Abstract
Objective
We examined walking limitations and associated characteristics among middle‐aged and older US adults with arthritis, overall, and by sex.
Methods
Using 2005‐2006 Arthritis Conditions and Health Effects Survey (ACHES) data (n = 1793), we estimated “a lot” and “any” (“a lot” or “a little” combined) walking limitation for more than 1 mile (1.6 km) among US adults 45 years or older with arthritis and examined associations (sociodemographics, arthritis symptoms and effects, psychosocial measures, and physical health) with walking limitations in unadjusted and multivariable (MV) adjusted logistic regression models using prevalence ratios (PRs) and 95% confidence intervals, accounting for the complex survey design.
Results
Respondents frequently reported “a lot” (48%) and “any” (72%) limitation for more than 1 mile. Women reported higher prevalence of all levels of walking limitation versus men (eg, 51% vs 42% for “a lot” overall); additionally, the gap for walking limitations between women and men widened with age. Limitation was high for both sexes at all ages, affecting 1‐in‐3 to 4‐in‐5, depending on level of walking limitation. The strongest MV associations for “a lot” of walking limitation among all respondents included substantial and modest arthritis‐attributable life interference (PR = 2.5 and 1.6, respectively), age 75 years or older (PR = 1.5), and physical inactivity and fair/poor self‐rated health (PR = 1.4 for both).
Conclusion
Walking limitations among middle‐aged and older adults are substantial. Existing proven interventions that improve walking ability and physical function may help this population to reduce and delay disability.
Introduction
Physical activity is an important arthritis self‐management strategy because of its numerous benefits, including reduced cancer, anxiety, depression, and chronic disease onset; improved function, mood, quality of life, sleep, and bone and brain health; decreased pain and mortality; weight control; and—among older adults—decreased fall‐related injuries 1. Walking is a popular strategy for increasing physical activity in general, especially for people with arthritis because it is low impact and accessible. Additionally, walking is associated with improvements in physical and self‐reported performance measures and reduced arthritis symptoms, such as fatigue, stiffness, and pain 2. Reports indicate that people with arthritis are receptive to walking as a potential physical activity and may prefer it over other more vigorous or high‐impact activities 3.
Multiple recent studies demonstrate that even small amounts of walking can reduce risk of disability onset for adults with arthritis. One longitudinal study among adults 50 years or older with, or at risk for, knee OA found that those who walked a minimum of 3000 steps or more per day (target 6000 steps or more per day) had reduced risk of developing functional disability 4. Also, a population‐based longitudinal study of adults aged 18 years or older found that, compared with walking less than 10 minutes/week, walking more than 10 minutes per week was significantly associated with decreased risk of limitations in walking 3 blocks, climbing 10 stairs, stooping/kneeling, reaching overhead, and grasping (hazard ratios 0.3‐0.5) 5. Still, walking prevalence among adults with arthritis is low; prevalence of walking for leisure or for transportation for 10 minutes or more in the past week was significantly lower among adults with arthritis versus those without: 46% vs 52% and 23% vs 32%, respectively, in a recent study 6.
Arthritis is recognized as a major cause of mobility limitations. For example, a longitudinal study demonstrated that people with arthritis had a 55% increased risk of developing persistent difficulty in mobility versus those without arthritis over the course of 10 years 7. For many people, mobility, a cornerstone of function and independence, depends on the ability to walk, and mobility limitations are associated with decreased social activity 8, reduced physical function, and greater depression 9. Walking limitations, specifically, are a strong predictor of disability 10. Cross‐sectional and longitudinal studies of arthritis, especially osteoarthritis (OA) and rheumatoid arthritis, have established associations between arthritis and limitations in walking multiple distances (eg, a mile [1.6 km] 11, a quarter mile [0.4 km] 12, 13), climbing stairs 10, 11, 13, walking speed 14, and the development of incident mobility 4, 7, impairments in activities of daily living 7, and functional limitations 4.
Addressing walking difficulty can prevent disability onset and thus early detection of, and interventions to reduce, walking limitations for longer distances (eg, more than 1 mile), which may be especially critical for preventing onset of walking limitations for shorter distances (eg, several hundred feet). Although reducing limitations at the population level could have profound benefits for US adults with arthritis, population‐based data sources for surveillance that inform resource allocation, planning, and disseminating public health interventions to address walking limitations remain scarce. The US Surgeon General's 2015 Call to Action to Promote Walking and Walkable Communities dedicated an entire chapter (Gaps in Surveillance, Research, and Evaluation) to the need for more data sources on walking prevalence, study of dimensions of walking (ability, amount, etc), and encouragement of the analysis and publication of existing data to inform the state of the science 15, which remain active strategic goals.
Despite recent documentation of either the lower prevalence of walking in people with arthritis or the association of arthritis mobility limitations with subsequent disability and functional decline, overall there has been limited recent study of the magnitude of self‐reported walking difficulties among adults with arthritis in the general population. Our objectives were to estimate the prevalence of walking limitations (each of “a lot” and “any”) for the distance of more than 1 mile among US adults 45 years or older with arthritis overall, by sex, and other characteristics (sociodemographic, physical, and psychosocial). We also examined the association of these characteristics with “a lot” of walking limitations to identify those most in need of strategies to reduce walking limitations.
Methods
We analyzed data from the US population–based Arthritis Conditions and Health Effects Survey (ACHES), a random‐digit‐dialed national telephone survey designed by the US Centers for Disease Control and Prevention (CDC) that was conducted from June 2005 to April 2006 16. The purpose of this cross‐sectional survey was to measure physical and psychosocial effects of arthritis as well as knowledge, attitudes, and behaviors about arthritis treatment and management. It was designed to provide estimates representative of the civilian, noninstitutionalized US population of adults 45 years or older with arthritis. The ACHES study protocol and methods were approved by the CDC and Battelle Centers for Public Health Research and Evaluation Institutional Review Boards and complies, as applicable, to the 1975 Declaration of Helsinki 16. Additional details on ACHES methodology have been previously described in detail 16.
