Abstract
Objectives
Medical residents can play key roles in improving health care quality by speaking up and giving suggestions for improvements. However, previous research on speaking up by medical residents has shown that speaking up is difficult for residents. This study explored: (i) whether two main aspects of medical residents’ work context (job control and supervisor support) are associated with speaking up by medical residents, and (ii) whether these associations differ between in‐hospital and out‐of‐hospital settings.
Methods
Speaking up was operationalised and measured as voice behaviour. Structural equation modelling using a cross‐sectional survey design was used to identify and test factors pertaining to speaking up and to compare hospital settings.
Results
A total of 499 medical residents in the Netherlands participated in the study. Correlational analysis showed significant positive associations between each of support and control, and voice behaviour. The authors assumed that the associations between support and control, and voice behaviour would be partially mediated by engagement. This partial mediation model fitted the data best, but showed no association between support and voice. However, multi‐group analysis showed that for residents in hospital settings, support is associated with voice behaviour. For residents outside hospital settings, control is more important. Engagement mediated the effects of control and support outside hospital settings, but not within the hospital.
Conclusions
This study shows that in order to enable medical residents to share their suggestions for improvement, it is beneficial to invest in supportive supervision and to increase their sense of control. Boosting medical residents’ support would be most effective in hospital settings, whereas in other health care organisations it would be more effective to focus on job control.
Short abstract
Job control and supervisor support are identified through this research as resources associated with residents “speaking up” and making suggestions for change, but the importance of each may depend on the setting in which residents work.
Introduction
In health care organisations it is important that employees at all levels speak up and express their ideas on maintaining or increasing the quality of health care.1, 2 This is especially relevant for medical residents because they work at the frontline of patient care, in the context of which they experience and see both good and bad practice.3, 4, 5 Resident rotations allow them to visit many different departments, in which they can take a fresh look at work processes. As well as improving the quality of care, speaking up can lead to increased feelings of control over one's work, which can, in turn, lead to higher levels of well‐being.6 Further, the proactive sharing of suggestions for change is an important component of postgraduate medical education programmes as it is integrated into medical roles such as those of medical leadership and health advocacy.7, 8, 9 However, proactively speaking up about key points for improvement is not easy. It is considered to be ‘extra‐role behaviour’, which means that it goes beyond what is expected of employees and requires sufficient amounts of time and energy, both of which are scarce for residents.3, 10, 11 Moreover, employees who speak up can be viewed as tiring or strenuous, neither of which is favourable for residents.12 Thus, the benefits of speaking up are not self‐evident, especially not in the traditionally authoritarian health care context.13, 14, 15, 16 The purpose of this study is to identify and test which factors are associated with speaking up by medical residents.
Speaking up by medical residents
In the social sciences, speaking up in order to exchange ideas, information or concerns that may benefit the organisation is often referred to as ‘voice behaviour’.1, 12, 17, 18, 19, 20 Three types of voice can be distinguished: the suggestion‐focused, the problem‐focused and the opinion‐focused voice.1, 21 Most research on speaking up by medical residents stems from the quality and safety literature, it describes speaking up with an expected preventive effect and refers to the problem‐focused voice. This voice makes expressions of concern about work practices, incidents or behaviours that can be harmful to the organisation, such as in speaking up about (un)professional behaviour, (hand) hygiene, ethical issues and risky or deficient actions on the part of medical staff.14, 15, 18, 22 In this study, we address a different type of speaking up, namely the use of the ‘suggestion‐focused voice’, which refers to the proactive communication of suggestions or ideas that might improve current work practices. Examples include the articulation of suggestions for changes in existing inefficient work routines, the pointing out of redundancies in administrative tasks and suggestions for the effective organisation of time, space and resources.1
Combining findings on speaking up from other professional fields with findings from research on the problem‐focused voice in medical residents, we argue that two basic considerations are important to medical residents who may wish to speak up and make suggestions for change. These concern: (i) whether it is safe to speak up (high support), and (ii) whether speaking up is likely to be effective (high control).1, 12, 14, 15, 16, 17, 22, 23 This is in line with well‐known behavioural models, such as the Job Demand–Control (–Support) (JDCS) Model, which argue that in highly demanding job contexts, high support and high perceived control over one's behaviour will lead to activation‐related outcomes such as motivation, learning and performance.6, 24, 25, 26, 27
Is it safe to speak up?
The social environment exerts a strong influence on a person's intentions and actions.28 A meta‐analysis on proactivity confirmed that social support is a major antecedent of proactive behaviour.17, 29 The receipt of support from peers or supervisors signals that an individual and his or her actions are accepted and valued.13, 30 We expect this relationship to be especially important in the medical context because of the close working relationships between residents and their supervisors. Thus, we expect supervisor support and speaking up to be positively associated (Hypothesis 1).
