Abstract
Background
Mobile phone use and exposure to radiofrequency electromagnetic fields (RF-EMF) from it have been associated with symptoms in some studies, but the studies have shortcomings and their findings are inconsistent. We conducted a prospective cohort study to assess the association between amount of mobile phone use at baseline and frequency of headache, tinnitus or hearing loss at 4-year follow-up.
Methods
The participants had mobile phone subscriptions with major mobile phone network operators in Sweden (n = 21 049) and Finland (n = 3120), gave consent for obtaining their mobile phone call data from operator records at baseline, and filled in both baseline and follow-up questionnaires on symptoms, potential confounders and further characteristics of their mobile phone use.
Results
The participants with the highest decile of recorded call-time (average call-time >276 min per week) at baseline showed a weak, suggestive increased frequency of weekly headaches at 4-year follow-up (adjusted odds ratio 1.13, 95% confidence interval 0.95–1.34). There was no obvious gradient of weekly headache with increasing call-time (P trend 0.06). The association of headache with call-time was stronger for the Universal Mobile Telecommunications System (UMTS) network than older Global System for Mobile Telecommunications (GSM) technology, despite the latter involving higher exposure to RF-EMF. Tinnitus and hearing loss showed no association with call-time.
Conclusions
People using mobile phones most extensively for making or receiving calls at baseline reported weekly headaches slightly more frequently at follow-up than other users, but this finding largely disappeared after adjustment for confounders and was not related to call-time in GSM with higher RF-EMF exposure. Tinnitus and hearing loss were not associated with amount of call-time.
Keywords: Cohort studies, cell phones, headache, tinnitus, hearing loss
Key Messages
Only limited research evidence exists about the possible association of long-term mobile phone use with headache and hearing symptoms, such as hearing loss and tinnitus.
In a prospective cohort study with data on call-time from network operators, we evaluated the relationship between amount of mobile phone use at baseline and occurrence of self-reported weekly headaches, tinnitus and hearing loss among those free of the symptom at baseline.
In unadjusted analysis, we found some indication of more common weekly headache in the participants in the top decile of mobile phone call-time, but, after adjustment for confounders, this was substantially attenuated.
No association was found between amount of call time and tinnitus or hearing loss.
Introduction
Health effects of radiofrequency electromagnetic fields (RF-EMF) from mobile phones have been studied for more than two decades, primarily motivated by a general concern that widely used novel technology could have adverse health effects, rather than any strong biophysically founded hypothesis. Although populations have been exposed to RF-EMF for decades, mainly from radio and TV broadcasting and industrial applications, the rapid uptake of mobile phone technology has increased RF-EMF exposure, particularly to the head. A wide range of health outcomes have been studied, such as different types of cancer (particularly intracranial tumours), neurodegenerative diseases, sleep disturbance, and other health-related symptoms. Several expert groups have reviewed the scientific evidence1–3 but have not found convincing evidence of adverse health effects at exposure levels encountered in the general population, although RF-EMF was classified as possibly carcinogenic to humans (class 2B) by the International Agency for Research on Cancer.
Studies with different designs have addressed potential effects of exposure to mobile phones on various symptoms. Provocation studies in controlled settings have focused on acute effects (i.e. immediate responses to the exposure), with outcomes including headache, wellbeing and physiological responses. Well-designed studies with double-blind exposure setup have not shown evidence of symptoms or physiological effects triggered by the RF-EMF exposure.4–8 The results of the short-term provocation studies do not, nevertheless, preclude the possibility of long-term effects on symptoms from repeated RF-EMF exposure to mobile phones.
Some cross-sectional population studies have reported increased prevalence of headaches, sleeping problems, concentration difficulties, or lower wellbeing with mobile phone exposure, but biases inherent in the cross-sectional design limit their interpretation.9,10 Cross-sectional studies cannot distinguish the time sequence of events, and hence reverse causation and nocebo effects (adverse effect due to negative expectations) are of major concern.
Few studies have addressed the occurrence of symptoms such as headache, tinnitus and other somatic complaints in relation to prospectively collected information on RF-EMF exposure.11,12 A Swiss study reported no association between mobile phone use and tinnitus or overall symptom score, but it had limited statistical power to assess the occurrence of outcomes among people free from the conditions at baseline, due to a relatively small sample size (n = 1122) and only 1 year of follow-up.11 A Dutch study found no association with sleep disturbances or other symptoms and focused on exposure from base stations rather than mobile phone use.12 In a large Danish cohort study of mobile phone subscribers, increased rates of hospitalizations for migraine and vertigo among subscribers were reported, but the study had no information on amount of mobile phone use and confounders were limited to age, sex and calendar period, due to the register-based approach.13 In addition, there is a growing field of research focusing on mobile phone use from a psychological or behavioural perspective, hypothesizing that excessive mobile phone use may be associated with psychosocial stress and addictive behaviour, and consequently various health problems and somatic and psychological symptoms.14–16
A large European collaborative prospective cohort study of mobile phone use was started in Sweden, Finland, Denmark, the UK and The Netherlands in 2007–2014 to provide improved scientific evidence on potential health hazards due to RF-EMF from mobile phone use.17 The rationale was to compile detailed mobile phone use data prospectively from operator databases, supplemented by self-reported information on usage behaviour, to overcome the uncertainty and bias in case-control studies due to retrospective assessment of mobile phone use, including recall bias.18,19 In addition, a prospective cohort study is less prone to selection bias and allows assessment of several health outcomes, chosen based on maximum exposure (to the head) in an exploratory manner in the absence of mechanistic hypotheses.
Here, we report the first findings from the Cohort Study of Mobile Phone Use and Health (COSMOS) on headache, tinnitus and hearing loss at follow-up, based on Swedish and Finnish data only, as these countries were the first to complete follow-up for specific health symptoms.
Methods
The study participants were recruited from the subscriber databases of mobile phone network operators in Sweden and Finland. Letters of invitation and questionnaires were mailed to random samples of mobile phone subscribers (in Finland, corporate subscriptions were excluded due to foreseen challenges in obtaining a valid consent for collection of traffic data, whereas in Sweden, all subscribers were eligible). We employed stratified sampling by age and amount of mobile phone use, and in Finland also by gender, with efforts to balance the usage distribution to increase statistical power. Detailed information about the cohort recruitment is reported elsewhere.17 The number of successfully recruited individuals who filled out the questionnaire and gave consent for access to operator data was 50 236 (20.4%) in Sweden and 12 163 in Finland (7.4%) (excluding participants aged 67 years or older). The baseline questionnaires were obtained in 2008–2009 in Sweden and 2009–2010 in Finland and covered mobile phone use history, phone numbers of currently used mobile phones, potential confounders, and health outcomes.