Briefly, ACHES used a probability‐based design and a stratified systematic sample of telephone numbers linked to US census blocks, which were partitioned into seven strata based on the percentages of Hispanics and non‐Hispanic (NH) blacks associated with each block. To ensure geographic representation and reduce sample variation, the percentages were sorted by census division and metropolitan status (ie, urban vs rural counties) in each stratum. Telephone numbers within each of the seven strata were selected with equal probability; there was oversampling of strata with high percentages of Hispanics and NH blacks 16.
At least two weeks prior to the first call, letters were mailed to the addresses associated with potential residential phone numbers in an effort to maximize response rates. Trained interviewers called each number to identify 1) residential numbers and 2) household members 45 years or older with doctor‐diagnosed arthritis. Interviews were conducted in English or Spanish after receiving oral consent using a standardized consent statement (written informed consent was waived because of the study design). All residents in each household who met inclusion criteria were eligible. Participants were offered compensation with a choice of a prepaid long distance phone card or a $5 donation to the Arthritis Foundation. Among eligible households, response and completion rates were 51% and 86%, respectively 17. Among eligible household members, response and completion rates were 31% and 75%, respectively, for the first household participant identified as eligible and 16% and 80%, respectively, for subsequent eligible household respondents. This report is based on information from respondents (n = 1793) who reported doctor‐diagnosed arthritis, defined as “yes” to the question: “Have you ever been told by a doctor or other health professional that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
Dependent variable
Walking limitation
We examined walking limitation for distances greater than a mile. Specifically, respondents were asked whether “your health now limits you a lot, limits you a little, or does not limit you at all.” We report results for “a lot” and “any” (“a lot” or “a little” combined) limitation walking more than 1 mile (Figure 1). These questions were from the SF‐12 Physical Function subscale 18.
Figure 1.
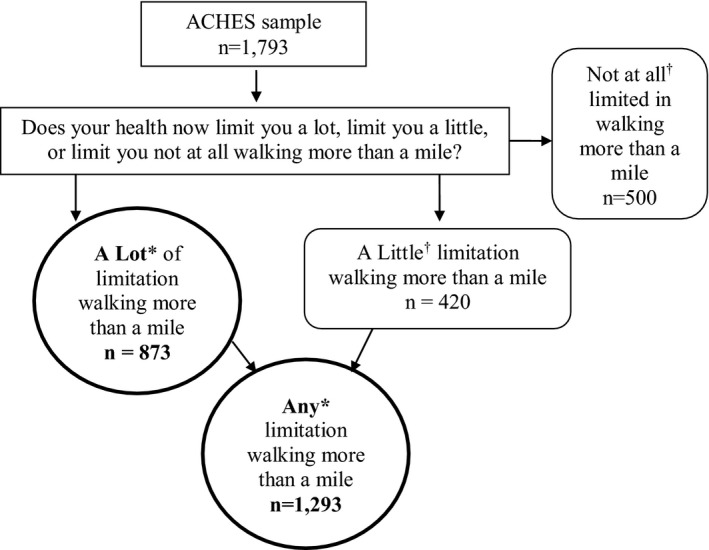
Selection of the study population. *Main outcome; †Category not separately analyzed.
Independent variables
A priori selection of independent variables used two criteria: 1) characteristics that were previously observed or hypothesized to be related to walking disability (eg, age, education 19), and/or 2) characteristics known to be modifiable through evidence‐based interventions (eg, confidence in ability to manage arthritis symptoms 20).
Sociodemographics
Characteristics were age, sex, highest educational attainment, race/ethnicity, and employment status.
Arthritis symptoms and effects
We examined severity of three arthritis symptoms (joint pain, joint stiffness, and arthritis‐related fatigue (severe being 7 or more on a 10‐point scale 21, where 0 is none and 10 is “as bad as it can be”) in the past seven days and three arthritis effects: arthritis‐attributable limitation in whether one works (“arthritis or joint symptoms now affect whether you work for pay or not”); arthritis interference with sleep in the past seven days; and a summary arthritis‐attributable life interference variable. The latter is a mutually exclusive three‐level summary variable: 1) substantial (“a lot” of interference with one or more of the following four activities: recreation/leisure/hobbies, household chores, errands/shopping, or social activities), 2) modest (1 or more occurrences of “a little” interference in the four activities), and 3) no interference 22.
Physical health
Characteristics included body mass index (BMI)(ie, weight in kg/height in m2) calculated from self‐reported weight and height (under/normal weight 24.9 or less, overweight 25.0‐29.9, obese 30.0 or more), physical activity level using 2008 US federal recommendations (meets physical activity guideline recommendations (150 minutes or more per week), insufficient (10 to less than 150 minutes/week), and inactive (less than 10 minutes/week)) 1 and general self‐rated health (excellent/very good, good, fair/poor).
Psychosocial characteristics
We examined 1) confidence in managing arthritis symptoms (no/low = 0‐3; moderate = 4‐6; high = 7 or greater on 0‐10 scale, where 0 is no confidence), 2) anxiety, and 3) depression. The latter two were measured with the Arthritis Impact Measurement Scales subscales, and presence of each was defined as a score of 4 or more 23, 24.
