Abstract
Ectopic varices are complex and highly variable entities that are not fully understood. Duodenal varices from pancreatitis have rarely been reported. Ectopic varices have much higher bleeding rates than the more common gastro-esophageal varices, and are associated with higher mortality. The ideal management of this difficult problem is not only to ensure prompt hemostasis, but also address the etiology or hemodynamics of the ectopic varices. We discuss the endovascular management of bleeding duodenal varices, which developed from superior mesenteric vein occlusion, following repeated attacks of pancreatitis. This unusual case was managed by a multidisciplinary collaborative approach between the gastrointestinal service and Interventional radiology. The classification system for ectopic varices and management options has been discussed in some detail. Medium term follow-up (8 months), at the time of this writing, showed that the patient is doing well, without interval hematemesis, imaging findings of recurrent/new varices or stent occlusion.
Keywords: Balloon-occluded antegrade transvenous obliteration, balloon-occluded retrograde transvenous obliteration, ectopic varices, endoscopic procedures, Gastrointestinal bleeding, pancreatitis, SMV recanalization, SMV stent, Transjugular intrahepatic porto-sytemic shunt
Background
Ectopic varices are dilated splanchnic veins and/or portosystemic collaterals that can occur anywhere in the gastrointestinal tract, other than the gastroesophageal and anorectal regions. [Table 1][1] Ectopic varices account for 2%-5% of all gastrointestinal tract variceal bleeding.[2] However, ectopic varices have a 4-fold increased risk of bleeding when compared with gastroesophageal varices,[2] and can have mortality rates as high as 40%.[3] Unfortunately, reports of ectopic varices in the literature are rare and no definite treatment algorithms have been established to ideally manage these varices.
Table 1.
Location of ectopic varices in the GI tract
| Primary location | Subtype | Frequency |
|---|---|---|
| Stomal or Parastomal | Ileostomy/Colostomy/Cecostomy/Diverting urinary ileostomy | 28% of ectopic varices 50% of ectopic bleeds |
| Jejunoileal (lower GI small bowel) | Intra-abdominal stomal or parastomal | 18% of ectopic varices 7-12% of ectopic bleeds |
| Duodenal (upper GI small bowel) | None | 17% of ectopic varies 25-33% of ectopic bleeds |
| Colonic (large bowel) | Intra-abdominal stomal or parastomal | 15% of ectopic varices 7-12% of ectopic bleeds |
| Ectopic Gastric (noncardiofundic; sarin classification type-IV) | Body of Stomach or Antrum/Gastric outlet | Not commonly clinically significant |
Reprinted from Techniques in Vascular and Interventional Radiology, Vol 16:2; Wael E.A Saad, Allison Lippert, Nael E. Saad, Stephen Caldwell; Ectopic Varices: Anatomical Classification, Hemodynamic Classification, and Hemodynamic-Based Management; Pages 158-175; Copyright Year 2013; with permission from Elsevier. Reformatted from the original
Case Presentation
A 41-year-old male patient presented to the emergency room (ER) with multiple episodes of dark bloody stools and left lower quadrant abdominal pain. Prior history (5 years ago), was significant for necrotizing gall stone pancreatitis, initially treated conservatively, followed by interval cholecystectomy. About three years following this event, the patient had episodes of hematemesis due to splenic vein thrombosis and formation of gastric varices, and was treated with splenectomy/distal pancreatectomy. Computed tomography (CT) imaging during his current visit demonstrated changes of distal pancreatectomy, splenectomy, 2.5 cm cyst in the region of the tail of the pancreas, and severe desmoplastic reaction surrounding the superior mesenteric vein (SMV), causing complete occlusion [Figures 1A and B]. Large duodenal varices were also identified.
Figure 1 (A and B).
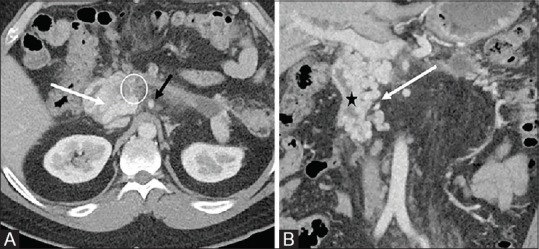
Axial (A), coronal (B) contrast enhanced abdominal CT showing large duodenal varices (white arrows). Severe desmoplastic reaction in the region of the superior mesenteric vein, causing complete occlusion (white circle). Superior mesenteric artery patent (black arrow). The black star corresponds to the duodenal lumen
Lab values were significant for a drop-in hemoglobin and hematocrit (H and H) at 10 g/dl (previously 14 g/dl).
He was admitted to the gastrointestinal (GI) service, and subsequently upper/lower GI tract endoscopies were performed. The upper GI endoscopy showed active oozing of bright red blood from the varices in the D2 segment of the duodenum. Two clips were placed at the site to successfully control the bleeding. The varices demonstrated high-risk stigmata for future bleeding.
