Abstract
Context.
Although measures exist that assess patient engagement in the advance care planning (ACP) process, there are no validated tools to assess surrogate decision-makers’ (SDM) role in ACP.
Objectives.
To adapt and begin to validate a patient-oriented questionnaire for use with SDMs of patients with chronic illness
Methods.
Questions from the 55-item patient-oriented ACP engagement survey were adapted for SDMs and assessed for face validity. The resultant 47-item questionnaire was administered to 65 SDMs of patient with chronic illness. Responses were assessed and items were flagged for removal based on item redundancy, nonresponses, and ceiling effects. A preliminary exploratory factor analysis was performed, internal consistency assessed, and domains constructed based on findings.
Results.
The 47-item questionnaire was administered to 65 participants (mean age 51.8; 81% female; 96% Caucasian). 17 items were removed due to redundancy (r>0.80), 13 items lacking face validity were removed. In preliminary exploratory factor analysis of the resultant 17-item questionnaire, a 3-factor solution was deemed most statistically and conceptually sound. Items were organized into domains: 1) serving as a SDM (7-items); 2) contemplation (4-items); 3) Readiness (6-items). Internal consistency for each domain was high (Cronbach alpha 0.90–0.91).
Conclusion.
The 17-item ACP Engagement Survey for SDMs (ACP-17-SDM) is a conceptually sound and reliable questionnaire adaptation of the original ACP Engagement Survey. This questionnaire may be used by researchers in parallel with the patient-oriented ACP Engagement survey to more fully understand the impact of ACP interventions on SDMs. Larger studies are needed to more closely examine construct validity.
Keywords: Advance care planning, Psychometrics, Surveys and questionnaires, Terminal care, Caregivers, Decision-making
INTRODUCTION
Advance care planning (ACP) was recently defined by an international consensus panel as a process intended to “help ensure people receive medical care that is consistent with their values, goals, and preferences during serious and chronic illness”.[1] The panel also noted that ACP should include selection of an surrogate decision-makers (SDM) capable of making medical decisions should the patient become incapacitated.[1] The role of the SDM may also vary based on legal and cultural factors. When ACP is performed in advance of major medical events, patients experience less distress, improved satisfaction with care and are more likely to receive care consistent with their wishes. [2–8] Similarly, SDMs of patients who have done ACP are less likely to experience distress from medical decision-making and have improved satisfaction with care. [9, 2, 10] Despite these known benefits, however, < 30% of Americans and Canadians have completed the ACP process. [11–14]
Finding new ways to engage patients and their families in these important conversations is critical if we hope to increase the number of individuals who have documented advance care plans so clinicians and families may carry out their wishes. It is equally important to consider the role of SDMs in the ACP process since studies have found that up to 70% of individuals will need some or all of their end of life decisions to be made by a surrogate.[4] As ACP interventions have been developed and tested, however, assessment has focused primarily on patient engagement with ACP, either by measuring advance directive completion rates, [15, 16] or more recently, engagement in the comprehensive ACP process as measured by the ACP Engagement Survey.[17, 18] Absent, however, is a measure of surrogate engagement in the ACP process.
To measure patient engagement in ACP, Sudore et. al developed and validated a questionnaire grounded in Social Cognitive Theory and the Trans-theoretical Model of Behavior Change that has been utilized as an important outcome measure in several studies and interventional trials.[17–22] Although the psychometrics of that questionnaire, called the ACP Engagement Survey, have been well studied, it has not been adapted for use with the patients’ SDMs. The purpose of this study was to adapt the existing 55-item patient-oriented ACP Engagement Survey for use with SDMs and begin to assess the validity of the adapted survey.
METHODS
The study was approved by the Penn State Hershey Institutional Review Board; all participants provided consent via implied consent via return of the questionnaire.
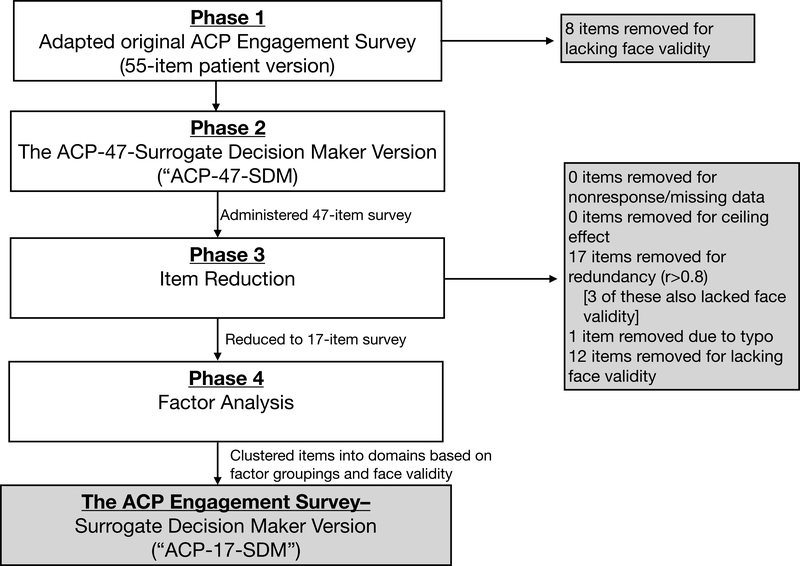
This prospective study was conducted in five phases (Figure 1).
Figure 1.
Methods for creating and validating the ACP Engagement Survey Surrogate Decision Maker Version (17 items)
Phase 1: Adapting the original ACP Engagement Survey for use with SDMs.
The patient version of the 55-item ACP Engagement Survey (ACP-55)[17] assesses four domains: 1) SDMs; 2) values and quality of life; 3) leeway in surrogate decision-making; and 4) asking doctors questions.[18] For each domain, items assess four behavior change constructs arising from the Trans-theoretical model of behavior change and Social Cognitive Theory: 1) knowledge; 2) contemplation; 3) self-efficacy; and 4) readiness.[18] The ACP-55 has been previously shown to have high reliability (Cronbach alpha 0.97) and construct validity based on both statistically significant associations between survey scores and completion of advance directives as well as correlations between change scores in response to an ACP intervention (r=0.89, p<0.001).[17] The survey has been used as an outcome in several studies examining the impact of ACP interventions.[23, 20, 21]
The ACP-55 question stems were reworded to apply to SDMs and then examined by an 8-person panel of ACP researchers, clinicians, and laypersons for face validity. Resultantly, 8 items were removed and 6 items flagged for re-evaluation after data collection. The result was a 47-item survey (ACP-SDM-47).
Phase 2: Administration of the ACP-SDM-47
After Institutional Review Board approval, the Penn State Survey Research Center recruited a convenience sample of participants identified from medical record databases using the following inclusion criterion: 1) >18 years old; 2) can read and write English; 3) had a family member who has a chronic illness (defined using Iezonni’s ICD-9 Criterion of chronic illness)[24]; and 4) were willing to complete and return the survey. The Iezonni chronic illness codes are grouped into eight categories that include: cancer with poor prognosis; chronic pulmonary disease; cornonary artery disease; congestive heart failure; peripheral vascular disease; severe, chronic liver disease; diabetes with end organ damage; and renal failure. Participants were also recruited from the community around Penn State University Park via flyers, social media postings, and community email lists. Interested participants contacted the survey center and screened by phone to confirm a) their family member had a qualifying chronic illness (via self- report) and b) that they did not have mental impairment as measured by a score of >21 on the Montreal Cognitive Assessment (MoCA, phone version).[25] Eligible participants were sent a paper copy of the ACP-SDM-47, a pre-paid return envelope, and a $10.00 stipend. Since this study focused on the feasibility, usability and acceptability of the adapted questionnaire and because we used a convience sampling strategy, a power analysis was not conducted.
Phase 3, Initial Item Reduction
First, frequency counts for each of the 47 items were examined for those with >10% nonresponses or missing data with the intention of item removal. Second, responses were examined for ceiling effect, defined as any item where the selection of the item at the top of the scale occurred in >80% of instances. Third, an item correlation matrix was constructed to assess for item redundancy, defined as those items with an r > 0.8. Redundant items were flagged for removal. Finally, the study team re-evaluated the face validity of all 47 items, informed by the psychometric results.
Phase 4, Preliminary Exploratory Factor Analysis
After removing items identified through the above item reduction process, a preliminary exploratory factor analysis (EFA) of this small sample was conducted to see if the remaining items grouped into domains. To avoid losing participants with some missing items, prior to the implementing the factor analysis, we used the Expectation-maximization (EM) algorithm to impute the most likely values for missing items given the values of the participants’ non-missing items and assuming the correlation structure observed between items among all participants.
We used the common factor model with PROMAX oblique factor rotation to allow for correlation between the underlying factors. The first step in the EFA was to decide how many factors should be retained. When making this decision we considered the amount of variance explained by the 2, 3, 4 and 5-factor solutions as well as the interpretability and parsimony of the resulting rotated factor solutions.[26]
Once the number of factors was decided upon and the rotated factor solution was obtained, we examined the factor loading matrix and identified the factors on which each item loaded most strongly. We grouped variables according to which item they loaded most heavily on (>0.5) and labelled the resultant grouping (‘domain’) to reflect the contents of its items. Face validity of the item groupings and the strength of the loadings and cross-loadings across domains were considered to determine whether any items should be placed in a domain other than the one that they loaded most heavily on. This was done through consensus among authors, only for situations where the factor loadings of an item were very similar between two domains, and if the item was felt to be more conceptually aligned to the domain with the slightly lower loading.
Phase 5, Evaluation of Internal Consistency
Internal reliability of the domains was assessed by Cronbach’s alpha. We reassessed Cronbach’s alpha after removing one item at a time from each domain to see if any item was reducing the internal consistency of the domain it was placed in.
All analyses were conducted in SAS Version 9.4 (SAS Institute Inc., Cary, NC, USA).