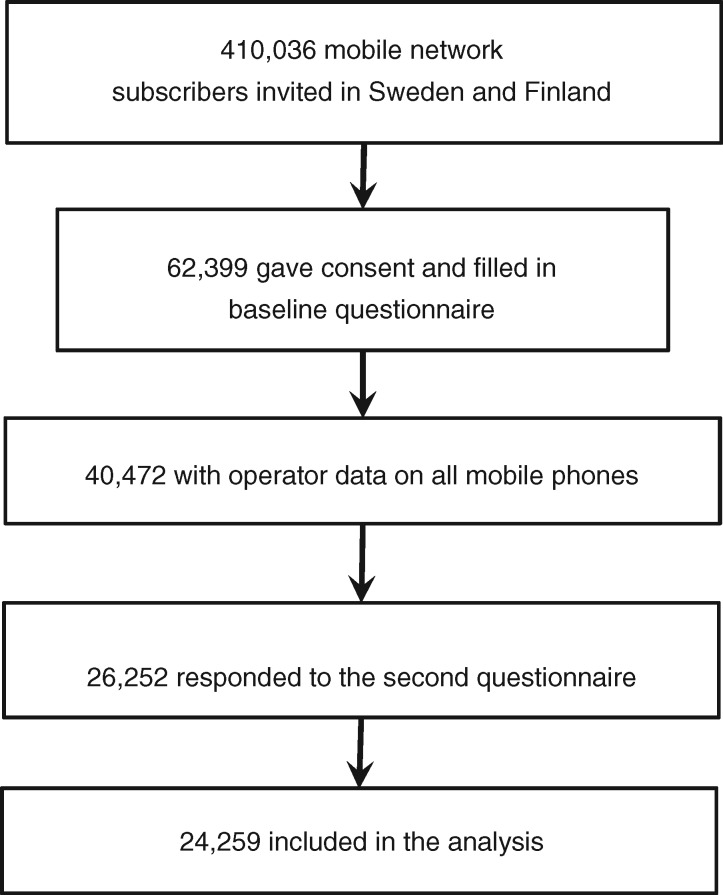
We obtained complete baseline data including operator data on mobile phones used at baseline (maximum of two, those using more than two were excluded) for 32 286 participants in Sweden (64%) and 8186 in Finland (67%) (Figure 1) . We sent a repeat questionnaire after a 4-year follow-up period (2013 in Sweden and 2014 in Finland) to collect information about health outcomes not available in health data registers. In the current analysis, we used only questionnaire data. The repeat questionnaire was completed by 22 487 (70%) of the eligible participants with complete baseline data in Sweden and 3765 (46%) in Finland.
Figure 1.
Flowchart of the COSMOS study data
Exposure assessment
Network operators provided data on duration of each call made and received over a period of ∼3 months at baseline for all consenting participants. We estimated cumulative call-time from data for all calls combined, and calculated average weekly call-time as the primary exposure measure.
Through the questionnaire, we collected information about previous history of mobile phone use prior to baseline, as well as details of mobile phone use habits, including use of hands-free devices, use of multiple mobile phones, and whether other people often used the mobile phone(s), for which operator data were obtained. Participants who reported that other people used their mobile phone ‘often’, as well as those with missing information about use of hands-free devices, were excluded from the analysis (1438 participants or 6.4% in Sweden and 430 participants or 11.4% in Finland).
The primary exposure indicator was the operator-recorded average call duration per week during the 3-month period at baseline. We subtracted an estimated proportion of call-time with hands-free devices from the recorded call-time based on self-report [with response options ‘hardly ever’ (68.5% of participants), ‘less than half of the time’ (13.1%), ‘about half of the time’ (5.7%), ‘more than half of the time’ (4.7%) and ‘always or nearly always’ (8.1%)]. The proportion of recorded call-time subtracted was zero, 5%, 10%, 25% and 50% for each hands-free use category, respectively, based on.20 In a sensitivity analysis, we used the recorded call-time without correction for hands-free devices to make sure the self-reported hands-free use did not unduly influence the findings.
We categorized the amount of call-time into the reference group defined as <50th percentile (<78 min per week on average), 50−74th percentile (78–175 min per week), 75−89th percentile (175–276 min per week) and the top decile (>276 min per week) at baseline. We also performed sensitivity analyses where exposure was categorized according to quartiles (<23, 23–78, 78–175 and >175 min per week).
We obtained information on network type based on the first base station, and conducted separate analyses for calls in GSM [Global System for Mobile Telecommunications, second generation (2 G) with 900 and 1800 MHz carrier frequencies] and UMTS [Universal Mobile Telecommunications System; third generation (3 G) at 900 and 2100 MHz]. The rationale was that any biological effects of RF-EMF should show stronger associations with 2 G than 3 G call-time, because GSM has substantially higher radiofrequency field strength (by approximately a factor of 150) than the third generation. The factor of 150 was based on the mean output power (mW) of phones for calls in UMTS (2100 MHz), GSM (1800 MHz) and GSM (900 MHz), estimated at 0.45, 44 and 90 mW, respectively.21 Using these estimates of output power, the relative contribution of UMTS versus GSM was calculated as UMTS2100/GSM900 + 1800 = 0.45/67 = 150. Given the uncertainty in these estimates, we repeated the analyses using a ratio of 50 and 200 to explore the influence of the choice of weighting factor.
Both network systems were used in parallel at the time of the study, so most cohort members would be using both in varying proportions depending on, for example, phone type, location and network characteristics, although 10 413 participants (42.9%) had no calls in a UMTS network. We used similar categorization (lowest 50% as reference, highest 10% as a separate group) for call-time in GSM and UMTS systems (for GSM, the cut-points were 32 100, and 206 min/week, and for UMTS, 36 105 and 185 min/week). Minutes in unknown networks (on average 15 min per week or 13% of total call-time) were imputed in accordance with call-time in specified systems (GSM vs UMTS). A sensitivity analysis was conducted excluding participants with >20% of call-time in an unspecified network (n = 4719).
Health outcomes
We used questionnaires to obtain self-reported information on headache, tinnitus and hearing loss. The main end-point for headache was self-reported headache at least once per week according to the follow-up questionnaire. To avoid potential reverse causation, we restricted all analyses of headache (weekly, daily and severe) at follow-up to participants who did not report weekly or more frequent headaches at baseline and included those with data on all covariates in the main analysis (n = 19 227 for Sweden and Finland combined, 122 had missing data on headache at follow-up). The response options for the headache frequency question were: almost daily; 5–6 days per week; 3–4 days per week; 1–2 days per week; 1–2 days per month; less often. In addition, we performed analyses of severe weekly headache and daily headaches. We used the Headache Impact Test (HIT-6), with a cut-off of 56 points to define severe headache.22
We assessed the presence of tinnitus by asking about persistent ringing, ‘buzzing’ or other sound in the ear(s). We restricted the analyses of tinnitus to individuals who did not report tinnitus at baseline (n = 20 024).
We defined hearing loss as a positive response to a question on use of a hearing aid (yes/no), or hearing much worse than among people of same age (yes/no) in the follow-up questionnaire among the participants who had reported no hearing loss at baseline (n = 19 852) 1321 participants had missing data on hearing loss at follow-up.
