Abstract
Purpose
To investigate vitreous levels of chemokines in eyes with ischemic retinal vein occlusion (RVO).
Methods
The vitreous humor was collected at the start of 23-gauge pars plana vitrectomy from patients with ischemic RVO and patients with idiopathic preretinal membranes (PRMs) and idiopathic macular holes (IMHs). The levels of 40 different chemokines were measured using magnetic color-bead-based multiplex assay. The chi-square test was performed for clinical variables such as sex, and the Mann–Whitney U test was performed to evaluate the differences in the chemokine levels between the RVO group and the control group.
Results
Vitreous humor was collected from 20 controls and 25 subjects with ischemic RVO. C-C motif ligand 17 (CCL17) was unmeasurable in more than 70% of the samples. The levels of 29 of 39 chemokines were statistically significantly elevated in the RVO group compared with the control group, including CCL21, C-X-C motif ligand (CXCL) 13, CCL27, CCL24, CX3CL1, CXCL6, interferon-gamma (IFN-γ), interleukin (IL) 1β, IL-2, IL-4, IL-6, IL-8, IL-10, IL-16, CXCL10, CXCL11, CCL8, CCL7, CCL13, CCL22, macrophage migration inhibitory factor (MIF), CXCL9, CCL3, CCL15, CCL20, CCL19, CCL23, CCL25, and tumor necrosis factor-alpha (TNF-α). Among the 29 elevated chemokines, we found that the levels of three chemokines (IL-8, CXCL9, and TNF-α) showed a more than six-fold increase in the RVO eyes versus controls, and CXCL9 expression showed the greatest change of all tested chemokines.
Conclusions
Dozens of chemokines were found to be elevated in the vitreous of RVO eyes complicated with vitreous hemorrhage, suggesting that inflammation is severe in the ischemic retina. The knowledge of specific upregulation of chemokines in ischemic RVO could allow more targeted future therapies.
Introduction
Retinal vein occlusion (RVO) is the second most common retinal vascular disease after diabetic retinopathy, and it is an important cause of visual loss [1,2]. RVO can be classified as branch retinal vein occlusion (BRVO), central retinal vein occlusion (CRVO), and hemispheric RVO. It is characterized by obstruction of the retinal vein, leading to macular edema, hemorrhage, and retinal ischemia [3]. Ischemia can lead to hypoxia and may trigger the release of inflammatory factors, including cytokines, chemokines, and vascular endothelial growth factors [3-5]. Vitreous hemorrhage is one of the major complications of ischemic RVO, and it is considered a result of neovascularization caused by retinal ischemia [3,6]. Vitreous hemorrhage is reported in 10% of ischemic CRVO by 9 months after the onset of occlusion and developed in 61%–73% of patients with ischemic BRVO during follow-up periods between 2 and 4 years [7,8].
The role of inflammation in the clinical consequences of RVO is a topic of growing interest. Chemokines are a family of small heparin-binding proteins, mostly known for their role in chemotaxis, immune surveillance, and inflammation [9]. The roles of some proinflammatory chemokines in RVO have been reported by a few research groups, and increased levels of some chemokines are associated with macular edema and retinal ischemia [3-5,10,11]. Overexpression of proinflammatory cytokines and chemokines may exacerbate hypoxia, and a vicious circle may follow. However, there are limited studies on the vitreous levels of chemokines in patients with RVO complicated with vitreous hemorrhage. In addition, most published studies on chemokine profiles have focused on the aqueous humor in patients with macular edema but not ischemic RVO complicated with vitreous hemorrhage. Having a better understanding of the chemokine profile in ischemic RVO enables us to know more about activation of the immune-inflammatory process in RVO, thus contributing to development of future therapeutic approaches. Therefore, we designed the present study to investigate the vitreous levels of chemokines in eyes with ischemic RVO in an attempt to obtain a better understanding of the pathophysiology in the disease and identify potential treatment targets.
Methods
This study was performed in accordance with the tenets of the Declaration of Helsinki. The study adhered to the ARVO statement on human subjects. Informed consent was obtained from all the study subjects, and the study was approved by the Research Ethics Committee of the Guangdong Provincial People’s Hospital (Number 2016232A). The control group comprised subjects with idiopathic macular holes (IMHs) and preretinal membranes (PRMs). The RVO group comprised subjects with central or branch retinal vein occlusion complicated with unresolved or condensed vitreous hemorrhage. Subjects with the following conditions were excluded: (1) patients with other ocular conditions (glaucoma, uveitis, etc.); (2) patients with a history of ocular surgery within the previous 6 months; (3) patients who had received anti-VEGF treatment; and (4) subjects with severe systemic inflammatory diseases. All subjects underwent a complete ocular examination. Vitreous humor was collected from 20 control subjects (six with PRMs and 14 with IMHs) and 25 subjects with ischemic RVO. The 23-gauge trocar and cannula system (Alcon Laboratories, Inc., Fort Worth, Texas) was used to perform pars plana vitrectomy under standardized operation procedures for all subjects. About 0.2 to 0.4 ml of undilute vitreous humor was aspirated into a sterile syringe before the intraocular infusion. The samples were immediately placed on ice and transferred to microcentrifuge tubes. After immediately centrifugation at 1,000 ×g at 4 °C for 10 min, the supernatants of the samples were aspirated and subsequently stored at −80 °C until further analysis.