RESULTS
Phase 1; Adaptation of the ACP-55 and Review for Face Validity
During Phase 1, we adapted the original Patient Version of the 55-item ACP Engagement survey by altering the question stems to apply to SDMs and key informants (Appendix 1). For example, the patient-oriented ACP-55 item “How confident are you that today you could ask someone to be your medical decision maker?” was changed to “As of today, how confident are you that you could serve as your loved one’s medical decision maker” for the ACP-47-SDM. We opted not to change the wording of the question stems from the original survey because these stems were generated from focus groups including both patients and surrogates and the original survey was vetted extensively by patients.[18, 23] Since our goal was to align the survey as closely as possible to the well-validated ACP-55, stems were kept as close to the original as possible.
After reviewing the stem adaptations, eight items were removed due to a lack of face validity. For example, one item for the patient-oriented survey asked “how much have you thought about whether or not certain health situations would make your life not worth living?” The adapted version of this question became “how much have you thought about whether or not your loved one has considered certain health situations that would make his/her life not worth living?” This was deemed to lack face validity because the item now examined whether the SDM thought about whether the patient thought about the issues, a somewhat abstract concept that is non-critical to serving in the role of an SDM.
Phase 2, Survey Administration
Next, the ACP-47-SDM was administered to 65 participants with mean age 51.8 years (SD 13.8) and 81% female. No participants were excluded due to cognitive dysfunction. Racial data was collected for 49 participants who were 96% Caucasian, 4% African American, and was missing for 21 participants due to administrative error.
Phase 3, Item Reduction
Table 1 shows the reasons for exclusion for each of the removed items. No items were deleted as a result of missing data, nonresponses, or ceiling effect. We removed 17 items due to redundancy (correlations with r>0.8; Appendix 2). Two items that were highly correlated (r=0.744) and therefore deleted due to their redundancy were: “how much have you thought about the possibility of being asked to make medical decisions for your loved one?” and “how much have you thought about your role as your loved one’s medical decision-maker?” The remaining items were reviewed for face validity and 13 additional items were deleted. Reasons for deletion based on face validity included items involving two separate ideas within a single question (item #5), for example, thinking about playing the role of SDM and also thinking about being part of a discussion with others. Seven items were deleted because the group felt that the question inquired about thoughts/behaviors that were not the role of the SDM to initiate (for example, discussing one’s role as a SDM with the patient’s doctor; items # 6, 8, 9, 11,12, 23) and are also behaviors that the SDM cannot ‘act’ upon unless the patient themselves invited the action. Thus, including these items could negatively impact the SDM’s engagement score with regards to behaviors outside their own control. Hence, these items were deleted. Some items had multiple reasons for deletion as noted in Table 1. The resulting survey consisted of 17 remaining items.
Table 1.
Reasons for item exclusions from the 47-item ACP Engagement Survey- Surrogate Decision Maker version (post-survey administration)
| Item | Question | Reason For Exclusion |
|---|---|---|
| 1 | How well informed are you about who can be a medical decision maker? | Not Excluded |
| 2 | How well informed are you about what makes someone a good medical decision maker? | Not Excluded |
| 3 | How well informed are you about the types of decisions that you may have to make for your loved one in the future? | Not Excluded |
| 4 | How much have you thought about your role as your loved one’s medical decision-maker? | Not Excluded |
| 5 | How much have you thought about being part of a discussion with your loved one’s DOCTORS about your role as a medical decision-maker for your loved one? | Lacked Face Validity; doublebarreled question |
| 6 | How much have you thought about being part of a discussion with your loved one’s OTHER family and friends about your role as your loved one’s medical decision-maker? | Lacked Face Validity |
| 7 | As of today, how confident are you that you could serve as your loved one’s medical decision maker? | Not Excluded |
| 8 | As of today, how confident are you that you could be part of a discussion with your loved one’s DOCTORS about your role as your loved one’s medical decision maker? | Redundant with other items, lacked face validity |
| 9 | As of today, how confident are you that you could be part of a discussion with your loved one’s OTHER FAMILY and FRIENDS about your role as your loved one’s medical decision maker? | Redundant with other items, lacked face validity |
| 10 | How ready are you to formally discuss with your loved one your role as their medical decision maker? | Not Excluded |
| 11 | How ready are you to be part of a discussion with your loved one’s DOCTOR about your role as your loved one’s medical decision-maker? | Lacked Face Validity |
| 12 | How ready are you to be part of a discussion with your loved one’s OTHER FAMILY and FRIENDS about your role as your loved one’s medical decision maker? | Redundant with other items, lacked face validity |
| 13 | How ready are you to be named a medical decision maker in OFFICIAL PAPERS that are signed by your loved one? | Lacked Face Validity |
| 14 | How much have you thought about talking with your loved one about whether or not there are certain health situations that would make your loved one’s life not worth living? | Not Excluded |
| 15 | How much have you thought about being part of a discussion with your loved one’s DOCTORS about whether or not there are certain health situations that would make your loved one’s life not worth living? | Not Excluded |
| 16 | How much have you thought about being part of a discussion with your loved ones OTHER FAMILY and FRIENDS about whether or not there are certain health situations that would make your loved one’s life not worth living? | Redundant with other items |
| 17 | As of today, how confident are you that you could talk with your loved one about whether or not certain health situations would their life not worth living? | Redundant with other items |
| 18 | As of today, how confident are you that you could be part of a discussion with your loved one’s DOCTORS about whether or not there are certain health situations that would make your loved one’s life not worth living? | Redundant with other items |
| 19 | As of today, how confident are you that you could talk with your loved one’s OTHER FAMILY and FRIENDS about whether or not there are certain health situations that would make your loved one’s life not worth living? | Redundant with other items items |
| 20 | How ready are you to talk with your loved one about whether or not there are certain health situations that would make their life not worth living? | Not Excluded |
| 21 | How ready are you to be part of a discussion with your loved one’s DOCTOR about whether or not there are certain health situations that would make your loved one’s life not worth living? | Not Excluded |
| 22 | How ready are you to be part of a discussion with your loved one’s OTHER FAMILY and FRIENDS about whether or not there are certain health situations that would make your loved one’s life not worth living? | Redundant with other items |
| 23 | How ready are you help your loved one SIGN OFFICIAL PAPERS putting his/her wishes in writing about whether or not there are certain health situations that would make your loved one’s life not worth living? | Lacked Face Validity |
| 24 | How much have you thought about talking with your loved one about the care he/she would want if they were very sick or near the end of life? | Not Excluded |
| 25 | How much have you thought about being part of a discussion with your loved one’s DOCTORS about the care your loved one would want if he/she was very sick or near the end of life? | Not Excluded |
| 26 | How much have you thought about being part of a discussion with your loved one’s OTHER FAMILY and FRIENDS about the care your loved one would want if he/she were very sick or near the end of life? | Redundant with other items |
| 27 | As of today, how confident are you that you could talk with your loved one about the care he/she would want if he/she were very sick or near the end of life? | Not Excluded |
| 28 | As of today, how confident are you that you could be part of a discussion with your loved one’s doctors about the care your loved one would want if he/she were very sick or near the end of life? | Not Excluded |
| 29 | As of today, how confident are you that you could be part of a discussion with your loved one’s OTHER FAMILY and FRIENDS about the care your loved one would want if he/she were very sick or near the end of life? | Redundant with other items |
| 30 | How ready are you to talk to your loved one about the kind of medical care he/she would want if they were very sick or near the end of life? | Not Excluded |
| 31 | How ready are you to be part of a discussion with your loved one’s DOCTOR about the kind of medical care your loved one would want if he/she were very sick or near the end of life? | Not Excluded |
| 32 | How ready are you to be part of a discussion with your loved one’s OTHER FAMILY and FRIENDS about the kind of medical care he/she would want if he/she were very sick or near the end of life? | Redundant with other items |
| 33 | How ready are you to help your loved one SIGN OFFICIAL PAPERS putting his/her wishes in writing about the kind of medical care he/she would want if he/she very sick or near the end of life? | Redundant with other items; lacked Face Validity |
| 34 | How well informed are you about the different amounts of flexibility a person can give their medical decision maker? | Lacked Face Validity |
| 35 | How much have you thought about the amount of flexibility you would have as your loved one’s medical decision maker? | Redundant with other items; lacked Face Validity |
| 36 | How much have you thought about talking with your loved one about the amount of flexibility he/she would want to give you as a medical decision maker? | Lacked Face Validity |
| 37 | How much have you thought about being part of a discussion with your loved one’s DOCTOR about the amount of flexibility you would have as the medical decision maker? | Redundant with other items; lacked Face Validity |
| 38 | How much have you thought about being part of a discussion with your loved one’s OTHER family and friends about the amount of flexibility you would have as the medical decision maker? | Lacked Face Validity |
| 39 | As of today, how confident are you that you could talk with your loved one about how much flexibility he/she would want to give you as a medical decision maker? | Lacked Face Validity |
| 40 | As of today, how confident are you that you could be part of a discussion with your loved one’s DOCTOR about how much flexibility your loved one would want to give you as a medical decision maker? | Lacked Face Validity |
| 41 | As of today, how confident are you that you could be part of a discussion with your loved one’s OTHER family and friends about how much flexibility your loved one would want to give you as a medical decision maker? | Lacked Face Validity |
| 42 | How ready are you to talk to your loved one about how much flexibility he/she would want to give you as a medical decision maker? | Lacked Face Validity |
| 43 | How ready are you to be part of a discussion with your loved one’s DOCTOR about how much flexibility your loved one would want to give you as a medical decision maker? | Redundant with other items; lacked Face Validity |
| 44 | How ready are you to be part of a discussion with your loved one’s OTHER FAMILY and FRIENDS about how much flexibility your loved one would want to give you as a medical decision maker? | Redundant with other items; lacked Face Validity |
| 45 | How ready are you to help your loved one SIGN OFFICIAL PAPERS about how much flexibility he/she would want to give you as a medical decision maker? | Redundant with other items; lacked Face Validity |
| 46 | How confident are you that today you could ask the right questions of your loved one’s doctors to help make good medical decisions for your loved one if your loved one was unable to speak for themselves? | Deleted due to typo in question stem |
| 47 | How ready are you to ask your loved one’s doctor questions to help you make a good medical decision for your loved one if your loved one was unable to speak for themselves? | Not Excluded |
Phase 4, Preliminary Exploratory Factor Analysis
Eight (12%) of the 65 participants had missing data for at least one of the 17 items. One participant, missed 7 items, and 7 respondents missed between 1 and 4 items. All missing item values were imputed priori to factor analysis so all 65 participants could be included (see methods).
