Abstract
Objective
Orthopedic literature on expectations is limited by lack of uniformity in how expectations are defined, conceptualized, and measured. Within this scoping review, we present a conceptual framework for understanding the construct of expectations and its derivatives (ie, expectation, expectancy, expectancies, etc) in studies of elective surgical orthopedic procedures. We also utilize this framework to map the current orthopedic surgery literature on expectations, highlighting its strengths, weaknesses, and gaps in its knowledge base.
Methods
We included articles that mentioned both expectations and one or more of 10 selected surgeries in their title or abstract. We focused on representative elective orthopedic surgeries that covered the body's major regions. We operationalized each study's individual expectation items into one of the expectation concept types within the presented conceptual model. We also extracted the name and type of expectations measurement tool used, whose expectations were measured, and descriptive information (eg, surgery type, publication date, country of origin, and study type).
Results
Ninety studies were included, with 70% published after 2008. A total of 64% investigated total knee and total hip arthroplasty, whereas 90% of studies investigated the expectations of patients, 5.6% investigated the expectations of physicians, and 4.4% investigated both. Of all studies, 72% utilized either study‐specific instruments with close‐ended, Likert‐type response formats or modifications of existing expectations questionnaires. Most studies focused on desirable, nontimeline‐related, treatment outcome expectations. Many studies aggregated multiple expectation results into a single score.
Conclusion
Adopting the standardized framework for expectations presented in this study will foster clearer communication and permit researchers to aggregate results across studies.
Introduction
Musculoskeletal disorders are among the most important contributors to global disability 1. In the US alone, direct and indirect costs of musculoskeletal disorders have been estimated to be $961.6 billion in 2016 USD 2, 3, 4, 5. Given the chronic nature of many of these conditions, their prevalence will grow as populations age. For many of these conditions, elective orthopedic surgical treatment provides effective intervention.
As orthopedic surgical utilization has increased, investigators have examined predictors of orthopedic surgical outcomes, focusing largely on technical factors, such as surgical approach, and clinical factors, such as functional status, comorbidity, and preoperative pain. Increasingly, investigators have also considered the effects of psychosocial factors, such as depression, pain catastrophizing, and expectations 6, 7, 8, 9, on surgical outcome. Literature on associations between expectations and outcomes is limited by lack of uniformity in how expectations are defined, conceptualized, and measured 9, 10, 11. The resulting heterogeneity hampers effective communication among investigators and may preclude aggregation of study results in meta‐analyses 12, 13.
The striking variability in studies of expectations within orthopedic outcomes research is partly explained by the large number of expectation types, each drawing from distinct theoretical frameworks. For example, some authors use the word “expectations” to denote a patient's estimation of the likelihood of reducing their pain as a result of surgery 14, whereas other authors use the word to refer to a patient's beliefs that they will see improvement in walking without assistance 15 or to a patient's overall sense of optimism and pessimism 16. In their 2017 review, Laferton et al integrated the most relevant theoretical concepts into a model of patients’ expectations of medical treatment 17. By developing a standardized, operationalizable system of classifying expectation concepts, their work facilitates analysis across different studies and serves as a theoretical framework for future work investigating expectations.
In order to characterize what authors actually mean when they purport to measure expectations in orthopedic surgical research, we performed a scoping review. A scoping review is designed to map the extent and types of research done on a particular topic and to identify gaps in the literature. The objective of this scoping review is to build on the foundation set forth by Laferton et al 17 and provide an adapted conceptual framework for understanding the construct of expectations and its derivatives (ie, expectation, expectancy, expectancies, etc) in studies of elective surgical orthopedic procedures. In doing so, we hope our work will help clinicians and clinical investigators better interpret articles that use the term “expectations” as well as serve as a guide for choosing appropriate expectations assessment tools. We will also utilize our adaptation of Laferton's framework to map the current orthopedic surgery literature on expectations, highlighting its strengths, weaknesses, and gaps.
Materials and Methods
Study design
Unlike traditional systematic reviews, which address relatively narrow questions, scoping reviews can be used to provide a broad overview of a particular topic 18. As the available literature continues to grow, this review method is increasing in popularity because it provides a descriptive overview of the extent of the literature in a given field, its gaps, and the conceptual or disciplinary approaches that authors have taken. The framework for this scoping review was based, in part, on the Joanna Briggs Institute's methodology for conducting scoping reviews 19, which draws on the framework first presented by Arksey and O'Malley 18 and later enhanced by Levac et al 20. A review protocol for this specific study does not currently exist.
Defining expectations
Throughout this manuscript, we refer to the term expectations as outlined in Laferton's work—future‐directed beliefs concerning the probability that an experience or event will occur 17. Within this framework, expectations are anticipatory cognitions (“predictive expectations”) and are distinguished from constructs such as ideal expectations (ie, what an individual wants/hopes to occur), normative expectations (ie, what an individual believes should occur), value expectations (ie, the importance an individual attributes to a result), and fantasies (ie, images of future desires) 21, 22, 23.
Adaptation of Laferton's model of expectations
Laferton's model consolidates the most medically relevant theoretical ideas on expectations into an integrative model of expectations of patients undergoing medical treatment 17. Some of these theories include the social learning and social cognitive theories, the response expectance theory, and the common sense model of illness representation 24, 25, 26, 27. We build on this foundational framework and provide an adaptation of Laferton's original model of expectations. Within our adaptation, expectations can be generalized, or they can relate to a patient's illness/treatment‐related behavior or the treatments the patient is receiving. These three major expectation concept types are further defined into more precise subconcepts. The nesting of each expectation concept type within our adaptation is shown in Figure 1, whereas a more detailed description for each is found below. Examples of each expectation concept type can be found in Table 1.
Figure 1.
