Abstract
Objective:
Mottling and pitting of enamel due to excess fluoride consumption may affect one's self-esteem due to unaesthetic appearance and also in turn can affect the quality of life. This present study was conducted to assess various treatment approaches available for patients with dental fluorosis.
Materials and Methods:
Literatures were searched from August 1998 to August 2019 for articles in the management of dental fluorosis. The databases used were National Center for Biotechnology Information (NCBI) and Google Scholar. In NCBI, the filters were modified to randomized controlled trial, clinical trial, human trial, and free full-text articles. The following queries were used in order to search for the article: treatment for dental fluorosis, intervention of dental fluorosis, and management of dental fluorosis.
Results:
All the five studies selected after screening were randomized controlled trials. Total number of patients included in this study were 304 with the mean age of 17.7 years old. They were treated with microabrasion, bleaching, resin infiltration or combination of microabrasion with bleaching, and resin infiltration with bleaching. Microabrasion resulted in less esthetic improvement compared with bleaching. Meanwhile, resin infiltration showed a greater improvement in esthetics in comparison to bleaching. Resin infiltration with additional infiltration time and combination of resin infiltration with bleaching are the best treatment options.
Conclusion:
Based on this systematic review, resin infiltration with increased infiltration time is the best treatment approach in treating dental fluorosis.
Keywords: Bleaching, ceramic veneers, dental fluorosis, microabrasion, resin infiltration
Introduction
Rationale
Fluorosis is an endemic disease characterized by excess deposition of fluorides in hard and soft tissues of the body. Dental fluorosis mostly affects families residing in high-fluoride belt areas with excessive amount of fluoride present in drinking water. Dental fluorosis is a health condition or can be described as a developmental disturbances of enamel due to the excessive exposure to fluoride usually seen among pediatric patients.[1] During tooth development, high concentration of fluoride will affect the enamel forming cell, ameloblast, especially during enamel formation.[2] There are subsequent changes happened in the enamel due to the interactions of developing enamel mineral matrix and ameloblast.[3,4] Due to increased fluoride during the mineralization of enamel, there is decrease of free calcium ion concentration in mineralizing matrix, which inhibits enzyme proteinases from degrading the matrix proteins during maturation phase.[3,5] Therefore, degradation of matrix proteins is delayed.[3] Besides, the presence of fluoride-induced retention of enamel matrix protein leads to impaired crystal growth such as amelogenins, ameloblastins, tuftelins, enamelins, and high molecular weight sulfated proteins.[3,6]
Fluoride is essential component in the primary prevention of caries. It increases the resistance of the tooth toward acid attack. Maintaining fluoride exposure at recommended levels is important in the primary prevention of fluorosis and at the same time to enjoy its beneficial effects in caries prevention.
The recommended daily intake of fluoride for primary prevention of fluorosis is 0.05 to 0.07 mg F/Kg/day.[7] However, there are consequences among children if fluoride concentration is more than 1.5 to 4 mg/L, which is higher than WHO recommendation known as dental fluorosis.[8] Skeletal fluorosis can occur if the fluoride concentration is in the range of 4 to 10 mg/L.[8] Parents and pediatrician should play an important role to achieve a maximum protection against dental caries and minimizing the risk of dental fluorosis among children. The most common sources of ingested fluoride are fluoridated drinking water, toothpaste, supplements, and formula for children.[7] The children at the age of 1 to 4 years old is at high risk. The risk of fluorosis subsequently decreases at around 8 years of age and it is highly prevalent among children below this age who is exposed to high floride.[9,10]
Dental fluorosis is characterized by the presence of mottled enamel, brownish discoloration of teeth, pitted enamel, and bilateral, diffuse, thin, horizontal white striations with stained plaque.[1] Apart from enamel, there is also a possibility of fluorosed dentin of permanent teeth, which is characterized histopathologically by increased interglobular dentin formation and accentuation of incremental lines of von Ebner.[11] Clinically, dental fluorosis is severe in premolars and second permanent molars and least in permanent mandibular incisors and first permanent molars.[12] Besides, the severity of dental fluorosis depends on the thickness of enamel. As such, the thicker the enamel, the more severe the dental fluorosis, which is characterized by the snow-capped appearance of cusp tips and incisal edges.[12] This condition lowers the patients’ self-esteem and erases the youngsters’ smile on their face. Dental fluorosis is endemic in certain countries that has high concentration of fluoride, such as India, Sri Lanka, China, Eastern Africa, Middle East, and South America.[1,13,14,15] In 1931, it was found that there was a correlation between fluoride from drinking water and dental fluorosis.[15] In 1937, dental fluorosis case was found in Nellore of Andhra Pradesh.[16] Dean's Index was introduced by Dean in year 1934, which is the classification of fluorosis based on his interpretation of clinical appearance and is still widely used.[17]
Dean's Index:[17]
Questionable: occasional white flecking and spotting of enamel.
