Abstract
Objective
To analyse mortality trends of liver diseases in China over the past 30 years.
Design
Age-period-cohort analyses were applied to liver diseases data obtained from the Chinese Health Statistics Annual Report (1987–2001) and the Chinese Health Statistics Yearbook (2003–2017).
Setting
General population in mainland China.
Outcomes
Mortality rates and age, period and cohort effects on three categories of liver diseases: primary liver cancer (PLC), chronic liver disease and cirrhosis (CLD), and viral hepatitis (VH).
Results
A total of 13.54 million deaths were attributable to liver diseases over the period between 1987 and 2016, resulting in an average of 36.15 deaths per 100 000 population per year. The risk of PLC mortality increased by 32.69% over the period after controlling for the effects of age and birth cohort. By contrast, the risk of CLD mortality decreased by 56.64% over the same period. The risk of VH mortality decreased first, followed by a resurgence after the period of 2002–2006. Similar mortality risk trends by age (increasing) and birth cohort (decreasing) were observed for PLC and CLD. The year 1952 represented a turning point for VH, with people born after 1950 experiencing a declining risk of VH mortality.
Conclusions
China has achieved great success in reducing the mortality of VH and CLD. However, significant challenges lie ahead in the efforts to prevent and control PLC and the resurgence of VH.
Keywords: China, liver diseases, virus hepatitis, primary liver cancer, chronic liver disease and cirrhosis, intrinsic estimator (IE)
Strengths and limitations of this study.
This is the first study that jointly analysed and compared the age, period and cohort effects on mortality due to VH, PLC and CLD in China.
The data covered a long-term period of three decades from 1987 to 2017, during which China had experienced huge socioeconomic and health system transitions.
Only population-level data were used for the analysis, and there was no individual-level clinical information included.
Diagnostic accuracy and misclassification might have affected the results.
Introduction
The burden of liver diseases has become a severe public health concern globally, not just in countries with a high prevalence of viral hepatitis. Deaths resulting from liver diseases in developed nations such as the USA and European countries are also increasing due to non-viral risk factors such as alcohol consumption.1–3 Globally, it was estimated that 2.06 million people (28.53 per 100 000 population) died from liver diseases in 2015. This represented a 23.35% increase compared with the figure in 2000 and accounted for 3.71% of the total deaths in 2015. Liver diseases became the fifth leading cause of death after ischaemic heart disease, stroke, lower respiratory tract infection and chronic obstructive pulmonary disease.4 As a result, the WHO called for global efforts to curb the rising threat of liver diseases, with a particular focus on strategies to eliminate viral hepatitis and interventions to reduce related health risk behaviours, such as alcohol abuse.5 6
China has suffered the most from the burden of liver diseases, with 300 million people being affected and 550 000 dying from liver diseases in 2015 alone.4 7 The hepatitis virus has been a major risk for liver diseases in China. But a dramatic decline in hepatitis B virus (HBV) infection has been evident over the past few decades due to a series of interventional strategies, including vaccinations and better medical infection control.8–10 Compared with 1992, the prevalence of hepatitis B surface antigen declined by 46% and 52% in 2006 and 2014, respectively.8–10 However, the risks associated with alcohol use and dietary problems are increasing.7 11 The annual alcohol consumption per capita in China has climbed from 3.3 L in 1987 to 5.74 L in 2016.12
Various liver diseases, including viral hepatitis (VH), primary liver cancer (PLC), and chronic liver disease and cirrhosis (CLD), are pathologically connected. It is important to draw out a comprehensive understanding of how the changing pattern of risk factors impacts on the mortality rates of various liver diseases in China by performing a systematic and comparative study. This could help to provide some new insights towards effective liver diseases control which could hardly be achieved by studies focused on a single liver disease or a specific risk factor.13 14 However, to the best of our knowledge, studies of this type are lacking. Herein, using macro-level, population-based vital surveillance data, we performed age-period-cohort (APC) analyses to decompose the variations in the mortality rates of VH, PLC and CLD from 1987 to 2016 by age, calendar period and birth cohort.
Methods
We examined the secular trends in mortality resulting from various liver diseases in mainland China from 1987 to 2016 using APC analysis, a method widely used for decomposing variations in secular trends of mortality or morbidity of diseases by age, period and cohort.3 15 16
Data source and processing
Year-specific and age-specific death data were extracted from the Chinese Health Statistics Annual Report (1987–2001) and the Chinese Health Statistics Yearbook (2003–2017). These reports/yearbooks collate data from the national death registry system (excluding Hong Kong, Macau and Taiwan). They were published officially and made available to the general public. Details about the reliability and validity of these data have been published elsewhere.17 The corresponding information on population counts by age groups was estimated using the four rounds of population census data in mainland China collected in 1982, 1990, 2000 and 2010.18
This study focused on deaths resulting from three broad categories of liver diseases: VH, PLC and CLD. They were identified through codes 070, 155 and 571 in the International Classification of Diseases (ICD)-9 before 2002, and codes B15-19, C22 and K70, 73–74 in ICD-10 from 2002 onwards.1
Age-specific mortality due to liver diseases was tabulated on a yearly basis, covering 16 age groups (from 5–9, 10–14, …, to 80–84 years), 6 periods (from 1987–1991, 1992–1996, …, to 2012–2016) and 21 overlapping birth cohorts (from 1903–1911, 1908–1916, …, to 2003–2011). The birth cohorts were labelled by the median year in each cohort (eg, 1907 for 1903–1911). The 0–4 years age group was excluded due to the extremely low incidence of deaths from PLC and CLD. The tabulated data were truncated at 84 years due to unavailability of age-specific mortality data beyond the age of 85 years.
