Abstract
Background:
Designing cancer prevention programs needs information on knowledge, attitude, and practice of the community. Unfortunately, this information is not available in Iran.
Materials and Methods:
We developed a questionnaire (NUTCANKAPQ) to assess the knowledge, attitude, and practice of Iranian women regarding cancer prevention dietary habits. We recruited women who had referred to public health-care centers in Tehran, Iran. To assess validity, we applied face, content, and construct validity methods. We performed test–retest approaches to assess reliability, and internal consistency of the questionnaire was assessed through Cronbach's alpha and intraclass correlation coefficients (ICCs).
Results:
Qualitative content validity was carried out by an expert panel, and internal consistency was deemed satisfactory (Cronbach's alpha, >0.6). We also observed high reliability in the questionnaire (ICC = 0.85). The mean (± standard deviation) scores for knowledge, attitude, and practice of study participants were 28.3 (±14.1), 67.1 (±18.9), and 53.7 (±8.3), respectively. The result of exploratory factor analysis, Kaiser–Meyer–Olkin (KMO), implied that the model was reasonably fit (KMO > 0.6). The final questionnaire included seventy items.
Conclusion:
NUTCANKAPQ is a valid and reliable tool for the assessment of cancer-related nutrition knowledge, attitude, and practice among the Iranian population. Application of NUTCANKAPQ may provide important clues for policy-making and improvement of cancer prevention programs among the Iranian population.
Keywords: Attitude, knowledge, neoplasms, nutrition, practice, questionnaire, reproducibility, surveys, validity
INTRODUCTION
Cancer is the second leading cause of death worldwide.[1] In 2018, 18,078,957 patients were diagnosed with various cancer types, and 9,555,027 patients died as a result of cancer across the world.[2] The age-standardized incidence rate of cancer was 141.6 in 100,000 among Iranians in 2018, with a total of 110,000 new cases and 55,000 deaths.[3] Similar to other low- and middle-income countries, the incidence of cancer is expected to rise and the number of new cases is predicted to reach 184,481 by 2035.[4] Based on previous studies, environmental and behavioral risk factors such as tobacco smoking, sedentary lifestyle, unhealthy diet, obesity, alcohol consumption, and infectious agents are responsible for more than 40% of cancer cases and deaths, which means that a staggering number of cancer cases could be avoided if these risk factors were somehow removed.[5] Although it appears improbable, and likely impossible to eliminate exposure to all environmental risk factors, this target can be partially achieved through increasing knowledge on cancer in the general population, particularly in low- and middle-income countries.[6] Cancer knowledge is a key element of cancer control programs, leading to both risk reduction and early diagnosis of cancer.[7]
Nutritional behavior, being one of the most important modifiable risk factors for cancer, is strongly associated with people's knowledge of and attitude toward a healthy diet. It has been depicted that increased nutritional knowledge could lead to a decrease in cancer incidence through a change in the dietary behaviors of target groups.[8,9] However, these behaviors are also associated with many other factors such as race, tradition, cost, constraints, risk perceptions, and attitude toward a healthy diet. Increasing nutrition knowledge will only be effective when the prerequisites are available, and people perceive themselves as being at risk. In such circumstances, this knowledge can increase the possibility of adoption of a healthy diet, therefore increasing overall health. Thus, it is important to consider all three domains (knowledge, attitude, and practice) for successful cancer prevention. Even though previous studies have attempted to develop cancer-specific nutrition questionnaires in other parts of the world,[10,11] no such study was found in Iran.
Iran is a developing country that has faced rapid changes during the past decades, such as urbanization and increased adoption of Western dietary habits. These changes have resulted in obesity and unhealthy diet among Iranian young adults.[12] Because the prevalence of both cancer and unhealthy diet is on the rise among the Iranian population, assessing cancer-related nutrition knowledge, attitude, and practice could be advantageous for both cancer control and promoting healthy diet.[13]
To our knowledge, a valid tool to assess the association between nutritional knowledge, food intake, and cancer is scarce in Iran.[14] In this study, we aimed to validate a questionnaire to evaluate the nutrition knowledge, attitude, and practice of Iranian women in regard to cancer.
MATERIALS AND METHODS
Development of questionnaire
To generate the dietary questions, we used three approaches. First, we used questions that had frequently been raised during several public education programs about dietary habits and cancer prevention that had been held in Tehran.