Is it effective to speak up?
Job control is also an important job characteristic in the literature on proactive behaviour and is associated with increased feelings of responsibility.13, 17 When employees feel control over situations, particularly if they feel they can influence work outcomes, their personal initiative may be increased.13 For residents, job control might refer to being able to influence current work routines. Therefore, we expect to find a positive association between job control and speaking up (Hypothesis 2).
The mediating role of work engagement
Work engagement is a ‘positive, fulfilling, work‐related state of mind that is characterised by vigour, dedication and absorption’.31, 32, 33, 34, 35 It is often studied as a form of well‐being. Similarly to speaking up, work engagement is contingent upon the presence of job resources such as control and support, but it also affects behaviour and performance at work.32 Work engagement may thus mediate the associations between job control, support and speaking up. Therefore, we expect that the effects of support and control on speaking up are at least partly mediated through engagement (Hypothesis 3).31
The influence of organisational context
Research on work behaviours in residents, such as burnout, engagement and workaholism, predominantly focuses on hospital residents. Little is known about residents who work in the settings of other health care organisations, such as in the public health sector.36, 37, 38 We hypothesise that there are cultural and contextual differences related to safety and support between work contexts within and outside hospital settings. Consequently, we explore whether the studied relationships are different for residents who work in hospital settings compared with residents outside hospital settings.
In summary, this study aims to explore whether two main aspects of medical residents’ work context, job control and supervisor support, are associated with speaking up by medical residents. Moreover, we examine whether these associations are mediated by residents’ work engagement. Figure 1 represents the hypothesised research model (M1). This paper will test the hypothesised model using structural equation modelling (SEM). In SEM, a researcher specifies a model based on existing theory and then tests this model by simultaneously analysing the entire system of relationships amongst the study variables. When doing so, the researcher analyses the extent to which the model is consistent with the data (i.e. its goodness‐of‐fit, as expressed in fit indices).39
Figure 1.
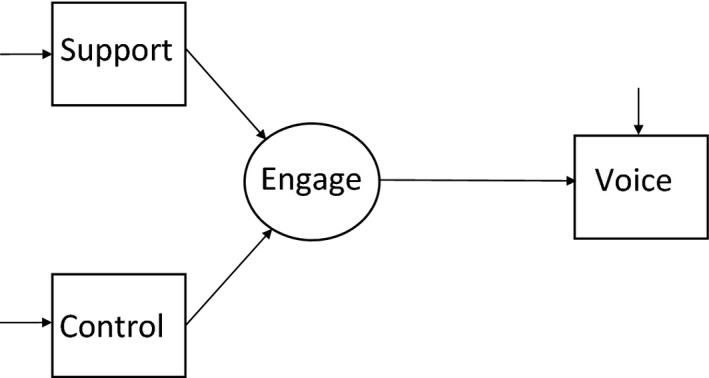
Full mediation model (M1) for the associations between supervisor support, job control, work engagement and voice behaviour
Methods
Design and participants
We tested the hypothesised model using a cross‐sectional survey design. The survey was distributed amongst residents in the Netherlands during March–May 2018. Participants were approached by means of newsletters, direct e‐mails, links in learning environments and social media. Of the 580 respondents, 81 cases were deleted for reasons of (partly) missing data. Of the remaining 499 participants, 70% were female. The mean ± standard deviation (SD) age of the sample was 33 ± 6.1 years. For the multi‐group analysis, respondents were assigned to an in‐ or out‐of‐hospital group, based on their current positions (Table 1). Of the respondents, 299 currently worked in hospital settings and 200 worked in other health care organisations such as mental health care centres, public health centres and occupational health agencies.
Table 1.
Characteristics of residents (n = 499) working in or outside hospital settings
| Residents working in hospital settings, n | Residents working outside hospital settings, n | |
|---|---|---|
| All residents | 299 | 200 |
| Specialty type* | ||
| Cluster 1: general physicians, elderly care physicians, physicians for patients with learning disabilities | 2 | 4 |
| Cluster 2: hospital specialties | 282 | 53 |
| Cluster 3: public health physicians | – | 142 |
| Missing data on specialty training programme | 15 | 1 |
| Current organisation | ||
| General affiliated teaching hospital | 124 | |
| Academic medical centre | 174 | |
| Other in‐hospital setting | 1 | |
| Mental health centre | 50 | |
| Public health centre | 70 | |
| Nursing home | 4 | |
| Employee service agency | 18 | |
| Occupational health agency | 16 | |
| Centre for youth and development | 7 | |
| Rehabilitation centre | 3 | |
| Other (e.g. politics, insurance company, commercial business) | 32 | |
In the Netherlands, residents are divided into three clusters. Cluster 1 represents residency training programmes for general physicians, elderly care physicians and physicians for patients with intellectual disabilities. Cluster 2 covers residency programmes for hospital physicians such as surgeons, neurologists, paediatricians, radiologists etc. Cluster 3 represents residency training programmes for public health physicians.