Statistical analyses
We performed APC analyses, which can determine changes in mortality over time after adjustment for the effects of age and birth cohort. APC analyses have been widely applied in population-based studies across a range of disciplines, including but not limited to sociology, demography and epidemiology.19 20 The APC analysis adopts a general linear equation model, which can be expressed as the following:
where denotes the number of deaths of liver diseases in the th age group and th period; represents the number of people exposed to the risk in the th age group and th period; indicates the effect of age; indicates the effect of period; indicates the effect of cohort (k=i+ j−1); is the intercept or adjusted mean rate; and is the random error.
There is a linear dependency between age, period and cohort. Independent effects of age, period and cohort cannot be estimated without further constraints on the coefficients of the three variables. This is referred to as the ‘identification problem’ in APC analyses.21 There is an ongoing debate about the appropriateness of forcing constraints on coefficients (eg, assuming two adjacent groups have the same condition) to solve the ‘identification problem’.22
Recently, the intrinsic estimator (IE) approach was developed in APC analysis, which does not require prior knowledge of establishing constraints. The IE approach generates an intrinsic estimator, which is unique and is only determined by the structure of the observed data. It avoids the need to impose constraints on coefficients. Previous studies proved that the IE approach can generate a stable estimation on the influence of age, period and cohort effects in comparison with the approach imposing forced constraints on coefficients.22
In this study, we used the IE approach to conduct APC analyses. We established single-factor (A, P, C) and two-factor (AP, AC, PC) models, as well as the full APC model. The results were presented with relative risk ratios of death from liver diseases. The fitness of data to the models was assessed using the Akaike’s information criterion (AIC) and the Bayesian information criterion (BIC), with a lower value indicating a better model fit. We reported the results of the models with the lowest AIC and BIC values. We also performed subpopulation APC analyses by residency and gender (reported in online supplementary file, figures S1–S3). The analyses were performed using Stata, version 12.0.
bmjopen-2019-029793supp001.pdf (170.5KB, pdf)
Patient and public involvement
This study is retrospectively based on statistical data sources. There was no patient involved in the recruitment and conduct of the study.
Results
Temporal trends
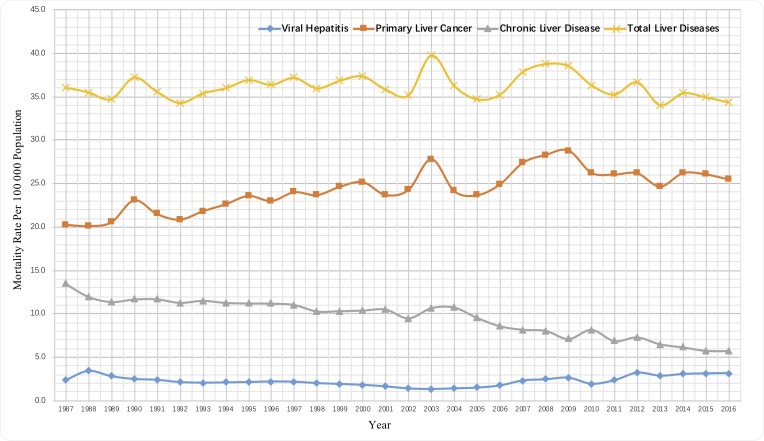
Over the past three decades, the three groups of liver diseases (VH, PLC and CLD) resulted in 13.54 million deaths in China, representing an average annual crude death rate (CDR) of 36.15 per 100 000 population and accounting for 5.22% of all deaths during 1987–2016. The overall annual CDR of liver diseases remained at a relatively stable level despite some fluctuations (figure 1). However, the composition of causes of deaths changed significantly over the years. PLC, CLD and VH contributed 56.16%, 37.36% and 6.48% of deaths from liver diseases, respectively, in 1987, compared with 74.18%, 16.64% and 9.17%, respectively, in 2016. The CDR of VH declined before a resurgence from 2004. In contrast, the CDR of PLC had been increasing, whereas the CDR of CLD had been decreasing.
Figure 1.
Trends of death rates from liver diseases in mainland China, 1987–2016.
APC model results
We report the results of the full APC analyses with the IE approach (table 1 and figure 2). The single-factor, two-factor and full APC models all indicate that the IE approach generated a good imitative effect (online supplementary file, table S1).
Table 1.