We used the Bio-Plex ProTM human chemokine panel 40-plex kit (Bio-Rad Laboratories, Inc., Hercules, CA) to measure the concentrations of the following 40 human chemokines: interleukin (IL)-10, IL-16, C-X-C motif ligand 10 (CXCL10(, CXCL11, C-C motif ligand 2 (CCL2), CCL8, CCL7, CCL13, CCL22, macrophage migration inhibitory factor (MIF), CXCL9, CCL3, CCL15, CCL20, CCL19, CCL23, CXCL16, CXCL12, CCL17, CCL25, TNF-α, CCL21, CXCL13, CXCL5, CCL11, CCL24, CCL26, CCL27, CX3CL1, CXCL6, granulocyte macrophage colony-stimulating factor (GM-CSF), CXCL1, CXCL2, CCL1, interferon-gamma (IFN-γ), IL-1β, IL-2, IL-4, IL-6, and IL-8. All experimental procedures were conducted according to the manufacturer’s instructions. The Bio-PlexTM 200 System (software version 6.1, Bio-Rad Laboratories) was used to analyze the fluorescence intensity of the assay. A chemokine concentration lower than the limit of detection was regarded as non-measurable.
The STRING database was used to demonstrate interactions between the different groups. The STRING database aims to collect and integrate all functional interactions between the expressed proteins by consolidating known and predicted protein–protein association data for a large number of organisms [12]. The associations in STRING include direct (physical) interactions, as well as indirect (functional) interactions, as long as both are specific and biologically meaningful [13].
Statistical analysis
The statistical analyses were performed using IBM SPSS Statistics version 19.0 (IBM SPSS Statistics; IBM Corporation, Chicago, IL). The chi-square test was performed for clinical variables such as sex, and the Mann–Whitney U test was performed for evaluation of differences in chemokine levels. A p value less than or equal to 0.05 was considered statistically significant.
Results
The clinical characteristics of the control group and the RVO group are shown in Table 1. In comparison to the control group, the mean systolic and diastolic blood pressures were higher in the RVO group, but they were not statistically significant (p=0.230 and p=0.736, respectively). No statistically significant differences in age and gender were found between the control group and the RVO group (p=0.630 and p=0.502, respectively).
Table 1. Demographic and clinical characteristics of the control group and RVO group.
| Clinical characteristics | Control group (n=20) | RVO group (n=25) | P value |
|---|---|---|---|
| Age (years) |
56.20.40±10.18 |
57.84±12.03 |
0.630* |
| Male/Female |
43,748 |
15/10 |
0.502# |
| SBP (mmHg) |
133.75±19.51 |
140.52±17.72 |
0.230* |
| DBP (mmHg) | 77.90±10.09 | 79.00±11.33 | 0.736* |
RVO=retinal vein occlusion; SBP=Systolic blood pressure; DBP=Diastolic blood pressure; *=data was described as mean±standard deviation and compared with one-way ANOVA; #=data was analyzed with chi-square test.
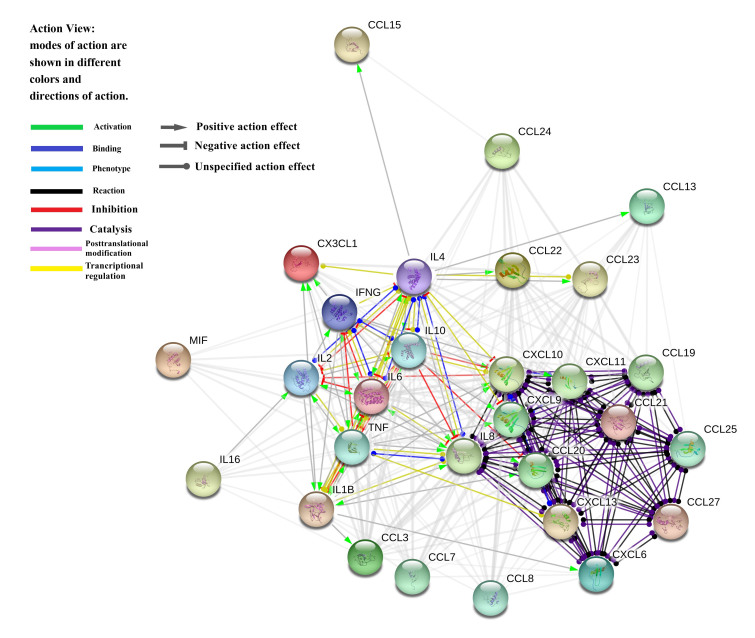
The following 29 chemokines were statistically significantly elevated in the RVO group compared with the control group (Table 2): CCL21, CXCL13, CCL27, CCL24, CX3CL1, CXCL6, IFN-γ, IL-1β, IL-2, IL-4, IL-6, IL-8, IL-10, IL-16, CXCL10, CXCL11, CCL8, CCL7, CCL13, CCL22, MIF, CXCL9, CCL3, CCL15, CCL20, CCL19, CCL23, CCL25, and TNF-α. Figure 1 shows the interactions among the 29 chemokines.