Mild: white opaque areas involving more of tooth surface.
Moderate and severe: pitting and brownish staining of tooth surface.
Corroded appearance of tooth.
According to Dean and McKay, the optimum level of water fluoride is less than 0.9 to 1.0 PPM.[18] Dental fluorosis can be either mild or severe based on several factors such as the duration and amount of exposure to fluoride, individual responses, weight, age, degree of physical activity, nutritional factors, and bone growth.[19] Mild form of fluorosis can appear as tiny white striations, which is unnoticeable. In moderate to severe form of fluorosis, it can appear as mottled enamel with brownish discoloration along with pit and wear on the enamel surface due to poor mineralization of enamel.[20]
Previously, it was suggested that soft tissue changes due to excessive fluoride intake in children may be reversible by withdrawal of fluoride intake, dietary supplementation with calcium, vitamin D3, ascorbic acid, and antioxidant; however, there is no evidence of reversible changes in dental hard tissue.[10] Damage to the soft tissues due to high doses of fluoride may occur when it passes through the blood-brain, blood-testis, and blood-placenta barrier.[21]
Thus, various treatment approaches have been recommended for dental fluorosis patient depending on the severity of the disease. Treatment options include micro/macro abrasion, bleaching, composite restorations, veneers, and full crowns.[22] Other conservative techniques for the treatment of dental fluorosis would be composite or ceramic veneers or crown, resin infiltration, and tooth jewelry technique. In a case study done by Budhwar et al.,[23] zirconia crown was given to the patient with moderate fluorosis as it offers a good esthetic result with minimum tooth preparation. Besides, it has intense strength and durability and long lasting. Currently, quantitative light-induced fluorescence has been introduced which able to quantify the enamel loss and helps in the diagnosis of dental fluorosis.
Objectives
Various treatment approaches have been introduced and practiced among the dental practitioner to treat mottling, pitting, and opacity of enamel. However, their effectiveness have not been compared to enable any clinical recommendations to treat dental fluorosis. Thus, the aim of this present systematic review was to assess various treatment approaches in dental fluorosis based on existing evidence from randomized clinical trials followed by most effective treatment recommendation according to the severity of dental fluorosis and also outlines on the recommended levels of fluoride exposure in primary prevention of fluorosis.
Materials and Methods
Protocol
This systematic review was conducted and reported according to PRISMA statement.
Eligibility criteria
The design of this systematic review was conducted by referring from Participants-Intervention-Comparison-Outcomes-Study design schema (PICOS). Randomized controlled trial was included which has criteria such as in vivo study, human trials with any kind of treatment on dental fluorosis. Other criterion includes full-text article in English language. The exclusion criteria of the systematic review were animal studies, case report, unpublished articles, non-randomized trials, incomplete trials, and trials without free full-text access.
Information source and literature research
Literature research was carried out to search for articles related to dental fluorosis. The screening was focused on the treatment approach and management of dental fluorosis. The literature was searched from August 1998 to August 2019 for randomized clinical trial and case history. The databases used were National Center for Biotechnology Information (NCBI) and Google Scholar. In NCBI, the filters were modified to randomized controlled trial, clinical trial, human trial, and free full text. The following queries were used in order to search for the article: treatment for dental fluorosis, intervention of dental fluorosis, and management of dental fluorosis.
