Abstract
Background:
Previous studies have suggested an association of asthma onset and exacerbation with cleaning and disinfecting activities in a number of industries, including healthcare. The objective of the current study was to investigate the association of asthma and related outcomes with occupations and tasks in urban healthcare workers in the United States.
Methods:
A questionnaire was implemented in a sample of workers from nine healthcare occupations in New York City. We used regression models to examine the association of post-hire asthma, current asthma, exacerbation of asthma, a symptom algorithm for bronchial hyper-responsiveness (BHR-related symptoms), a symptom-based asthma score, and the symptom wheeze with occupation and four healthcare tasks, while adjusting for other risk factors and potential confounders.
Results:
A total of 2030 participants completed the questionnaire. The task of cleaning fixed surfaces was significantly associated with most outcome variables, including current asthma (odds ratio (OR) = 1.84, 95% confidence interval (CI) 1.26–2.68), moderate exacerbation (OR = 3.10, 95% CI 1.25–7.67), and BHR-related symptoms (OR = 1.38, 95% CI 1.08–1.77). In comparison to nursing assistants, the occupations environmental service workers and registered nurses were at higher risk for current asthma, and licensed practical nurses were at higher risk for moderate exacerbation. Other tasks associated with outcomes were administering aerosolized medications with current asthma and moderate exacerbation, and sterilizing medical equipment with BHR-related symptoms.
Conclusions:
These findings add to the growing body of evidence for the association of asthma with cleaning and other activities in healthcare. Further research is especially needed to investigate the association of asthma-related outcomes with exposure metrics based on tasks, products, and chemical exposures in healthcare.
Keywords: Asthma, Healthcare, Occupation, Work tasks, Cleaning, Disinfecting
1. Introduction
Asthma is a common respiratory disease, with approximately 7.7% of adults in the United States (U.S.) having current asthma (Moorman et al., 2012). Work-related asthma (WRA) subsumes two categories of disease: occupational asthma (OA) that is caused by work, and work-exacerbated asthma (WEA) that is worsening of existing asthma due to workplace conditions (Henneberger et al., 2011). Occupation accounts for an estimated 16.9% of new cases (Torén and Blanc, 2009), and WEA has a prevalence of approximately 21.5% among adult asthma cases (Henneberger et al., 2011). The 1996 estimated annual cost of WRA was $1.6 billion, or $1082 per worker (Leigh et al., 2002). By adjusting for a 111% increase in medical care costs between 1996 and 2016 (BLS, 2017a), the resulting 2016 cost for WRA was estimated to be $2281 per case. With 2.7 million U.S. workers having WRA in 2016 (Dodd and Mazurek, 2016), the projected annual cost of WRA was approximately $6 billion.
Epidemiologic evidence indicates that some healthcare occupations have an elevated risk for asthma and related symptoms such as wheeze (Bakerly et al., 2008; Koehoorn et al., 2013; Liss et al., 2011; Pechter et al., 2005). In order to inform prevention, it is important to identify the healthcare jobs and tasks most strongly associated with asthma and related symptoms. The healthcare industry is hierarchical, with occupations requiring different training and responsible for distinctive functions defined by skills, tasks, and tools used. Occupation can arguably serve as an effective surrogate for the totality of all work-related exposures experienced in a job, although such a surrogate is prone to exposure misclassification and precludes the identification of specific exposures or tasks that pose a health risk. For example, the US-based Nurses’ Health Study found a statistically significant association between severe persistent asthma and operating room nursing when compared to administrative nursing (Le Moual et al., 2013). This analysis assumed that all operating room nurses were similarly exposed. At the same time, task can potentially be a more relevant surrogate of exposure than occupation, especially if multiple occupations perform a task that involves high-risk exposures. For example, several studies have identified an association between respiratory problems and the cleaning and disinfecting activities that are common in several healthcare occupations (Arif and Delclos, 2012; Dumas et al., 2012; Gonzalez et al., 2014; Walters et al., 2013).
Starting in 2011, the National Institute for Occupational Safety and Health (NIOSH) of the U.S. Centers for Disease Control and Prevention conducted a project to identify asthma and related outcomes in healthcare workers, and investigate associations between these respiratory outcomes and different workplace exposure metrics. Healthcare workers were recruited from nine occupations, and participants completed a questionnaire that inquired about demographic characteristics, tasks performed and products used in healthcare occupations, and the occurrence of asthma and related health outcomes. In the current study, we examined the association of asthma outcomes with work in the nine healthcare occupations and with performance of four tasks common in healthcare (i.e., clean fixed surfaces, sterilize medical instruments, administer aerosolized medications, and use chemicals on patients).
2. Materials and methods
2.1. Study population and data collection
The NIOSH Institutional Review Board for Human Subjects reviewed and approved the protocol and study documents. Invitees received a letter that included an invitation, explained the purpose of the study, and included text that allowed them to subsequently make an informed decision about participation. Invitees provided informed consent before participating.
Members of the Service Employees International Union Local 1199 in New York City were invited to participate. A search of electronic union records identified 24,562 members who lived in New York City and were in one of nine target occupations, which provided a range of occupational exposures as indicated by prior field studies of exposures in hospitals (LeBouf et al., 2014; Saito et al., 2015). The union had email addresses for only about 10% of the members, so mail and telephone services were used to contact invitees. The 502 union members lacking a phone number and three without a mailing address were excluded, leaving a final sample frame of 24,057.
The 24,057 were distributed unequally by the nine occupations, ranging from a low of 284 dental assistants to a high of 10,454 nursing assistants (NAs). Numbers for the other occupations were: 4246 environmental service workers (ESWs), 2907 licensed practical nurses (LPNs), 2616 registered nurses (RNs), 2060 laboratory technicians (lab techs), 600 operating room technicians (OR techs), 571 respiratory therapists or technicians (respiratory therapists), and 319 central supply workers (CSWs). We selected 18,243 members (76% of 24,057) using a random sample stratified by occupation. This number was based on sample size calculations and an anticipated 60% participation rate. With such a large number of NAs, we selected a considerably lower percentage of them (52%) compared to other occupations. We selected 100% of the four smallest occupations (i.e., dental assistants, CSWs, OR techs, and respiratory therapists) to maximize the chance of attaining adequate numbers. We also took high percentages of ESWs (98%) because of our interest in workers who performed cleaning tasks and of LPNs (100%) because they had not always been included in other studies of nurses, and only somewhat lower percentages of lab techs (85%) and RNs (86%).
Starting in February 2014, the first round of 12,000 invitees were contacted with two mailings (introductory material followed by information about the study and informed consent), two reminder postcards, and at least seven phone calls initiated at various times on both weekdays and weekends. Invitees could complete the main survey either online or with an interviewer on the telephone. Telephone interviews were conducted for 14 weeks after sending the invitation letters, with inbound calls the first four weeks and both inbound and outbound calls the last ten weeks. Strategies used to increase the likelihood of contact and cooperation included calling alternative numbers from the fifth pass onwards and using a direct mailing services company to update addresses of non-responders before sending the second reminder postcard. The same methods were used with the second round of 6243 invitees.
A short telephone questionnaire was offered to non-responders after the conclusion of attempts to contact the second round of invitees. The non-responder sample included 13,845 and excluded invitees who had completed the main questionnaire or were on the union no-call list, or for whom call attempts had yielded any of the following outcomes: ineligible (i.e., deceased, < 18 years old or not employed in healthcare, not currently working in a target occupation, or not currently living and working in New York City); bad or wrong telephone number; hostile refusal; language barrier; or hearing impairment. The goal to administer the non-responder survey to 3% (or 547) of the 18,243 invitees was met by the second pass through the phone numbers.