Table 2. Summary of chemokine in the measured vitreous.
| Chemokine (pg/ml) | Control (n=20) |
RVO (n=25) |
p Value | ||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| CCL21 |
116.26 |
41.31 |
203.43 |
56.44 |
<0.001* |
| CXCL13 |
0.41 |
0.15 |
0.65 |
0.2 |
<0.001* |
| CCL27 |
1.37 |
0.51 |
4.1 |
1.25 |
<0.001* |
| CXCL5 |
162.54 |
31.5 |
150.32 |
27.03 |
0.144 |
| CCL11 |
1.78 |
0.52 |
2.12 |
0.6 |
0.073 |
| CCL24 |
3.89 |
0.71 |
5.67 |
0.97 |
<0.001* |
| CCL26 |
1.23 |
0.11 |
1.36 |
0.3 |
0.064 |
| CX3CL1 |
5.91 |
1.95 |
8.43 |
1.46 |
<0.001* |
| CXCL6 |
0.24 |
0.56 |
0.86 |
0.15 |
0.001* |
| GM-CSF |
4.2 |
1.23 |
3.99 |
1.06 |
0.335 |
| CXCL1 |
6.31 |
3.58 |
8.12 |
2.85 |
0.096 |
| CXCL2 |
7.95 |
1.17 |
8.23 |
1.54 |
0.138 |
| CCL1 |
4.42 |
0.75 |
5.08 |
0.74 |
0.07 |
| IFN-γ |
1.42 |
0.51 |
2.03 |
0.26 |
<0.001* |
| IL-1β |
0.26 |
0.07 |
0.37 |
0.06 |
<0.001* |
| IL-2 |
0.53 |
0.01 |
0.73 |
0.04 |
<0.001* |
| IL-4 |
0.88 |
0.74 |
2.76 |
0.73 |
<0.001* |
| IL-6 |
2.89 |
7.65 |
9.13 |
0.84 |
0.038* |
| IL-8 |
1.35 |
1.22 |
8.93 |
7.09 |
<0.001* |
| IL-10 |
0.83 |
0.23 |
2.14 |
0.71 |
<0.001* |
| IL-16 |
11.24 |
2.21 |
31.03 |
21.83 |
<0.001* |
| CXCL10 |
9.78 |
11.42 |
63.35 |
13.37 |
<0.001* |
| CXCL11 |
0.11 |
0.04 |
0.17 |
0.04 |
<0.001* |
| CCL2 |
73.24 |
36.6 |
72.56 |
25.68 |
0.411 |
| CCL8 |
0.23 |
0.21 |
0.94 |
0.09 |
<0.001* |
| CCL7 |
7.95 |
1.49 |
10.19 |
0.4 |
<0.001* |
| CCL13 |
0.2 |
0.04 |
0.33 |
0.07 |
<0.001* |
| CCL22 |
3.51 |
0.79 |
6.15 |
0.32 |
<0.001* |
| MIF |
146.2 |
177.09 |
513.21 |
27.28 |
<0.001* |
| CXCL9 |
7.02 |
9.98 |
54.32 |
19.78 |
<0.001* |
| CCL3 |
0.76 |
0.53 |
1.41 |
0.29 |
<0.001* |
| CCL15 |
55.1 |
40.98 |
101.12 |
6.38 |
<0.001* |
| CCL20 |
0.37 |
0.14 |
0.65 |
0.11 |
<0.001* |
| CCL19 |
2.78 |
2.05 |
16.12 |
1.39 |
<0.001* |
| CCL23 |
1.94 |
0.66 |
3.51 |
0.61 |
<0.001* |
| CXCL16 |
82.11 |
17.04 |
87.54 |
13.14 |
0.936 |
| CXCL12 |
44.89 |
17.09 |
52.34 |
20.39 |
0.178 |
| CCL25 |
7.44 |
2.67 |
14.21 |
1.23 |
<0.001* |
| TNF-α | 1.03 | 0.98 | 6.87 | 1.78 | <0.001* |
RVO=retinal vein occlusion; IQR=interquantile range; CCL=C-C motif ligand;CXCL=C-X-C motif ligand; GM-CSF=granulocyte macrophage colony-stimulating factor ; IFN-γ=interferon-gamma ; IL=Interleukin; MIF=macrophage migration inhibitory factor; TNF-α=tumor necrosis factor-alpha; *=Statistical significant p value by Mann–Whitney U test
Figure 1.
A STRING pathway demonstrating the relationships of the 29 chemokines. CSF-2, colony-stimulating factor; GM-CSF, granulocyte macrophage colony-stimulating factor; IFN-γ, interferon-gamma; CXCL, C-X-C motif ligand; IL, interleukin; CCL, C-C motif ligand; TNF-α, tumor necrosis factor-alpha; MIF, macrophage migration inhibitory factor.
