Abstract
Introduction:
The diabetes mellitus type 2 is a result of hyperglycemia due to insulin resistance caused by insufficient secretion of insulin from the beta cells of pancreas. The detection and controlling of diabetes mellitus type 2 (DMT2) at primary health-care centers in Saudi Arabia is well justified and widely practiced. The knowledge and awareness of DMT2 patients should be increased through the determination of its prevalence which may decrease the rates of comorbidities.
Methods:
A questionnaire of 159 patients registered at Home Care Center at Family and Community Medicine Department, Al-Kharj Military Industries Corporation Hospital, Saudi Arabia was used. Hemoglobin A1C (HbA1C) percentage and blood pressure were measured for all participants. Statistical analysis was performed for all data.
Results:
A total of 36.5% of cases were males and 63.5% were females with a mean age of 77.6 years. 94.3% of participants had DMT2 where 3.8% had type 1. 74.2% of cases experienced only one to two complications other than diabetes where 20.8% had more than three diseases. 47.2% of cases had HbA1C% <7.5% where 29 cases had HbA1C% ranged from 7.5% to 8% and about 32.8% of patients had poor glycemic control with HbA1C >8%. 81.1% of cases had hypertension, while 25.8% suffered from Stroke complication, 8.8% of patients had a congestive cardiac failure, 7.5% had ischemic heart disease, and 6.3% suffered from chronic kidney disease. The treatment goals, HbA1C 7.5--8%, have been achieved for about 64% of DMT2 patients where 51 patients still had uncontrolled DMT2 with HbA1C >8%.
Conclusion:
Despite the majority of cases had good glycemic control, more attention should be paid to those over 65 years as they commonly had more morbidities that definitely affect their treatment regimes. Patients should be involved in different home health care programs to increase their awareness and knowledge of the possible risk factors and diabetes comorbidities.
Keywords: Diabetes mellitus, glycemic control, home health care
Introduction
Diabetes mellitus type 2 (DMT2) accounts for 90% to 95% of patients who are, frequently, obese and undiagnosed for many years because of the gradual development of hyperglycemia.[1] The report of International Diabetes Federation, 2013 mentioned that adult diabetic patients of Saudi Arabia (30--80 years old) represent 24% of the population where 23.7% suffered from DMT2.[2] The glycemic control of higher glycated hemoglobin A1C (HbA1C) can reduce the risk factors of DMT2.[3] The new guidelines of the American Diabetic Association (ADA), 2019, have shown the importance of the home health care (HHC) in the lifestyle management for the older adults with DMT2 those may require frequent intervention and home nursing.[4] In the current study we aim to determine the prevalence of diabetes and its complications among home care patients at the Al Kharj Military Industries Corporation Hospital, Saudi Arabia.
Subjects and Methodology
Subjects selection, sample size, and data collection
The project and data forms were approved by the committee of the Institutional Review Board in compliance with the Helsinki Declaration (https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/) with an approval letter for the project no. (1053).
The inclusion criteria for eligible participants included all Saudi adult patients older than 18 years who were registered at HHC center at Al-Kharj Military industries corporation hospital. Detailed information regarding the study procedures was provided to all participants and those agreed to and signed the consent form was included in the study.
The current study was conducted in Home Care Center at Family and Community Medicine Department, Al-Kharj Military Industries Corporation Hospital, Saudi Arabia for 159 patients who are registered at the center and periodically visited by time schedule. The medical records data of blood glucose-lowering drugs in the last 4 weeks were collected for all participants. The criteria for the Diabetes diagnosis of ADA were followed.
Data were collected from Home Care Center at Family and Community Medicine Department which provide complete health care as well as a continuous and comprehensive follow-up through a qualified medical team for treating and controlling the disease. The sample size was calculated with statistical software, Population Proportion Sample size according to the following formula:
Sample size (n) = N*X/(X + N-1)
Where X = Za/22*p*(1-p)/MOE2
Za/2 is the critical value of the normal distribution for a confidence level 95%, P is the migration error, P is the sample proportion, and N is the population size (360 patients).
Direct interview between all subjects and trained interviewers was conducted using a questionnaire to capture information on diabetic-related characteristics, and complications. Information on the diagnosis of diabetic complications including the duration and details of the diagnosis were collected. All subjects were asked to have a free HbA1C test where 5 ml blood samples were collected and sent to the hematology department using the common procedure. The treatment goal for the glycemic control for older patients (>65 years) was an HbA1C target of 7.5–8% overall, as recommended by the American Geriatrics Society (AGS) and ADA.[5]
Data management and statistical analysis
Statistical analyses were performed in IBM SPSS version 22. Continuous variables were summarized with mean and median, and categorical variables as percentages. Bivariate correlation and Chi-square tests were used to explore the relationship between the categorical and ordinal data, respectively. Fully adjusted multiple linear regression models were run to assess associations of HbA1C values with Study variables. A two-tailed test was performed with the significance level at 0.05 and 0.01.
Results
A total of 159 participants were eligible in the study, where 150 (94.3%) were type 2 diabetic patients DMT2, six (3.8%) patients were type 1 diabetes and three cases were nondiabetic. 124 patients (68.5%) had experienced diabetes for more than 10 years. 58 (36.5%) of cases were males and 101 (63.5%) were females with a mean age of 77.6 years (range: 48--95 years). The mean period between the diagnosis of DMT2 and enrolment in the study was 18.8 years (median: 15 years, 1--50 years). The cases were clustered into six age groups as group 1 (<50 years, n = 1, 0.6%), group 2 (51--60 years, n = 11, 6.9%), group 3 (61--70 years, n = 20, 12.6%), group 4 (71--80 years, n = 63, 39.6%), group 5 (81--90 years, n = 54, 34%), and group 6 (>90 years, n = 10, 6.3%). Medical records and data collected from the completed questionnaires of all participants showed that 6.3% (n = 10) are surgical patients where the majority 93.7% (n = 149) were nonsurgical patients. 127 (79.9%) of the cases had an earlier diagnosis of diabetes (more than 3 months postsymptomatic, with more comorbidities) where 29 cases (18.2%) had a recent diagnosis (less than 3 months postsymptomatic, with less or no comorbidities). Home care services were provided to all patients where 5.7% (n = 9) had home care services for 4--7 years, 25.2% (n = 40) had 1--3 years, 16.4% (n = 26) had 6 months to 1 year visits, 35.8% (n = 57) had visits for 2--6 months, 10.1% (n = 16) had home care services for less than 1 month, and 6.9% (n = 11) had one or two visits for less than one week. 144 patients had commitments to the regular taking of medication which was classified as only oral antidiabetic drugs, prescribed for 47.2% (n = 75) of the patients, followed by Insulin only for 30.2% (n = 48), mixed prescription of insulin and oral drugs 16.4% (n = 26), and 10 patients (6.3%) have not any prescribed medications (patients on diet only or nondiabetic individuals). Marital status, education, occupations, family history, activity, mobility, and nutrition information were collected as well, Table 1.
