Abstract
Objective
Racial/ethnic disparities in pain are well‐recognized, with non‐Hispanic blacks (NHBs) experiencing greater pain severity and pain‐related disability than non‐Hispanic whites (NHWs). Although numerous risk factors are posited as contributors to these disparities, there is limited research addressing how resilience differentially influences pain and functioning across race/ethnicity. Therefore, this study examined associations between measures of psychosocial resilience, clinical pain, and functional performance among adults with knee osteoarthritis (OA), and assessed the moderating role of race/ethnicity on these relationships.
Methods
In a secondary analysis of the Understanding Pain and Limitations in Osteoarthritic Disease (UPLOAD‐2) study, 201 individuals with knee OA (NHB = 105, NHW = 96) completed measures of resilience (ie, trait resilience, optimism, positive well‐being, social support, positive affect) and clinical pain, as well as a performance‐based measure assessing lower‐extremity function and movement‐evoked pain.
Results
Bivariate analyses showed that higher levels of psychosocial resilience were associated with lower clinical pain and disability and more optimal physical functioning. NHBs reported greater pain and disability, poorer lower‐extremity function, and higher movement‐evoked pain compared with NHWs; however, measures of psychosocial resilience were similar across race/ethnicity. In moderation analyses, higher optimism and positive well‐being were protective against movement‐evoked pain in NHBs, whereas higher levels of positive affect were associated with greater movement‐evoked pain in NHWs.
Conclusion
Our findings underscore the importance of psychosocial resilience on OA‐related pain and function and highlight the influence of race/ethnicity on the resilience‐pain relationship. Treatments aimed at targeting resilience may help mitigate racial/ethnic disparities in pain.
Keywords: disability, osteoarthritis, pain, race/ethnicity, resilience
Introduction
Osteoarthritis (OA) is the most prevalent joint disease and leading source of pain among adults, affecting more than 30 million individuals in the United States alone 1. Although OA can affect any diarthrodial joint in the body, the knee is the most frequently affected site 2, with approximately 14 million adults experiencing symptomatic knee OA and over half having advanced disease 3. In addition to being one of the principal causes of disability, knee OA is associated with lower psychological functioning, tremendous economic burden, and decreased quality of life 4, 5, 6.
Significance & Innovations.
In adults with knee osteoarthritis, higher levels of psychosocial resilience were associated with lower clinical pain, disability, and functional impairment.
Non‐Hispanic blacks reported greater pain and functional limitations than non‐Hispanic whites despite similar ratings of psychosocial resilience.
The associations between optimism, positive well‐being, and positive affect with movement‐evoked pain were differentially expressed across race/ethnicity, suggesting that positive psychosocial resources may contribute to racial/ethnic disparities in pain.
Racial/ethnic disparities in pain and disability are widely reported as non‐Hispanic blacks (NHBs) experience more frequent, severe, and disabling pain relative to non‐Hispanic whites (NHWs) 7, 8. Moreover, several studies have found that NHBs report greater experimental pain sensitivity to a number of quantitative sensory testing methods when compared with NHWs 8, 9. These effects also extend to OA, as NHBs experience higher rates of symptomatic and radiographic OA 10, 11, report greater average pain severity, and have higher levels of disability than NHWs 7, 11, 12, 13.
Although numerous psychosocial and clinical risk factors are suggested to contribute to these differences 12, 14, there is limited understanding of how positive resilience factors influence racial/ethnic disparities in pain and functioning. Resilience is broadly defined as a dynamic process promoting adaptation to adversity or severe stress 4, and there is an emerging literature supporting the protective nature that resilience has on chronic pain. Though resilience can be studied as a unitary measure, it can also be quantified in terms of the positive psychosocial factors that comprise it (eg, positive affect, social support, and optimism, among others). The studies that have explored resilience processes in OA have found higher levels of optimism and social support to be associated with decreased clinical and experimental pain 13, 15, greater life satisfaction 16, as well as lower depressive symptoms 16 and pain catastrophizing 15. Positive affect (ie, pleasant mood or emotion) is shown to be a strong predictor of lower daily clinical pain 17 and buffers against weekly elevations in negative affect during periods of increased pain and stress 18. Furthermore, a recent report found that trait resilience interacts with optimism to predict enhanced pain inhibition in individuals with knee OA 19.
Although these findings are promising and suggest that positive psychological constructs have the ability to modulate pain and associated symptoms, relatively little is known regarding the extent to which race/ethnicity differentially influences the resilience‐pain relationship. In the one study examining this, optimism was associated with greater endogenous pain inhibition in pain‐free adults; however, the strength of the relationship between optimism and pain modulation did not differ across participant ethnicity (ie, NHBs, NHWs, Asian Americans) 20. To the best of our knowledge, no studies have yet examined these interrelationships among individuals with chronic pain. Given the extensive literature recognizing variations in social and economic stressors, as well as differential patterns of pain coping across racial/ethnic groups 21, 22, it is reasonable to speculate that protective resilience factors known to mitigate the adverse effects of pain could also vary as a function of race/ethnicity. Understanding these differences may be particularly critical in terms of optimizing current pain treatments and reducing racial disparities in pain.
The primary aim of this study was to examine the associations between measures of psychosocial resilience (ie, trait resilience, optimism, positive well‐being, social support, positive affect), clinical pain, and functional performance among individuals with knee osteoarthritis. It was hypothesized that greater levels of psychosocial resilience would be associated with less clinical pain severity and higher functional performance. A secondary aim was to determine if race/ethnicity moderated the associations between resilience measures with self‐reported pain and functioning. Given the absence of previous research in this area regarding resilience, no a priori hypotheses were made.
