among other disease groups, the area under the curve (AUC) of the receiver operating characteristics (ROC) curve was calculated. The best cut-off was determined according to Youden's index. Correlation analyses between RET levels and mPAP, mRAP, CI, PVR as well as SvO2, 6MWD and NT-proBNP were performed using Spearman's coefficient.
Results are presented as median (interquartile range (IQR)) for continuous variables and absolute or percentage for categorical variables, unless otherwise stated. Statistical significance was accepted at p<0.05.
Results
Population and haemodynamic characteristics
Study population characteristics are shown in table 1. In PAH, 21 patients (43.8%) were diagnosed with idiopathic PAH, two patients (4.2%) with familial PAH, 17 patients (35.4%) with systemic sclerosis (SSc)-associated PAH, four patients (8.3%) with SSc-associated PAH without interstitial lung disease and four patients (8.3%) with other connective tissue disease-associated PAH. Median (IQR) 6MWD at diagnosis was 242 (172.5–349) m in PAH and 300 (220–337.5) m in CTEPH. 6MWD data were missing for two PAH patients and three CTEPH patients. In PAH, one patient (2.1%) was classified in WHO FC 1, nine patients (18.8%) in WHO FC 2, 28 patients (58.3%) in WHO FC 3 and two patients (4.2%) in WHO FC 4. In CTEPH, six patients (30.0%) were classified in WHO FC 2 and 13 patients (65.0%) in WHO FC 3. WHO FC data were missing for eight PAH patients and one CTEPH patient. The controls had no events of ischaemic heart disease, atrial fibrillation, stroke or diabetes mellitus.
TABLE 1.
Population characteristics
| Control | PAH | CTEPH | PH-HFpEF | PH-HFrEF | Non-PH-HF | |
| Subjects n (% female) | 20 (55) | 48 (83) | 20 (65) | 33 (64) | 36 (19) | 15 (53) |
| Age years | 41 (26.8–50.5) | 71.5 (64.0–76.0) | 75 (70.8–77.8) | 75.0 (68.5–83.0) | 54.0 (47.3–59.5) | 60.0 (46.0–76.0) |
| BSA m2 | 1.9 (1.8–2.0) | 1.7 (1.6–2.0) | 1.8 (1.8–2.0) | 1.9 (1.7–2.1) | 2.0 (1.9–2.1) | 2.0 (1.7–2.1) |
| mAP mmHg | 89.0 (95.0–100.0) | 96.0 (89.4–104.0) | 98.5 (94.0–110.3) | 98.0 (91.5–104.5) | 79.5 (75.3–88.8) | 89.0 (80.0–96.0) |
| mPAP mmHg | 43.0 (37.0–54.8) | 42.0 (35.0–54.3) | 34.0 (28.5–46.0) | 34.5 (29.0–40.8) | 20.0 (17.0–22.0) | |
| PAWP mmHg | 8.0 (6.0–11.0) | 9.5 (7.0–13.0) | 18.0 (16.0–22.5) | 25.0 (19.0–28.0) | 15.0 (9.0–18.0) | |
| mRAP mmHg | 7.0 (4.0–11.0) | 5.5 (3.3–8.0) | 10.0 (6.5–14.0) | 14.5 (9.0–17.0) | 6.0 (2.0–16.0) | |
| CI L·min−1·m−2 | 2.2 (1.8–2.8) | 2.3 (1.9–2.5) | 2.4 (2.1–2.8) | 1.6 (1.4–1.9) | 1.9 (1.6–2.2) | |
| PVR WU | 9.5 (6.2–11.8) | 9.3 (5.9–10.8) | 3.6 (2.4–4.9) | 3.0 (2.3–3.7) | 1.5 (1.0–2.0) | |
| LVSWI mmHg·mL·m−2 | 2488.0 (2045.0–3213.0) | 2508.0 (2330.0–3187.0) | 2664 (2189.0–3308.0) | 1152.0 (957.0–1636.0) | 2168.0 (1650.0–2716.0) | |
| RVSWI mmHg·mL·m−2 | 990.5 (807.2–1246.0) | 1111.0 (844.5–1298.0) | 831.5 (670.7–1140.0) | 439.6 (305.8–649.3) | 382.4 (195.5–494.5) | |
| SvO2 % | 60.5 (51.6–66.6) | 62.5 (54.9–67.9) | 64.1 (57.8–66.8) | 50.3 (46.5–55.2) | 61.2 (58.5–69.2) | |
| NT-proBNP AU | 3.1 (2.1–3.8) | 2.6 (1.0–4.2) | 2.9 (2.4–3.3) | 4.9 (4.1–5.4) | 3.2 (1.3–4.4) | |
| Creatinine μmol·L−1 | 90.0 (70.8–113.5) | 88.0 (73.0–122.5) | 99.0 (79.0–117.0) | 121.0 (90.0–145.0) | 93.0 (80.5–123.0) | |
| Hypertension | 17 (35) | 11 (55) | 22 (67) | 7 (19) | 7 (47) | |
| Diabetes mellitus | 12 (25) | 0 (0) | 11 (33) | 4 (11) | 3 (20) | |
| Atrial fibrillation | 4 (8) | 3 (15) | 25 (76) | 15 (42) | 8 (53) | |
| Stroke | 2 (4) | 1 (5) | 6 (18) | 4 (11) | 2 (13) | |
| Ischaemic heart disease | 7 (15) | 1 (5) | 6 (18) | 6 (17) | 6 (40) | |
| Thyroid disease | 11 (23) | 1 (5) | 2 (6) | 3 (8) | 3 (20) | |
| ACEi | 10 (21) | 2 (10) | 12 (36) | 19 (53) | 3 (20) | |
| β-blockers | 16 (33) | 9 (45) | 25 (76) | 35 (97) | 11 (73) | |
| ARB | 4 (8) | 7 (35) | 10 (30) | 14 (39) | 5 (33) | |
| MRA | 11 (23) | 3 (15) | 9 (27) | 21 (58) | 7 (47) |
Data are presented as median (interquartile range) or n (%), unless otherwise stated. PAH: pulmonary arterial hypertension; CTEPH: chronic thromboembolic pulmonary hypertension; PH-HFpEF: pulmonary hypertension due to diastolic heart failure (preserved ejection fraction); PH-HFrEF: pulmonary hypertension due to systolic heart failure (reduced ejection fraction); non-PH-HF: heart failure without pulmonary hypertension; BSA: body surface area; mAP: mean arterial pressure; mPAP: mean pulmonary arterial pressure; PAWP: pulmonary arterial wedge pressure; mRAP: mean right atrial pressure; CI: cardiac index; SV: stroke volume; PVR: pulmonary vascular resistance; WU: Wood Units; LVSWI: left ventricular stroke work index; RVSWI: right ventricular stroke work index; SvO2: mixed venous oxygen saturation; NT-proBNP: N-terminal pro-brain natriuretic peptide; AU: arbitrary units; ACEi: angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blocker; MRA: mineralocorticoid receptor antagonist.