Table 1.
General characteristics and for the study population (n=159)
| Variable | Frequency (%) |
|---|---|
| Gender: | |
| Male | 58 (36.5%) |
| Female | 101 (63.5%) |
| Age (Min-Max) | (48-95) |
| (Mean±SD) | (77.6±9.54) |
| <50 years | 1 (0.6%) |
| 51-60 years | 11 (6.9%) |
| 61-70 years | 20 (12.6%) |
| 71-80 years | 63 (39.6%) |
| 81-90 years | 54 (34%) |
| >90 years | 10 (6.3%) |
| Marital Status: | |
| Single | 2 (1.3%) |
| Married | 104 (65.4%) |
| Divorced | 0 (0.0%) |
| Widow/ed | 53 (33.3%) |
| Education: | |
| Primary | 18 (11.3%) |
| Secondary | 7 (4.4%) |
| Tertiary Illiterate | 3 (1.9%) 131 (82.4%) |
| Occupation: | |
| Employed | 23 (14.5%) |
| Unemployed | 103 (64.8%) |
| Housewife | 33 (20.8%) |
| Smoking: | |
| Smoker Nonsmoker | 13 (8.2%) 146 (91.8%) |
| Family History: | |
| Yes | 85 (53.5%) |
| No | 74 (46.5%) |
| Patient type: | |
| Nonsurgical | 149 (93.7%) |
| Surgical | 10 (6.3%) |
| Type of diabetes: | |
| Nondiabetic | 3 (1.9%) |
| Type 1 | 6 (3.8%) |
| Type 2 | 150 (94.3%) |
| Time of diagnosis: | |
| Early diagnosed | 127 (79.9%) |
| Recently diagnosed | 29 (18.2%) |
| None (nondiabetic) | 3 (1.9%) |
| Duration of diabetes: | |
| (Min.-Max.) | (0-50) |
| (Mean±SD) | (18.8±9.6) |
| <10 years | 50 (31.4%) |
| More than 10 years | 109 (68.6%) |
| Length of HHC: | |
| 1 week or less | 11 (6.9%) |
| 2 weeks to 1 month | 16 (10.1%) |
| 2 months to 6 months | 57 (35.8%) |
| 6 months to 1 year | 26 (16.4%) |
| 1 year to 3 years | 40 (25.2%) |
| 4-7 years | 9 (5.7%) |
| Adherence to medication: | |
| Yes | 144 (90.6%) |
| No | 12 (7.5%) |
| Not applicable (nondiabetic) | 3 (1.9%) |
| Type of drugs: | |
| No drugs | 10 (6.3%) |
| Oral antidiabetic drugs only | 75 (47.2%) |
| Insulin only | 48 (30.2%) |
| Oral and insulin | 26 (16.4%) |
| Activity: | |
| Bedfast | 84 (52.8%) |
| Chairfast | 58 (36.5%) |
| Walks occasionally | 11 (6.9%) |
| Walks frequently | 6 (3.8%) |
| Mobility: | |
| Completely immobile | 30 (18.9%) |
| Very limited | 89 (56%) |
| Slightly limited | 33 (20.8%) |
| No limitation | 7 (4.4%) |
| Nutrition: | |
| Very poor | 6 (3.8%) |
| Probably inadequate | 13 (8.2%) |
| Adequate | 131 (82.4%) |
| Excellent | 5 (3.1%) |
| Obese | 4 (2.5%) |
| Comorbidities: | |
| None | 8 (5%) |
| 1-2 diseases | 118 (74.2%) |
| ≥3 diseases | 33 (20.8%) |
| Obese | 8 (5%) |
| HbA1C% | |
| (Min.-Max.) | (4.6-14) |
| (Mean±SD) | (8.31±1.75) |
| Not measured | 4 (2.5%) |
| <7.5% | 75 (47.2%) |
| 7.5-8% | 29 (18.2%) |
| >8% | 51 (32.1%) |
| Capillary blood glucose level (mg/dl) | |
| (Min.-Max.) | (59-577) |
| (Mean±SD) | (200±88.48) |
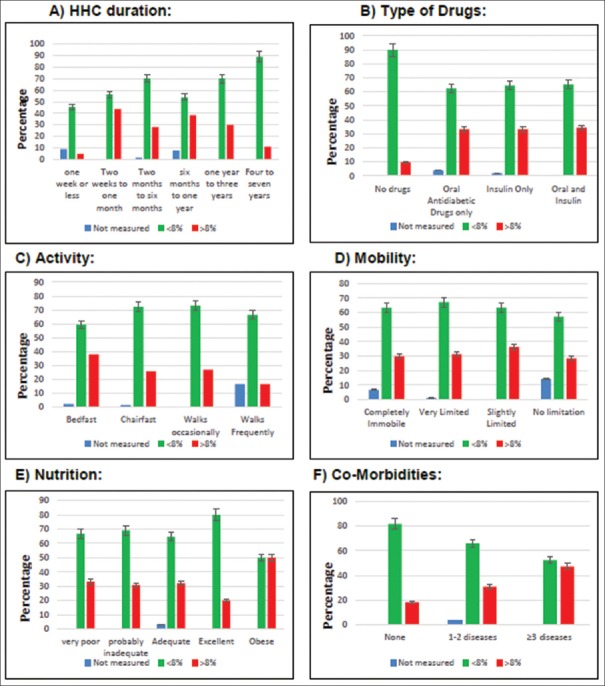
From the overall of the 150 DMT2 patients, 129 (81.1%) had hypertension (HTN) while 41 (25.8%) suffered from old Cerebrovascular attack (CVA) complication, stroke. 14 (8.8%) of patients suffered from congestive cardiac failure (CCF), 12 (7.5%) suffered from ischemic heart disease (IHD), 10 (6.3%) suffered from chronic kidney disease, 7 (4.4%) suffered from benign prostatic hyperplasia (BPH), 5 (3.1%) suffered from dementia (BPSD), 5 (3.1%) suffered from depression, 3 (1.9%) had previous leg amputation due to diabetes (AKA, above-knee amputation), 3 (1.9%) had osteoporosis (OP), and 2 (1.3%) experienced the chronic obstructive pulmonary disease (COPD). Minor single complications were found in some cases, such as elephantiasis, left ventricle failure (LVF), pearly penile papules (PPP), osteoarthritis (OA), subdural hematoma (SDH), hip fracture (HF), bedsores, deep vein thrombosis (DVT), and right hemiplegia (RH). Other unrelated complications included asthma, anemia, epilepsy, breast cancer, and others were found as well, Table 2 and Figure 1. Statistical analysis for the effect of gender type and age category according to the product moment correlation coefficient (PMCC, also known as the Pearson correlation) was conducted for the relation between all the recorded complications and HBA1C% values. The results were significant for stroke, HTN, and BPH for the older patients, while CCF was recorded only in the female category by a direct positive relationship according to Pearson analysis (P < 0.05). Higher HbA1C% was conducted to DMT2 patients, generally and to the female patients, particularly (P < 0.05) as shown in Table 2.