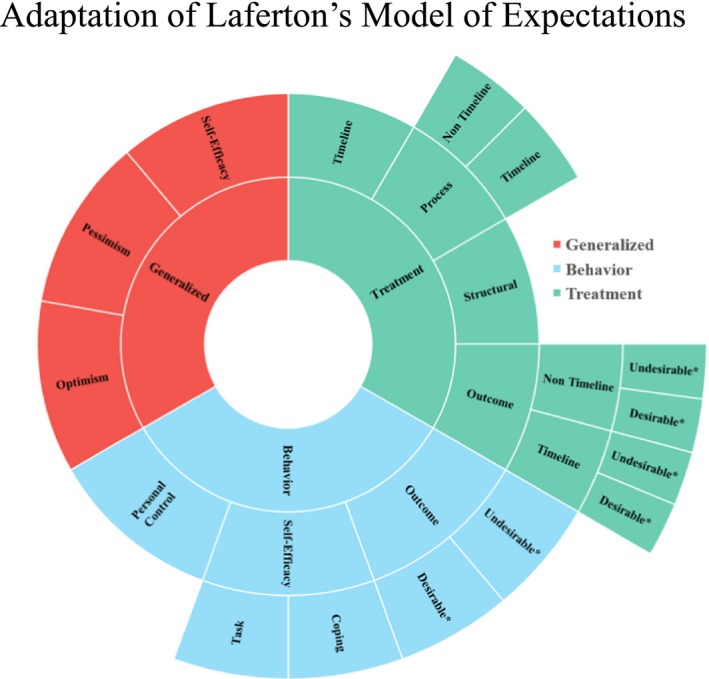
Sunburst representation of the adaptation of Laferton's model of expectations. *Can be further classified into internal, external, function/quality of life, and general outcomes.
Table 1.
Expectation concept types with examples
| Expectation Concept Type | Expectation Concept Examplea |
|---|---|
| Generalized | Examples |
| Self‐Efficacy | ‘I am confident I will be able to handle whatever comes my way no matter the circumstances’; ‘I am certain I can get through whatever challenge I come across in any circumstance’; ‘I believe I can do anything no matter the scenario |
| Optimism | ‘Things will work out my way’; ‘In uncertain times, I usually expect the best’; ‘There will always be reasons for life to be worth living |
| Pessimism | ‘Things will not work out my way’; ‘If something can go wrong for me, it will’; ‘Things will always come up and ruin my day |
| Behavior | Examples |
| Personal Control | ‘No matter what I do, or how hard I try, I just can't seem to get relief from my pain’; ‘I will be able to exercise but it will not affect my pain’; ‘Getting surgery will remove the control my leg pain has on my life’ |
| Self‐Efficacy, Task | ‘I am not very confident I can perform the required exercise when I am feeling tired after a long day at work’; ‘I am 100% certain I can manage my finances after surgery throughout the recovery process’; ‘I am extremely confident I can take my anticoagulation medication every day after dinner’ |
| Self‐Efficacy, Coping | ‘I am certain I can endure the physical pain that can accompany exercising after surgery’; ‘I cannot overcome the frustrations of having less arm mobility when grocery shopping’; ‘I can deal with the discomfort of wearing a neck brace’ |
| Outcome, Benefit (General) | ‘Exercising after surgery will improve my recovery’; ‘Stretching will make my hip better’; ‘Following what the doctor tells me will result in things going well’ |
| Outcome, Benefit (Internal) | ‘If I reach out to people for help during my surgical recovery, I will feel less stressed’; ‘If I exercise after surgery, I will have less pain’; ‘Maintaining a healthy lifestyle will keep me from worrying about my shoulder’ |
| Outcome, Benefit (Fxn/QoL) | ‘If I follow my doctor's post‐operative instructions, I will be able to return to sports’; ‘Going back to work after surgery will improve my quality of life’; ‘If I play sports I will improve my knee mobility’ |
| Outcome, Benefit (External) | ‘Doing what the doctor says will make my wife happy’; ‘After surgery, I will be able to grocery shop, which will reduce my husband's stress’; ‘If I continue to lose weight, my doctor will think I am taking my recovery seriously’ |
| Outcome, Side Effect (General) | ‘Not exercising after surgery will slow my recovery’; ‘Continuing to run will make my knees worse’; ‘Smoking will worsen my health’ |
| Outcome, Side Effect (Internal) | ‘If I continue to smoke, I will probably have a heart attack’; ‘If I forget to take my anticoagulation medication post‐operatively, I will get a clot’; ‘If I worry too much, my pain will not go away’ |
| Outcome, Side Effect (Fxn/QoL) | ‘Not moving my arm will decrease my range of motion’; ‘If I continue to run on my knees when they hurt, I will eventually end up in a wheelchair’; ‘If I continue to live an unhealthy life, I will not be able to play with my grandkids’ |
| Outcome, Side Effect (External) | ‘I will probably get fired if I take time off work’; ‘If I ask for pain medication too often, the doctor will think I am addicted’; ‘If I am not careful when walking after surgery, my knee replacement will break’ |
| Treatment | Examplesb |
| Outcome, Nontimeline, Benefit (General) | ‘I expect a lot of improvement in my recovery as a result of physical therapy’; ‘The cortisone shot will make things better’; ‘Surgery will improve my health’ |
| Outcome, Nontimeline, Benefit (Internal) | ‘I expect the knee replacement will relieve my knee pain’; ‘The numbness in my hands will improve as a result of my surgery’; ‘Surgery will make me feel happier’ |
| Outcome, Nontimeline, Benefit (Fxn/QoL) | ‘Surgery will improve my ability to dance’; ‘I expect surgery will allow me to throw a ball’; ‘I will be able to go back to work because of my surgery’ |
| Outcome, Nontimeline, Benefit (External) | ‘Surgery will reduce my wife's stress’; ‘My friends will invite me to play golf more if I have surgery’; ‘People won't have to help me if I have the surgery’ |
| Outcome, Nontimeline, Side Effect (General) | ‘Physical therapy will make my knee worse’; ‘My health will worsen as a result of my surgery’; ‘Surgery will ruin my life’ |
| Outcome, Nontimeline, Side Effect (Internal) | ‘I expect to have a lot of post‐surgical pain’; ‘I expect to have nausea as a result of taking the anti‐inflammatory medication’; ‘I expect to gain unhealthy weight as a result of the cortisone shots’ |
| Outcome, Nontimeline, Side Effect (Fxn/QoL) | ‘Surgery will prevent me from playing sports’; ‘Surgery will limit my movements at work’; ‘I will not be able to go to class because of my surgery’ |
| Outcome, Nontimeline, Side Effect (External) | ‘I expect to lose my job as a result of my surgery’; ‘My income will go down because of my back surgery’; ‘If I have a knee replacement, my friends will think I am weak’ |
| Outcome, Timeline, Benefit (General) | ‘It will take 2 months to fully recover from surgery’; ‘I will be better in 3 weeks’; ‘My health will improve two weeks after the surgery’ |
| Outcome, Timeline, Benefit (Internal) | ‘I expect it will take 3 weeks for the cortisone shot to reduce my pain’; ‘I expect it will be 3 months until radiation improves my back pain’; ‘I expect it will take 30 minutes for the pain medication to take away my pain’ |
| Outcome, Timeline, Benefit (Fxn/QoL) | ‘I expect I will be able to walk up and down the stairs in 2 days’; ‘I expect to be able to run in 2 months’; ‘I expect I will be able to play sports in 6 months’ |
| Outcome, Timeline, Benefit (External) | ‘I expect my friends will start inviting me to play golf more within a month of having recovered’; ‘My wife will be less stressed immediately after my surgery’; ‘My children will stop treating me like a cripple within a month of surgery’ |
| Outcome, Timeline, Side Effect (General) | ‘My health will decline 2 months after my surgery’; ‘Physical therapy will make my knee worse within a month’; ‘My life will be ruined immediately after my surgery’ |
| Outcome, Timeline, Side Effect (Internal) | ‘I expect the post‐surgical pain will last for 2 days after surgery’; ‘I expect to feel nauseous for no more than 1 day after surgery’; ‘I expect I will have numbness for less than 1 week’ |
| Outcome, Timeline, Side Effect (Fxn/QoL) | ‘I will not be able to play sports for 6 months because of my surgery’; ‘I will not be able to wear the shoes I like for 3 weeks after my procedure’; ‘I will not be able to write with my right hand for 2 days after surgery’ |
| Outcome, Timeline, Side Effect (External) | ‘I expect to lose my job immediate after surgery’; ‘I expect my son will think of me as fragile for at least 6 months after surgery’; ‘If I have a knee replacement, my friends will always think I am weak’ |