2.2. Survey instruments
The main questionnaire underwent extensive development and modification, with input from survey instrument experts and two researchers who had conducted studies of healthcare workers. It addressed various topics, including demographics, smoking, employment history, frequency of task and product use, and presence of asthma-related outcomes. Many questions were from frequently-used standardized instruments (Burney et al., 1994; Ferris, 1978; Jarvis, 2002; Sunyer et al., 2007) and a previous study of healthcare workers in Texas (Delclos et al., 2006). We prepared the main questionnaire in English and Spanish for telephone presentation and English for the online version, field-tested it, and developed scripts and training for telephone interviewers.
The non-responders survey instrument included questions from the main questionnaire for gender, age, race/ethnicity, occupation, place of work, smoking, and wheeze in the last 12 months. An additional question inquired about the primary reason for not completing the main survey.
2.3. Inverse probability weights for selection and non-participation
We used weights equal to the occupation-specific inverse probability of selection so that the 18,243 invitees more closely resembled the final sample frame regarding distribution by occupation. Two additional interim inverse probability weights were also calculated to address non-participation. The first interim weight accounted for invitees whose eligibility status was unknown due to insufficient information from union records or the main or non-responder survey. Those with known eligibility status had sufficient information to classify them as either eligible (i.e., were alive, > 18 years old and employed in healthcare, working in one of the target occupations, and living and working in New York City) or ineligible (i.e., failed to fulfill at least one criterion). We derived these weights by fitting a regression model with the outcome of known eligibility status among the 18,243 invitees, using the SAS Survey logistic procedure with the selection weight in the weight statement. The independent covariates were age (< 39 (reference), 40–49, 50–59, > 60), gender, and occupation. We selected NAs as the common reference category for occupation because they were the largest occupation and had lower prevalence of cleaning and disinfecting tasks. The age, gender, and occupation data for each eligible invitee were inserted into the fitted model to yield an individual log odds that was converted to a probability. The inverse of this probability was the desired weight.
The second set of interim weights for non-participation was based on modelling completion of the main questionnaire among eligible invitees, using the SAS Survey logistic procedure and weights equal to the product of the selection weight and the first non-participation weight. This model included independent covariates for gender, age, occupation, smoking status (former, current, and never as reference), and wheeze in the last 12 months. We tested all pairwise interactions of wheeze with the other covariates, and retained two interaction terms that had p < 0.15: wheeze x female and wheeze x LPNs. We calculated this set of interim weights using the same methods as already described. Final weights equaled the product of the selection weight and the two interim non-participation weights, and had the following characteristics for the 2030 who completed the main survey: range 5.03–17.24, interquartile range 7.96–12.38, median 9.08, and mean 9.98 (SD = 2.63).
2.4. Dependent variables
We used two definitions of asthma identified among the participants with physician-diagnosed asthma. The first was “post-hire asthma”, which was the same as what researchers termed “reported asthma” in a study of healthcare workers in Texas (Delclos et al., 2007). This was defined as physician-diagnosed asthma with onset after starting in the healthcare profession. The second definition was “current asthma,” assessed as an individual with physician-diagnosed asthma who met any of the following criteria: an attack of asthma in the last 12 months, medication use for asthma in the last 12 months, hospitalized overnight for asthma in the last 12 months, urgent care/treatment for asthma in the last 12 months, or an asthma score ≥1. These criteria were based on previous definitions of current asthma from the European Community Respiratory Health Survey (ECRHS) (Kogevinas et al., 1999).
As a subset of current asthma, exacerbation of asthma was examined through questions on treatment and medication use in the last 12 months. Exacerbation was divided into the two categories of either moderate or severe. An individual with current asthma was considered to have experienced moderate exacerbation if he or she sought urgent treatment for asthma (e.g., at a doctor’s office, urgent care facility, or emergency room) in the last 12 months without increasing usage of oral steroids; or if he or she increased usage of inhaled steroids, or fast-acting or rescue bronchodilators on a short-term basis in the last 12 months. An individual was determined to have severe asthma exacerbation if he or she were hospitalized overnight for asthma or increased oral steroid usage as treatment for asthma in the last 12 months. Further, we examined the binary outcome of any exacerbation, which included any of those with either moderate or severe asthma exacerbation. These criteria for exacerbation are consistent with definitions recommended by professional organizations (Reddel et al., 2009).
In order to identify individuals with asthma-related symptoms but not necessarily a definitive asthma diagnosis, we employed the use of a validated asthma score and an algorithm for bronchial hyper-responsiveness (BHR)-related symptoms. ECRHS researchers developed a five-item asthma score, which can evaluate asthma both as a continuous and a dichotomous outcome (Sunyer et al., 2007). The score aims to detect risk factors and different markers for asthma, such as asthma attacks, use of asthma medication, and bronchial responsiveness. An individual’s asthma score is calculated as the sum of the positive answers to five questions (“no” = 0; “yes” = 1) regarding breathlessness while wheezing, woken with a feeling of chest tightness, attack of shortness of breath (SOB) at rest, attack of SOB after activity, and woken by attack of SOB. All five items represent symptoms that may have occurred within the 12-month period before completing the questionnaire (Sunyer et al., 2007). The asthma score has been validated against several clinical indicators of asthma and used in a variety of epidemiologic studies, including both worker-based and larger population-based studies conducted in Europe (Sunyer et al., 2007; Vizcaya Fernández et al., 2011).
We also employed a symptom-based BHR algorithm that was developed by researchers evaluating the respiratory health of healthcare workers in Texas (Arif et al., 2009; Delclos et al., 2006, 2007). We decided to use this outcome in addition to the asthma score because it included questions about allergic responses as well as respiratory symptoms, and because it was developed for and used in the study of healthcare workers in Texas, thus providing a basis for comparison in the same country as the current study sample. The algorithm yields a dichotomous outcome for BHR-related symptoms based on responses to questions regarding the following eight symptom scenarios: trouble with breathing; attack or episode of SOB in the last 12 months; wheezing or whistling in the chest in the last 12 months; woken by an attack of cough in the last 12 months; woken by an attack of chest tightness in the last 12 months; itchy or watery eyes when near animals, feathers, or in a dusty part of the house; feeling of chest tightness when near animals, feathers, or in a dusty part of the house; and itchy or watery eyes when near flowers or pollen (Delclos et al., 2006). In the development process, these questions were validated against the clinical testing of provocative concentration of methacholine that resulted in at least a 20% decrease in forced expiratory volume in 1 s (PC20) from baseline. Ultimately, BHR was defined with a cut point of PC20 ≤ 4 mg/ml. The BHR-related symptom algorithm provided estimates of 61% sensitivity and 85% specificity for PC20 ≤ 4 mg/ml (Delclos et al., 2006).
Wheeze is a sentinel symptom of asthma, and we defined it as a positive response to the following survey question: “Have you had wheezing or whistling in your chest at any time in the last 12 months?”
