Abstract
Background:
Fiber-optic nasopahryngolaryngoscopy is a visual examination of the larynx and its related structures. It is an effective procedure for ascertaining the causes of laryngeal disorders, pain in the throat, and difficulty in swallowing and hence should be used in all ENT clinics routinely. This study established the diagnostic effectiveness of fiber-optic nasoparyngolaryngoscopy in our clinics in Federal Teaching Hospital Ido-Ekiti, Ekiti State, Nigeria. It also analyzed the indications, findings, and the role it played in the management of the patients.
Materials and Methods:
This was a one-year (May 2015 to April 2019) prospective study involving 100 patients who had nasolaryngoscopy procedures done in the ear, nose, and throat (ENT) surgery clinics of Federal Teaching Hospital Ido-Ekiti, Ekiti State, Nigeria. A structured proforma was designed for the study. The data collected included the biodata (age and sex), presenting symptoms/indications for the procedure and findings at nasopharyngolaryngoscopy. These were entered into SPSS version 24 computer software and analyzed descriptively.
Results:
A total of 100 patients had the procedure during the study period. The mean age and standard deviation of respondents were 47.3 ± 16.4 years with more than half (71.0%) being females. The male to female ratio was 1:2.4. Majority of the patients were in the age range of 60 years and above (28.0%) while the minority were less than 20 years (6.0%).
Conclusion:
This study substantiates the contention that flexible nasopharyngolaryngoscopy is a very effective diagnostic tool for the patients presenting with upper airway related symptoms.
Keywords: Goiter, hoarseness, nasal mass, nasopharyngolaryngoscope
Introduction
Upper airway diseases can involve any anatomical site from the nose to the carina necessitating thorough visualization of the affected area. These regions are in dark narrow passages and its visualization is essential for the practice of otorhinolaryngology. Traditionally, this visualization has been achieved with the use of mirrors and various sources of light. The technique of mirror visualization is one of the skills of the practicing otorhinolaryngologist, which enables him to visualize the areas of his interest for the purpose of making a diagnosis and/or at times to perform limited interventions.[1] Progressive technological advancement in the areas of optics, illumination, and video technology has improved our ability to conduct such visualization with improved image quality and its ability to store these images in retrievable formats.[1] Flexible nasopharyngoscope enables examination of the upper airway, hypopharynx, and larynx, and also provides the capability to concurrently perform a biopsy from any suspicious area or growth. Fiber-optic nasopharyngoscopy can allow visualization of the following structures: nasal cavity, septum, middle meatal space and infundibulum, frontal recess, sphenoid ethmoid recess, turbinates, posterior choanae, eustachian tube orifices, adenoids, nasopharynx, posterior surface of the uvula and palate, velopharyngeal valve, adenoids, base of the tongue, pharyngeal and lingual tonsils, vallecula, pyriform spaces, epiglottis/supraglottis, glottis with mobility or immobility of the vocal folds and arytenoids, and immediate subglottis space.
This study aimed to evaluate the diagnostic effectiveness of flexible nasopharyngolaryngoscopy.
Materials and Methods
A total of 100 patients with upper airway related symptoms or with anterior neck swelling and for whom thyroidectomy procedure was indicated, were included in the study. Informed consent was taken for the procedure.
The equipment used was Xion Flexible Fiber-optic nasopharyngolaryngoscope with video monitoring [Figure 1].
Figure 1.

Xion Flexible Fiber-optic nasopharyngolaryngoscope with video monitoring
As preparation, the nose was sprayed with a solution of topical decongestant agent and local anesthetic (4% xylocaine solution and xylometazoline) 10 min before the procedure. The nose was not packed with this solution. The throat was further sprayed with the local anesthetic.
Under sterile conditions, the flexible nasopharyngolaryngoscope was passed transnasally and the required area visualized and examined. Savlon (Cetrimide 3.0% w/v + Chlorhexidine Gluconate 0.3% w/v) solution was used as defogging solution whenever necessary. All procedures were done as day cases. A structured proforma was designed for the study. The data collected included the biodata (age and sex), presenting symptoms/indications for the procedure and findings at nasopharyngolaryngoscopy. The data were statistically analyzed using SPSS version 24.
The patients who did not consent and patients less than 5 years of age who might not cooperate well for the procedure were excluded from the study.