Methods
Participants
This is a secondary data analysis of a larger, multisite (University of Florida, University of Alabama at Birmingham) study examining race/ethnic group differences in central pain processing among individuals with or at risk for knee OA (Understanding Pain and Limitations in Osteoarthritic Disease [UPLOAD‐2]) 19. Individuals (N = 201) aged 45 and older who self‐identified as non‐Hispanic and “Black/African American” or “White/Caucasian/European” were recruited from the community via posted fliers, radio and print media announcements, orthopedic clinic recruitment, and word‐of‐mouth referral. All participants provided written informed consent and were compensated for their involvement.
Procedures
All procedures were approved by the University of Florida and University of Alabama Institutional Review Boards. Participants’ eligibility for study inclusion was determined through a telephone screening. The following sociodemographic and physical health data were acquired as part of the screening: self‐reported sex, age, ethnic/racial identity, and a brief health history including symptoms of knee OA. Participants were included if they were between the ages of 45 and 85 years and screened positive for clinical knee OA 23. This screening questionnaire showed 87% sensitivity and 92% specificity for radiographically confirmed symptomatic knee OA 24. Given widespread variability in definitions of OA, we adopted this approach to be as inclusive as possible in recruitment, as our primary focus was on understanding factors associated with knee pain rather than OA pathophysiology itself. Moreover, because this study was designed to evaluate progression of OA‐related symptoms, we wished to enroll a cohort with a broad range of OA characteristics, from very early signs to more advanced disease. Exclusion criteria included the following conditions: 1) prosthetic knee replacement or other clinically significant surgery to the arthritic knee; 2) heart disease, congestive heart failure, or history of acute myocardial infarction; 3) peripheral neuropathy; 4) systemic rheumatic disorders, including rheumatoid arthritis, systemic lupus erythematosus, and fibromyalgia; 5) chronic daily opioid use; or 6) hospitalization within the preceding year for psychiatric illness.
Participants who met the initial study inclusion criteria completed a health assessment session approximately 1 to 2 weeks later. During this session, health history was collected and a Short Physical Performance Battery (SPPB) test 25 was conducted. Height and weight were documented for measurement of body mass index (BMI). Furthermore, all individuals completed a bilateral knee joint evaluation by the study's rheumatologists or nurse practitioners and were classified as either having, or being at risk for, knee OA. After the health examination, participants completed questionnaires on self‐reported knee pain symptoms and measures of resilience.
Measures
Brief Resilience Scale
The Brief Resilience Scale (BRS) 26 is a six‐item questionnaire that examines the ability to bounce back and recover from stress. Each item ranges from 1 (strongly disagree) to 5 (strongly agree), with higher scores indicative of greater psychological resilience. The BRS demonstrates good reliability and validity, with adequate internal consistency noted in the present sample (α = 0.81).
Life Orientation Test–Revised
As a measure of dispositional optimism, participants completed the Life Orientation Test–Revised (LOT‐R), which consists of six items (including four filler items not included in the calculation) to assess generalized positive expectancies. Items were rated on a five‐point scale ranging from 0 (strongly disagree) to 4 (strongly agree), with higher scores signifying greater optimism. The LOT‐R has good internal validity, test‐retest reliability, and convergent and discriminant validity 27. Internal consistency for the sample was adequate (α = 0.77).
Positive Affect and Well‐Being–Short Form
The Neuro‐QOL Positive Affect and Well‐being (PAW) Short Form 28 is a nine‐item questionnaire reflecting components of positive affect, life satisfaction, and an overall sense of purpose and meaning. Items are rated on a five‐point scale ranging from 1 (never) to 5 (always), with a total score ranging from 9 to 45. The PAW demonstrates good reliability and validity, with excellent internal consistency observed in the current sample (α = 0.94).
Multidimensional Scale of Perceived Social Support
This 12‐item questionnaire measures perceptions of perceived support from family, friends, and a significant other, with items rated on a 7‐point scale ranging from 1 (very strongly disagree) to 7 (very strongly agree). The total score assessing global perceived social support was used in the current study. Consistent with this sample (α = 0.95), good internal consistency reliability and test‐retest stability for the total scale and subscales have been found 29.
Positive and Negative Affect Schedule
Positive and negative affect are underlying dimensions of a broad set of emotional states characterized by pleasant and unpleasant moods or emotions, respectively. As a measurement of affect, participants completed the Positive and Negative Affect Schedule and indicated the frequency with which they generally experience 10 positive (ie, interested, excited, strong, enthusiastic, proud, alert, inspired, determined, attentive, active) and 10 negative (ie, distressed, upset, nervous, scared, hostile, irritable, ashamed, jittery, afraid, guilty) feelings 30. Items are rated on a five‐point scale ranging from 1 (very slightly or not at all) to 5 (extremely) with a total subscale ranging from 10 to 50. It yields two scores, one for positive affect (PA) and one for negative affect (NA). Because our aim was to target positive psychological factors, only the PA subscale was used in the analysis. For the current study, the internal consistency estimate for PA was excellent (α = 0.90).
Graded Chronic Pain Scale
The seven‐item Graded Chronic Pain Scale (GCPS) 31 was used to assess current, worst, and average knee pain during the past 6 months (characteristic pain intensity score), as well as the degree to which knee pain interfered with daily activities (disability score). Items were averaged and multiplied by 10 to generate index scores for pain intensity and disability, with higher scores indicating greater symptomatology. Cronbach's α for the GCPS was 0.91.
Short Physical Performance Battery
The Short Physical Performance Battery (SPPB) is comprised of three performance tests of lower‐extremity function: standing balance, 4‐m walking speed, and ability to rise from a chair. These tests have been standardized and are frequently utilized in older participants as assessments of lower‐extremity function 25. Each measure is scored from 0 (worst performance) to 4 (best performance), and a total score ranging from 0 to 12 is calculated. Immediately after each performance test, participants were asked to rate the overall knee pain they experienced on a scale from 0 (no knee pain) to 100 (most intense knee pain imaginable) 32 as a measurement of movement‐evoked pain 33, 34, 35.