Statistical analysis
At all stages of contact (ie, person 1 or person 2+ eligibility ascertainment or interview), the most common reasons for incomplete interviews were that respondent refused to start/complete the interview and unavailability/unwillingness to participate, followed by physical/mental impairment, interviewing terminated prior to minimum number of screener calls made, and other (eg, phone disconnected). Sampling weights were constructed in multiple steps to address 1) residential number nonresponse, 2) person‐level nonresponse, and 3) poststratification adjustment, including person‐level screening, interview nonresponse, adjusting for differential probabilities associated with multiple telephone lines and compensation for undercoverage of nontelephone households. In subsequent steps, iterative proportional fitting (raking) was applied to weight ACHES respondents to counts of adults 45 years or older reporting doctor‐diagnosed arthritis derived from the National Health Interview Survey by age group, sex, and race/ethnicity to generate nationally representative estimates.
To address our research questions, we first estimated the percentage of both levels of walking limitations (“a lot” or “any”). Next, we conducted a stratified analysis to examine the percentage with “a lot” of walking limitation across independent variables.
For both levels of limitation, we performed an age‐stratified analysis to identify age‐specific patterns in walking limitations. We further stratified these age‐specific estimates by sex to identify sex‐specific differences in walking limitations in middle‐aged and older adults.
Finally, we estimated associations between each independent variable and walking limitation in unadjusted and multivariable adjusted logistic regression models. We modeled the associations comparing “a lot” relative to “a little or no” using prevalence ratios (PRs) and 95% confidence intervals (CIs). We generated unadjusted estimates to quantify the independent association between each characteristic and distance and then conducted multivariable analyses to determine which characteristics had the strongest (ie, statistically significant) independent associations with the distance. Our model contained characteristics intended to help identify potential target groups (eg, age) and/or potentially modifiable characteristics that have been linked to walking disability. We entered all candidate variables in an initial multivariable regression model and then proceeded to reduce the model through manual backward deletion. We used the Wald F statistic at α ≤ 0.10 as the inclusion criterion for the final model 25, which contained age, sex, race/ethnicity, employment status, joint pain severity, joint stiffness severity (both in past seven days), work limited because of arthritis, arthritis‐attributable interference, confidence in ability to manage arthritis symptoms, BMI, physical activity level, and self‐rated health.
We used SAS v.9.3 survey procedures to estimate percentages and SUDAAN v.11 to estimate PRs. We applied sampling weights in all analyses to produce estimates representative of US civilian noninstitutionalized adults 45 years or older with arthritis. Variance was estimated with 95% CIs and accounted for the complex design of the survey. Statistically significant differences were interpreted as nonoverlapping CIs 26.
We used methods recommended by the SF‐12 developers to impute values for missing responses on the walking variables 18. For all independent variables, we classified a response of “do not know” or “refused” as missing.
Results
Nearly half of respondents (47.5%, 95% CI = 44.9‐50.1) reported “a lot” of walking limitation (Table 1) and almost three‐quarters (71.9%, 95% CI = 69.5‐74.3) reported “any” walking limitation for more than a mile (Appendix).
Table 1.
Weighted percentage (overall and stratified), unadjusted, and multivariable adjusted prevalence ratios (PRs) with 95% confidence intervals (CIs) for associations with “a lot” of limitation walking more than 1 mile among US adults ages ≥45 years with arthritis (n = 1793)
| Characteristicsa | Unweighted Sample Size (Numerators) | Weighted Percentage | Unadjusted (n = 1793) | Multivariable Adjustedb (n = 1661) | |||
|---|---|---|---|---|---|---|---|
| n | % | 95% CI | PR | 95% CI | PR | 95% CI | |
| Overall | 873 | 47.5 | (44.9‐50.1) | ||||
| Sociodemographics | |||||||
| in | |||||||