Statistical analysis
To evaluate the association between weekly mobile phone call-time and other characteristics, we used Mann−Whitney U and Kruskal−Wallis tests, as well as Spearman rho (rank correlation), due to non-normal distribution of call-time.
We used logistic regression to analyse the association between mobile phone use and dichotomous outcomes, defined as presence vs absence of headache, tinnitus or hearing loss at follow-up. We adjusted for, or stratified by, age, gender and country in all analyses. For headaches, we assessed potential confounders at baseline, including: self-reported daily painkiller use (yes/no), self-rated physical and mental health score from RAND Short Form Survey 12 (SF-12) v2 (continuous), self-reported diagnosis of depression (yes/no), sleep disturbance score from the Medical outcomes study sleep scale survey instrument (MOS-Sleep) questionnaire (continuous), education (basic, secondary and university), body mass index (based on self-reported height and weight, categorized as normal or underweight vs overweight or obese with a cut-off point 25 kg/m2), current smoking (yes/no), alcohol use (various beverages asked separately and total consumption used; cut-point for men 24 alcohol units per normal week and women 16 units), and hypertension diagnosed by a physician (yes/no). For tinnitus and hearing loss, we regarded smoking and education, as well as SF-12 physical and mental health scores, as potential confounders. In Finland, we also asked about history of exposure to loud noise at work (ever/never) and listening to loud music (at least weekly) and used those as potential confounders in country-specific analyses of tinnitus and hearing loss.
We used trend tests with the indicator for exposure category as a continuous variable. We assessed interactions between call-time and potential modifiers (age group, gender and country) on risk of each of the outcomes using a likelihood ratio test for significance of an interaction term added to the model with both main effects.
We performed a drop-out analysis to assess possible selection effects by comparing the amount of call-time and frequency of symptoms at entry among those who responded only to the baseline questionnaire with those completing both baseline and follow-up surveys.
Ethics committees reviewed the study protocol in Sweden (Regional Ethical Review Board in Stockholm 2007/1285–31/5, 2012/1608–32) and Finland (Pirkanmaa Hospital District, tracking numbers R04179 and R09105).
Results
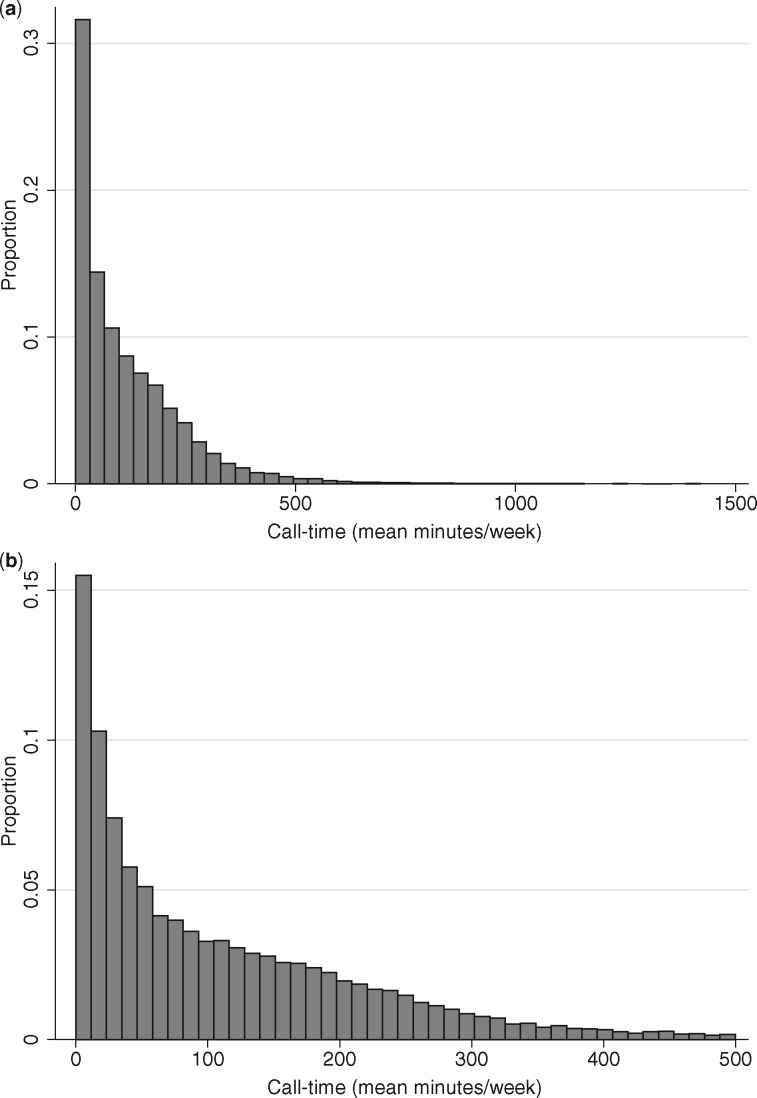
The amount of weekly call-time at baseline was highly skewed toward low values, with a long tail at the high end (Figure 2). The average weekly call-time was slightly higher among men than women, in younger age groups, and in Finnish rather than Swedish participants (Table 1).
Figure 2.
(a) Distribution of weekly call-time (min) at baseline. (b) Distribution of weekly call-time (min) at baseline among participants with <500 min/week
Table 1.
Characteristics of the participants by amount of mobile phone use at baseline (weekly minutes of call-time), Cohort Study of Mobile Phone Use and Health (COSMOS) in Sweden and Finland
| Average weekly call-time at baselinea |
|||||
|---|---|---|---|---|---|
| Lowest 50% | 51 − 75th percentile | 76 − 89th percentile | 90 − 100th percentile | Total | |
| Gender, n (%) | |||||
| Men | 5061 (47) | 2750 (26) | 1709 (16) | 1240 (12) | 10 760 |
| Women | 7066 (52) | 3302 (25) | 1854 (14) | 1187 (9) | 13 409 |
| Age group (years), n (%) | |||||
| 18 – 29 | 1839 (45) | 1030 (25) | 698 (17) | 510 (13) | 4077 |
| 30 – 39 | 2420 (53) | 1088 (24) | 596 (13) | 479 (10) | 4583 |
| 40 – 49 | 2636 (50) | 1319 (25) | 724 (14) | 544 (10) | 5223 |
| 50 – 59 | 2725 (46) | 1592 (27) | 1013 (17) | 641 (11) | 5971 |
| 60 – 66 | 2507 (58) | 1023 (24) | 532 (12) | 253 (6) | 4315 |
| Country, n (%) | |||||
| Finland | 1317 (42) | 1008 (32) | 473 (15) | 322 (10) | 3120 |
| Sweden | 10 810 (51) | 5044 (24) | 3090 (15) | 2105 (10) | 21 049 |
| Total | 12 127 (50) | 6052 (25) | 3563 (15) | 2427 (10) | 24 169 |
Excluding call-time with hands-free devices: 50th percentile 78 min, 75th 175 min, and 90th 275 min, group medians 23-122-217-359.