Results
A total of 100 patients had the procedure being performed during the study period. Table 1 showed the age and gender distribution of the patients. The mean age and standard deviation of the respondents were 47.3 ± 16.4 years with more than half (71.0%) of them being females. The male to female ratio was 1:2.4. The majority of the patients were in the age range of 60 years and above (28.0%) while the minority were less than 20 years (6.0%). Figure 2 showed that majority of the patients were 40 years and above. Indications for nasopharyngoscopy among the patients were illustrated in Table 2. Goiter/Thyroid cyst (45.0%) accounted for the highest indication. Others were hoarseness (26.0%), epistaxis (6.0%), and foreign body (5.0%). Most of the patients who had the procedure done had normal findings (59.0%) [Table 3]. Nasal mass was seen in 15.0%, bilateral vocal cord nodules (5.0%), sloughs over the oropharynx and epiglottis in 6.0%, laryngeal tumor in 4.0%, and right atrophic vocal cord in 2.0%. Table 4 illustrated the indications distributed by gender. There was a statistically significant relationship between different indications for nasopharyngoscopy and gender at the 0.05 level (P < 0.001). All the patients with goiter/thyroid cyst were female (n = 45,100%). Most of the patients who had the procedure for epistaxis were male (n = 4,66.7%) and female accounted for (n = 2,33.3%). However, those patients who had it for chronic rhinosinusitis, throat pain, laryngeal tumor, and corrosive ingestion were all male (100.0%). Table 5 depicted that the relationship between nasopharyngoscopic findings and gender was statistically significant at the 0.05 level (P < 0.001). Of the 59 patients with normal findings, 47 (79.7%) were female and 12 (20.3%) were male [Table 5]. All patients with vocal cord nodules and paresis were female (100.0%). Table 6 showed that there was a statistically significant relationship between different indications for nasopharyngoscopy and age at 0.05 level (P = 0.001). Majority of the patients were 40 years and above in age (71.0%) with goiter (preoperative for thyroidectomy) being the highest followed by hoarseness (n = 18,69.2%). The relationship between nasopharyngoscopic findings and age [Table 7] was not however statistically significant at 0.05 level (P = 0.317).
Table 1.
Age and gender of patients
| Variable | Frequency (n=100) | Percentage (%) |
|---|---|---|
| Age group (in years) | ||
| <20 | 6 | 6.0 |
| 20-29 | 8 | 8.0 |
| 30-39 | 15 | 15.0 |
| 40-49 | 30 | 30.0 |
| 50-59 | 13 | 13.0 |
| 60 and above | 28 | 28.0 |
| Mean±SD | 47.3±16.4 | |
| Range | 10-82 | |
| Gender | ||
| Male | 29 | 29.0 |
| Female | 71 | 71.0 |
Figure 2.
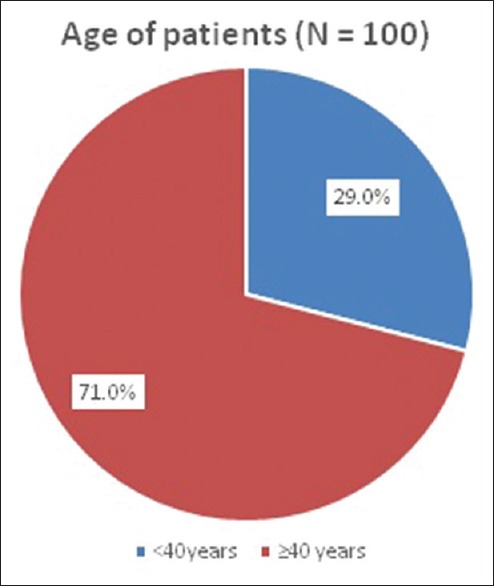
Age <40 and ≥40 years
Table 2.
Indications for nasopharyngoscopy
| Variable | Frequency (n=100) | Percentage (%) |
|---|---|---|
| Indication | ||
| Foreign body | 5 | 5.0 |
| Goitre/Thyroid cyst. | 45 | 45.0 |
| Hoarseness | 26 | 26.0 |
| Epistaxis | 6 | 6.0 |
| Difficulty in swallowing | 2 | 2.0 |
| Nasal mass | 8 | 8.0 |
| Chronic rhinosinositis | 2 | 2.0 |
| Throat pain/Odynophagia | 2 | 2.0 |
| Laryngeal tumour | 2 | 2.0 |
| Corrosive ingestion | 2 | 2.0 |
Table 3.
Patients’ nasopharyngoscopic findings
| Variable | Frequency (n=100) | Percentage (%) |
|---|---|---|
| Finding | ||
| Normal | 59 | 59.0 |
| Bilateral vocal cord nodules | 5 | 5.0 |
| Left vocal cord paresis | 3 | 3.0 |
| Slough over the oropharynx and the epiglottis | 6 | 6.0 |
| Fish bone in the left vallecular area | 2 | 2.0 |
| Nasal mass | 15 | 15.0 |
| Right vocal nodules | 2 | 2.0 |
| Atrophic right vocal cord | 2 | 2.0 |
| Bilateral vocal cord paresis | 2 | 2.0 |
| Laryngeal tumour | 4 | 4.0 |
Table 4.
