Abstract
Objectives
Neck circumference has emerged as a predictor of obesity and metabolic syndrome, but its clinical usefulness for different groups of population is not clearly defined. The aim is to evaluate the predictive capacity of neck circumference in order to detect cardiovascular risks (CVRs) on the Chilean population and to compare it with waist circumference performance.
Design
Cross-sectional study.
Setting
General Chilean population.
Participants
Data of 4607 adults aged 18 and over from the Chilean National Health Survey 2009–2010 were analysed.
Primary and secondary outcome measures
Anthropometrics measures included neck and waist circumference, height and weight. CVR was identified according to the Framingham tables adapted for the Chilean population. Receiver operating characteristics curves and logistic regression models were made to evaluate the performance of neck circumference to predict a moderate/high CVR, comparing it to waist circumference.
Results
Almost 10% of the sample had a moderate or high CVR. The probability of having a moderate/high cardiovascular risk increase with cervical obesity (OR 1.95, 95% CI 1.04 to 3.68) and central obesity (OR 4.5, 95% CI 2.47 to 8.22). The area under the curves were high for cervical obesity (AUC 81.4%, 95% CI 78.8% to 84.0%) and central obesity (AUC 82.2%, 95% CI 79.7% to 84.7%) and not statistically different (p=0.152).
Conclusions
Neck obesity has a high capacity to predict moderate/high CVR in the Chilean population. Its good performance appears as an opportunity to use it in clinical practice when waist circumference measurement is difficult to measure and eventually replace the waist circumference measurement as the technique is easier.
Keywords: neck circumference, cardiovascular risk, overweight, waist circumference
Strengths and limitations of this study.
To our knowledge, this is the first study that directly evaluates the performance of neck circumference to predict a moderate/high cardiovascular risk in the general population.
The study adds local cut-off points for neck circumference.
The study does not include an imaging examination to ensure the correlation between neck circumference and the upper subcutaneous fat.
This is a cross-sectional study, so it is not possible to ensure a temporal association.
Introduction
A systematic increase regarding cardiovascular risk (CVR) factors has been observed during the last decade in Chile as cardiovascular diseases are the main cause of death among the Chilean population. According to preliminary results from the Chilean National Health Survey (NHS) 2016–2017, 71% of the population suffers malnutrition due to overweight, 27.9% have suspected arterial hypertension (self-reported, antihypertensive treatment or an average of three blood pressures >140/90) and 12.3% have suspected type 2 diabetes mellitus (fasting glycaemic ≥126 mg/dL), showing gender differences.1
The mathematical models that estimate CVR quantitatively in literature are numerous, and the Framingham equations are the most known.2 In 2009, Framingham’s CVR tables were developed for the Chilean population, which estimated the possibility of suffering a coronary event or stroke in a 10-year period for people between 35 and 74 years without a history of a previous cardiovascular event.3 The tables classify the levels of risk in three categories: high (≥10% chance), medium (5%–9% chance) and low (<5% chance). According to the NHS 2016–2017, 25.5% of the population has a high-risk chance, showing a 7.8% increase compared with the NHS 2009–2010. Nevertheless, as the methodologies in both surveys and the age spectrum were different, the data gathered cannot be compared.
Central obesity has been described as a better metabolic and CVR predictor than the determination of obesity through a body mass index (BMI) analysis,4–7 as abdominal obesity possesses a better correlation with the visceral fat mass.8–10 Because of this, it has been used for many years as an easy tool to evaluate CVR in clinical practice.11 Nonetheless, its measurement can be affected by bloating provoked by certain food, the subject’s air inhalation, the tape measure and the implemented technique,12 considering the five conceived techniques for its measurement.13
Neck circumference is regarded as a promising tool to detect CVRs as it possesses a better correlation with the body’s upper trunk fat.14 15 The neck circumference is an easily accessible, non-invasive and economic measure that does not change during the course of the day.16 17 Even though there is still some missing evidence to establish the relationship between cervical obesity and CVR, it has been observed that the body’s upper trunk fat accumulation is related to metabolic syndrome in children and adults.17–20 It is also associated with the obstructive sleep apnoea syndrome (OSAS),21 22 which increases CVR due to the deterioration of the endothelial function caused by repeated hypoxia.23
Evidence suggests that the measurement of neck circumference could contribute to clinical practice as a complementary procedure apart from the procedure currently used to determine CVRs.24 25 That is why this research is looking forward to the predictive capacity of neck circumference for the Chilean population in order to detect CVRs and compare it with waist circumference.