The case was presented at the multidisciplinary conference for input from Interventional radiology (IR), Hepato-biliary and Vascular surgery. From the history and imaging, it was obvious that the varices were from the SMV occlusion, and the best way to relieve the obstruction was to create a bypass or a shunt to divert the flow into the portal vein. However, vascular and hepatobiliary surgery were not keen about surgical reconstruction or bypass, quoting poor patency for surgical reconstruction and the difficulty of abdominal surgery in the background of prior operations (cholecystectomy, distal pancreatectomy, splenectomy) and pancreatitis. At this point IR was asked to attempt endovascular recanalization of the occluded SMV.
Recanalization Procedure
Ultrasound guided right portal vein access was obtained with a micro puncture needle. Following a series of exchanges, a 6 French 25 cm vascular sheath (Terumo Medical Corp, Somerset, New Jersey) was placed in the main portal vein. Contrast venogram via a pigtail catheter introduced through the sheath, showed a patent portal vein. A nubbin was noted at the expected inflow of the SMV. The pigtail catheter was exchanged for a Kumpe catheter (AngioDynamics, Latham, NY) over a stiff Glidewire (Terumo Medical Corp, Somerset, New Jersey), and this combination was utilized to perform recanalization of the superior mesenteric vein. After successfully crossing the occlusion, a digital subtraction angiography (DSA) was performed with the Kumpe catheter in the distal superior mesenteric vein branches. This confirmed the CT findings of SMV occlusion and massive duodenal varices [Figure 2] (Porto-Portal collaterals). After performing appropriate measurements, a 12 × 60 mm Protégé self-expanding stent (Medtronic, Minneapolis, MN), was deployed across the stenosis, and followed by balloon angioplasty. Final venogram demonstrated excellent antegrade flow through the stent and resolution of the previously seen duodenal varices [Figure 3].
Figure 2.

DSA through the Kumpe catheter positioned in the branches of the SMV (white arrows), after crossing the SMV occlusion. The varices bypassing the occlusion are seen during the injection (white arrow heads)
Figure 3.
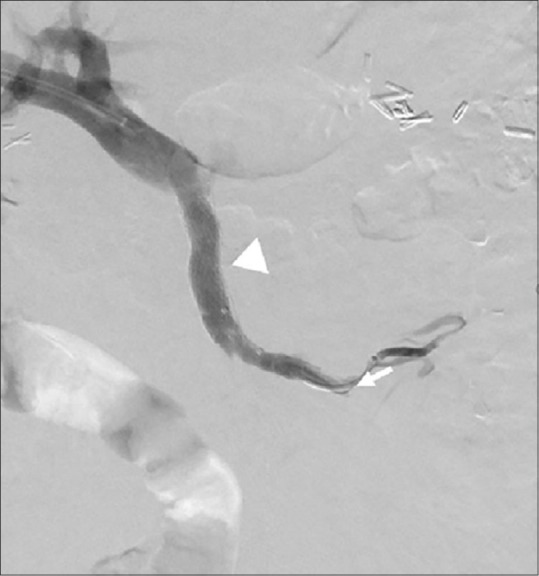
DSA obtained following injection though the catheter in the SMV (white arrow), post stent placement and angioplasty demonstrates brisk flow through a well-expanded stent (arrow head). The previously seen varices are not visualized
The parenchymal access tract was occluded with Azur 0.035 coils (Terumo Medical Corp, Somerset, New Jersey) and gelfoam. The patient tolerated the procedure well and was discharged home in stable condition. Discharge medications included clopidogrel 75 mg daily, after an initial loading dose of 300 mg and Apixaban 5 mg twice daily. A follow up CT [Figures 4A and B], obtained when the patient was seen in the IR clinic 6 months after the procedure, demonstrated a patent stent and disappearance of the previously seen collaterals.
Figure 4 (A and B).
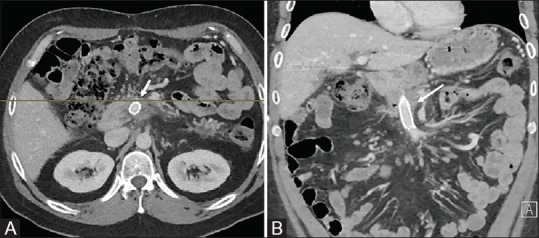
Contrast enhanced axial (A) and coronal (B) CT images obtained 3 months post stent placement. Patent SMV stent (arrow). No varices seen
Discussion
Duodenal varices are ectopic varices which may result from generalized portal hypertension in the absence of splanchnic venous thrombosis (oncotic or type A) or due to splanchnic venous thrombosis (occlusive or type B).[1] The classification of ectopic varices is based on the etiology, afferent (portal feeders) and efferent pathways (systemic drainage). They can be purely porto-portal or mixed type with varying contributions from the portal and systemic circulations [Table 2].[1] Some of the common and rare etiologies of duodenal varices have been mentioned in Table 3.[4]
Table 2.
