Abstract
Introduction
Effective approaches to increase engagement in treatment for opioid use disorder (OUD) and reduce the risk of recurrent overdose and death following emergency department (ED) presentation for opioid overdose remain unknown. As such, we aim to compare the effectiveness of behavioural interventions delivered in the ED by certified peer recovery support specialists relative to those delivered by licensed clinical social workers (LCSWs) in promoting OUD treatment uptake and reducing recurrent ED visits for opioid overdose.
Methods and analysis
Adult ED patients who are at high risk for opioid overdose (ie, are being treated for an opioid overdose or identified by the treating physician as having OUD) (n=650) will be recruited from two EDs in a single healthcare system in Providence, Rhode Island into a two-arm randomised trial with 18 months of follow-up postrandomisation. Eligible participants will be randomly assigned (1:1) in the ED to receive a behavioural intervention from a certified peer recovery support specialist or a behavioural intervention from an LCSW. The primary outcomes are engagement in formal OUD treatment within 30 days of the initial ED visit and recurrent ED visits for opioid overdose within 18 months of the initial ED visit, as measured through statewide administrative records.
Ethics and dissemination
This protocol was approved by the Rhode Island Hospital institutional review board (Approval Number: 212418). Data will be presented at national and international conferences and published in peer-reviewed journals.
Trial registration number
Keywords: Opioid Overdose, Emergency Department, Peer Support, Recovery, RandomisedTrial
Strengths and limitations of this study.
This study represents the first randomised controlled trial to assess the impact of a peer recovery support intervention on uptake of opioid use disorder (OUD) treatment and recurrent emergency department (ED) presentation for opioid-involved overdose.
This study leverages a statewide comprehensive data sharing infrastructure to use administrative records to characterise the primary outcomes (eg, OUD treatment enrolment, recurrent ED presentation), thus overcoming biases associated with self-reported outcomes and loss to follow-up in previous studies.
Although the administrative databases used to characterise the primary outcomes are meant to be representative, they are by no means comprehensive (ie, individuals who enroll in OUD treatment programmes or who present to EDs in other states will not be captured in these resources).
Introduction
Background and rationale
Deaths attributable to accidental drug overdose, particularly those involving opioids, have reached epidemic levels in the United States (US).1–4 In the last two decades, US overdose mortality rates have more than tripled, from 6.2 per 100 000 persons in 2000 to 21.7 per 100 000 persons in 2017.2 3 There have been 700 000 opioid overdose deaths between 2000 to 2015 in the US,5 and the crisis is expected to worsen under current trends.6 Since 2013, the opioid overdose epidemic has been marked by significant increases in deaths involving powerful synthetic opioids (eg, fentanyl).3 The burden of the drug overdose epidemic is greatly elevated in New England, where fentanyl has been present in the illicit drug supply since as early as 2012.7–10 Rhode Island has one of the highest drug overdose rates in the nation,3 and in 2014 reported the third and fourth highest rate of opioid-related emergency department (ED) visits and inpatient hospital stays, respectively.11
In addition to increases in fatal opioid overdoses, EDs have witnessed substantial increases in visits for non-fatal opioid overdoses.12–14 About 120 000 ED visits were reported for suspected non-fatal opioid overdoses between July 2016 and September 2017 in 16 states participating in the Enhanced State Opioid Overdose Surveillance, representing a 35% increase over this period.15 As such, the ED serves as a critical intervention site for providing services to people at high risk of opioid overdose and those with opioid use disorder (OUD). In the year after presenting to the ED for a drug overdose, a person is at heightened risk for death.16 17 In a nested case–control study in New York, the odds of death due to prescription drug overdose were 4.9 times higher for those with two ED visits, 16.6 times higher for those with three ED visits, and 48.2 times higher for those with four or more visits relative to one ED visit or less in the year preceding death.16 Thus, the ED is both a critical and timely place for intervention and the reason for the ED visit itself (ie, overdose) can be used as an opportunity to identify patients at highest risk of fatal drug overdose and deliver interventions.18