Material/subjects and methods
Design and sample
A cross-sectional study was carried out with the data gathered from the Chilean NHS 2009–2010.26 Initially, all adults aged 18 and over were included, excluding the ones that did not have their neck circumference measured and the ones who presented a measurement lower than 25 cm or higher than 60 cm, as these values were considered extreme and unlikely for neck circumference.
Patient and public involvement
There were no patients or public involved in this study.
Variables and measurements
Neck circumference was measured under the laryngeal prominence on men and from the middle point between the base of the neck and the upper part of the sternum on women, while waist circumference was measured from the middle point between the rib flange and the iliac crest following the midaxillary line. Central obesity was defined as having a waist circumference >80 cm for women and >90 cm for men, according to the technical norms provided by the Chilean Health Ministry (MINSAL).27 Both measures were made by trained nurses.
CVR was identified according to the Framingham tables adapted for the Chilean population,28 based on gender, age, diabetes mellitus diagnosis, smoking condition, blood pressure, total cholesterol and high-density lipoprotein (HDL) cholesterol. For the statistical analysis, this variable was dichotomised on low CVR and medium/high CVR.
As for the categorisation of the sample for the predictive analysis, variables regarding sex, educational level categorised according to the school years (low: <8, medium: 8–12, high: >12) and obesity (BMI ≥30 kg/m2) were considered.
Statistical analysis
Receiver operating characteristics curves were obtained for neck and waist circumferences as predictors of moderate/high CVR. Cut-off points for cervical obesity in both genders were selected based on the best performance of neck circumference to predict moderate/high CVR. Sensibilities and the specificities of cervical and central obesity as predictors of moderate/high CVR were compared.
Additionally, the probability of moderate/high CVR due to cervical or central obesity conditions was analysed by using two models of logistic regression. The first one considered cervical obesity as an explicative variable (model 1), whereas central obesity was considered for the second one (model 2). Both models considered gender, educational level and obesity as covariables. The area under the curve (AUC) was compared using the X2 test for AUC equality. For all the analyses, a 0.05 significance level and the corresponding expansion factors were considered. Data were analysed using STATA V.12.0 software.
Ethical issues
The present study is based on the analysis of the data resulting from the NHS 2009–2010, without direct intervention in human beings. The survey included the application of informed consent and information about the results of laboratory tests to individuals. The NHS database is anonymised and openly available in the Chilean Ministry of Health web page.29
Results
The NHS sample was formed by 5069 adults, but 423 were excluded because they did not have their neck circumference measured and 39 due to extreme values. Hence, the analysed sample consisted of 4607 individuals, with a mean age of 47.6 years and predominately women (60.3%). Almost 10% had moderate or high CVR (table 1).
Table 1.
Sample characteristics
| Both genders (n=4607) |
Men (n=1830) |
Women (n=2777) |
P value* | |
| Age mean (SD) | 47.6 (17.8) | 47.5 (17.5) | 47.7 (18.0) | 0.877 |
| Educational level n (%) | ||||
| Low | 1261 (27.5) | 462 (25.3) | 799 (28.9) | 0.029 |
| Middle | 2434 (53.0) | 995 (54.5) | 1439 (52.0) | |
| High | 896 (19.5) | 368 (20.2) | 528 (19.1) | |
| Cardiovascular risk n (%) | ||||
| Low | 2246 (90.1) | 817 (79.9) | 1429 (97.2) | <0.001 |
| Moderate | 217 (8.70) | 176 (17.2) | 41 (2.80) | |
| High | 30 (1.20) | 30 (2.90) | 0 (0.00) | |
| Diabetes mellitus n (%) | 278 (6.30) | 125 (7.20) | 153 (5.80) | 0.040 |
| Arterial hypertension n (%) | 1220 (26.7) | 538 (32.3) | 637 (23.1) | <0.001 |
| Smoking n (%) | 1619 (35.3) | 708 (38.8) | 911 (32.9) | <0.001 |
| Obesity n (%) | 1367 (30.0) | 441 (24.4) | 926 (33.8) | <0.001 |
| Cervical obesity† n (%) | 1757 (38.1) | 652 (35.6) | 1105 (39.8) | 0.002 |
| Central obesity n (%) | 3394 (74.1) | 1223 (67.2) | 2171 (78.7) | <0.001 |
*Wilcoxon-Mann-Whitney test or Fisher's exact test.