Biomarker levels
RET plasma levels are lower in PAH
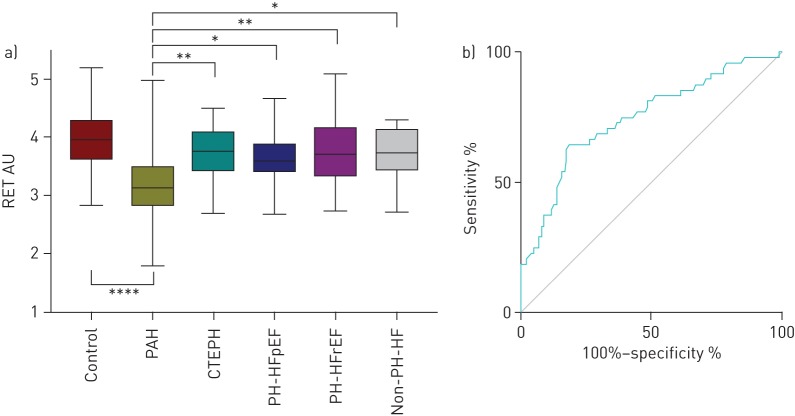
RET plasma levels were lower in PAH compared with all the other disease groups (p<0.038) and controls (p<0.001) (table 2 and figure 1). ROC analyses for plasma RET generated an AUC of 0.747 (95% CI 0.659–0.834) (p<0.001) with a sensitivity of 64.6% and a specificity of 81.6% for PAH (figure 1). No specific correlations were, however, detected between plasma RET and mPAP, mRAP, CI, PVR, SvO2, 6MWD and NT-proBNP (all nonsignificant).
TABLE 2.
Biomarker plasma levels
| Control | PAH | CTEPH | PH-HFpEF | PH-HFrEF | Non-PH-HF | |
| TAM receptor kinase family | ||||||
| MERTK | 3.58 (3.47–3.90) | 4.05 (3.82–4.36)# | 4.32 (4.12–4.56)# | 4.37 (4.13–4.62)# | 4.15 (3.89–4.68)# | 4.33 (4.19–4.57)# |
| AXL | 7.35 (7.18–7.63) | 7.35 (6.93–7.65) | 7.23 (7.03–7.43) | 7.47 (7.20–8.02) | 7.68 (7.38–8.05)¶,+ | 7.50 (7.23–8.01) |
| VEGF family | ||||||
| VEGFR-2 | 6.58 (6.38–6.68) | 6.18 (5.96–6.41)# | 6.18 (6.02–6.40)# | 6.01 (5.86–6.18)# | 6.18 (5.99–6.32)# | 6.10 (5.88–6.34)# |
| VEGFR-3 | 5.74 (5.42–5.79) | 5.74 (5.51–5.92) | 5.80 (5.55–5.95) | 5.77 (5.51–5.91) | 5.88 (5.74–6.06)#,¶ | 5.73 (5.49–5.96) |
| VEGF-A | 9.13 (8.94–9.43) | 9.83 (9.45–10.22)# | 9.87 (9.61–10.54)# | 10.02 (9.78–10.45)# | 9.76 (9.37–10.18)# | 9.77 (9.45–10.02)# |
| VEGF-D | 6.78 (6.56–6.92) | 7.23 (7.01–7.48)# | 7.47 (7.24–7.66)# | 7.47 (7.20–7.74)# | 7.97 (7.74 –8.05)#,¶,+,§ | 7.36 (6.65–7.74)ƒ |
| PlGF | 6.92 (6.78–7.26) | 7.61 (7.43–8.08)# | 7.64 (7.46–7.93)# | 7.92 (7.57–8.31)# | 7.62 (7.31–8.03)# | 7.72 (7.42–7.89)# |
| EGF family | ||||||
| EGFR | 1.38 (1.26–1.56) | 0.82 (0.65–1.08)# | 1.04 (0.82–1.10)# | 0.99 (0.73–1.15)# | 1.08 (0.97–1.23)#,¶ | 1.06 (0.92–1.24)# |
| HER2 | 6.44 (6.20–6.69) | 6.39 (6.09–6.55) | 6.54 (6.37–6.72) | 6.43 (6.16–6.71) | 6.72 (6.63–6.92)#,¶,§ | 6.68 (6.47–6.74) |
| HER3 | 7.46 (7.31–7.54) | 7.26 (7.11–7.44) | 7.42 (7.27–7.63) | 7.32 (7.08–7.38) | 7.37 (7.20–7.62) | 7.30 (7.20–7.56) |
| HER4 | 4.55 (4.24–4.65) | 4.50 (4.36–4.66) | 4.56 (4.38–4.67) | 4.48 (4.33–4.68) | 4.80 (4.63–5.00)#,¶,§ | 4.76 (4.27–4.93) |
| Pro-EGF | 8.63 (7.36–9.48) | 7.76 (6.57–8.62) | 7.96 (6.84–8.61) | 7.97 (7.16–8.85) | 7.12 (5.93–8.05)# | 7.85 (7.25–8.96) |
| Amphiregulin | 1.43 (1.21–1.57) | 2.43 (2.09–2.79)# | 2.14 (1.99–2.49)# | 2.30 (1.99–2.83)# | 2.62 (2.02–3.15)# | 1.99 (1.76–2.61)# |
| HB-EGF | 5.90 (5.44–6.33) | 5.77 (5.53–6.24) | 6.52 (5.84–6.98)¶ | 6.13 (5.57–6.48) | 5.75 (5.37–6.17)+ | 6.28 (5.75–6.70) |
| TGF-α | 1.20 (0.93–1.39) | 1.82 (1.62–2.15)# | 2.07 (1.60–2.37)# | 2.05 (1.67–2.48)# | 2.06 (1.77–2.35)# | 1.56 (1.48–2.09)# |
| TIE family of angiopoietin receptors | ||||||
| Tie2 | 7.53 (7.35–7.64) | 7.57 (7.40–7.82) | 7.81 (7.59–7.98)# | 7.72 (7.57–7.97) | 8.09 (7.79–8.17)#,¶,§ | 7.90 (7.60–8.11)# |
| Ang-1 | 8.26 (7.68–8.97) | 8.27 (7.84–9.03) | 9.20 (8.09–9.75) | 8.57 (7.87–9.36) | 8.11 (7.32–8.81)+ | 9.00 (7.89–9.50) |
| PDGF family | ||||||