Effects of age, period and birth cohort on mortality due to viral hepatitis, primary liver cancer and chronic liver disease in mainland China
| Viral hepatitis | Primary liver cancer | Chronic liver disease | |||||||
| Coefficient | 95% CI | P value | Coefficient | 95% CI | P value | Coefficient | 95% CI | P value | |
| Intercept | −11.34 | −11.49 to −11.2 | <0.001 | −9.25 | −9.49 to −9.01 | <0.001 | −9.95 | −10.08 to −9.83 | <0.001 |
| Age (in group) | |||||||||
| 5–9 | −1.38 | −1.68 to −1.08 | <0.001 | −3.33 | −4.07 to −2.6 | <0.001 | −2.83 | −3.29 to −2.38 | <0.001 |
| 10–14 | −1.63 | −1.89 to −1.36 | <0.001 | −3.05 | −3.59 to −2.51 | <0.001 | −2.65 | −3.01 to −2.3 | <0.001 |
| 15–19 | −1.56 | −1.78 to −1.35 | <0.001 | −2.35 | −2.72 to −1.98 | <0.001 | −2.25 | −2.51 to −1.99 | <0.001 |
| 20–24 | −1.32 | −1.49 to −1.15 | <0.001 | −1.71 | −1.98 to −1.44 | <0.001 | −1.49 | −1.67 to −1.3 | <0.001 |
| 25–29 | −1.01 | −1.16 to −0.87 | <0.001 | −1.00 | −1.21 to −0.79 | <0.001 | −1.09 | −1.24 to −0.93 | <0.001 |
| 30–34 | −0.67 | −0.79 to −0.55 | <0.001 | −0.25 | −0.41 to −0.08 | 0.003 | −0.45 | −0.58 to −0.33 | <0.001 |
| 35–39 | −0.33 | −0.42 to −0.23 | <0.001 | 0.23 | 0.1 to 0.36 | 0.001 | 0.00 | −0.1 to 0.1 | 0.928 |
| 40–44 | 0.00 | −0.08 to 0.08 | 0.930 | 0.63 | 0.53 to 0.74 | <0.001 | 0.46 | 0.38 to 0.54 | <0.001 |
| 45–49 | 0.16 | 0.09 to 0.24 | <0.001 | 0.85 | 0.76 to 0.94 | <0.001 | 0.75 | 0.68 to 0.82 | <0.001 |
| 50–54 | 0.46 | 0.38 to 0.53 | <0.001 | 1.08 | 1 to 1.17 | <0.001 | 1.00 | 0.93 to 1.06 | <0.001 |
| 55–59 | 0.62 | 0.54 to 0.7 | <0.001 | 1.20 | 1.11 to 1.29 | <0.001 | 1.10 | 1.03 to 1.16 | <0.001 |
| 60–64 | 0.84 | 0.75 to 0.93 | <0.001 | 1.35 | 1.24 to 1.45 | <0.001 | 1.24 | 1.17 to 1.32 | <0.001 |
| 65–69 | 1.06 | 0.95 to 1.16 | <0.001 | 1.47 | 1.33 to 1.6 | <0.001 | 1.38 | 1.29 to 1.47 | <0.001 |
| 70–74 | 1.35 | 1.23 to 1.48 | <0.001 | 1.59 | 1.43 to 1.76 | <0.001 | 1.53 | 1.42 to 1.64 | <0.001 |
| 75–79 | 1.60 | 1.45 to 1.74 | <0.001 | 1.63 | 1.43 to 1.82 | <0.001 | 1.62 | 1.49 to 1.75 | <0.001 |
| 80–84 | 1.81 | 1.64 to 1.98 | <0.001 | 1.66 | 1.43 to 1.89 | <0.001 | 1.69 | 1.53 to 1.84 | <0.001 |
| Period (calendar year) | |||||||||
| 1987–1991 | 0.36 | 0.3 to 0.43 | <0.001 | −0.17 | −0.27 to −0.08 | <0.001 | 0.18 | 0.12 to 0.25 | <0.001 |
| 1992–1996 | 0.07 | 0.01 to 0.12 | 0.016 | −0.11 | −0.17 to −0.05 | 0.001 | 0.16 | 0.11 to 0.2 | <0.001 |
| 1997–2001 | −0.08 | −0.13 to −0.03 | 0.001 | 0.03 | 0 to 0.07 | 0.060 | 0.16 | 0.13 to 0.19 | <0.001 |