The amount of call-time (excluding hands-free use) in both systems was comparable for GSM and UMTS (means 74 min/week for GSM users and 72 min/week for UMTS users), with little correlation (Spearman rho –0.14). The distribution of call-time by age, gender and country for both GSM and UMTS resembled that of overall call-time.
Of the 19 230 participants free of weekly headache at baseline and with complete information on confounders, 1635 (8.5%) reported such headache at follow-up [of whom 130 (8.0%) reported daily headache]. Overall, weekly headache at follow-up was equally common in Sweden and Finland (8.6% versus 8.1%). Of the weekly headaches at follow-up, 544 (33.3%) were rated as severe.
In total, 1572 participants reported tinnitus at follow-up (7.9% of the 20 025 individuals free of tinnitus at entry and with information on the confounders). Tinnitus was equally common in both ears (only left 242, only right 291, both ears 884 cases, laterality missing 155). The Finnish participants reported tinnitus more commonly than the Swedish (13.4% vs 7.2%).
Hearing loss was uncommon at follow-up: 270 individuals reported it (1.4% of the 19 857 participants free of hearing loss at baseline). The Swedish participants reported hearing loss more often than the Finnish participants (1.4% vs 0.8%).
The 10% of the participants with the largest amount of weekly call-time at baseline had an increased odds ratio (OR) of weekly headache at follow-up of 1.21 [95% confidence interval (CI) 1.02–1.43] compared with the reference group with the lowest 50% weekly call-time, when adjusted only for age, gender and country; after further adjustment for SF-12 physical and mental health score, daily use of painkillers, sleep disturbance score, as well as prior diagnosis of depression at baseline, the OR was reduced to 1.13 (95% CI 0.95–1.34), with P-value for trend 0.06 across the usage categories (Table 2). Additional adjustment for education, current smoking, hypertension, overweight/obesity, or amount of alcohol use did not materially affect the OR estimate (Supplementary Table 1, available as Supplementary data at IJE online).
Table 2.
Odds ratio (OR, with 95% CI) for headache, tinnitus and hearing loss at follow-up by amount of mobile phone use at baseline (weekly minutes of call-time) among those free of the symptom at baseline, Cohort Study of Mobile Phone Use and Health (COSMOS). Number of participants with the outcome indicated in square brackets
| Health outcome | No. of participants | Lowest 50% | 50 − 74th percentile | 75 − 89th percentile | 90 − 100th percentile | P trend |
|---|---|---|---|---|---|---|
| Weekly headachea | 19 230 [1635] | 1 (reference) [785] | 1.01 (0.88 − 1.14) [394] | 1.14 (0.98 − 1.32) [268] | 1.13 (0.95 − 1.34) [188] | 0.06 |
| Severe weekly headachea,b | 19 230 [544] | 1 (reference) [263] | 1.00 (0.80 − 1.24) [131] | 1.00 (0.77 − 1.29) [82] | 1.15 (0.87 − 1.52) [68] | 0.47 |
| Daily headachea | 19 230 [130] | 1 (reference) [56] | 1.39 (0.91 − 2.11) [38] | 1.21 (0.73 − 2.01) [21] | 1.23 (0.69 − 2.19) [15] | 0.35 |
| Tinnitusc | 20 205 [1572] | 1 (reference) [746] | 1.08 (0.95 − 1.22) [411] | 1.19 (1.03 − 1.38) [262] | 1.04 (0.87 − 1.25) [153] | 0.12 |
| Hearing lossc | 19 857 [270] | 1 (reference) [153] | 0.97 (0.72 − 1.31) [66] | 0.75 (0.50 − 1.11) [30] | 0.89 (0.56 − 1.41) [21] | 0.25 |
Adjusted for country, gender, age group, depression, daily painkiller use, as well as SF-12 mental and physical health score at baseline; excluding participants with weekly headache at baseline.
Severe headache defined as HIT6 score >56.
Adjusted for country, gender, and age group.
For severe weekly headache, the adjusted OR for the highest call-time decile was 1.15 (95% CI 0.87–1.52, P trend 0.47, Table 2). Daily headache showed an adjusted OR 1.23 (95% CI 0.69–2.19) for the highest call-time decile, with no apparent increase across the usage categories (P trend 0.35).
Tinnitus was not more frequent in the highest decile of mobile phone use (OR 1.03, 95% CI 0.86–1.24 for the highest decile with adjustment for age, gender and country, Table 2) and it showed no strong gradient by amount of mobile phone use (P trend 0.14, Table 2). Adjustment for other covariates did not materially alter the results (Supplementary Table 1, available as Supplementary data at IJE online). Additional data on self-reported exposure to loud noise at work or during leisure time was available from Finland, but adjustment for loud noise did not affect the results (not shown).
In the analysis of hearing loss, we found no association with the amount of mobile phone use (OR = 0.89, 95% CI 0.56–1.41 for the highest decile with adjustment for age, gender and country, Table 2), with no gradient by call time (P trend 0.25). Additional adjustment for education, smoking, SF12 mental and physical health scores did not substantially affect the estimates for those with the largest amount of call-time (Supplementary Table 1, available as Supplementary data at IJE online). In the Finnish data, adjustment for loud noise did not materially alter the findings for mobile phone use (not shown).
In the analysis of call-time by network (GSM vs UMTS), weekly headache showed point estimates above unity for the two highest call-time categories in UMTS (adjusted OR for the highest decile 1.16, 95% CI 0.93–1.46, P trend 0.14), similar to the pattern observed for overall call-time, but there was no even suggestive association with weekly call-time in GSM (adjusted OR for the highest decile 1.06, 95% CI 0.89–1.26, P trend 0.99) (Table 3). The results by network type remained largely unchanged when limited to severe headache or daily headache (Supplementary Table 2, available as Supplementary data at IJE online). When call-time in both GSM and UMTS was simultaneously included in the model, UMTS still dominated and showed stronger association with headache (Supplementary Table 2, available as Supplementary data at IJE online). Excluding the participants without any calls in UMTS or those with missing network data for >20% of the call-time did not materially affect the results (Supplementary Table 2, available as Supplementary data at IJE online). When we divided the call-time with UMTS by 150 to approximate the difference in output power between the two network technologies, we observed no association with weighted call-time (adjusted OR for the highest decile 1.02, 95% CI 0.85–1.23, P trend 0.98).
Table 3.