A 1-factor solution explained 78% of the variance in the 17 items, 2 factors explained 86%, 3 factors explained 91%, 4 factors explained 95%, and 5 factors explained 99%. We reviewed the 2, 3, 4 and 5-factor solutions and selected the 3-factor solution for its simplicity and interpretability. The three factors were correlated with each other with the three pairwise Pearson’s correlation coefficients ranging from 0.59 to 0.63.
We reviewed the items that loaded onto the 3-factor solution and grouped items according to their factor loadings (Table 2). The 7 items grouped in Factor 1 were reviewed for face validity by assessing the common features of these items with regards to their theoretical construct (e.g. self-perceived confidence). The identified similarities were that all items assessed either knowledge or self-efficacy about serving as a SDM, and thus the factor was labeled “serving as SDMs”. No changes were made to Factor 1 based on face validity or clinical sensibility. The loadings of Factor 1 ranged from 0.48 to 0.89.
Table 2.
Exploratory Analysis of the 17-item questionnaire
| Items | Theoretical construct |
Factor 1 Serving as SDM Domain |
Factor 2 Contemplation Domain |
Factor 3 Readiness Domain |
Communality1 |
|---|---|---|---|---|---|
| 1. How well informed are you about who can be a medical decision maker? | Knowledge | 0.89 | −0.03 | −0.02 | 0.74 |
| 2. How well informed are you about what makes someone a good medical decision maker? | Knowledge | 0.89 | −0.12 | 0.06 | 0.75 |
| 3. How well informed are you about the types of decisions that you may have to make for your loved one in the future? | Knowledge | 0.70 | 0.09 | 0.03 | 0.62 |
| 4. How much have you thought about your role as your loved one’s medical decisionmaker? | Contemplation | 0.52 | 0.19 | 0.12 | 0.53 |
| 5. As of today, how confident are you that you could serve as your loved one’s medical decision maker? | Self-efficacy | 0.70 | 0.06 | 0.03 | 0.57 |
| 6. As of today, how confident are you that you could talk with your loved one about the care he/she would want if he/she were very sick or near the end of life? | Self-efficacy | 0.48 | 0.23 | 0.14 | 0.55 |
| 7. As of today, how confident are you that you could be part of a discussion with your loved one’s DOCTOR about the care your loved one would want if he/she were very sick or near the end of life? | Self-efficacy | 0.51 | 0.31 | 0.11 | 0.67 |
| 8. How much have you thought about talking with your loved one about whether or not there are certain health situations that would make your loved one’s life not worth living? | Contemplation | 0.29 | 0.24 | 0.38 | 0.62 |
| 9. How much have you thought about being part of a discussion with your loved one’s DOCTORS about whether or not there are certain health situations that would make your loved one’s life not worth living? | Contemplation | 0.06 | 0.49 | 0.30 | 0.57 |
| 10. How much have you thought about talking with your loved one about the care he/she would want if they were very sick or near the end of life? | Contemplation | 0.14 | 0.62 | 0.28 | 0.86 |
| 11. How much have you thought about being part of a discussion with your loved one’s DOCTORS about the care he/she would want if they were very sick or near the end of life? | Contemplation | 0.05 | 1.04 | −0.12 | 1.00 |
| 12. How ready are you to formally discuss with your loved one your role as their medical decision maker? | Readiness | 0.38 | −0.06 | 0.50 | 0.56 |
| 13. How ready are you to talk to your loved one about the kind of medical care he/she would want if they were very sick or near the end of life? | Readiness | −0.04 | 0.09 | 0.93 | 0.92 |
| 14. How ready are you to talk to your loved one about whether or not there are certain health situations that would make your loved one’s life not worth living? | Readiness | 0.16 | 0.07 | 0.72 | 0.76 |
| 15. How ready are you to be part of a discussion with your loved one’s DOCTOR about whether or not there are certain health situations that would make your loved one’s life not worth living? | Readiness | 0.20 | 0.22 | 0.49 | 0.63 |
| 16. How ready are you to be part of a discussion with your loved one’s DOCTOR about the kind of medical care your loved one would want if he/she were very sick or near the end of life? | Readiness | 0.00 | 0.42 | 0.46 | 0.63 |
| 17. How ready are you to ask your loved one’s DOCTOR questions to help you make a good medical decision for your loved one if your loved one was unable to speak for themselves? | Readiness | −0.11 | 0.47 | 0.28 | 0.37 |
The communality is the proportion of the variance of the item accounted for by the 3 factors solution. Ideally, the communality would be near 1 and would be caused by a near 1 loading on single factor, but communalities greater than 0.4 or 0.5 are typically considered acceptable.
Factor 2 had 5 items which were reviewed using similar procedures. It was noted that 3 of the 5 items involved contemplation about various aspects of surrogate decision-making. One item (item #8; how much have you thought about talking with your loved one about whether or not there are certain health situations that would make your loved one’s life not worth living?) ) that was related to contemplation loaded weakly into the 3rd factor (0.38) with a loading of 0.24 in Factor 2. We decided to move this item into Factor 2 based on face validity since the other items in factor 2 all assessed contemplation. It was also noted that one item (item#17; how ready are you to ask your loved one’s doctor questions to help you make a good medical decision for your loved one if your loved one was unable to speak for themselves?) loaded into Factor 2 with a value of 0.47 but had higher face validity in Factor 3 and was therefore moved to Factor 3. Factor 2 was named “Contemplation”. The resulting Factor 2 had factor loadings ranging from 0.24 to 1.04.
After moving item#17 to Factor 3, that factor contained 6 items with a loading range of 0.28 to 0.93. All items in Factor 3 were related to readiness to serve in the role of SDM, and the factor was thus named “Readiness”.
The resultant survey consists of 17-items with three factors (‘domains’) (see Appendix 3 for final survey): 1) Serving as SDM (7 items), 2) Contemplation (4 items), and 3) Readiness (6 items).
Phase 5, Evaluation of Internal Consistency
The Cronbach’s alpha for factors 1, 2 and 3 were 0.91, 0.91 and 0.90 which is generally considered an indication of excellent internal consistency. In no cases did the Cronbach’s alpha significantly increase when an item was removed.
DISCUSSION
It is increasingly recognized that ACP is a complex process involving multiple stakeholders in addition to patients themselves, such as family, friends, and clinicians. While much attention has been paid to the study of how ACP interventions engage patients in the ACP process, less work has focused on engaging the SDMs in ACP, despite their equally important role.[27] This may be due, in part, to a lack of validated measures that assess how interventions impact SDMs.
This study resulted in a questionnaire that measures the extent to which SDMs have engaged in the ACP process. To do so, we adapted a well-validated patient-centered survey that is grounded in behavior change theories and related constructs relevant to ACP (knowledge, contemplation, self-efficacy, and readiness). The result was a 47 item adapted questionnaire that was then shortened into a short, 17 item questionnaire. This questionnaire could be useful for researchers seeking to measures engagement in the ACP process by SDMs, but also may provide utility by allowing comparisons between engagement of the patients (using the original survey) with engagement of their SDMs. That said, relevant ACP behaviors for a patient may be slightly different than for a surrogate. For this reason, we did not anticipate that all items of the original 55-item survey would map onto the adapted SDM survey. Further, shortened versions of the original patient-oriented survey (4, 9, 15, and 34-items) have been published and are being validated.[17]
While our preliminary exploratory factor analysis is limited by small sample size, it provides useful information it resulted in identification of three domains within the final 17-item questionnaire (The ACP-17-SDM; Appendix 3). Domain 1, ‘Serving as SDM’, includes 7 items that assess knowledge (3-items), contemplation (1 item), self-efficacy (3-items). Domain 2, ‘Contemplation’, includes 4-items that assess contemplation (how much surrogates have thought about end-of-life issues).
The third domain, ‘Readiness’, includes 6 items that assess readiness and measure participants’ stage of readiness to engage in various ACP behaviors. Responses to the readiness question are based on the trans-theoretical model’s five stages of change, allowing the respondent’s ‘stage of change’ for each of the 6 ACP behaviors to be assessed in addition to the total domain score. Given the limited precision of the factor loadings due to the small sample size, we recommend each factor be reported as a domain score computed as the unweighted average of the items in that domain. Larger studies are needed to verify the validity of these domains.
Still, the domain scores may be helpful for interventionalists examining mechanisms by which an intervention engages participants in ACP. For example, an intervention intended to start conversations would be expected to increase participants’ contemplation scores with lesser effect on ‘readiness’ scores (which assesses subsequent actions). Ideal ACP interventions will increase participants’ overall engagement in the ACP process and effect all of these domains equally, yet the complexity of the ACP process likely makes a single intervention insufficient, and consideration should be given to how ACP interventions effect each of these domains.
A limitation of this study is the small, homogenous, convenience sample which could limit the stability and generalizability of the results. Further, using convenience sampling may result in selection bias related to literacy or other factors. Second, we did not collect data on the patients’ medical conditions. Third, we have not yet assessed the tool’s responsiveness to intervention.[17] Fourth, some items had fairly low loadings on the factors they were assigned. Even so, this study introduces a brief, 17-item questionnaire that assesses SDM engagement in ACP and is derived from a well-validated patient-oriented survey. Additional studies with larger sample size and varied demographics, literacy and cultures are needed to further validate and possibly shorten the questionnaire to mirror work in the patient-oriented version of survey[17] and to assess its’ responsiveness to intervention.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the Pennsylvania State University Survey Research Center for assistance with participant recruitment and data collection, Jean Reading for assistance with protocol/IRB development and data entry, and the research team of Drs. Michael Green and Benjamin Levi for reviewing early versions of the survey adaptation.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Appendix
Appendix 1.