Table 2.
Relation of gender type and age with the type of diabetes, comorbidities, and HbA1C percentages, descriptive statistics, and bivariate correlations
| Variables | Gender | Age | ||||
|---|---|---|---|---|---|---|
| °PMCC | P | PMCC | P | |||
| Type of diabetes | 0.207** | <0.001 | 0.049 | 0.411 | ||
| HbA1C % (ADA standards)# | 0.224** | <0.001 | 0.054 | 0.054 | ||
| Duration of diabetes | 0.057 | 0.336 | 0.126* | 0.033 | ||
| Comorbidities | Frequency | (%) | ||||
| Cerebrovascular attack | 41 | (25.8%) | 0.033 | 0.575 | 0.186** | 0.002 |
| Hypertension | 129 | (81.1%) | -0.094 | 0.114 | 0.146* | 0.014 |
| Congestive cardiac failure | 14 | (8.8%) | 0.311** | <0.001 | -0.068 | 0.249 |
| Benign prostatic Hyperplasia | 7 | (4.4%) | -0.038 | 0.523 | 0.129* | 0.029 |
| Chronic kidney disease | 10 | (6.3%) | 0.085 | 0.15 | -0.014 | 0.813 |
| Dementia | 5 | (3.1%) | 0.013 | 0.821 | -0.002 | 0.98 |
| Ischemic heart disease | 12 | (7.5%) | -0.056 | 0.342 | 0.103 | 0.081 |
| Depression | 5 | (3.1%) | 0.088 | 0.137 | 0.011 | 0.848 |
| Diabetic leg amputation | 3 | (1.9%) | -0.098 | 0.097 | -0.048 | 0.42 |
| Osteoporosis | 3 | (1.9%) | -0.056 | 0.342 | 0.016 | 0.786 |
| Chronic obstructive Pulmonary disease | 2 | (1.3%) | -0.08 | 0.177 | -0.07 | 0.239 |
| Not related complications | 23 | (14.5%) | -0.052 | 0.518 | -0.014 | 0.858 |
*Correlation is significant at the 0.05 level (2-tailed). **Correlation is significant at the 0.01 level (2-tailed). #American diabetic association. °PMCC: The Product Moment Correlation Coefficient also known as “The Pearson correlation”
Figure 1.
Comorbidities recorded among the study population. Bar chart describing the comorbidities accompanied with DMT2, recorded in the study population
Medical records had also shown that 74.2% (n = 118) of cases experienced only one to two complications other than diabetes where 20.8% (n = 33) had more than three diseases. According to the classification guidelines at 2019 of ADA, the glycemic control of the diabetic patients is assessed according to their HbA1C protein percentage (HbA1C%). In the current study, HbA1C% results were available for only 97.5% (n = 155) of cases with mean value of (8.31 ± 1.75) where it had not been measured for four participants due to kidney failure (uremia), Anemia or Acute blood loss. About 47.2% (n = 75) of cases had HbA1C% <7.5% and were considered controlled according to the ADA guidelines where 29 cases (18%) had HbA1C% ranged from 7.5% to 8% and that could reach the goals of the treatment for DMT2 old patients (>65 years) as recommended by ADA guidelines and about 32.8% (n = 51) of patients had poor glycemic control with HbA1C >8% and accordingly complicated health diabetic situation, Table 3.
Table 3.
Characteristics of the study population from the perspective of HHC and glycemic control assessment according to ADA standards
| Variable | Total % of total population | HbA1C% (ADA standards) (Min. 4.6-Max. 14) (Mean 8.31±1.75) | |||
|---|---|---|---|---|---|
| Not-measured | <7.5% | 7.5-8% | >8% | ||
| Age | (Min. 48- Max. 95), Mean (77.6±9.54) | ||||
| <50 years | 1 (0.6%) | 0 (0%) | 0 (0%) | 1 (100%) | 0 (0%) |
| 51-60 years | 11 (6.9%) | 0 (0%) | 6 (54.5%) | 5 (45.5%) | 0 (0%) |
| 61-70 years | 20 (12.6%) | 1 (5%) | 8 (40%) | 4 (20%) | 7 (35%) |
| 71-80 years | 63 (39.6%) | 1 (1.6%) | 32 (50%) | 5 (7.9%) | 25 (39.7%) |
| 81-90 years | 54 (34%) | 1 (1.9%) | 23 (42.6%) | 13 (24.1%) | 17 (31.5%) |
| More than 90 years | 10 (6.3%) | 1 (10%) | 6 (60%) | 1 (10%) | 2 (20%) |
| Patient type: | |||||
| Nonsurgical | 149 (93.7%) | 3 (2%) | 71 (47.7%) | 28 (18.8%) | 47 (31.5%) |
| Surgical | 10 (6.3%) | 1 (10%) | 4 (40%) | 1 (10%) | 4 (40%) |
| Type of diabetes: | |||||
| Nondiabetic | 3 (1.9%) | 0 (0%) | 3 (100%) | 0 (0%) | 0 (0%) |
| Type 1 | 6 (3.8%) | 1 (16.7%) | 3 (50%) | 2 (33.3%) | 0 (0%) |
| Type 2 | 150 (94.3%) | 3 (2%) | 69 (46%) | 27 (18%) | 51 (34%) |
| Time of diagnosis: | |||||