As we did not know how many potential participants had been reached by our efforts, it was impossible to compute a response rate. However, our sample included 5% of the total population of residents in the Netherlands. To account for response bias, we compared our participant group with the general population of residents in the Netherlands for age, gender and organisation type. Of the respondents, 60% worked in hospital settings and 40% worked outside the hospital (e.g. in community health centres or mental health care facilities). This equates to the distribution of residents across in‐ and out‐of‐hospital settings in the Netherlands (60% and 40%, respectively).40 Moreover, we checked whether the means and SDs of work engagement in our sample were comparable with those of a large study (n = 2114; response rate: 41%) on work engagement in Dutch medical residents38 and found a strong degree of similarity. Thus, we believe that our sample is largely representative for the topic of work engagement in the total population of residents in the Netherlands.
This study falls outside the scope of the Dutch Medical Research Involving Human Subjects Act (WMO) and therefore ethical approval was not formally requested. However, we did protect our participants. The residents were informed that participation was both voluntary and anonymous and that it was possible to withdraw from the survey at any time. All study materials were anonymised and saved by one researcher (JV) on a protected server.
Measures
Speaking up
We operationalised speaking up as suggestion‐focused voice, which was measured with six items taken from the work of van Dyne and LePine.20 The original items were translated into Dutch by a native translator using back‐and‐forth translation. Because our questionnaire was based on self‐reports, the words ‘this employee’ were replaced by ‘I’, such as in the example item: ‘I speak up in this group with ideas for new projects or changes in procedures.’ Responses to items were given on a scale of 1 (never) to 7 (always). Appendix S1 provides an English‐language version of the complete survey.
Control
We measured control using the 10‐item ‘Influence at work’ scale of the Copenhagen Psychosocial Questionnaire.41 An example item is: ‘Do you have a large degree of influence concerning your work?’
Supervisor support
We measured supervisor support using the eight items of the Supportive Supervision Scale.42 An example item is: ‘My supervisor encourages employees to speak up when they disagree with a decision.’
Work engagement
We measured work engagement as a three‐factor model using the nine items of the Utrecht Work Engagement Scale.33, 43 Three items tapped vigour (e.g. ‘At my work, I feel bursting with energy’), three items tapped dedication (e.g. ‘I am enthusiastic about my job’) and three tapped absorption (e.g. ‘I feel happy when I am working intensely’). Work engagement has been extensively studied and previous confirmatory factor analyses showed that a three‐factor model was superior to a one‐factor model.32
Background variables
Background variables included age, gender, specialty training programme, year of training, work experience and organisation.
Statistical analyses
Preliminary analyses
We checked the data for normality. Reliability estimates showed good internal consistency for all scales (Table 2), except ‘supportive supervision’. We deleted one item as a result of a low factor loading and a negative association with ‘voice’ (i.e. ‘My supervisor refuses to explain his or her actions’), which resulted in a scale of seven items with good internal consistency. We performed a Harman single‐factor test to account for common method variance.44
Table 2.
Means, standard deviations (SDs), correlations and reliabilities (Cronbach's alpha, on the diagonal) of the study variables in data for 499 residents in the Netherlands, 2018
| Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 Voice | 4.61 | 1.02 | 0.91 | |||||||
| 2 Support | 4.33 | 1.11 | 0.27† | 0.90 | ||||||
| 3 Control | 3.84 | 0.92 | 0.37† | 0.48† | 0.89 | |||||
| 4 Absorption | 3.92 | 1.00 | 0.18† | 0.32† | 0.26† | – | ||||
| 5 Dedication | 4.56 | 0.87 | 0.17† | 0.40† | 0.30† | 0.70† | – | |||
| 6 Vigour | 4.05 | 0.92 | 0.30† | 0.38† | 0.37† | 0.63† | 0.70† | – | ||
| Demographic variables | ||||||||||
| 7 Age | 33 | 6.1 | 0.10* | −0.09* | 0.10* | −0.08 | −0.10* | 0.02 | − | |
| 8 Gender, female | 0.79 | 0.41 | 0.00 | 0.01 | −0.01 | −0.00 | −0.02 | 0.01 | −0.02 | − |
p ≤ 0.05.
p ≤ 0.01.