Odds ratio (OR, with 95% CI) for weekly headache at follow-up (adjusted for country, gender, age group, depression, daily painkiller use, as well as SF-12 mental and physical health score at baseline) by amount of mobile phone use at baseline (weekly minutes of call-time) in GSM (2 G) and UMTS (3 G) systems at baseline among those free of weekly headache at baseline, Cohort Study of Mobile Phone Use and Health (COSMOS). Number of participants with weekly headache at follow-up shown in square brackets
| Amount of mobile phone use (call-time in percentiles) at baseline by network type | |||
|---|---|---|---|
| GSM (2G) network | UMTS (3G) network | Calls with UMTS call-time divided by 150 | |
| No. of participants | 19 005 [1617] | 10 896 [958] | 17 150 [1466] |
| Lowest 50% | 1 (reference) [809] | 1 (reference) [476] | 1 (reference) |
| 50 − 74th percentile | 0.96 (0.85 − 1.10) [389] | 0.90 (0.76 − 1.07) [216] | 0.99 (0.86 − 1.13) [354] |
| 75 − 89th percentile | 0.93 (0.80 − 1.09) [235] | 1.13 (0.93 − 1.37) [159] | 0.98 (0.83 − 1.15) [221] |
| 90 − 100th percentile | 1.06 (0.89 − 1.26) [184] | 1.16 (0.93 − 1.46) [107] | 1.02 (0.85 − 1.23) [160] |
| P trend | 0.99 | 0.14 | 0.98 |
In a sensitivity analysis, where we categorized the amount of weekly call-time into quartiles, we found no substantially increased ORs of weekly headache or trends with increasing call-time (OR for the highest quartile 1.11, 95% CI 0.96–1.28, P trend 0.14, Table 4). We also observed similar findings for daily headaches (OR for the highest quartile 1.30, 95% CI 0.78–2.17, p trend 0.21) and severe headaches (OR for the highest quartile 1.09, 95% CI 0.85–1.40, p trend 0.55).
Table 4.
Odds ratio (with 95% CI) for weekly headache at follow-up by amount of mobile phone use at baseline (weekly minutes of call-time), adjusted for depression, pain, sleep disorders, as well as SF-12 score for mental and physical health at baseline and mutually for gender/age/country, Cohort Study of Mobile Phone Use and Health (COSMOS). Number of participants with the outcome indicated in square brackets
| Subgroup | Amount of mobile phone use at baseline (call-time in percentiles)a |
|||||
|---|---|---|---|---|---|---|
| Lowest 50% | 50 − 74th percentile | 75 − 89th percentile | 90 − 100th percentile | P interaction | ||
| Gender | ||||||
| Men | 1 (reference) [245] | 1.07 (0.86 − 1.33) [142] | 1.25 (0.98 − 1.59) [106] | 1.04 (0.78 − 1.37) [68] | Gendera call-time 0.46 | |
| Women | 1 (reference) [540] | 0.96 (0.82 − 1.13) [252] | 1.06 (0.88 − 1.28) [162] | 1.19 (0.96 − 1.48) [120] | ||
| Age group (years) | ||||||
| 18 − 29 | 1 (reference) [162] | 0.96 (0.73 − 1.27) [91] | 1.16 (0.85 − 1.57) [72] | 1.11 (0.78 − 1.56) [52] | Age groupa call-time 0.15 | |
| 30 − 39 | 1 (reference) [203] | 1.16 (0.89 − 1.50) [100] | 0.83 (0.58 − 1.18) [45] | 1.12 (0.79 − 1.58) [48] | ||
| 40 − 49 | 1 (reference) [160] | 1.26 (0.96 − 1.66) [97] | 1.55 (1.13 − 2.13) [64] | 1.08 (0.73 − 1.61) [34] | ||
| 50 − 59 | 1 (reference) [175] | 0.78 (0.59 − 1.04) [79] | 0.95 (0.70 − 1.29) [61] | 1.13 (0.80 − 1.62) [44] | ||
| 60 − 67 | 1 (reference) [85] | 0.80 (0.51 − 1.26) [27] | 1.53 (0.96 − 2.43) [26] | 1.20 (0.60 − 2.38) [10] | ||
| Country | ||||||
| Sweden | 1 (reference) [702] | 1.03 (0.89 − 1.18) [336] | 1.13 (0.96 − 1.32) [232] | 1.08 (0.90 − 1.30) [158] | Countrya call-time 0.47 | |
| Finland | 1 (reference) [83] | 0.89 (0.62 − 1.28) [58] | 1.19 (0.78 − 1.83) [36] | 1.41 (0.89 − 2.24) [30] | ||
| Other exposure indices | ||||||
| Mobile phone use including use with hands-free devices | Trend test | |||||
| All participants | 1 (reference) [789] | 0.98 (0.86 − 1.11) [385] | 1.15 (1.00 − 1.34) [277] | 1.12 (0.95 − 1.34) [184] | 0.06 | |
| Call-time divided into quartiles | ||||||
| Q1 (1 − 22 min/week) | Q2 (22 − 77 min/week) | Q3 (77 − 175 min/week) | Q4 (175 − 1420 min/week) | |||
| All participants | 1 (reference) [396] | 0.96 (0.82 − 1.11) [389] | 0.98 (0.85 − 1.14) [394] | 1.11 (0.96 − 1.28) [456] | 0.14 | |
Quantiles defined based on the entire study population and applied with the same cut-off values in each subgroup.
An analysis of weekly headache in relation to weekly call-time, including calls with hands-free devices, showed similar results to the main analysis (Table 4); the correlation of the two measures was strong (rho = 0.99), as typically only approximately 6% of the call-time in the analysis was with hands-free devices. Assigning alternative weights of 50 or 200 instead of 150 to GSM for approximating the relative difference in power output compared with UMTS did not affect the findings (not shown).
Secondary analyses that evaluated the risk of weekly headache in subgroups by age, gender and country did not indicate any significant effect modification (Table 4). To assess whether an association with weekly headaches might be found only in long-term mobile phone users, we carried out analyses separately for those starting mobile phone use before and after 1998 (median first year of use); the results were similar for both groups. Exclusion of the 886 (4.5%) participants who worried about health risks of mobile phone use also did not alter the findings (not shown). An alternative analysis with headache frequency (at least 3 days per week, 1–2 days per week, 1–2 days per month, <1 per month, less) as the outcome using ordinal logistic regression showed no increasing gradient by call-time (results not shown).
A dropout analysis did not reveal any obvious difference in amount of mobile phone use or symptom prevalence at baseline between those included in and those ineligible for the analysis (due to incomplete mobile phone data or missing second questionnaire data) (Supplementary Table 3, available as Supplementary data at IJE online). The latter group did have a slightly larger proportion of users in the highest decile of call-time.
Discussion
In this large prospective cohort study of mobile phone users in Sweden and Finland using mobile phone operator records to estimate average weekly call-time, we found little indication of an association between increasing call-time at baseline and increased occurrence of headache at the follow-up survey four years later—except for a suggestive increase in the occurrence of weekly headache among participants in the highest decile of weekly call-time (odds ratio was 1.13, 95% CI 0.95–1.34), with no clear trend with increasing call-time (trend P = 0.06). The findings for weekly severe headaches and daily headaches were comparable with any weekly headaches. Estimates adjusted for several potential confounders at baseline (including age, gender, sleep disturbance, depression, health status, and daily painkiller use) were lower than unadjusted results. There was no association between weekly call-time at baseline and tinnitus or hearing loss 4 years later among those free of these conditions at baseline.