Data Analysis
All data were analyzed using SPSS 24.0 (IBM). Prior to data analysis, data were checked for normality, outliers, and missing values. Race/ethnicity differences in demographic and clinical characteristics were assessed using chi‐square for dichotomous variables and independent samples t‐tests for continuous variables. Pearson's correlations were conducted to examine associations between measures of resilience and pain outcomes, and group differences in these variables were tested using multivariate analysis of variance/covariance. Unadjusted and adjusted (controlling for sociodemographic covariates) models were analyzed for comparison. Hayes’ PROCESS macro 36 was used to examine the potential moderating effect of race/ethnicity on the relationships between resilience measures (ie, trait resilience, optimism, positive well‐being, social support, PA) and pain outcomes (ie, pain intensity, pain disability, functional performance, movement‐evoked pain). This regression‐based path‐analytic modeling tool generates automatic mean centering and conditional effects in moderation models. Given race/ethnicity differences in age, income, education, marital status, employment, and BMI, as well as their association with clinical pain in prior research, these variables were included as covariates in the moderation analysis. Study site was also included as a covariate. To obtain effect size estimates, partial eta squared (η p 2) and Cohen's ƒ2 were calculated from generalized linear model and linear regression (ie, moderation) analyses, respectively (η p 2: small = 0.01, medium = 0.06, and large = 0.14; ƒ2: small = 0.02, medium = 0.15, and large = 0.35). Significance was set at P < 0.05 (two‐tailed test).
Results
Participant characteristics
Demographic and clinical characteristics of the sample are shown in Table 1. The majority of the participants were female, had an income less than $20,000, completed a high school degree or greater, not married, employed either full‐ or part‐time, and experienced knee pain for more than 5 years. The mean age was 57.9 years, and the average BMI was 31.9 kg/m2. Age, income, education, marital status, employment status, and BMI were significantly different between NHBs and NHWs.
Table 1.
Demographic and clinical characteristics of participants across race/ethnicity
| Overall N = 201 | NHB N = 105 | NHW N = 96 | P | |
|---|---|---|---|---|
| M or N (SD or %) | M or N (SD or %) | M or N (SD or %) | ||
| Age (years) | 57.9(7.7) | 56.4(6.5) | 59.6(8.5) | 0.004 |
| Sex | 0.277 | |||
| Female | 123(61.2) | 60(57.1) | 63(65.6) | |
| Male | 78(38.8) | 45(42.9) | 33(34.4) | |
| Race | ||||
| NHB | 105(52.2) | … | … | |
| NHW | 96(47.8) | … | … | |
| Income a | <0.001 | |||
| <$20,000 | 86(42.8) | 58(56.9) | 28(29.5) | |
| $20,000‐39,999 | 37(18.4) | 23(22.5) | 14(14.7) | |
| $40,000‐59,999 | 31(15.4) | 8(7.8) | 23(24.2) | |
| $60,000‐99,999 | 26(12.9) | 10(9.8) | 16(16.8) | |
| >$100,000 | 17(8.5) | 3(2.9) | 14(14.7) | |
| Education | 0.002 | |||
| Some high school | 14(7.0) | 12(11.4) | 2(2.1) | |
| High school degree | 86(42.8) | 51(48.6) | 35(36.5) | |
| Associates or Bachelors | 72(35.8) | 33(31.4) | 39(40.6) | |
| Graduate/professional | 29(14.4) | 9(8.6) | 20(20.8) | |
| Marital status a | 0.001 | |||
| Married | 69(34.3) | 24(23.3) | 45(47.4) | |
| Not married | 129(64.2) | 79(76.7) | 50(52.6) | |
| Employment | 0.002 | |||
| Employed | 80(39.8) | 42(40.0) | 38(39.6) | |
| Not employed | 72(35.8) | 47(44.8) | 25(26.0) | |
| Retired | 49(24.4) | 16(15.2) | 33(34.4) | |
| Knee pain duration a | 0.384 | |||
| <1 year | 26(12.9) | 15(14.4) | 11(11.7) | |
| 1 to 5 years | 79(39.3) | 45(43.3) | 34(36.2) | |
| >5 years | 93(46.3) | 44(42.3) | 49(52.1) | |
| BMI (kg/m2) | 31.9(7.7) | 33.0(7.9) | 30.7(7.2) | 0.036 |
| Testing site | 0.185 | |||
| UF | 132(65.7) | 64(61.0) | 68(70.8) | |
| UAB | 69(34.3) | 41(39.0) | 28(29.2) |
Abbreviation: BMI, body mass index; NHB, non‐Hispanic black; NHW, non‐Hispanic white; UAB, University of Alabama at Birmingham; UF, University of Florida.
Some data not reported.
Pearson correlations across clinical measures
Pearson correlations amongst measures of resilience, pain, and function are presented in Table 2. Although no significant relationships were found between PA and pain intensity (P = 0.40), pain disability (P = 0.08), and movement‐evoked pain (P = 0.25), the overall pattern of results suggests that individuals higher in trait resilience, optimism, positive well‐being, and social support exhibited lower levels of pain intensity, pain disability, and movement‐evoked pain, as well as higher levels of physical functioning. Furthermore, all measures of resilience were significantly and positively correlated with one another (r = 0.28 to 0.64).
Table 2.