| 2002–2006 | −0.39 | −0.44 to −0.34 | <0.001 | 0.08 | 0.05 to 0.12 | <0.001 | 0.10 | 0.07 to 0.13 | <0.001 |
| 2007–2011 | −0.09 | −0.15 to −0.04 | <0.001 | 0.11 | 0.05 to 0.17 | <0.001 | −0.21 | −0.25 to −0.16 | <0.001 |
| 2012–2016 | 0.13 | 0.07 to 0.19 | <0.001 | 0.05 | −0.04 to 0.14 | 0.246 | −0.40 | −0.47 to −0.34 | <0.001 |
| Birth cohort (birth year) | |||||||||
| 1907 | 0.16 | −0.15 to 0.48 | 0.304 | 1.01 | 0.69 to 1.33 | <0.001 | 1.15 | 0.95 to 1.35 | <0.001 |
| 1912 | 0.23 | 0.01 to 0.45 | 0.037 | 0.99 | 0.74 to 1.25 | <0.001 | 1.04 | 0.89 to 1.19 | <0.001 |
| 1917 | 0.32 | 0.15 to 0.5 | <0.001 | 1.00 | 0.78 to 1.22 | <0.001 | 0.98 | 0.86 to 1.11 | <0.001 |
| 1922 | 0.52 | 0.37 to 0.67 | <0.001 | 1.03 | 0.83 to 1.23 | <0.001 | 0.95 | 0.85 to 1.06 | <0.001 |
| 1927 | 0.66 | 0.52 to 0.79 | <0.001 | 1.03 | 0.84 to 1.22 | <0.001 | 0.89 | 0.79 to 0.98 | <0.001 |
| 1932 | 0.72 | 0.59 to 0.84 | <0.001 | 0.95 | 0.76 to 1.13 | <0.001 | 0.76 | 0.67 to 0.85 | <0.001 |
| 1937 | 0.72 | 0.59 to 0.84 | <0.001 | 0.82 | 0.63 to 1.01 | <0.001 | 0.59 | 0.5 to 0.69 | <0.001 |
| 1942 | 0.76 | 0.63 to 0.9 | <0.001 | 0.70 | 0.5 to 0.9 | <0.001 | 0.45 | 0.35 to 0.56 | <0.001 |
| 1947 | 0.87 | 0.73 to 1.01 | <0.001 | 0.67 | 0.46 to 0.89 | <0.001 | 0.40 | 0.29 to 0.52 | <0.001 |
| 1952 | 0.92 | 0.77 to 1.07 | <0.001 | 0.62 | 0.39 to 0.86 | <0.001 | 0.33 | 0.19 to 0.46 | <0.001 |
| 1957 | 0.82 | 0.65 to 0.98 | <0.001 | 0.37 | 0.12 to 0.63 | 0.005 | 0.16 | 0.01 to 0.32 | 0.033 |
| 1962 | 0.80 | 0.62 to 0.98 | <0.001 | 0.24 | −0.04 to 0.52 | 0.097 | 0.09 | −0.08 to 0.26 | 0.295 |
| 1967 | 0.77 | 0.57 to 0.96 | <0.001 | 0.11 | −0.2 to 0.42 | 0.470 | 0.11 | −0.08 to 0.3 | 0.258 |
| 1972 | 0.54 | 0.33 to 0.76 | <0.001 | −0.18 | −0.52 to 0.16 | 0.308 | −0.10 | −0.32 to 0.11 | 0.349 |
| 1977 | 0.18 | −0.07 to 0.42 | 0.152 | −0.52 | −0.89 to −0.14 | 0.007 | −0.47 | −0.72 to −0.23 | <0.001 |
| 1982 | −0.12 | −0.39 to 0.15 | 0.375 | −0.73 | −1.15 to −0.3 | 0.001 | −0.86 | −1.15 to −0.56 | <0.001 |
| 1987 | −0.49 | −0.82 to −0.17 | 0.003 | −0.75 | −1.23 to −0.27 | 0.002 | −0.97 | −1.32 to −0.62 | <0.001 |
| 1992 | −0.95 | −1.37 to −0.54 | <0.001 | −1.15 | −1.75 to −0.55 | <0.001 | −1.13 | −1.57 to −0.69 | <0.001 |
| 1997 | −1.81 | −2.55 to −1.08 | <0.001 | −1.28 | −2.14 to −0.42 | 0.004 | −1.29 | −1.97 to −0.61 | <0.001 |
| 2002 | −2.76 | −4.22 to −1.3 | <0.001 | −2.53 | −4.94 to −0.12 | 0.040 | −1.98 | −3.45 to −0.5 | 0.009 |
| 2007 | −2.84 | −4.95 to −0.72 | 0.009 | −2.41 | −6.27 to 1.44 | 0.220 | −1.12 | −2.81 to 0.58 | 0.196 |
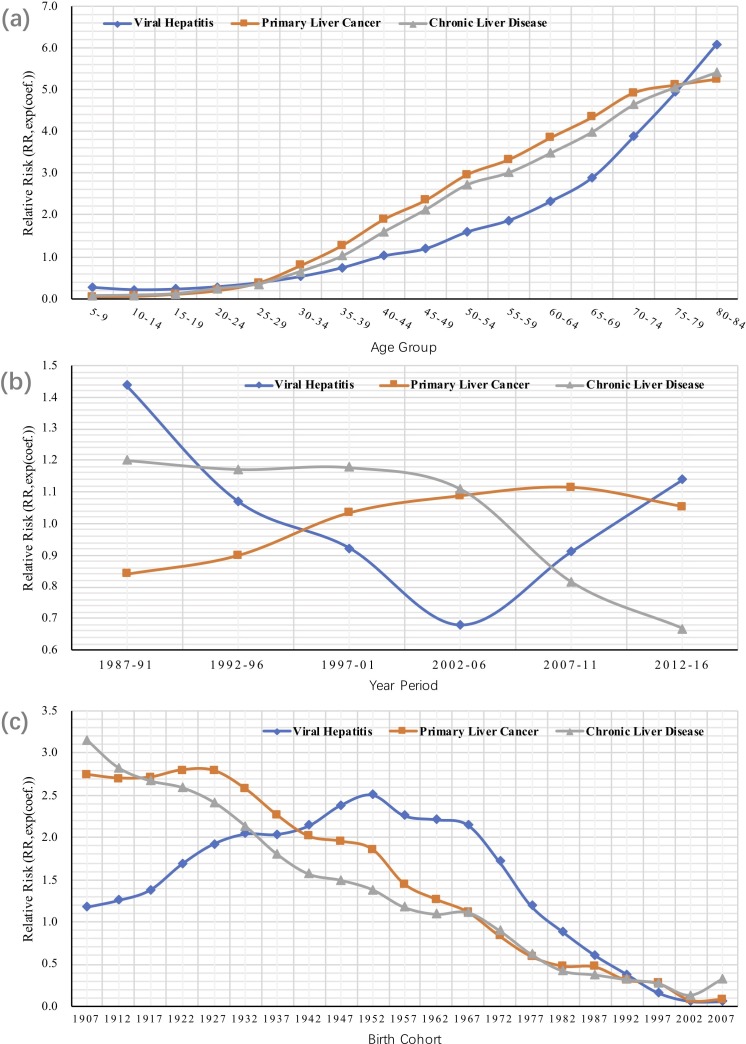
Figure 2.