Second, a comprehensive literature review was done to gather questionnaires and educational materials used in different countries. Finally, we reviewed a series of leaflets and pamphlets that had been used in educational programs at public health-care centers in Tehran.[7,10,15,16,17,18,19,20] In this questionnaire, we assessed knowledge, attitude, and practice in terms of nutritional causes of cancer including high body mass index (BMI), food groups (foods that increased and decreased cancer risk), micro and macronutrients (regarding their high and low intake), hazardous cooking methods, safe preservation of foods, safe cooking instruments, reading and understanding food labels, and supplement consumption.
The knowledge domain consisted of procedural (e.g., “high intake of fruit and vegetables prevents cancer”) and declarative (e.g., “the food pyramid advises a daily intake of four portions of cereals”) nutrition knowledge questions.
To design the attitude questions, we used the health belief model, which is one of the most recommended models in increasing the impact of educational programs.[21] This model was developed to characterize a disease prevention model.[22] The components of this model are susceptibility, severity, benefits, self-efficacy, barriers, and actions. Finally, the practice domain asked questions related to consumption of local foods, beverages, and additives (healthy and unhealthy) in participants. Other aspects of dietary habits such as preparation and preservation of foods, cooking instruments, food labeling, and supplements were also included in the practice dimension.
The final version of the nutrition-related cancer prevention knowledge, attitude, and practice questionnaire (NUTCANKAP) contained 78 questions, including six demographic questions, i.e., name, phone number, age, weight and height, education level, and marital status; 15 questions on socioeconomic status; 2 questions on cues of action; 11 questions on knowledge; 27 questions on attitude (i.e., 11 questions on perceived susceptibility and four questions each regarding perceived severity, perceived benefit, perceived self-efficacy, and perceived barriers); and finally 17 questions on practice measurements. The NUTCANKAP questionnaire is available on the website of the Cancer Research Center of the Cancer Institute of Iran (http://cri.tums.ac.ir/crc).
Validity assessment
We used content, face, and construct validity methods to assess the questionnaire validity. Qualitative content validity was carried out by an expert panel including three nutritionists, one epidemiologist, and one health promotion expert. In this step, the primary questionnaire was reviewed and commented on by an expert panel. Irrelevant items were removed based on expert opinion, and alterations were made to the remaining items to make them more precise and to enhance clarity. In the next step, to assess face validity, we asked 29 women among the study population to comment on whether or not the concepts of the questionnaire were clear and understandable.
Regarding construct validity, the NUTCANKAP questionnaire was completed by 189 women in different age groups and education levels. Participants were recruited from women who referred to public health centers in Tehran via convenience sampling. The design and aim of the study were explained, and oral informed consent was obtained. We performed exploratory factor analysis (EFA) to find the best place for each item in its associated domain. The questionnaire was self-administered under the supervision of an interviewer, and the maximum time for completion was 45 min.
Scoring method
Correct responses were given a score of one, and incorrect responses, don't know answers, or blanks were attributed a score of zero. The total raw scores of “nutritional knowledge” ranged from 0 to 11, which were proportionately transformed to 0–100. The “attitude” section was evaluated by a Likert scale ranging from 1 as least desirable to 5 as most desirable or vice versa. The total raw scores of attitude ranged from 27 to 135, which were proportionately transformed to 0–100. Finally, in the items related to the practice domain, correct choices of food received a score of one, and incorrect or blank responses were regarded as zero. We also scored 15 multiple-choice questions (sure, somewhat, not much, and not necessary) from 1 to 4. The total raw score of this section ranged from 0 to 16, which was proportionately transformed to 0–100. To construct the final questionnaire, we conducted an item analysis and discarded those items that were answered correctly by fewer than 20% or more than 80% of study participants.[15]
Reliability assessment
To assess the questionnaire's reliability, we measured internal consistency through calculation of Cronbach's alpha for items which were on Likert scale (attitude dimension). In addition, as questions of knowledge and practice dimensions were on binary scale, Kuder–Richardson 20 (KR-20) was estimated as a measure of internal consistency for knowledge and practice dimensions. In internal consistency, we explore how each question is consistent within each domain of the questionnaire. Cronbach's alpha and KR-20 values range from 0 to 1, and a score above 0.7 is generally regarded as acceptable.[23]
Test–retest reliability
We used the test–retest approach to assess the reliability and reproducibility of our findings, which is repeating an identical test on two separate occasions. In this step, the questionnaire was completed twice in a 2-week period by 29 women. The reliability coefficient is the correlation between the scores obtained by the same persons on two different occasions.[24] Higher values of intraclass correlation coefficient (ICC) indicate greater reliability.