2.5. Independent variables
When investigating the association of health with occupation, NAs were the common reference category for the other eight occupations. Other analyses investigated the association of health with four different self-reported healthcare tasks: clean or disinfect fixed surfaces, equipment, or instruments; sterilize or high-level disinfect medical instruments; administer aerosolized medications; and use chemicals, adhesives, antiseptics, alcohols, or solvents on patients. Other risk factors and potential confounding variables included in all regression models of health outcomes were gender (female, male), age (years, continuous), race (African American, white, other, unspecified), smoking status (never, former, current), and history of allergies (dichotomous, based on self-reported history of nasal or sinus allergies (including hay fever), ever eczema or other skin allergies, ever animal allergies, ever dust or dust mite allergies, or latex or adhesive allergies).
2.6. Statistical analysis
Data management, summaries of crude data, and all analyses were accomplished using SAS® 9.4 statistical software (SAS Institute Inc., Cary, NC, USA). Weights based on the inverse probability of selection and participation were included in regression models to adjust for possible bias. Simple descriptive statistics were produced for the entire study sample, by occupation, and by healthcare task. The associations of post-hire asthma, current asthma, any exacerbation, BHR-related symptoms, and wheeze with both the occupational and task variables were examined using binary logistic regression. The odds ratio (OR), corresponding 95% confidence interval (95% CI), and p-value were calculated for each covariate. The association of the multinomial outcome of moderate and severe exacerbation of asthma with occupation and task was assessed using polytomous logistic regression. We did not report effect estimates for any models when < 5 participants had the outcome of interest.
Sparse data necessitated combining cells when analyzing asthma score relative to the occupations but not the tasks. All but two occupations (NAs and ESWs) had at least one instance of < 5 participants with an asthma score in the range of 2–5 (see Online Supplement Table S1). Consequently, we combined these categories when analyzing the association of occupation with asthma score, creating an ordinal outcome variable with scores 0, 1, and 3. With both the abbreviated range of asthma scores to study the association with occupation and the full range of values to study the association with task, there was over dispersion in the distribution of data. Consequently, we used a negative binomial regression model, and results were expressed as ratios of the mean asthma score with corresponding 95% confidence intervals (Pekkanen et al., 2005).
3. Results
3.1. Eligibility and participation status
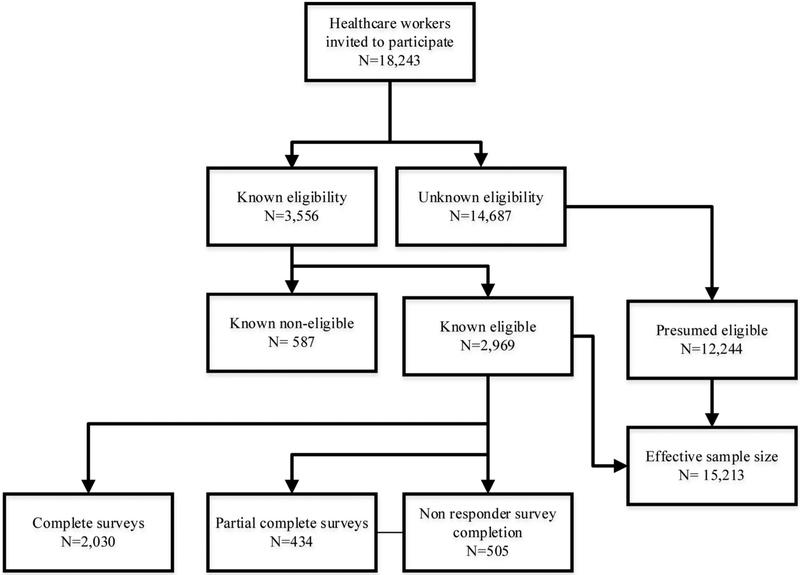
Eligibility and participation status for the 18,243 invitees is summarized in Fig. 1. Information was insufficient to confirm eligibility for 14,687: 1046 provided some data in the main or non-responder survey; 6201 were contacted by telephone but no data were collected; and 7440 were never reached by telephone and provided no data online. Data were sufficient to confirm eligibility status for 3,556, of whom 587 were ineligible and 2969 eligible. The eligible participants included 2030 who completed the main survey (406 online, 1624 by telephone), 434 who finished part of the main survey at least through questions about current occupation, and 505 with complete data on the non-responders survey.
Fig. 1.
Eligibility and participation status of 18,243 invitees.
We calculated an effective eligible sample size by presuming the 14,687 with unconfirmed eligibility status had the same percentage of eligible invitees as the 3556 with confirmed eligibility status. The 2969 eligible accounted for 83.5% of the 3,556, and the percentage eligible by occupation ranged from a low of 75.3% for ESWs to a high of 88.2% for RNs. We applied the occupation-specific eligibility percentages to the counts of invitees with eligibility not confirmed, to yield an estimated 12,244 presumed eligible (data not shown). The effective sample size of eligible invitees was the sum of those confirmed and presumed eligible, or 2969 + 12,244 = 15,213, and was the denominator used to calculate the following participation rates. The 2969 eligible invitees represented 19.5% of the effective sample, including 2030 (13.3%) completes and 434 (2.9%) partials for the main survey, and 505 (3.3%) who finished the non-responder survey. The occupation-specific participation rate for completing the main survey ranged from a low of 11.2% for lab techs to a high of 15.2% for respiratory therapists (Online Supplement Table S2). The participation rate for the non-responder survey after two rounds of telephone calls was 505 of 13,845, or 3.6%.
Those who completed the non-responder survey were asked why they did not complete the main questionnaire, and were given a series of answers from which to choose and the option to write in an answer. The two most common answers accounted for approximately 80% of non-responders: “not aware/didn’t know about it” with 44.2% (n = 223) and “survey is too long/too busy to complete” with 35.4% (n = 179). The other reasons individually represented < 3% of the group. Only 1.8% (n = 9) of non-responders reported they did not participate because the topic was not relevant to them.
3.2. Descriptive characteristics of participants
Descriptive characteristics of the study cohort are presented in Table 1. The average age of the study sample was 48.6 years (SD = 11.4), and women were three times as numerous as men (76% vs 24%). The majority of participants were African American (62%), with just 13% identifying their race as white, another 13% as other, and 12% as unspecified. Approximately 17% of the sample reported ever smoking, with only 5.6% currently smoking. Half (51%) of all participants indicated a history of allergies. The occupation-specific distribution of participants by descriptive characteristics is available in Table S3 in the Online Supplement.
Table 1.
Descriptive characteristics of the 2030 study participants.