Pearson product‐moment correlations among clinical characteristics
| Trait resilience | Optimism | Positive well‐being | Social support | Positive affect | GCPS pain | GCPS disability | SPPB function | SPPB pain | |
|---|---|---|---|---|---|---|---|---|---|
| Trait resilience | … | ||||||||
| Optimism | 0.46** | … | |||||||
| Positive well‐being | 0.56** | 0.57** | … | ||||||
| Social support | 0.32** | 0.34** | 0.43** | … | |||||
| Positive affect | 0.49** | 0.44** | 0.64** | 0.28** | … | ||||
| GCPS pain | −0.17* | −0.25** | −0.20** | −0.24** | −0.06 | … | |||
| GCPS disability | −0.20** | −0.28** | −0.23** | −0.21** | −0.13 | 0.72** | … | ||
| SPPB function | 0.23** | 0.30** | 0.22** | 0.22** | 0.18* | −0.26** | −0.41** | … | |
| SPPB pain | −0.17* | −0.22** | −0.16* | −0.22** | −0.09 | 0.61** | 0.47** | −0.20** | … |
Abbreviation: GCPS, Graded Chronic Pain Scale; SPPB, Short Physical Performance Battery.
Note: *P < 0.05, **P < 0.01.
Race/ethnic differences in measures of psychosocial resilience and pain
Group comparisons across psychosocial resilience and pain outcomes are presented in Tables 3 and 4. Although there were no differences across race/ethnicity in resilience measures, significant differences emerged for measures of clinical pain and function. When compared with NHWs, black participants reported higher levels of pain intensity (P < 0.001), pain disability (P < 0.001), physical functioning (P = 0.01), and movement‐evoked pain (P < 0.001). With the exception of physical functioning (P = 0.18), these effects remained after controlling for age, income, education, marital status, employment, BMI, and study site (all values P < 0.01).
Table 3.
Descriptive and inferential statistics for measures of psychosocial resilience
| Measures | Unadjusted | Adjusted | ||||||
|---|---|---|---|---|---|---|---|---|
| NHB N = 105 | NHW N = 96 | Comparison | NHB N = 105 | NHW N = 96 | Comparison | |||
| M (SD) | M (SD) | F | η p 2 | M (SD) | M (SD) | F | η p 2 | |
| Trait resilience (1‐6) | 3.7(0.7) | 3.8(0.8) | 0.14 | 0.00 | 3.8(0.7) | 3.6(0.8) | 2.03 | 0.01 |
| Optimism (0‐24) | 17.1(4.5) | 18.4(4.9) | 3.21† | 0.02 | 17.8(4.5) | 17.6(4.9) | 0.09 | 0.00 |
| Positive well‐being (9‐45) | 36.2(7.0) | 36.4(6.9) | 0.05 | 0.00 | 37.1(6.9) | 35.4(6.9) | 2.46 | 0.02 |
| Social support (12‐96) | 62.1(20.2) | 64.9(16.0) | 1.04 | 0.01 | 63.7(20.3) | 62.8(16.1) | 0.10 | 0.00 |
| Positive affect (10‐50) | 34.1(8.4) | 34.9(7.4) | 0.49 | 0.00 | 34.7(8.5) | 34.1(7.3) | 0.20 | 0.00 |
† P = 0.07. Adjusted models controlled for age, income, education, marital status, employment, body mass index, and study site.
Abbreviation: NHB, non‐Hispanic black; NHW, non‐Hispanic white.
Table 4.
Descriptive and inferential statistics for measures of pain and function
| Unadjusted | Adjusted | |||||||
|---|---|---|---|---|---|---|---|---|
| NHB N = 105 | NHW N = 96 | Comparison | NHB N = 105 | NHW N = 96 | Comparison | |||
| M (SD) | M (SD) | F | ηp 2 | M (SD) | M (SD) | F | ηp 2 | |
| GCPS pain (0‐100) | 66.6(20.3) | 43.5(20.1) | 61.77** | 0.25 | 63.4(20.4) | 47.1(20.1) | 29.03** | 0.14 |
| GCPS disability (0‐100) | 57.0(27.7) | 36.6(29.6) | 23.99** | 0.11 | 52.9(28.3) | 40.5(29.6) | 7.84** | 0.04 |
| SPPB function (0‐12) | 9.1(1.8) | 9.7(1.5) | 6.26* | 0.03 | 9.2(1.8) | 9.6(1.5) | 1.85 | 0.01 |
| SPPB pain (0‐100) | 29.6(29.2) | 14.0(17.9) | 19.08** | 0.09 | 29.0(29.5) | 16.2(18.0) | 10.93** | 0.06 |
*P < 0.05, **P < 0.01. Adjusted models controlled for age, income, education, marital status, employment, body mass index, and study site. Abbreviation: NHB, non‐Hispanic black; NHW, non‐Hispanic white; GCPS, Graded Chronic Pain Scale; SPPB, Short Physical Performance Battery.
Moderation Analysis
Adjusting for covariates, race/ethnicity was examined as a moderator of the relationship between psychosocial resilience measures and pain and physical function outcomes. Interaction effects between race/ethnicity and each resilience factor are displayed in Table 5. There was a significant interaction (b = 1.94, 95% confidence interval [CI] = 0.26 to 3.62, ΔR 2 = 0.03, ƒ2 = 0.04) between race/ethnicity and optimism with movement‐evoked pain (overall model: R 2 = 0.23, F(10, 164) = 4.71, P < 0.001). The interaction plot (Figure 1A) revealed a negative association between optimism and movement‐evoked pain in NHBs (b = −1.67, P = 0.02), which was not significant in NHWs (b = 0.27, P = 0.57). Similarly, a significant interaction (b = 1.44, 95% CI = 0.15 to 2.72, ΔR 2 = 0.03, ƒ2 = 0.04) was found between race/ethnicity and positive well‐being (overall model R 2 = 0.23, F(10, 164) = 4.34, P < 0.001). Simple slopes analysis (Figure 1B) revealed that for NHBs there was a trend toward an inverse relationship between positive well‐being and movement‐evoked pain (b = −0.95, P = 0.10); however, these effects were in the opposite direction for NHWs (b = 0.48, P = 0.13). The interaction (b = 1.02, 95% CI = 0.04 to 1.99, ΔR 2 = 0.02, ƒ2 = 0.03) between race/ethnicity and PA for movement‐evoked pain was also significant (Figure 1C), with the overall model explaining 22% of the variance in SPPB pain scores (overall model: R 2 = 0.22, F(10, 163) = 4.74, P < 0.001). Movement‐evoked pain was lower in NHWs as PA decreased (b = 0.59, P = 0.03); however, this relationship was nonsignificant for NHBs (b = −0.49, P = 0.30). Supplementary Table 1 reports the full linear regression analysis for significant movement‐evoked pain results. There were no other significant moderation effects observed in the analysis, including those for pain intensity, pain disability, and physical function (P > 0.05).