The most effective means to promote engagement in substance use disorder (SUD) treatment and reduce the risk of recurrent overdose and death following presentation to an ED for opioid overdose remains unknown. One of the only randomised studies of overdose education combined with a brief motivational interviewing-based intervention delivered in the ED by licensed mental health counsellors resulted in reductions in overdose risk behaviours among individuals presenting to the ED and reporting non-medical prescription opioid use.19 However, a trial deploying a similar intervention did not reduce overdose rates or prevent subsequent ED visits or hospitalisations compared with usual care.20 It is possible, however, that these types of interventions may be more effective if delivered by people with lived experiences with SUD and recovery. Peer-based interventions are an effective component of care across non-clinical settings and in other aspects of healthcare for other conditions.21 A recent systematic review by Ramchand and colleagues21 found that group-based interventions that use peers as educators commonly improve knowledge, attitudes, beliefs and perceptions and improve connectedness and engagement with health promotion activities.21 Further, a recent systematic review of peer recovery support services in care for SUD found that existing randomised controlled trials have been subject to several limitations, particularly poorly defined and non-manualised roles for peers, and, as such, there remains a need for more rigorous evaluation to determine the efficacy, effectiveness, and cost-effectiveness of peer recovery support services.22 However, little is known about their effectiveness in improving outcomes for persons at high risk for opioid overdose. In response to Rhode Island’s overdose crisis, individuals in long-term recovery with specialised training in SUD management, known as certified peer recovery support specialists, have been deployed in EDs since 2014.23 The goal of their work is to help patients navigate obstacles to recovery through problem-solving, goal setting, avoiding relapse triggers, and planning and obtaining services. Despite the promise of and significant national interest in this approach,24 no studies have rigorously evaluated whether peer-based behavioural interventions delivered in the ED result in improved outcomes for patients at high risk of opioid overdose.
Objectives
We aim to test the effectiveness of behavioural interventions delivered in the ED by certified peer recovery support specialists in improving outcomes for patients at high risk of opioid overdose relative to those delivered by licensed clinical social workers (LCSWs). We hypothesise that, because certified peer recovery support specialists are able to draw from their own lived experiences with SUD and recovery, patients who are randomly assigned to receive a behavioural intervention from a peer recovery support specialist, as compared with receiving an intervention from an LCSW, will be: (1) more likely to engage in formal SUD treatment within 30 days following the initial visit and (2) less likely to experience a recurrent ED visit for an opioid overdose during the succeeding 18 months.
Trial design
The trial utilises a parallel design where patients at high risk for opioid overdose who present to the ED are randomly assigned 1:1 to receive a behavioural intervention from a certified peer recovery support specialist or an LCSW.
Methods: participants, interventions, outcomes
Study setting
Rhode Island is home to over one million residents. Since 2000, the state has experienced a high burden of opioid overdose. According to the 2016–2017 cycle of the National Survey on Drug Use and Health, 4.7% of Rhode Islanders used heroin or misused a prescription opioid in the last year.25 Between 2013 and 2017, the age-adjusted rate of death due to opioid overdose increased by 44.2%, from 18.1 to 26.1 per 100 000 persons, with these increases largely driven by synthetic opioids other than methadone (16.8% of opioid overdose deaths in 2013 vs 72.6% in 2017).26
Eligibility criteria
To be eligible, participants must also be in the ED because they are: (1) being treated for an opioid overdose; (2) receiving treatment related to OUD (eg, infectious complication of injection drug use, opioid withdrawal); or (3) self-report an opioid overdose within the previous 12 months. The presence of an opioid overdose will be determined by the treating physician and is generally defined as (1) the presence of decreased levels of consciousness or respiratory depression and occurring after the consumption of opioids or resolving after the administration of naloxone. Potential participants will be deemed ineligible if they are critically ill or injured, have previously enrolled in the trial, are in police custody or incarcerated, pregnant, or live outside of Rhode Island. Patients who are critically ill or injured will be eligible for screening and enrolment once cleared to participate by their treating physician.