The limited evidence for an association between call-time and weekly headaches is further weakened by the fact that call-time on the UMTS network (3 G) showed a similar pattern to that observed for overall usage, with imprecise point estimates slightly above unity for the two highest call-time categories, whereas the call-time in the older GSM network (2 G) did not show any association. This speaks against an effect of RF-EMF, as the field strength of the RF-EMF emitted by mobile phones when using GSM is higher than in UMTS by a factor of approximately 150. The pattern of mobile phone use is likely different for the 3G (UMTS, notably providing an Internet connection) than the older 2G (GSM) phones, and this behavioural aspect may be more likely than RF-EMF to explain this finding. Also, the finding that the call-time with hands-free devices showed similar results to an analysis excluding hands-free use argues against a biological effect of the RF-EMF emitted by the phone, although hands-free devices were used on average only 5–10% of the call-time (and the amount of call-time with and without hands-free devices was highly correlated, rho = 0.99).
Adjustment for several potential confounders including age, gender, country, overweight/obesity, depression, sleep disorders and health status at baseline weakened the association with headache, and residual confounding may have inflated the observed estimates. Several other postulated risk factors for headaches (education, smoking, hypertension, and amount of alcohol use) did not confound the observation, as adjustment did not affect the results. People who use a mobile phone more extensively may differ from others in terms of lifestyle, e.g. have a busier and more stressful life situation, or problematic or addictive mobile phone use.15,23 Psychological features associated with amount of use include stress, anxiety and depression.24,25 Stress and high workload have been reported as risk factors for headache.26,27
Strengths and weaknesses
This is the first large cohort study to investigate mobile phone use and headaches, with objective, prospectively collected exposure information. The findings are based on follow-up over 4 years among individuals who were free of the symptoms at baseline. A key strength of our study is the use of objectively recorded data on mobile phone call-time, obtained from network operator databases at entry, prior to assessment of outcome.
Changes over time in the amount of mobile phone use are likely. However, this would not materially affect our results unless alterations in usage are dissimilar across the categories, so that the between-group differences are affected. The consistency of the amount of call-time was, however, reasonably high (observed agreement 58%, i.e. more than half remained in the same usage category, kappa 0.5), when comparing baseline data and follow-up 4 years later. Also, the relevance of the baseline usage depends on the latency (i.e. how quickly changes in exposure could affect headache and other symptoms) and on how long-lasting those potential effects are.
The participants included in the analysis were not necessarily representative of all mobile phone users. The low participation among those contacted is, however, unlikely to affect the internal comparisons within the cohort, based on contrasting symptom occurrence in groups with different amounts of mobile phone use. As those groups were formed through a similar selection process, their comparability is likely to be high and selection bias in such analysis would not be a major threat to validity. In Finland, the participants had to own their subscriptions to be able to give consent for retrieving mobile phone data from the operators. This resulted in exclusion of people with employer-owned subscriptions from the Finnish but not the Swedish cohort. Also, we chose to exclude participants with uncertain estimates of use (i.e. those with phones not fully covered by the operator data) and those lending their phones for a substantial proportion of the time to other people. We do not believe these exclusions would affect the validity of the internal comparisons, the basis of our results. A dropout analysis comparing all participants with those who could not be included in the analysis due to missing or incomplete data (operator data on mobile phone use or follow-up questionnaire) did not show any major difference in mobile phone use or symptoms at entry, suggesting lack of major selection bias.
The symptoms were self-reported, with a validated questionnaire instrument for headache severity. However, the outcomes were subjective complaints and their precise assessment is challenging, which was evident in, for example, major difference in prevalence of tinnitus between the two countries. Symptoms such as headache often fluctuate over time, and our questionnaires covered only two time periods around baseline and the follow-up assessment. It is possible that these assessments do not properly capture the symptoms occurring between these time points. However, less fluctuation can be assumed for hearing loss and tinnitus, which are more chronic in nature. Self-reported hearing loss is, nevertheless, not a highly sensitive indicator of minor hearing impairment and might miss a subtle effect.
Even though reporting of the symptoms relies on recall, differential reporting by amount of mobile phone use should be less likely than in a case-control study, since the assessment of mobile phone use was objective, conducted at baseline from the operator databases, while symptoms were reported in the follow-up survey 4 years later.
We used weekly headaches as the main outcome but were not able to determine the type of headache that was increased in frequency. The overall pattern of headache presentation, with a female:male ratio around two for weekly, daily and severe headache, and decreasing headache prevalence with age are consistent with results from population-based studies.28,29
Exposure assessment
We collected exposure information at entry to the study, typically 3 months before or after consent. We had no data on the intensity of the RF-EMF, such as the specific absorption rate (SAR), or even power level used, but network type (GSM vs UMTS) is a major predictor of those characteristics,30 and we were able to use the network type where the call was first connected as a proxy for exposure intensity, in combination with call-time. Also, to better focus on RF-EMF exposure to the head, we excluded mobile phone usage with hands-free devices (self-reported proportion of call-time at baseline) from the main analyses.
To what extent mobile phone call-time reflects RF-EMF exposure to the head is a matter of ongoing research. While there appeared to be a reasonable correlation between call-time and RF-EMF exposure with technologies and usage patterns in the early 2000s,31–33 this is believed to be weaker with lower exposure levels using modern mobile phone technology and increasing use of wireless technology in other applications.34 In addition, network provider data may not be error-free, as data extraction and linkage are complicated. However, exposure misclassification from such sources is likely to be non-differential.
Consistency with other studies
Few prospective studies have addressed the relationship between mobile phone use and headache. A Swiss cohort study with 1-year follow-up of 1124 participants found a non-significant increase in the headache severity (HIT-6 score) in relation to the highest 10% of call-time in operator data, but no association with self-reported call-time.11 It found no association between call-time and tinnitus. In that study, the average call-time was only 31 min per week, compared with 95 min per week in our study. A recent Swiss study of 439 adolescents followed up for 1 year reported a weak positive association between mobile phone call time and new-onset headache.35 The study did not evaluate tinnitus or hearing loss but reported associations between several symptoms and amount of phone usage, concluding that the likely culprit was not the RF-EMF but other aspects of extensive use of media and communication technology. In a Danish study, children with any mobile phone use at age 7 years were also more likely to have headache-related symptoms.36 Amount of phone use was relatively low, as only 1% of the participants had used their phone for ≥1 h per week. The cross-sectional nature of the study limited the conclusions that could be drawn. Similarly, the Danish study indicated an association of borderline significance between maternal mobile phone use during pregnancy and hearing loss in children at age 7 years, but the authors were cautious about drawing inference due to potential biases.37 A large Danish cohort study reported 10–20% higher rates of hospitalizations and outpatient visits for migraine among mobile phone subscribers, especially those with a recent subscription.13 This result was difficult to interpret and may reflect reverse causation, i.e. people with migraine being more likely to use a mobile phone. This limitation was overcome in our study by prospective follow-up of participants free of headache at baseline.