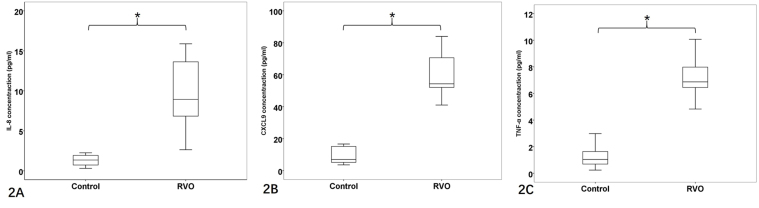
Three chemokines were elevated more than six times in the RVO group compared with the control group, including IL-8, CXCL9, and TNF-α (Figure 2). The levels of the following ten chemokines were comparable between the control group and the RVO group: CXCL5, CCL11, CCL26, GM-CSF, CXCL1, CXCL2, CCL1, CCL2, CXCL12, and CXCL16. CCL17 was not included in the analysis because it was non-measurable in more than 70% of the samples of each group.
Figure 2.
Box plots of chemokines in the RVO group (n=25) and control group (n=20). A: IL-8, B: CXCL9 and C: TNF-α. *=Statistically significant (Mann-Whitney U test, all p<0.001).
Discussion
In the present study, we investigated and compared the vitreous levels of 40 chemokines in 20 relatively healthy subjects and 25 patients with ischemic RVO. We found that the levels of 29 of 39 chemokines were statistically significantly elevated in the RVO group compared with the control group. Moreover, the levels of IL-8, CXCL9, and TNF-α showed a more than six-fold increase in the RVO group versus the control group, and CXCL9 expression showed the greatest change of all the tested chemokines. String pathway analysis showed that the chemokines of the C-C motif ligand family and the C-X-C motif ligand family tended to interact in a cluster, while CXCL10 and IL-8 played roles linking them to the interleukin family. CX3CL1 could be activated by IFN-γ, TNF-α, and IL-1β. IL-2 could be activated by IL-6, IL-16, and TNF-α, while it could be inhibited by IL-4, CXCL10, and IL-6. IL-1β could be activated by IL-2, IL-8, IFN-γ, and TNF-α, and IL-1β activated CCL3, CCL20, CXCL6, and CX3CL1. IL-8 could be activated by IL-4, IFN-γ, IL-2, TNF-α, and IL-1β, but it could be inhibited by IL-10 and IL-6. CXCL10 can be activated by IFN-γ, TNF-α, and IL-1β, while it could be inhibited by IL-4 and IL-10.
Previous studies have reported that some chemokines are elevated in the aqueous humor or vitreous humor of patients with ischemic or non-ischemic RVO, and we found 11 chemokines in the panel were among them, including IL-1β, IL-2, IL-6, IL-8, IL-10, CCL3, CCL11, CXCL9, CXCL10, IFN-γ, and TNF-α [5,8,14-17]. Regarding the intraocular levels of chemokines in ischemic RVO, IL-1β, IL-6, IL-8, IFN-γ, CCL2, and TNF-α were found to be elevated and were reported to play a role in the pathogenesis of the ischemic form of RVO as well as the associated neuronal cell death occurring within the retina [8]. Noma et al. found that aqueous levels of IL-6 are correlated with the size of the non-perfused area in BRVO, indicating that IL-6 could be used to determine the severity of the ischemic condition [10]. Although studies have found the elevation of the chemokines above in ischemic RVO, few of them investigated ischemic subjects with vitreous hemorrhage. Thus, the present study demonstrated a comprehensive insight and provides more information for further investigation in patients with RVO complicated with vitreous hemorrhage.
Studies reported that the levels of CCL2 and CXCL12 were higher in the intraocular fluid of patients with RVO, while we found that the vitreous concentrations of these chemokines were comparable between the control group and the RVO group. Suzuki and colleagues reported that the vitreous levels of CCL2 was elevated in patients with CRVO compared to healthy controls [14]. In conditions of iris neovascularization secondary to ischemic RVO, the vitreous levels of CXCL12 were upregulated. Kii et al. found that vitreous CXCL12 levels in active RVO (four eyes with iris neovascularization) were statistically significantly higher than those in quiescent RVO (16 eyes without iris neovascularization) and the negative controls, whereas there was no statistically significant difference between patients with quiescent RVO and the negative controls [18]. The present study showed that CXCL12 in the subjects with vitreous hemorrhage secondary to ischemic RVO was not statistically different from the controls. It is interesting that different phenotypes of ischemic RVO (e.g., RVO with iris neovascularization and RVO with vitreous hemorrhage) had different expression of CXCL12. In an animal experiment, the expression of CXCL12 was reduced at 2 days after the RVO models were induced, while it was upregulated at 20 days after the induction, suggesting that this chemokine may play a role in the progression of RVO [19]. More investigations are needed to clarify the controversial results of CXCL12 in RVO eyes.