Main analyses
We examined the research model using SEM in MPlus Version 8.1 (Muthén & Muthén, Los Angeles, CA, USA). Control, support and voice were treated as observed variables (using the means of corresponding scales) and work engagement was treated as a latent variable with dedication, vigour and absorption as its three indicators. Missing data were handled using full information maximum likelihood methods. Model fit was assessed using the chi‐squared statistic, the Tucker–Lewis index (TLI) (> 0.90 indicates acceptable fit), the root mean square error of approximation (RMSEA) (< 0.08 indicates mediocre fit, < 0.05 indicates good fit) and the Akaike information criterion (AIC).39 For the mediation analysis, we applied a bootstrapping procedure. We calculated the total indirect effects of support and control on voice through work engagement to examine possible mediation effects.45 For the multi‐group analysis, we compared the model fit of a constrained model (all parameters were constrained to be equal across both groups) with the fit of an unconstrained model (with parameters differing across groups). To assess the strength of our results compared with previous findings amongst other professional groups, we used the pooled data from a meta‐analysis on voice and compared the model fit using their effect sizes compared with ours.17
Results
Correlational analysis
Table 2 presents the means, correlations and reliabilities of the study variables. There were positive associations between support (r = 0.27, p < 0.01) and control (r = 0.37, p < 0.01) with voice, confirming Hypotheses 1 and 2. The Harman single‐factor test did not provide strong indications for common method variance, as the explained variance by a single factor was < 50% (33.7%).
Table 3.
Means and correlations of the study variables compared between hospital residents (n = 299, below the diagonal line) and residents working outside hospital settings (n = 200, above the diagonal line) in 499 residents in the Netherlands in 2018
| Mean in hospital | Mean outside hospital | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 Voice | 4.4‡ | 4.9‡ | 1 | 0.13 | 0.29† | 0.19† | 0.21† | 0.31† | 0.04 | 0.03 |
| 2 Support | 4.3 | 4.4 | 0.39† | 1 | 0.51† | 0.29† | 0.37† | 0.27† | −0.12 | 0.03 |
| 3 Control | 3.5‡ | 4.3‡ | 0.34† | 0.51† | 1 | 0.30† | 0.36† | 0.39† | −0.10 | −0.12 |
| 4 Absorption | 3.9 | 3.9 | 0.19† | 0.36† | 0.29† | 1 | 0.65† | 0.55† | −0.08 | 0.06 |
| 5 Dedication | 4.6 | 4.5 | 0.17† | 0.44† | 0.36† | 0.72† | 1 | 0.65† | −0.08 | 0.02 |
| 6 Vigour | 4.0 | 4.1 | 0.29† | 0.47† | 0.40† | 0.68† | 0.74† | 1 | 0.07 | 0.02 |
| Demographic variables | ||||||||||
| 7 Age | 30.8‡ | 36.2‡ | −0.01 | −0.13* | −0.10 | −0.09 | −0.03* | −0.00 | 1 | −0.10 |
| 8 Gender, female | 0.77 | 0.83 | −0.04 | −0.01 | 0.00 | −0.03 | −0.03 | −0.00 | −0.02 | 1 |
p ≤ 0.05.
p ≤ 0.01.
Significant difference between groups.
Structural equation analysis
The full mediation model (M1) fitted the data only marginally (χ2[degrees of freedom, d.f. = 8] = 74.318; RMSEA = 0.129, 90% confidence interval [CI] 0.103–0.156; TLI = 0.837; AIC = 7259.280). The partial mediation model (M2) fitted the data considerably better (χ2[d.f. = 6] = 27.211; RMSEA = 0.084, 90% CI 0.054–0.117; TLI = 0.946; AIC = 7216.173). The difference in χ2‐values between the competing models was significant (Δχ2[d.f. = 2] = 47.107; p < 0.01), which indicates that the partial mediation model is preferred to the full mediation model. Appendix S2 shows the path coefficients of the partial mediation model. We found a significant association between control and voice (0.29, p < 0.01), but not between support and voice (0.08, p > 0.05). Our results showed that work engagement does not mediate the effects of job control and supervisor support on voice behaviour within the full sample and reject Hypothesis 3 (0.11, p > 0.05).
To assess the relative importance of control and support for residents compared with other employees, we compared our path coefficients with the pooled effect sizes in previous research (0.37 versus 0.20 for control and 0.27 versus 0.15 for support).17 We found that for control, our study reports significantly stronger associations compared with previous studies (Δχ2 = 4.761, Δd.f. = 1, p = 0.03).
Multi‐group comparison
Table 3 shows the means and correlations of the study variables compared between residents working in‐ or outside hospital settings. Multi‐group SEM analysis showed that the model results differ between the resident groups (Δχ2 = 28.927 [d.f. = 8], p < 0.01). The path coefficient between voice and support was significant for hospital residents (0.29, p < 0.01), but not for residents who work outside hospital settings (−0.08, p = 0.32). Moreover, the path coefficient between engagement and voice was significant for residents who work outside hospital settings (0.22, p < 0.05) but not for hospital residents (0.03, p = 0.70) (Fig. 2). Mediation analysis showed that work engagement partly mediates the effect between control, support and voice for residents outside hospital settings (0.08, standard error [SE] = 0.04 [95% CI 0.02–0.19] and 0.04, SE = 0.02 [95% CI 0.01–0.10], respectively).