Conclusions
In conclusion, we found a small increase in weekly headache at 4-year follow-up among those in the highest decile of amount of call-time but free of weekly headache at baseline, but it largely disappeared after adjustment for confounders. There was no clear gradient in occurrence of weekly headache with amount of call-time. Any association between call-time and weekly headaches was limited to call-time in the third-generation UMTS network and was not found for the older GSM system characterized by higher RF-EMF exposure levels. This suggests that other factors related to the amount of mobile phone use (e.g. lifestyle, when and how the phone is used) may explain the weak association, rather than an effect of RF-EMF. We observed no association in our prospective study with occurrence of tinnitus or hearing loss.
Funding
The Finnish cohort was supported by funding from the National Technology Agency (TEKES), with contributions to the research program from Nokia, mobile network providers TeliaSonera and Elisa; Pirkanmaa Hospital District competitive research funding (grant no. VTR 9T003); Yrjö Jahnsson Foundation (grant no. 5692); Kone Foundation, and an unrestricted grant from Mobile Manufacturers’ Forum (with Pirkanmaa Hospital District as a firewall) with a contract guaranteeing the complete scientific independence of the researchers to analyse, interpret and report the results with no influence for the funding sources.
The Swedish part of COSMOS was supported by the Swedish Research Council (50096102); AFA Insurance (T-26: 04); the Swedish Research Council for Health, Working Life and Welfare (2010–0082, 2014–0889); the Swedish Radiation Safety Authority (SSM2015-2408); and VINNOVA (P31735-1). VINNOVA received funds for this purpose from TeliaSonera AB, Ericsson AB and Telenor Sverige AB, to cover part of the data collection (ended 2012). The provision of funds to the COSMOS study investigators via VINNOVA was governed by agreements that guarantees COSMOS’ complete scientific independence. TeliaSonera, Telenor, 3, and Tele2 made it possible for their subscribers to participate with traffic data.
The UK part of COSMOS was supported for an initial 5-year period by the Mobile Telecommunications and Health Research (MTHR), an independent programme of research into mobile phones and health jointly supported by the UK Department of Health and the mobile telecommunications industry (project reference number 091/0006) and, subsequently, funded by the UK Department of Health & Social Care via its Policy Research Programme (project reference number PR-ST-0713–00003); as well as by the National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Health Impact of Environmental Hazards at King’s College London in partnership with Public Health England (PHE) and Imperial College London (HPRU-2012–10141). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR, the Department of Health & Social Care or Public Health England. P.E. is Director of the MRC-PHE Centre for Environment and Health supported by the Medical Research Council and Public Health England (MR/L01341X/1), and the UK MEDical BIOinformatics partnership (UK MED-BIO) supported by the Medical Research Council (MR/L01632X/1). P.E. acknowledges support from the NIHR Imperial Biomedical Research Centre. P.E. is a UK Dementia Research Institute (DRI) Professor, UK DRI at Imperial College London. The UK DRI is funded by the Medical Research Council, Alzheimer’s Society and Alzheimer’s Research UK.
The Dutch part of the COSMOS study was supported by The Netherlands Organization for Health Research (ZonMW) within the programme Electromagnetic Fields and Health Research, under grant numbers 85200001, 85500003 and 85800001.
All financial support for the submitted work is described in the acknowledgments; there are no financial relationships with any organizations that might have an interest in the submitted work in the previous three years, nor any other relationships or activities that could appear to have influenced the submitted work. The funders and non-scientific collaborators (commercial entities i.e. network operators) had no role in planning, conducting or reporting the study, had no access to the data and have not seen the manuscript being submitted (but it will be provided for them once the paper has been accepted for publication).
Supplementary Material
Acknowledgements
We thank all participants who joined the COSMOS cohort study. We thank mobile phone network operators in Finland and Sweden for allowing invitation of their subscribers and/or provision of operator traffic data; as well as Dr Markus Färkkilä, MD and Dr Mikko Kallela, MD, Department of Neurology, Helsinki University Hospital for expert advice on classification of headaches. We also thank the members of the Scientific Advisory Board of the COSMOS study: Prof. Heidi Danker-Hopfe, Prof. Hazel Inskip and Prof. Martin Röösli. Where the authors are identified as personnel of the International Agency for Research on Cancer/World Health Organization, the authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policies or views of the International Agency for Research on Cancer/World Health Organization.
Conflict of interest: M.F. is vice chairman of the International Commission on Non-Ionizing Radiation Protection, an independent body setting guidelines for non-ionizing radiation protection. She has served as advisor to a number of national and international public advisory and research steering groups concerning the potential health effects of exposure to non-ionizing radiation, for example the World Health Organization. H.K. is the chair of the Committee on Electromagnetic Fields of the Health Council of The Netherlands. All other authors have declared no conflict of interest.