Indications distributed by gender
| Variable | Gender | Chi square | P | |
|---|---|---|---|---|
| Male n (%) | Female n (%) | |||
| Indication | ||||
| Foreign body | 2 (40.0) | 3 (60.0) | 47.161 | <0.001 |
| Goitre/Thyroid cyst. | 0 (0.0) | 45 (100.0) | ||
| Hoarseness | 11 (42.3) | 15 (57.7) | ||
| Epistaxis | 4 (66.7) | 2 (33.3) | ||
| Difficulty in swallowing | 0 (0.0) | 2 (100.0) | ||
| Nasal mass | 4 (50.0) | 4 (50.0) | ||
| Chronic rhinosinositis | 2 (100.0) | 0 (0.0) | ||
| Throat pain/Odynophagia | 2 (100.0) | 0 (0.0) | ||
| Laryngeal tumour | 2 (100.0) | 0 (0.0) | ||
| Corrosive ingestion | 2 (100.0) | 0 (0.0) | ||
| Total | 29 (29.0) | 71 (71.0) | ||
Table 5.
Patients’ nasopharyngoscopic findings distributed by gender
| Variable | Gender | Chi square | P | |
|---|---|---|---|---|
| Male n (%) | Female n (%) | |||
| Finding | ||||
| Normal | 12 (20.3) | 47 (79.7) | 35.441 | <0.001 |
| Bilateral vocal cord nodules | 0 (0.0) | 5 (100.0) | ||
| Left vocal cord paresis | 0 (0.0) | 3 (100.0) | ||
| Slough over the oropharynx and the epiglottis | 2 (33.3) | 4 (66.7) | ||
| Fish bone in the left vallecular area | 2 (100.0) | 0 (0.0) | ||
| Nasal mass | 9 (60.0) | 6 (40.0) | ||
| Right vocal nodules | 0 (0.0) | 2 (100.0) | ||
| Atrophic right vocal cord | 0 (0.0) | 2 (100.0) | ||
| Bilateral vocal cord paresis | 0 (0.0) | 2 (100.0) | ||
| Laryngeal tumour | 4 (100.0) | 0 (0.0) | ||
Table 6.
Indication of findings distributed by age
| Variable | Age (in years) | Chi-square | P | |
|---|---|---|---|---|
| <40 n (%) | ≥40 n (%) | |||
| Indication | ||||
| Foreign body | 5 (100.0) | 0 (0.0) | 28.042 | 0.001 |
| Goitre/Thyroid cyst. | 10 (22.2) | 35 (77.8) | ||
| Hoarseness | 8 (30.8) | 18 (69.2) | ||
| Epistaxis | 0 (0.0) | 6 (100.0) | ||
| Difficulty in swallowing | 0 (0.0) | 2 (100.0) | ||
| Nasal mass | 2 (25.0) | 6 (75.0) | ||
| Chronic rhinosinositis | 2 (100.0) | 0 (0.0) | ||
| Throat pain/Odynophagia | 0 (0.0) | 2 (100.0) | ||
| Laryngeal tumour | 0 (0.0) | 2 (100.0) | ||
| Corrosive ingestion | 0 (0.0) | 2 (100.0) | ||
| Total | 29 (29.0) | 71 (71.0) | ||
Table 7.
Patients’ nasopharyngoscopic findings distributed by age
| Variable | Age (in years) | Chi square | P | |
|---|---|---|---|---|
| <40 n (%) | ≥40 n (%) | |||
| Finding | ||||
| Normal | 19 (32.2) | 40 (67.8) | 11.536 | 0.317 |
| Bilateral vocal cord nodules | 2 (40.0) | 3 (60.0) | ||
| Left vocal cord paresis | 0 (0.0) | 3 (100.0) | ||
| Slough over the oropharynx & the epiglottis | 2 (33.3) | 4 (66.7) | ||
| Fish bone in the left vallecular area | 2 (100.0) | 0 (0.0) | ||
| Nasal mass | 4 (26.7) | 11 (73.3) | ||
| Right vocal nodules | 0 (0.0) | 2 (100.0) | ||
| Atrophic right vocal cord | 0 (0.0) | 2 (100.0) | ||
| Bilateral vocal cord paresis | 0 (0.0) | 2 (100.0) | ||
| Laryngeal tumour | 0 (0.0) | 4 (100.0) | ||
| Total | 29 (29.0) | 71 (71.0) | ||
Discussion
The development of flexible endoscope has increased both the diagnostic and therapeutic indications in clinical practice,[2] with the advantage of its simplicity in usage[3] and the need for only local anesthesia. Fiber-optic imaging was initially developed in the 1930s by a medical student named Heinrich Lamm who intended to visualize inaccessible regions of the body with his invention. Fiber-optic imaging became more visible in the medical literature during the 1950s with further innovations by Hopkins and Storz.[4] By 1963, Hirschowitz designed a medically functional fiber-optic scope with higher resolution, lighting, suction, and instrument ports.[5] Current fiber-optic nasopharyngoscopes are lighted, are flexible with 2-way articulation, provide inline viewing with photo and video capabilities, and can have a distal diameter as small as 2 mm. Endoscopes with calibrations provide useful sizing information for laryngeal structures.[6,7,8] and help in determining the extent of airway lesions.[7,8]
Nasolaryngoscopy is very useful in the visualization of the nose, pharynx, and larynx in head and neck examination.[9,10] The procedure has diverse indications.