Table 5.
Moderation analysis for interactions between psychosocial resilience measures and race/ethnicity
| GCPS Pain | GCPS Disability | SPPB Function | SPPB Pain | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | P | b | SE | P | b | SE | P | b | SE | P | |
| Interactions | ||||||||||||
| Trait Resilience X Race/Ethnicity | 2.57 | 3.94 | .516 | 2.25 | 5.45 | .679 | ‐.40 | .30 | .187 | 8.52 | 6.11 | .165 |
| Optimism X Race/Ethnicity | .50 | .63 | .422 | ‐.25 | 1.00 | .805 | ‐.01 | .06 | .859 | 1.94 | .85 | .024 |
| Positive Well‐Being X Race/Ethnicity | .67 | .45 | .142 | .13 | .62 | .827 | .02 | .04 | .622 | 1.44 | .65 | .028 |
| Social Support X Race/Ethnicity | .11 | .17 | .502 | ‐.01 | .25 | .956 | .00 | .01 | .964 | .32 | .22 | .150 |
| Positive Affect X Race/Ethnicity | .29 | .46 | .533 | .23 | .61 | .702 | .01 | .04 | .717 | 1.02 | .49 | .041 |
Models adjusted for age, income, education, marital status, employment, BMI, and study site.
Abbreviation: b, unstandardized beta; GCPS, Graded Chronic Pain Scale; SPPB, Short Physical Performance Battery.
Figure 1.
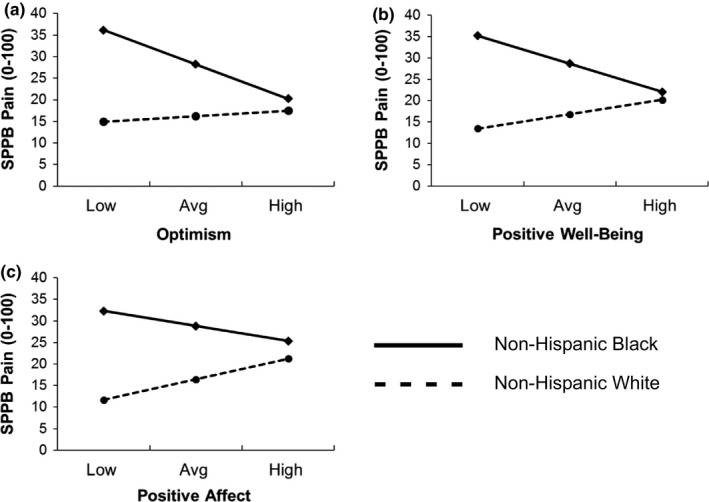
Illustration of the associations between measures of psychosocial resilience and race/ethnicity for movement‐evoked pain. As depicted in panels (a) and (b), lower levels of optimism and positive well‐being were associated with higher movement‐evoked pain for non‐Hispanic blacks. For non‐Hispanic whites (c), lower PA was associated with attenuated movement‐evoked pain.
Discussion
Race/ethnic differences in clinical and experimental pain have been widely documented 8, 9, 13, and a growing literature has recognized resilience as an important resource for individuals with chronic pain 4, 37. Expanding on prior research, our study provides evidence regarding the influence of psychosocial resilience on pain and functioning among adults with knee OA and is the first to examine whether these relationships are differentially expressed across race/ethnicity.
Aligning with study hypotheses, we found that more psychologically resilient individuals report lower clinical pain and disability and experience higher levels of functional performance, signifying that resilience may promote more adaptive functioning by attenuating adverse pain outcomes. Although risk mechanisms (eg, catastrophizing, depression) associated with chronic pain vulnerability have traditionally dominated the literature, studies focusing on resilience suggest that positive psychological factors are instrumental in supporting a number of health benefits, including higher quality of life, lower clinical pain and disability, adaptive pain coping, greater physical functioning, reduced NA, and positive pain adjustment 4, 16, 37. These effects extend beyond those associated with pain‐related vulnerability, as recent evidence supports the unique contribution of resilience factors in psychological health 38. Together, these findings suggest that capitalizing on positive resources may increase one's capacity for effectively managing their pain.
Corroborating the health care disparities literature, as well as our own work 13, 39, NHBs with knee OA reported greater knee pain severity and disability, poorer functional performance, and greater knee pain with movement than did NHWs. However, there were no distinct group differences in measures of psychosocial resilience despite a vast literature reporting race/ethnic differences in pain coping 21, 22. In fact, overall pain‐coping strategies are used more frequently among NHBs, particularly passive coping methods, such as catastrophizing, hoping, and praying 8, 21, 22. Furthermore, perceived racial discrimination 39, catastrophizing 40, and prayer 22, 40 have all been found to partially account for observed racial/ethnic differences in both experimental and clinical pain. Although there is some evidence that positive psychological factors may also differ across race/ethnicity, results have been mixed, and studies have predominantly been conducted in nonclinical (ie, pain‐free) populations. Of these, similar levels of optimism 20, resilience 41, social support 41, and dispositional hope 42 have been observed across race/ethnicity, whereas other studies have found higher PA among NHBs relative to white participants 42, 43. In the two studies exploring pain‐coping differences in an OA population, one found lower arthritis self‐efficacy in NHBs 12; however, comparable levels of pain self‐efficacy across race/ethnicity have also been noted 22. Although the present study provides a unique opportunity to expand upon this limited research, future work is warranted to delineate potential race/ethnic differences in other positive resources known to foster resilience in OA.