Statistical analysis
Cronbach's alpha and ICC were used as a measure of internal consistency and reliability. We also assessed construct validity to determine the final questions of the NUTCANKAP questionnaire. EFA and Kaiser–Meyer–Olkin (KMO) were used to evaluate model adequacy. Moreover, we performed principal component extraction and varimax rotation to decide on the remaining questions of the questionnaire based on factor loading values. We regarded factor loading values >0.3 as acceptable. All statistical analyses were performed using Stata 14.1, StataCorp LP, College Station, Texas, USA.
RESULTS
A total of 189 adult women aged 24–69 (57.4 ± 129.1) years and with a BMI average of 27.6 ± 4.73 participated in the current study. More than 39% of study participants were in the age group of 40–49 years, and participants were mostly married (87.9%). More than half of the participants had a diploma, and the percentage of overweight persons and obesity was 63% [Table 1]. The final NUTCANKAP included seventy items (with demographic questions).
Table 1.
Demographic characteristics of the study participants (n=189)
| Variable | n (%) |
|---|---|
| Age, years (24-69) | |
| <30 | 12 (7.06) |
| 30-39 | 37 (21.76) |
| 40-49 | 67 (39.41) |
| 50-59 | 42 (24.71) |
| 60-69 | 12 (7.06) |
| Marital status | |
| Single | 14 (8.05) |
| Married | 153 (87.93) |
| Divorced | 5 (2.87) |
| Widowed | 2 (1.15) |
| Educational level | |
| Primary school | 8 (5.19) |
| Middle school, high school, and diploma | 99 (64.28) |
| Bachelor’s degree | 32 (20.78) |
| Postgraduate or higher | 15 (9.74) |
| BMI (kg/m2) | |
| Underweight (<18.5) | 4 (2.44) |
| Normal weight (18.5-24.9) | 55 (33.54) |
| Overweight (25.0-29.9) | 63 (38.41) |
| Obese Class I (30.0-39.9) | 41 (25.00) |
| Obese Class II (≥40.0) | 1 (0.61) |
BMI=Body mass index
As presented in Table 2, the Cronbach's alpha score for attitude domain was 0.80, and KR-20 for knowledge and practice domains was 0.82 and 0.75, respectively. The result of EFA, KMO, implied that the model was reasonably fit (KMO >0.6), and sphericity assumption in each domain was confirmed by Bartle's test (P < 0.001). Furthermore, Table 3 depicts the results of factor analysis and factor loading values for each of the domains of the questionnaire. Items with factor loadings <0.3 were deleted. For knowledge, attitude, and practice domains, a total of four, one, and four components were extracted, respectively (eigenvalue >1). The extracted factors of knowledge were named general knowledge (i), nutrition knowledge (ii), bodyweight knowledge (iii), and healthy food knowledge (iv). The names of extracted factors for practice were food choice (i), oil and additive choice (ii), fruit and vegetables choice (iii), and cooking methods choice (iv). Because questions regarding cues of action decreased the overall Cronbach's alpha score, we decided to delete these questions.
Table 2.
Internal consistency and intraclass correlation coefficient of main domains of knowledge, attitude, and practice questionnaire
| Domains | Internal consistency | ICC | 95% CI for ICC |
|---|---|---|---|
| Knowledgea | 0.82 | 0.87 | 0.72-0.94 |
| Attitudeb | 0.80 | 0.83 | 0.65-0.92 |
| Practicea | 0.75 | 0.87 | 0.72-0.94 |
aKR-20 as internal consistency; bCronbach’s alpha as internal consistency. KR-20=Kuder-Richardson 20; ICC=Intraclass correlation coefficient; CI=Confidence interval
Table 3.