†Cut-off values based on ROC curves.
ROC, receiver operating characteristics.
For men, waist circumference had a better capacity to predict moderate/high CVR than neck circumference (AUC 0.67, 95% CI 0.39 to 0.71 vs AUC 0.58, 95% CI 0.53 to 0.62, p<0.001). However, for women, the difference was not significant (AUC 0.70, 95% CI 0.64 to 0.77 vs AUC 0.66, 95% CI 0.58 to 0.74, p<0.197), indicating a similar performance to predict moderate/high CVR between both measures (figure 1). Based on these analyses, the best performance of neck circumference to predict moderate/high CVR was obtained with cut-off points of 37 cm for men and 32 cm for women. Compared with waist circumference, neck circumference showed a higher sensitivity in men (86.4% vs 82.8%) and a similar sensitivity in women (97.6%), but lower specificities in both genders (table 2).
Figure 1.
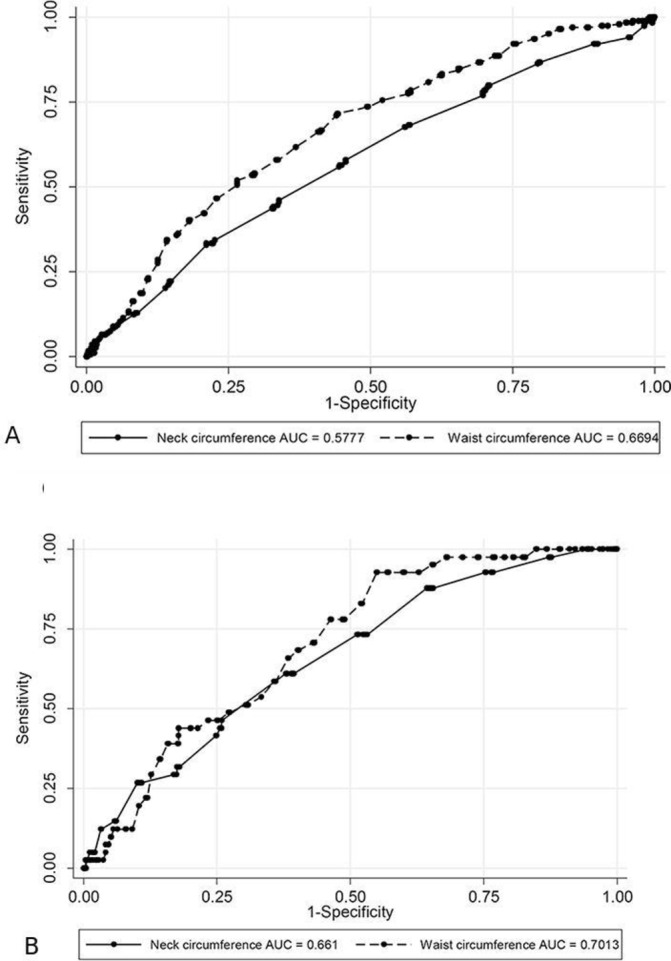
ROC curves for the prediction of moderate/high cardiovascular risk by neck and waist circumferences in (A) men and (B) women. AUC, area under the curves; ROC, receiver operating characteristics.
Table 2.
Sensitivity and specificity of cervical and central obesity to predict moderate/high cardiovascular risk, by gender
| Men | Women | |||||
| Cut-off (cm) |
Sensitivity % |
Specificity % |
Cut-off (cm) |
Sensitivity % |
Specificity % |
|
| Cervical obesity | 37 | 86.4 | 20.6 | 32 | 97.6 | 12.9 |
| Central obesity | 90 | 82.8 | 37.7 | 80 | 97.6 | 23.2 |
Cervical or central obesity increases the probability of having moderate/high CVR compared with the population without these conditions. However, the CIs overlap (OR 1.95, 95% CI 1.04 to 3.68 for cervical obesity and OR 4.5, 95% CI 2.47 to 8.22 for central obesity) and both models had an AUC of over 80%, with a non-significant statistical difference between them (equity AUC test: p=0.152) (table 3).