| PDGF subunit A | 2.89 (2.41–3.40) | 2.89 (2.04–3.36) | 3.57 (3.01–4.63) | 3.12 (2.09–3.77) | 2.70 (2.16–3.42)+ | 3.22 (2.30–3.90) |
| PDGF subunit B | 9.48 (8.65–9.92) | 9.17 (8.52–9.77) | 9.55 (8.94–10.16) | 9.50 (8.27–9.83) | 8.82 (7.87–9.54) | 9.45 (8.66–9.98) |
| Non-RTK family | ||||||
| SRC | 6.87 (6.77–7.11) | 6.93 (6.51–7.17) | 6.82 (6.52–7.12) | 6.96 (6.68–7.14) | 6.88 (5.95–7.22) | 7.12 (6.64–7.28) |
| LYN | 2.80 (2.13–3.21) | 2.38 (1.89–2.97) | 2.30 (2.11–2.54) | 2.49 (2.17–3.11) | 2.28 (1.87–2.75) | 2.48 (2.13–3.32) |
| ABL-1 | 4.57 (3.05–5.31) | 3.87 (3.24–4.99) | 4.15 (3.93–4.71) | 4.57 (4.08–5.33)¶ | 4.11 (3.71–4.88) | 4.88 (4.04–5.37) |
| Ephrin receptor family | ||||||
| EPHA2 | 1.50 (1.39–1.59) | 1.89 (1.63–2.18)# | 1.69 (1.52–1.97) | 2.10 (1.83–2.38)# | 1.67 (1.48–2.24)# | 1.81 (1.70–2.10)# |
| EPHB4 | 1.44 (1.29–1.54) | 1.50 (1.13–1.77) | 1.54 (1.39–1.65) | 1.72 (1.46–2.02)#,¶ | 1.72 (1.41–1.89) | 1.62 (1.36–1.68) |
| Other tyrosine kinases | ||||||
| RET | 3.96 (3.59–4.32) | 3.13 (2.77–3.53)# | 3.75 (3.37–4.12)¶ | 3.58 (3.36–3.91)¶ | 3.71 (3.30–4.19)¶ | 3.73 (3.4–4.16)¶ |
| SCF | 8.45 (8.34–8.80) | 8.01 (7.37–8.36)# | 8.29 (8.00–8.68) | 8.26 (7.78–8.48) | 7.72 (7.31–8.08)#,+,§ | 8.11 (7.71–8.46) |
| HGF | 5.50 (5.24–5.85) | 6.35 (6.18–6.66)# | 6.54 (6.06–6.81)# | 6.66 (6.20–7.02)# | 6.59 (6.33–7.38)# | 6.60 (6.13–7.22)# |
| FGF-BP1 | 4.30 (4.19–4.34) | 4.59 (4.38–4.89)# | 4.61 (4.36–4.72) | 4.5 (4.33–4.81) | 4.83 (4.40–5.19)# | 4.49 (4.26–4.81) |
Levels are presented as median (interquartile range) of arbitrary units. PAH: pulmonary arterial hypertension; CTEPH: chronic thromboembolic pulmonary hypertension; PH-HFpEF: pulmonary hypertension due to diastolic heart failure (preserved ejection fraction); PH-HFrEF: pulmonary hypertension due to systolic heart failure (reduced ejection fraction); non-PH-HF: heart failure without pulmonary hypertension; MERTK: tyrosine-protein kinase MER; AXL: tyrosine-protein kinase receptor UFO; VEGF: vascular endothelial growth factor; VEGFR: VEGF receptor; PlGF: placental growth factor; pro-EGF: pro-epidermal growth factor; EGFR: EGF receptor; HER: human EGFR; HB-EGF: heparin-binding EGF-like growth factor; TGF: transforming growth factor; Tie2: angiopoietin receptor TEK tyrosine kinase; Ang-1: angiopoietin 1; PDGF: platelet-derived growth factor; RTK: receptor tyrosine kinase; SRC: proto-oncogene tyrosine-protein kinase Src; LYN: tyrosine-protein kinase Lyn; ABL-1: tyrosine-protein kinase ABL1; EPHA2: ephrin type A receptor 2; EPHB4: ephrin type B receptor 4; RET: proto-oncogene tyrosine-protein kinase receptor Ret; SCF: stem cell factor; HGF: hepatocyte growth factor; FGF-BP1: fibroblast growth factor-binding protein 1. #: significantly different compared with controls; ¶: significantly different compared with PAH; +: significantly different compared with CTEPH; §: significantly different compared with PH-HFpEF; ƒ: significantly different compared with PH-HFrEF.