Classification of Ectopic Varices
| Non-occlusive (oncotic) Type: (Type-a) | Occlusive Type: (Type-b) | |
|---|---|---|
| Portoportal Collaterals | Type-1a | Type-1b |
| Portoportal Collaterals with portosystemic branches | Type-2a | Type-2b |
| Portosysstemic Collaterals with portoportal branches | Type-3a | Type-3b |
Reprinted from Techniques in Vascular and Interventional Radiology, Vol 16:2; Wael E.A Saad, Allison Lippert, Nael E. Saad, Stephen Caldwell; Ectopic Varices: Anatomical Classification, Hemodynamic Classification, and Hemodynamic-Based Management; Pages 158-175; Copyright Year 2013; with permission from Elsevier. Reformatted from the original
Table 3.
Etiology of duodenal varices
| Cirrhosis of Liver |
| Thrombotic disorders and coagulopathies |
| Schistosomiasis |
| Pancreatitis |
| Omphalophlebitis (surgical catheterization of umbilicus in adults) |
| Pancreatic and periportal tumors |
| Mesenteric metastasis |
| Surgical procedure or trauma |
| Visceral hemangiomata (Klipple-Treaunay-Weber Syndrome) |
| Vascular Anomalies (Occlusion of SMV by abnormal ileocecal artery) |
| Retroperitoneal Fibrosis |
Reproduced with permission from reference.[4] Reformatted from the original
Duodenal varices are most commonly found in the first (duodenal bulb), and second (duodenal sweep) portions of the duodenum.[5] The afferent feeders (portal venous) for duodenal varices include superior and inferior pancreaticoduodenal, cystic branches of the superior mesenteric, gastroduodenal, and pyloric veins.[5] The efferent drainage (systemic venous) for the duodenal varices are the right gonadal and the renal capsular veins, which in turn empty into the inferior vena cava.[5] The left gonadal vein may drain duodenal varices that are in the distal duodenum (third and fourth portion), but these are rare.
Diagnosis of duodenal varices is usually made by endoscopy performed for GI bleeding.[6] Doppler ultrasound is mainly used to evaluate the patency and the direction of flow in the portal vein. Contrast-enhanced cross-sectional imaging (MRI and CT) is crucial for the evaluation and management of ectopic varices. These modalities show findings of hepatic cirrhosis, establish the patency of the portal, mesenteric, splenic veins, identify the full extent of the varices and deeper collaterals that are not identified by endoscopy and sometimes demonstrate critical changes in bowel wall and mesentery from splanchnic vein thrombosis.[7] Evaluating the patency of the splanchnic vessels is paramount in classifying the type of ectopic varices, and thus management, of these varices.
As previously discussed, bleeding from ectopic varices, is difficult to control, and is potentially fatal.[3] The ideal management strategy for ectopic varices is not well established, as most of the literature consists of a few case reports and small case series.[2] Interventions for bleeding ectopic varices include local endoscopic treatment, traditional surgical management, transvenous obliteration, decompression utilizing TIPS, percutaneous meso caval shunt or recanalization of the occluded splanchnic vessel.[1]
Endoscopic sclerotherapy has been tried for duodenal varices, but is associated with high rates of rebleeding and ulcers, resulting in life threatening hemorrhage.[8] TIPS and transvenous obliteration either via retrograde (BRTO) or antegrade (BATO) approach, or combination of both have very favorable outcomes in treatment of gastroesophageal varices. In fact, in a recent retrospective study, Mukund et al. showed no re-bleeding from gastric varices, following Sodium Tetradecyl Sulfate (STS) foam sclerosis of portosystemic shunts with a mean diameter of 19 mm.[9] However both these techniques have a very high re-bleeding rate when used to treat ectopic varices.[1] Surgical management of ectopic varcies includes resection of varices with the involved bowel (e.g., duodenectomy). Portocaval shunt surgery has been used in some patients, however the postoperative morbidity and mortality rates are high.[10] Recently, the meso-Rex shunt has been successfully used to treat patients with extrahepatic portal vein obstruction.[11]
Reports of bleeding duodenal varices as a complication of chronic pancreatitis and SMV occlusion is extremely rare.[4]
There have been a very few case reports of SMV recanalization in English literature, which involved combined transhepatic and transmesenteric laproscopic approach[12] or a TIPS approach.[13] There has been no case report in the English literature which describes successful transhepatic endovascular recanalization of a completely occluded superior mesenteric vein in the setting of chronic pancreatitis. We felt this made our case unique and reportable.