Adaptation of the 55-item Patient-Oriented ACP Engagement Survey
| Item | Original Question (Patient Oriented) | Adapted Question (Surrogate Decision Maker oriented) | Group Decision After Phase 1 review |
|---|---|---|---|
| 1 | How well informed are you about who can be a medical decision maker? | Unchanged | Continued testing |
| 2 | How well informed are you about what makes someone a good medical decision maker? | Unchanged | Continued testing |
| 3 | How well informed are you about the types of decisions that a medical decision maker may have to make for you in the future? | How well informed are you about the types of decisions that you may have to make for your loved one in the future? | Continued testing |
| 4 | How much have you thought about who your medical decision maker should be? | How much have you thought about your role as your loved one’s medical decision-maker? | Continued testing |
| 5 | How much have you thought about asking someone to be your medical decision maker? | How much have you thought about the possibility of being asked to make medical decisions for your loved one? | Excluded due to a lack of face validity |
| 6 | How much have you thought about Talking with your doctors about who you want your medical decision maker to be? | How much have you thought about being part of a discussion with your loved one’s DOCTORS about your role as a medical decision-maker for your loved one? | Continued testing |
| 7 | How much have you thought about Talking with your OTHER family and friends about who you want your medical decision maker to be? | How much have you thought about being part of a discussion with your loved one’s OTHER family and friends about your role as your loved one’s medical decision-maker? | Continued testing |
| 8 | How confident are you that today you could Ask someone to be your medical decision maker? | As of today, how confident are you that you could serve as your loved one’s medical decision maker? | Continued testing |
| 9 | How confident are you that today you could Talk with your doctors about who you want your medical decision maker to be? | As of today, how confident are you that you could be part of a discussion with your loved one’s DOCTORS about your role as your loved one’s medical decision maker? | Continued testing |
| 10 | How confident are you that today you could Talk with your OTHER family and friends about who you want your medical decision maker to be? | As of today, how confident are you that you could be part of a discussion with your loved one’s OTHER FAMILY and FRIENDS about your role as your loved one’s medical decision maker? | Continued testing |
| 11 | How ready are you to formally ask someone to be your medical decision maker | How ready are you to formally discuss with your loved one your role as their medical decision maker? | Continued testing |
| 12 | How ready are you to talk with your DOCTOR about who you want your medical decision maker to be? | How ready are you to be part of a discussion with your loved one’s DOCTOR about your role as your loved one’s medical decision-maker? | Continued testing |
| 13 | How ready are you to talk to your OTHER FAMILY and FRIENDS about who you want your medical decision maker to be? | How ready are you to be part of a discussion with your loved one’s OTHER FAMILY and FRIENDS about your role as your loved one’s medical decision maker? | Continued testing |
| 14 | How ready are you to SIGN OFFICIAL PAPERS naming a person or group of people to make medical decisions for you? | How ready are you to be named a medical decision maker in OFFICIAL PAPERS that are signed by your loved one? | Continued testing |
| 15 | How much have you thought about Whether or not certain health situations would make your life not worth living? | How much have you thought about whether or not your loved one has considered certain health situations that would make his/her life not worth living? | Excluded due to a lack of face validity |
| 16 | How much have you thought about Talking with your DECISION MAKER about whether or not certain health situations would make your life not worth living? | How much have you thought about talking with your loved one about whether or not there are certain health situations that would make your loved one’s life not worth living? | Continued testing |
| 17 | How much have you thought about Talking with your DOCTORS about whether or not certain health situations would make your life not worth living? | How much have you thought about being part of a discussion with your loved one’s DOCTORS about whether or not there are certain health situations that would make your loved one’s life not worth living? | Continued testing |
| 18 | How much have you thought about Talking with your OTHER family and friends about whether or not certain health situations would make your loved one’s life not worth living? | How much have you thought about being part of a discussion with your loved ones OTHER FAMILY and FRIENDS about whether or not there are certain health situations that would make your loved one’s life not worth living? | Continued testing |
| 19 | How confident are you that today you could Talk with your decision maker about whether or not certain health situations would make your life not worth living? | As of today, how confident are you that you could talk with your loved one about whether or not certain health situations would their life not worth living? | Continued testing |
| 20 | How confident are you that today you could Talk with your doctors about whether or not certain health situations would make your life not worth living? | As of today, how confident are you that you could be part of a discussion with your loved one’s DOCTORS about whether or not there are certain health situations that would make your loved one’s life not worth living? | Continued testing |
| 21 | How confident are you that today you could Talk with your OTHER family and friends about whether or not certain health situations would make your life not worth living? | As of today, how confident are you that you could talk with your loved one’s OTHER FAMILY and FRIENDS about whether or not there are certain health situations that would make your loved one’s life not worth living? | Continued testing |
| 22 | How ready are you to decide whether or not certain health situations would make your life not worth living? | How ready are you to help your loved one decide whether or not certain health situations would make their life not worth living? | Excluded due to a lack of face validity |
| 23 | How ready are you to talk to your DECISION MAKER about whether or not certain health situations would make your life not worth living? | How ready are you to talk with your loved one about whether or not there are certain health situations that would make their life not worth living? | Continued testing |
| 24 | How ready are you to talk to your DOCTOR about whether or not certain health situations would make your life not worth living? | How ready are you to be part of a discussion with your loved one’s DOCTOR about whether or not there are certain health situations that would make your loved one’s life not worth living? | Continued testing |
| 25 | How ready are you to talk to your OTHER FAMILY and FRIENDS about whether or not certain health situations would make your life not worth living? | How ready are you to be part of a discussion with your loved one’s OTHER FAMILY and FRIENDS about whether or not there are certain health situations that would make your loved one’s life not worth living? | Continued testing |
| 26 | How ready are you to SIGN OFFICIAL PAPERS putting your wishes in writing about whether or not certain health situations would make your loved one’s life not worth living? | How ready are you help your loved one SIGN OFFICIAL PAPERS putting his/her wishes in writing about whether or not there are certain health situations that would make your loved one’s life not worth living? | Continued testing |
| 27 | How much have you thought about the care you would want if you were very sick or near the end of life? | How much have you thought about The care your loved one would want if he/she were very sick or near the end of life? | Excluded due to a lack of face validity |
| 28 | How much have you thought about talking with your decision maker about the care you would want if you were very sick or near the end of life? | How much have you thought about talking with your loved one about the care he/she would want if they were very sick or near the end of life? | Continued testing |
| 29 | How much have you thought about talking with your doctors about the care you would want if you were very sick or near the end of life? | How much have you thought about being part of a discussion with your loved one’s DOCTORS about the care your loved one would want if he/she was very sick or near the end of life? | Continued testing |
| 30 | How much have you thought about talking with your OTHER family and friends about the care you would want if you were very sick or near the end of life? | How much have you thought about being part of a discussion with your loved one’s OTHER FAMILY and FRIENDS about the care your loved one would want if he/she were very sick or near the end of life? | Continued testing |
| 31 | How confident are you that today you could Talk with your decision maker about the care you would want if you were very sick or near the end of life? | As of today, how confident are you that you could talk with your loved one about the care he/she would want if he/she were very sick or near the end of life? | Continued testing |
| 32 | How confident are you that today you could Talk with your doctors about the care you would want if you were very sick or near the end of life? | As of today, how confident are you that you could be part of a discussion with your loved one’s doctors about the care your loved one would want if he/she were very sick or near the end of life? | Continued testing |
| 33 | How confident are you that today you could Talk with your OTHER family and friends about the care you would want if you were very sick or near the end of life? | As of today, how confident are you that you could be part of a discussion with your loved one’s OTHER FAMILY and FRIENDS about the care your loved one would want if he/she were very sick or near the end of life? | Continued testing |
| 34 | How ready are you to decide on the medical care you would want if you were very sick or near the end of life? | How ready are you to help your loved one decide on the medical care he/she would want if he/she were very sick or near the end of life? | Excluded due to a lack of face validity |
| 35 | How ready are you to talk to your DECISION MAKER about the kind of medical care you would want if you were very sick or near the end of life? | How ready are you to talk to your loved one about the kind of medical care he/she would want if they were very sick or near the end of life? | Continued testing |
| 36 | How ready are you to talk to your DOCTOR about the kind of medical care you would want if you were very sick or near the end of life? | How ready are you to be part of a discussion with your loved one’s DOCTOR about the kind of medical care your loved one would want if he/she were very sick or near the end of life? | Continued testing |
| 37 | How ready are you to talk to your OTHER FAMILY and FRIENDS about the kind of medical care you would want if you were very sick or near the end of life? | How ready are you to be part of a discussion with your loved one’s OTHER FAMILY and FRIENDS about the kind of medical care he/she would want if he/she were very sick or near the end of life? | Continued testing |
| 38 | How ready are you to SIGN OFFICIAL PAPERS putting your wishes in writing about the kind of medical care you would want if you were very sick or near the end of life? | How ready are you to help your loved one SIGN OFFICIAL PAPERS putting his/her wishes in writing about the kind of medical care he/she would want if he/she very sick or near the end of life? | Continued testing |
| 39 | How well informed are you about what it means to give a medical decision maker flexibility to make future decisions? | Unchanged | Excluded due to a lack of face validity |
| 40 | How well informed are you about the different amounts of flexibility a person can give their medical decision maker? | Unchanged | Continued testing |
| 41 | How much have you thought about The amount of flexibility you would want to give your medical decision maker? | How much have you thought about the amount of flexibility you would have as your loved one’s medical decision maker | Continued testing |
| 42 | How much have you thought about Talking with your decision maker about how much flexibility you want to give a medical decision maker? | How much have you thought about talking with your loved one about the amount of flexibility he/she would want to give you as a medical decision maker? | Continued testing |
| 43 | How much have you thought about Talking with your DOCTOR about how much flexibility you want to give your decision maker? | How much have you thought about being part of a discussion with your loved one’s DOCTOR about the amount of flexibility you would have as the medical decision maker? | Continued testing |
| 44 | How much have you thought about Talking with OTHER friends and family about how much flexibility you want to give your decision maker? | How much have you thought about being part of a discussion with your loved one’s OTHER family and friends about the amount of flexibility you would have as the medical decision maker? | Continued testing |
| 45 | How confident are you that today you could Talk with your DECISION MAKER about how much flexibility you want to give them as a medical decision maker? | As of today, how confident are you that you could talk with your loved one about how much flexibility he/she would want to give you as a medical decision maker? | Continued testing |
| 46 | How confident are you that today you could Talk with your DOCTOR about how much flexibility you want to give your medical decision maker? | As of today, how confident are you that you could be part of a discussion with your loved one’s DOCTOR about how much flexibility your loved one would want to give you as a medical decision maker? | Continued testing |
| 47 | How confident are you that today you could Talk with your OTHER family and friends about how much flexibility you want to give your medical decision maker? | As of today, how confident are you that you could be part of a discussion with your loved one’s OTHER family and friends about how much flexibility your loved one would want to give you as a medical decision maker? | Continued testing |
| 48 | How ready are you to talk to your DECISION MAKER about how much flexibility you want to give a medical decision maker? | How ready are you to talk to your loved one about how much flexibility he/she would want to give you as a medical decision maker? | Continued testing |
| 49 | How ready are you to talk to your DOCTOR about how much flexibility you want to give your decision maker? | How ready are you to be part of a discussion with your loved one’s DOCTOR about how much flexibility your loved one would want to give you as a medical decision maker? | Continued testing |
| 50 | How ready are you to talk to your OTHER FAMILY and FRIENDS about how much flexibility you want to give your medical decision maker? | How ready are you to be part of a discussion with your loved one’s OTHER FAMILY and FRIENDS about how much flexibility your loved one would want to give you as a medical decision maker? | Continued testing |
| 51 | How ready are you to SIGN OFFICIAL PAPERS putting your wishes in writing about how much flexibility to give your decision maker? | How ready are you to help your loved one SIGN OFFICIAL PAPERS about how much flexibility he/she would want to give you as a medical decision maker? | Continued testing |
| 52 | How well informed are you about The types of questions you can ask your doctor that will help you make a good medical decision? | How well informed are you about the types of questions you and your loved one can ask his/her doctor that will help them make a good medical decision for your loved one? | Excluded due to a lack of face validity |
| 53 | How much have you thought about Questions you will ask your doctor to help make good medical decisions? | How much have you thought about questions you will ask your loved one’s doctor to help make good medical decisions for your loved one? | Excluded due to a lack of face validity |
| 54 | How confident are you that today you could Ask the right questions of your doctor to help make good medical decisions? | How confident are you that today you could ask the right questions of your loved one’s doctors to help make good medical decisions for your loved one if your loved one was unable to speak for themselves? | Continued testing (underline words were accidentally deleted from survey) |
| 55 | How ready are you to ask your doctor questions to help you make a good medical decision? | How ready are you to ask your loved one’s doctor questions to help you make a good medical decision for your loved one if your loved one was unable to speak for themselves? | Continued testing |
Appendix 2.