Conclusion
This study substantiates the contention that flexible nasopharyngolaryngoscopy is a very effective diagnostic tool for the patients presenting with upper airway related symptoms However, this is not amenable for use in patients with laryngeal/hypopharyngeal tumor, which requires rigid direct laryngoscopy under general anesthesia. Some of the tumor patients may not be fit for general anesthesia due to comorbid conditions; in such patients, flexible nasoendoscopy can prove to be an effective tool particularly to obtain a tissue diagnosis.
Ethical approval
The study was approved by the Institutional Ethics Committee.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
My appreciation goes to my wife, Mrs Rukayat Olaitan Aremu and my children (Tiwalola, Lolade, Ojuolape, Olamide and Nifemi) for their advice when forming the concept of the study and their assistance and supports during the process of collecting and analyzing the data. I also acknowledge all the current residents of ENT Department, Federal Teaching Hospital Ido-Ekiti.
References
- 1.Adeyemo A, Ameye SA, Amusa YB, Eziyi JAE, Owojuyigbe AM, Badmus SA, et al. Setting-up office ENT endoscopy in low resource setting in semi-urban Hospital: Adaptations and modifications. Nigerian Journal of Otorhinolaryngology. 2017;14:14–7. [Google Scholar]
- 2.Hormann K, Schmidt H. Flexible endoscopy in the ENT area. HNO. 1998;46:654–9. doi: 10.1007/s001060050290. [DOI] [PubMed] [Google Scholar]
- 3.Dewitt DE. Fiberoptic rhinolaryngoscopy in primary care. A new direction for expanding in-office diagnostics. Postgrad Med. 1988;84:125–6. doi: 10.1080/00325481.1988.11700439. [DOI] [PubMed] [Google Scholar]
- 4.Fuchs GJ. Milestones in endoscope design for minimally invasive urologic surgery: The sentinel role of a pioneer. Surg Endosc. 2006;20(Suppl 2):S493–9. doi: 10.1007/s00464-006-0078-4. [DOI] [PubMed] [Google Scholar]
- 5.Hirschowitz B. A fiberoptic flexible esophagoscope. JAMA. 1963;2:388. doi: 10.1016/s0140-6736(63)93065-4. [DOI] [PubMed] [Google Scholar]
- 6.Kobler JB, Rosen DI, Burns JA, Akst LM, Broadhurst MS, Zeitels SM, et al. Comparison of a flexible laryngoscope with calibrated sizing function to intraoperative measurements. Ann Otol Rhinol Laryngol. 2006;115:733–40. doi: 10.1177/000348940611501004. [DOI] [PubMed] [Google Scholar]
- 7.Nouraei SA, McPartlin DW, Nouraei SM, Patel A, Ferguson C, Howard DJ, et al. Objective sizing of upper airway stenosis: A quantitative endoscopic approach. Laryngoscope. 2006;116:12–7. doi: 10.1097/01.mlg.0000186657.62474.88. [DOI] [PubMed] [Google Scholar]
- 8.Lucky OO, Chibuike N. Laryngoscopy: Appraisal of 202 procedures carried out in two centers in Port Harcourt, Nigeria. Niger Health J. 2017;17:256. [Google Scholar]
- 9.Olaosun AO, Oguntola AS, Adegbosin O, Akinloye A. Mirror laryngoscopy: A review of 43 cases. Surg J. 2009;4:29–34. [Google Scholar]
- 10.Iqbal Z, Rabbani MZ, Zafar MJ. Flexible nasopharyngolaryngoscopy: Diagnostic yield. Rawal Med J. 2009;34:148–50. [Google Scholar]