Contributor Information
COSMOS Study Group:
Prof. Heidi Danker-Hopfe, Prof. Hazel Inskip, and Prof. Martin Röösli
References
- 1.AGNIR 2012. Advisory Group on Non-Ionising Radiation. Health Effects of Radiofrequency Electromagnetic Fields http://webarchive.nationalarchives.gov.uk/20140629102627/http://www.hpa.org.uk/webw/HPAweb&HPAwebStandard/HPAweb_C/1317133826368
- 2. Non-Ionizing Radiation, Part 2. Radiofrequency Electromagnetic Fields. IARC Monograph 102. Lyon: International Agency for Research on Cancer, 2013. [Google Scholar]
- 3.SCENIHR. Scientific Committee on Emerging and Newly Identified Health Risks. Potential Health Effects of Exposure to Electromagnetic Fields. European Commission, 2015. http://ec.europa.eu/health/scientific_committees/emerging/docs/scenihr_o_041.pdf
- 4. Oftedal G, Straume A, Johnsson A, Stovner LJ.. Mobile phone headache: a double-blind sham-controlled provocation study. Cephalalgia 2007;27:447–55. [DOI] [PubMed] [Google Scholar]
- 5. Eltiti S, Wallace D, Ridgewell A.. Does short-term exposure to mobile phone base station signals increase symptoms in individuals who report sensitivity to electromagnetic fields? Environ Health Perspect 2007;115:1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cinel C, Russo R, Boldini A, Fox E.. Exposure to mobile phone electromagnetic fields and subjective symptoms. J Psychosom Res 2008;2008:65:453–60. [DOI] [PubMed] [Google Scholar]
- 7. Rubin GJ, Hillert L, Nieto-Hernandez R, van Rongen E, Oftedal G.. Do people with idiopathic environmental intolerance attributed to electromagnetic fields display physiological effects when exposed to electromagnetic fields? A systematic review of provocation studies. Bioelectromagnetics 2011;32:593–609. [DOI] [PubMed] [Google Scholar]
- 8. van Moorselaar I, Slottje P, Heller P. et al. Effects of personalized exposure on self-rated electromagnetic hypersensitivity and sensibility—a double-blind randomized controlled trial. Environ Int 2017;99:255–62. [DOI] [PubMed] [Google Scholar]
- 9. Thomas S, Kühnlein A, Heinrich S. et al. Personal exposure to mobile phone frequencies and well-being in adults. Bioelectromagnetics 2008;29:463–70. [DOI] [PubMed] [Google Scholar]
- 10. Heinrich S, Thomas S, Heumann C, von Kries R, Radon K.. Association between exposure to radiofrequency electromagnetic fields assessed by dosimetry and acute symptoms in children and adolescents. Environ Health 2010;9:75.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Frei P, Mohler E, Braun-Fahrländer C, Fröhlich J, Neubauer G, Röösli M.. Cohort study on the effects of everyday life radiofrequency electromagnetic field exposure on non-specific symptoms and tinnitus. Environ Int 2012;38:29–36. [DOI] [PubMed] [Google Scholar]
- 12. Martens AL, Slottje P, Timmermans DRM. et al. Modeled and perceived exposure to radiofrequency electromagnetic fields from mobile phone base stations and the development of symptoms over time in a general population cohort. Am J Epidemiol 2017;186:210–19. [DOI] [PubMed] [Google Scholar]
- 13. Schüz P, Waldemar G, Olsen JH, Johansen C.. Risks for central nervous system diseases among mobile phone subscribers. PLoS One 2009;4:e4389.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Thomee S, Harenstam A, Hagberg M.. Mobile phone use and stress, sleep disturbances, and symptoms of depression among young adults—a prospective cohort study. BMC Public Health 2011;11:6. doi: 10.1186/1471-2458-11-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Roser K, Schoeni A, Foerster M, Röösli M.. Problematic mobile phone use of Swiss adolescents: Is it linked with mental health or behaviour? Int J Public Health 2016;61:307–15. [DOI] [PubMed] [Google Scholar]
- 16. Jun S. The reciprocal longitudinal relationships between mobile phone addiction and depressive symptoms among Korean adolescents. Comput Human Behav 2016;58:179–86. [Google Scholar]
- 17. Schüz J, Elliott P, Auvinen A. et al. An international prospective cohort study of mobile phone users. Cancer Epidemiol 2011;35:37–43. [DOI] [PubMed] [Google Scholar]
- 18. Vrijheid M, Armstrong BK, Bedárd D. et al. Recall bias in the assessment of exposure to mobile phones. J Expo Sci Environ Epidemiol 2009;19:369–81. [DOI] [PubMed] [Google Scholar]
- 19. Aydin D, Feychting M, Schüz J. et al. Impact of random and systematic recall errors and selection bias in case-control studies on mobile phone use and brain tumors in adolescents (CEFALO study). Bioelectromagnetics 2011;32:396–407. [DOI] [PubMed] [Google Scholar]
- 20. Goedhart G, Kromhout H, Wiart J, Vermeulen R.. Validating self-reported mobile phone use in adults using a newly developed smartphone application. Occup Environ Med 2015;72:812–18. [DOI] [PubMed] [Google Scholar]
- 21. Persson T, Törnevik C, Larsson LE, Lovén J.. Output power distributions of terminals in a 3G mobile communication network. Bioelectromagnetics 2012;33:320–25. [DOI] [PubMed] [Google Scholar]
- 22. Kosinski M, Bayliss MS, Bjorner JB. et al. A six-item short-form survey for measuring headache impact: the HIT-6. Qual Life Res 2003;12:963–74. [DOI] [PubMed] [Google Scholar]
- 23. Gutiérrez JD, de Fonseca FR, Rubio G.. Cell-phone addiction—a review. Front Psychiatry 2016;7:175.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vahedi Z, Saiphoo A.. The association between smartphone use, stress and anxiety: a meta-analytic view. Stress Health 2018;34:347–58. [DOI] [PubMed] [Google Scholar]
- 25. Elhai JD, Dvorak RD, Levine JC, Hall BJ.. Problematic smartphone use: a conceptual overview and systematic review of relations with anxiety and depression psychopathology. J Affect Disord 2017;207:251–59. [DOI] [PubMed] [Google Scholar]
- 26. Lyngberg AC, Rasmussen BK, Jorgensen T, Jensen R.. Incidence of primary headache. Am J Epidemiol 2005;161:1066–73. [DOI] [PubMed] [Google Scholar]
- 27. Schramm SH, Moebus S, Lehmann N. et al. The association between stress and headache: a longitudinal population-based study. Cephalalgia 2015;156:1747–54. [DOI] [PubMed] [Google Scholar]
- 28. Straube A, Aicher B, Förderreuther S. et al. Period prevalence of self-reported headache in the general population of Germany from 1995-2005 and 2009. J Headache Pain 2013;14:11.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Smitherman TA, Burch R, Sheikh H, Loder E.. The prevalence, impact and treatment of migraine and severe headaches in the United States. Headache 2013;53:427–36. [DOI] [PubMed] [Google Scholar]
- 30. Lauer O, Frei P, Gosselin MC, Joseph W, Röösli M, Fröhlich J.. Combining near and far-field exposure for an organ-specific and whole-body RF-EMF proxy for epidemiological research. Bioelectromagnetics 2013;34:366–74. [DOI] [PubMed] [Google Scholar]
- 31. Frei P, Mohler E, Bürgi A. et al. A prediction model for personal radiofrequency electromagnetic field exposure. Sci Total Environ 2009;408:102–108. [DOI] [PubMed] [Google Scholar]
- 32. Frei P, Mohler E, Neubauer G. et al. Temporal and spatial variability of personal exposure to radiofrequency electromagnetic fields. Environ Res 2009;109:779–85. [DOI] [PubMed] [Google Scholar]
- 33. Vrijheid M, Mann S, Vecchia P. et al. Determinants of mobile phone output power in a multinational study: implications for exposure assessment. Occup Environ Health 2009;66:664–71. [DOI] [PubMed] [Google Scholar]
- 34. Urbinello D, Joseph W, Verloock L, Martens L, Röösli M.. Temporal trends of radiofrequency electromagnetic field exposure in everyday environments across European cities. Environ Res 2014;134:134–42. [DOI] [PubMed] [Google Scholar]
- 35. Schoeni A, Roser K, Röösli M.. Symptoms and the use wireless communication devices. Environ Res 2017;154:275–83. [DOI] [PubMed] [Google Scholar]
- 36. Sudan M, Kheifets L, Arah O, Olsen J, Zeltzer L.. Prenatal and postnatal cell phone exposure and headaches in children. Open Pediatr Med J 2012;6:46–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sudan M, Kheifets L, Arah OA, Olsen J.. Cell phone exposures and hearing loss in children. Paediatr Perinat Epidemiol 2013;27:247–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.