FIGURE 1.
a) Proto-oncogene tyrosine-protein kinase receptor Ret (RET) in controls and disease groups. AU: arbitrary units; PAH: pulmonary arterial hypertension; CTEPH: chronic thromboembolic pulmonary hypertension; PH-HFpEF: pulmonary hypertension due to diastolic heart failure (preserved ejection fraction); PH-HFrEF: pulmonary hypertension due to systolic heart failure (reduced ejection fraction); non-PH-HF: heart failure without pulmonary hypertension. RET was reduced in plasma in PAH compared with the other disease groups and controls. *: p<0.05; **: p<0.01; ****: p<0.0001. b) Receiver operating characteristics of RET as a predictor of PAH among other pulmonary hypertension groups.
Plasma VEGF ligands are higher and VEGFR-2 is lower in pulmonary hypertension
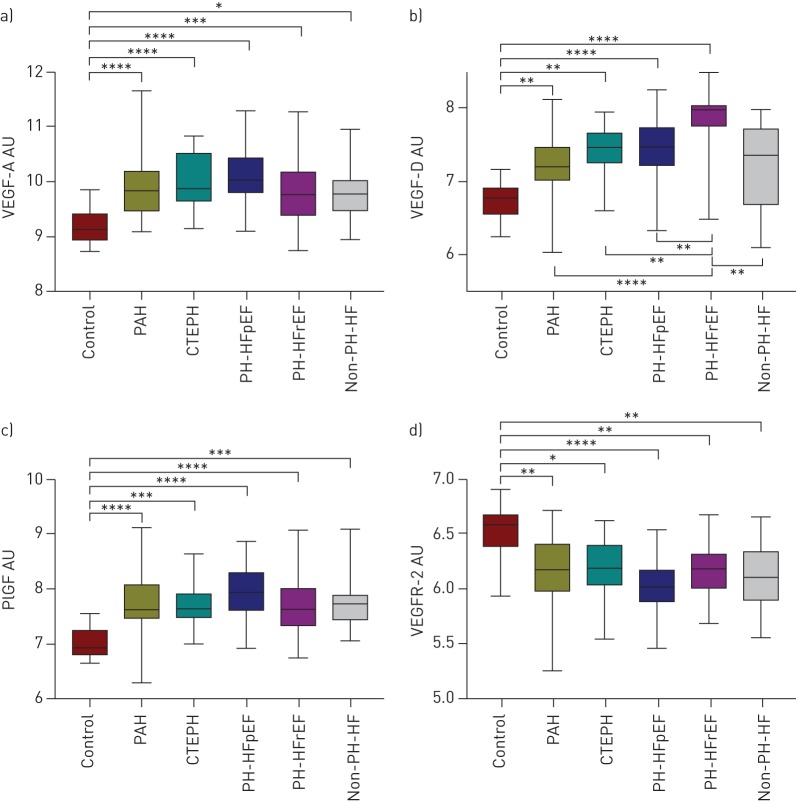
Controls had lower levels of VEGF-A (p<0.013), VEGF-D (p<0.010) and PlGF (p<0.001) and higher levels of VEGFR-2 (p<0.036) compared with the pulmonary hypertension patient groups (table 2 and figure 2).
FIGURE 2.
Vascular endothelial growth factor (VEGF) ligands a) VEGF-A, b) VEGF-D and c) placental growth factor (PlGF) are upregulated and d) tyrosine kinase receptor VEGF receptor (VEGFR)-2 is downregulated in pulmonary hypertension compared with controls. AU: arbitrary units; PAH: pulmonary arterial hypertension; CTEPH: chronic thromboembolic pulmonary hypertension; PH-HFpEF: pulmonary hypertension due to diastolic heart failure (preserved ejection fraction); PH-HFrEF: pulmonary hypertension due to systolic heart failure (reduced ejection fraction); non-PH-HF: heart failure without pulmonary hypertension. *: p<0.05; **: p<0.01; ***: p<0.001; ****: p<0.0001.