Factor analysis with principal component extraction using varimax rotation
| KAP questionnaire | Question | Factor loading extracted component with EV >1 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Knowledge | Attitude | Practice | ||||||||
| I | II | III | IV | I | II | III | IV | |||
| Knowledge | Method of weight reduction | 0.80 | - | - | - | - | - | - | - | - |
| Method of cancer prevention | 0.80 | - | - | - | - | - | - | - | - | |
| True or false message | 0.47 | - | - | - | - | - | - | - | - | |
| Bad fat | - | 0.80 | - | - | - | - | - | - | - | |
| Food group | - | 0.72 | - | - | - | - | - | - | - | |
| Food with higher fiber | - | 0.60 | - | - | - | - | - | - | - | |
| Factor affecting body weight | - | - | 0.80 | - | - | - | - | - | - | |
| Self-imaging | - | - | 0.50 | - | - | - | - | - | - | |
| Range of BMI for adults | - | - | - | 0.86 | - | - | - | - | - | |
| Anti-cancer foods | - | - | - | 0.48 | - | - | - | - | - | |
| KMO, χ2, P | 0.76, 153, <0.001 | |||||||||
| Attitude | Perceived susceptibility (10 questions) | - | - | - | - | 0.65 | - | - | - | - |
| Perceived severity (4 questions) | - | - | - | - | 0.58 | - | - | - | - | |
| Perceived benefits (4 questions) | - | - | - | - | 0.81 | - | - | - | - | |
| Perceived barriers (4 questions) | - | - | - | - | 0.90 | - | - | - | - | |
| Self-efficacy (4 questions) | - | - | - | - | 0.70 | - | - | - | - | |
| KMO, χ2, P | 0.65, 54, <0.001 | |||||||||
| Practice | Food choice | - | - | - | - | - | 0.76 | - | - | - |
| Beverage choice | - | - | - | - | - | 0.66 | - | - | - | |
| Oil choice | - | - | - | - | - | - | 0.78 | - | - | |
| Additive choice | - | - | - | - | - | - | 0.70 | - | - | |
| Amount of vegetable intake | - | - | - | - | - | - | - | 0.63 | - | |
| Amount of fruit intake | - | - | - | - | - | - | - | 0.60 | - | |
| Choice of side dished | - | - | - | - | - | - | - | 0.59 | - | |
| True or false nutrition practice | - | - | - | - | - | - | - | 0.54 | - | |
| Vegetable cooking methods | - | - | - | - | - | - | - | - | 0.74 | |
| Methods of cooking | - | - | - | - | - | - | - | - | 0.53 | |
| KMO, χ2, P | 0.70, 157, <0.001 | |||||||||
EV=Eigenvalue; BMI=Body mass index; KMO=Kaiser-Meyer-Olkin; KAP=Knowledge, attitude, and practices
The result of test–retest reliability (ICC = 0.85) indicated good questionnaire stability. The mean (± standard deviation) knowledge, attitude, and practice scores and numbers of items in each dimension are presented in Table 4. The practice domain had the highest mean (46.01 ± 16.94), and knowledge had the lowest (28.58 ± 12.06) among the subscales.
Table 4.
Mean standard deviation for cancer-related nutrition knowledge, attitude, and practice of the study population
| Constructs | na | Meanb | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| Knowledge | 11 | 28.58 | 12.06 | 10.59 | 54.97 |
| Attitude | 27 | 38.02 | 13.48 | 19.87 | 58.14 |
| Practice | 17 | 46.01 | 16.94 | 5.49 | 73.37 |
aNumber of questions; bData are presented in 0-100 scale. SD=Standard deviation
We also assessed knowledge, attitude, and practice of study participants by education level. We observed an increase in the mean score of knowledge by increasing education level, which reached a peak in the postgraduate group (mean = 40.6), whereas a downward trend was observed for mean attitude score. The highest mean score of attitude was 71.6, which was observed in the primary education group, and this score continuously decreased until it reached 57.5 among the postgraduate group. We also found a direct association between practice score and level of education. University graduate groups had slightly higher values of practice compared to those with a bachelor's degree (55.8 vs. 53.6) [Figure 1].
Figure 1.
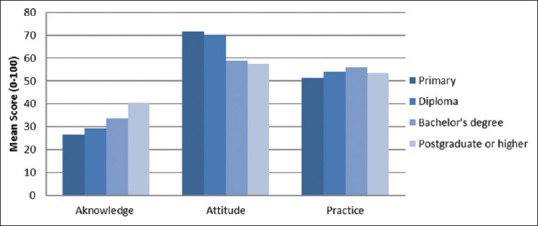
Mean comparison of NUTCANKAP subscales for education
We studied associations between knowledge, attitude, and practice scores and age. According to our findings, the mean score of knowledge and practice was slightly higher among participants who were younger than 30 years (knowledge = 36.4 and practice = 55.8) compared to those who were older than 30 years (knowledge = 35.0 and practice = 53.7). However, it appeared that older groups had slightly higher mean attitude scores than younger groups (64.2 vs. 57.7) [Figure 2].