Item by item correlation analysis
| Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 | |
| Item 1 | 1.000 | .734 | .672 | .514 | .448 | .516 | .516 | .379 | .476 | .500 |
| Item 2 | .734 | 1.000 | .715 | .563 | .576 | .495 | .549 | .526 | .582 | .454 |
| Item 3 | .672 | .715 | 1.000 | .450 | .441 | .517 | .559 | .516 | .532 | .464 |
| Item 4 | .514 | .563 | .450 | 1.000 | .744 | .589 | .431 | .367 | .454 | .539 |
| Item 5 | .448 | .576 | .441 | .744 | 1.000 | .735 | .429 | .440 | .508 | .459 |
| Item 6 | .516 | .495 | .517 | .589 | .735 | 1.000 | .494 | .469 | .544 | .519 |
| Item 7 | .516 | .549 | .559 | .431 | .429 | .494 | 1.000 | .892 | .738 | .516 |
| Item 8 | .379 | .526 | .516 | .367 | .440 | .469 | .892 | 1.000 | .792 | .454 |
| Item 9 | .476 | .582 | .532 | .454 | .508 | .544 | .738 | .792 | 1.000 | .472 |
| Item 10 | .500 | .454 | .464 | .539 | .459 | .519 | .516 | .454 | .472 | 1.000 |
| Item 11 | .386 | .423 | .462 | .590 | .608 | .602 | .504 | .494 | .537 | .742 |
| Item 12 | .395 | .368 | .423 | .493 | .537 | .767 | .543 | .531 | .636 | .667 |
| Item 13 | .570 | .487 | .523 | .568 | .573 | .597 | .467 | .394 | .519 | .713 |
| Item 14 | .475 | .478 | .445 | .487 | .513 | .611 | .611 | .544 | .566 | .581 |
| Item 15 | .420 | .433 | .318 | .525 | .677 | .669 | .499 | .481 | .473 | .436 |
| Item 16 | .398 | .460 | .421 | .469 | .615 | .768 | .509 | .499 | .558 | .445 |
| Item 17 | .408 | .477 | .214 | .306 | .453 | .362 | .442 | .401 | .446 | .292 |
| Item 18 | .451 | .466 | .374 | .481 | .640 | .621 | .610 | .527 | .540 | .401 |
| Item 19 | .390 | .469 | .322 | .386 | .565 | .562 | .539 | .508 | .628 | .327 |
| Item 20 | .504 | .536 | .493 | .420 | .446 | .644 | .543 | .492 | .516 | .559 |
| Item 21 | .535 | .626 | .562 | .468 | .562 | .654 | .514 | .429 | .499 | .487 |
| Item 22 | .473 | .541 | .434 | .432 | .562 | .733 | .492 | .461 | .518 | .475 |
| Item 23 | .552 | .478 | .445 | .512 | .553 | .610 | .450 | .406 | .512 | .612 |
| Item 24 | .539 | .600 | .580 | .510 | .630 | .714 | .550 | .472 | .463 | .567 |
| Item 25 | .453 | .481 | .481 | .500 | .669 | .697 | .537 | .462 | .502 | .353 |
| Item 26 | .507 | .525 | .404 | .468 | .642 | .797 | .477 | .467 | .565 | .415 |
| Item 27 | .502 | .583 | .434 | .421 | .531 | .507 | .497 | .492 | .526 | .414 |
| Item 28 | .558 | .578 | .590 | .595 | .770 | .794 | .665 | .638 | .727 | .554 |
| Item 29 | .421 | .525 | .473 | .461 | .687 | .719 | .593 | .627 | .803 | .481 |
| Item 30 | .462 | .560 | .505 | .507 | .507 | .695 | .510 | .494 | .531 | .671 |
| Item 31 | .505 | .523 | .519 | .556 | .595 | .772 | .493 | .422 | .471 | .591 |
| Item 32 | .487 | .557 | .489 | .472 | .598 | .756 | .441 | .448 | .516 | .530 |
| Item 33 | .518 | .473 | .515 | .425 | .520 | .582 | .390 | .348 | .465 | .566 |
| Item 34 | .540 | .491 | .539 | .451 | .548 | .584 | .520 | .436 | .388 | .351 |
| Item 35 | .364 | .432 | .411 | .512 | .660 | .688 | .517 | .400 | .505 | .336 |
| Item 36 | .410 | .464 | .410 | .469 | .646 | .658 | .582 | .468 | .542 | .503 |
| Item 37 | .384 | .364 | .376 | .415 | .597 | .611 | .530 | .432 | .462 | .470 |
| Item 38 | .356 | .450 | .336 | .406 | .626 | .700 | .518 | .475 | .517 | .467 |
| Item 39 | .451 | .522 | .357 | .239 | .393 | .399 | .443 | .403 | .393 | .431 |
| Item 40 | .451 | .508 | .495 | .427 | .613 | .601 | .636 | .522 | .575 | .411 |
| Item 41 | .419 | .488 | .446 | .320 | .548 | .565 | .595 | .484 | .647 | .347 |
| Item 42 | .549 | .542 | .599 | .554 | .617 | .668 | .518 | .443 | .487 | .733 |
| Item 43 | .450 | .478 | .475 | .438 | .567 | .610 | .410 | .372 | .449 | .462 |
| Item 44 | .495 | .555 | .528 | .484 | .619 | .702 | .447 | .421 | .506 | .457 |
| Item 45 | .526 | .478 | .530 | .446 | .552 | .631 | .431 | .414 | .462 | .628 |
| Item 46 | .350 | .501 | .416 | .375 | .472 | .557 | .658 | .632 | .665 | .439 |
| Item 47 | .395 | .470 | .493 | .417 | .539 | .621 | .429 | .461 | .497 | .447 |
| Item 11 | Item 12 | Item 13 | Item 14 | Item 15 | Item 16 | Item 17 | Item 18 | Item 19 | Item 20 | |
| Item 1 | .386 | .395 | .570 | .475 | .420 | .398 | .408 | .451 | .390 | .504 |
| Item 2 | .423 | .368 | .487 | .478 | .433 | .460 | .477 | .466 | .469 | .536 |
| Item 3 | .462 | .423 | .523 | .445 | .318 | .421 | .214 | .374 | .322 | .493 |
| Item 4 | .590 | .493 | .568 | .487 | .525 | .469 | .306 | .481 | .386 | .420 |
| Item 5 | .608 | .537 | .573 | .513 | .677 | .615 | .453 | .640 | .565 | .446 |
| Item 6 | .602 | .767 | .597 | .611 | .669 | .768 | .362 | .621 | .562 | .644 |
| Item 7 | .504 | .543 | .467 | .611 | .499 | .509 | .442 | .610 | .539 | .543 |
| Item 8 | .494 | .531 | .394 | .544 | .481 | .499 | .401 | .527 | .508 | .492 |
| Item 9 | .537 | .636 | .519 | .566 | .473 | .558 | .446 | .540 | .628 | .516 |
| Item 10 | .742 | .667 | .713 | .581 | .436 | .445 | .292 | .401 | .327 | .559 |
| Item 11 | 1.000 | .770 | .666 | .575 | .531 | .462 | .132 | .358 | .299 | .486 |
| Item 12 | .770 | 1.000 | .617 | .595 | .572 | .671 | .149 | .414 | .450 | .516 |
| Item 13 | .666 | .617 | 1.000 | .539 | .521 | .518 | .309 | .520 | .430 | .612 |
| Item 14 | .575 | .595 | .539 | 1.000 | .746 | .702 | .530 | .719 | .636 | .744 |
| Item 15 | .531 | .572 | .521 | .746 | 1.000 | .806 | .467 | .788 | .634 | .671 |
| Item 16 | .462 | .671 | .518 | .702 | .806 | 1.000 | .488 | .688 | .693 | .689 |
| Item 17 | .132 | .149 | .309 | .530 | .467 | .488 | 1.000 | .683 | .669 | .579 |
| Item 18 | .358 | .414 | .520 | .719 | .788 | .688 | .683 | 1.000 | .874 | .727 |
| Item 19 | .299 | .450 | .430 | .636 | .634 | .693 | .669 | .874 | 1.000 | .664 |
| Item 20 | .486 | .516 | .612 | .744 | .671 | .689 | .579 | .727 | .664 | 1.000 |
| Item 21 | .591 | .517 | .577 | .665 | .643 | .623 | .433 | .669 | .637 | .792 |
| Item 22 | .551 | .699 | .464 | .688 | .740 | .813 | .415 | .668 | .695 | .781 |
| Item 23 | .549 | .521 | .896 | .526 | .643 | .598 | .428 | .661 | .578 | .722 |
| Item 24 | .489 | .489 | .499 | .678 | .654 | .705 | .622 | .635 | .515 | .743 |
| Item 25 | .482 | .507 | .467 | .574 | .722 | .767 | .508 | .608 | .544 | .591 |
| Item 26 | .434 | .668 | .484 | .563 | .753 | .865 | .388 | .640 | .654 | .578 |
| Item 27 | .289 | .326 | .370 | .523 | .420 | .517 | .848 | .559 | .522 | .551 |
| Item 28 | .607 | .699 | .638 | .691 | .724 | .730 | .472 | .776 | .712 | .609 |
| Item 29 | .543 | .724 | .570 | .618 | .559 | .738 | .487 | .643 | .779 | .569 |
| Item 30 | .590 | .620 | .616 | .669 | .565 | .668 | .498 | .554 | .494 | .884 |