Exponential coefficients of intrinsic estimator for (A) age, (B) period and (C) cohort effects on mortality due to viral hepatitis, primary liver cancer, and chronic liver disease and cirrhosis.
Age effect
The lowest mortality risk of VH was found in the 10–14 years age group. The VH mortality risk increased exponentially with age afterwards, with the rate in the 80–84 years age group being 31 times that of the 10–14 years age group.
Similarly, the mortality risk of PLC and CLD also increased with age. A linear correlation between age and the mortality risk of PLC and CLD was found in those whose age ranged from 15 years to 74 years. The highest mortality risk was found in the 80–84 years age group, this being 146.99 times greater for PLC and 91.86 times greater for CLD than those in the age range of 5–9 years.
Period effect
The risk of VH mortality declined from 1987–1991 to 2002–2006, followed by a resurgence from 2007 to 2011. It was lowest in 2002–2006, 47.12% that in 1987–1991, compared with 59.52% of the figure in 2012–2016.
The risk of PLC mortality increased from 1987 before it reached its peak in 2007–2011 (1.33 times that in 1987–1991) and then declined. The risk of PLC mortality dropped by 5.43% in 2012–2016 compared with its level in 2007–2011.
The risk of CLD mortality declined significantly from 2002 to 2006 despite it being relatively stable from 1987 to 2001. The risk of CLD mortality in 2012–2016 was 56.64% that in 1997–2001.
Cohort effect
The risk of VH mortality increased for those born between 1907 and 1952 (2.13 times that of the 1907 cohort), after which it declined. The drop accelerated from the 1972 cohort. The risk of VH mortality for those who were born in 2007 was 2.33% of those born in 1952.
The mortality risk of PLC and CLD shared a similar declining trend overall, but with a slight resurgence in the most recent cohort (2007) of the populations. The highest risk of PLC mortality occurred in those born in 1922, this being 35.2 times higher than those born in 2002. In contrast, the highest risk of CLD mortality was found in those born in 1907, this being 22.8 times higher than those born in 2002. But the mortality risk increased by 12.73% for PLC and 135.34% for CLD for those born in 2007 compared with those born in 2002.
Discussion
Over the past 30 years, China has achieved great progress in population health, with life expectancy increasing from 68.84 years in 1987 to 76.25 years in 2016.23 But the high mortality rate from liver diseases remains a significant challenge. This study reveals, despite some fluctuations, the overall mortality rates from liver diseases in China have been stagnant at a high level. Deaths from liver diseases still accounted for 5.72% of all deaths in 2015. This is significantly higher than in the USA (2.73%), England (2.16%), Australia (2.05%) and Japan (3.87%).4 However, the number of deaths resulting from the various liver diseases has changed significantly in China during the same period. While similar to the trends observed in developed countries,1 15 16 24 CLD mortality rates have declined dramatically in China, and PLC mortality rates have risen continually over the same period. Furthermore, VH mortality rates started to rise in 2004 after more than a decade of decline.
Based on the aforementioned changing profile of mortality due to the three main categories of liver diseases, our findings of the APC analyses, which would be discussed in the following paragraphs, provided important implication for the future efforts to curb liver diseases in China and in other parts of the world as well. To our knowledge, no previous study has analysed the mortality trends of VH and CLD in China using the APC model, nor have any studies undertaken a comprehensive analysis of the changing profiles of deaths resulting from liver diseases. Using an APC model to compare changes in the mortality risk of multiple liver diseases can assist us to develop a better understanding of the impact of liver diseases and enable us to develop appropriate strategies for the prevention and control of liver diseases. Our finding regarding age effects on liver diseases might be well generalisable outside the population in mainland China, and the cohort and period effects, although largely subject to a China-specific context, might still be referential for other countries that have experienced similar transitions.
Mortality due to VH
The changing trend in the CDR of VH is aligned with the period effect, reflecting the achievements and challenges China has been facing in the prevention and control of VH. The decline in the risk of VH mortality from the period of 1987–1991 to 2002–2006 is perhaps a reflection of the success of vaccination campaigns against hepatitis viruses. China licensed the world’s first live attenuated liquid hepatitis A virus (HAV) vaccine in 1992. Since the same year, the HAV vaccine has been offered in schools and universities, as well as to those who were vulnerable and had close contact with those infected with HAV.8 25 26 This coincides with the dramatic drop in VH mortality for those born between 1970 and 1974 as this group was the cohort who received the vaccination either at school or university. Indeed, HAV infections dropped from 55.7 per 100 000 people in 1991 to less than 5 per 100 000 people in 2004.27 Adding to the achievement of the HAV vaccination, the three-dose HBV vaccine was also introduced in 1992 and was made accessible to newborn babies, resulting in reduced deaths from HBV.27 The impact of vaccination was also indicated by the results of cohort effects which demonstrate the influences of specific events on specific birth cohorts.28 The cohort effects on VH mortality have decreased dramatically among those born after the early 1970s, who were the earliest generations to be vaccinated against VH in China.