To our knowledge, little is known about the intraocular concentration of the following chemokines in patients with RVO: IL-4, IL-16, CCL7, CCL8, CCL13, CCL15, CCL20, CCL21, CCL22, CCL23, CCL24, CCL25, CCL26, CCL27, CXCL5, CXCL6, CXCL11, CXCL13, CX3CL1, and MIF. IL-4 was reported as an anti-inflammatory factor and has been considered an antiangiogenesis factor in diabetic retinopathy [20,21]. In addition, IL-4 has the function to increase the survival of retinal ganglion cells [22]. IL-16 is a chemoattractant for various CD4+ immune cells, and it contributes to the regulatory process of CD4+ cell recruitment and activation at sites of inflammation in association with asthma and several autoimmune diseases [23]. Few studies have been reported to reveal the role of IL-16 in ocular diseases, except that it is known to be associated with allergic conjunctival disorders and thyroid-associated ophthalmopathy [24,25]. Elevated aqueous levels of CCL15, CXCL5, CXCL11, and CX3CL1 are associated with dry eye disease, and CXCL6 is associated with dry age-related macular degeneration [26-28]. Moreover, Abu and colleagues found that CCL20 and CXCL13 might be novel biomarkers of specific endogenous uveitic entities [29]. However, there are extremely limited published studies on the CC chemokine ligands and CXC chemokine ligands mentioned above (CCL7–8, CCL13, CCL15, CCL20–27, CXCL5, CXCL6, CXCL11, and CXCL13) in RVO or even in ophthalmic fundus disorders, and their roles in ischemic retinal diseases warrant further study.
CX3CL1 is the sole member of the CX3C chemokine family, and it is a chemoattractant and adhesion molecule for leukocytes [30]. An experimental study showed that CX3CL1 is able to induce endothelial cell chemotaxis, endothelial cell tube formation, and corneal neovascularization, indicating that it may be a mediator of ocular angiogenesis [31]. Regarding MIF, Wang et al. found that areas of vascular obliteration increased by 49%, sprouting tips reduced by 27%, and preretinal angiogenesis inhibited by 35% were observed in an MIF knockout mice model with oxygen induced retinopathy, indicating that MIF has proangiogenic and proinflammatory properties in retinal neovascularization [32]. Considering that CX3CL1 and MIF was found to be associated with angiogenesis in other ischemic retinopathies, we assume that they may play a role in the progression of ischemic RVO. Further investigations are needed to verify the roles of CXCL3 and MIF in the progression of RVO. In the present study, we found that the levels of three chemokines (IL-8, CXCL9, and TNF-α) were elevated more than five times in the RVO group compared with the control group, and CXCL9 expression showed the greatest change of all tested chemokines. A previous study reported that the levels of aqueous IL-8 and TNF-α were statistically significantly higher in the ischemic RVO group than in the nonischemic RVO group [3]. Noma et al. found that the number of intravitreal ranibizumab injections was positively correlated with the baseline aqueous level of IL-8 in patients with BRVO, suggesting that IL-8 may influence the recurrence of macular edema [33]. In a pig model of BRVO, neural cell death occurred early and was accompanied by upregulation of IL-8 and glial acidic fibrillary protein, indicating that therapeutic strategies aimed at preservation of retinal neural cells were important in the management of RVO [19]. CXCL9 is known to be a monokine induced by gamma interferon, which may bind its receptor CXCR3 to exert an effect on neuroinflammation, and neurodegeneration in the central nervous system [34]. There are limited studies in CXCL9 and ocular conditions including RVO. Given that the present study revealed CXCL9 as the most increased chemokine in the vitreous of RVO, the role of CXCL9 in the pathogenesis of ischemic RVO warrants further study.
The elevated vitreous chemokines in ischemic RVO indicated that a complex chemokine network was involved in the retinal vascular occlusive disease, which may contribute to the impairment of neurovascular structures. Although anti-VEGF agents are effective in the management of patients with RVO complicated with macular edema or neovascularization, many inflammatory factors are also related to the pathological status, and anti-VEGF agents are not effective in lowering the intraocular concentrations of the inflammatory factors [35]. The study showed that variations in VEGF levels were responsible for about 30% of the variance in retinal thickness in patients with macular edema due to BRVO or CRVO, indicating that about 70% of the contribution is from factors other than VEGF [36,37]. The intraocular levels of chemokines have found to be associated with morphological changes in patients with RVO [3,38]. Blocking the actions of inflammatory cytokines and chemokines using steroids is also effective in reducing inflammation in patients with RVO [15]. For patients with RVO complicated with unresolved vitreous hemorrhage, pars plana vitrectomy and retinal photocoagulation are the major treatment options [8]. However, such procedures may worsen the inflammation due to trauma and thermal damage. In the present study, dozens of chemokines were elevated, suggesting that the inflammation in ischemic RVO was severe, and postoperative anti-inflammation therapy using a steroid such as dexamethasone implant or steroid eye drops is important. Identifying the inflammatory biomarkers of the complications in RVO could allow us to know more about different phenotypes of the disease, and may provide us with valuable information on modulating the therapeutic strategy.
There are several limitations in the present study. It would be better if the sample size had been larger. In addition, we did not collect serum samples; thus, we could not study the systemic circulating chemokines and compare them with ocular chemokines. In clinical practice, vitreous humor of healthy subjects is not available because of the invasive nature of the procedures and ethical issues. The vitreous humor of patients with idiopathic preretinal membranes and idiopathic macular holes are commonly used as controls in experiments, because the changes in vitreous components in these conditions are relatively lower than those in other oculopathy [39-42]. This is truly a weak point of the investigation, but these samples are the best choice we have in clinical practice. Hemorrhage is the one of the signs of ischemic RVO. The ischemic condition may lead to hemorrhage, and in contrast, the blood may exacerbate the inflammation when in contact with the retina. Thus, further studies concerning the association of serum and vitreous levels of chemokines in ischemic RVO, as well as the association of vitreous hemorrhage with and without ischemia (such as in traumatic retinal hemorrhage), may be needed to resolve this question.