| Structural | ‘I expect to be given better care at a large hospital than a small hospital’; ‘Surgeries performed by residents will result in more complications’; ‘I expect a doctor will be able to diagnose my condition more effectively than a physician assistant’ |
| Process, Nontimeline | ‘I expect the doctor will only let me go home after surgery if I have zero pain’; ‘I expect to go home, and not a rehab facility, at discharge’; ‘I expect to be given post‐surgical instructions’ |
| Process, Timeline | ‘I expect to be in the hospital for 6 days after my surgery’; ‘I expect the doctor will see me for 30 mins every morning’; ‘I expect the doctor will come see me within an hour after the surgery’ |
| Timeline | ‘I expect my knee replacement will last 30 years’; ‘I expect the stitches will disintegrate after 2 weeks’; ‘I expect the nails will never be replaced’ |
Abbreviation: Fxn/QoL, function/quality of life. aThese examples (developed by authors of this review) are a patient's expectations, but they can be rephrased to be those of a spouse, family member, friend, health care professional or any other individual associated directly or indirectly with the patient or their care. bAll treatment outcome expectation examples (developed by authors of this review) refer to the expectations of certain outcomes resulting from a treatment, irrespective of whether it is explicitly stated by the example (examples reflect what an individual would express when asked a question—”As a result of your surgery when do you expect to be able to walk up and down stairs?”
Generalized expectations, unlike specific expectations that apply to a narrow context (eg, total knee replacement surgery), are expectations that apply to an unlimited number of contexts (eg, life as a whole). These generalized expectations can be divided into optimism, pessimism, and generalized self‐efficacy. Optimism refers to an individual's disposition to hold positive expectations for their future, whereas pessimism refers to an individual's inclination toward negative expectations. Though Laferton's original model includes the concept of optimism and not pessimism, we chose to include the concept of pessimism in our adapted model because there exists evidence in the orthopedic literature to suggest that these are two distinguishable concepts 16. Finally, generalized self‐efficacy refers to an individual's personal judgement about their generalized competencies (eg, “handling whatever comes my way”) and their ability to exercise such competencies in generalized situations and domains (eg, “no matter the circumstances”).
A patient's illness/treatment‐related behavior expectations consist of self‐efficacy, behavior outcome expectations, and personal control expectancies. Self‐efficacy is further categorized as task self‐efficacy and coping self‐efficacy. Task self‐efficacy refers to the perceived ability to carry out a behavior, whereas coping self‐efficacy refers to the perceived ability to manage and cope with the demands that might arise when performing such a behavior. Behavior outcome expectations, defined as the expectations of an outcome resulting from a behavior, are classified as either desirable expectations (ie, an outcome generally accepted as being positive) or undesirable expectations (ie, an outcome generally accepted as being negative), and refer to a range of outcomes from internal (eg, symptoms, autonomic functions, psychological states, specific health conditions, etc) to external (eg, reactions of an individual's environment such as a spouse/family member or income potential). Outcomes that are neither exclusively internal nor external (eg, conducting or managing activities of daily living or specific tasks, performing sports, returning to work, quality of life, disability, mobility of a limb joint, etc) are labeled Fxn/QoL (for Function/Quality of Life). We specifically used the term “function” in our adaptation as it is a critical outcome considered in orthopedic interventions. In addition, nondescript, nonspecific outcomes (eg, general health state) are classified as general. The term “general” was also included in our adapted model because it is a common outcome type measured in orthopedics. Lastly, personal control expectancy refers to the combination of both behavior outcome expectations and self‐efficacy—the belief that “certain behaviors will allow one to control what one wants to control” (behavior outcome expectations) and “that one can enact those behaviors” (self‐efficacy) 28. Of note, the terms “desirable” and “undesirable” in our adaptation of Laferton's model of expectations replace the terms “benefit” and “side effect,” respectively, of Laferton's original model. We believe these new terms offer a more accurate and precise description of the intended concepts (eg, having to miss work because of surgery is better described as an “undesirable” outcome than a “side effect” of surgery) and avoid the negative connotations associated with the term “side effect” (eg, weight loss might be a side effect of a particular drug, yet be a desirable outcome for the patient). Treatment expectations, similar to the structure set forth by Donabedian for modeling the assessment of quality of care 29, consist of treatment structural expectations (eg, expectations that treatment differs between settings—community vs. teaching hospitals), treatment process expectations (eg, frequency of physical therapy), and treatment outcome expectations (eg, pain relief). In addition to these three categories, our adaptation of Laferton's model includes treatment timeline expectations (ie, expectations regarding inherent time characteristics of a treatment that are not tied to the structure, process, or outcome of the treatment) as a type of treatment expectations. This type of expectation (which would include, for example, how long a patient expects an implant to last), was not covered under the original model but is particularly important in orthopedic surgery. In our adapted model, both treatment process expectations and treatment outcome expectations can be further classified into timeline vs. nontimeline expectations. A designation of timeline is given if time is the dependent variable in the expectation (eg, “It will take 6 months until I am pain free,” an answer to the question “How long do you expect it will take after surgery to be pain free?”). If a treatment outcome expectation has no time component or if the time component of the expectation is not the dependent variable, the expectation is labeled as nontimeline (eg, “At 6 months I will be in moderate pain,” an answer to the question “In how much pain will you be in at 6 months?”). Though Laferton's original model includes timeline expectations as a factor applicable across concepts, we chose to designate the labels of timeline and nontimeline only to those expectations for which a time component is a relevant factor in orthopedics. In addition, by providing these labels, we were able to not only explicitly represent the granularity found within expectation types but were able to highlight the nuances one might encounter when operationalizing expectations into the various types. Finally, treatment outcome expectations, like behavior outcome expectations, are either desirable or undesirable and refer to outcomes that can be classified as general, internal, Fxn/QoL, or external.