Study selection
The study selection was proceed after a pilot study to evaluate the feasibility of the current study. The screening of the identified study including the title, abstract, and full-text studies was done. It was followed by checking the eligibility of the study whether to include or exclude in the systematic review.
Data collection and data items
The information gathered from the selected article were extracted and reviewed. All the information include author name, publication year, treatment approach, inclusion criteria, exclusion criteria, and number of participants were thoroughly reviewed. Based on PICOS, the data were sought.
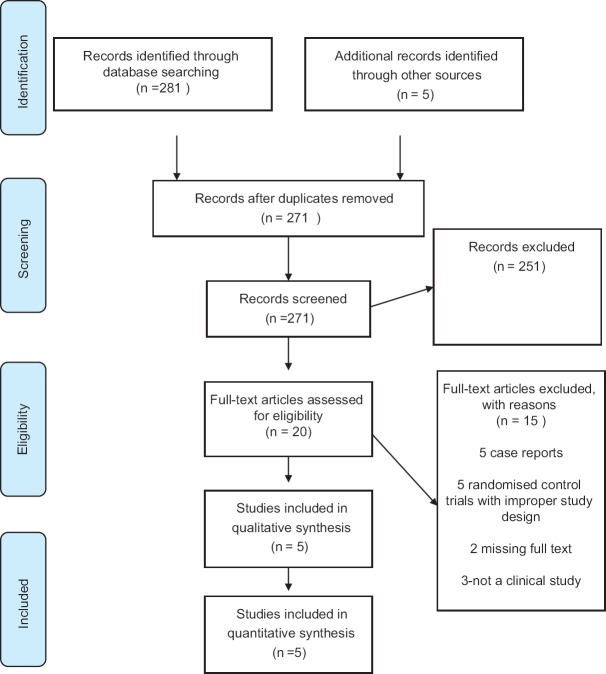
A total of 286 papers were identified through the electronic and five through manual searches, respectively, as shown in Figure 1. After removal of duplicated and initial screening, 20 papers were assessed for eligibility from which 15 papers were not eligible. Only five papers could be included in the study.
Figure 1.
Flow chart of identification and selection of eligible trials
Study characteristics
All the five studies were randomized controlled trials. Total number of patients included in this study were 304 with the mean age of 17.7 years old. The inclusion criteria described in each paper were mostly patient with esthetics as the chief complaint, with good oral hygiene, maxillary anterior teeth which is vital, not fractured or without loss of tooth structure. The patients with history of allergy, systemic or local condition, any previous orthodontic treatment, and pregnant patients were excluded. Fluorosis severity was assessed using Dean's Fluorosis index, Thylstrup-Fejerskov index, and one trial was not recorded. Based on the fluorosis index, most of the patient included in their study were from questionable to moderate fluorosis. The intervention used in the study included microabrasion, external bleaching, microabrasion with at-home bleaching, resin infiltration, resin infiltration with increased infiltration time, or combination of bleaching and infiltration.
Results of individual studies and data synthesis
The interventions and outcome of the five selected randomized clinical trial were described in Table 1. Bleaching was preferably used in four out of five trials, which are selected as the reference interventions.[24] In the study done by Castro et al.,[25] patients were evaluated after one month after the treatment. The statistical analysis between the baseline and after follow-up was done using Mann–Whitney U and t-test to determine the significant differences in staining area, esthetic perception, and tooth and gingival sensitivity (P < 0.05). The result shows that there was significant reduction in enamel opacity area (P = 0.00001) in group 1 and group 2 after follow-up. Regarding the visual analogue scale (VAS), it revealed that group 2 patients were satisfied and happy with their dental appearance after the treatment compared with group 1 (P = 0.004). Based on the tooth and gingival sensitivity after the follow-up, it was reported that both group 1 and group 2 experienced no or mild sensitivity and gingival irritation (P > 0.05).
Table 1.