| 45‐54 | 201 | 42.1 | (37.0‐47.3) | 1.0 | ref | 1.0 | ref |
| 55‐64 | 251 | 46.3 | (41.6‐51.0) | 1.1 | (0.9‐1.3) | 1.1 | (1.0‐1.3) |
| 65‐74 | 218 | 45.1 | (40.1‐50.2) | 1.1 | (0.9‐1.3) | 1.2 | (1.0‐1.4) |
| ≥75 | 194 | 61.0 | (55.1‐67.0) | 1.4 | (1.2‐1.7) | 1.5 | (1.3‐1.7) |
| Sex | |||||||
| Men | 236 | 41.5 | (36.9‐46.0) | 1.0 | ref | 1.0 | ref |
| Women | 637 | 51.4 | (48.4‐54.4) | 1.2 | (1.1‐1.4) | 1.1 | (1.0‐1.2) |
| Race/Ethnicity | |||||||
| Non‐Hispanic white | 655 | 46.3 | (43.3‐49.2) | 1.0 | ref | 1.0 | ref |
| Hispanic | 54 | 50.2 | (39.0‐61.4) | 1.1 | (0.9‐1.4) | 0.8 | (0.7‐1.0) |
| Non‐Hispanic black | 105 | 51.1 | (43.6 ‐ 58.6) | 1.1 | (0.9‐ 1.3) | 0.8 | (0.7‐1.0) |
| Non‐Hispanic other | 35 | 55.2 | (41.7 ‐ 68.7) | 1.2 | (0.9‐ 1.5) | 1.0 | (0.8‐1.3) |
| Highest educational attainment | |||||||
| College or greater | 143 | 29.8 | (25.0‐34.5) | 1.0 | ref | ─ | ─ |
| Some college | 246 | 51.9 | (46.9‐56.9) | 1.7 | (1.4‐2.1) | ─ | ─ |
| High school | 297 | 51.4 | (46.8‐56.1) | 1.7 | (1.4‐2.1) | ─ | ─ |
| Less than high school | 184 | 62.4 | (56.0‐68.9) | 2.1 | (1.7‐2.5) | ─ | ─ |
| Employment status | |||||||
| Employed | 192 | 31.0 | (26.8‐35.3) | 1.0 | ref | 1.0 | ref |
| Not working | 342 | 69.4 | (65.1‐73.8) | 2.2 | (1.9‐2.6) | 1.2 | (1.1‐1.4) |
| Retired | 338 | 47.1 | (43.0‐51.2) | 1.5 | (1.3‐1.8) | 1.0 | (0.9‐1.2) |
| Arthritis symptoms and effects | |||||||
| Severity of joint pain in past 7 days | |||||||
| None/mild (0‐3) | 106 | 21.3 | (17.3‐25.2) | 1.0 | ref | 1.0 | ref |
| Moderate (4‐6) | 363 | 49.8 | (45.8‐53.9) | 2.3 | (1.9‐2.9) | 1.2 | (1.0‐1.4) |
| Severe (7‐10) | 399 | 71.4 | (67.2‐75.7) | 3.4 | (2.8‐4.1) | 1.3 | (1.1‐1.6) |
| Severity of joint stiffness in past 7 days | |||||||
| None/mild (0‐3) | 156 | 25.4 | (21.7‐29.2) | 1.0 | ref | 1.0 | ref |
| Moderate (4‐6) | 336 | 52.3 | (47.9‐56.7) | 2.1 | (1.7‐2.4) | 1.1 | (1.0‐1.3) |
| Severe (7‐10) | 373 | 69.9 | (65.5‐74.2) | 2.7 | (2.3‐3.2) | 1.0 | (0.9‐1.2) |
| Severity of arthritis‐related fatigue in past 7 days | |||||||
| None/mild (0‐3) | 175 | 24.9 | (21.4‐28.4) | 1.0 | ref | … | … |
| Moderate (4‐6) | 285 | 52.9 | (48.2‐57.7) | 2.1 | (1.8‐2.5) | … | … |
| Severe (7‐10) | 391 | 76.2 | (71.9‐80.5) | 3.1 | (2.6‐3.6) | … | … |
| Arthritis‐Attributable limitation in whether one works | |||||||
| No | 443 | 35.8 | (32.8‐38.7) | 1.0 | ref | 1.0 | ref |
| Yes | 415 | 73.8 | (69.7‐78.0) | 2.1 | (1.9‐2.3) | 1.1 | (1.0‐1.3) |
| Arthritis interference with sleep in past 7 days | |||||||
| A little or no difficulty | 478 | 37.1 | (34.1‐40.1) | 1.0 | ref | … | … |
| A lot of difficulty | 391 | 72.5 | (68.4‐76.6) | 2.0 | (1.8‐2.2) | … | … |
| Arthritis‐Attributable life interference | |||||||
| None | 48 | 13.0 | (9.2‐16.7) | 1.0 | ref | 1.0 | ref |
| Modest | 257 | 35.1 | (31.2‐39.0) | 2.7 | (2.0‐3.7) | 1.6 | (1.3‐2.0) |
| Substantial | 568 | 79.9 | (76.8‐83.1) | 6.2 | (4.6‐8.3) | 2.5 | (1.9‐3.3) |
| Psychosocial | |||||||
| Confidence to manage arthritis symptoms | |||||||
| High | 434 | 38 | (34.8‐41.2) | 1.0 | ref | 1.0 | ref |
| Moderate | 303 | 59.3 | (54.4‐64.1) | 1.6 | (1.4‐1.8) | 1.1 | (1.0‐1.2) |
| No/Low | 116 | 73.4 | (65.9‐81.0) | 1.9 | (1.7‐2.2) | 1.2 | (1.0‐1.4) |
| Anxiety | |||||||
| No | 506 | 40.1 | (37.1‐43.2) | 1.0 | ref | … | … |
| Yes | 361 | 63.9 | (59.4‐68.4) | 1.6 | (1.4‐1.8) | … | … |
| Depression | |||||||
| No | 636 | 42.6 | (39.7‐45.4) | 1.0 | ref | … | … |
| Yes | 230 | 70.3 | (65.0‐75.6) | 1.7 | (1.5‐1.8) | … | … |
| Physical health | |||||||
| Body mass index (kilogram/meter2) | |||||||
| Under/normal (<25) | 206 | 38.2 | (33.7‐42.7) | 1.0 | ref | 1.0 | ref |
| Overweight (25‐<30) | 263 | 43.2 | (38.6‐47.7) | 1.1 | (1.0‐1.3) | 1.2 | (1.0‐1.3) |
| Obese (≥30) | 374 | 59.4 | (55.1‐63.8) | 1.6 | (1.4‐1.8) | 1.3 | (1.1‐1.5) |
| Physical activity level | |||||||
| Meets recommendations | 397 | 36.8 | (33.6‐40.1) | 1.0 | ref | 1.0 | ref |
| Insufficient | 210 | 51.6 | (46.3‐57.0) | 1.4 | (1.2‐1.6) | 1.2 | (1.0‐1.3) |
| Inactive | 266 | 76.5 | (71.6‐81.3) | 2.1 | (1.9‐2.3) | 1.4 | (1.2‐1.6) |
| General self‐rated health status | |||||||
| Very good/excellent | 153 | 25.4 | (21.5‐29.4) | 1.0 | ref | 1.0 | ref |
| Good | 249 | 41.3 | (36.8‐45.8) | 1.6 | (1.3‐2.0) | 1.1 | (1.0‐1.3) |
| Fair/Poor | 466 | 75.0 | (71.1‐78.8) | 2.9 | (2.5‐3.5) | 1.4 | (1.2‐1.6) |
Characteristics with ≥2% (n≥36) missing observations across the study sample: race/ethnicity (n=43), fatigue severity(n=38), body mass index (n=49).