Figure 2.
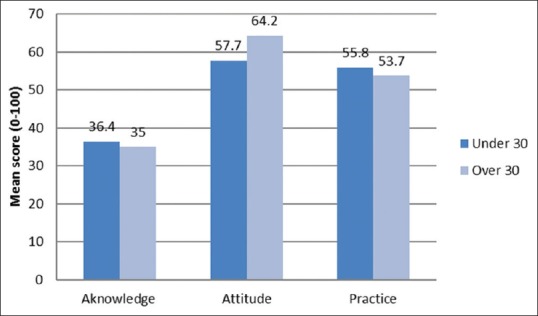
Mean comparison of NUTCANKAP subscales for age
DISCUSSION
The current study was the first attempt to develop and validate a cancer-related nutrition knowledge, attitude, and practice (KAP) questionnaire, among Iranian women. This requires a valid and reliable instrument to execute future health policies. Our findings supported initial validity and reliability of the instrument. Qualitative content validity assessment by experts suggested that the scale had good content validity. The reliability of NUTCANKAP in different constructs was supported by a Cronbach's alpha and KR-20 of >0.60. The results of EFA suggested that four components in knowledge and practice must be removed after pooling items. The overall ICC was 0.85, which suggested good reproducibility.
Nutrition knowledge is in relation to several factors such as education, age, sex, and socioeconomic status.[25] Naturally, knowledge relates to education, and our findings are in agreement with the results of other studies that report that higher education or socioeconomic status is related to higher levels of nutrition knowledge.[25,26,27] In contrast with the knowledge domain, no difference was observed between well-educated and low-educated people in terms of attitude and practice. It seems that although well-educated people have more information about cancer, their perceived risk of cancer is low, which decreases the possibility of their showing preventive activities. This study showed higher scores of knowledge in younger participants. This could be partly explained by the fact that younger people have more access to information, which may result in their being more knowledgeable. On the other hand, people become more worried about disease as they grow older; therefore, their attitude toward cancer changes with increased age. Previous studies reported that KAP scores of people over 30 years were completely different from those under 30 years, which is similar to our results.[25,28] However, the observed differences in the KAP scores of different age groups were not statistically significant.
Based on our findings, there was a lack of nutritional awareness regarding cancer among Iranian women. Because the participants of our study had attended regular classes on healthy diet, we expected them to have high nutritional knowledge. This affected the type of questions used in this tool. We used difficult questions in the knowledge domain, which could have led to low scores in this part. However, our findings were consistent with the results of other studies which depicted poor knowledge regarding the role of nutrition in cancer prevention.[10,14] In general, people performed weakly in the practice domain. It might be that they are unaware of the link between nutrition and disease. For example, one study showed that people had poor knowledge about the link between fruits and vegetables and cancer. On the other hand, people may be unable to translate their knowledge into practice due to barriers such as the higher price of organic/healthy/nutritious foods, lack of available time to prepare foods, the effects of advertising, habits, and because they perceive unhealthy foods as tasting better.[25]
Most nutrition questionnaires have been designed to assess adherence to dietary guidelines, with particular attention toward developed countries.[15,16,18,19,29] Ironically, despite the fact that nutrition problems are greater in low- and middle-income countries, fewer studies have been conducted in these regions.[10,17]
The main limitation of our study is that all of our participants were women; therefore, we cannot generalize its validity to the whole population. However, it is noticeable that women are the main decision-makers regarding food choice, and they are responsible for food preparation in the family. Educational interventions are also generally conducted in female groups. Mothers decide on the dietary patterns of children at an early age and can provide them with a healthy diet. Moreover, children learn nutritional habits from their parents. Several studies have shown that children's dietary habits are similar to that of their parents.[30] Therefore, educating children will result in them acquiring healthier eating habits which they may carry throughout life. The study population was recruited from the south of Tehran and may not be representative of the Iranian population, which is composed of different ethnic groups, cultures, and socioeconomic status. However, because Tehran is the capital city of Iran and includes immigrants from across Iran, it is home to a variety of cultures. We included the common foods and beverages consumed by Iranians in our questionnaire. Although considerations must be taken into account when generalizing results to various provinces, the results can, however, be generalized to the entire country. Unfortunately, our budget did not allow us to conduct a national survey.