Figure 2.
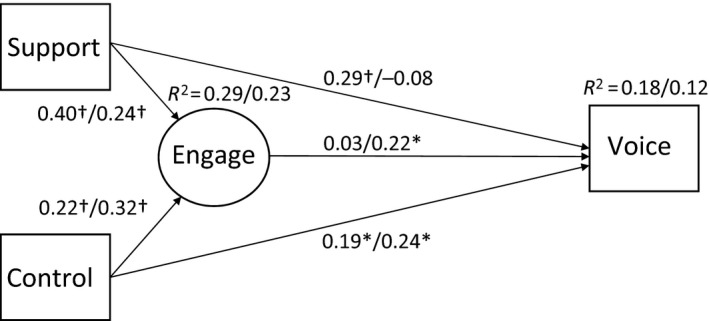
Structural paths from the multi‐group analysis of the partial mediation model (M2). Coefficients represent standardised estimates for hospital residents (n = 299)/residents working outside hospital settings (n = 200). Total n = 499 residents, the Netherlands, 2018. *, p < 0.05; †, p < 0.01
Discussion
This study showed that both job control and supervisor support are job resources that are associated with speaking up by medical residents. However, their associations differ across settings. Support was an important resource for speaking up for hospital residents, whereas work engagement had no significant mediating effect. For residents outside hospital settings, control was an important resource for speaking up. In this group, work engagement positively related to speaking up and partially mediated the effect of control. Although we tested only for associations, previous studies on job resources and active work behaviours such as speaking up support the proposed direction of the effect as depicted in the research model.6, 26, 32, 46, 47, 48, 49
We found that the relationship between control and voice is stronger in our study than in other work settings. Thus, control is a relatively important resource for residents.17 A possible explanation for the absent associations between work engagement and speaking up by medical residents in hospital settings is that contextual factors might inhibit residents from voicing their opinions, which may overwhelm their levels of engagement. One such contextual factor could be the frequent change of work environment that results from the rotational character of in‐hospital specialty training programmes. Residents spend only a few months in a specific department before switching to the next. This may negatively influence their motivation to speak up as previous research shows that speaking up is positively related to longer organisational tenure and experience.1, 50 It is possible that hospital residents feel they lack the time or credibility to make effective suggestions for change, which also relates to a lower sense of control.
Our results show that supervisor support is important for medical residents, but does not influence speaking up by residents outside hospital settings. Hospital residents generally work closely with their supervisors in a ‘master–apprentice’‐like context. In hospitals, physicians are socialised through what is referred to as the ‘hidden curriculum’ in an informal learning process in which novices learn how to behave according to professional and occupational standards.51, 52 Hierarchy is an important element of this curriculum. This may explain why the support of supervisors is especially important for hospital residents when trying to speak up. Outside hospital settings, medical residents usually spend more time in the same department or organisation, and thus build stronger networks and are less dependent on their supervisors. This may explain why support and speaking up are not significantly related for ut‐of‐hospital residents as the influence of a direct supervisor may be less important in a stronger network. In our sample, female residents were slightly over‐represented (79% in our sample versus 71% in the Dutch population) and our respondents were, on average, slightly younger (33 years versus 34 years) than the total population of residents in the Netherlands. Note that the literature provides no conclusive evidence on the influence of gender on speaking up and we did not find any significant correlations between gender and our variables of interest.1
Limitations
One limitation of the current study is its low response rate, which may have resulted in non‐response bias. We calculated the response rate based on all residents in the Netherlands because we used social media as part of our distribution strategy. However, it is unlikely that we reached all residents via these communication channels, meaning that our actual response rate is higher.
Further, the cross‐sectional design means that our results must be interpreted as associations rather than causal relationships. Moreover, as is common in behavioural research, we were able to explain only a relatively small part of the variance of the study concepts. In line with the literature on proactive behaviour at work, we focused on two main factors: job control and supervisor support. However, it is likely that other variables that were not included in our study also influence speaking up by residents.
Implications
Our results provide starting points for medical education programmes to enable residents to speak up and make suggestions for change, using specific organisational and occupational interventions that are targeted towards increasing residents’ sense of control and support. For example, it may be worthwhile to train supervisors in supporting residents in stepping forward with suggestions for change, thereby creating a positive learning climate. When speaking up becomes part of local culture, the threshold at which residents will step forward with their suggestions is lowered. We do not believe (nor do we think it would be beneficial to organisations) that employees should be able to speak up about each and every issue they come across. We do believe that there is a minimal level at which residents should be able to speak up. Moreover, enhancing residents’ sense of control such as by involving them in staff meetings and think‐tanks or by simply asking for their opinions could stimulate them to speak up. This is different from most current postgraduate medical education strategies, which are more focused on individual (competency) training.53 When local training programmes acknowledge that speaking up can be difficult for residents who are junior employees, this acknowledgement represents an important first step in creating a culture of speaking up and sharing novel ideas, suggestions and experiences.