Patient and public involvement
No patient involved.
Interventions
Current standard of care
The current standard of care following an ED visit for an opioid overdose at the study sites is to receive a behavioural intervention delivered by a certified peer recovery support specialist or an LCSW. Whether a patient meets with a social worker or a peer recovery support specialist can depend on the time of day, staff availability and preferences or views of the provider or patient. In the trial, patients will be randomly assigned to receive a behavioural intervention in the ED delivered by (1) a staff LCSW or (2) a certified peer recovery support specialist trained by the Anchor Recovery Community Center (figure 1).
Figure 1.
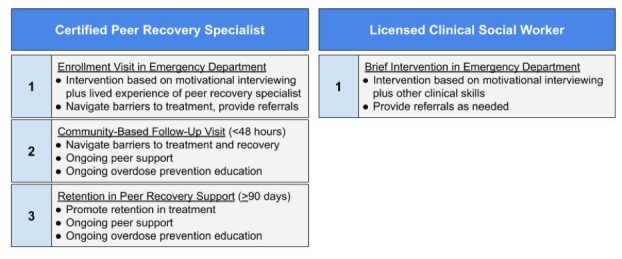
Intervention arms in a randomised clinical trial of an emergency department-based peer recovery support intervention to increase treatment uptake and reduce recurrent overdose among individuals at high risk for opioid overdose.
Behavioural intervention delivered by certified peer recovery support specialists
The Anchor Recovery Community Center is Rhode Island’s first community-based peer recovery centre.23 It is designed as an access point for those with SUD, providing services such as job counselling, health and wellness activities, and individualised long-term peer recovery coaching.23 Through one of its outreach programmes, known as AnchorED, the Anchor Recovery Community Center has deployed certified peer recovery support specialists to EDs across Rhode Island since 2014.23 As part of AnchorED, certified peer recovery support specialists arrive in the ED within 30 min of consultation, assess individuals for readiness to seek treatment, provide linkage to treatment and educate patients on overdose prevention and response.23 Peer recovery specialists call every day for 10 days in an attempt to make contact following discharge from the ED. Once contact is made, peer recovery specialists and their clients make plans for regular contact and follow-up. There are 30 peer recovery support specialists available to deliver these interventions between the two study sites.
To become a certified peer recovery support specialist, applicants must be in recovery for at least 2 years, undergo a 45-hour training programme at Anchor Recovery Community Center based on the Connecticut Community for Addiction Recovery curriculum, and accrue 500 hours of supervised work experience providing peer recovery support services.23 All peer recovery support specialists obtain certification from the International Certification and Reciprocity Consortium.23 The certification programme focuses on advocacy, wellness and recovery, motivational interviewing techniques, mentoring and education, and ethics as well as additional training on the provision of trauma-informed care and the transtheoretical model of behaviour change. In addition to employing motivational interviewing techniques, peer recovery support specialists support individuals’ self-efficacy and prevent relapse by addressing social, environmental and personal factors, such as awareness and avoidance of relapse triggers, polysubstance use, stigma associated with SUD and their treatment, knowledge of treatment services (including the use of medications for OUD treatment), and addressing financial and transportation barriers to treatment.23 Certified peer recovery support specialists are uniquely positioned to deliver behavioural interventions to individuals who have experienced overdose as they couple their training with lived experiences of SUD and recovery.23
Behavioural intervention delivered via licensed clinical social workers
There are 35 full and part-time LCSW on staff in the Department of Social Work between the two study sites. Staff social workers arrive in the ED within 30 min of consultation. Staff social workers are trained and available to deliver interventions to patients presenting with an opioid overdose and/or with OUD in the ED. As LCSWs, these individuals are capable of delivering a variety of interviewing and intervention techniques that are rooted in social work theory and practice models. Social work practice models are strategies that the social worker can incorporate into their interventions to help people meet their goals (eg, task-centred practice, cognitive behavioural therapy, crisis intervention model). Although the intervention delivered by LCSWs and their associated theoretical underpinnings are similar in some respects to those associated with those delivered by certified peer recovery support specialists, the social worker intervention is intended to be a single session with referral to SUD treatment.