| Item 31 | .688 | .726 | .531 | .508 | .662 | .682 | .250 | .500 | .442 | .638 |
| Item 32 | .621 | .764 | .506 | .558 | .625 | .781 | .318 | .519 | .571 | .659 |
| Item 33 | .524 | .484 | .798 | .356 | .524 | .494 | .301 | .477 | .401 | .646 |
| Item 34 | .387 | .389 | .405 | .235 | .364 | .458 | .409 | .445 | .386 | .460 |
| Item 35 | .422 | .486 | .427 | .435 | .593 | .686 | .391 | .590 | .510 | .526 |
| Item 36 | .528 | .576 | .444 | .535 | .557 | .651 | .516 | .535 | .482 | .596 |
| Item 37 | .543 | .618 | .422 | .411 | .548 | .593 | .279 | .431 | .420 | .483 |
| Item 38 | .508 | .644 | .423 | .519 | .664 | .744 | .316 | .542 | .524 | .523 |
| Item 39 | .257 | .234 | .305 | .375 | .316 | .350 | .746 | .478 | .383 | .522 |
| Item 40 | .412 | .440 | .487 | .420 | .537 | .555 | .549 | .748 | .663 | .601 |
| Item 41 | .360 | .487 | .462 | .420 | .493 | .595 | .530 | .665 | .692 | .526 |
| Item 42 | .747 | .674 | .747 | .579 | .550 | .499 | .321 | .453 | .311 | .636 |
| Item 43 | .547 | .559 | .534 | .330 | .548 | .502 | .271 | .403 | .303 | .458 |
| Item 44 | .513 | .597 | .526 | .398 | .551 | .632 | .315 | .443 | .416 | .531 |
| Item 45 | .585 | .528 | .760 | .494 | .617 | .552 | .298 | .572 | .443 | .697 |
| Item 46 | .455 | .455 | .424 | .532 | .587 | .617 | .410 | .670 | .575 | .579 |
| Item 47 | .605 | .588 | .438 | .353 | .536 | .491 | .231 | .361 | .299 | .508 |
| Item 20 | Item 21 | Item 22 | Item 23 | Item 24 | Item 25 | Item 26 | Item 27 | Item 28 | Item 29 | |
| Item 1 | .504 | .535 | .473 | .552 | .539 | .453 | .507 | .502 | .558 | .421 |
| Item 2 | .536 | .626 | .541 | .478 | .600 | .481 | .525 | .583 | .578 | .525 |
| Item 3 | .493 | .562 | .434 | .445 | .580 | .481 | .404 | .434 | .590 | .473 |
| Item 4 | .420 | .468 | .432 | .512 | .510 | .500 | .468 | .421 | .595 | .461 |
| Item 5 | .446 | .562 | .562 | .553 | .630 | .669 | .642 | .531 | .770 | .687 |
| Item 6 | .644 | .654 | .733 | .610 | .714 | .697 | .797 | .507 | .794 | .719 |
| Item 7 | .543 | .514 | .492 | .450 | .550 | .537 | .477 | .497 | .665 | .593 |
| Item 8 | .492 | .429 | .461 | .406 | .472 | .462 | .467 | .492 | .638 | .627 |
| Item 9 | .516 | .499 | .518 | .512 | .463 | .502 | .565 | .526 | .727 | .803 |
| Item 10 | .559 | .487 | .475 | .612 | .567 | .353 | .415 | .414 | .554 | .481 |
| Item 11 | .486 | .591 | .551 | .549 | .489 | .482 | .434 | .289 | .607 | .543 |
| Item 12 | .516 | .517 | .699 | .521 | .489 | .507 | .668 | .326 | .699 | .724 |
| Item 13 | .612 | .577 | .464 | .896 | .499 | .467 | .484 | .370 | .638 | .570 |
| Item 14 | .744 | .665 | .688 | .526 | .678 | .574 | .563 | .523 | .691 | .618 |
| Item 15 | .671 | .643 | .740 | .643 | .654 | .722 | .753 | .420 | .724 | .559 |
| Item 16 | .689 | .623 | .813 | .598 | .705 | .767 | .865 | .517 | .730 | .738 |
| Item 17 | .579 | .433 | .415 | .428 | .622 | .508 | .388 | .848 | .472 | .487 |
| Item 18 | .727 | .669 | .668 | .661 | .635 | .608 | .640 | .559 | .776 | .643 |
| Item 19 | .664 | .637 | .695 | .578 | .515 | .544 | .654 | .522 | .712 | .779 |
| Item 20 | 1.000 | .792 | .781 | .722 | .743 | .591 | .578 | .551 | .609 | .569 |
| Item 21 | .792 | 1.000 | .818 | .614 | .672 | .587 | .602 | .441 | .625 | .596 |
| Item 22 | .781 | .818 | 1.000 | .522 | .633 | .591 | .783 | .428 | .635 | .669 |
| Item 23 | .722 | .614 | .522 | 1.000 | .572 | .572 | .571 | .424 | .662 | .567 |
| Item 24 | .743 | .672 | .633 | .572 | 1.000 | .842 | .659 | .721 | .658 | .546 |
| Item 25 | .591 | .587 | .591 | .572 | .842 | 1.000 | .751 | .578 | .669 | .587 |
| Item 26 | .578 | .602 | .783 | .571 | .659 | .751 | 1.000 | .448 | .706 | .716 |
| Item 27 | .551 | .441 | .428 | .424 | .721 | .578 | .448 | 1.000 | .620 | .596 |
| Item 28 | .609 | .625 | .635 | .662 | .658 | .669 | .706 | .620 | 1.000 | .850 |
| Item 29 | .569 | .596 | .669 | .567 | .546 | .587 | .716 | .596 | .850 | 1.000 |
| Item 30 | .884 | .734 | .736 | .650 | .795 | .565 | .544 | .615 | .614 | .606 |
| Item 31 | .638 | .741 | .785 | .561 | .732 | .706 | .713 | .366 | .634 | .549 |
| Item 32 | .659 | .760 | .922 | .501 | .614 | .561 | .790 | .415 | .636 | .696 |
| Item 33 | .646 | .620 | .472 | .840 | .563 | .557 | .484 | .385 | .585 | .503 |
| Item 34 | .460 | .458 | .443 | .429 | .605 | .648 | .486 | .552 | .531 | .452 |
| Item 35 | .526 | .515 | .567 | .491 | .679 | .784 | .655 | .419 | .624 | .564 |
| Item 36 | .596 | .535 | .590 | .441 | .745 | .733 | .579 | .544 | .615 | .572 |
| Item 37 | .483 | .444 | .565 | .416 | .603 | .675 | .563 | .314 | .549 | .532 |
| Item 38 | .523 | .463 | .687 | .477 | .582 | .635 | .710 | .346 | .643 | .606 |
| Item 39 | .522 | .383 | .347 | .352 | .699 | .464 | .311 | .771 | .445 | .398 |
| Item 40 | .601 | .597 | .520 | .569 | .658 | .627 | .563 | .560 | .729 | .651 |
| Item 41 | .526 | .532 | .519 | .512 | .612 | .638 | .632 | .511 | .689 | .720 |
| Item 42 | .636 | .624 | .536 | .657 | .691 | .573 | .429 | .447 | .647 | .518 |
| Item 43 | .458 | .570 | .549 | .528 | .620 | .623 | .566 | .390 | .509 | .460 |
| Item 44 | .531 | .631 | .664 | .511 | .655 | .642 | .659 | .416 | .570 | .576 |
| Item 45 | .697 | .595 | .541 | .832 | .634 | .518 | .512 | .345 | .624 | .495 |
| Item 46 | .579 | .564 | .591 | .544 | .615 | .593 | .589 | .431 | .643 | .571 |
| Item 47 | .508 | .506 | .543 | .492 | .638 | .674 | .551 | .393 | .532 | .479 |
| Item 29 | Item 30 | Item 31 | Item 32 | Item 33 | Item 34 | Item 35 | Item 36 | Item 37 | Item 38 | Item 39 | |
| Item 1 | .421 | .462 | .505 | .487 | .518 | .540 | .364 | .410 | .384 | .356 | .451 |
| Item 2 | .525 | .560 | .523 | .557 | .473 | .491 | .432 | .464 | .364 | .450 | .522 |
| Item 3 | .473 | .505 | .519 | .489 | .515 | .539 | .411 | .410 | .376 | .336 | .357 |
| Item 4 | .461 | .507 | .556 | .472 | .425 | .451 | .512 | .469 | .415 | .406 | .239 |
| Item 5 | .687 | .507 | .595 | .598 | .520 | .548 | .660 | .646 | .597 | .626 | .393 |
| Item 6 | .719 | .695 | .772 | .756 | .582 | .584 | .688 | .658 | .611 | .700 | .399 |
| Item 7 | .593 | .510 | .493 | .441 | .390 | .520 | .517 | .582 | .530 | .518 | .443 |
| Item 8 | .627 | .494 | .422 | .448 | .348 | .436 | .400 | .468 | .432 | .475 | .403 |
| Item 9 | .803 | .531 | .471 | .516 | .465 | .388 | .505 | .542 | .462 | .517 | .393 |
| Item 10 | .481 | .671 | .591 | .530 | .566 | .351 | .336 | .503 | .470 | .467 | .431 |
| Item 11 | .543 | .590 | .688 | .621 | .524 | .387 | .422 | .528 | .543 | .508 | .257 |