| Type of characteristic | Variable | n (mean, SD) | % |
|---|---|---|---|
| Demographic and health-related | Age, in years (mean, SD) | (48.6, 11.4) | |
| Sex | |||
| Female | 1542 | 76 | |
| Male | 487 | 24 | |
| Race | |||
| African American | 1249 | 62 | |
| White | 266 | 13 | |
| Other | 274 | 13 | |
| Unspecified | 241 | 12 | |
| Smoking status | |||
| Never smokers | 1676 | 83 | |
| Former smokers | 226 | 11 | |
| Current Smokers | 113 | 5.6 | |
| History of allergiesa | 1033 | 51 | |
| Healthcare occupation | NAs | 702 | 35 |
| CSWs | 41 | 2.0 | |
| Dental Assistants | 32 | 1.6 | |
| ESWs | 374 | 18 | |
| Lab Techs | 166 | 8.2 | |
| LPNs | 297 | 15 | |
| OR Techs | 63 | 3.1 | |
| RNs | 280 | 14 | |
| Respiratory Therapists | 75 | 3.7 | |
| Major healthcare tasks | Clean fixed surfaces | 1291 | 64 |
| Sterilize medical equipment | 301 | 15 | |
| Administer aerosolized medications | 395 | 19 | |
| Use chemicals, adhesives, or solvents on patients | 646 | 32 | |
| Asthma-related outcomes | Physician-diagnosed asthma | 223 | 11 |
| Post-hire asthma | 103 | 5.1 | |
| Current asthma | 173 | 8.5 | |
| Any exacerbation | 74 | 3.6 | |
| Moderate exacerbation | 41 | 2.0 | |
| Severe exacerbation | 33 | 1.6 | |
| BHR-related symptoms | 522 | 26 | |
| Asthma symptom score (mean, SD) | (0.48, 1.02) | ||
| Asthma symptom score, frequency | |||
| 0 | 1511 | 74 | |
| 1 | 277 | 14 | |
| 2 | 115 | 5.7 | |
| 3 | 63 | 3.1 | |
| 4 | 35 | 1.7 | |
| 5 | 29 | 1.4 | |
| Wheezing or whistling in last 12 months | 291 | 14 |
Abbreviations for occupations - NAs: nursing assistants, CSWs: central supply workers, ESWs: environmental service workers, Lab Techs: laboratory technicians, LPNs: licensed practical nurses, OR Techs: operating room technicians, RNs: registered nurses, Resp. Therapists: respiratory therapists or technicians.
Defined as a positive response to any of the following: ever nasal or sinus allergies (including hay fever), ever eczema or any kind of skin allergy, ever allergies to animals, ever allergies to dust or dust mites, or ever allergies to latex or adhesives.
The 2030 who completed the main questionnaire had a similar distribution by gender as the other 16,213 invitees, with 76% and 74% female, respectively. The participants’ mean age of 48.6 years (SEM = 0.25) was only somewhat greater than the comparable value of 48.1 years (SEM = 0.09) for the others (p = 0.08). The two groups differed in their crude distribution by occupation (p < 0.05), with participants more likely to work as NAs (33% versus 29%) and less likely to work as ESWs (19% versus 23%).
The number of participants varied by occupation, with NAs representing the largest group with about one-third of the cohort (n = 702, 35% of 2030). At the other extreme, five occupations had fewer than 200 participants (CSWs, dental assistants, lab techs, OR techs, and respiratory therapists) and collectively represented 18.6% of the cohort. Of the four major healthcare tasks, cleaning fixed surfaces was the most common with 64%, and sterilizing medical equipment was the least common with 15%. For the asthma-related outcomes, 5.1% fulfilled the criteria for post-hire asthma and 8.5% for current asthma, 26% had BHR-related symptoms, and 26% had a nonzero asthma score. The number of participants declined as the asthma score increased, and the top three categories (i.e., 3, 4, and 5) each had fewer than 65 people. Wheeze was reported by 14% of the participants.
The frequency of healthcare tasks varied by occupation (Table 2). As expected, 82% of ESWs cleaned fixed surfaces, but at least 70% of the participants in six other occupations also performed this task. The other three tasks had fewer occupations with high frequencies. Using chemicals, adhesives, or solvents on patients was the second most common task with approximately one-third of the sample, and was conducted by a majority of RNs (72%), LPNs (65%), and OR techs (56%). Administering aerosolized medications was uncommon overall (19%), but over half of the respiratory therapists (89%), LPNs (56%), and RNs (55%) performed this task. Only 15% of all participants reported sterilizing medical equipment, but four of every five CSWs (80%) and dental assistants (81%) performed this task. LPNs and RNs were the only occupations with values of at least 50% for three tasks, and NAs were the only occupation that did not exceed 50% for any task.
Table 2.
Frequency of tasks performed by different healthcare occupations, n (%).
| General healthcare task | Total | Healthcare Occupation | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| NAs | CSWs | Dental Assistants | ESWs | Lab Techs | LPNs | OR Techs | RNs | Resp. Therapists | ||
| N | 2030 | 702 | 41 | 32 | 374 | 166 | 297 | 63 | 280 | 75 |
| Clean fixed surfaces | 1291 (64) | 284 (40) | 30 (73) | 27 (84) | 307 (82) | 117 (70) | 218 (73) | 29 (46) | 222 (79) | 57 (76) |
| Sterilize medical equipment | 301 (15) | 52 (7.4) | 33 (80) | 26 (81) | 48 (13) | 27 (16) | 43 (14) | 16 (25) | 33 (12) | 23 (38) |
| Administer aerosolized medications | 395 (19) | 3a (0.4) | 1a (2.4) | 2a (6.3) | 0a (0.0) | 1a (0.6) | 167 (56) | 1a (1.6) | 153 (55) | 67 (89) |
| Use chemicals, adhesives, or solvents on patients | 646 (32) | 130 (19) | 5 (12) | 13 (41) | 12 (3.2) | 28 (17) | 193 (65) | 35 (56) | 201 (72) | 29 (39) |
Abbreviations for occupations - NAs: nursing assistants, CSWs: central supply workers, ESWs: environmental service workers, Lab Techs: laboratory technicians, LPNs: licensed practical nurses, OR Techs: operating room technicians, RNs: registered nurses, Resp. Therapists: respiratory therapists or technicians.
Cell has < 5 participants.
3.3. Association of asthma outcomes with occupation
The crude frequencies of asthma-related outcomes by occupation (Table 3) revealed that the five occupations with fewer than 200 participants (i.e., CSWs, dental assistants, OR techs, respiratory therapists, and lab techs) were more likely to have < 5 participants with an outcome than the other four more populous occupations. For results without small numbers, the highest crude values included 7.5% posthire asthma and 12% current asthma for RNs, 5.4% any exacerbation for LPNs and RNs, 32% BHR-related symptoms for CSWs, a mean asthma score of 0.66 for dental assistants, and 19% wheeze for respiratory therapists. When cell sizes were sufficiently large, there were few statistically significant associations of asthma outcomes with occupation, based on the results from regression models that adjusted for other risk factors and potential confounders (Online Supplement Table S4). The odds of having current asthma was significantly increased in both ESWs and RNs compared to NAs, with OR = 1.70 (95% CI 1.01, 2.84) and OR = 1.89 (95% CI 1.15, 3.13), respectively. In addition, LPNs had an elevated OR for moderate exacerbation of asthma (OR = 2.84, 95% CI 1.17, 6.92).
Table 3.
Frequency of asthma-related outcomes by occupation.