The main strength of this study was question design, which incorporated different aspects of cancer-related nutrition and also its novelty in evaluating KAP regarding this matter among the Iranian population. However, the questionnaire is lengthy, which may lead to a reduced response rate. It may be useful to develop a shorter version of the NUTCANKAP questionnaire in the future.
CONCLUSION
This study presents the NUTCANKAP questionnaire, which is a valid and reliable questionnaire developed for the assessment of cancer-related nutrition KAP among the Iranian population. Our results show that population knowledge regarding the role of nutrition in cancer prevention is low, and educational interventions are required to improve it. Using this questionnaire in large- or national-scale surveys could increase the validity of the developed tool and provide policy-makers with important information on how to change dietary habits among the Iranian population.
Financial support and sponsorship
This study was supported by a fund of research from the Cancer Research Center in Tehran University of Medical Science (no. 38349).
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We are grateful to personnel of public health centers which helped us to conduct our study in their sites. Moreover, we should thank our participants who generously allocate their time to our study. The authors would like to thank Maryam Zarrif Yeganeh for her precious advice on the development of the questionnaire. This study was supported by a fund of research from Cancer Research Center in Tehran University of Medical Science (no. 38349).
REFERENCES
- 1.World Health Organization. Cancer: Key Facts. Fact Sheets. World Health Organization; 2018. [Last accessed on 2019 Jan 10]. Available from: https://www.who.int/news-room/fact-sheets/detail/cancer . [Google Scholar]
- 2.The International Agency for Research on Cancer. GLOBOCAN. 2019. [Last accessed on 2019 Jan 30]. Available from: https://gco.iarc.fr/tomorrow/graphic-bar .
- 3.The International Agency for Research on Cancer. GLOBOCAN. 2018. [Last accessed on 2019 Feb 02]. Available from: https://gco.iarc.fr/today/online-analysis-map .
- 4.Mohebbi E, Nahvijou A, Hadji M, Rashidian H, Seyyedsalehi MS, Nemati S. Iran cancer statistics in 2012 and projection of cancer incidence by 2035. Basic Clin Cancer Res. 2017;9:3–22. [Google Scholar]
- 5.Islami F, Goding Sauer A, Miller KD, Siegel RL, Fedewa SA, Jacobs EJ, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin. 2018;68:31–54. doi: 10.3322/caac.21440. [DOI] [PubMed] [Google Scholar]
- 6.Montazeri A, Vahdaninia M, Harirchi I, Harirchi AM, Sajadian A, Khaleghi F, et al. Breast cancer in Iran: Need for greater women awareness of warning signs and effective screening methods. Asia Pac Fam Med. 2008;7:6. doi: 10.1186/1447-056X-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ryan AM, Cushen S, Schellekens H, Bhuachalla EN, Burns L, Kenny U, et al. Poor awareness of risk factors for cancer in Irish adults: Results of a large survey and review of the literature. Oncologist. 2015;20:372–8. doi: 10.1634/theoncologist.2014-0453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De Vriendt T, Matthys C, Verbeke W, Pynaert I, De Henauw S. Determinants of nutrition knowledge in young and middle-aged Belgian women and the association with their dietary behaviour. Appetite. 2009;52:788–92. doi: 10.1016/j.appet.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 9.CR-UK, CancerStats Incidence. UK: Cancer Research; 2011. p. 2014. [Google Scholar]
- 10.Loo JL, Ang YK, Yim HS. Development and validation of a cancer awareness questionnaire for Malaysian undergraduate students of Chinese ethnicity. Asian Pac J Cancer Prev. 2013;14:565–70. doi: 10.7314/apjcp.2013.14.1.565. [DOI] [PubMed] [Google Scholar]
- 11.Petrovici DA, Ritson C. Factors influencing consumer dietary health preventative behaviours. BMC Public Health. 2006;6:222. doi: 10.1186/1471-2458-6-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sadegholvad S, Yeatman H, Omidvar N, Parrish AM, Worsley A. Essential nutrition and food systems components for school curricula: Views from experts in Iran. Iran J Public Health. 2017;46:938–47. [PMC free article] [PubMed] [Google Scholar]