Theoretically, this study further strengthens the evidence that control and support are positively associated with speaking up by (medical) employees. This association differs between hospital residents and residents who work outside hospital settings. Moreover, we demonstrated that work engagement is associated with job resources, which is in line with the findings of previous research.1, 17, 20, 54
Conclusions
This study showed that perceived control and support are associated with speaking up and sharing suggestions for change by medical residents. This emphasises the suggestion that residents do not act in a vacuum; rather, they are embedded in their professional and organisational contexts. This embeddedness calls for attention to contextual factors such as job control and supervisor support that positively influence residents to speak up and share their ideas for change.
Contributors
JJV, TWT and MFvdS contributed to the theoretical and statistical design, the analysis and interpretation of the data and the preparation of the manuscript. ELJvR, MMES and MN contributed to the design of the study, the interpretation of results and the critical review of the manuscript. All authors (JJV, TWT, ELJvR, MMES, MN and MFvdS) approved the final manuscript for submission.
Funding
none.
Conflicts of interest
none.
Ethical approval
not required.
Supporting information
Appendix S1. Survey guide.
Appendix S2. Path coefficients of the partial mediation model.
Acknowledgements
the authors wish to thank Barbara Flunger, Department of Education, Utrecht University, for her help and expertise during the preparation and analysis stages of this study.
References
- 1. Morrison EW. Employee voice behavior: integration and directions for future research. Acad Manag Ann 2011;5 (1):373–412. [Google Scholar]
- 2. Dixon‐Woods M, Campbell A, Martin G, Willars J, Tarrant C, Aveling EL, Sutcliffe K, Clements J, Carlstrom M, Pronovost P. Improving employee voice about transgressive or disruptive behavior: a case study. Acad Med 2019;94 (4):579–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lemer C, Moss F. Patient safety and junior doctors: are we missing the obvious? BMJ Qual Saf 2013;22 (1):8–10. [DOI] [PubMed] [Google Scholar]
- 4. Roueche A, Hewitt J. ‘Wading through treacle’: quality improvement lessons from the frontline. BMJ Qual Saf 2012;21 (3):179–83. [DOI] [PubMed] [Google Scholar]
- 5. Vidyarthi AR, Green AL, Rosenbluth G, Baron RB. Engaging residents and fellows to improve institution‐wide quality: the first six years of a novel financial incentive program. Acad Med 2014;89 (3):460–8. [DOI] [PubMed] [Google Scholar]
- 6. Häusser JA, Mojzisch A, Niesel M, Schulz‐Hardt S. Ten years on: a review of recent research on the Job Demand–Control (–Support) Model and psychological well‐being. Work Stress 2010;24 (1):1–35. [Google Scholar]
- 7. Dath D, Chan M‐K, Abbott C. CanMEDS 2015: from Manager to Leader. Ottawa, ON: The Royal College of Physicians and Surgeons of Canada. 2015. http://www.royalcollege.ca/rcsite/documents/cbd/canmeds-2015-manager-to-leader-e.pdf. [Accessed 10 October 2018.]
- 8. NHS Institute for Innovation and Improvement and Academy of Medical Royal Colleges . Medical Leadership Competency Framework: Enhancing Engagement in Medical Leadership, 3rd edn Coventry, UK: NHS Institute for Innovation and Improvement and Academy of Medical Royal Colleges; 2010. [Google Scholar]
- 9. Noordegraaf M. Risky business: how professionals and professional fields (must) deal with organizational issues. Organ Stud 2011;32 (10):1349–71. [Google Scholar]
- 10. Bevan H. Rocking the boat and staying in it: how to succeed as a radical in healthcare. BMJ Quality 2013. http://blogs.bmj.com/quality/2013/07/29/a-call-to-action-helen-bevans-blog/. [Accessed 10 October 2018.]