Table 3.
Adjusted performance of cervical and central obesity to predict moderate/high cardiovascular risk
| Model 1 | Model 2 | |||
| OR | P value | OR | P value | |
| Sex | ||||
| Men | 1 | – | 1 | – |
| Women | 0.09 (0.05 to 0.17) | <0.001 | 0.08 (0.04 to 0.16) | <0.001 |
| Educational level | ||||
| Low | 1 | – | 1 | – |
| Middle | 0.22 (0.13 to 0.38) | <0.001 | 0.22 (0.13 to 0.39) | <0.001 |
| High | 0.12 (0.06 to 0.27) | <0.001 | 0.13 (0.06 to 0.27) | <0.001 |
| Obesity | 1.86 (1.09 to 3.17) | 0.022 | 1.31 (0.76 to 2.25) | 0.332 |
| Cervical obesity | 1.95 (1.04 to 3.68) | <0.001 | – | – |
| Central obesity | – | – | 4.50 (2.47 to 8.22) | <0.001 |
AUC model 1=81.38% (78.8–84.0).
AUC model 2=82.20% (79.7–84.7).
Equality AUC test: p=0.152.
AUC, area under the curve.
Discussion
This study demonstrates that the cut-off points proposed for cervical obesity (neck circumference ≥32 cm for women and ≥37 cm for men) have a high capacity to predict moderate/high CVRs in the Chilean population. This result, adjusted by sex, educational level and obesity, is similar to that shown by abdominal obesity measured using the waist circumference.
The results are the same way as previous studies that have found a positive association between neck circumference and cardiometabolic risk factors.30 Neck circumference has been positively correlated with glucose and insulin resistance, systolic and diastolic blood pressure, free-fatty acids, the production of very low-density lipoprotein cholesterol and triglycerides, while there is an inverse association with HDL cholesterol.24 30–33 It is possible to hypothesise that upper subcutaneous fat has similar pathophysiological characteristics as abdominal visceral fat. In fact, neck circumference is also related to oxidative stress, endothelial cell dysfunction and vascular injury24 31 32 and it is correlated with visceral adipose tissue, as measured by CT.30 34 35 Therefore, neck circumference seems to be an important anthropometric marker to identify patients with a high cardiometabolic risk.36
The performance of a neck circumference to predict moderate/high CVRs could be explained as the neck circumference is a good predictor of obesity, at least in adolescents.37 38 However, our results were controlled by obesity and the association between cardiometabolic risk factors and neck circumference seems to be independent of the association between cardiometabolic risk factors and BMI and visceral fat, but synergistic with the latter.30
The neck circumference cut-off points selected in our study for the Chilean population differ considerably from the ones used for other populations to predict related outcomes. For example, to predict metabolic syndrome in the Brazilian population the values used were 39.6 cm for men and 36.1 cm for women39 and for the Chinese population of 65 years old and over were 38 cm for men and 35 cm for women.40 There is evidence about a lack of consistency between neck circumference cut-off points in pooled analyses,38 so it is recommendable to use local values. In this study, the cut-off points were based on the best sensitivity and specificity of neck circumference to predict moderate/high CVR in both genders.
To our knowledge, this is the first study that directly evaluates the performance of neck circumference to predict moderate/high CVRs in the general population. However, some studies have evaluated the capacity of neck circumference to predict other related metabolic outcomes like obesity or metabolic syndrome with an acceptable result.39 40
The Chilean NHS had some outliers in the neck circumference measurements that could have a relationship with the not common use of this anthropometric measure in clinical practice. These extreme data were not considered in the analysis and it is unlikely that they would have changed the results. Another limitation is that we do not have an imaging examination that confirms that neck circumference adequately represents the upper subcutaneous fat in the sample. As almost all anthropometric measures, neck circumference has some limitations that need to be taken into consideration, such as, it should not be used in some medical situations such as goitre, cervical spine abnormalities or Cushing syndrome. However, it is easy to measure in clinical practice and it does not require undressing or measuring height.