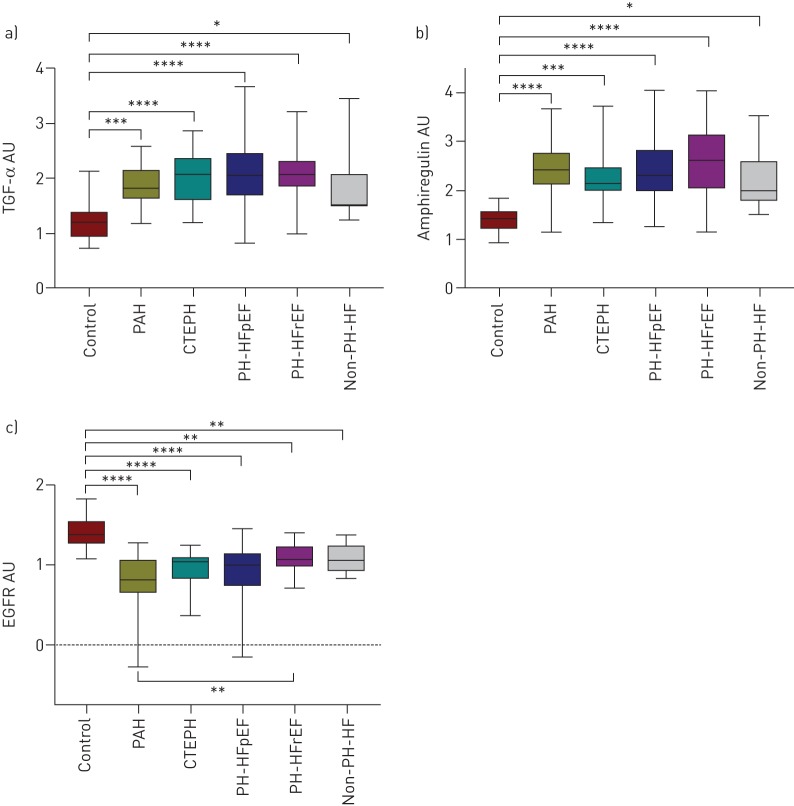
Plasma TGF-α and amphiregulin are higher and EGFR is lower in pulmonary hypertension and heart failure
Controls had lower levels of TGF-α (p<0.042) and amphiregulin (p<0.014) as well as higher levels of EGFR (p<0.008) compared with pulmonary hypertension patient groups and heart failure without pulmonary hypertension (table 2 and figure 3).
FIGURE 3.
a) Transforming growth factor (TGF)-α and b) amphiregulin are upregulated and c) receptor tyrosine kinase epidermal growth factor receptor (EGFR) is downregulated in pulmonary hypertension plasma. AU: arbitrary units; PAH: pulmonary arterial hypertension; CTEPH: chronic thromboembolic pulmonary hypertension; PH-HFpEF: pulmonary hypertension due to diastolic heart failure (preserved ejection fraction); PH-HFrEF: pulmonary hypertension due to systolic heart failure (reduced ejection fraction); non-PH-HF: heart failure without pulmonary hypertension. *: p<0.05; **: p<0.01; ***: p<0.001; ****: p<0.0001.
Plasma MERTK and HGF levels are higher in pulmonary hypertension and heart failure
Controls had lower levels of MERTK (p<0.009) and HGF (p<0.001) (table 2) compared with pulmonary hypertension patient groups and heart failure without pulmonary hypertension. The p-values of multiple comparisons between controls and patient groups are shown in supplementary table S1.
Discussion
The present study indicates that RET plasma levels may be of use to identify patients with PAH among other conditions presenting with similar symptoms, such as heart failure with or without pulmonary hypertension as well as CTEPH. Plasma RET furthermore differentiates PAH patients from healthy controls. Previous studies have shown RTKs to be dysregulated in PAH pathology, involving cellular pathways of proliferation, inhibition of apoptosis and angiogenesis, with characteristics similar to cancer pathology [14–16, 27]. However, to the best of our knowledge, RET as a plasma biomarker has not previously been investigated in the field of pulmonary hypertension. The present study identifies a potential link between RTKs and PAH pathophysiology, which may pave the way for new diagnostic approaches in the future.
Although the list of investigated biomarkers in pulmonary hypertension is constantly growing [1], so far NT-proBNP and its precursors, which reflect myocardial stress, are the only circulating biomarkers widely used clinically in pulmonary hypertension [1]. This conveys the need for further research to understand the pathophysiology of various causes of pulmonary hypertension, and to enable the development of new diagnostic methods and novel targets for therapy.
RET is a transmembrane tyrosine kinase with ligands of the glial cell line-derived neurotrophic factor (GDNF) family, which requires GDNF family receptor α co-receptors to exert its functions [28]. Mutations in the RET gene have been linked to human cancers, including papillary and medullary thyroid carcinoma, multiple endocrine neoplasia types 2A and 2B, and Hirschsprung's disease [28, 29]. RET has been reported to initiate signalling pathways involved in cell survival, differentiation, proliferation and migration [28, 29], and could thus also be involved in the vascular remodelling in PAH. In the present study, however, no correlations were detected between haemodynamic parameters and RET. This may indicate that RET is not involved in the disease progression. Pathological changes in RET systems may instead drive the initial changes seen in PAH. RET may consequently be of use as a biomarker in PAH diagnosis, but potentially not when evaluating disease severity or in risk stratification.
In this study, deranged levels of both growth factors and their receptors were seen in the pulmonary hypertension groups. In pulmonary hypertension, plasma VEGF-A, VEGF-D and PlGF levels were higher and VEGFR-2 levels were lower compared with controls. Elevated levels of VEGF family growth factors have previously also been observed in pulmonary hypertension when compared with control subjects [19–21], in line with our findings. Partovian et al. [30] have suggested that elevated levels of VEGFs are protective in hypoxic pulmonary hypertension in rats. Furthermore, VEGFR-2 has been reported to be upregulated in plexiform lesions in pulmonary hypertension [18].
In the EGF family, deranged levels of both growth factors and their receptors were also seen, with higher levels of the ligands TGF-α and amphiregulin, as well as lower levels of EGFR in pulmonary hypertension patients compared with controls. Le Cras et al. [31] showed that mice overexpressing TGF-α developed severe pulmonary hypertension with extensive pulmonary vascular remodelling. Interestingly, reduced VEGF-A protein levels were observed in the lungs of these TGF-α mice. Amphiregulin has been shown to be a potent mitogen of vascular smooth muscle cells [32] and elevated levels in pulmonary hypertension patients could therefore potentially be involved in pulmonary vascular remodelling.