Study design, interventions, and outcome of clinical trials
| Author | Study design | Total patient; age | Patient info | Fluorosis index | Intervention | Outcome |
|---|---|---|---|---|---|---|
| Loguercio 2007[28] | Randomized Controlled Trial | 36; 10-12 years | Moderate-Good Oral hygiene | DFI; questionable, very mild, mild | Group 1: enamel microabrasion PREMA | Esthetic improvement in VAS |
| Group 2: enamel microabrasionOpalustre | Participant satisfaction Tooth surface | |||||
| Bharath 2014[33] | Randomized Controlled Trial | 30; 9-14 years | Objectionable esthetics | DFI; mild. moderate | Group 1: McInnes bleaching (36% HCl, 30% H2O2, Diethyl ether) | Esthetic improvement in VAS |
| Group 2: enamel microabrasion (18% HCl, pumice powder) | Tooth sensitivity | |||||
| Castro 2014[25] | Randomized Controlled Trial | 70; 15-39 years | Good oral hygiene, vital anterior teeth without loss or fracture, previously no orthodontic treatment. | TFI; mild, moderate | Group 1: enamel microabrasion (37% phosphoric acid, pumice) Group 2: enamel microabrasion (37% phosphoric acid, pumice), at-home bleaching (10% carbamide peroxide) | Reduction in opacity Esthetic improvement in VAS Participant satisfaction in VAS Tooth sensitivity/gingival irritation in VAS |
| Gugnani 2017[27] | Randomized Controlled Trial | 80; 6-12 years old | School children, no history of allergy to dental materials, systemic or local conditions and treatment of dental fluorosis. | TFI; mild, moderate | Group 1: in-office bleaching (35% H2O2 | Esthetic changes in VAS |
| Group 2: resin infiltration (15% HClgel, ethanol drying agent, resin infiltration) | Improvement in opacity or stain in VAS | |||||
| Group 3: resin infiltration with double application of infiltrant | ||||||
| Group 4: in-office bleaching (35% H2O2) resin infiltration | ||||||
| SôniaSaeger 2018[26] | Randomized Controlled Trial | 70; 15-39 years | Good oral hygiene, vital anterior teeth without loss or fracture, previously no orthodontic treatment, non-pregnant | TFI; mild, moderate | Group 1: enamel microabrasion (37% phosphoric acid), fine-grained pumice Group 2: microabrasion and at-home tooth bleaching (10% carbamide peroxide) | Reduction in stained area Tooth sensitivity/gingival irritation in OIDP Esthetic improvement in OIDP |
Similarly, in the study done by SôniaSaeger et al.,[26] the patients were followed for one month and the statistical analysis was done to determine the reduction in stained areas, improvement in esthetics using oral impacts on daily performance (OIDP), tooth sensitivity, and gingival irritation. In this study, the participants who had completed the questionnaires at the baseline and follow-up were included. Based on the OIDP performances of both group, there was significant difference between the baseline and follow-up related to daily performances such as eating and enjoying food (P < 0.01), speaking and pronouncing, cleaning teeth (P < 0.01), smiling, laughing and showing teeth without embarrassment, and maintaining usual emotional state without being irritable (P = 0.032). However, the study also reported slight increase in between the baseline and follow-up in difficulty in sleeping and relaxing. Meanwhile, there was also significant reduction in stained areas in both groups.
In randomized controlled trial done by Gugnani et al.,[27] the results revealed that 3-min increased resin infiltration provides the best treatment approach based on the parameters assessed. There was significant difference in mean and standard deviation in the change of esthetics and improvement in opacities (P < 0.01). Mann–Whitney U test revealed significantly better results for resin infiltration or combination with bleaching compared with bleaching alone (P < 0.001).
In the study done by Loguercio et al.,[28] microabrasion procedure was selected as the treatment option for very mild and mild fluorosis. This study suggests that enamel microabrasion using PREMA or Opalustre compounds is effective for the removal of stains and improves the appearance of the teeth. However, when the performance of both materials was compared after the first clinical appointment, the Opalustre compound showed a significant difference rating for improvement in appearance (3.4 ± 0.7) than the PREMA compound (2.4 ± 0.5) (Wilcoxon test, P = 0.002).