Characteristics in the final model were selected through manual backward deletion at Wald alpha ≥0.10; all variables were entered in the initial model; final variables selected were: age, sex, race/ethnicity, employment status, severity of joint pain in past 7 days, severity of joint stiffness in past 7 days, work limited because of arthritis, arthritis‐attributable interference, confidence in ability to manage arthritis symptoms, body mass index, physical activity level, and general self‐rated health status.
Across all characteristics, at least half of respondents in at least one subgroup reported “a lot” of limitation walking for more than a mile. In the following subgroups, at least two‐thirds of respondents reported “a lot” of limitation (in order of frequency): substantial life interference (80%), physically inactive (77%), severe fatigue (76%), fair/poor self‐rated health (75%), arthritis‐attributable limitation in whether one works (74%), no or low confidence in managing arthritis symptoms (73%), a lot of arthritis‐attributable interference with sleep (73%), severe joint pain (71%), severe joint stiffness (71%), depression (70%), and not working (69%).
Patterns in “any” limitation were similar, but the percentage of people reporting “any” limitation was considerably greater (at least 75% for many subgroups) (Appendix).
Walking limitations by age and by age and sex (Figure 2)
Figure 2.
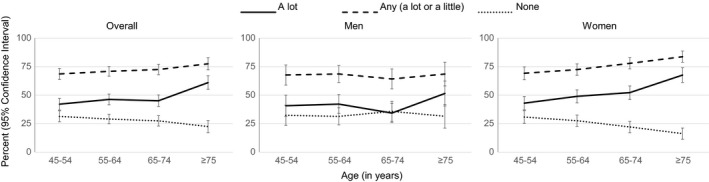
Level of difficulty walking more than 1 mile, by age.
Level of walking limitations (“any,” “a lot,” and none) for more than 1 mile overall is presented in the leftmost panel of Figure 2, men in the center, and women in the rightmost panel. The dramatic increase at age 65 for “a lot” and “any” limitations and a corresponding decrease in no limitation is clear in all three panels. Overall, Figure 2 also demonstrates the high percentage of walking limitations among middle‐aged adults (45‐54 and 54‐64 years) with more than two‐thirds (68%) reporting “any” limitation walking more than 1 mile.
The percentage of women reporting limitations is greater with increasing age, whereas it remains relatively stable for men across age groups (Figure 2, center and right panels). The increase in “a lot” of walking limitation that begins at age 65 is slightly more pronounced for men. Overall, however, the gap for walking limitations between women and men widens with age, resulting in substantially larger percentages of walking limitations among the oldest (75 years or older) women compared with men. Importantly, walking limitation is high for both sexes (34% (a lot, 65‐74 years) to 69% (any, 55‐64 and 75 years or older) for men; 43% (a lot, 45‐54 years) to 84% (any, 75 years or older) for women) at all ages.
Regression analyses
The univariable association of three characteristics had PRs of 3.0 or greater: substantial life interference (PR = 6.2, 95% CI = 4.6‐8.3), severe join pain (PR = 3.4, 95% CI = 2.8‐4.1), and severe fatigue (PR = 3.1, 95% CI = 2.6‐3.6).
In the multivariable model, statistically significant associations were observed for substantial and modest life interference (PR = 2.5, 95% CI = 1.9‐3.3 and PR = 1.6, 95% CI = 1.3‐2.0, respectively); age 75 years or older (PR = 1.5, 95% CI = 1.3‐1.7); inactive (PR = 1.4, 95% CI = 1.2‐1.6); fair/poor self‐rated health (PR = 1.4, 95% CI = 1.2‐1.6); severe joint pain (PR = 1.3, 95% CI = 1.4‐1.6); obese (PR = 1.3, 95% CI = 1.1‐1.5); and not working (PR = 1.2, 95% CI = 1.1‐1.4).
Discussion
In this study of walking limitations among middle‐aged and older adults with arthritis, the prevalence of “a lot” of limitations was very high, reported by 48% of respondents for distances of more than a mile. Importantly, the percentages with walking limitation were high for both sexes and for middle age and older ages. We found strong associations between potentially modifiable characteristics—eg, arthritis symptoms 27, 28, substantial life interference 29, 30, 31, 32, and physical inactivity 1and walking limitations in this population.
Several characteristics were associated with “a lot” of limitation. Logically, people develop limitations for longer walking distances before shorter walking distances. By this reasoning, those reporting “a lot” of limitation walking for more than a mile constitute a priority population for intervention because these individuals are probably early in the development of disability. Those who reported “a little” or “any” limitation in walking more than a mile may be an even more promising early intervention/prevention target group. Fortunately, evidence‐based public health and clinical interventions are available to mitigate walking limitations for all levels of function.
Evidence‐based community‐delivered physical activity and self‐management education interventions (see: https://www.cdc.gov/arthritis/interventions/index.htm ) are a promising area of community‐clinical linkages to manage and reduce arthritis effects. One of these programs focuses specifically on walking. Walk With Ease is designed to be delivered in a group by a trained leader or used as a self‐directed program. The group meets three times a week and features a prewalk discussion, warm‐up, 10‐40 minute walk, and cooldown 2. In addition to walking being an optimal method for meeting aerobic physical activity recommendations because of its availability, lack of expense, low impact, and negligible equipment requirements 1, maintaining and improving the ability to walk distances relevant for daily life is a strategy to retain community engagement and independnce. For example, a rule of thumb in community design is that people will typically be willing to walk about 10 minutes (interpreted as about 0.5 miles (0.8 km)) to get between community destinations, and policies are currently being encouraged to make this kind of walking easier and more accessible 33. Ability to walk these distances allows individuals to engage in community recreation, leisure time activities, active transport, and, ultimately, to meet physical activity recommendations through a no‐cost and highly accessible form of exercise, making them meaningful targets. Additionally, minimum expected gait speeds for pedestrians to clear crosswalks are typically set at 3.0‐4.0 feet/second (0.91‐1.2 m/s) 34, with evidence that slower gait speeds are associated with inability to cross streets independently 35. In a separate study among adults with or at high risk for knee OA, gait speed less than 1.2 m/s was associated with 2.1 times the odds of the worst depressive symptom trajectory compared with those without slow gait speed 36. So, maintaining or regaining walking ability has a variety of personal, social, and other benefits.