| Asthma-related Outcomes | NAs N = 702 | CSWs N = 41 | Dental Assistants N = 32 | ESWs N = 374 | Lab Techs N = 166 | LPNs N = 297 | OR Techs N = 63 | RNs N = 280 | Resp. Therapists N = 75 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (mean, SEM) | % | n (mean, SEM) | % | n (mean, SEM) | % | n (mean, SEM) | % | n (mean, SEM) | % | n (mean, SEM) | % | n (mean, SEM) | % | n (mean, SEM) | % | n (mean, SEM) | % | |
| Physician-diagnosed asthma | 68 | 9.7 | 3a | 7.3 | 3a | 9.4 | 42 | 11 | 10 | 6.0 | 40 | 13 | 6 | 10 | 41 | 15 | 10 | 13 |
| Post-hire asthma | 34 | 4.8 | 1a | 2.4 | 3a | 9.4 | 15 | 4.0 | 4a | 2.4 | 19 | 6.4 | 3a | 4.8 | 21 | 7.5 | 3a | 4.0 |
| Current asthma | 50 | 7.1 | 3a | 7.3 | 3a | 9.4 | 34 | 9.1 | 6 | 3.6 | 33 | 11 | 4a | 6.3 | 33 | 12 | 7 | 9.3 |
| Any exacerbation | 25 | 3.6 | 2a | 4.9 | 2a | 6.3 | 9 | 2.4 | 3a | 1.8 | 16 | 5.4 | 0a | 0.0 | 15 | 5.4 | 2a | 2.7 |
| Moderate exacerbation | 10 | 1.4 | 1a | 2.4 | 1a | 3.1 | 7 | 1.9 | la | 0.6 | 13 | 4.4 | 0a | 0.0 | 7 | 2.5 | 1a | 1.3 |
| Severe exacerbation | 15 | 2.1 | 1a | 2.4 | 1a | 3.1 | 2a | 0.5 | 2a | 1.2 | 3a | 1.0 | 0a | 0.0 | 8 | 2.9 | 1a | 1.3 |
| BHR-related symptoms | 178 | 25 | 13 | 32 | 9 | 28 | 99 | 26 | 36 | 22 | 87 | 29 | 14 | 22 | 72 | 26 | 14 | 19 |
| Asthma symptom score (mean, SEM) | (0.48, 0.04) | (0.44, 0.15) | (0.66, 0.24) | (0.49, 0.05) | (0.40, 0.07) | (0.53, 0.06) | (0.40, 0.09) | (0.48, 0.06) | (0.52, 0.13) | |||||||||
| Asthma symptom score | ||||||||||||||||||
| 0 | 526 | 75 | 30 | 73 | 23 | 72 | 283 | 76 | 127 | 77 | 214 | 72 | 46 | 73 | 204 | 73 | 58 | 77 |
| 1 | 95 | 14 | 7 | 17 | 3a | 9.4 | 45 | 12 | 27 | 16 | 40 | 13 | 11 | 17 | 44 | 16 | 5 | 6.7 |
| 2–5 | 81 | 12 | 4a | 9.8 | 6 | 19 | 46 | 12 | 12 | 7.2 | 43 | 14 | 6 | 9.5 | 32 | 11 | 12 | 16 |
| Wheezing or whistling in last 12 months | 92 | 13 | 5 | 12 | 3a | 9.4 | 54 | 14 | 20 | 12 | 54 | 18 | 7 | 11 | 42 | 15 | 14 | 19 |
Abbreviations for occupations - NAs: nursing assistants, CSWs: central supply workers, ESWs: environmental service workers, Lab Techs: laboratory technicians, LPNs: licensed practical nurses, OR Techs: operating room technicians, RNs: registered nurses, Resp. Therapists: respiratory therapists or technicians.
Cell has < 5 participants with the outcome.
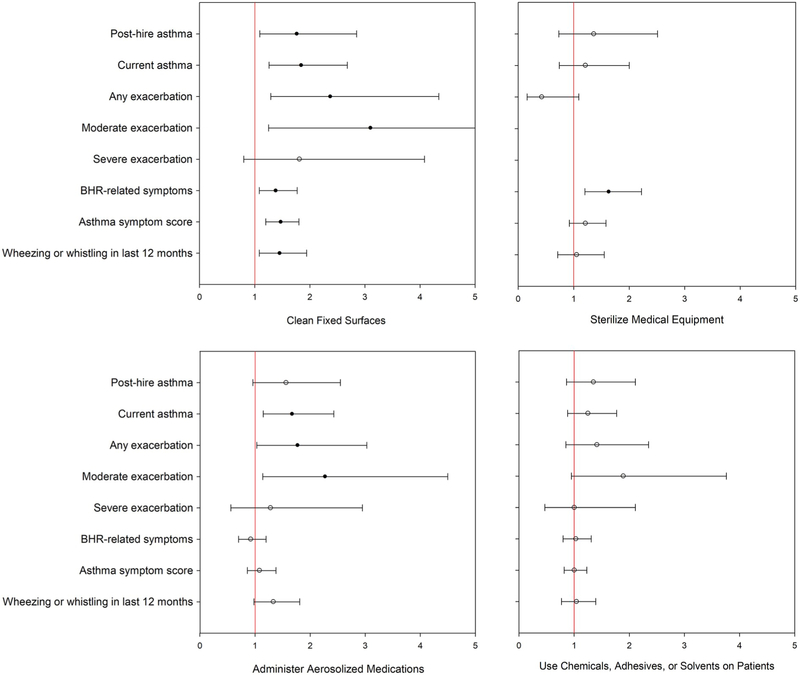
3.4. Association of asthma outcomes with healthcare task
The crude frequency of outcomes by the four healthcare tasks are available in Table 4. Participants who administered aerosolized medications had the highest percentages for post-hire asthma (6.6%), current asthma (12%), any exacerbation (5.3%), and wheeze (18%); sterilizing medical equipment had the top frequency of 32% for BHR-related symptoms; and all four tasks were more likely to have nonzero asthma scores relative to the entire sample. From regression models that adjusted for other risk factors and potential confounders, cleaning fixed surfaces had statistically significant associations with most outcomes, as seen in Fig. 2 and Table S5 in the Online Supplement. These associations included OR = 1.76 (95% CI 1.09, 2.85) for post-hire asthma, OR = 1.84 (95% CI 1.26, 2.68) for current asthma, OR = 3.10 (95% CI 1.25, 7.67) for moderate exacerbation, OR = 1.38 (95% CI 1.08, 1.77) for BHR-related symptoms, a ratio mean asthma score of 1.47 (95% CI 1.20, 1.80), and OR = 1.45 (95% CI 1.08, 1.94) for wheeze. Results for the other three tasks were more like those for occupations, with few or no statistically significant results. Current asthma (OR = 1.67, 95% CI 1.15, 2.43), any exacerbation (OR = 1.77, 95% CI 1.03, 3.03), and moderate exacerbation (OR = 2.27, 95% CI 1.14, 4.50) were associated with administering aerosolized medications; BHR-related symptoms was associated with sterilizing medical equipment (OR = 1.63, 95% CI 1.20, 2.22); and using chemicals, adhesives, or solvents on patients had no statistically significant associations with any health outcome.
Table 4.
Frequency of asthma-related outcomes by work tasks.