This systematic review revealed that resin infiltration with increased infiltration time, resin infiltration followed by bleaching, and resin infiltration alone have a better treatment results compared with bleaching alone. Besides, microabrasion method showed no significant difference with microabrasion followed by bleaching.
Discussion
This current systematic review summarizes the treatment approaches available for treating mild-to-moderate dental fluorosis based on the five randomized controlled trials. In comparison to bleaching, microabrasion results in less esthetic improvement and patient satisfaction. Meanwhile, combination of microabrasion and at-home bleaching reveals greater improvement and patient satisfied with the treatment. However, one of the studies revealed that there is no significant added value in microabrasion followed by at-home bleaching which gave the same results as microabrasion alone. On the other hand, one report suggested that microabrasion is effective in treating mild fluorosis but less effective against moderate fluorosis. Some disadvantages of microabrasion include difficulties in the complete elimination of deep white opaque area and brown stain from the tooth, slightly yellowish color of enamel after treatment, and uniformity of the tooth appearance is disrupted.[29]
Besides, resin infiltration is found to be the best option in improving esthetics in dental fluorosis. Based on the study done by Gugnani et al.,[30] resin infiltration with additional infiltrant provides the best esthetic result compared with bleaching alone. One of the benefits of resin infiltration is its’ efficacy and capability to arrest caries and it was also suggested for the treatment of post orthodontic white spot lesions.[20,31,32] Some study suggests that increasing the etching time would result in a better masking fluorosis stain.[30] The recommended etching time in resin infiltration technique is 120 s. However, it is only recommended in active early carious. In fluorosis stain, it will stimulate inactive lesions. In active caries fluorosis stain, the hypomineralized zone may be deep seated, which increases the resistant to the infiltration process. Thus, in order to assure that there is erosion up to the depth of hypomineralized zone and subsequent penetration of infiltrant till the depth of hypomineralized zone, etching of the inactive surface is repeated a few times until there is visual change in the color of tooth surface. The etching step was repeated maximum of three times. Through this, the deeper penetration of infiltrant will improve esthetic function.[30,33]
Some study revealed that patient complains of tooth sensitivity and gingival irritation after treatment, especially microabrasion.[25,26] This may be due to the reduction of enamel thickness. However, the problem should not be a major concern as it will dissipate after a while.
In this systematic review, there are few limitations that may affect the results of this study. Small trials and limited sample size may be one of the reason.
Conclusion
In conclusion, the treatment approach in dental fluorosis depends on its severity. Based on this systematic review, it is proven in the trials that resin infiltration with increased infiltration time, resin infiltration followed by bleaching, and resin infiltration alone will provide a better esthetic results. Thus, these treatments are recommended in mild-to-moderate dental fluorosis. Meanwhile, in mild fluorosis, microabrasion, bleaching, and combination of both are also preferable treatment options. Therefore, it is essential to analyze the fluorosis index before treating the patient with a complaint of tooth discoloration to determine the most effective