However, the period effects on VH mortality have been increasing again from 2002 to 2006 onwards after reaching the bottom and have reached the same level of the early 1990s in 2012–2016. The emerging challenges in VH prevention and control, which have already caused a resurgence in VH mortality, are mainly due to the increasing epidemic of hepatitis E virus (HEV) and hepatitis C virus (HCV) in more recent years. Regarding HEV, although the number of reported deaths resulting from HBV remained largely unchanged since 2007, accounting for nearly 80% of all VH deaths in China,1 4 27 29 the incidence and mortality rate of HEV rose, overtaking those of HAV in 2011 and 2004, respectively.26 27 30 It is anticipated that the availability of the HEV vaccine may eventually curb the rising epidemic of HEV.10 Regarding HCV, it has attracted growing concerns in recent years. Effective vaccines for HCV are still not available. The number of reported HCV cases in China exceeded 20 000 in 2012, nearly 10 times the cases reported in 2003.29 The number of reported deaths resulting from HCV in 2013 was almost double that in 2004.27
Mortality due to CLD
A dramatic decline in the risk of CLD mortality is evident after the period of 2002–2006, in contrast to the resurgence in the risk of VH mortality. Like lessons from other countries, the declining trends in CLD mortality usually occur in countries with a better healthcare system, especially the existence of universal health coverage.24 It is also plausible to infer that this decrease in CLD mortality is likely to be attributed to China’s health system strengthening in recent decades. Because, in China, 67.49% of patients who died from CLD in 2013 were infected by hepatitis viruses,31 and statistical evidence showed the behavioural risk of CLD, including alcohol consumption, has continued to increase in the past few decades in China.12
The current Chinese health system started to take shape in 2003, when the central government decided to introduce universal health insurance coverage for all citizens. The new rural cooperative medical scheme and urban resident basic medical scheme subsidised by the government were introduced in 2003 and 2007, respectively. Along with the urban employee-based basic medical scheme, social health insurance covers almost every citizen, enhancing the accessibility and affordability of medical services significantly32 (see online supplementary figure S1). In 2005, the national guidelines for chronic HBV antiviral therapy were released in China to promote early detection and treatment of chronic HBV infections.33 In 2009, the essential public health services package was introduced to all community health services, ensuring equal access to public health services, including those related to the prevention and control of VH.
Our supplementary analysis further supported above speculation by showing rural residents, who are generally more disadvantaged and hence might benefit more from the enhanced health system, have experienced a more pronounced decline in the risk of CLD mortality compared with urban residents (see online supplementary figure S2).
Mortality due to PLC
PLC and CLD share similar risk factors. This is evident in this study given that the effects of age and birth cohort on the mortality risk of PLC and CLD have followed very similar trends over the past 30 years. However, unlike CLD, the risk of PLC mortality increased throughout the study except for the most recent decline after the period of 2007–2011, which is consistent with another APC study undertaken in China using another data set (Disease Surveillance Points data of Chinese Center for Disease Control and Prevention) for the period from 1991 to 2014.33
The difference in period effects between PLC and CLD might be due to PLC being one of the cancers that are difficult to detect at an early stage, which leads to poor prognosis. This may jeopardise the effects of improved healthcare systems on PLC mortality as argued by researchers in the USA.1 Meanwhile, the increase in chronic hepatitis virus infections and alcohol consumption in China may shed some light on the difficulties in containing PLC mortality. In some European countries such as the UK, alcohol use has become the main risk of deaths from liver diseases.2 3 To explore the role of alcohol consumption on deaths from PLC and CLD in China, we performed APC analyses by gender (see online supplementary figure S3–S4). Because men consume much more alcohol than women, 33 times more in China,11 it is reasonable to assume a great gender disparity in both PLC and CLD mortality could be attributed to difference in alcohol consumption between genders.34 Future studies would be needed to further test this hypothesis in China.
The risk of PLC mortality declined slightly after the period of 2007–2011, which was also observed in a previous study.33 Although we cannot assume that this is a permanent change, there are signs it is trending in a positive direction. Recent studies have revealed declining chronic infections of the hepatitis virus in the Chinese population.35 36 The new developments in HCV therapy and advancements in the medical treatment of PLC bring hope that the prognosis of PLC will be improved.37
This study has several limitations. The data for this study were derived from statistical reports, not from individual clinical records. We were unable to further track the specific causes of deaths in the analyses. It is not clear what percentage of patients who died from PLC and CLD were infected with hepatitis viruses. However, we were able to reveal the overall trend of the mortality rate from liver diseases. The two sources of data are reliable, representative and authoritative. We explored the roles of different risk factors on the APC effects. However, we were not able to consider diet risk factors and obesity due to the unavailability of data. Some studies predict that obesity will gradually replace hepatitis virus infections as the main driver of CLD and PLC morbidity and mortality in China and the world in the future.1 7
Another potential limitation we have to acknowledge is that the possible bias induced by changes in the diagnostic accuracy of the cause of death from liver diseases over time and across urban and rural areas is inevitable in our long-term trends analysis, as we were looking into trends over nearly three decades, during which period China had made impressive economic and social development and its health system has experienced dramatic improvements. Chinese residents’ use of healthcare and the quality of care had largely enhanced. Alongside this trend, the diagnostic accuracy had improved, particularly for rural residents. Thereby, caution should be taken in the interpretation of our results, with a consideration of the direction of this potential bias. A possible misclassification might have occurred between PLC and CLD in the context of insufficient knowledge and perception about the spectrum of disease and diagnosis of liver cancer among clinicians and limited capability to make accurate diagnosis in health facilities. This possible inaccuracy in diagnoses would have been more severe in rural areas and have both declined in rural and urban population over the study period; therefore, it might have led to an overestimation of the increasing trend in PLC mortality and the decreasing trend in CLD mortality and their period effects. Nonetheless, the changing pattern of PLC and CLD revealed in the current study is in line with global trends and consistent with previous reports from China.24 38 The mortality data we used in the current work are from China’s national mortality surveillance system for death registration and mortality surveillance, which is a well-developed national system with the highest level of credibility in the country, and yield accurate estimates of the proportion of deaths due to specific causes.39 Although we were not able to rule out or estimate the size of this possible misclassification, we think the bias would unlikely affect our conclusion.