| Early diagnosed | 127 (79.9%) | 4 (3.1%) | 52 (40.9%) | 26 (20.5%) | 45 (35.4%) |
| Recently diagnosed | 29 (18.2%) | 0 (0%) | 20 (69%) | 3 (10.3%) | 6 (20.7%) |
| None (nondiabetic) | 3 (1.9%) | 0 (0%) | 3 (100%) | 0 (0%) | 0 (0%) |
| Duration of diabetes: | (Min. 0- Max. 50), Mean (18.8±9.6) | ||||
| Less than 10 years | 50 (31.4%) | 3 (6%) | 29 (58%) | 8 (16%) | 10 (20%) |
| More than 10 years | 109 (68.6%) | 1 (0.9%) | 46 (42.2%) | 21 (19.3%) | 41 (37.6%) |
| Length of HHC: | |||||
| 1 week or less | 11 (6.9%) | 1 (9.1%) | 3 (27.3%) | 2 (18.2%) | 5 (45.5%) |
| 2 weeks to 1 month | 16 (10.1%) | 0 (0%) | 9 (56.3%) | 0 (0%) | 7 (43.8%) |
| 2 months to 6 months | 57 (35.8%) | 1 (1.8%) | 26 (45.6%) | 14 (24.6%) | 16 (28.1%) |
| 6 months to 1 year | 26 (16.4%) | 2 (7.7%) | 8 (30.8%) | 6 (23.1%) | 10 (38.5%) |
| 1 year to 3 years | 40 (25.2%) | 0 (0%) | 23 (57.5%) | 5 (12.5%) | 12 (30%) |
| 4-7 years | 9 (5.7%) | 0 (0%) | 6 (66.7%) | 2 (22.2%) | 1 (11.1%) |
| Adherence to medication: | |||||
| Yes | 144 (90.6%) | 4 (2.8%) | 66 (45.8%) | 26 (18.1%) | 48 (33.3%) |
| No | 12 (7.5%) | 0 (0%) | 6 (50%) | 3 (25%) | 3 (25%) |
| Not applicable (nondiabetic) | 3 (1.9%) | 0 (0%) | 3 (100%) | 0 (0%) | 0 (0%) |
| Type of drugs: | |||||
| No drugs | 10 (6.3%) | 0 (0%) | 7 (70%) | 2 (20%) | 1 (10%) |
| Oral antidiabetic drugs only | 75 (47.2%) | 3 (4%) | 34 (45.3%) | 13 (17.3%) | 25 (33.3%) |
| Insulin only | 48 (30.2%) | 1 (2.1%) | 22 (45.8%) | 9 (18.8%) | 16 (33.3%) |
| Oral and Insulin | 26 (16.4%) | 0 (0%) | 12 (46.2%) | 5 (19.2%) | 9 (34.6%) |
| Activity: | |||||
| Bedfast | 84 (52.8%) | 2 (2.4%) | 40 (47.6%) | 10 (11.9%) | 32 (38.1%) |
| Chairfast | 58 (36.5%) | 1 (1.7%) | 26 (44.8%) | 16 (27.6%) | 15 (25.9%) |
| Walks occasionally | 11 (6.9%) | 0 (0%) | 5 (45.5%) | 3 (27.3%) | 3 (27.3%) |
| Walks Frequently | 6 (3.8%) | 1 (16.7%) | 4 (66.7%) | 0 (0%) | 1 (16.7%) |
| Mobility: | |||||
| Completely immobile | 30 (18.9%) | 2 (6.7%) | 18 (60%) | 1 (3.3%) | 9 (30%) |
| Very limited | 89 (56%) | 1 (1.1%) | 43 (48.3%) | 17 (19.1%) | 28 (31.5%) |
| Slightly limited | 33 (20.8%) | 0 (0%) | 12 (36.4%) | 9 (27.3%) | 12 (36.4%) |
| No limitation | 7 (4.4%) | 1 (14.3%) | 2 (28.6%) | 2 (28.6%) | 2 (28.6%) |
| Nutrition: | |||||
| Very poor | 6 (3.8%) | 0 (0%) | 4 (66.7%) | 0 (0%) | 2 (33.3%) |
| Probably inadequate | 13 (8.2%) | 0 (0%) | 8 (61.5%) | 1 (7.7%) | 4 (30.8%) |
| Adequate | 131 (82.4%) | 4 (3.1%) | 59 (45%) | 26 (19.8%) | 42 (32.1%) |
| Excellent | 5 (3.1%) | 0 (0%) | 2 (40%) | 2 (40%) | 1 (20%) |
| Obese | 4 (2.5%) | 0 (0%) | 2 (50%) | 0 (0%) | 2 (50%) |
| Comorbidities: | |||||
| None | 8 (5%) | 0 (0%) | 6 (54.5%) | 3 (27.3%) | 2 (18.2%) |
| 1-2 diseases | 118 (74.2%) | 4 (3.10%) | 60 (46.5%) | 25 (19.4%) | 40 (31%) |
| ≥3 diseases | 33 (20.8%) | 0 (0%) | 9 (47.4%) | 1 (5.3%) | 9 (47.4%) |
| Total | 159 | 4 | 75 | 29 | 51 |
| (for each category) | 100% | 2% | 47.2% | 18% | 32.8% |
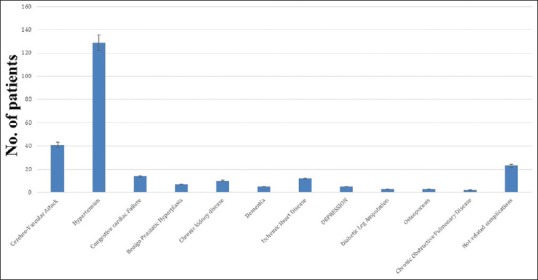
The deep calculation of the HbA1C% in each cluster of variables showed that the majority of patients is at ages of 71--80 (n = 63) years where 50% of them had HbA1C level <7.5%, 7.9% at 7.5--8%, and 39.7% had higher HbA1C5 >8%. For DMT2 patients (n = 150), 46% had HbA1C level <7.5%, 18% at 7.5--8%, and 34% had higher HbA1C5 >8%. Patients with early diabetic diagnosis (n = 127) had HbA1C level <7.5% for 40.9%, HbA1C level 7.5--8% for 20.5%, and HbA1C5 >8% for 35.4% of patients of this category. For patients with duration of diabetes more than 10 years, (n = 109), 42.2% had HbA1C level <7.5%, 19.3% at 7.5--8%, and 37.6% had higher HbA1C5 >8% [Table 3]. The levels of HbA1C showed the robust effect of HHC according to HHC duration, type of drugs, activity, mobility, nutrition, and number of comorbidities, as it was found the majority of patients had HbA1C% less than 8% (controlled) in all categories except for obese patients and those with more than three accompanied morbidities which had less or no noticeable effect [Figure 2].
Figure 2.