| Asthma-related Outcomes | Total N = 2030 | Clean fixed surfaces N = 1291 | Sterilize medical equipment N = 301 | Administer aerosolized drugs N = 395 | Use chemicals on patients N = 646 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n (mean, SEM) | % | n (mean, SEM) | % | n (mean, SEM) | % | n (mean, SEM) | % | n (mean, SEM) | % | |
| Physician-diagnosed asthma | 223 | 11 | 161 | 12 | 37 | 12 | 60 | 15 | 82 | 13 |
| Post-hire asthma | 103 | 5.1 | 74 | 5.7 | 15 | 5.0 | 26 | 6.6 | 40 | 6.2 |
| Current asthma | 173 | 8.5 | 129 | 10 | 25 | 8.3 | 48 | 12 | 64 | 9.9 |
| Any exacerbation | 74 | 3.6 | 58 | 4.5 | 5 | 1.7 | 21 | 5.3 | 30 | 4.6 |
| Moderate exacerbation | 41 | 2.0 | 34 | 2.6 | 3a | 1.0 | 13 | 3.3 | 19 | 2.9 |
| Severe exacerbation | 33 | 1.6 | 24 | 1.9 | 2a | 0.7 | 8 | 2.0 | 11 | 1.7 |
| BHR-related symptoms | 522 | 26 | 363 | 28 | 95 | 32 | 105 | 27 | 175 | 27 |
| Asthma symptom score (mean, SEM) | (0.46, 0.02) | (0.55, 0.03) | (0.55, 0.06) | (0.55, 0.05) | (0.50, 0.04) | |||||
| Asthma symptom score, n and % | ||||||||||
| 0 | 1511 | 74 | 922 | 71 | 210 | 70 | 280 | 71 | 468 | 72 |
| 1 | 277 | 14 | 192 | 15 | 52 | 17 | 59 | 15 | 95 | 15 |
| 2 | 115 | 5.7 | 83 | 6.4 | 19 | 6.3 | 30 | 7.6 | 48 | 7.4 |
| 3 | 63 | 3.1 | 48 | 3.7 | 10 | 3.3 | 15 | 3.8 | 15 | 2.3 |
| 4 | 35 | 1.7 | 24 | 1.9 | 5 | 1.7 | 3a | 0.8 | 10 | 1.5 |
| 5 | 29 | 1.4 | 22 | 1.7 | 5 | 1.7 | 8 | 2.0 | 10 | 1.5 |
| Wheezing or whistling in last 12 months | 291 | 14 | 206 | 16 | 42 | 14 | 73 | 18 | 100 | 15 |
Cell has < 5 participants with the outcome.
Fig. 2.
Odds ratios and ratio mean scores with 95% confidence intervals for association of asthma-related outcomes with four healthcare tasks.
Solid dots indicate p ≤ 0.05 and open dots indicate p > 0.05.
The vertical red line in each graph represents the null value of 1.0.
Most results are an odds ratio (OR) and 95% confidence interval (95% CI) from logistic regression models. However, for the asthma symptom score, the results are a ratio mean score and 95% CI from a negative binomial regression model. All results were adjusted for age, gender, race, smoking status, and history of allergies. Moderate and severe exacerbation were included as outcomes in the same model using polytomous regression.
ORs were not reported for the association of moderate and severe exacerbation with sterilize medical equipment because < 5 participants who performed this task had the outcome.
4. Discussion
4.1. Summary of findings
The ECRHS was one of the first large studies to describe the association of asthma outcomes with cleaning-related activities (Kogevinas et al., 1999). Subsequent studies have confirmed this association in healthcare settings (Arif and Delclos, 2012; Arif et al., 2009; Mirabelli et al., 2007; Vizcaya Fernández et al., 2011). We surveyed a sample of urban healthcare workers in the U.S. to investigate the association of asthma-related outcomes with healthcare occupations and tasks, including cleaning and disinfecting. ESWs were the workers in this study whose primary responsibility was cleaning, and they had increased odds of current asthma. Two occupations responsible for patient care, LPNs and RNs, had elevated ORs for moderate exacerbation of asthma and current asthma, respectively. Among the tasks, sterilizing medical equipment was significantly associated with BHR-related symptoms and administering aerosolized medications was associated with current asthma, any exacerbation, and moderate exacerbation. However, the most notable findings were for the task of cleaning fixed surfaces, which was significantly associated with nearly all the outcome variables, including post-hire asthma, current asthma, any exacerbation, moderate exacerbation, BHR-related symptoms, asthma score, and wheeze. These findings are consistent with reports from other studies that exposure to cleaning-related substances have a significant impact on the development of adverse respiratory health outcomes (Arif and Delclos, 2012; Bello et al., 2009; Delclos et al., 2007; Gonzalez et al., 2014). Further, the current findings suggest that task was a more proximal surrogate of cleaning-related exposures than occupation when studying asthma outcomes in this workforce.
4.2. Post-hire asthma, current asthma and exacerbation of current asthma
The study of healthcare workers conducted in Texas focused on post-hire asthma, defined as asthma with onset after entering healthcare work, with prevalence estimates of 6.6% overall, 7.3% for nurses, and 5.6% for respiratory therapists (Delclos et al., 2007). The prevalence of post-hire asthma in the current sample was somewhat lower, with 5.1% (n = 103) overall, 6.9% for nurses (RNs and LPNs combined), and 4.0% for respiratory therapists. The positive associations of this health outcome in our analyses were limited to cleaning fixed surfaces, while the researchers in Texas reported associations with nurses and all four tasks considered in the current study (Delclos et al., 2007).
The 8.5% prevalence estimate for current asthma observed in this study is similar to results from the National Health Interview Survey (NHIS) in the U.S. Based on 2004–2011 NHIS data, the prevalence of current asthma was 7.5% for health diagnosing and treating practitioners, 7.1% for health technologists and technicians, 10.0% for nursing, psychiatric, and home health aides, and 6.3% for other healthcare support occupations (NIOSH, 2015). However, a recent study of 347 healthcare workers in Milwaukee, Wisconsin, reported a higher prevalence of 17.6% for current asthma (Kurth et al., 2017).
Both ESWs and RNs had elevated odds of current asthma (Online Supplement Table S4), but the responsible exposures may have differed between these two occupations. While the vast majority of both ESWs (82%) and RNs (79%) cleaned fixed surfaces, very few ESWs did other tasks, while most RNs also performed the patient-care tasks of administering aerosolized medications and using substances on patients (Table 2). Current asthma was associated with both cleaning fixed surfaces and administering aerosolized medications (Online Supplement Table S5). A majority of LPNs and respiratory therapists also engaged in these two activities, and their ORs for current asthma were elevated but not statistically significant (Online Supplement Table S4). Moderate exacerbation of asthma was significantly associated with LPNs and the tasks of cleaning fixed surfaces and administering aerosolized medications, two tasks that a majority of LPNs performed.
4.3. BHR-related symptoms
The prevalence of BHR-related symptoms was nearly the same for the current and Texas studies of healthcare workers, with estimates of 26% and 27%, respectively (Delclos et al., 2007). While the prevalence among nurses was similar in the current and Texas samples (28% and 29%, respectively), it was greater for respiratory therapists surveyed in Texas (19% and 30%, respectively) (Delclos et al., 2007). The Texas study found BHR-related symptoms associated with three occupations (nurses, respiratory and occupational therapists) relative to physicians, and with all four tasks that were also evaluated in the current investigation. The current results for this health outcome included statistically significant relationships with the two tasks of cleaning fixed surfaces and sterilizing medical equipment, but with none of the occupations (Online Supplement Tables S5 and S4, respectively). The association of sterilizing medical equipment with BHR-related symptoms but not current asthma suggests the participants who fulfilled the criteria for this symptom algorithm but not current asthma had a considerable influence on the association. While 75% (130/173) of participants with current asthma also fulfilled the criteria for BHR-re-lated symptoms, there were also many (n = 392) with the latter but not the former.
4.4. Strengths and limitations
The population sample accounts for many of the strengths of the current research. Although other researchers have examined the effect of healthcare occupation on various respiratory outcomes (Arif et al., 2009; Delclos et al., 2007; Le Moual et al., 2013), this study examined the association of asthma-related outcomes with a broad array of occupations that included predominantly lower-skill jobs such as NAs and ESWs that were not previously studied. For example, research in Texas examined physicians, occupational therapists, nurses, and respiratory therapists (Delclos et al., 2007), and the Nurses’ Health Study was limited to RNs (Le Moual et al., 2013). Further, the current study sample had a different race distribution than in many other studies, with substantial minority representation, notably 62% African American (Delclos et al., 2007; Le Moual et al., 2013). Multiple measures of asthma were available for analysis, weights were applied to adjust for potential selection and non-participation bias, and covariates were included to adjust for other risk factors and potential confounders when modelling health outcomes.