Although walking itself may be particularly appealing to people with arthritis because it is simple and its general safety may assuage some fears about injury 3, additional evidence‐based interventions are available to improve the health and well‐being of people with arthritis. EnhanceFitness is another group‐based intervention program that is specifically aimed at physical activity and is designed to improve flexibility, balance, aerobic capacity, and incorporate strength training exercises. Additional evidence‐based physical activity programs are available, however, for those who are too intimidated or otherwise not ready to begin an actual physical activity program. Self‐management education programs (eg, Chronic Disease Self‐Management Program (CDSMP), Tomando Control de su Salud (Spanish CDSMP), Arthritis Self‐Management Program) that focus on problem solving, evaluating appropriate exercise and treatments, medication management, and effective communications are also available. These courses result in significant improvements in exercise, social and household abilities, increased confidence in condition management, and less depression, fear/frustration, worry about health, and reduced pain.
Both cycling and community‐delivered aquatics programs can also improve outcomes (pain, function 37, flexibility, and strength 38) that improve ability to walk and are effective options for physical activity and the benefits it confers. Additionally, men and women have the same responses to exercise interventions for functional health (eg, walking), so these benefits apply equally 1. However, women may have a greater need for intervention, as demonstrated in our study and in reports of higher physiological and functional status in men compared with women at all ages 1.
Clinically, among people with chronic hip or knee pain, mobility problems are the most strongly associated characteristic with seeking a health care consultation (OR = 2.6, 95% CI = 1.6‐4.2) 39, suggesting that health care providers need to consider virtually anyone with chronic hip and knee pain as a good candidate for a mobility assessment and for referral to community‐delivered public health interventions. People with arthritis who experience walking disability may benefit from working with a physical therapist to identify and treat underlying causes. Reducing sedentary behavior, particularly for adults with mobility disability, can result in meaningful health gains and potential improvement in walking ability, regardless of reaching moderate/vigorous activity levels 40.
This study is subject to at least four limitations. First, all variables were based on self‐report, including the walking measure. We used a walking question from a standard instrument (SF‐12) with high reliability 18. The extent and direction of misclassification in difficulty of walking is unclear: one study found difficulty in walking was slightly overreported 41, but another found this differed by characteristics, such as race 42. The case finding question used to identify people with self‐reported, doctor‐diagnosed arthritis has high positive predictive value for arthritis diagnosis (45‐64 years = 74.9%; ≥65 years = 91.0%) and is valid for public health surveillance purposes 16, 43. Second, because they were not measured in ACHES, we were unable to examine some characteristics that have been linked to walking disability (eg, comorbidities such as cardiovascular disease 44, chronic obstructive pulmonary disease 12, 45, cognitive function 45, and fear of falling 45), or physical environment features that can serve as barriers (eg, lack of sidewalks) or facilitators (eg, benches for resting) to walking 46, 47. Third, consistent with declining contact rates for national random‐digit‐dial surveys in general, the overall response rate for ACHES was low. We took several steps at multiple study stages 16 to improve the generalizability of results to the target population (US adults that were 45 years or older with arthritis). Importantly, ACHES sampling weights, which accounted for survey nonresponse and undercoverage, were applied in all analyses. These weights were also calculated to match the weighted distributions of age, sex, race/ethnicity, and employment status of US adults 45 years or older with arthritis from the National Health Interview Survey, a standard in public health surveillance. Fourth, these data are cross sectional and cannot be used to infer causation. Our study examines walking limitation among adults with arthritis but cannot attribute all walking limitation in this population to arthritis alone.
Our study also has important strengths and extends the literature by including estimates for middle‐aged adults with arthritis (ie, 45‐55 years old) for whom data on mobility and walking limitation have been sparse. We also featured an infrequently studied measure of distance—more than 1 mile—and identified multiple modifiable characteristics that can be addressed though evidence‐based interventions. Because ACHES measured a range of variables, including symptoms and psychosocial characteristics, we were able to examine multiple characteristics that have not been measured in other surveys that are relevant to the daily lives of people with arthritis; furthermore, our sample size was sufficiently large to detect small (eg, PR < 1.5), statistically significant associations in multivariable adjusted models.
In conclusion, we found that walking limitation is substantial among middle‐aged and older adults with arthritis, being perhaps even more common than previously recognized, especially among younger (45‐64 years) age groups. By characterizing which groups have the highest levels of limitations, we have identified target groups in need of interventions to improve mobility, increase quality of life, and, potentially, delay or prevent disability.
Author Contributions
All authors drafted the article or revised it critically for important intellectual content as well as gave final approval of the version of the article to be published.
Study conception and design
Theis, Murphy, Baker, Hootman.
Acquisition of data
Theis, Murphy.
Analysis and interpretation of data
Theis, Murphy, Baker, Hootman.
Supporting information
Acknowledgments
We would like to thank Battelle staff for coordinating the Arthritis Conditions and Health Effects Survey (ACHES), the ACHES steering committee for their time and expertise, and, especially, the ACHES respondents for their participation in this study. We also gratefully acknowledge graphics input from Mr. Glen Murray and valuable comments during manuscript preparation from Dr. Jeffrey J. Sacks.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Informed consent was obtained from all individual participants included in the study.