approach in treating the patient. Other approaches such as crown and laminated veneer can also be done. However, no randomized controlled trials on crown and veneer have been done. Because dental fluorosis is an endemic disease and one of the public health concerns, these treatment options will provide a better outcome to the patients who demand curative options. Besides, it is important for the pediatrician and dentist to emphasis on the prevention of dental fluorosis to minimize the risk of dental fluorosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Gupta A, Dhingra R, Chaudhuri P, Gupta A. A comparison of various minimally invasive techniques for the removal of dental fluorosis stains in children. J Indian Soc Pedod Prev Dent. 2017;35:260–8. doi: 10.4103/JISPPD.JISPPD_138_16. [DOI] [PubMed] [Google Scholar]
- 2.Ng F, Manton D. Aesthetic management of severely fluorosed incisors in an adolescent female. Aust Dent J. 2007;52:243–8. doi: 10.1111/j.1834-7819.2007.tb00495.x. [DOI] [PubMed] [Google Scholar]
- 3.Aoba T, Fejerskov O. Dental fluorosis: Chemistry and biology. Crit Rev Oral Biol Med. 2002;13:155–70. doi: 10.1177/154411130201300206. [DOI] [PubMed] [Google Scholar]
- 4.Wright J, Chen S, Hall K, Yamauchi M, Bawden J. Protein characterization of fluorosed human enamel. J Dent Res. 1996;75:1936–41. doi: 10.1177/00220345960750120401. [DOI] [PubMed] [Google Scholar]
- 5.DenBesten P. Biological mechanisms of dental fluorosis relevant to the use of fluoride supplements. Community Dent Oral Epidemiol. 1999;27:41–7. doi: 10.1111/j.1600-0528.1999.tb01990.x. [DOI] [PubMed] [Google Scholar]
- 6.Robinson C, Connell S, Kirkham J, Brookes S, Shore R, Smith A. The effect of fluoride on the developing tooth. Caries Res. 2004;38:268–76. doi: 10.1159/000077766. [DOI] [PubMed] [Google Scholar]
- 7.Abanto Alvarez J, Rezende KMP, Salazar Marocho SM, Bucholdz Teixeira Alves F, Celiberti P, Ciamponi AL. Dental fluorosis: Exposure, prevention and management. Med Oral Patol Oral Cir Bucal. 2009;14:E103–7. [PubMed] [Google Scholar]
- 8.Wong EY, Stenstrom MK. Onsite defluoridation system for drinking water treatment using calcium carbonate. J Environ Manage. 2018;216:270–4. doi: 10.1016/j.jenvman.2017.06.060. [DOI] [PubMed] [Google Scholar]
- 9.Arora M, Maheshwari RC. Fluoride in drinking water and its removal. J Hazard Mater. 2006;137:456–63. doi: 10.1016/j.jhazmat.2006.02.024. [DOI] [PubMed] [Google Scholar]
- 10.Majumder BP. Brown teeth-diagnosis and management: A case report. EC Dent Sci. 2019;18:285–9. [Google Scholar]
- 11.Fejerskov O, Yaeger J, Thylstrup A. Microradiography of the effect of acute and chronic administration of fluoride on human and rat dentine and enamel. Arch Oral Biol. 1979;24:123–30. doi: 10.1016/0003-9969(79)90060-8. [DOI] [PubMed] [Google Scholar]
- 12.Akpata E. Therapeutic management of dental fluorosis: A critical review of literature. Saudi J Oral Sci. 2014;1:3–13. [Google Scholar]
- 13.Govila V, Govila S, Gupta S, Singh D. Prevention of dental fluorosis and its varied treatment options ‘A case series’. Int J Oral Health Dent. 2016;2:50–5. [Google Scholar]
- 14.Berhane Y, Demissie B, Zerihun L, Makonnen E, Eshete B. Preventing dental fluorosis. Ethiop J Health Dev. 2002;16:225–6. [Google Scholar]
- 15.Churchill H. Occurrence of fluorides in some waters of the United States. Ind Eng Chem. 1931;23:996–8. [Google Scholar]
- 16.Shortt H, Pandit C, Raghavachari RST. Endemic fluorosis in the Nellore district of South India. Indian Med Gaz. 1937;72:396–8. [PMC free article] [PubMed] [Google Scholar]
- 17.Dean HT. Classification of mottled enamel diagnosis. J Am Dent Assoc (1922) 1934;21:1421–6. [Google Scholar]