The study had several limitations. The low participation rate of 13.3% raises concerns about whether participants were representative of the sample frame. Several factors suggest that the current results are not necessarily impacted by non-participation bias. First, there is a robust literature demonstrating that participation rate alone is a poor determinant of bias (Galea and Tracy, 2007; Groves, 2006; Mannetje et al., 2011; Morton et al., 2012; Peytchev, 2013). The potential for bias exists across the range of participation rates, including the current study and studies with higher participation rates. There is neither a participation rate below which the results are always biased nor a rate above which the results are always safe from bias. Second, non-participants as well as participants provided enough data to develop weights that were applied in regression models to adjust for potential selection and non-participation bias, with the goal of yielding results representative of the sample frame. However, we cannot be certain that the 939 individuals who finished either the non-responder survey or part of the main survey, and whose information was used in the calculating the non-participation weights, were truly representative of all non-participants. In other words, despite our best efforts to adjust for non-participation, we cannot be certain that the current results are free from bias due to unequal participation. Finally, the observation that results from this study are similar to results from other studies of healthcare workers, notably the study in Texas, argues against bias.
It is relevant to consider other potential limitations as well. First, due to the study’s cross-sectional design, the temporal sequence of occupational exposures followed by respiratory outcomes is uncertain. Second, small sample sizes were common when examining outcomes that had fewer than 200 cases overall (e.g., post-hire asthma, current asthma, exacerbation), especially in occupations with fewer than 200 participants. We did not report adjusted ORs for cells with < 5 cases, and the missing OR estimates in Online Supplement Table S4 illustrate the limitations of this study to test whether healthcare occupations were risk factors for asthma-related outcomes. As an example of the limited power for certain comparisons, the prevalence of post-hire asthma was almost twice as great for dental assistants (9.4%, 3/32) as for NAs (4.8%, 34/702) (Table 3), but the two-tail Fisher exact test for this comparison yielded p = 0.21. With the same number of NA participants and no change in the prevalences of the health outcome, the number of dental assistants would have to be five times as great (or n = 160) to yield p ≤ 0.05. Third, the study relied on self-reports of health outcomes and tasks, and differential reporting of tasks, and especially over-reporting by participants with symptoms or diseases, could have possibly biased effect estimates away from the null (De Vocht et al., 2005). However, the questions that made up the outcome definitions mostly pertained to the last 12 months, which likely limited inaccurate recall compared to requesting details about health events that occurred years earlier. Fourth, the current assessment of occupational exposure is basic and would be improved by using reports of product use and metrics that estimate chemical exposures. With this in mind, we are constructing job/task exposure matrices based on measurements of airborne exposures in healthcare settings. We plan to apply the new matrices in future analyses of health data from this project. Fifth, the current sample was not representative of all healthcare workers in the U.S., which could limit the generalization of findings. For example, the percentage of participants who were African American in this study was 79% for NAs, 72% for LPNs, and 51% for RNs, compared to national estimates of 38%, 30%, and 12%, respectively (Online Supplement Table S3) (BLS, 2017).
4.5. Conclusions and additional research
Healthcare settings provide opportunities for possible exposure to various irritants and sensitizers that may contribute to adverse respiratory effects. In the current study, work task, and especially cleaning fixed surfaces, performed better as a risk factor for asthma-related outcomes than healthcare occupation. The association of asthma outcomes with cleaning fixed surfaces suggests that additional refinement of the cleaning task variable (e.g., by type of surface cleaning task and products used) might provide additional insights for prevention. While fewer associations were observed between asthma outcomes and the tasks of sterilizing medical equipment and administering aerosolized medications, an analysis of specific activities and products related to these tasks might also provide findings that could inform prevention. Future studies of the association of asthma-related outcomes with different exposure metrics based on the tasks, products, and chemicals encountered when conducting cleaning and other activities in healthcare could potentially lead to focused recommendations for reducing exposures of concern.
Supplementary Material
Acknowledgements
The authors express sincere thanks to the healthcare workers who completed the surveys; the social scientists at the National Center for Health Statistics who conducted cognitive interviewing, the results of which were used to improve the questionnaires; staff of RTI International who coordinated the field work; and staff at the Service Employees International Union Survey Research Center who administered the telephone surveys.
Funding source
National Institute for Occupational Safety and Health.
Footnotes
Publisher's Disclaimer: Disclaimer
Publisher's Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention.
Declarations of interest
None.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijheh.2018.10.001.
References
- Arif AA, Delclos GL, 2012. Association between cleaning-related chemicals and work-related asthma and asthma symptoms among healthcare professionals. Occup. Environ. Med 69, 35–40. [DOI] [PubMed] [Google Scholar]
- Arif AA, Delclos GL, Serra C, 2009. Occupational exposures and asthma among nursing professionals. Occup. Environ. Med 66, 274–278. [DOI] [PubMed] [Google Scholar]
- Bakerly ND, Moore VC, Vellore AD, Jaakkola MS, Robertson AS, Burge PS, 2008. Fifteen-year trends in occupational asthma: data from the Shield surveillance scheme. Occup. Med. (Lond.) 58, 169–174. [DOI] [PubMed] [Google Scholar]
- Bello A, Quinn MM, Perry MJ, Milton DK, 2009. Characterization of occupational exposures to cleaning products used for common cleaning tasks-a pilot study of hospital cleaners. Environ. Health 8, 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BLS, 2017. Employed Persons by Detailed Occupation, Sex, Race, and Hispanic or Latino Ethnicity. U.S. Bureau of Labor Statistics. https://www.bls.gov/cps/cpsaat11.pdf (accessed 18.01.08).
- BLS, 2017a. 12-Month Percent Change: Medical Care in U.S. City Average, All Urban Consumers, Not Seasonally Adjusted. U. S. Bureau of Labor Statistics. https://data.bls.gov/pdq/SurveyOutputServlet (accessed 17.05.16).