Another limitation of the study is that the CVR was not assessed directly by cardiovascular morbidity or mortality, but through Framingham tables adapted for the Chilean population. However, tables and scores based on risk factors are widely recommended in clinical practice to measure cardiovascular risk.41
The present study shows that the local cut-offs of neck circumference have a high capacity to predict moderate/high CVRs in the Chilean population. Nevertheless, this measure does not have a better performance than waist circumference to estimate CVRs in the Chilean population. However, its good performance appears to be an opportunity to use it in clinical practice when a waist circumference measurement is difficult or eventually replace waist circumference measurement because of the neck circumference’s easy technique.
Future research is needed among specific populations for whom it is difficult to estimate the CVRs, such as extreme elderly people, multimorbidity patients or ethnic groups. It would be also recommendable to evaluate if a reduction of neck circumference postbariatric surgery or weight loss is a good marker of a cardiometabolic improvement and it would also be recommendable to incorporate an imaging analysis of upper subcutaneous fat in these studies.
Supplementary Material
Footnotes
Contributors: PC, XG and GW made substantial contributions to the research design. PC and AC led the statistical analyses. PC and CS contributed to manuscript drafting and editing. All authors critically reviewed and approved the final version of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The 2009–2010 NHS protocol was approved by the Research Ethics Committee of the Pontificia Universidad Católica de Chile (1 September 2009).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available in a public, open access repository.
References
- 1. Chilean Health Ministry National health survey 2016-2017. First results. Santiago: MINSAL, 2017. Available: http://www.minsal.cl/wp-content/uploads/2017/11/ENS-2016-17_PRIMEROS-RESULTADOS.pdf [Accessed 18 Jul 2018].
- 2. Beswick A, Brindle P, Fahey T, Ebrahim S. A systematic review of risk scoring methods and clinical decision AIDS used in the primary prevention of coronary heart disease (supplement). Report No.: NICE clinical guidelines, no. 67S. London: Royal College of General Practitioners (UK); 2008. https://www.ncbi.nlm.nih.gov/books/NBK55821/ [PubMed] [Google Scholar]
- 3. Icaza G, Núñez L, Marrugat J, et al. [Estimation of coronary heart disease risk in Chilean subjects based on adapted Framingham equations]. Rev Med Chil 2009;137:1273–82. doi:/S0034-98872009001000001 [PubMed] [Google Scholar]
- 4. Banerji MA, Lebowitz J, Chaiken RL, et al. Relationship of visceral adipose tissue and glucose disposal is independent of sex in black NIDDM subjects. Am J Physiol 1997;273:E425–32. 10.1152/ajpendo.1997.273.2.E425 [DOI] [PubMed] [Google Scholar]
- 5. Lebovitz HE, Banerji MA. Point: visceral adiposity is causally related to insulin resistance. Diabetes Care 2005;28:2322–5. 10.2337/diacare.28.9.2322 [DOI] [PubMed] [Google Scholar]
- 6. Carey DG, Jenkins AB, Campbell LV, et al. Abdominal fat and insulin resistance in normal and overweight women: direct measurements reveal a strong relationship in subjects at both low and high risk of NIDDM. Diabetes 1996;45:633–8. 10.2337/diab.45.5.633 [DOI] [PubMed] [Google Scholar]
- 7. Lemieux I, Pascot A, Couillard C, et al. Hypertriglyceridemic waist: a marker of the atherogenic metabolic triad (hyperinsulinemia; hyperapolipoprotein B; small, dense LDL) in men? Circulation 2000;102:179–84. 10.1161/01.cir.102.2.179 [DOI] [PubMed] [Google Scholar]
- 8. Burrows A R, Leiva B L, Weistaub G, et al. [Prevalence of metabolic syndrome in a sample of Chilean children consulting in an obesity clinic]. Rev Med Chil 2007;135:174–81. doi:/S0034-98872007000200005 [DOI] [PubMed] [Google Scholar]
- 9. Ying X, Jiang Y, Qin G, et al. Association of body mass index, waist circumference, and metabolic syndrome with serum cystatin C in a Chinese population. Medicine 2017;96:e6289 10.1097/MD.0000000000006289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Guan X, Sun G, Zheng L, et al. Associations between metabolic risk factors and body mass index, waist circumference, waist-to-height ratio and waist-to-hip ratio in a Chinese rural population. J Diabetes Investig 2016;7:601–6. 10.1111/jdi.12442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lean ME, Han TS, Morrison CE. Waist circumference as a measure for indicating need for weight management. BMJ 1995;311:158–61. 10.1136/bmj.311.6998.158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. World Health Organization Waist circumference and waist–hip ratio: report of a WHO expert consultation, Geneva, 8–11 December 2008. Geneva: WHO, 2011. Available: http://www.who.int/nutrition/publications/obesity/WHO_report_waistcircumference_and_waisthip_ratio/en/ [Accessed 18 Jul 2018].