Despite similar levels of psychosocial resilience across race/ethnicity, optimism and positive well‐being had an inverse association with movement‐evoked pain in NHBs, suggesting that these resources may be particularly protective in this group. Efforts to enhance optimistic beliefs and positive well‐being, as opposed to simply reducing risk, may be a critical directive for yielding improvements in pain among NHBs. Even more striking, we found that lower levels of PA were protective against movement‐evoked pain among NHWs, with a similar pattern noted for positive well‐being (although nonsignificant). Although this may seem counterintuitive, especially given the wealth of literature denoting the measurable health benefits of PA, it is also known that the level of activation or arousal can dictate the directionality of these effects 44. Indeed, studies suggest an adverse effect of high‐arousal positive emotions on health, that are ostensibly due to increased sympathetic activation 44. Consistent with this interpretation, recent empirical work has noted the association between low‐arousal PA and lower C‐reactive protein in patients with breast cancer 45. Similarly, Hassett and colleagues showed that individuals with low positive and NA (low affect balance style, reflective of a calm or relaxed temperament) had an attenuated risk of experiencing a pain or somatization disorder 46. Together, these findings point to the possibility that low‐arousal PA may dampen physiological arousal, which could lead to the downregulation of neural processes associated with pain facilitation in NHWs. This hypothesis is speculative but certainly encourages further exploration.
Notably, the associations of psychological resilience with self‐reported measures of pain and function were largely independent of racial/ethnic group, yet a distinct pattern emerged for movement‐evoked pain. Research designed to explore the effects of movement‐related pain have found it to be associated with poorer physical performance and work‐related disability, and there is evidence for its unique contribution to self‐reported and functional measures of disability, beyond the variance attributed by spontaneous pain measures 34, 35. Thus, movement‐evoked pain may reflect a more disability‐relevant index of the pain experience. In light of our own findings, increased pain during movement may initiate a pattern of avoidance that reduces activity engagement and thereby exacerbates pain and functional limitations. Intervening across measures of resiliency may help mitigate these effects. Importantly, efforts to understand how these relationships operate across racial/ethnic groups may facilitate initiatives that target the improvement of movement‐evoked pain.
There is a growing appreciation for the contribution of positive psychosocial factors in pain adaptation and interest in whether these crucial resources have utility in clinical practice. Although cognitive‐behavioral therapy remains the gold standard of psychological treatments, not all patients benefit equally, and thus therapeutic effects tend to be modest 47. Research focused on cultivating resilience through the strengthening of psychological assets (eg, PA, gratitude, optimism) has shown promise in improving both pain and psychological outcomes 48, 49, 50, yet little is known about how these interventions operate in OA populations. An additional shortcoming of previous research has been the failure to consider how psychosocial resilience manifests differently across racial/ethnic groups and whether this may be a contributor to pain disparities. Given race‐specific sociocultural influences (eg, disproportionate exposure to racial discrimination and socioeconomic inequities among NHBs) on pain, emotional well‐being, and physical health 39, the factors that promote positive adjustment may not be equivalent across NHBs and NHWs. Understanding how racial/ethnic groups experience pain and the protective mechanisms that influence those variations may be a critical step in optimizing our current pain treatments.
Several limitations merit acknowledgement. First, because of the cross‐sectional nature of the study, conclusions are limited as to the direction of the observed relationships. Second, our study population consisted of NHBs and NHWs with knee OA, most of whom were older in age; therefore, it is unclear whether results are generalizable to other demographic (eg, other chronic pain conditions, younger cohorts) and racial/ethnic groups. Third, although we adjusted analyses for many covariates known to potentially affect the outcomes of interest, it is possible that other unmeasured social or demographic factors confounded these relationships. This limitation warrants particular caution in interpreting racial/ethnic disparities. Fourth, although we had a large sample size of 201 individuals with OA, it is likely that our study was not adequately powered to detect interaction effects amongst other key variables found to be nonsignificant. We also recognize that the effect sizes for our significant interactions were small and only contributed an additional 2%‐3% of the variance in outcomes. Future studies with larger samples are needed to replicate findings and to ascertain their clinical relevance. And finally, a large number of statistical tests were conducted, which could increase Type I error. However, given that there was a clear pattern to our results, in that measures of resilience had a stronger impact on movement‐evoked pain in the moderation analysis (relative to functional performance and self‐reported measures of pain and disability), we do not believe this reflects spurious findings.
Although these factors may limit the generalizability of our findings, this study represents an important step in understanding how psychosocial resilience differentially influences pain and functioning across racial/ethnic groups. Some strengths include the recruitment of a large community sample and the inclusion of several measures of resilience rather than relying on a unitary measure. Additionally, the current investigation is the first to examine the contributions of resilience to movement‐evoked pain. Measures of dynamic pain during movement have been suggested to be a stronger predictor of disability 35 than spontaneous pain measures; however, most studies to date have not routinely assessed task‐oriented pain. Because activity‐related pain is a driver of disability, utilizing real‐time functional pain measurements may be a more sensitive method by which to assess pain burden.
In summary, our findings support the larger literature on race/ethnic differences in pain and physical functioning and suggest that positive psychosocial measures may have salutary effects on knee OA symptoms. Given the limited research in this area, continued work is warranted as resilience factors are amendable and may be important targets for medical care designed to prevent and treat knee OA pain. In particular, treatments that address optimism and positive well‐being in NHBs may have downstream effects that reduce the overall burden of pain in this group. Examining the factors that affect pain and physical functioning may ultimately allow for the development of more optimal and culturally sensitive treatments to alleviate chronic pain.