- Burney PGJ, Luczynska C, Chinn S, Jarvis D, 1994. The European community respiratory health survey. Eur. Respir. J 7, 954–960. [DOI] [PubMed] [Google Scholar]
- De Vocht F, Zock JP, Kromhout H, Sunyer J, Antó JM, Burney P, Kogevinas M, 2005. Comparison of self-reported occupational exposure with a job exposure matrix in an international community-based study on asthma. Am. J. Ind. Med 47, 434–442. [DOI] [PubMed] [Google Scholar]
- Delclos GL, Arif AA, Aday L, Carson A, Lai D, Lusk C, Stock T, Symanski E, Whitehead LW, Benavides FG, Anto JM, 2006. Validation of an asthma questionnaire for use in healthcare workers. Occup. Environ. Med 63, 173–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delclos GL, Gimeno D, Arif AA, Burau KD, Carson A, Lusk C, Stock T, Symanski E, Whitehead LW, Zock JP, Benavides FG, Anto JM, 2007. Occupational risk factors and asthma among health care professionals. Am. J. Respir. Crit. Care Med 175, 667–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodd KE, Mazurek JM, 2016. Asthma among employed adults, by industry and occupation - 21 states, 2013. MMWR Morb. Mortal. Wkly. Rep 65, 1325–1331. [DOI] [PubMed] [Google Scholar]
- Dumas O, Donnay C, Heederik DJ, Hery M, Choudat D, Kauffmann F, Le Moual N, 2012. Occupational exposure to cleaning products and asthma in hospital workers. Occup. Environ. Med 69, 883–889. [DOI] [PubMed] [Google Scholar]
- Ferris BG, 1978. Epidemiology standardization project (american thoracic society). Am. Rev. Respir. Dis 118, 1–120. [PubMed] [Google Scholar]
- Galea S, Tracy M, 2007. Participation rates in epidemiologic studies. Ann. Epidemiol 17, 643–653. [DOI] [PubMed] [Google Scholar]
- Gonzalez M, Jégu J, Kopferschmitt MC, Donnay C, Hedelin G, Matzinger F, Velten M, Guilloux L, Cantineau A, de Blay F, 2014. Asthma among workers in healthcare settings: role of disinfection with quaternary ammonium compounds. Clin. Exp. Allergy 44, 393–406. [DOI] [PubMed] [Google Scholar]
- Groves RM, 2006. Nonresponse rates and nonresponse bias in household surveys. Publ. Opin. Q 70, 646–675. [Google Scholar]
- Henneberger PK, Redlich CA, Callahan DB, Harber P, Lemiere C, Martin J, Tarlo SM, Vandenplas O, Toren K, 2011. An official american thoracic society statement: work-exacerbated asthma. Am. J. Respir. Crit. Care Med 184, 368–378. [DOI] [PubMed] [Google Scholar]
- Jarvis D, 2002. The European community respiratory health survey II. Eur. Respir. J 20, 1071–1079. [DOI] [PubMed] [Google Scholar]
- Koehoorn M, Tamburic L, McLeod CB, Demers PA, Lynd L, Kennedy SM, 2013. Population-based surveillance of asthma among workers in British Columbia, Canada. Chronic Diseases and Injuries in Canada 33, 88–94. [PubMed] [Google Scholar]
- Kogevinas M, Antó JM, Sunyer J, Tobias A, Kromhout H, Burney P, 1999. Occupational asthma in Europe and other industrialised areas: a population-based study. Lancet 353, 1750–1754. [DOI] [PubMed] [Google Scholar]
- Kurth L, Virji MA, Storey E, Framberg S, Kallio C, Fink J, Laney AS, 2017. Current asthma and asthma-like symptoms among workers at a veterans administration medical center. Int. J. Hyg Environ. Health 220, 1325–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Moual N, Varraso R, Zock JP, Henneberger P, Speizer FE, Kauffmann F, Camargo CA, 2013. Are operating room nurses at higher risk of severe persistent asthma? the nurse’s health study. J. Occup. Environ. Med 55, 973–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBouf RF, Virji MA, Saito R, Henneberger PK, Simcox N, Stefaniak AB, 2014. Exposure to volatile organic compounds in healthcare settings. Occup. Environ. Med 71, 642–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh JP, Romano PS, Schenker MB, Kreiss K, 2002. Costs of occupational COPD and asthma. Chest 121, 264–272. [DOI] [PubMed] [Google Scholar]
- Liss GM, Buyantseva L, Luce CE, Ribeiro M, Manno M, Tarlo SM, 2011. Work-related asthma in health care in Ontario. Am. J. Ind. Med 54, 278–284. [DOI] [PubMed] [Google Scholar]
- Mannetje A, Eng A, Douwes J, Ellison-Loschmann L, McLean D, Pearce N, 2011. Determinants of non-response in an occupational exposure and health survey in New Zealand. Aust. N. Z. J. Public Health 35, 256–263. [DOI] [PubMed] [Google Scholar]
- Mirabelli MC, Zock JP, Plana E, Anto JM, Benke G, Blanc PD, Dahlman-Hoglund A, Jarvis DL, Kromhout H, Lillienberg L, Norback D, Olivieri M, Radon K, Sunyer J, Toren K, van Sprundel M, Villani S, Kogevinas M, 2007. Occupational risk factors for asthma among nurses and related healthcare professionals in an international study. Occup. Environ. Med 64, 474–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moorman JE, Akinbami LJ, Bailey CM, Zahran HS, King ME, Johnson CA, Liu X, 2012. National surveillance of asthma: United States, 2001–2010. Vital Health Statistics - Ser. 3 Anal. Epidemiol. Stud 1–58. [PubMed] [Google Scholar]
- Morton SMB, Bandara DK, Robinson EM, Atatoa Carr PE, 2012. In the 21st Century, what is an acceptable response rate? Aust. N. Z. J. Public Health 36, 106–108. [DOI] [PubMed] [Google Scholar]
- NIOSH, 2015. Current Asthma: Estimated Prevalence by Occupation and Sex U.S. Working Adults Aged ≥18 Years, NHIS 2004–2011, Work-related Lung Disease Surveillance System (EWoRLD). 2015–870. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, Respiratory Health Division, Morgantown, WV. [Google Scholar]
- Pechter E, Davis LK, Tumpowsky C, Flattery J, Harrison R, Reinisch F, Reilly MJ, Rosenman KD, Schill DP, Valiante D, Filios M, 2005. Work-related asthma among health care workers: surveillance data from California, Massachusetts, Michigan, and New Jersey, 1993–1997. Am. J. Ind. Med 47, 265–275. [DOI] [PubMed] [Google Scholar]
- Pekkanen J, Sunyer J, Antó JM, Burney P, 2005. Operational definitions of asthma in studies on its aetiology. Eur. Respir. J 26, 28–35. [DOI] [PubMed] [Google Scholar]
- Peytchev A, 2013. Consequences of survey nonresponse. Ann. Am. Acad. Pol. Soc. Sci 645, 88–111. [Google Scholar]
- Reddel HK, Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, Casale TB, Chanez P, Enright PL, Gibson PG, De Jongste JC, Kerstjens HAM, Lazarus SC, Levy ML, O’Byrne PM, Partridge MR, Pavord ID, Sears MR, Sterk PJ, Stoloff SW, Sullivan SD, Szefler SJ, Thomas MD, Wenzel SE, 2009. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations - standardizing endpoints for clinical asthma trials and clinical practice. Am. J. Respir. Crit. Care Med 180, 59–99. [DOI] [PubMed] [Google Scholar]
- Saito R, Virji MA, Henneberger PK, Humann MJ, LeBouf RF, Stanton ML, Liang X, Stefaniak AB, 2015. Characterization of cleaning and disinfecting tasks and product use among hospital occupations. Am. J. Ind. Med 58, 101–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunyer J, Pekkanen J, Garcia-Esteban R, Svanes C, Künzli N, Janson C, De Marco R, Antó JM, Burney P, 2007. Asthma score: predictive ability and risk factors. Allergy 62, 142–148. [DOI] [PubMed] [Google Scholar]
- Torén K, Blanc PD, 2009. Asthma caused by occupational exposures is common - a systematic analysis of estimates of the population-attributable fraction. BMC Pulm. Med 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vizcaya Fernández D, Mirabelli MC, Antó JM, Orriols R, Burgos F, Arjona L, Zock JP, 2011. A workforce-based study of occupational exposures and asthma symptoms in cleaning workers. Occup. Environ. Med 68, 914–919. [DOI] [PubMed] [Google Scholar]
- Walters GI, Moore VC, McGrath EE, Burge PS, Henneberger PK, 2013. Agents and trends in health care workers’ occupational asthma. Occup. Med. (Lond.) 63, 513–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.