- 13. World Health Organization Physical status: the use and interpretation of anthropometry. Report of a WHO expert Committee. World Health organization technical report series No. 854. Geneva, 1995. Available: http://www.who.int/childgrowth/publications/physical_status/en/ [Accessed 30 Jul 2018]. [PubMed]
- 14. Svensson M, Lindberg E, Naessen T, et al. Risk factors associated with snoring in women with special emphasis on body mass index: a population-based study. Chest 2006;129:933–41. 10.1378/chest.129.4.933 [DOI] [PubMed] [Google Scholar]
- 15. Seidell JC. Waist circumference and waist/hip ratio in relation to all-cause mortality, cancer and sleep apnea. Eur J Clin Nutr 2010;64:35–41. 10.1038/ejcn.2009.71 [DOI] [PubMed] [Google Scholar]
- 16. Kurtoglu S, Hatipoglu N, Mazicioglu MM, et al. Neck circumference as a novel parameter to determine metabolic risk factors in obese children. Eur J Clin Invest 2012;42:623–30. 10.1111/j.1365-2362.2011.02627.x [DOI] [PubMed] [Google Scholar]
- 17. Joshipura K, Muñoz-Torres F, Vergara J, et al. Neck circumference may be a better alternative to standard anthropometric measures. J Diabetes Res 2016;2016:1–8. 10.1155/2016/6058916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Torriani M, Gill CM, Daley S, et al. Compartmental neck fat accumulation and its relation to cardiovascular risk and metabolic syndrome. Am J Clin Nutr 2014;100:1244–51. 10.3945/ajcn.114.088450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Verhulst SL, Schrauwen N, Haentjens D, et al. Sleep-Disordered breathing and the metabolic syndrome in overweight and obese children and adolescents. J Pediatr 2007;150:608–12. 10.1016/j.jpeds.2007.01.051 [DOI] [PubMed] [Google Scholar]
- 20. Namazi N, Larijani B, Surkan PJ, et al. The association of neck circumference with risk of metabolic syndrome and its components in adults: a systematic review and meta-analysis. Nutr Metab Cardiovasc Dis 2018;28:657–74. 10.1016/j.numecd.2018.03.006 [DOI] [PubMed] [Google Scholar]
- 21. Yuan H, Schwab RJ, Kim C, et al. Relationship between body fat distribution and upper airway dynamic function during sleep in adolescents. Sleep 2013;36:1199–207. 10.5665/sleep.2886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pahkala R, Seppä J, Ikonen A, et al. The impact of pharyngeal fat tissue on the pathogenesis of obstructive sleep apnea. Sleep Breath 2014;18:275–82. 10.1007/s11325-013-0878-4 [DOI] [PubMed] [Google Scholar]
- 23. Gonzaga C, Bertolami A, Bertolami M, et al. Obstructive sleep apnea, hypertension and cardiovascular diseases. J Hum Hypertens 2015;29:705–12. 10.1038/jhh.2015.15 [DOI] [PubMed] [Google Scholar]
- 24. Sjöström CD, Håkangård AC, Lissner L, et al. Body compartment and subcutaneous adipose tissue distribution--risk factor patterns in obese subjects. Obes Res 1995;3:9–22. 10.1002/j.1550-8528.1995.tb00116.x [DOI] [PubMed] [Google Scholar]
- 25. Fitch KV, Stanley TL, Looby SE, et al. Relationship between neck circumference and cardiometabolic parameters in HIV-infected and non-HIV-infected adults. Diabetes Care 2011;34:1026–31. 10.2337/dc10-1983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chilean Ministry of Health National health survey. Chile 2009-2010, 2010. Available: http://www.minsal.cl/estudios_encuestas_salud/ [Accessed 15 Jul 2018].