Supporting information
Funding and support was provided by NIH/NIA grants R37‐AG033906‐14 to Dr. Fillingim and R01‐AG054370 to Dr. Sibille; University of Florida CTSA grant UL1TR001427 and University of Alabama at Birmingham CTSA grant UL1TR001417 by the NIH Center for Advancing Translational Sciences; Dr. Terry was recipient of 1K22NS102334, provided to the University of Florida and McKnight Brain Institute Career Development Award; Dr. Booker was funded by grant T32AG049673, Dr. Vaughn was funded by grant 3R37AG033906‐12S1, and Mr. Cardoso was recipient of minority supplement provided to the University of Florida; Ms. Thompson and Dr. Bulls were funded by NIH training grants TL‐1TR001418 and R25‐CA090314, respectively; and Dr. Bartley was recipient of NIH/NIA grant R00‐AG052642.
Correction added after online publication 08 May 2019: the author affiliations have been corrected.
References
- 1. Cisternas MG, Murphy L, Sacks JJ, Solomon DH, Pasta DJ, Helmick CG. Alternative methods for defining osteoarthritis and the impact on estimating prevalence in a US population‐based survey. Arthritis Care Res (Hoboken) 2016;68:574–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Allen KD, Golightly YM. Epidemiology of osteoarthritis: state of the evidence. Curr Opin Rheumatol 2015;27:276–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Deshpande BR, Katz JN, Solomon DH, Yelin EH, Hunter DJ, Messier SP, et al. Number of persons with symptomatic knee osteoarthritis in the US: impact of race and ethnicity, age, sex, and obesity. Arthritis Care Res (Hoboken) 2016;68:1743–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bartley EJ, Palit S, Staud R. Predictors of osteoarthritis pain: the importance of resilience. Curr Rheumatol Rep 2017;19:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Iijima H, Aoyama T, Fukutani N, Isho T, Yamamoto Y, Hiraoka M, et al. Psychological health is associated with knee pain and physical function in patients with knee osteoarthritis: an exploratory cross‐sectional study. BMC Psychology 2018;6:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Alkan BM, Fidan F, Tosun A, Ardıçoğlu Ö. Quality of life and self‐reported disability in patients with knee osteoarthritis. Mod Rheumatol 2014;24:166–71. [DOI] [PubMed] [Google Scholar]
- 7. Burns R, Graney MJ, Lummus AC, Nichols LO, Martindale‐Adams J. Differences of self‐reported osteoarthritis disability and race. J Natl Med Assoc 2007;99:1046–51. [PMC free article] [PubMed] [Google Scholar]
- 8. Campbell CM, Edwards RR. Ethnic differences in pain and pain management. Pain Manag 2012;2:219–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kim HJ, Yang GS, Greenspan JD, Downton KD, Griffith KA, Renn CL, et al. Racial and ethnic differences in experimental pain sensitivity: systematic review and meta‐analysis. Pain 2017;158:194–211. [DOI] [PubMed] [Google Scholar]
- 10. Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol 2007;34:172–80. [PubMed] [Google Scholar]
- 11. Vina ER, Ran D, Ashbeck EL, Kwoh CK. Natural history of pain and disability among African‐Americans and whites with or at risk for knee osteoarthritis: a longitudinal study. Osteoarthritis Cartilage 2018;26:471–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Allen KD, Helmick CG, Schwartz TA, DeVellis RF, Renner JB, Jordan JM. Racial differences in self‐reported pain and function among individuals with radiographic hip and knee osteoarthritis: the Johnston County Osteoarthritis Project. Osteoarthritis Cartilage 2009;17:1132–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cruz‐Almeida Y, Sibille KT, Goodin BR, Petrov ME, Bartley EJ, Riley JL 3rd, et al. Racial and ethnic differences in older adults with knee osteoarthritis. Arthritis Rheumatol 2014;66:1800–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Meints SM, Edwards RR. Evaluating psychosocial contributions to chronic pain outcomes. Prog Neuropsychopharmacol Biol Psychiatry 2018;87:168–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Goodin BR, Glover TL, Sotolongo A, King CD, Sibille KT, Herbert MS, et al. The association of greater dispositional optimism with less endogenous pain facilitation is indirectly transmitted through lower levels of pain catastrophizing. J Pain 2013;14:126–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ferreira VM, Sherman AM. The relationship of optimism, pain and social support to well‐being in older adults with osteoarthritis. Aging Ment Health 2007;11:89–98. [DOI] [PubMed] [Google Scholar]
- 17. Finan PH, Quartana PJ, Smith MT. Positive and negative affect dimensions in chronic knee osteoarthritis: effects on clinical and laboratory pain. Psychosom Med 2013;75:463–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zautra AJ, Johnson LM, Davis MC. Positive affect as a source of resilience for women in chronic pain. J Consult Clin Psychol 2005;73:212–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Thompson KA, Bulls HW, Sibille KT, Bartley EJ, Glover TL, Terry EL, et al. Optimism and psychological resilience are beneficially associated with measures of clinical and experimental pain in adults with or at risk for knee osteoarthritis. Clin J Pain 2018;34:1164–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Goodin BR, Kronfli T, King CD, Glover TL, Sibille K, Fillingim RB. Testing the relation between dispositional optimism and conditioned pain modulation: Does ethnicity matter? J Behav Med 2013;36:165–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Meints SM, Miller MM, Hirsh AT. Differences in pain coping between black and white Americans: a meta‐analysis. J Pain 2016;17:642–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jones AC, Kwoh CK, Groeneveld PW, Mor M, Geng M, Ibrahim SA. Investigating racial differences in coping with chronic osteoarthritis pain. J Cross Cult Gerontol 2008;23:339–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis: classification of osteoarthritis of the knee. Arthritis Rheum 1986;29:1039–49. [DOI] [PubMed] [Google Scholar]