The plasma levels of another tyrosine kinase receptor, MERTK, were also shown to be altered, with lower levels in the control group compared with pulmonary hypertension groups and heart failure without pulmonary hypertension. MERTK is expressed on phagocytic cells and platelets, and has been shown to be involved in many cellular processes, including inflammation, and in both tethering and phagocytosis of apoptotic cells [33, 34]. Thorp et al. [35] showed that mice with mutated MERTK exhibited increased apoptotic cell accumulation and formation of necrotic plaques. The expression of MERTK has also been shown to be reduced in hypoxic mice, with subsequent repression of efferocytosis [36].
Defective clearance of apoptotic bodies with accumulation of cellular debris leading to pro-inflammatory stimulation and presence of autoantigens has been suggested to be the underlying mechanism in systemic autoimmune diseases [37]. Of interest, PAH may be related to autoimmune diseases, such as SSc and systemic lupus erythematosus [1]. Defective MERTK, leading to reduced efferocytosis, could therefore potentially be involved in PAH pathogenesis. Furthermore, in PAH, deranged levels of cytokines, as well as perivascular inflammatory infiltrates, have been reported, supporting disturbed inflammation as a part of the pathological process [19, 21, 38].
HGF plasma levels were observed to be higher in pulmonary hypertension groups compared with controls. In a previous study, HGF levels were shown to be elevated in PAH compared with controls, with higher levels observed in severe PAH compared with mild and moderate disease severity [39]. However, in a PAH rat model, 14 days administration of recombinant human HGF resulted in vascular lumen enlargement, decreased pulmonary arterial pressure and ultimately prolonged survival [40], emphasising the complexity of pulmonary hypertension pathophysiology.
Herein, we demonstrate that several circulating tyrosine kinases and their related ligands are of interest in the field of pulmonary hypertension. However, the results should be interpreted with caution and study limitations should be considered. First, this is an exploratory study evaluating a wide range of circulating biomarkers, with the bias of multiple comparisons and potential false-positive results. Thus, further studies are encouraged to outline the precise mechanisms of these plasma biomarkers, especially RET, in PAH. Moreover, the understanding of the pathological role of the investigated biomarkers is complex. In this study, biomarkers were analysed isoform independently. Soluble receptors may exert antagonistic or synergistic functions of the main cell membrane-bound isoform [41]. It is consequently important to clarify differences between these forms, and when and where they are secreted. The influence of medications and other factors, such as food intake or daily variation, also remain to be investigated. Second, the somewhat unmatched control group and the low number of patients may have influenced the results. Most importantly, however, we show that several markers in the tyrosine kinase domain indeed differ between different disease aetiologies and may have the potential to be used as biomarkers in pulmonary hypertension differentiation. Therefore, multicentre studies are encouraged to further investigate the role of these biomarkers in pulmonary hypertension pathophysiology and assess their possible diagnostic potential.
Conclusions
The present study indicates that plasma RET may be of future use to identify and differentiate PAH patients from other groups of patients with pulmonary hypertension, including CTEPH, systolic or diastolic heart failure with pulmonary hypertension, as well as heart failure without pulmonary hypertension and healthy controls. MERTK, VEGF-A, VEGF-D, PlGF, VEGFR-2, amphiregulin, EGFR, HGF and TGF-α may, in addition to RET, also be involved in the complex nature of pulmonary hypertension pathophysiology, which encourages future international collaborative multicentre studies.
Supplementary material
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
TABLE S1 Multiple comparison between all groups 00037-2019.tableS1 (74.1KB, pdf)
Acknowledgements
We acknowledge the support of the staff at the Hemodynamic Lab, The Section for Heart Failure and Valvular Disease, Skåne University Hospital (Lund, Sweden), the Dept of Clinical Sciences, Cardiology, Lund University (Lund, Sweden) and Olink Bioscience (Uppsala, Sweden) for analysing the plasma samples. We especially thank Anneli Ahlqvist for support in assembling the plasma samples and LCPR registration. We furthermore acknowledge the biobank services and retrieval of blood samples from the LCPR performed at Labmedicine Skåne, University and Regional Laboratories, Region Skåne, Sweden.
Footnotes
This article has supplementary material available from openres.ersjournals.com
Support statement: The work was supported by unrestricted research grants from the Anna-Lisa and Sven-Erik Lundgren Foundation, the Swedish Society of Pulmonary Hypertension, and Actelion Pharmaceuticals Sweden AB. The funding organisations played no role in the collection, analysis or interpretation of the data and had no right to restrict the publishing of the manuscript.
Conflict of interest: J. Säleby reports grants from the Swedish Society of Pulmonary Hypertension on behalf of GlaxoSmithKline and lecture fees from Actelion, outside the submitted work.
Conflict of interest: H. Bouzina reports an unrestricted research grant from Actelion during the conduct of the study; and speakers fees from Actelion, grants from the Swedish Society of Pulmonary Hypertension on behalf of GlaxoSmithKline and nonfinancial support from GlaxoSmithKline, outside the submitted work.
Conflict of interest: S. Ahmed has nothing to disclose.
Conflict of interest: J. Lundgren reports personal lecture fees from Actelion Pharmaceuticals Sweden AB, outside the submitted work.
Conflict of interest: G. Rådegran reports an unrestricted research grant from Actelion, during the conduct of the study; and speaker fees from Actelion and Orion Pharma, advisory boards for Actelion and MSD, and that he was a principal investigator for Actelion, GlaxoSmithKline, Bayer and Novartis, outside the submitted work.