Operationalization of expectations
We operationalized each study's individual expectation measurement items into one of the expectation concepts within the adaptation of Laferton's model of expectations (Figure 1). Though Laferton's original model centered around patients’ expectations, we utilized our model to also operationalize the expectations of physicians, other health care providers, spouses, family members, and friends.
Orthopedic surgery procedures included
We focused on representative elective orthopedic surgeries that covered the body's major regions (upper extremity, lower extremity, spine). We included total knee arthroplasty, total hip arthroplasty, anterior cruciate ligament repair, correction of hallux valgus, total shoulder arthroplasty, rotator cuff repair, carpal tunnel release, laminectomy/discectomy, and spinal fusion.
Eligibility criteria
Studies were included if 1) they were peer‐reviewed articles; 2) they explicitly mentioned measuring expectations or its derivatives in the title or abstract; 3) the measured expectations were explicitly labeled as “expectations” or another of its derivatives within the full text; 4) the measured expectations were predictive expectations; 5) authors measured expectations in the context of our selected orthopedic procedures (primary, revision, or both); 6) the questions/surveys were available for inspection or the expectations questions were clearly stated in the text and the response categories were available for inspection; 7) the participants were at least 18 years old; 8) the article was published in 1980 or later.
We did not exclude studies based on their country of origin or the language they were written in. We considered “meeting expectations” or “fulfilling expectations” as outcomes and not as expectations and thus excluded studies that only included meeting/fulfilling expectations. We did not include published abstracts, reviews, commentaries, or editorials.
Data sources, search strategies, and study selection
We searched four databases (MEDLINE, Embase, CINAHL, and Web of Science) in conjunction with an expert reference librarian. Full search terms used can be found in Appendix 1. Date of the last search was September 2017.
We implemented a two‐stage screening process to determine eligibility. We first screened the titles and abstracts of the retrieved studies for those that explicitly mentioned measuring expectations or its derivatives in the context of one or more of our selected surgeries. The full‐texts of those articles were then analyzed to determine final inclusion using the previously mentioned eligibility criteria. One reviewer (AC) performed the two‐stage screening process for 100% of the retrieved articles, whereas a second reviewer (SM) independently completed the same process on a random 10% sample. Cohen's κ, a measure of interreviewer reliability, was calculated to be 0.94, indicating almost perfect agreement between authors on whether studies were indeed eligible.
Data extraction
We operationalized each study's individual expectation measurement items into one of the expectation concepts found within the adaptation of Laferton's model of expectations (Figure 1). We also extracted the type of expectations measurement tool (eg, existing expectations questionnaire), the name of the tool (eg, Hospital for Special Surgery [HSS] Cervical Spine Surgery Expectations Survey), whose expectations were measured (eg, patient, physician, spouse, etc), and descriptive information (ie, type of surgical procedure, publication date, study population's country of origin, and study type). We managed the data with a REDCap database hosted at Brigham and Women's Hospital 30. We used a two‐person strategy for extracting the data, with one author (AC) extracting data from 100% of the included studies and a second author (SM) extracting data from a random 10% sample of studies. The interreviewer agreement on how each study's individual expectation measurement items were operationalized into our expectations model was very high, with Cohen's κ = 0.97.
No formal assessment of the methodological quality of the included studies was performed because the aim of the scoping review was to provide a map of current published work on expectations, rather than synthesizing the best available evidence to answer a specific question. This approach is consistent with the Joanna Briggs Institute's methodology for conducting scoping reviews 19.
Results
Study selection
The literature search revealed a total of 4089 studies: 1166 studies from MEDLINE, 1293 from Embase, 466 from CINAHL, and 1164 from Web of Science (Figure 2). Of these, 1974 duplicates were excluded. An additional 1615 studies were excluded after their titles and abstracts were screened. Five hundred full‐text articles were analyzed for eligibility criteria, of which 90 were included in the scoping review (references can be found in Appendix 2). Notably, 83 of the 500 full‐text articles were excluded because the expectations evaluated did not align with our definition. These expectations were either fantasies, ideal expectations, normative expectations, or value expectations.
Figure 2.
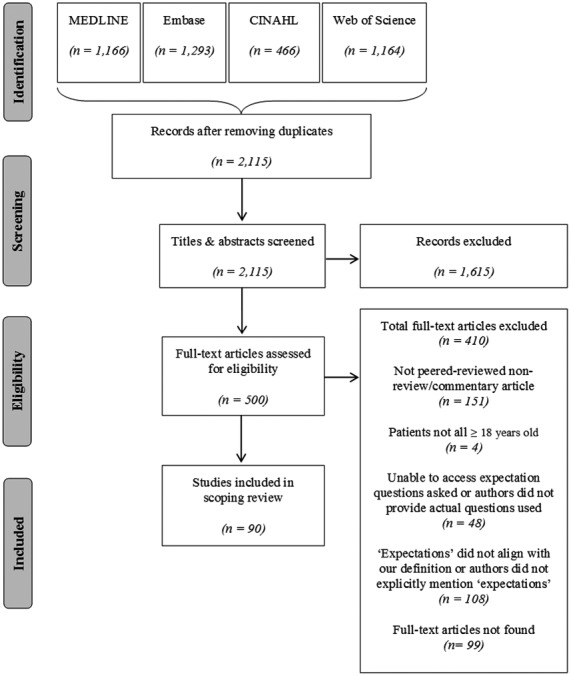
Flowchart presenting the scoping review process.