Conclusion
In the setting of ectopic varices form splanchnic vein thrombosis, an attempt to restore anatomical flow would be the most prudent treatment strategy. However, in general ectopic varices are complex and highly variable entities that are not fully understood. All treatment strategies and techniques that have been utilized in managing these potentially lethal varices have shown poor results. Hopefully, in the future, more reporting on this entity leads to a better understanding, description, and categorization of ectopic varices, and there will be a more systematic approach to this rare but menacing problem.
Permission
As part of the standard informed consent for his procedure, the patient agreed that his case may be used to further medical education. It is standard at our academic medical institution to include this on consent forms for all procedures.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
Authors would like to thank the Interventional Radiology Department at the University of Missouri, Columbia for their exceptional care of this patient. We also thank Joanne Cassani our Director of Research for coordinating and putting together the materials needed to publish this case report.
References
- 1.Saad WE, Lippert A, Saad NE, Caldwell S. Ectopic varices: Anatomical classification, hemodynamic classification, and hemodynamic-based management. Tech Vasc Interv Radiol. 2013;16:158–75. doi: 10.1053/j.tvir.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 2.Kochar N, Tripathi D, McAvoy NC, Ireland H, Redhead DN, Hayes PC. Bleeding ectopic varices in cirrhosis: The role of transjugular intrahepatic portosystemic stent shunts. Aliment Pharmacol Ther. 2008;28:294–303. doi: 10.1111/j.1365-2036.2008.03719.x. [DOI] [PubMed] [Google Scholar]
- 3.Khouqeer F, Morrow C, Jordan P. Duodenal varices as a cause of massive upper gastrointestinal bleeding. Surgery. 1987;102:548–52. [PubMed] [Google Scholar]
- 4.Bommana V, Shah P, Kometa M, Narwal R, Sharma P. A case of isolated duodenal varices secondary to chronic pancreatitis with review of literature. Gastroenterology Res. 2010;3:281–6. doi: 10.4021/gr249w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hashizume M, Tanoue K, Ohta M, Ueno K, Sugimachi K, Kashiwagi M, et al. Vascular anatomy of duodenal varices: Angiographic and histopathological assessments. Am J Gastroenterol. 1993;88:1942–5. [PubMed] [Google Scholar]
- 6.Cottam DR, Clark R, Hayn E, Shaftan G. Duodenal varices: A novel treatment and literature review. Am Surg. 2002;68:407–9. [PubMed] [Google Scholar]
- 7.Rajesh S, Mukund A, Arora A. Imaging diagnosis of splanchnic venous thrombosis. Gastroenterol Res Pract. 2015;2015:101029. doi: 10.1155/2015/101029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jonnalagadda SS, Quiason S, Smith OJ. Successful therapy of bleeding duodenal varices by TIPS after failure of sclerotherapy. Am J Gastroenterol. 1998;93:272–4. doi: 10.1111/j.1572-0241.1998.270_3.x. [DOI] [PubMed] [Google Scholar]
- 9.Mukund A, Deogaonkar G, Rajesh S, Shasthry SM, Sarin SK. Safety and efficacy of sodium tetradecyl sulfate and lipiodol foam in balloon-occluded retrograde transvenous obliteration (BRTO) for large porto-systemic shunts. Cardiovasc Intervent Radiol. 2017;40:1010–6. doi: 10.1007/s00270-017-1593-5. [DOI] [PubMed] [Google Scholar]
- 10.Isaksson B, Jeppsson B, Bengtsson F, Hannesson P, Herlin P, Bengmark S. Mesocaval shunt or repeated sclerotherapy: Effects on rebleeding and encephalopathy--a randomized trial. Surgery. 1995;117:498–504. doi: 10.1016/s0039-6060(05)80248-x. [DOI] [PubMed] [Google Scholar]
- 11.Salzedas-Netto AA, Duarte AA, Linhares MM, Mattar RH, Medeiros KL, Cury EK, et al. Variation of the Rex shunt for treating concurrent obstruction of the portal and superior mesenteric veins. J Pediatr Surg. 2011;46:2018–20. doi: 10.1016/j.jpedsurg.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 12.Sabri SS, Caldwell SH, Kumer SC, Schmitt TM, Maluf DG, Angle JF, et al. Combined transmesenteric and transhepatic recanalization of chronic portal and mesenteric vein occlusion to treat bleeding duodenal varices. J Vasc Interv Radiol. 2014;25:1295–9. doi: 10.1016/j.jvir.2013.11.021. [DOI] [PubMed] [Google Scholar]
- 13.Martin EC, Laffey KJ, Bixon R. Recanalization of the superior mesenteric vein for massive bleeding in Crohn disease. J Vasc Interv Radiol. 1995;6:703–5. doi: 10.1016/s1051-0443(95)71168-x. [DOI] [PubMed] [Google Scholar]