References
- 1.Galiè N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Respir J 2015; 46: 903–975. doi:10.1183/13993003.01032-2015 [DOI] [PubMed] [Google Scholar]
- 2.Simonneau G, Montani D, Celermajer DS, et al. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J 2019; 53: 1801913 10.1183/13993003.01913-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown LM, Chen H, Halpern S, et al. Delay in recognition of pulmonary arterial hypertension: factors identified from the REVEAL Registry. Chest 2011; 140: 19–26. doi:10.1378/chest.10-1166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benza RL, Miller DP, Barst RJ, et al. An evaluation of long-term survival from time of diagnosis in pulmonary arterial hypertension from the REVEAL Registry. Chest 2012; 142: 448–456. doi:10.1378/chest.11-1460 [DOI] [PubMed] [Google Scholar]
- 5.Rådegran G, Kjellström B, Ekmehag B, et al. Characteristics and survival of adult Swedish PAH and CTEPH patients 2000–2014. Scand Cardiovasc J 2016; 50: 243–250. doi:10.1080/14017431.2016.1185532 [DOI] [PubMed] [Google Scholar]
- 6.Pietra GG, Capron F, Stewart S, et al. Pathologic assessment of vasculopathies in pulmonary hypertension. J Am Coll Cardiol 2004; 43: 12 Suppl. S, 25S–32S. doi:10.1016/j.jacc.2004.02.033 [DOI] [PubMed] [Google Scholar]
- 7.Rubin LJ. Primary pulmonary hypertension. N Engl J Med 1997; 336: 111–117. doi:10.1056/NEJM199701093360207 [DOI] [PubMed] [Google Scholar]
- 8.Fedullo PF, Auger WR, Kerr KM, et al. Chronic thromboembolic pulmonary hypertension. N Engl J Med 2001; 345: 1465–1472. doi:10.1056/NEJMra010902 [DOI] [PubMed] [Google Scholar]
- 9.Lang IM, Pesavento R, Bonderman D, et al. Risk factors and basic mechanisms of chronic thromboembolic pulmonary hypertension: a current understanding. Eur Respir J 2013; 41: 462–468. doi:10.1183/09031936.00049312 [DOI] [PubMed] [Google Scholar]
- 10.Lundgren J, Radegran G. Pathophysiology and potential treatments of pulmonary hypertension due to systolic left heart failure. Acta Physiol 2014; 211: 314–333. doi:10.1111/apha.12295 [DOI] [PubMed] [Google Scholar]
- 11.Vachiery JL, Adir Y, Barbera JA, et al. Pulmonary hypertension due to left heart diseases. J Am Coll Cardiol 2013; 62: Suppl. 25, D100–D108. doi:10.1016/j.jacc.2013.10.033 [DOI] [PubMed] [Google Scholar]
- 12.Lettieri CJ, Nathan SD, Barnett SD, et al. Prevalence and outcomes of pulmonary arterial hypertension in advanced idiopathic pulmonary fibrosis. Chest 2006; 129: 746–752. doi:10.1378/chest.129.3.746 [DOI] [PubMed] [Google Scholar]
- 13.Oswald-Mammosser M, Weitzenblum E, Quoix E, et al. Prognostic factors in COPD patients receiving long-term oxygen therapy. Importance of pulmonary artery pressure. Chest 1995; 107: 1193–1198. doi:10.1378/chest.107.5.1193 [DOI] [PubMed] [Google Scholar]
- 14.Gomberg-Maitland M, Bull TM, Saggar R, et al. New trial designs and potential therapies for pulmonary artery hypertension. J Am Coll Cardiol 2013; 62: Suppl. 25, D82–D91. doi:10.1016/j.jacc.2013.10.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Godinas L, Guignabert C, Seferian A, et al. Tyrosine kinase inhibitors in pulmonary arterial hypertension: a double-edge sword? Semin Respir Crit Care Med 2013; 34: 714–724. doi:10.1055/s-0033-1356494 [DOI] [PubMed] [Google Scholar]
- 16.Batchu SN, Korshunov VA. Novel tyrosine kinase signaling pathways: implications in vascular remodeling. Curr Opin Nephrol Hypertens 2012; 21: 122–127. doi:10.1097/MNH.0b013e3283503ce9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoeper MM, Barst RJ, Bourge RC, et al. Imatinib mesylate as add-on therapy for pulmonary arterial hypertension: results of the randomized IMPRES study. Circulation 2013; 127: 1128–1138. doi:10.1161/CIRCULATIONAHA.112.000765 [DOI] [PubMed] [Google Scholar]
- 18.Tuder RM, Chacon M, Alger L, et al. Expression of angiogenesis-related molecules in plexiform lesions in severe pulmonary hypertension: evidence for a process of disordered angiogenesis. J Pathol 2001; 195: 367–374. doi:10.1002/path.953 [DOI] [PubMed] [Google Scholar]
- 19.Saleby J, Bouzina H, Lundgren J, et al. Angiogenic and inflammatory biomarkers in the differentiation of pulmonary hypertension. Scand Cardiovasc J 2017; 51: 261–270. doi:10.1080/14017431.2017.1359419 [DOI] [PubMed] [Google Scholar]
- 20.Kumpers P, Nickel N, Lukasz A, et al. Circulating angiopoietins in idiopathic pulmonary arterial hypertension. Eur Heart J 2010; 31: 2291–2300. doi:10.1093/eurheartj/ehq226 [DOI] [PubMed] [Google Scholar]
- 21.Selimovic N, Bergh CH, Andersson B, et al. Growth factors and interleukin-6 across the lung circulation in pulmonary hypertension. Eur Respir J 2009; 34: 662–668. doi:10.1183/09031936.00174908 [DOI] [PubMed] [Google Scholar]