In conclusion, we investigated vitreous levels of chemokine profile in eyes with ischemic RVO using one of the most comprehensive panels in the study. Dozens of chemokines were found to be elevated in the vitreous of patients with RVO complicated with vitreous hemorrhage, suggesting that inflammation is severe in the ischemic retina. The elevated chemokines might be used as treatment targets in the future, and further investigations are needed to verify the roles of chemokines in the progression of RVO.
Acknowledgments
This study was supported by National Natural Science Foundation of China (Grant Number 81,500,737) and Medical Scientific Research Foundation of Guangdong Province, China (Grant Number B2018096). The sponsors or funding organizations had no role in the design or conduct of this research.
References
- 1.Cugati S, Wang JJ, Rochtchina E, Mitchell P. Ten-Year Incidence of Retinal Vein Occlusion in an Older Population: The Blue Mountains Eye Study. Arch Ophthalmol. 2006;124:726–32. doi: 10.1001/archopht.124.5.726. [DOI] [PubMed] [Google Scholar]
- 2.Jaulim A, Ahmed B, Khanam T, Chatziralli IP. BRANCH RETINAL VEIN OCCLUSION: Epidemiology, Pathogenesis, Risk Factors, Clinical Features, Diagnosis, and Complications. An Update of the Literature. Retina. 2013;33:901–10. doi: 10.1097/IAE.0b013e3182870c15. [DOI] [PubMed] [Google Scholar]
- 3.Jung SH, Kim K, Sohn SW, Yang SJ. Association of Aqueous Humor Cytokines with the Development of Retinal Ischemia and Recurrent Macular Edema in Retinal Vein Occlusion. Invest Ophthalmol Vis Sci. 2014;55:2290–6. doi: 10.1167/iovs.13-13587. [DOI] [PubMed] [Google Scholar]
- 4.Ehlken C, Grundel B, Michels D, Junker B, Stahl A, Schlunck G, Hansen LL, Feltgen N, Martin G, Agostini HT. Increased Expression of Angiogenic and Inflammatory Proteins in the Vitreous of Patients with Ischemic Central Retinal Vein Occlusion. PLoS One. 2015;10:0126859. doi: 10.1371/journal.pone.0126859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koss MJ, Pfister M, Rothweiler F, Michaelis M, Cinatl J, Schubert R, Koch F. Comparison of cytokine levels from undiluted vitreous of untreated patients with retinal vein occlusion. Acta Ophthalmologica. 2012;90:e98–e103. doi: 10.1111/j.1755-3768.2011.02292.x. [DOI] [PubMed] [Google Scholar]
- 6.Hayreh SS, Rojas P, Podhajsky P, Montague PR, Woolson RF. Ocular Neovascularization with Retinal Vascular Occlusion-III: Incidence of Ocular Neovascularization with Retinal Vein Occlusion. Ophthalmology. 1983;90:488–506. doi: 10.1016/s0161-6420(83)34542-5. [DOI] [PubMed] [Google Scholar]
- 7.Mcintosh R, Rogers S, Lim LL, Cheung N, Wang JJ, Mitchell P, Kowalski JW, Nguyen H, Wong TY. Natural history of central retinal vein occlusion: an evidence-based systematic review. Ophthalmology. 2010;117:1113–23. doi: 10.1016/j.ophtha.2010.01.060. [DOI] [PubMed] [Google Scholar]
- 8.Khayat M, Williams M, Lois N. Ischemic Retinal Vein Occlusion: characterizing the more severe spectrum of retinal vein occlusion. Surv Ophthalmol. 2018;63:816–50. doi: 10.1016/j.survophthal.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 9.Dimberg A. Chemokines in Angiogenesis. Curr Top Microbiol Immunol. 2010;341:59–80. doi: 10.1007/82_2010_21. [DOI] [PubMed] [Google Scholar]
- 10.Noma H, Funatsu H, Yamasaki M, Tsukamoto H, Mimura T, Sone T, Jian K, Sakamoto I, Nakano KE, Yamashita H. Pathogenesis of Macular Edema With Branch Retinal Vein Occlusion and Intraocular Levels of Vascular Endothelial Growth Factor and Interleukin-6. Am J Ophthalmol. 2005;140:256–61. doi: 10.1016/j.ajo.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 11.Fonollosa A, Garciaarumi J, Santos E, Macia C, Fernandez P, Segura RM, Zapata MA, Rodriguezinfante R, Boixadera A, Martinezcastillo V. Vitreous levels of interleukine-8 and monocyte chemoattractant protein-1 in macular oedema with branch retinal vein occlusion. Eye (Lond) 2010;24:1284–90. doi: 10.1038/eye.2009.340. [DOI] [PubMed] [Google Scholar]