Efficacy of HHC according to HbA1C%. The glycemic control was estimated by HbA1C% as if <8% (controlled) and >8% (uncontrolled) for all the study variables
The current study included the results DMT2 leading risk factors, such as smoking, family history, type and duration of diabetes, type of drugs used, activity, mobility, and nutrition records as stated by ADA.[1,6] Statistical analysis was conducted by the fully adjusted linear regression model for the relationship of HbA1C% with risk factors and comorbidities. HbA1C was significantly associated with mobility (β = 0.177, 95% confidence of interval [CI] 0.174--0.666 and P = 0.001), and Blood glucose level (β = 0.439, 95% CI 0.007--0.011 and P < 0.001), while it was inversely associated with activity (β = -0.144, 95% CI -0.595 to -0.097 and P = 0.007) as shown in Table 4. HbA1C was significantly associated with osteoporosis disease (β = 0.120, 95% CI 0.212--2.726 and P = 0.022) while it was inversely associated with BPH disease (β = -0.103, 95% CI -1.787 to -0.005 and P = 0.049), dementia (β = -0.149, 95% CI -2.206 to -0.399 and P = 0.005), and depression (β = -0.211, CI -2.551 to -0.874 and P < 0.001) as shown in Table 5.
Table 4.
Fully adjusted linear regression model for the relation between HbA1C % (ADA standards) and risk factors
| β-coefficient | 95% confidence interval | P | |||
|---|---|---|---|---|---|
| Risk factors: | |||||
| Age | -0.59 | -0.062 | To | 0.041 | 0.68 |
| Smoking | 0.020 | -0.609 | To | 0.883 | 0.718 |
| Family history | -0.001 | -0.351 | To | 0.341 | 0.977 |
| Type of diabetes | 0.076 | -0.591 | To | 1.64 | 0.355 |
| Duration of DM | -0.17 | -1.287 | To | -0.28 | 0.526 |
| Type of drugs | 0.017 | -0.176 | To | 0.248 | 0.739 |
| Activity | -0.144** | -0.595 | To | -0.097 | 0.007 |
| Mobility | 0.177** | 0.174 | To | 0.666 | 0.001 |
| Nutrition | -0.057 | -0.509 | To | 0.173 | 0.333 |
| Others | |||||
| Blood glucose | 0.439** | 0.007 | To | 0.011 | <0.001 |
*Correlation is significant at the 0.05 level (2-tailed). **Correlation is significant at the 0.01 level (2-tailed). ***Correlation is significant at the 0.001 level (2-tailed)
Table 5.
Fully adjusted linear regression model for the relation between HbA1C % (ADA standards) and comorbidities
| β-coefficient | 95% Confidence interval | p | |||
|---|---|---|---|---|---|
| Comorbidities: | |||||
| Cerebrovascular attack | 0.066 | -0.148 | To | 0.683 | 0.206 |
| Hypertension | 0.04 | -0.292 | To | 0.644 | 0.459 |
| Congestive cardiac failure | -0.003 | -0.608 | To | 0.57 | 0.949 |
| Benign prostatic hyperplasia | -0.103* | -1.787 | To | -0.005 | 0.049 |
| Chronic kidney disease | 0.088 | -0.022 | To | 1.495 | 0.057 |
| Dementia | -0.149** | -2.206 | To | -0.399 | 0.005 |
| Ischemic heart disease | -0.056 | -1 | To | 0.251 | 0.239 |
| Depression | -0.211*** | -2.551 | To | -0.874 | 0 |
| Diabetic leg amputation | 0.091 | -0.254 | To | 2.682 | 0.105 |
| Osteoporosis | 0.12* | 0.212 | To | 2.726 | 0.022 |
| Chronic obstructive pulmonary disease | 0.078 | -0.205 | To | 2.517 | 0.096 |
| Not related complications | 0.098 | 0.086 | To | 1.018 | 0.464 |
*Correlation is significant at the 0.05 level (2-tailed). **Correlation is significant at the 0.01 level (2-tailed). ***Correlation is significant at the 0.001 level (2-tailed)
According to the guidelines of ADA and AGS, the treatment goals considerations for goals for those ≥65 years old, suggesting an HbA1C target of 7.5–8% overall, 7–7.5% if few comorbidities and good functional status, and 8–9% if poor health and limited life expectancy.[5] In the current study, it was found that treatment goals have been achieved for about 64% (n = 96) of DMT2 patients (69 patients with HbA1C <7.5% and 27 with HbA1C 7.5--8%) where 51 patients still had uncontrolled DMT2 with HbA1C >8%. The category of patients achieved glycemic control comprises of 69 cases (46%) with HbA1C <7% and 27 cases (18%) with HbA1C 7.5--8%. From the 69 patients with HbA1C <7.5%, only 46 patients (66.7%) reached random blood glucose levels between 100 and 150 mg/dl where 57 patients (82.6%) maintained blood pressure <140/90. From the 27 patients with HbA1C 7.5--8%, only 10 patients (37%) reached blood glucose levels between 110 and 200 mg/dl where 24 patients (88.9%) maintained blood pressure <150/90, according to ADA guidelines[1] as shown in Table 6.
Table 6.
Assessment of the treatment goals for glycaemia and blood pressure in the perspective of HbA1C% for older DMT2 patients (n=150) according to ADA guidelines
| ADA criteria | HbA1C% | Capillary blood glucose level | Blood pressure |
|---|---|---|---|
| Not measured | 3 (2%) | - | - |
| Healthy (HbA1C <7.5%) Blood glucose 100-150 mg/dl Blood pressure <140/90 |
69 (46%) | 46 (66.7%) (of the 69 patients with HbA1C <7.5%) | 57 (82.6%) (of the 69 patients with HbA1C <7.5%) |
| Treatment goals for DMT2 patients >65 years (HbA1C 7.5-8%) Blood glucose 110-200 mg/dl Blood pressure <150/90 |
27 (18%) | 10 (37%) (of the 27 patients with HbA1C 7.5-8%) | 24 (88.9%) (of the 27 patients with HbA1C 7.5-8%) |
| Uncontrolled (HbA1C >8%) | 51 (34%) | - | - |
Discussion
DMT2 is one of the most complicated health problems which attract international concern in the past few decades. Almost 30 billion Saudi riyals is the annual cost of health care for diabetic patients in Saudi Arabia.[7] DMT2 management programs affected DMT2 patients positively and have shown enhanced glycemic control and retardation of the disease progression and its comorbidities of diabetic patients despite poor participation.[8] Diabetic patients with chronic health issues require extensive health care which can be fulfilled by providing the healthcare teams with sufficient, comprehensive, reliable, compatible, and correlating patients’ information across the different health sectors.[9] So, the current study was conducted to investigate if the Homecare controlled DMT2 patients, at Al Kharj Military Industries Corporation Hospital, Saudi Arabia, have fewer rates of complications compared to home care uncontrolled DMT2.