- 13.Sarrafzadegan N, Kelishadi R, Esmaillzadeh A, Mohammadifard N, Rabiei K, Roohafza H, et al. Do lifestyle interventions work in developing countries? Findings from the Isfahan healthy heart program in the Islamic republic of Iran. Bull World Health Organ. 2009;87:39–50. doi: 10.2471/BLT.07.049841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spronk I, Kullen C, Burdon C, O'Connor H. Relationship between nutrition knowledge and dietary intake. Br J Nutr. 2014;111:1713–26. doi: 10.1017/S0007114514000087. [DOI] [PubMed] [Google Scholar]
- 15.Dickson-Spillmann M, Siegrist M, Keller C. Development and validation of a short, consumer-oriented nutrition knowledge questionnaire. Appetite. 2011;56:617–20. doi: 10.1016/j.appet.2011.01.034. [DOI] [PubMed] [Google Scholar]
- 16.Kliemann N, Wardle J, Johnson F, Croker H. Reliability and validity of a revised version of the general nutrition knowledge questionnaire. Eur J Clin Nutr. 2016;70:1174–80. doi: 10.1038/ejcn.2016.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bovell-Benjamin A, Elmubarak E. Diet-nutrition-related cancer prevention knowledge and beliefs of Sudanese in Khartoum: A descriptive study. Open J Prev Med. 2013;3:320. [Google Scholar]
- 18.Gibbs HD, Ellerbeck EF, Gajewski B, Zhang C, Sullivan DK. The nutrition literacy assessment instrument is a valid and reliable measure of nutrition literacy in adults with chronic disease. J Nutr Educ Behav. 2018;50:247–570. doi: 10.1016/j.jneb.2017.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jones AM, Lamp C, Neelon M, Nicholson Y, Schneider C, Wooten Swanson P, et al. Reliability and validity of nutrition knowledge questionnaire for adults. J Nutr Educ Behav. 2015;47:69–74. doi: 10.1016/j.jneb.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 20.Alidosti M, Sharifirad GR, Golshiri P, Azadbakht L, Hasanzadeh A, Hemati Z, et al. An investigation on the effect of gastric cancer education based on health belief model on knowledge, attitude and nutritional practice of housewives. Iran J Nurs Midwifery Res. 2012;17:256–62. [PMC free article] [PubMed] [Google Scholar]
- 21.Sharifirad G, Entezari MH, Kamran A, Azadbakht L. The effectiveness of nutritional education on the knowledge of diabetic patients using the health belief model. J Res Med Sci. 2009;14:1–6. [PMC free article] [PubMed] [Google Scholar]
- 22.Kim HS, Ahn J, No JK. Applying the health belief model to college students' health behavior. Nutr Res Pract. 2012;6:551–8. doi: 10.4162/nrp.2012.6.6.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hair JF, Black WC, Babin BJ, Anderson RE, Tatham RL. Multivariate Data Analysis. Vol. 5. Upper Saddle River, NJ: Prentice Hall; 1998. [Google Scholar]
- 24.Urbina S, Anastasi A. Study Guide [to] Psychological Testing. 7th ed. New York: Macmillan; 1997. [Google Scholar]
- 25.Parmenter K, Waller J, Wardle J. Demographic variation in nutrition knowledge in England. Health Educ Res. 2000;15:163–74. doi: 10.1093/her/15.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Worsley A. Nutrition knowledge and food consumption: Can nutrition knowledge change food behaviour? Asia Pac J Clin Nutr. 2002;11(Suppl 3):S579–85. doi: 10.1046/j.1440-6047.11.supp3.7.x. [DOI] [PubMed] [Google Scholar]
- 27.Dallongeville J, Marécaux N, Cottel D, Bingham A, Amouyel P. Association between nutrition knowledge and nutritional intake in middle-aged men from Northern France. Public Health Nutr. 2001;4:27–33. doi: 10.1079/phn200052. [DOI] [PubMed] [Google Scholar]
- 28.Kung AW, Lee KK. Knowledge of vitamin D and perceptions and attitudes toward sunlight among Chinese middle-aged and elderly women: A population survey in Hong Kong. BMC Public Health. 2006;6:226. doi: 10.1186/1471-2458-6-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mötteli S, Barbey J, Keller C, Bucher T, Siegrist M. Measuring practical knowledge about balanced meals: Development and validation of the brief PKB-7 scale. Eur J Clin Nutr. 2016;70:505–10. doi: 10.1038/ejcn.2015.173. [DOI] [PubMed] [Google Scholar]
- 30.Alderman H, Headey DD. How important is parental education for child nutrition? World Dev. 2017;94:448–64. doi: 10.1016/j.worlddev.2017.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