Outcomes
Primary outcomes
The two primary outcomes of the trial are (1) engagement with a formal SUD treatment programme within 30 days of the initial ED visit and (2) recurrent ED visit(s) for a suspected opioid overdose over 18 months. Both endpoints will be assessed via statewide administrative databases as outlined below. All records will be linked deterministically to participant data using identifiable information in a secure, Health Insurance Portability and Accountability Act-compliant computing environment.
The first primary outcome of the trial is treatment engagement, defined as admission to a formal, publicly licensed SUD treatment programme within 30 days of the initial ED visit. The Rhode Island Department of Behavioral Health, Developmental Disabilities, and Hospitals maintains the Behavioral Health Online Database (BHOLD), a state database containing information on all admission and discharge events of clients of all licensed behavioural healthcare organisations in the state.27 BHOLD is a comprehensive database on all licensed treatment programmes, including inpatient detoxification programmes, day treatment programmes, residential treatment programmes, intensive outpatient programmes and opioid treatment programmes.27 Records in BHOLD include individuals who receive methadone or buprenorphine from a licensed opioid treatment programme. In addition to this data resource, records from the prescription drug monitoring programme maintained by the Rhode Island Department of Health will be used to supplement BHOLD to identify patients who initiate buprenorphine in office-based settings.28
The second primary outcome of the trial is recurrent visits to the ED for a suspected opioid overdose, defined as any presentation to an ED in Rhode Island for an opioid overdose within the 18 months following the initial ED visit at the two sites. The Rhode Island Quality Institute maintains CurrentCare, a health information exchange that provides a unified data system for electronic medical records (EMRs) for all major health systems in Rhode Island, allowing us to identify repeat visits for suspected opioid overdoses at all 12 EDs in the state.29 Opioid overdoses will be defined according to the Centers for Disease Control and Prevention guidelines for all opioid poisonings and utilise International Statistical Classification of Diseases and Related Health Problems codes.30 31 The Rhode Island Department of Health mandates that all suspected overdoses presenting to a hospital be reported to the department within 48 hours. This data source, referred to as the 48-hour overdose surveillance system,32 will be used to supplement the EMRs in CurrentCare.
Sample size
Based on preliminary assessments from the study sites, we are assuming that 7% of participants assigned to receive a behavioural intervention from an LCSW will enrol in a formal SUD treatment programme within 30 days of their ED visit. Given this assumption for a sample size of 650 participants, we have at least 80% power to detect a twofold increase in treatment engagement among participants assigned to receive a behavioural intervention from a peer recovery specialist (risk difference: 0.07; 95% CI 0.02 to 0.12). This twofold increase was identified by community stakeholders as an appropriate benchmark for this outcome. Based on a recent medical record review from one of the study sites and estimates from other studies,20 33 we are assuming that 15% of participants who receive a behavioural intervention from an LCSW will experience a subsequent repeat ED visit for opioid overdose. Given this assumption and our sample, we have at least 80% power to detect a 50% relative reduction in the risk of recurrent ED visits for opioid overdose within 18 months following the initial visit among those assigned to receive a behavioural intervention from a peer recovery specialist (risk difference: 0.075; 95% CI 0.02 to 0.13).
Recruitment
Participants will be recruited from two EDs—level 1 and level 2 trauma centres—located in the state’s capital of Providence. Together, these two EDs receive over 175 000 adult visits each year. Between 2017 and 2018, the two EDs reported a total of 1446 visits for suspected opioid overdoses, representing 45% of all ED visits for suspected opioid overdose reported to the Rhode Island Department of Health (n=3239). A consecutive sample of ED patients will be assessed for eligibility by 1 of 11 full-time research assistants employed in the two EDs who can recruit participants 24 hours/day, 7 days/week. Potential participants will be identified by the research assistants by screening EMRs or by referral from treating providers in the ED. Potential participants will be considered eligible if they are 18 years of age or older and speak English. Given the specificity of the pool of LCSWs and certified peer recovery support specialists to the ED, recruitment will occur in the ED only.