- 11. Panagioti M, Geraghty K, Johnson J, Zhou A, Panagopoulou E, Chew‐Graham C, Peters D, Hodkinson A, Riley R, Esmail A. Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta‐analysis. JAMA Intern Med 2018;178 (10):1317–30. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 12. Frese M, Fay D. Personal initiative: an active performance concept for work in the 21st century. Res Organ Behav 2001;23:133–87. [Google Scholar]
- 13. Parker SK, Williams HM, Turner N. Modeling the antecedents of proactive behavior at work. J Appl Psychol 2006;91 (3):636–52. [DOI] [PubMed] [Google Scholar]
- 14. Landgren R, Alawadi Z, Douma C, Thomas EJ, Etchegaray J. Barriers of pediatric residents to speaking up about patient safety. Hosp Pediatr 2016;6 (12):738–43. [DOI] [PubMed] [Google Scholar]
- 15. Okuyama A, Wagner C, Bijnen B. Speaking up for patient safety by hospital‐based health care professionals: a literature review. BMC Health Serv Res 2014;14 (1):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Martinez W, Etchegaray JM, Thomas EJ, Hickson GB, Lehmann LS, Schleyer AM, Best JA, Shelburne JT, May NB, Bell SK. ‘Speaking up’ about patient safety concerns and unprofessional behaviour among residents: validation of two scales. BMJ Qual Saf 2015;24 (11):671–80. [DOI] [PubMed] [Google Scholar]
- 17. Tornau K, Frese M. Construct clean‐up in proactivity research: a meta‐analysis on the nomological net of work‐related proactivity concepts and their incremental validities. Appl Psychol 2013;62 (1):44–96. [Google Scholar]
- 18. Schwappach D, Richard A. Speak up‐related climate and its association with healthcare workers’ speaking up and withholding voice behaviours: a cross‐sectional survey in Switzerland. BMJ Qual Saf 2018;27 (10):827–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Martin GP, Aveling EL, Campbell A, Tarrant C, Pronovost PJ, Mitchell I, Dankers C, Bates D, Dixon‐Woods M. Making soft intelligence hard: a multi‐site qualitative study of challenges relating to voice about safety concerns. BMJ Qual Saf 2018;27 (9):710–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Van Dyne L, LePine JA. Helping and voice extra‐role behaviors: evidence of construct and predictive validity. Acad Manag J 1998;41 (1):108–19. [Google Scholar]
- 21. Schwappach DLB, Gehring K. Trade‐offs between voice and silence: a qualitative exploration of oncology staff's decisions to speak up about safety concerns. BMC Health Serv Res 2014;14 (1):303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Martinez W, Lehmann LS, Thomas EJ et al. Speaking up about traditional and professionalism‐related patient safety threats: a national survey of interns and residents. BMJ Qual Saf 2017;26 (11):869–80. [DOI] [PubMed] [Google Scholar]
- 23. Morrison EW. Employee voice and silence. Ann Rev Organ Psychol Organ Behav 2014;1 (1):173–97. [Google Scholar]
- 24. Karasek RA. Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q 1979;24 (2):285–308. [Google Scholar]
- 25. Karasek R. Lower health risk with increased job control among white collar workers. J Organ Behav 1990;11 (3):171–85. [Google Scholar]
- 26. van der Doef M, Maes S. The Job Demand–Control (–Support) Model and psychological well‐being: a review of 20 years of empirical research. Work Stress 1999;13 (2):87–114. [Google Scholar]
- 27. Taris TW, Kompier MAJ. Job characteristics and learning behavior: review and psychological mechanisms In: Perrewe PL, Ganster DC, eds. Exploring Interpersonal Dynamics. Bingley: Emerald Group Publishing; 2004;127–66. [Google Scholar]
- 28. Fishbein M, Ajzen I. Predicting and Changing Behavior. The Reasoned Action Approach, 1st edn New York, NY: Psychology Press; 2010. [Google Scholar]
- 29. Crant JM, Bateman TS. Charismatic leadership viewed from above: the impact of proactive personality. J Organ Behav 2000;21 (1):63–75. [Google Scholar]
- 30. Baer M, Oldham GR. The curvilinear relation between experienced creative time pressure and creativity: moderating effects of openness to experience and support for creativity. J Appl Psychol 2006;91 (4):963–70. [DOI] [PubMed] [Google Scholar]
- 31. Salanova M, Schaufeli WB. A cross‐national study of work engagement as a mediator between job resources and proactive behaviour. Int J Hum Resour Manag 2008;19 (1):116–31. [Google Scholar]
- 32. Schaufeli WB, Taris TW. A critical review of the job demands–resources model: implications for improving work and health In: Bauer GF, Hämmig O, eds. Bridging Occupational, Organizational and Public Health: A Transdisciplinary Approach. Dordrecht: Springer Science & Business Media; 2014;43–67. [Google Scholar]