Patient age and duration of diabetes are mainly the major predictors of morbidity and mortality rates. Adult diabetic patients of Saudi Arabia (30--80 years old) represent 24% of the population and 25% suffered from DMT2.[10] In the current study, 159 patients registered at Home Care Center have shown a privilege of DMT2 by 94.9% of the study population in which 74.2% of cases experienced only one to two complications other than diabetes where 20.8% had more than three diseases. The prevalence of these comorbidities showed that hypertension (81.1%), cerebrovascular attack (25.8%), congestive cardiac failure (8.8%), ischemic heart disease (7.5%), chronic kidney disease (6.3%), dementia (3.1%), depression (3.1%), osteoporosis (1.9%), and diabetic leg amputation (1.9%) were the major related comorbidities, whereas the bivariate correlation has shown that age is significantly proportioned to duration of diabetes as well as, the older diabetic patients tends to grow a severe comorbidities, such as stroke, hypertension, and benign prostatic hyperplasia which, statistically and significantly, accompanied with the older ages at P < 0.05. In agreement with these findings, a previous study showed that among older adults with long diabetes duration where cardiovascular complications had the highest incidence rates followed by chronic kidney diseases, amputation, and acute hyperglycemic events.[11] In another retrospective study from Cameron, 628 DMT2 older-aged patients had acute metabolic complications (22.2%), cardiovascular diseases (16.7%), cancers (14.8%), nephropathy (14.8%), and diabetic foot syndrome (13.0%) which increases the mortality rates by 2.5% compared to nondiabetic or type 1 patients.[12]
The bivariate correlations in our study showed that DMT2 were the most common in the females participating this study which, significantly, codiseased with congestive cardiac failure (PMCC = 0.311) at P < 0.001 where the other comorbidities were not significant to either age or gender. In agreement with our findings, a study included 103 DMT2 patients from the German National Health Interview and Examination Survey 1998 (GNHIES98) showed that age and gender mortality rates are twice as high for adults with DMT2 and higher for women at older ages.[13] In a previous cross-sectional study in Australia at 2010, the findings showed that the standardized mortality ratios for DMT2 patients with cardiovascular disease were 29.2% in males compared to 31.6% in females (P < 0.001) which occasionally agree with our results, as well.[14] Another multicenter retrospective study for 932 chronic DMT2 patients in Spain revealed that ischemic cardiopathy, the peripheral vascular disease did not increase the mortality ratios compared to heart failure and cognitive impairment ratios were higher and seemed to wane with advancing age.[15] Another meta-analysis study from Saudi Arabia where findings indicated that the incidence and prevalence rate of DMT2 is rising particularly among females and in urban areas of the Eastern Province, Jeddah, and Riyadh than those in rural areas which highlights the importance of Saudi healthcare system skills of all healthcare professionals involved with diabetes management.[16]
The current study discusses the impact of continuous glycose monitoring for the primary care practices and setting by enhancing of the overall glycemic control. Older age, medication adherence, and the adequate knowledge of DMT2 causes and risk factors, achieved by HCC, may improve the glycemic control and prevent the correlated comorbidities.[17,18] HHC service is an important regimen in the screening and controlling of diabetes and corresponding complications in older adults which might assist the framing of the therapeutic approaches and glycemic control targets.[19] The mortality rates are usually higher in the cases of diabetic old patients because of increased risk for depression which may require periodical and careful screening and treatment in order assess the medical, psychological, functional, and social behavior.[20] HbA1c, or the glycosylated glycated hemoglobin is a reflection of the blood glucose levels over the past 6 to 8 weeks, whereas higher HbA1c levels might indicate the poor glycemic control which usually accompanied with type 1 or type 2 diabetes.[21,22,23] In the current study, HbA1C% were measured at the time of HHC visit with mean value of 8.31 ± 1.75, we found that for the patients over 60 years, 69 (44%) could reach the treatment goal of HbA1C <7.5% in addition to 23 (15%) could reach the goal of 7.5--8% and only 51 (32%) of the cases did not reach the glycemic target with HbA1C >8%. HbA1C values were statistically tested against the diabetes duration and time of diagnosis to result in overall 101 (64%) of study population reached the glycemic goals versus 51 (32%) of HbA1C >8%. The levels of HbA1C showed the robust effect of HHC according to HHC duration, type of drugs, activity, mobility, nutrition, and number of comorbidities, as it was found the majority of patients had HbA1C% less than 8% (controlled) in all categories except for obese patients and those with more than three accompanied morbidities. In a previous cross-sectional study design included 1111 DMT2 patients attending diabetes centers in Riyadh, Hofuf, and Jeddah cities, Saudi Arabia, it was found that 55% of patients had poor glycemic control of HbA1C >8%, whereas 19% were >60 years with longer diabetic durations.[24] Another comprehensive study in Al-Wazarat Health Care (WHC) Family Medicine Center in Riyadh, Saudi Arabia, 263 patients with poorly controlled DMT2 were involved in a multidisciplinary care program for 10 months, and there was a statistically significant reduction in the levels of HbA1c which decreased in the number of patients with an HbA1c ≥10 from 167 patients at enrollment to 11 patients.[25]