| Item 12 | .724 | .620 | .726 | .764 | .484 | .389 | .486 | .576 | .618 | .644 | .234 |
| Item 13 | .570 | .616 | .531 | .506 | .798 | .405 | .427 | .444 | .422 | .423 | .305 |
| Item 14 | .618 | .669 | .508 | .558 | .356 | .235 | .435 | .535 | .411 | .519 | .375 |
| Item 15 | .559 | .565 | .662 | .625 | .524 | .364 | .593 | .557 | .548 | .664 | .316 |
| Item 16 | .738 | .668 | .682 | .781 | .494 | .458 | .686 | .651 | .593 | .744 | .350 |
| Item 17 | .487 | .498 | .250 | .318 | .301 | .409 | .391 | .516 | .279 | .316 | .746 |
| Item 18 | .643 | .554 | .500 | .519 | .477 | .445 | .590 | .535 | .431 | .542 | .478 |
| Item 19 | .779 | .494 | .442 | .571 | .401 | .386 | .510 | .482 | .420 | .524 | .383 |
| Item 20 | .569 | .884 | .638 | .659 | .646 | .460 | .526 | .596 | .483 | .523 | .522 |
| Item 21 | .596 | .734 | .741 | .760 | .620 | .458 | .515 | .535 | .444 | .463 | .383 |
| Item 22 | .669 | .736 | .785 | .922 | .472 | .443 | .567 | .590 | .565 | .687 | .347 |
| Item 23 | .567 | .650 | .561 | .501 | .840 | .429 | .491 | .441 | .416 | .477 | .352 |
| Item 24 | .546 | .795 | .732 | .614 | .563 | .605 | .679 | .745 | .603 | .582 | .699 |
| Item 25 | .587 | .565 | .706 | .561 | .557 | .648 | .784 | .733 | .675 | .635 | .464 |
| Item 26 | .716 | .544 | .713 | .790 | .484 | .486 | .655 | .579 | .563 | .710 | .311 |
| Item 27 | .596 | .615 | .366 | .415 | .385 | .552 | .419 | .544 | .314 | .346 | .771 |
| Item 28 | .850 | .614 | .634 | .636 | .585 | .531 | .624 | .615 | .549 | .643 | .445 |
| Item 29 | 1.000 | .606 | .549 | .696 | .503 | .452 | .564 | .572 | .532 | .606 | .398 |
| Item 30 | .606 | 1.000 | .740 | .731 | .645 | .486 | .552 | .652 | .548 | .555 | .590 |
| Item 31 | .549 | .740 | 1.000 | .838 | .642 | .563 | .672 | .668 | .689 | .653 | .415 |
| Item 32 | .696 | .731 | .838 | 1.000 | .505 | .460 | .537 | .584 | .589 | .676 | .332 |
| Item 33 | .503 | .645 | .642 | .505 | 1.000 | .499 | .531 | .473 | .484 | .415 | .376 |
| Item 34 | .452 | .486 | .563 | .460 | .499 | 1.000 | .639 | .682 | .647 | .512 | .621 |
| Item 35 | .564 | .552 | .672 | .537 | .531 | .639 | 1.000 | .843 | .792 | .735 | .418 |
| Item 36 | .572 | .652 | .668 | .584 | .473 | .682 | .843 | 1.000 | .859 | .798 | .613 |
| Item 37 | .532 | .548 | .689 | .589 | .484 | .647 | .792 | .859 | 1.000 | .787 | .415 |
| Item 38 | .606 | .555 | .653 | .676 | .415 | .512 | .735 | .798 | .787 | 1.000 | .350 |
| Item 39 | .398 | .590 | .415 | .332 | .376 | .621 | .418 | .613 | .415 | .350 | 1.000 |
| Item 40 | .651 | .574 | .584 | .499 | .583 | .686 | .701 | .685 | .635 | .552 | .675 |
| Item 41 | .720 | .488 | .566 | .510 | .529 | .560 | .681 | .671 | .617 | .556 | .635 |
| Item 42 | .518 | .749 | .758 | .600 | .782 | .506 | .557 | .656 | .649 | .526 | .504 |
| Item 43 | .460 | .563 | .736 | .622 | .635 | .586 | .577 | .602 | .706 | .551 | .475 |
| Item 44 | .576 | .642 | .800 | .735 | .648 | .594 | .688 | .673 | .689 | .641 | .471 |
| Item 45 | .495 | .705 | .645 | .566 | .811 | .483 | .504 | .535 | .555 | .577 | .442 |
| Item 46 | .571 | .602 | .575 | .534 | .474 | .473 | .648 | .530 | .492 | .581 | .454 |
| Item 47 | .479 | .604 | .761 | .614 | .618 | .573 | .593 | .598 | .708 | .553 | .466 |
| Item 40 | Item 41 | Item 42 | Item 43 | Item 44 | Item 45 | Item 46 | Item 47 | |
| Item 1 | .451 | .419 | .549 | .450 | .495 | .526 | .350 | .395 |
| Item 2 | .508 | .488 | .542 | .478 | .555 | .478 | .501 | .470 |
| Item 3 | .495 | .446 | .599 | .475 | .528 | .530 | .416 | .493 |
| Item 4 | .427 | .320 | .554 | .438 | .484 | .446 | .375 | .417 |
| Item 5 | .613 | .548 | .617 | .567 | .619 | .552 | .472 | .539 |
| Item 6 | .601 | .565 | .668 | .610 | .702 | .631 | .557 | .621 |
| Item 7 | .636 | .595 | .518 | .410 | .447 | .431 | .658 | .429 |
| Item 8 | .522 | .484 | .443 | .372 | .421 | .414 | .632 | .461 |
| Item 9 | .575 | .647 | .487 | .449 | .506 | .462 | .665 | .497 |
| Item 10 | .411 | .347 | .733 | .462 | .457 | .628 | .439 | .447 |
| Item 11 | .412 | .360 | .747 | .547 | .513 | .585 | .455 | .605 |
| Item 12 | .440 | .487 | .674 | .559 | .597 | .528 | .455 | .588 |
| Item 13 | .487 | .462 | .747 | .534 | .526 | .760 | .424 | .438 |
| Item 14 | .420 | .420 | .579 | .330 | .398 | .494 | .532 | .353 |
| Item 15 | .537 | .493 | .550 | .548 | .551 | .617 | .587 | .536 |
| Item 16 | .555 | .595 | .499 | .502 | .632 | .552 | .617 | .491 |
| Item 17 | .549 | .530 | .321 | .271 | .315 | .298 | .410 | .231 |
| Item 18 | .748 | .665 | .453 | .403 | .443 | .572 | .670 | .361 |
| Item 19 | .663 | .692 | .311 | .303 | .416 | .443 | .575 | .299 |
| Item 20 | .601 | .526 | .636 | .458 | .531 | .697 | .579 | .508 |
| Item 21 | .597 | .532 | .624 | .570 | .631 | .595 | .564 | .506 |
| Item 22 | .520 | .519 | .536 | .549 | .664 | .541 | .591 | .543 |
| Item 23 | .569 | .512 | .657 | .528 | .511 | .832 | .544 | .492 |
| Item 24 | .658 | .612 | .691 | .620 | .655 | .634 | .615 | .638 |
| Item 25 | .627 | .638 | .573 | .623 | .642 | .518 | .593 | .674 |
| Item 26 | .563 | .632 | .429 | .566 | .659 | .512 | .589 | .551 |
| Item 27 | .560 | .511 | .447 | .390 | .416 | .345 | .431 | .393 |
| Item 28 | .729 | .689 | .647 | .509 | .570 | .624 | .643 | .532 |
| Item 29 | .651 | .720 | .518 | .460 | .576 | .495 | .571 | .479 |
| Item 30 | .574 | .488 | .749 | .563 | .642 | .705 | .602 | .604 |
| Item 31 | .584 | .566 | .758 | .736 | .800 | .645 | .575 | .761 |
| Item 32 | .499 | .510 | .600 | .622 | .735 | .566 | .534 | .614 |
| Item 33 | .583 | .529 | .782 | .635 | .648 | .811 | .474 | .618 |
| Item 34 | .686 | .560 | .506 | .586 | .594 | .483 | .473 | .573 |
| Item 35 | .701 | .681 | .557 | .577 | .688 | .504 | .648 | .593 |
| Item 36 | .685 | .671 | .656 | .602 | .673 | .535 | .530 | .598 |
| Item 37 | .635 | .617 | .649 | .706 | .689 | .555 | .492 | .708 |
| Item 38 | .552 | .556 | .526 | .551 | .641 | .577 | .581 | .553 |
| Item 39 | .675 | .635 | .504 | .475 | .471 | .442 | .454 | .466 |
| Item 40 | 1.000 | .910 | .571 | .604 | .622 | .589 | .647 | .582 |
| Item 41 | .910 | 1.000 | .494 | .586 | .644 | .520 | .565 | .558 |
| Item 42 | .571 | .494 | 1.000 | .695 | .676 | .756 | .448 | .719 |
| Item 43 | .604 | .586 | .695 | 1.000 | .867 | .712 | .471 | .875 |
| Item 44 | .622 | .644 | .676 | .867 | 1.000 | .682 | .496 | .759 |
| Item 45 | .589 | .520 | .756 | .712 | .682 | 1.000 | .548 | .679 |
| Item 46 | .647 | .565 | .448 | .471 | .496 | .548 | 1.000 | .519 |
| Item 47 | .582 | .558 | .719 | .875 | .759 | .679 | .519 | 1.000 |
Appendix 3.