Temporal and geographic study characteristics
Each of the 90 studies included was published between 1996 and 2017 (Figure 3), with 70% being published after 2008. Most studies (58 of 90, 64%) investigated total knee or total hip arthroplasty, followed by spine surgery (20%), rotator cuff repair (10%), hallux valgus correction (3.3%), and carpal tunnel release (2.2%). Our search did not retrieve any eligible studies of total shoulder arthroplasty or anterior cruciate ligament repair.
Figure 3.
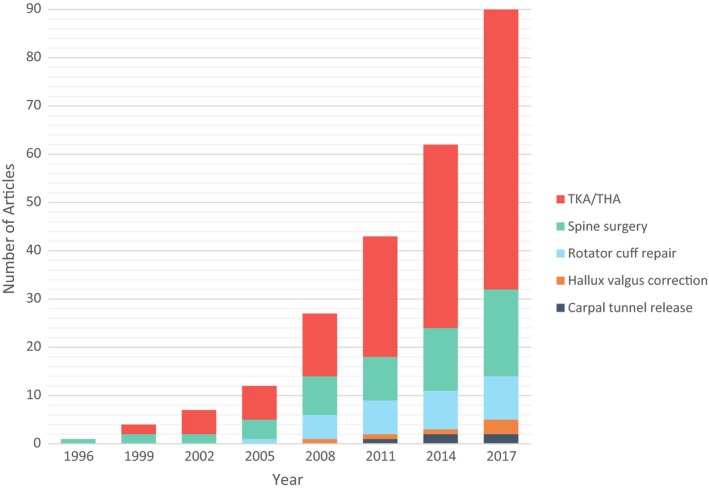
Flowchart presenting the scoping review process.
Single‐country studies were far more common than multiple‐country studies (94% vs. 5.6%) (Table 2). Over half (54%) of single‐country studies explored expectations of North American populations, with another 31% from Europe, 12% from Asia, and 3.5% from Australia. The countries with the most single‐country studies were the United States, Canada, and the Netherlands (34, 10, and 6 studies, respectively). Two of the five multiple‐country studies compared expectations across continents.
Table 2.
Geographical origin for population of included studies
| Location | Study Number | % of Total (N = 90) |
|---|---|---|
| Single‐country studies | 85 | 94 |
| North America | 46 | 51 |
| USA | 34 | 38 |
| Canada | 10 | 11 |
| Dominican Republic | 2 | 2.2 |
| Europe | 26 | 29 |
| Netherlands | 6 | 6.7 |
| UK | 5 | 5.6 |
| Spain | 4 | 4.4 |
| Sweden | 4 | 4.4 |
| Belgium | 2 | 2.2 |
| Germany | 2 | 2.2 |
| Switzerland | 2 | 2.2 |
| France | 1 | 1.1 |
| Asia | 10 | 11 |
| Japan | 4 | 4.4 |
| South Korea | 2 | 2.2 |
| India | 1 | 1.1 |
| Iran | 1 | 1.1 |
| Israel | 1 | 1.1 |
| Turkey | 1 | 1.1 |
| Australia | 3 | 3.3 |
| Australia | 3 | 3.3 |
| Multiple‐Country Studies | 5 | 5.6 |
| EUROHIPa | 2 | 2.2 |
| 89 Country Studyb | 1 | 1.1 |
| USA, Canada | 1 | 1.1 |
| USA, UK, Australia | 1 | 1.1 |
aEUROHIP Cohort: Austria, Switzerland, Germany, Hungary, Poland, Spain, Italy, France, Sweden, Iceland, Finland, UK. bStudy included countries from six continents: North America, South America, Europe, Asia, Africa, Australia.
Expectation measurement tool format and scoring algorithm types
Of the 90 included studies, only 19 (21%) utilized existing expectations questionnaires (Table 3). Of these, over half (12 of 19, 63%) used either the Musculoskeletal Outcomes Data Evaluation and Management System (MODEMS) survey or a translation of the New (2011) Knee Society Score (KSS) survey (see Appendix 4 for citations). The most popular formats for assessing expectations were study‐specific, close‐ended, Likert‐type response surveys (45 of 90, 50%) and modifications of existing expectations questionnaires (20 of 90, 22%). Modified versions of the HSS Knee and Hip Replacement Expectation surveys were used in 17 out of 20 studies (85%) that used modified existing expectations questionnaires (see Appendix 4 for citations). Study‐specific, open‐ended questions were used by the least number of studies (8 of 90, 8.9%).
Table 3.
Expectations measurement tool format and scoring algorithm types
| Expectations Measurement Tool Format | Study Numbera | % of Total (N = 90) |
|---|---|---|
| Study‐specific (close‐ended, Likert‐type responses) | 45 | 50 |
| Study‐specific (open‐ended) | 8 | 8.9 |
| Existing expectations questionnaires | 19f | 21 |
| HSS Cervical Spine Surgery Expectations Survey | 1d | 1.1 |
| HSS Foot & Ankle Surgery Expectations Survey | 2d | 2.2 |
| HSS Lumbar Spine Surgery Expectations Survey | 1d | 1.1 |
| Japanese translation of the New (2011) KSS | 2d | 2.2 |
| The New (2011) KSS | 2d | 2.2 |
| Korean translation of the New (2011) KSS | 1d | 1.1 |
| French translation of the New (2011) KSS | 1d | 1.1 |
| Life Orientation Test‐Revised (LOT‐R) | 2d | 2.2 |
| Musculoskeletal Outcomes Data Evaluation and Management System (MODEMS) | 6d | 6.7 |
| Patient Reported Fulfillment of Expectation (PROFEX) | 1d | 1.1 |
| Postvisit Questionnaire of Patient Expectations of Healthcare | 1d | 1.1 |
| Credibility Expectancy Questionnaire (CEQ) expectancy subscale | 1d | 1.1 |
| Arthritis Helplessness Index | 1d | 1.1 |
| Modified existing expectations questionnaires | 20f | 22 |
| Modified version of the HSS Knee Replacement Expectations Survey | 16b , d | 18 |
| Modified version of the HSS Hip Replacement Expectations Survey | 11c , d | 12 |
| German translation for modified version of the New (2011) KSS | 1d | 1.1 |
| Modified version of the Total Hip Arthroplasty Outcome Evaluation Questionnaire | 1d | 1.1 |
| Scoring Algorithm Types | Study Numbera | % of Total (N = 82e) |
|---|---|---|
| Separate Score for Each Expectation Concept | 41 | 50 |
| Single Aggregated Score | 34 | 41 |
| Separate Score for Each Expectation Concept & Single Aggregated Score | 7 | 8.5 |
Abbreviation: HSS, Hospital for Special Surgery; KSS, Knee Society Score. aStudies can include multiple tool formats and scoring algorithm types; bIncludes two studies of the French translation and two studies of the Dutch translation; cIncludes two studies of the French translation and two studies of the Dutch translation; dSee Appendix 4 for citations; eTotal of 82 studies because 8 studies did not score expectations (qualitative studies); fNot the sum of individual questionnaires because single studies can have multiple questionnaires (two studies used two existing expectations questionnaires; 10 studies used 2 modified existing expectations questionnaires).