- 12.Szklarczyk D, Morris JH, Cook HV, Kuhn M, Wyder S, Simonovic M, Santos A, Doncheva NT, Roth A, Bork P. The STRING database in 2017: quality-controlled protein–protein association networks, made broadly accessible. Nucleic Acids Research 2017; 45:0. [DOI] [PMC free article] [PubMed]
- 13.Szklarczyk D, Franceschini A, Wyder S, Forslund K, Heller D, Huerta-Cepas J, Simonovic M, Roth A, Santos A, Tsafou KP, Kuhn M, Bork P, Jensen LJ, von Mering C. STRING v10: protein–protein interaction networks, integrated over the tree of life. Nucleic Acids Res. 2015;43:D447–52. doi: 10.1093/nar/gku1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suzuki Y, Nakazawa M, Suzuki K, Yamazaki H, Miyagawa Y. Expression profiles of cytokines and chemokines in vitreous fluid in diabetic retinopathy and central retinal vein occlusion. Jpn J Ophthalmol. 2011;55:256–63. doi: 10.1007/s10384-011-0004-8. [DOI] [PubMed] [Google Scholar]
- 15.Rezardreindl S, Eibenberger K, Pollreisz A, Buhl W, Georgopoulos M, Krall C, Dunavolgyi R, Weigert G, Kroh M, Schmidterfurth U. Effect of intravitreal dexamethasone implant on intra‐ocular cytokines and chemokines in eyes with retinal vein occlusion. Acta Ophthalmologica. 2017;95:e119–e127. doi: 10.1111/aos.13152. [DOI] [PubMed] [Google Scholar]
- 16.Cehofski LJ, Honore B, Vorum HA. Review: Proteomics in Retinal Artery Occlusion, Retinal Vein Occlusion, Diabetic Retinopathy and Acquired Macular Disorders. Int J Mol Sci. 2017;18:907. doi: 10.3390/ijms18050907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Okunuki Y, Usui Y, Katai N, Takeuchi M, Kezuka T, Wakabayashi Y, Goto H. Analysis of Multiple Chemokines and Growth Factors in the Vitreous of Patients With Branch Retinal Vein Occlusion. Invest Ophthalmol Vis Sci. 2009;50:5397. [Google Scholar]
- 18.Kii Y, Arimura N, Noda Y, Yamakiri K, Doi N, Hashiguchi T, Maruyama I, Shimura M, Sakamoto T. Stromal-Derived Factor-1 and Inflammatory Cytokines in Retinal Vein Occlusion. Curr Eye Res. 2007;32:1065–72. doi: 10.1080/02713680701758727. [DOI] [PubMed] [Google Scholar]
- 19.Mcallister IL, Vijayasekaran S, Zhang D, Mclenachan S, Chen FK, Yu D. Neuronal degeneration and associated alterations in cytokine and protein in an experimental branch retinal venous occlusion model. Exp Eye Res. 2018;174:133–46. doi: 10.1016/j.exer.2018.05.025. [DOI] [PubMed] [Google Scholar]
- 20.Hopps E, Canino B, Caimi G. Effects of exercise on inflammation markers in type 2 diabetic subjects. Acta Diabetol. 2011;48:183–9. doi: 10.1007/s00592-011-0278-9. [DOI] [PubMed] [Google Scholar]
- 21.Xie M, Hu A, Luo Y, Sun W, Hu X, Tang S. Interleukin-4 and melatonin ameliorate high glucose and interleukin-1β stimulated inflammatory reaction in human retinal endothelial cells and retinal pigment epithelial cells. Mol Vis. 2014;20:921–8. [PMC free article] [PubMed] [Google Scholar]
- 22.De Araujomartins L, Oliveira RM, Santos GVGD, Santos RCCD, Santos AAD, De Araujo EG. Treatment in vitro of retinal cells with IL-4 increases the survival of retinal ganglion cells: the involvement of BDNF. Neurochem Res. 2013;38:162–73. doi: 10.1007/s11064-012-0904-0. [DOI] [PubMed] [Google Scholar]
- 23.Cruikshank WW, Kornfeld H, Center DM. Interleukin-16. J Leukoc Biol. 2000;67:757–66. doi: 10.1002/jlb.67.6.757. [DOI] [PubMed] [Google Scholar]
- 24.Shoji J, Aso H, Inada N. Clinical Usefulness of Simultaneous Measurement of the Tear Levels of CCL17, CCL24, and IL-16 for the Biomarkers of Allergic Conjunctival Disorders. Curr Eye Res. 2017;42:677–84. doi: 10.1080/02713683.2016.1242755. [DOI] [PubMed] [Google Scholar]
- 25.Fang S, Huang Y, Zhong S, Zhang Y, Liu X, Wang Y, Gu P, Zhou H, Fan X. IL-17A Promotes RANTES Expression, But Not IL-16, in Orbital Fibroblasts Via CD40–CD40L Combination in Thyroid-Associated Ophthalmopathy. Invest Ophthalmol Vis Sci. 2016;57:6123–33. doi: 10.1167/iovs.16-20199. [DOI] [PubMed] [Google Scholar]
- 26.Na K, Mok J, Kim JY, Rho CR, Joo C. Correlations between tear cytokines, chemokines, and soluble receptors and clinical severity of dry eye disease. Invest Ophthalmol Vis Sci. 2012;53:5443–50. doi: 10.1167/iovs.11-9417. [DOI] [PubMed] [Google Scholar]