- 33. Schaufeli WB, Bakker AB, Salanova M. The measurement of work engagement with a short questionnaire: a cross‐national study. Educ Psychol Meas 2006;66 (4):701–16. [Google Scholar]
- 34. Schaufeli WB, Bakker AB. Job demands, job resources, and their relationship with burnout and engagement: a multi‐sample study. J Organ Behav 2004;25 (3):293–315. [Google Scholar]
- 35. Taris TW. The Psychology of Working Life, 1st edn London, UK: Routledge; 2018. [Google Scholar]
- 36. Schaufeli WB, Bakker AB, van der Heijden FMMA, Prins JT. Workaholism, burnout and well‐being among junior doctors: the mediating role of role conflict. Work Stress 2009;23 (2):155–72. [Google Scholar]
- 37. The Young Specialist Doctors Foundation . National Resident Survey Report 2015 (Rapport Nationale aios enquête 2015). the Netherlands: The Young Specialist Doctors Foundation; 2015. https://www.dejongespecialist.nl/themabestanden/Rapport Aios Enquete De Jonge Specialist.pdf. [Accessed 1 November 2018.] [Google Scholar]
- 38. Prins JT, Hoekstra‐Weebers JEHM, Gazendam‐Donofrio SM, Dillingh GS, Bakker AB, Huisman M, Jacobs B, van der Heijden FM. Burnout and engagement among resident doctors in the Netherlands: a national study. Med Educ 2010;44 (3):236–47. [DOI] [PubMed] [Google Scholar]
- 39. Byrne BM. Structural Equation Modeling with MPlus: Basic Concepts, Applications, and Programming. London, UK: Routledge; 2013. [Google Scholar]
- 40. Koninklijke Nederlandsche Maatschappij tot bevordering der Geneeskunst (KNMG) [Royal Dutch Medical Association] . KNMG RGS Overzicht aantal aios per specialisme/profiel 2008–2018. KNMG 2019. https://www.knmg.nl/opleiding-herregistratie-carriere/rgs/registers/aantal-registraties-specialistenaois.htm. [Accessed 4 January 2019.]
- 41. Kristensen TS, Hannerz H, Høgh A, Borg V. The Copenhagen Psychosocial Questionnaire – a tool for the assessment and improvement of the psychosocial work environment. Scand J Work Environ Health 2005;31 (6):438–49. [DOI] [PubMed] [Google Scholar]
- 42. Oldham GR, Cummings A. Employee creativity: personal and contextual factors at work. Acad Manag J 1996;39 (3):607–34. [Google Scholar]
- 43. Schaufeli WB, Bakker AB. UWES–Utrecht Work Engagement Scale: Preliminary Manual. Version 1.1. Utrecht, NL: Occupational Health Psychology Unit, Utrecht University; 2003. https://www.wilmarschaufeli.nl/publications/Schaufeli/Test%20Manuals/Test_manual_UWES_English.pdf. [Accessed 2 February 2018.] [Google Scholar]
- 44. Brannick MT, Chan D, Conway JM, Lance CE, Spector PE. What is method variance and how can we cope with it? A panel discussion Organ Res Methods 2010;13 (3):407–20. [Google Scholar]
- 45. MacKinnon DP. Introduction to Statistical Mediation Analysis. New York, NY: Lawrence Erlbaum Associates; 2008. [Google Scholar]
- 46. Xanthopoulou D, Bakker AB, Demerouti E, Schaufeli WB. Reciprocal relationships between job resources, personal resources, and work engagement. J Vocat Behav 2009;74 (3):235–44. [Google Scholar]
- 47. Mauno S, Kinnunen U, Ruokolainen M. Job demands and resources as antecedents of work engagement: a longitudinal study. J Vocat Behav 2007;70 (1):149–71. [Google Scholar]
- 48. Schaufeli WB, Bakker AB, van Rhenen W. How changes in job demands and resources predict burnout, work engagement, and sickness absenteeism. J Organ Behav 2009;30 (7):893–917. [Google Scholar]
- 49. Frese M, Garst H, Fay D. Making things happen: reciprocal relationships between work characteristics and personal initiative in a four‐wave longitudinal structural equation model. J Appl Psychol 2007;92 (4):1084–102. [DOI] [PubMed] [Google Scholar]
- 50. Burris ER, Detert JR, Chiaburu DS. Quitting before leaving: the mediating effects of psychological attachment and detachment on voice. J Appl Psychol 2008;93 (4):912–22. [DOI] [PubMed] [Google Scholar]
- 51. Witman Y, Smid GAC, Meurs PL, Willems DL. Doctor in the lead: balancing between two worlds. Organization 2010;18 (4):477–95. [Google Scholar]
- 52. Hafferty FW, Franks R. The hidden curriculum, ethics teaching, and the structure of medical education. Acad Med 1994;69 (11):861–71. [DOI] [PubMed] [Google Scholar]
- 53. Sklar DP. Leadership in academic medicine: purpose, people, and programs. Acad Med 2018;93 (2):145–8. [DOI] [PubMed] [Google Scholar]
- 54. Tangirala S, Ramanujam R. Exploring nonlinearity in employee voice: the effects of personal control and organizational identification. Acad Manag J 2008;51 (6):1189–203. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Survey guide.
Appendix S2. Path coefficients of the partial mediation model.