Information on the type of scoring algorithm used by the included studies can also be seen in Table 3. Most studies (82 of 90, 91%) reported expectations quantitatively. Each expectation item could either be scored independently, aggregated with other expectation items into a single score, or both. Fifty percent (41 of 82) of the studies treated each expectation independently (15 of these were single‐item studies), 41% (34 of 82) aggregated multiple expectation items into a single score, and 8.5% (7 of 82) did both. Expectation items were aggregated in 61% of studies (41 of 67) that had more than a single item.
Study type and expectations source
The studies in this review included several designs (Table 4). More than half (48 of 90, 53%) were cohort studies, 27% (24 of 90) were cross‐sectional, and 4.4% (4 of 90) were randomized control trials (one trial also had a cohort component). Another 10% (9 of 90) were survey development and validation studies, and 5.6% (5 of 90) were qualitative studies.
Table 4.
Study type and source of expectations for included studies
| Study Type | Study Number | % of Total (N = 90) |
|---|---|---|
| Observational (analytical) | 72 | 80 |
| Cohort | 48 | 53 |
| Cross‐sectional | 24 | 27 |
| Observational (descriptive) | 14 | 16 |
| Survey development & validation | 9 | 10 |
| Qualitative | 5 | 5.6 |
| Experimental | 3 | 3.3 |
| RCT | 3a | 3.3 |
| Mixed | 1 | 1.1 |
| Combination Cohort + RCT | 1 | 1.1 |
| Whose Expectations Measured | Study Number | % of total (N = 90) |
|---|---|---|
| Patient | 81 | 90 |
| Physician | 5 | 5.6 |
| Patient & Physician | 4 | 4.4 |
Abbreviation: RCT, randomized control trial. aOne study investigated the extent that intervention modified expectations.
Most studies (81 of 90, 90%) investigated the expectations of patients, whereas 5.6% (5 of 90) studied the expectations of physicians and 4.4% (4 of 90) studied both (Table 4). None addressed expectations of other health care providers, family members, or patients’ friends.
Expectation concepts
All 90 studies evaluated treatment expectations. Several of these studies also evaluated additional types of expectations. Two evaluated generalized expectations, and one evaluated illness/treatment‐related behavior expectations. Detailed information about the number of studies (by surgery type) that examined each of the expectation concept types within the adaptation of Laferton's model of expectations can be found in Appendix 3.
Both studies that examined generalized expectations specifically measured optimism and pessimism. The single study that examined illness/treatment‐related behavior expectations specifically measured personal control, self‐efficacy (both coping and task), desirable general outcome expectations, and undesirable internal outcome expectations.
Treatment expectations were studied in all the included studies (Table 5). The three most commonly examined treatment expectations were nontimeline desirable Fxn/QoL outcome expectations (65 of 90, 72%), nontimeline desirable internal outcome expectations (61 of 90, 68%), and nontimeline desirable general outcome expectations (24 of 90, 27%). Of the studies that measured treatment outcome expectations (84 of 90, 93%), 90% (76 of84) studied nontimeline expectations, 2.4% (2 of 84) studied timeline expectations, and 7.1% (6 of 84) studied both timeline and nontimeline expectations. Most of the studies that measured treatment outcome expectations only measured desirable outcomes (86%, 72 of 84), whereas 3.6% (3 of 84) measured undesirable outcome expectations, and 11% (9 of 84) measured both desirable and undesirable expectations. In terms of outcome type among treatment outcome expectations, 9.5% of studies (8 of 84) measured general outcomes, 7.1% (6 of 84) measured internal outcomes, 9.5% (8 of 84) measured Fxn/QoL outcomes, 0% (0 of 84) measured external outcomes, and 74% (62 of 84) measured some combination of the four types.
Table 5.
Types of treatment expectation concepts
| Outcome Structural Process Timeline | Timeline/Nontimeline | Desirable/Undesirable | General Internal Fxn/QoL External | Study Numbera | % of Total (N = 90) |
|---|---|---|---|---|---|
| Outcome | Nontimeline | Desirable | General | 24 | 27 |
| Outcome | Nontimeline | Desirable | Internal | 61 | 68 |
| Outcome | Nontimeline | Desirable | Fxn/QoL | 65 | 72 |
| Outcome | Nontimeline | Desirable | External | 0 | 0 |
| Outcome | Nontimeline | Undesirable | General | 9 | 10 |
| Outcome | Nontimeline | Undesirable | Internal | 4 | 4.4 |
| Outcome | Nontimeline | Undesirable | Fxn/QoL | 0 | 0 |
| Outcome | Nontimeline | Undesirable | External | 0 | 0 |
| Outcome | Timeline | Desirable | General | 5 | 5.6 |
| Outcome | Timeline | Desirable | Internal | 1 | 1.1 |
| Outcome | Timeline | Desirable | Fxn/QoL | 1 | 1.1 |
| Outcome | Timeline | Desirable | External | 0 | 0 |
| Outcome | Timeline | Undesirable | General | 0 | 0 |
| Outcome | Timeline | Undesirable | Internal | 0 | 0 |
| Outcome | Timeline | Undesirable | Fxn/QoL | 1 | 1.1 |
| Outcome | Timeline | Undesirable | External | 0 | 0 |
| Structural | 1 | 1.1 | |||
| Process | Nontimeline | 3 | 3.3 | ||
| Process | Timeline | 2 | 2.2 | ||
| Timeline | 2 | 2.2 |
Abbreviation: Fxn/QoL, Function/Quality of Life. aNumber of studies sum to more than 90 because studies may include multiple types of expectation concepts.
The studies assessed a limited number of expectation concepts. Most studies (69 of 90, 77%) only investigated one or two expectation concept types, whereas 18% (16 of 90) investigated three types, 3.3% (3 of 90) investigated four, and 2.2% (2 of 90) investigated five or more.