Methods: assignment of interventions
Allocation
Participants will be randomly assigned 1:1 within each study site to receive either a behavioural intervention delivered by a certified peer recovery support specialist or by an LCSW. Allocations will be randomly assigned using the Research Electronic Data Capture (REDCap) randomisation feature. The randomisation schedule will be maintained by a data manager not involved with participant recruitment or the final study analyses.
Blinding (masking)
Participants and providers cannot be blinded to their intervention assignment. However, investigators and analysts performing the study analyses will be blinded to arm allocation.
Methods: data collection, management, analysis
Data collection methods
The primary outcomes assessments will rely on the use of administrative data (see Primary Outcomes).
Data management
All data collection instruments will be designed using REDCap software and administered using a tablet computer connected to the wireless network at the two study sites.
Statistical methods
We will use an intention-to-treat approach in all analyses to estimate the average treatment effect. For the two primary outcomes (engagement in formal SUD treatment within 30 days of the initial ED visit and occurrence of a subsequent ED visit for opioid overdose within 18 months of the initial ED visit), we will use separate logistic regression models with indicators for treatment allocation. Analyses with binary outcomes were selected based on input from community stakeholders. In exploratory analyses, we will use survival methods (eg, Cox proportional hazards models) to assess the impact of treatment on the time to events for both outcomes (ie, days from discharge to enrolment in formal SUD treatment and days from discharge to first recurrent ED visit for opioid overdose). In addition, on an exploratory basis, we will conduct moderation analyses to understand potential heterogeneity of treatment effects by age and gender. Given the multicentre design of the trial, the effect of treatment site will be quantified by the intraclass correlation coefficient (ICC), representing the variance due to the between-centre variability.34 Should the ICC suggest that a large portion of the variance is explained by between-centre variability, we will control for treatment site using a generalised estimating equations approach to estimate population-average treatment effects across the two sites.
Methods: monitoring
Data monitoring
A single data safety monitoring board (DSMB) will be convened and include members external to the research team and funding source and without potential conflicts of interest. The DSMB will be notified within 24 hours of any serious adverse event in which the relationship to the study is possible. The DSMB will convene at the earliest possible time (no more than 30 days from time of notification) to discuss this adverse event. Further, the DSMB will meet on a quarterly basis with the study coordinator and coprincipal investigators to review protocol adherence and adverse events.
Harms
An adverse event is considered any physical or clinical change experienced by the patient, including the onset of new symptoms or the exacerbation of pre-existing conditions.
Ethics and dissemination
Protocol amendments
Any modifications to the protocol which may impact on the conduct of the study, potential benefit of the patient or may affect patient safety, including changes of study objectives, study design, patient population, sample sizes, study procedures or significant administrative aspects will require a formal amendment.
Consent
Trained research assistants will introduce and discuss the trial with potential participants. These potential participants will then be able to have an informed discussion with the research assistant about their potential participation. Following this discussion, research assistants will obtain written informed consent.
Confidentiality
The privacy of all trial participants is protected by a Certificate of Confidentiality issued by the National Institutes of Health. Unique identification numbers will be assigned to participants. All data forms and interviews will be coded with this number rather than with a name. All paper forms will be stored in locked file cabinets. Informed consent documents will be stored separately, as they contain identifying information. On completion of the study, identifying information will be destroyed.
Access to data
The institutional review boards at the Lifespan health system representing the two clinical sites will have access to anonymised data at their discretion. However, no third-party investigators will have access to study data prior to synthesis and dissemination.