In conclusion, the period changes in the mortality risk of VH, CLD and PLC point to the historical achievements and challenges China has faced and will continue to face. Successful vaccination campaigns against HAV and HBV that began in the early 1990s have led to a decade of decline in VH mortality; however, a more recent resurgence in VH mortality has been observed, which alerts the rising epidemics of other types of VH infections in China. While CLD mortality has been declining since the late 1980s, perhaps due to the improved accessibility of healthcare and medical advancement, the increased risk of PLC mortality remains. The substantial gender differences in both period and cohort effects on CLD and PLC mortality have revealed that behavioural risk factors have played a major role. Our findings speak to the urgency and policymakers’ imperative double duty to reduce liver disease burden in China—to prevent new VH infections, with a focus on HAV and HBV and on HCV and HEV, and to intervene lifestyle-related risk factors in the population, with a specific focus on alcoholic drinking.
Supplementary Material
Footnotes
Contributors: YS and JC designed the study. YS and JC collected the data and performed the statistical analyses. YS, JC and XL did the analysis of the literature. YS, CL and JC wrote the article, and all the authors revised it critically for important intellectual content. JC planned the analyses and takes responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation. All authors reviewed and approved the final manuscript.
Funding: The study was supported by the Humanities and Social Sciences Project of the China Ministry of Education (17YJCZH155), the National Natural Science Foundation of China (71573192,71303012), and the China Postdoctoral Science Foundation (2015M580862, 2016T90935).
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data of this study have been officially made available to the general public. Researcher can download from China Statistical Yearbooks Database (http://tongji.oversea.cnki.net/oversea/engnavi/navidefault.aspx).
References
- 1. Kim Y, Ejaz A, Tayal A, et al. Temporal trends in population-based death rates associated with chronic liver disease and liver cancer in the United States over the last 30 years. Cancer 2014;120:3058–65. 10.1002/cncr.28843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Williams R, Aspinall R, Bellis M, et al. Addressing liver disease in the UK: a blueprint for attaining excellence in health care and reducing premature mortality from lifestyle issues of excess consumption of alcohol, obesity, and viral hepatitis. Lancet 2014;384:1953–97. 10.1016/S0140-6736(14)61838-9 [DOI] [PubMed] [Google Scholar]
- 3. Corrao G, Ferrari P, Zambon A, et al. Trends of liver cirrhosis mortality in Europe, 1970-1989: age-period-cohort analysis and changing alcohol consumption. Int J Epidemiol 1997;26:100–9. 10.1093/ije/26.1.100 [DOI] [PubMed] [Google Scholar]
- 4. World Health Organization Global health estimates 2015: deaths by cause, age, sex, by country and by region, 2000-2015. Available: http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html
- 5. World Health Organization Global health sector strategy on viral hepatitis, 2016-2021. Available: http://apps.who.int/iris/bitstream/10665/246177/1/WHO-HIV-2016.06-eng.pdf?ua=1
- 6. World Health Organization Global strategy to reduce the harmful use of alcohol 2010. Available: http://apps.who.int/iris/bitstream/10665/44395/1/9789241599931_eng.pdf?ua=1&ua=1 [DOI] [PMC free article] [PubMed]
- 7. Wang F-S, Fan J-G, Zhang Z, et al. The global burden of liver disease: the major impact of China. Hepatology 2014;60:2099–108. 10.1002/hep.27406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cui F, Hadler SC, Zheng H, et al. Hepatitis A surveillance and vaccine use in China from 1990 through 2007. J Epidemiol 2009;19:189–95. 10.2188/jea.JE20080087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cui F, Shen L, Li L, et al. Prevention of chronic hepatitis B after 3 decades of escalating vaccination policy, China. Emerg Infect Dis 2017;23:765–72. 10.3201/eid2305.161477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhang J, Zhang X-F, Huang S-J, et al. Long-term efficacy of a hepatitis E vaccine. N Engl J Med 2015;372:914–22. 10.1056/NEJMoa1406011 [DOI] [PubMed] [Google Scholar]
- 11. Jiang H, Room R, Hao W. Alcohol and related health issues in China: action needed. Lancet Glob Health 2015;3:e190–1. 10.1016/S2214-109X(15)70017-3 [DOI] [PubMed] [Google Scholar]
- 12. World Health Organization Global Information System on alcohol and health - levels of consumption. Available: http://apps.who.int/gho/data/node.main.A1022?lang=en
- 13. Gao J, Xie L, Chen W-Q, et al. Rural-Urban, sex variations, and time trend of primary liver cancer incidence in China, 1988-2005. Eur J Cancer Prev 2013;22:448–54. 10.1097/CEJ.0b013e32835de82a [DOI] [PubMed] [Google Scholar]