Discussion
We performed a scoping review that conceptualized what authors mean when they claim to measure expectations in orthopedic surgical research. Our review also mapped the instruments utilized to measure such expectations, whose expectations were measured, the geographic origin for the studied populations, the studies’ publication dates, and their designs. We found that research on expectations in orthopedic surgery has expanded considerably in recent years. Contributions to this literature have been primarily from high‐income countries. Most studies investigated the expectations of patients, whereas a minority investigated the expectations of physicians. None of the studies investigated expectations of other health care providers, spouses and other family members, or patients’ friends. Most studies utilized either study‐specific instruments with close‐ended, Likert‐type response formats or modifications of existing expectations questionnaires. Of note, almost all the studies that used a modified version of an existing expectations questionnaire used modified versions of the HSS Knee and Hip Replacement Expectation surveys.
Though expectations have been shown to be associated with certain outcomes in orthopedic surgery 9, 10, 11, the aggregation of results across studies has been limited 12, 13. This has partly been a result of the large number of existing expectation types. In their 2017 review 17, Laferton et al proposed an integrative model of patients’ expectations in medical treatment, which created a standardized system to classify expectations concepts. In our review, we build on this work, and present an adaptation of Laferton's model. To the best of our knowledge, this is the first review that utilized such a model to characterize the use of the term “expectations” in the context of a wide range of orthopedic surgeries.
Several findings from our review merit highlighting. A large portion of studies aggregated multiple expectation results into a single score. Summing different expectations into a single score implies that each expectation measures a shared underlying construct. That assumption may be correct in many instances but it is not always tenable. For example, a patient may expect dramatic pain relief after total knee arthroplasty but little improvement in walking distance because they have other problems that limit their walking. Indeed, Venkataramanan et al reported in a study of revision knee arthroplasty that aggregating the scores from five different expectation concept types resulted in low internal consistency (Cronbach's α = 0.63), suggesting that these concepts did not represent the same underlying construct 31. In some instances, investigators may wish to examine the unique content of each item. For example, the hypothetical patient noted above may have high expectations of pain relief post total knee arthroplasty and low expectations of improvement in mobility. If we were to add these expectation results together into a single score, we would conclude that the patient has neutral expectations and would miss the opportunity to discuss with the patient whether the disparate expectations of pain and function are realistic. To summarize, we suggest that investigators consider carefully whether the unique findings from distinct expectations items are relevant to their research question, and they should ensure (using Cronbach's α, for example) that the items measure a unidimensional construct before aggregating.
We also found that the range of expectation concept types investigated across studies, as well as the dimensionality of expectations concepts within studies, is notably narrow. Though it is no surprise that we found a predominance of treatment expectations types within the studies, given our focus on surgical treatments, the types of treatment expectations addressed were limited. For example, we identified few studies of expectations on the timeline of treatment outcomes and the expectations of undesirable treatment outcomes. This may be a lost opportunity as the timeline of outcomes of elective surgeries (when patients will achieve particular milestones, such as pain‐free walking) and the likelihood of poor outcomes are important to patients.
The HSS Knee and Hip Expectations Surveys do a careful job in listing the range of expectations of patients undergoing surgery. Though these are popular tools, there are several important considerations. Both surveys aggregate the results of multiple expectations into a single score, and both offer limited heterogeneity in terms of types of expectation concepts addressed (eg, lack of timeline expectations, undesirable treatment outcomes expectations, etc). Finally, though the studies included in this review modified the HSS surveys to measure predictive expectations (ie, what individuals believe will occur), the original HSS surveys were developed and validated to measure value expectations (ie, the importance one puts on a specific outcome). These versions measure different things. For example, a patient may find walking 1 mile after surgery very important but consider it an unlikely outcome. Authors should consider carefully which of these very different concepts they wish to investigate, and they should explicitly state which version they choose to use. Of note, 23 out of the 83 studies that were excluded in the screening process because the expectations evaluated did not align with our definition were an HSS version that measured value expectations.
The findings of our study should be interpreted in the context of certain limitations. Our search strategy was designed to capture studies that explicitly mentioned in the title or the abstract “expectations” or its derivatives and thus could have missed studies that only mentioned expectations somewhere within the body of the article. In addition, expectation concepts such as self‐efficacy and personal control were only captured under our search strategy when handled in direct connection with the term “expectations” (or any of its derivatives). This likely resulted in biased frequency estimates for these expectation concepts. Also, though our review included common, representative elective surgeries, it did not include all existing elective orthopedic surgeries. Finally, though our adaptation of Laferton's model attempts to address and categorize the most relevant expectation concepts one would encounter within the field of orthopedics, it is possible that certain expectation concepts are not represented.
Moving forward, the distinct categorization of expectation concept types within the model presented in this manuscript will allow researchers to better describe their intent when measuring expectations. Adopting this standardized framework will foster clearer communication within the field and allow researchers to better aggregate results across studies. Future research is needed to examine empirically whether expectation measures developed according to the model we presented will perform better than existing tools. Researchers that wish to develop new expectation measurement tools should also consider incorporating a wider range of expectation concept types to provide a more complete understanding of the intricacies of expectations. Investigators should consider the consequences of aggregating expectation items. If the items measure different concepts, the summary score may obscure clinically important findings. By aggregating expectations into a single score, a health care provider loses the opportunity to identify and correct inaccurate expectations (such as an expectation that dislocation is vanishingly rare following total hip arthroplasty). Finally, as health care shifts toward systems that tie physician evaluations, incentives, and reimbursements to a patient's evaluation of results, discussion of patient expectations will become increasingly important. The framework of the model presented in this manuscript can provide clarity to such discussion.
Author Contributions
Mr. Cortes drafted the manuscript. All authors were responsible for revisions and approved the final version of the manuscript to be published.
Study conception and design
Cortes, Katz, Meints.
Acquisition of data
Cortes, Meints.
Analysis and interpretation of data
Cortes.
Supporting information
Appendix 1. Search strategy: database, terms
Appendix 2. Citations for included studies
Appendix 3. Heat map for expectation concept type by surgery type (% of total studies within surgical category)
Appendix 4. Expectations measurement tool citations for results
Acknowledgments
The authors would like to thank Dr. Bain for his invaluable assistance in developing the search strategy for this review.
This study was supported by National Institutes of Health T32 grant AR055885.
No potential conflicts of interest relevant to this article were reported.