- 27.Spindler J, Zandi S, Pfister IB, Gerhardt C, Garweg JG. Cytokine profiles in the aqueous humor and serum of patients with dry and treated wet age-related macular degeneration. PLoS One. 2018;13:e0203337. doi: 10.1371/journal.pone.0203337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yoon K, Park C, You I, Choi H, Lee KH, Im S, Park H, Pflugfelder SC. Expression of CXCL9, −10, −11, and CXCR3 in the Tear Film and Ocular Surface of Patients with Dry Eye Syndrome. Invest Ophthalmol Vis Sci. 2010;51:643–50. doi: 10.1167/iovs.09-3425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Elasrar AMA, Berghmans N, Alobeidan SA, Mousa A, Opdenakker G, Van Damme J, Struyf S. The Cytokine Interleukin-6 and the Chemokines CCL20 and CXCL13 Are Novel Biomarkers of Specific Endogenous Uveitic Entities. Invest Ophthalmol Vis Sci. 2016;57:4606–13. doi: 10.1167/iovs.16-19758. [DOI] [PubMed] [Google Scholar]
- 30.Liu W, Jiang L, Bian C, Liang Y, Xing R, Yishakea M, Dong J. Role of CX3CL1 in Diseases. Arch Immunol Ther Exp (Warsz) 2016;64:371–83. doi: 10.1007/s00005-016-0395-9. [DOI] [PubMed] [Google Scholar]
- 31.You J, Yang C, Huang J, Chen M, Yang C. Fractalkine, a CX3C Chemokine, as a Mediator of Ocular Angiogenesis. Invest Ophthalmol Vis Sci. 2007;48:5290–8. doi: 10.1167/iovs.07-0187. [DOI] [PubMed] [Google Scholar]
- 32.Wang J, Lin J, Kaiser U, Wohlfart P, Hammes H. Absence of macrophage migration inhibitory factor reduces proliferative retinopathy in a mouse model. Acta Diabetol. 2017;54:383–92. doi: 10.1007/s00592-016-0956-8. [DOI] [PubMed] [Google Scholar]
- 33.Noma H, Mimura T, Yasuda K, Nakagawa H, Motohashi R, Kotake O, Shimura M. Cytokines and Recurrence of Macular Edema after Intravitreal Ranibizumab in Patients with Branch Retinal Vein Occlusion. Ophthalmologica. 2016;236:228–34. doi: 10.1159/000451062. [DOI] [PubMed] [Google Scholar]
- 34.Koper OM, Kaminska J, Sawicki K, Kemona H. CXCL9, CXCL10, CXCL11, and their receptor (CXCR3) in neuroinflammation and neurodegeneration. Adv Clin Exp Med. 2018;27:849–56. doi: 10.17219/acem/68846. [DOI] [PubMed] [Google Scholar]
- 35.Noma H, Mimura T, Yasuda K, Shimura M. Cytokine Kinetics after Monthly Intravitreal Bevacizumab for Retinal Vein Occlusion Associated with Macular Oedema. Ophthalmic Res. 2016;56:207–14. doi: 10.1159/000445211. [DOI] [PubMed] [Google Scholar]
- 36.Vujosevic S, Midena E. Controversies in Pharmacological Treatment of Inflammatory Component of Macular Edema. Curr Pharm Des. 2015;21:4688–93. doi: 10.2174/1381612821666150909095645. [DOI] [PubMed] [Google Scholar]
- 37.Noma H, Funatsu H, Mimura T, Harino S, Hori S. Vitreous levels of interleukin-6 and vascular endothelial growth factor in macular edema with central retinal vein occlusion. Ophthalmology. 2009;116:87–93. doi: 10.1016/j.ophtha.2008.09.034. [DOI] [PubMed] [Google Scholar]
- 38.Noma H, Mimura T, Eguchi S. Association of inflammatory factors with macular edema in branch retinal vein occlusion. JAMA Ophthalmol. 2013;131:160–5. doi: 10.1001/2013.jamaophthalmol.228. [DOI] [PubMed] [Google Scholar]
- 39.Angi M, Kalirai H, Coupland SE, Damato B, Semeraro F, Romano MR. Proteomic Analyses of the Vitreous Humour. Mediators Inflamm. 2012;2012:148039. doi: 10.1155/2012/148039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chernykh VV, Varvarinsky EV, Smirnov EV, Chernykh DV, Trunov AN. Proliferative and inflammatory factors in the vitreous of patients with proliferative diabetic retinopathy. Indian J Ophthalmol. 2015;63:33–6. doi: 10.4103/0301-4738.151464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yoshimura T, Sonoda K, Sugahara M, Mochizuki Y, Enaida H, Oshima Y, Ueno A, Hata Y, Yoshida H, Ishibashi T. Comprehensive Analysis of Inflammatory Immune Mediators in Vitreoretinal Diseases. PLoS One. 2009;4:e8158. doi: 10.1371/journal.pone.0008158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Maier R, Weger M, Hallerschober E, Elshabrawi Y, Wedrich A, Theisl A, Aigner R, Barth A, Haas A. Multiplex bead analysis of vitreous and serum concentrations of inflammatory and proangiogenic factors in diabetic patients. Mol Vis. 2008;14:637–43. [PMC free article] [PubMed] [Google Scholar]