Depression, lifestyle, obesity, smoking, alcohol, and some types of medications can affect the blood glucose which may limit and interrupt the use of health data in health research.[19] Our findings showed that HbA1C% levels were significantly higher for less active patients, (β = - 0.144, 95% CI - 0.595 to - 0.097, and P = 0.007); however, the majority of them could reach the glycemic goals (HbA1C <8%). In agreement with our findings, a previous study included 329 women enrolled in the Women's Health and Aging Studies II, Maryland and showed that HbA1c at levels ≥8 was significantly associated with incidence of walking difficulty and low physical performance; and three-times increased risk of incident frailty and three-to-five times increased risk of lower extremity mobility limitations.[26] Despite of the previous findings, we found that HCC could improve the glycemic targets where almost 60% of the bedfast patients and 70% of the patients using chair wheels reached HbA1C levels less than 8%. In agreement with our results, a previous study from France included 236 nursing home residents with DMT2 where most of them had higher levels of comorbidities, impaired cognitive performance, and reduced mobility, and the results showed that the glycemic control was observed in 59.3% of cases.[27] Another study from Bisha, Saudi Arabia, 465 DMT2 patients was enrolled in 30 min diabetic education program for 1 year and there was a significant improvement in glycemic control from HbA1c 10.41 ± 1.89% to 8.22 ± 1.68% (P < 0.05).[28] In another cross-sectional study of 490 DMT2 patients enrolled in the public health-care institution in Riyadh, HbA1C levels were significantly lower in patients who had a periodical follow-up with a dietitian (P < 0.0001).[29]
DMT2 in older adults is significantly related to the cognitive decline and progression to dementia,[30] anxiety and depression,[31] and BPH.[32] Linear regression analysis for the relationship of HbA1C%, in evaluation of the HHC achievement of glycemic control of DMT2 patients, with comorbidities in the mean study showed that HbA1C was significantly lower with BPH disease (β = - 0.103, 95% CI - 1.787 to - 0.005, and P = 0.049), dementia (β = - 0.149, 95% CI -2.206 to - 0.399, and P = 0.005), and depression (β = - 0.211, CI - 2.551 to - 0.874, and P < 0.001). Multiple studies showed that decrease in HbA1C level is usually associated with a decreased risk of diabetic complications, whether microvascular or macrovascular despite it will not reduce the risk of stroke, arthritis or amputation of the lower limbs, heart failure and total mortality.[33] In contrary to our results, a cross-sectional study from Lebanon showed no significant relationship between depression and glycemic control despite a significant association between was found between retinopathy, nephropathy, and stroke with it.[34] Across sectional study from Pakistan included consisted of 490 elderly (>65 years) DMT2 patients and showed significant predictors of impaired glycemic control (HbA1c) for those with poor diabetes self-care, whereas most of them had severe depression and dementia and failed to reach the targeted HbA1c levels.[35] Another study from Saudi Arabia showed that DMT2 patients with HbA1c ≥7% had higher mean score of anxiety (10.3 ± 1.7) and a higher mean score of depression (9.8 ± 1.3) and that good diabetes self-care management may improve the glycemic control.[36]
The current study reported the prevalence of diabetes mellitus type 2 among the elderly patients registered in the Home Health Care center of Al-Kharj Military Industries Corporation Hospital. Despite the majority of cases had good glycemic control, more attention should be paid to those over 65 years as they commonly had more morbidities which definitely affect their treatment regimes. DMT2 patients should be involved in different home health care programs involving a multidisciplinary team approach, frequent clinic visits, and appropriate medication regimens to, markedly, improve their glycemic control, and decreases the cardiovascular risk factors in addition increasing their awareness and knowledge of the possible risk factors and diabetes comorbidities.
Implementation of a patient-specific integrated care program intensified insulin treatment was associated with marked improvement in glycemic control and cardiovascular risk factors of poorly controlled T2DM patients in a safe and reproducible manner.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We would like to thank Dr. El-Sadig Ahmed Ali, S.H.O. Department of Family Medicine, Al-Kharj Military Industries Corporation Hospital, Al-Kharj, Saudi Arabia for his kind assistance. A very special thanks to the nursing team of the Home Care Center at Al-Kharj Military Industries Corporation Hospital, Al-Kharj, Saudi Arabia for great assistance appreciated in data collection and questionnaire of the study population.
References
- 1.American Diabetes Association. Older Adults. Diabetes Care. 2019;42:S139–47. doi: 10.2337/dc19-S012. [DOI] [PubMed] [Google Scholar]
- 2.Guariguata L, Nolan T, Beagley J, Linnenkamp U, Jacqmainet O, editors. IDF Diabetes Atlas. 6th edition. Brussels, Belgium: International Diabetes Federation; 2013. International Diabetes Federation Team. Regional overviews; pp. 51–69. Available from: https://www.idf.org . [Google Scholar]
- 3.Ivers NM, Jiang M, Alloo J, Singer A, Ngui D, Casey CG, et al. Diabetes Canada 2018 clinical practice guidelines: Key messages for family physicians caring for patients living with type 2 diabetes. Can Fam Physician. 2019;65:14–24. [PMC free article] [PubMed] [Google Scholar]
- 4.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2019;42:S31–28. [Google Scholar]
- 5.Quartuccio M, Buta B, Kalyani RR. Comparative effectiveness for glycemic control in older adults with diabetes. Curr Geriatr Rep. 2017;6:175–86. doi: 10.1007/s13670-017-0215-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Begic E, Arnautovic A, Masic I. Assessment of risk factors for diabetes mellitus type 2. Mater Sociomed. 2016;28:187–90. doi: 10.5455/msm.2016.28.187-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alkadi SH. The healthcare system in Saudi Arabia and its challenges: The case of diabetes care pathway. J Health Inform Dev Ctries. 2016;10:1–29. [Google Scholar]
- 8.Williams JS, Walker RJ, Smalls BL, Hill R, Egede LE. Patient-centered care, glycemic control, diabetes self-care, and quality of life in adults with type 2 diabetes. Diabetes Technol Ther. 2016;18:644–9. doi: 10.1089/dia.2016.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alkraiji AI, El-Hassan O, Amin FA. Health informatics opportunities and challenges: Preliminary study in the cooperation council for the Arab States of the Gulf. J Health Inform Dev Ctries. 2014;8:36–45. [Google Scholar]
- 10.Huang ES, Laiteerapong N, Liu JY, John PM, Moffet HH, Karter AJ. Rates of complications and mortality in older patients with diabetes mellitus: The diabetes and aging study. JAMA Intern Med. 2014;174:251–8. doi: 10.1001/jamainternmed.2013.12956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naeem Z. Burden of diabetes mellitus in Saudi Arabia. Int J Health Sci. 2015;9:V–VI. doi: 10.12816/0024690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Foryoung JB, Ditah C, Nde Fon P, Mboue-Djieka Y, Nebongo DN, Mbango ND, et al. Long-term mortality in outpatients with type 2 diabetes in a reference hospital in Cameroon: A retrospective cohort study. BMJ Open. 2018;8:e019086. doi: 10.1136/bmjopen-2017-019086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Röckl S, Brinks R, Baumert J, Paprott R, Du Y, Heidemann C, et al. All-cause mortality in adults with and without type 2 diabetes: Findings from the national health monitoring in Germany. BMJ Open Diab Res Care. 2017;5:e000451. doi: 10.1136/bmjdrc-2017-000451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harding JL, Shaw JE, Peeters A, Guiver T, Davidson S, Magliano DJ. Mortality trends among people with type 1 and type 2 diabetes in Australia: 1997–2010. Diabetes Care. 2014;37:2579–86. doi: 10.2337/dc14-0096. [DOI] [PubMed] [Google Scholar]