References
- 1. Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990‐2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2163–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. The Burden of Musculoskeletal Diseases in the United States . Share of GDP. 2014. URL: http://www.boneandjointburden.org/2014-report/xe2/share-gdp#footnote1_jr4bjgk.
- 3. Agency for Healthcare Research and Quality . Medical Expenditure Panel Survey. 2017. URL: https://meps.ahrq.gov/about_meps/Price_Index.shtml. [PubMed]
- 4. U.S. Bureau of Economic Analysis . Personal Consumption Expenditures: Services: Health Care (DHLCRC1Q027SBEA). 2017. URL: https://fred.stlouisfed.org/series/DHLCRC1Q027SBEA.
- 5. Centers for Medicare and Medicaid Services . National Health Expenditure Accounts: Personal Health Care. 2017. URL: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical.html.
- 6. Ayers DC, Franklin PD, Trief PM, Ploutz‐Snyder R, Freund D. Psychological attributes of preoperative total joint replacement patients: implications for optimal physical outcome. J Arthroplasty 2004;19 Suppl 2:125–30. [DOI] [PubMed] [Google Scholar]
- 7. Dave AJ, Selzer F, Losina E, Usiskin I, Collins JE, Lee YC, et al. The association of pre‐operative body pain diagram scores with pain outcomes following total knee arthroplasty. Osteoarthritis Cartilage 2017;25:667–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lopez‐Olivo MA, Landon GC, Siff SJ, Edelstein D, Pak C, Kallen MA, et al. Psychosocial determinants of outcomes in knee replacement. Ann Rheum Dis 2011;70:1775–81. [DOI] [PubMed] [Google Scholar]
- 9. Mahomed NN, Liang MH, Cook EF, Daltroy LH, Fortin PR, Fossel AH, et al. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. J Rheumatol 2002;29:1273–9. [PubMed] [Google Scholar]
- 10. Gandhi R, Davey JR, Mahomed N. Patient expectations predict greater pain relief with joint arthroplasty. J Arthroplasty 2009;24:716–21. [DOI] [PubMed] [Google Scholar]
- 11. Gepstein R, Arinzon Z, Adunsky A, Folman Y. Decompression surgery for lumbar spinal stenosis in the elderly: preoperative expectations and postoperative satisfaction. Spinal Cord 2006;44:427–31. [DOI] [PubMed] [Google Scholar]
- 12. Zywiel MG, Mahomed A, Gandhi R, Perruccio AV, Mahomed NN. Measuring expectations in orthopaedic surgery: a systematic review. Clin Orthop Relat Res 2013;471:3446–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Haanstra TM, van den Berg T, Ostelo RW, Poolman RW, Jansma EP, Cuijpers P, et al. Systematic review: do patient expectations influence treatment outcomes in total knee and total hip arthroplasty? [review] [published erratum appears in Health Qual Life Outcomes 2013;11:72]. Health Qual Life Outcomes 2012;10:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Grayson CW, Warth LC, Ziemba‐Davis MM, Michael Meneghini R. Functional improvement and expectations are diminished in total knee arthroplasty patients revised for flexion instability compared to aseptic loosening and infection. J Arthroplasty 2016;31:2241–6. [DOI] [PubMed] [Google Scholar]
- 15. Harris IA, Harris AM, Naylor JM, Adie S, Mittal R, Dao AT. Discordance between patient and surgeon satisfaction after total joint arthroplasty. J Arthroplasty 2013;28:722–7. [DOI] [PubMed] [Google Scholar]
- 16. Haanstra TM, Tilbury C, Kamper SJ, Tordoir RL, Vliet Vlieland TP, Nelissen RG, et al. Can optimism, pessimism, hope, treatment credibility and treatment expectancy be distinguished in patients undergoing total hip and total knee arthroplasty? [research support]. PLoS One 2015;10:e0133730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Laferton JA, Kube T, Salzmann S, Auer CJ, Shedden‐Mora MC. Patients’ expectations regarding medical treatment: a critical review of concepts and their assessment. Front Psychol 2017;8:233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Social Res Methodol 2005;8:19–32. [Google Scholar]
- 19. Peters M, Godfrey C, McInerney P, Soares CB, Khalil H, Parker D. Methodology for JBI scoping reviews In: The Joanna Briggs Institute reviewers manual 2015. South Australia: The Joanna Briggs Institute; 2015. p. 3–24. [Google Scholar]
- 20. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bialosky JE, Bishop MD, Cleland JA. Individual expectation: an overlooked, but pertinent, factor in the treatment of individuals experiencing musculoskeletal pain. Phys Ther 2010;90:1345–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wright JG, Young NL, Waddell JP. The reliability and validity of the self‐reported patient‐specific index for total hip arthroplasty. J Bone Joint Surg Am 2000;82:829–37. [DOI] [PubMed] [Google Scholar]
- 23. Oettingen G, Mayer D. The motivating function of thinking about the future: expectations versus fantasies. J Pers Soc Psychol 2002;83:1198–212. [PubMed] [Google Scholar]
- 24. Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs (NJ): Prentice Hall; 1986. [Google Scholar]
- 25. Kirsch I. Response expectancy as a determinant of experience and behavior. American Psychologist 1985;40:1189–202. [Google Scholar]
- 26. Leventhal H, Meyer D, Nerenz D. The common sense representation of illness danger In: Rachman S, editor. Contributions to medical psychology. Oxford: Pergamon Press; 1980. p. 7–30. [Google Scholar]
- 27. Maddux JE. Expectancies and the social‐cognitive‐perspective: basic principles, processes, and variables In: Kirsch I, editor. How expectancies shape experience. Washington, DC: American Psychological Association; 1999. p. 17–39. [Google Scholar]
- 28. Gosselin JT, Maddux JE. Self‐efficacy In: Leary MR, Tangney JP, editors. Handbook of self and identity. New York: The Guilford Press; 2003. p. 198–224. [Google Scholar]
- 29. Donabedian A. The quality of care. How can it be assessed? [review]. JAMA 1988;260:1743–8. [DOI] [PubMed] [Google Scholar]
- 30. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Venkataramanan V, Gignac MA, Mahomed NN, Davis AM. Expectations of recovery from revision knee replacement. Arthritis Rheum 2006;55:314–21. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 1. Search strategy: database, terms
Appendix 2. Citations for included studies
Appendix 3. Heat map for expectation concept type by surgery type (% of total studies within surgical category)
Appendix 4. Expectations measurement tool citations for results