- 24. Roux CH, Saraux A, Mazieres B, Pouchot J, Morvan J, Fautrel B, et al. Screening for hip and knee osteoarthritis in the general population: predictive value of a questionnaire and prevalence estimates. Ann Rheum Dis 2008;67:1406–11. [DOI] [PubMed] [Google Scholar]
- 25. Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self‐reported disability and prediction of mortality and nursing home admission. J Gerontol 1994;49:M85–94. [DOI] [PubMed] [Google Scholar]
- 26. Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med 2008;15:194–200. [DOI] [PubMed] [Google Scholar]
- 27. Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self‐mastery, and self‐esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol 1994;67:1063–78. [DOI] [PubMed] [Google Scholar]
- 28. Salsman JM, Victorson D, Choi SW, Peterman AH, Heinemann AW, Nowinski C, et al. Development and validation of the positive affect and well‐being scale for the neurology quality of life (Neuro‐QOL) measurement system. Qual Life Res 2013;22:2569–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J Pers Assess 1990;55:610–7. [DOI] [PubMed] [Google Scholar]
- 30. Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol 1988;54:1063–70. [DOI] [PubMed] [Google Scholar]
- 31. Von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain 1992;50:133–49. [DOI] [PubMed] [Google Scholar]
- 32. Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain 1983;17:45–56. [DOI] [PubMed] [Google Scholar]
- 33. Corbett DB, Simon CB, Manini TM, George SZ, Riley JL 3rd, Fillingim RB. Movement‐evoked pain: transforming the way we understand and measure pain. Pain 2018. E‐pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mankovsky‐Arnold T, Wideman TH, Thibault P, Lariviere C, Rainville P, Sullivan MJ. Sensitivity to movement‐evoked pain and multi‐site pain are associated with work‐disability following whiplash injury: a cross‐sectional study. J Occup Rehabil 2017;27:413–21. [DOI] [PubMed] [Google Scholar]
- 35. Mankovsky‐Arnold T, Wideman TH, Lariviere C, Sullivan MJ. Measures of spontaneous and movement‐evoked pain are associated with disability in patients with whiplash injuries. J Pain 2014;15:967–75. [DOI] [PubMed] [Google Scholar]
- 36. Hayes AF. Introduction to mediation, moderation, and conditional process analysis, second edition: a regression‐based approach. New York: Guilford Press; 2017. [Google Scholar]
- 37. Goubert L, Trompetter H. Towards a science and practice of resilience in the face of pain. Eur J Pain 2017;21:1301–15. [DOI] [PubMed] [Google Scholar]
- 38. Alschuler KN, Kratz AL, Ehde DM. Resilience and vulnerability in individuals with chronic pain and physical disability. Rehabil Psychol 2016;61:7–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Goodin BR, Pham QT, Glover TL, Sotolongo A, King CD, Sibille KT, et al. Perceived racial discrimination, but not mistrust of medical researchers, predicts the heat pain tolerance of African Americans with symptomatic knee osteoarthritis. Health Psychol 2013;32:1117–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Meints SM, Hirsh AT. In vivo praying and catastrophizing mediate the race differences in experimental pain sensitivity. J Pain 2015;16:491–7. [DOI] [PubMed] [Google Scholar]
- 41. Herbert MS, Leung DW, Pittman JO, Floto E, Afari N. Race/ethnicity, psychological resilience, and social support among OEF/OIF combat veterans. Psychiatry Res 2018;265:265–70. [DOI] [PubMed] [Google Scholar]
- 42. Chang EC, Banks KH. The color and texture of hope: some preliminary findings and implications for hope theory and counseling among diverse racial/ethnic groups. Cultur Divers Ethnic Minor Psychol 2007;13:94–103. [DOI] [PubMed] [Google Scholar]
- 43. Krok‐Schoen JL, Baker TA. Race differences in personality and affect between older white and black patients: an exploratory study. J Racial Ethnic Health Dispar 2014;1:283–90. [Google Scholar]
- 44. Pressman SD, Cohen S. Does positive affect influence health? [review]. Psychol Bull 2005;131:925–71. [DOI] [PubMed] [Google Scholar]
- 45. Moreno PI, Moskowitz AL, Ganz PA, Bower JE. Positive affect and inflammatory activity in breast cancer survivors: examining the role of affective arousal. Psychosom Med 2016;78:532–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hassett AL, Simonelli LE, Radvanski DC, Buyske S, Savage SV, Sigal LH. The relationship between affect balance style and clinical outcomes in fibromyalgia. Arthritis Rheum 2008;59:833–40. [DOI] [PubMed] [Google Scholar]
- 47. Eccleston C, Morley SJ, Williams AC. Psychological approaches to chronic pain management: evidence and challenges. Br J Anaesth 2013;111:59–63. [DOI] [PubMed] [Google Scholar]
- 48. Müller R, Gertz KJ, Molton IR, Terrill AL, Bombardier CH, Ehde DM, et al. Effects of a tailored positive psychology intervention on well‐being and pain in individuals with chronic pain and a physical disability: a feasibility trial. Clin J Pain 2016;32:32–44. [DOI] [PubMed] [Google Scholar]
- 49. Hausmann LR, Youk A, Kwoh CK, Ibrahim SA, Hannon MJ, Weiner DK, et al. Testing a positive psychological intervention for osteoarthritis. Pain Med 2017;18:1908–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Peters ML, Smeets E, Feijge M, van Breukelen G, Andersson G, Buhrman M, et al. Happy despite pain: a randomized controlled trial of an 8‐week internet‐delivered positive psychology intervention for enhancing well‐being in patients with chronic pain. Clin J Pain 2017;33:962–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