This study was performed as part of regular duties by federal employees; no additional funding was granted.
K. A. Theis, PhD, L. B. Murphy, PhD, JM Hootman, PhD: Centers for Disease Control and Prevention, Atlanta, Georgia; 2N. A. Baker, ScD: Tufts University, Medford, Massachusetts.
No potential conflicts of interest relevant to this article were reported.
This article has been contributed to by US Government employees and their work is in the public domain in the USA.
References
- 1. U.S. Department of Health and Human Services . Physical Activity Guidelines for Americans, 2nd edition 2018. URL: https://health.gov/paguidelines/second-edition/pdf/Physical_Activity_Guidelines_2nd_edition.pdf.
- 2. Callahan LF, Shreffler JH, Altpeter M, Schoster B, Hootman J, Houenou LO, et al. Evaluation of group and self‐directed formats of the Arthritis Foundation's Walk With Ease Program. Arthritis Care Res (Hoboken) 2011;63:1098–107. [DOI] [PubMed] [Google Scholar]
- 3. Der Ananian C, Wilcox S, Saunders R, Watkins K, Evans A. Factors that influence exercise among adults with arthritis in three activity levels. Prev Chronic Dis 2006;3:A81. [PMC free article] [PubMed] [Google Scholar]
- 4. White DK, Tudor‐Locke C, Zhang Y, Fielding R, LaValley M, Felson DT, et al. Daily walking and the risk of incident functional limitation in knee OA: an observational study. Arthritis Care Res (Hoboken) 2014;66:1328–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cisternas MG, Murphy LB, Carlson SA. Walking and the 2‐year risk of functional decline: an observational study of US adults with arthritis. Prev Med 2019;119:100–7. [DOI] [PubMed] [Google Scholar]
- 6. Hootman JM, Theis KA, Barbour KE, Paul P, Carlson SA. Leisure time and transportation walking among adults with and without arthritis in the United States, 2010. Arthritis Care Res (Hoboken) 2019;71:178–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Covinsky KE, Lindquist K, Dunlop DD, Gill TM, Yelin E. Effect of arthritis in middle age on older‐age functioning. J Am Geriatr Soc 2008;56:23–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. James BD, Boyle PA, Buchman AS, Bennett DA. Relation of late‐life social activity with incident disability among community‐dwelling older adults. J Gerontol A Biol Sci Med Sci 2011;66:467–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Weinberger MI, Raue PJ, Meyers BS, Bruce ML. Predictors of new onset depression in medically ill, disabled older adults at 1 year follow‐up. Am J Geriatr Psychiatry 2009;17:802–09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Heesh KC, van Uffelen JG, van Gellecum YR, Brown WJ. Dose‐response relationships between physical activity, walking and health‐related quality of life in mid‐age and older women. J Epidemiol Community Health 2012;66:670–7. [DOI] [PubMed] [Google Scholar]
- 11. Guccione AA, Felson DT, Anderson JJ, Anthony JM, Zhang Y, Wilson PW, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health 1994;84:351–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Verbrugge LM, Lepkowski JM, Konkol LL. Levels of disability among U.S. adults with arthritis. J Gerontol 1991;46:S71–83. [DOI] [PubMed] [Google Scholar]
- 13. Theis KA, Murphy L, Hootman JM, Wilkie R. Social participation restriction among US adults with arthritis: a population‐based study using the International Classification of Functioning, Disabilty and Health. Arthritis Care Res (Hoboken) 2013;65:1059–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lusa AL, Amigues I, Kramer HR, Dam T, Giles JT. Indicators of walking speed in rheumatoid arthritis: relative influence of articular, psychosocial, and body composition characteristics. Arthritis Care Res (Hoboken) 2015;67:21–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. U.S. Department of Health and Human Services . Step It Up! The Surgeon General's Call to Action to Promote Walking and Walkable Communities. 2015. URL: https://www.hhs.gov/sites/default/files/call-to-action-walking-and-walkable-communites.pdf. [PubMed]
- 16. Theis KA, Murphy L. Arthritis Conditions Health Effects Survey (ACHES) Data Documentation. 2011. URL: https://www.cdc.gov/arthritis/data_statistics/pdf/TheisACHES.pdf.
- 17. Council of American Survey Research Organizations. URL: http://www.casro.org.