- 14. Wang X, Lin S-X, Tao J, et al. Study of liver cirrhosis over ten consecutive years in southern China. World J Gastroenterol 2014;20:13546–55. 10.3748/wjg.v20.i37.13546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dal Maso L, Lise M, Zambon P, et al. Incidence of primary liver cancer in Italy between 1988 and 2002: an age-period-cohort analysis. Eur J Cancer 2008;44:285–92. 10.1016/j.ejca.2007.11.009 [DOI] [PubMed] [Google Scholar]
- 16. Park J, Jee YH. Age-period-cohort analysis of liver cancer mortality in Korea. Asian Pac J Cancer Prev 2015;16:8589–94. 10.7314/APJCP.2015.16.18.8589 [DOI] [PubMed] [Google Scholar]
- 17. Chang J, Liu X, Sun Y. Mortality due to acute myocardial infarction in China from 1987 to 2014: secular trends and age-period-cohort effects. Int J Cardiol 2017;227:229–38. 10.1016/j.ijcard.2016.11.130 [DOI] [PubMed] [Google Scholar]
- 18. National Bureau of Statistics of China Census data. Available: http://www.stats.gov.cn/english/statisticaldata/censusdata/
- 19. Kraus L, Tinghög ME, Lindell A, et al. Age, period and cohort effects on time trends in alcohol consumption in the Swedish adult population 1979-2011. Alcohol Alcohol 2015;50:319–27. 10.1093/alcalc/agv013 [DOI] [PubMed] [Google Scholar]
- 20. Hu A. Changing perceived importance of religion in mainland China, 1990-2012: an age-period- cohort analysis. Soc Sci Res 2017;66:264–78. 10.1016/j.ssresearch.2016.10.014 [DOI] [PubMed] [Google Scholar]
- 21. Glenn ND. Age, period, and cohort effects : Kempf-Leonard K, Encyclopedia of social measurement. Amsterdam: Elsevier, 2005: 27–32. [Google Scholar]
- 22. Yang Y, Schulhofer‐Wohl S, Fu WJ, et al. The intrinsic estimator for Age‐Period‐Cohort analysis: what it is and how to use it. Am J Sociol 2008;113:1697–736. 10.1086/587154 [DOI] [Google Scholar]
- 23. World Bank Life expectancy at birth. Available: https://data.worldbank.org/indicator/SP.DYN.LE00.IN?locations=CN
- 24. Mokdad AA, Lopez AD, Shahraz S, et al. Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med 2014;12:145 10.1186/s12916-014-0145-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cui F, Liang X, Wang F, et al. Development, production, and postmarketing surveillance of hepatitis A vaccines in China. J Epidemiol 2014;24:169–77. 10.2188/jea.JE20130022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ren X, Wu P, Wang L, et al. Changing epidemiology of hepatitis A and hepatitis E viruses in China, 1990-2014. Emerg Infect Dis 2017;23:276–9. 10.3201/eid2302.161095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Zhang M, Yuan Y, Mao P, et al. [Analysis on morbidity and mortality of viral hepatitis in China, 2004-2013]. Zhonghua Liu Xing Bing Xue Za Zhi 2015;36:144–7. [PubMed] [Google Scholar]
- 28. Yang Y, Land KC. Age-period-cohort analysis: new models, methods, and empirical applications. Florida: CRC, 2013. [Google Scholar]
- 29. Duan Z, Jia J-D, Hou J, et al. Current challenges and the management of chronic hepatitis C in mainland China. J Clin Gastroenterol 2014;48:679–86. 10.1097/MCG.0000000000000109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Liu ZQ, Zuo JL, Yan Q, et al. [Epidemiologic and spatio-temporal characteristics of hepatitis E in China, 2004-2014]. Zhonghua Liu Xing Bing Xue Za Zhi 2017;38:1380–5. 10.3760/cma.j.issn.0254-6450.2017.10.017 [DOI] [PubMed] [Google Scholar]
- 31. Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990-2013: a systematic subnational analysis for the global burden of disease study 2013. Lancet 2016;387:251–72. 10.1016/S0140-6736(15)00551-6 [DOI] [PubMed] [Google Scholar]
- 32. Meng Q, Fang H, Liu X, et al. Consolidating the social health insurance schemes in China: towards an equitable and efficient health system. Lancet 2015;386:1484–92. 10.1016/S0140-6736(15)00342-6 [DOI] [PubMed] [Google Scholar]
- 33. Sun Y, Wang Y, Li M, et al. Long-term trends of liver cancer mortality by gender in urban and rural areas in China: an age-period-cohort analysis. BMJ Open 2018;8:e020490 10.1136/bmjopen-2017-020490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wilsnack RW, Wilsnack SC, Kristjanson AF, et al. Gender and alcohol consumption: patterns from the multinational GENACIS project. Addiction 2009;104:1487–500. 10.1111/j.1360-0443.2009.02696.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Liu J, Fan D. Hepatitis B in China. Lancet 2007;369:1582–3. 10.1016/S0140-6736(07)60723-5 [DOI] [PubMed] [Google Scholar]
- 36. World Health Organization Global hepatitis report, 2017. Available: http://www.who.int/hepatitis/publications/global-hepatitis-report2017/en/
- 37. Kubo S, Takemura S, Sakata C, et al. Adjuvant therapy after curative resection for hepatocellular carcinoma associated with hepatitis virus. Liver Cancer 2013;2:40–6. 10.1159/000346214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Zheng R, Qu C, Zhang S, et al. Liver cancer incidence and mortality in China: temporal trends and projections to 2030. Chin J Cancer Res 2018;30:571–9. 10.21147/j.issn.1000-9604.2018.06.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Liu S, Wu X, Lopez AD, et al. An integrated national mortality surveillance system for death registration and mortality surveillance, China. Bull World Health Organ 2016;94:46–57. 10.2471/BLT.15.153148 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-029793supp001.pdf (170.5KB, pdf)