- 27. Ben-Noun LL, Laor A. Relationship between changes in neck circumference and cardiovascular risk factors. Exp Clin Cardiol 2006;11:14–20. [PMC free article] [PubMed] [Google Scholar]
- 28. Kunstmann S, Lira MT, Icaza G, et al. Cardiovascular risk stratification in Chilean population. Rev Médica Clínica Las Condes 2012;23:657–65. [Google Scholar]
- 29. Chilean Health Ministry [Pupulation surveys databases], 2019. Available: http://epi.minsal.cl/bases-de-datos/ [Accessed 1Dec 2018].
- 30. Preis SR, Massaro JM, Hoffmann U, et al. Neck circumference as a novel measure of cardiometabolic risk: the Framingham heart study. J Clin Endocrinol Metab 2010;95:3701–10. 10.1210/jc.2009-1779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cizza G, de Jonge L, Piaggi P, et al. Neck circumference is a predictor of metabolic syndrome and obstructive sleep apnea in short-sleeping obese men and women. Metab Syndr Relat Disord 2014;12:231–41. 10.1089/met.2013.0093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Horská K, Kučerová J, Suchý P, et al. Metabolic syndrome - dysregulation of adipose tissue endocrine function. Ceska Slov Farm 2014;63:152–9. [PubMed] [Google Scholar]
- 33. Vallianou NG, Evangelopoulos AA, Bountziouka V, et al. Neck circumference is correlated with triglycerides and inversely related with HDL cholesterol beyond BMI and waist circumference. Diabetes Metab Res Rev 2013;29:90–7. 10.1002/dmrr.2369 [DOI] [PubMed] [Google Scholar]
- 34. Li H-X, Zhang F, Zhao D, et al. Neck circumference as a measure of neck fat and abdominal visceral fat in Chinese adults. BMC Public Health 2014;14:311 10.1186/1471-2458-14-311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rosenquist KJ, Therkelsen KE, Massaro JM, et al. Development and reproducibility of a computed tomography-based measurement for upper body subcutaneous neck fat. J Am Heart Assoc 2014;3:e000979 10.1161/JAHA.114.000979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Borel A-L, Coumes S, Reche F, et al. Waist, neck circumferences, waist-to-hip ratio: which is the best cardiometabolic risk marker in women with severe obesity? The soon cohort. PLoS One 2018;13:e0206617 10.1371/journal.pone.0206617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Patnaik L, Pattnaik S, Rao EV, et al. Validating neck circumference and waist circumference as anthropometric measures of Overweight/Obesity in adolescents. Indian Pediatr 2017;54:377–80. 10.1007/s13312-017-1110-6 [DOI] [PubMed] [Google Scholar]
- 38. Ma C, Wang R, Liu Y, et al. Diagnostic performance of neck circumference to identify overweight and obesity as defined by body mass index in children and adolescents: systematic review and meta-analysis. Ann Hum Biol 2017;44:223–9. 10.1080/03014460.2016.1224387 [DOI] [PubMed] [Google Scholar]
- 39. Stabe C, Vasques ACJ, Lima MMO, et al. Neck circumference as a simple tool for identifying the metabolic syndrome and insulin resistance: results from the Brazilian metabolic syndrome study. Clin Endocrinol 2013;78:874–81. 10.1111/j.1365-2265.2012.04487.x [DOI] [PubMed] [Google Scholar]
- 40. Yan Q, Sun D, Li X, et al. Neck circumference is a valuable tool for identifying metabolic syndrome and obesity in Chinese elder subjects: a community-based study. Diabetes Metab Res Rev 2014;30:69–76. 10.1002/dmrr.2464 [DOI] [PubMed] [Google Scholar]
- 41. Piepoli MF, Hoes AW, Agewall S, et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice: the sixth joint Task force of the European Society of cardiology and other societies on cardiovascular disease prevention in clinical practice. Eur Heart J 2016;37:2315–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