- 15.Clua-Espuny JL, González-Henares MA, Queralt-Tomas MLL, Campo-Tamayo W, Muria-Subirats E, Panisello-Tafalla A, et al. Mortality and cardiovascular complications in older complex chronic patients with type 2 diabetes. BioMed Res Int. 2017;2017:1–6. doi: 10.1155/2017/6078498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alotaibi A, Perry L, Gholizadeh L, Al-Ganmi A. Incidence and prevalence rates of diabetes mellitus in Saudi Arabia: An overview. J Epidemiol Glob Health. 2017;7:211–8. doi: 10.1016/j.jegh.2017.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Young-Hyman D, de Groot M, Hill-Briggs F, Gonzalez JS, Hood K, Peyrot M. Psychosocial care for people with diabetes: A position statement of the American Diabetes Association. Diabetes Care. 2016;39:2126–40. doi: 10.2337/dc16-2053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shrivastav M, Gibson W, Shrivastav R, Elzea K, Khambatta C, Sonawane R, et al. Type 2 diabetes management in primary care: The role of retrospective, professional continuous glucose monitoring. Diabetes Spectrum. 2018;31:279–87. doi: 10.2337/ds17-0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Radwan M, Elsous A, Al-Sharif H, Abu Mustafa A. Glycemic control among primary care patients with type 2 diabetes mellitus in the Gaza Strip, Palestine. Ther Adv Endocrinol Metab. 2018;9:3–14. doi: 10.1177/2042018817742070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kimbro LB, Mangione CM, Steers WN, Duru OK, McEwen L, Karter A, et al. Depression and all-cause mortality in persons with diabetes mellitus: Are older adults at higher risk? Results from the Translating Research into Action for Diabetes Study. J Am Geriatr Soc. 2014;62:1017–22. doi: 10.1111/jgs.12833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Owora AH. Commentary: Diagnostic validity and clinical utility of HbA1c tests for type 2 diabetes mellitus. Curr Diabetes Rev. 2018;14:196–9. doi: 10.2174/1573399812666161129154559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moreno G, Mangione CM, Kimbro L, Vaisberg E American Geriatrics Society Expert Panel on Care of Older Adults with Diabetes Mellitus. Guidelines abstracted from the American Geriatrics Society Guidelines for improving the care of older adults with diabetes mellitus: 2013 update. J Am Geriatr Soc. 2013;61:2020–6. doi: 10.1111/jgs.12514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee EA, Gibbs NE, Martin J, Ziel F, Polzin JK, Palmer-Toy D. Improving care in older patients with diabetes: A focus on glycemic control. Perm J. 2016;20:15–080. doi: 10.7812/TPP/15-080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alramadan MJ, Magliano DJ, Almigbal TH, Batais MA, Afroz A, Alramadhan HJ, et al. Glycaemic control for people with type 2 diabetes in Saudi Arabia-An urgent need for a review of management plan. BMC Endocr Disord. 2018;18:62. doi: 10.1186/s12902-018-0292-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tourkmani AM, Abdelhay O, Alkhashan HI, Alaboud AF, Bakhit A, Elsaid T, et al. Impact of an integrated care program on glycemic control and cardiovascular risk factors in patients with type 2 diabetes in Saudi Arabia: An interventional parallel-group controlled study. BMC Fam Pract. 2018;19:1. doi: 10.1186/s12875-017-0677-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schernthaner G, Schernthaner-Reiter MH. Diabetes in the older patient: Heterogeneity requires individualisation of therapeutic strategies. Diabetologia. 2018;61:1503–16. doi: 10.1007/s00125-018-4547-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Retornaz F, Grino M, Mari L, Oliver C. Assessment of glycemic control in nursing home residents with diabetes. J Nutr Health Aging. 2017;21:457–63. doi: 10.1007/s12603-016-0776-0. [DOI] [PubMed] [Google Scholar]
- 28.AL-Shahrani AM. Impact of health education program on diabetic control among diabetic patient managed at diabetic and endocrine center in Bisha, Saudi Arabia. Biomed Res. 2018;29:2391–4. [Google Scholar]
- 29.Alshareef SM, Alkhathlan MA, Alwabel AA, Al-Bawardi AA, Alqarni AH, Almuryidi AS, et al. How does the utilization of diabetes dietitian and educator service in Saudi Arabia affect glycemic outcomes? J Fam Community Med. 2018;25:108–13. doi: 10.4103/jfcm.JFCM_126_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cholerton B, Baker LD, Montine TJ, Craft S. Type 2 diabetes, cognition, and dementia in older adults: Toward a precision health approach. Diabetes Spectr. 2016;29:210–9. doi: 10.2337/ds16-0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Naicker K, Johnson JA, Skogen JC, Manuel D, Øverland S, Sivertsen B, et al. Type 2 diabetes and comorbid symptoms of depression and anxiety: Longitudinal associations with mortality risk. Diabetes Care. 2017;40:352–8. doi: 10.2337/dc16-2018. [DOI] [PubMed] [Google Scholar]
- 32.Elabbady A, Hashad MM, Kotb AF, Ghanem AE. Studying the effect of type 2 diabetes mellitus on prostate-related parameters: A prospective single institutional study. Prostate Int. 2016;4:156–9. doi: 10.1016/j.prnil.2016.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Boussageon R, Pouchain D, Renard V. Prevention of complications in type 2 diabetes: Is drug glucose control evidence based? Br J Gen Pract. 2017;67:85–7. doi: 10.3399/bjgp17X689317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ahmadieh H, Itani H, Itani S, Sidani K, Kassem M, Farhat K, et al. Diabetes and depression in Lebanon and association with glycemic control: A cross-sectional study. Diabetes Metab Syndr Obes. 2018;11:717–28. doi: 10.2147/DMSO.S179153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chaturvedi SK, Manche Gowda S, Ahmed HU, Alosaimi FD, Andreone N, Bobrov A, et al. More anxious than depressed: Prevalence and correlates in a 15-nation study of anxiety disorders in people with type 2 diabetes mellitus. Gen Psychiatry. 2019;32:e100076. doi: 10.1136/gpsych-2019-100076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gemeay EM, Moawed SA, Mansour EA, Ebrahiem NE, Moussa IM, Nadrah WO. The association between diabetes and depression. Saudi Med J. 2015;36:1210–5. doi: 10.15537/smj.2015.10.11944. [DOI] [PMC free article] [PubMed] [Google Scholar]