Final 17-item ACP Engagement Survey- Surrogate Decision-Maker
| Item | Theoretical Construct |
Domain (Factor) |
|---|---|---|
| 1. How well informed are you about who can be a medical decision maker? | Knowledge | Serving as surrogate decision-maker |
| 2. How well informed are you about what makes someone a good medical decision maker? | Knowledge | Serving as surrogate decision-maker |
| 3. How well informed are you about the types of decisions that you may have to make for your loved one in the future? | Knowledge | Serving as surrogate decision-maker |
| 4. How much have you thought about your role as your loved one’s medical decision-maker? | Contemplation | Serving as surrogate decision-maker |
| 5. As of today, how confident are you that you could serve as your loved one’s medical decision maker? | Self-efficacy | Serving as surrogate decision-maker |
| 6. As of today, how confident are you that you could talk with your loved one about the care he/she would want if he/she were very sick or near the end of life? | Self-efficacy | Serving as surrogate decision-maker |
| 7. As of today, how confident are you that you could be part of a discussion with your loved one’s DOCTOR about the care your loved one would want if he/she were very sick or near the end of life? | Self-efficacy | Serving as surrogate decision-maker |
| 8. How much have you thought about talking with your loved one about whether or not there are certain health situations that would make your loved one’s life not worth living? | Contemplation | Contemplation |
| 9. How much have you thought about being part of a discussion with your loved one’s DOCTORS about whether or not there are certain health situations that would make your loved one’s life not worth living? | Contemplation | Contemplation |
| 10. How much have you thought about talking with your loved one about the care he/she would want if they were very sick or near the end of life? | Contemplation | Contemplation |
| 11. How much have you thought about being part of a discussion with your loved one’s DOCTORS about the care he/she would want if they were very sick or near the end of life? | Contemplation | Contemplation |
| 12. How ready are you to formally discuss with your loved one your role as their medical decision maker? | Readiness | Readiness |
| 13. How ready are you to talk to your loved one about the kind of medical care he/she would want if they were very sick or near the end of life? | Readiness | Readiness |
| 14. How ready are you to talk to your loved one about whether or not there are certain health situations that would make your loved one’s life not worth living? | Readiness | Readiness |
| 15. How ready are you to be part of a discussion with your loved one’s DOCTOR about whether or not there are certain health situations that would make your loved one’s life not worth living? | Readiness | Readiness |
| 16. How ready are you to be part of a discussion with your loved one’s DOCTOR about the kind of medical care your loved one would want if he/she were very sick or near the end of life? | Readiness | Readiness |
| 17. How ready are you to ask your loved one’s DOCTOR questions to help you make a good medical decision for your loved one if your loved one was unable to speak for themselves? | Readiness | Readiness |
Footnotes
DISCLOSURES
No authors have any conflicts of interest to disclose.
REFERENCES
- 1.Sudore RL, Lum HD, You JJ, Hanson LC, Meier DE, Pantilat SZ et al. Defining Advance Care Planning for Adults: A Consensus Definition From a Multidisciplinary Delphi Panel. J Pain Symptom Manage. 2017;53(5):821–32 e1. doi: 10.1016/j.jpainsymman.2016.12.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ. 2010;340:1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kirchhoff KT, Hammes BJ, Kehl KA, Briggs LA, Brown RL. Effect of a disease-specific advance care planning intervention on end-of-life care. Journal of the American Geriatrics Society. 2012;60(5):946–50. doi: 10.1111/j.1532-5415.2012.03917.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Silveira MJ, Kim SYH, Langa KM. Advance directives and outcomes of surrogate decision making before death. The New England journal of medicine. 2010;362(13):1211–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Teno JM, Gozalo PL, Bynum JPW, Leland NE, Miller SC, Morden NE et al. Change in end-of-life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013;309(5):470–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Casarett D, Karlawish J, Morales K, Crowley R, Mirsch T, Asch DA. Improving the use of hospice services in nursing homes: a randomized controlled trial. JAMA. 2005;294(2):211–7. doi: 10.1001/jama.294.2.211. [DOI] [PubMed] [Google Scholar]
- 7.Wright AA, Keating NL, Ayanian JZ, Chrischilles EA, Kahn KL, Ritchie CS et al. Family Perspectives on Aggressive Cancer Care Near the End of Life. JAMA. 2016;315(3):284–92. doi: 10.1001/jama.2015.18604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morrison RS, Chichin E, Carter J, Burack O, Lantz M, Meier DE. The effect of a social work intervention to enhance advance care planning documentation in the nursing home. J Am Geriatr Soc. 2005;53(2):290–4. doi: 10.1111/j.1532-5415.2005.53116.x. [DOI] [PubMed] [Google Scholar]
- 9.Kramer BJ, Boelk AZ, Auer C. Family conflict at the end of life: Lessons learned in a model program for vulnerable older adults. Journal of palliative medicine. 2006;9(3):791–801. [DOI] [PubMed] [Google Scholar]
- 10.Kramer BJ, Kavanaugh M, Trentham-Dietz A, Walsh M, Yonker JA. Predictors of family conflict at the end of life: the experience of spouses and adult children of persons with lung cancer. Gerontologist. 2010;50(2):215–25. doi: 10.1093/geront/gnp121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rao JK, Anderson LA, Lin FC, Laux JP. Completion of advance directives among U.S. consumers. Am J Prev Med. 2014;46(1):65–70. doi: 10.1016/j.amepre.2013.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Resnick HE, Hickman S, Foster GL. Documentation of Advance Directives Among Home Health and Hospice Patients: United States, 2007. Am J Hosp Palliat Care. 2012;29(1):26–35. [DOI] [PubMed] [Google Scholar]
- 13.Greenberg MR, Weiner M, Greenberg GB. Risk-reducing legal documents: controlling personal health and financial resources. Risk Anal. 2009;29(11):1578–87. [DOI] [PubMed] [Google Scholar]
- 14.Howard M, Bernard C, Klein D, Tan A, Slaven M, Barwich D et al. Older patient engagement in advance care planning in Canadian primary care practices. Results of a multisite survey. 2018;64(5):371–7. [PMC free article] [PubMed] [Google Scholar]
- 15.Bravo G, Dubois M-F, Wagneur B. Assessing the effectiveness of interventions to promote advance directives among older adults: a systematic review and multi-level analysis. Soc Sci Med. 2008;67(7):1122–32. doi: 10.1016/j.socscimed.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 16.Tamayo-Velazquez MI, Simon-Lorda P, Villegas-Portero R, Higueras-Callejon C, Garcia-Gutierrez JF, Martinez-Pecino F et al. Interventions to promote the use of advance directives: an overview of systematic reviews. Patient Educ Couns. 2010;80(1):10–20. doi: 10.1016/j.pec.2009.09.027. [DOI] [PubMed] [Google Scholar]
- 17.Sudore RL, Heyland DK, Barnes DE, Howard M, Fassbender K, Robinson CA et al. Measuring Advance Care Planning: Optimizing the Advance Care Planning Engagement Survey. Journal of Pain and Symptom Management. doi: 10.1016/j.jpainsymman.2016.10.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sudore RL, Stewart AL, Knight SJ, McMahan RD, Feuz M, Miao Y et al. Development and validation of a questionnaire to detect behavior change in multiple advance care planning behaviors. PloS one. 2013;8(9):e72465. doi: 10.1371/journal.pone.0072465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sudore R, Le GM, McMahon R, Feuz M, Katen M, Barnes DE. The advance care planning PREPARE study among older Veterans with serious and chronic illness: study protocol for a randomized controlled trial. Trials. 2015;16:570. doi: 10.1186/s13063-015-1055-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Radhakrishnan K, Van Scoy LJ, Jillapalli R, Saxena S, Kim MT. Community-based game intervention to improve South Asian Indian Americans’ engagement with advanced care planning. Ethn Health. 2017:1–19. doi: 10.1080/13557858.2017.1357068. [DOI] [PubMed] [Google Scholar]
- 21.Van Scoy L, Reading J, Hopkins M, Smith B, Dillon J, Green MJ, Levi BH. Community Game Day: Using an end-of-life conversation game to encourage advance care planning. Journal of Pain and Symptom Management. 2017;In Press. [DOI] [PubMed] [Google Scholar]
- 22.Zapata C, Wistar E, Horton C, Lum H, Sudore R. Using A Video-Based Advance Care Planning (ACP) Website to Facilitate Group Visits for Diverse Older Adults in Primary Care Is Feasible And Improves ACP Engagement (TH307D). Journal of Pain and Symptom Management. 2017;53(2):318–9. [Google Scholar]
- 23.Howard M RC, McKenzie M, Fyles G, Sudore R, Andersen E, Arora N, Barwich D, Bernard C, Elston D, Heyland R, Klein D, McFee E, Mroz L, Slaven M, Tan A, Heyland DK. Effectiveness of an interactive website to engage patients in advance care planning in outpatient settings: a multicenter, prospective, before-after study. Annals of Family Medicine. Under Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iezzoni LI. Multiple chronic conditions and disabilities: implications for health services research and data demands. Health Serv Res. 2010;45(5 Pt 2):1523–40. doi: 10.1111/j.1475-6773.2010.01145.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wong A, Nyenhuis D, Black SE, Law LS, Lo ES, Kwan PW et al. Montreal cognitive assessment 5-minute protocol is a brief, valid, reliable, and feasible cognitive screen for telephone administration. Stroke; a journal of cerebral circulation. 2015;46(4):1059–64. doi: 10.1161/STR0KEAHA.114.007253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fabrigar LR, Wegener DT. Exploratory factor analysis. Oxford University Press; 2011. [Google Scholar]
- 27.Jimenez G, Tan WS, Virk AK, Low CK, Car J, Yan Ho AH. Overview of Systematic Reviews of Advance Care Planning: Summary of Evidence and Global Lessons. J Pain Symptom Manage. 2018. doi: 10.1016/j.jpainsymman.2018.05.016. [DOI] [PubMed] [Google Scholar]