- 18.Dean HT, McKay FS. Production of mottled enamel halted by a change in common water supply. Am J Public Health Nations Health. 1939;29:590–6. doi: 10.2105/ajph.29.6.590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Black GV. Mottled teeth: An endemic developmental imperfection of the enamel of the teeth heretofore unknown in the literature of dentistry. Dental Cosmos. 1916;58:129–56. [Google Scholar]
- 20.Shafiei F, Tavangar M, Alavi A. Direct esthetic rehabilitation of teeth with severe fluorosis: A case report. J Dent (Shiraz) 2014;15:44–7. [PMC free article] [PubMed] [Google Scholar]
- 21.Shen L, Feng C, Xia S, Wei Y, Zhang H, Zhao D, et al. Progressive Research in the Molecular Mechanisms of Chronic Fluorosis. Fluoride Pollution-Facts and Fundamental Findings of Health and Environmental Remediation: IntechOpen. 2019 [Google Scholar]
- 22.ES A. Occurrence and management of dental fluorosis. Int Dent J. 2001;51:325–33. doi: 10.1002/j.1875-595x.2001.tb00845.x. [DOI] [PubMed] [Google Scholar]
- 23.Budhwar P, Yadav R, Rao PL. Aesthetic management of discoloured anterior teeth with zirconia: A case report. J Appl Dent Med Sci. 2019;5:1. [Google Scholar]
- 24.Di Giovanni T, Eliades T, Papageorgiou SN. Interventions for dental fluorosis: A systematic review. J Esthet Restor Dent. 2018;30:502–8. doi: 10.1111/jerd.12408. [DOI] [PubMed] [Google Scholar]
- 25.Castro KS, de Araújo Ferreira AC, Duarte RM, Sampaio FC, Meireles SS. Acceptability, efficacy and safety of two treatment protocols for dental fluorosis: A randomized clinical trial. J Dent. 2014;42:938–44. doi: 10.1016/j.jdent.2014.01.011. [DOI] [PubMed] [Google Scholar]
- 26.Meireles SS, Goettems ML, Castro KS, Sampaio FC, Demarco FF. Dental fluorosis treatment can improve the individuals’ OHRQoL? Results from a randomized clinical trial. Braz Dent J. 2018;29:109–16. doi: 10.1590/0103-6440201801733. [DOI] [PubMed] [Google Scholar]
- 27.Gugnani N, Pandit I, Gupta M, Gugnani S, Soni S, Goyal V. Comparative evaluation of esthetic changes in nonpitted fluorosis stains when treated with resin infiltration, in-office bleaching, and combination therapies. J Esthet Restor Dent. 2017;29:317–24. doi: 10.1111/jerd.12312. [DOI] [PubMed] [Google Scholar]
- 28.Loguercio A, Correia L, Zago C, Tagliari D, Neumann E, Gomes O, et al. Clinical effectiveness of two microabrasion materials for the removal of enamel fluorosis stains. Oper Dent. 2007;32:531–8. doi: 10.2341/06-172. [DOI] [PubMed] [Google Scholar]
- 29.Celik E, Yazkan B, Yildiz G, Tunac A. Clinical performance of a combined approach for the esthetic management of fluorosed teeth: Three-year results. Niger J Clin Pract. 2017;20:943–51. doi: 10.4103/1119-3077.180066. [DOI] [PubMed] [Google Scholar]
- 30.Gugnani N, Pandit I, Goyal V, Gugnani S, Sharma J, Dogra S. Esthetic improvement of white spot lesions and non-pitted fluorosis using resin infiltration technique: Series of four clinical cases. J Indian Soc Pedod Prev Dent. 2014;32:176. doi: 10.4103/0970-4388.130996. [DOI] [PubMed] [Google Scholar]
- 31.Paris S, Meyer-Lueckel H. Masking of labial enamel white spot lesions by resin infiltration--A clinical report. Quintessence Int. 2009;40:713–8. [PubMed] [Google Scholar]
- 32.Höchli D, Hersberger-Zurfluh M, Papageorgiou SN, Eliades T. Interventions for orthodontically induced white spot lesions: A systematic review and meta-analysis. Eur J Orthodont. 2016;39:122–33. doi: 10.1093/ejo/cjw065. [DOI] [PubMed] [Google Scholar]
- 33.Bharath K, Subba Reddy V, Poornima P, Revathy V, Kambalimath H, Karthik B. Comparison of relative efficacy of two techniques of enamel stain removal on fluorosed teeth. An in vivo study. J Clin Pediatr Dent. 2014;38:207–14. doi: 10.17796/jcpd.38.3.0h120nkl8852p568. [DOI] [PubMed] [Google Scholar]