- 18. Ware JE, Kosinski MA, Dewey J. How to Score Version 2 of the SF‐36® Health Survey. Lincoln, RI: QualityMetric, Inc.; 2000. [Google Scholar]
- 19. Guralnik JM, LaCroix AZ, Abbott RD, Berkman LF, Satterfield S, Evans DA, et al. Maintaining mobility in late life. I. Demographic characteristics and chronic conditions. Am J Epidemiol 1993;137:845–57. [DOI] [PubMed] [Google Scholar]
- 20. Brady TJ, Murphy L, O'Colmain BJ, Beauchesne D, Daniels B, Greenberg M, et al. A meta‐analysis of health status, health behaviors, and health care utilization outcomes of the Chronic Disease Self‐Management Program. Prev Chronic Dis 2013;10:120112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kapstad H, Hanestad B, Langeland N, Rustoen T, Stavern K. Cutpoints for mild, moderate and severe pain in patients with osteoarthritis of the hip or knee ready for joint replacement surgery. BMC Musculoskelet Disord 2008;9:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Theis KA, Brady TJ, Helmick CG, Murphy L, Barbour KE. Arthritis‐attributable interference with routine life activities: a modifiable source of compromised quality‐of‐life. ACR Open Rhematology 2019. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Söderlin MK, Hakala M, Nieminen P. Anxiety and depression in a community‐based rheumatoid arthritis population. Scand J Rhematol 2000;29:177–83. [DOI] [PubMed] [Google Scholar]
- 24. Hawley DJ, Wolfe F. Depression is not more common in rheumatoid arthritis: a 10‐year longitudinal study of 6,153 patients with rheumatic disease. J Rheumatol 1993; 20: 2025–31. [PubMed] [Google Scholar]
- 25. SUDAAN, software for the statistical analysis of correlated data: release 11.0. Research Triangle Park, NC: Research Triangle Institute; 2012. [Google Scholar]
- 26. Fleiss J. Reasons for and warnings against standardization In: Statistical Methods for Rates and Proportions. 2nd ed New York: John Wiley; 1981. p. 629. [Google Scholar]
- 27. Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies for osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2012;64:465–74. [DOI] [PubMed] [Google Scholar]
- 28. Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treatment guidelines and systematic review of current research evidence. Osteoarthritis Cartilage 2007;15:981–1000. [DOI] [PubMed] [Google Scholar]
- 29. Katz PP, Yelin EH. Activity loss and the onset of depressive symtpoms: do some activities matter more than others? Arthritis Rheum 2001;44:1194–202. [DOI] [PubMed] [Google Scholar]
- 30. Katz P, Morris A, Gregorich S, Yazdany J, Eisner M, Yelin E, et al. Valued life activitiy disability played a significant role in self‐rated health among adults with chronic health conditions. J Clin Epidemiol 2009;62:158–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gignac MA, Backman CL, Davis AM, Lacaille D, Mattison CA, Montie P, et al. Understanding social role participation: what matters to people with arthritis? J Rheumatol 2008;35:1655–36. [PubMed] [Google Scholar]
- 32. Ahlstrand I, Björk M, Thyberg I, Börsbo B, Falkmer T. Pain and daily activities in rheumatoid arthritis. Disabil Rehabil 2012;34:1245–53. [DOI] [PubMed] [Google Scholar]
- 33. Chriqui JF, Thrun E, Sanghera A. Components of local land development and related zoning policies associated with increased walking: a primer for public health practitioners. 2018. URL: https://www.ihrp.uic.edu/files/Zoning_Primer_508.pdf.
- 34. U.S. Department of Transportation Federal Highway Administration . Traffic Signal Timing Manual. 2017. URL: https://ops.fhwa.dot.gov/publications/fhwahop08024/chapter5.htm.
- 35. Langlois JA, Keyl PM, Guralnik JM, Foley DJ, Marottoli RA, Wallace RB. Characteristics of older pedestrians who have difficulty crossing the street. Am J Public Health 1997;87:393–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. White DK, Neogi T, Zhang Y, Niu J, Katz PP. Association of slow gait speed with trajectories of worsening depressive symptoms in knee osteoarthritis: an observational study. Arthritis Care Res (Hoboken) 2017;69:209–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Salacinski AJ, Krohn K, Lewis SF, Holland ML, Ireland K, Marchetti G. The effects of group cycling on gait and pain‐related disability in individuals with mild‐to‐moderate knee osteoarthritis: a randomized controlled trial. J Orthop Sports Phys Ther 2012;42:985–95. [DOI] [PubMed] [Google Scholar]
- 38. Wang TJ, Belza B, Thompson EF, Whitney JD, Bennett K. Effects of aquatic exercise on flexibility, strength and aerobic fitness in adults with osteoarthritis of the hip or knee. J Adv Nurs 2007;57:141–52. [DOI] [PubMed] [Google Scholar]
- 39. Thorstensson CA, Gooberman‐Hill R, Adamson J, Williams S, Dieppe P. Help‐seeking behaviour among people living with chronic hip or knee pain in the community. BMC Musculoskelet Disord 2009;10:153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Dunlop DD, Song J, Arnston EK, Semanik PA, Lee J, Chang RW, et al. Sedentary time in US older adults associated with disability in activities of daily living independent of physical activity. J Phys Act Health 2015;12:93–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Beauchamp MK, Leveille SG, Patel KV, Kiely DK, Phillips CL, Bandinelli S, et al. What physical attributes underlie self‐reported vs. observed ability to walk 400 m in later life? An analysis from the InCHIANTI Study. Am J Phys Med Rehabil 2014;93:396–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Burns R, Graney MJ, Lummus AC, Nichols LO, Martindale‐Adams J. Differences of self‐reported osteoarthritis disability and race. J Natl Med Assoc 2007;99:1046–51. [PMC free article] [PubMed] [Google Scholar]
- 43. Sacks JJ, Harrold LR, Helmick CG, Gurwitz JH, Emani S, Yood RA. Validation of a surveillance case definition for arthritis. J Rheumatol 2005;32:340–7. [PubMed] [Google Scholar]
- 44. Nüesch E, Dieppe P, Reichenbach S, Williams S, Iff S, Jüni P. All cause and disease specific mortality in patients with knee or hip osteoarthritis: population based cohort study. BMJ 2011;342:d1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bootsma‐van der Wiel A, Gussekloo J, De Craen AJ, Van Exel E, Bloem BR, Westendorp RG. Common chronic diseases and general impairments as determinats of walking disability in the oldest‐old population. J Am Geriatr Soc 2002;50:1405–10. [DOI] [PubMed] [Google Scholar]
- 46. Keysor JJ, Jette AM, LaValley MP, Lewis CE, Torner JC, Nevitt MC, et al. Community environmental factors are associated with disability in older adults with functional limitations: the MOST study. J Gerontol Series A Biol Sci Med Sci 2010;65:393–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Theis KA, Furner S. Shut‐In? Impact of chronic conditions on community participation restriction among older adults. J Aging Res 2011:759158. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