- 22.Partovian C, Adnot S, Eddahibi S, et al. Heart and lung VEGF mRNA expression in rats with monocrotaline- or hypoxia-induced pulmonary hypertension. Am J Physiol 1998; 275: H1948–H1956. [DOI] [PubMed] [Google Scholar]
- 23.Campbell AI, Zhao Y, Sandhu R, et al. Cell-based gene transfer of vascular endothelial growth factor attenuates monocrotaline-induced pulmonary hypertension. Circulation 2001; 104: 2242–2248. doi:10.1161/hc4201.097838 [DOI] [PubMed] [Google Scholar]
- 24.Jankov RP, Kantores C, Belcastro R, et al. A role for platelet-derived growth factor beta-receptor in a newborn rat model of endothelin-mediated pulmonary vascular remodeling. Am J Physiol Lung Cell Mol Physiol 2005; 288: L1162–L1170. doi:10.1152/ajplung.00180.2004 [DOI] [PubMed] [Google Scholar]
- 25.Perros F, Montani D, Dorfmuller P, et al. Platelet-derived growth factor expression and function in idiopathic pulmonary arterial hypertension. Am J Respir Crit Care Med 2008; 178: 81–88. doi:10.1164/rccm.200707-1037OC [DOI] [PubMed] [Google Scholar]
- 26.Assarsson E, Lundberg M, Holmquist G, et al. Homogenous 96-plex PEA immunoassay exhibiting high sensitivity, specificity, and excellent scalability. PLoS One 2014; 9: e95192 doi:10.1371/journal.pone.0095192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bouzina H, Rådegran G. Low plasma stem cell factor combined with high transforming growth factor α identify high risk patients in pulmonary arterial hypertension. ERJ Open Res 2018; 4: 00035-2018 doi:10.1183/23120541.00035-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ibanez CF. Structure and physiology of the RET receptor tyrosine kinase. Cold Spring Harb Perspect Biol 2013; 5: a009134 doi:10.1101/cshperspect.a009134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arighi E, Borrello MG, Sariola H. RET tyrosine kinase signaling in development and cancer. Cytokine Growth Factor Rev 2005; 16: 441–467. doi:10.1016/j.cytogfr.2005.05.010 [DOI] [PubMed] [Google Scholar]
- 30.Partovian C, Adnot S, Raffestin B, et al. Adenovirus-mediated lung vascular endothelial growth factor overexpression protects against hypoxic pulmonary hypertension in rats. Am J Respir Cell Mol Biol 2000; 23: 762–771. doi:10.1165/ajrcmb.23.6.4106 [DOI] [PubMed] [Google Scholar]
- 31.Le Cras TD, Hardie WD, Fagan K, et al. Disrupted pulmonary vascular development and pulmonary hypertension in transgenic mice overexpressing transforming growth factor-α. Am J Physiol Lung Cell Mol Physiol 2003; 285: L1046–L1L54. doi:10.1152/ajplung.00045.2003 [DOI] [PubMed] [Google Scholar]
- 32.Kato M, Inazu T, Kawai Y, et al. Amphiregulin is a potent mitogen for the vascular smooth muscle cell line, A7r5. Biochem Biophys Res Commun 2003; 301: 1109–1115. doi:10.1016/S0006-291X(03)00093-7 [DOI] [PubMed] [Google Scholar]
- 33.Dransfield I, Zagorska A, Lew ED, et al. Mer receptor tyrosine kinase mediates both tethering and phagocytosis of apoptotic cells. Cell Death Dis 2015; 6: e1646 doi:10.1038/cddis.2015.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zagórska A, Través PG, Lew ED, et al. Diversification of TAM receptor tyrosine kinase function. Nat Immunol 2014; 15: 920 doi:10.1038/ni.2986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Thorp E, Cui D, Schrijvers DM, et al. Mertk receptor mutation reduces efferocytosis efficiency and promotes apoptotic cell accumulation and plaque necrosis in atherosclerotic lesions of Apoe−/− mice. Arterioscler Thromb Vasc Biol 2008; 28: 1421–1428. doi:10.1161/ATVBAHA.108.167197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marsch E, Theelen TL, Demandt JA, et al. Reversal of hypoxia in murine atherosclerosis prevents necrotic core expansion by enhancing efferocytosis. Arterioscler Thromb Vasc Biol 2014; 34: 2545–2553. doi:10.1161/ATVBAHA.114.304023 [DOI] [PubMed] [Google Scholar]
- 37.Munoz LE, Lauber K, Schiller M, et al. The role of defective clearance of apoptotic cells in systemic autoimmunity. Nat Rev Rheumatol 2010; 6: 280–289. doi:10.1038/nrrheum.2010.46 [DOI] [PubMed] [Google Scholar]
- 38.Groth A, Vrugt B, Brock M, et al. Inflammatory cytokines in pulmonary hypertension. Respir Res 2014; 15: 47 doi:10.1186/1465-9921-15-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liang M, Pang Y, Zhang S, et al. Utility of hepatocyte growth factor as a biomarker for early diagnosis of pulmonary artery hypertension. Mol Diagn Ther 2016; 20: 463–468. doi:10.1007/s40291-016-0214-3 [DOI] [PubMed] [Google Scholar]
- 40.Hiramine K, Sata N, Ido A, et al. Hepatocyte growth factor improves the survival of rats with pulmonary arterial hypertension via the amelioration of pulmonary hemodynamics. Int J Mol Med 2011; 27: 497–502. [DOI] [PubMed] [Google Scholar]
- 41.Heaney M, Golde D. Soluble cytokine receptors. Blood 1996; 87: 847–857. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
TABLE S1 Multiple comparison between all groups 00037-2019.tableS1 (74.1KB, pdf)