Dissemination policy
The study has been registered on ClinicalTrials.gov. A summary of the results of the trial will be published there when available. Results will be published at national scientific meetings and the final results will be submitted for publication in peer-reviewed journals.
Discussion
The AnchorED programme of Anchor Recovery Community Center, which deploys certified peer recovery support specialists to EDs across Rhode Island to deliver behavioural interventions to individuals who have experienced an opioid overdose, is the first statewide programme of its kind in the nation.23 Despite a lack of evidence to demonstrate the effectiveness of this programme and improved long-term outcomes for patients, several other jurisdictions in the US have created or are initiating programmes based on the AnchorED model.24 Given the intense interest in peer recovery models, the results of this trial have a strong potential to fundamentally change clinical practice paradigms for treating patients at high risk for opioid overdose who present to EDs across the nation.
The current study benefits from support from a unique policy environment in Rhode Island. In 2015, Governor Gina Raimondo signed an executive order to establish the Rhode Island Overdose Prevention and Intervention Task Force, which charged experts to develop a strategic plan to guide efforts to tackle the state’s overdose crisis.35 An important outcome of this plan was a comprehensive data sharing infrastructure between key state agencies (including the Rhode Island Departments of Health and Behavioral Healthcare, Developmental Disabilities and Hospitals) and academic researchers.36 These data sharing agreements offer unprecedented access to population-based data on overdose morbidity and mortality.36 As a result, the trial investigators can create a large database linking participant data with multiple administrative databases to ascertain our primary and secondary outcomes. The ability to conduct these robust data linkages is an important methodological innovation that overcomes biases associated with self-reported outcomes and loss to follow-up in previous studies.
The results of this trial will need to be considered in light of some caveats. Although Good Samaritan laws are present in many jurisdictions across the US, including Rhode Island, to protect individuals from criminal prosecutions,37 many people do not call emergency medical services in the event of an overdose.38 It is possible that the intervention may increase participants’ self-efficacy and willingness to engage with emergency medical services in the event of an overdose. As a result, those receiving the peer recovery intervention might be more likely to present to the ED in the event of an overdose. Should the intervention reduce the overall rate of non-fatal overdose but increase the proportion of non-fatal overdoses that are treated in the ED, the findings related to the impact of the intervention on recurrent ED visits may be null or counterintuitive. Although the administrative databases used to characterise the primary outcomes are meant to be representative, they are by no means comprehensive. Individuals who enrol in SUD treatment programmes or who present to EDs in other states will not be captured in these resources. Given the pragmatic nature of the trial, fidelity monitoring and process checking are not being conducted, thus limiting potential understanding of what components of the intervention were performed should they be deemed efficacious.
This trial represents the first systematic evaluation of behavioural interventions delivered by certified peer recovery support specialists in the ED to individuals at high risk for opioid overdose. Should the trial be successful, its findings have the potential to establish the evidence base for peer recovery support services as an effective intervention and provide support for the large-scale implementation of these services in EDs. Amidst a national crisis, peer recovery support interventions could be an effective means for improving SUD treatment engagement and reducing rates of fatal and non-fatal overdose.
Supplementary Material
Footnotes
Contributors: WCG led the manuscript preparation. The research was conceived by FLB and BDLM. All authors provided feedback on several drafts of the study protocol and this manuscript. WCG, BDLM, EAS, MGB, DD, KJL, LAM, RCM, TN, GAO, SER, JLY and FLB read and approved of the final manuscript.
Funding: This research is funded by a grant from the Laura and John Arnold Foundation (Principal Investigators: Francesca L Beaudoin, MD, PhD and Brandon DL Marshall, PhD) with support from the Center for Biomedical Research Excellence (COBRE) on Opioids and Overdose at Rhode Island Hospital (funded by the National Institute of General Medical Sciences, Award: P20GM125507; Principal Investigator: Josiah D Rich, MD). In addition, Mr Goedel is supported by the Brown University Clinical and Community Based HIV Research Training Fellowship (funded by the National Institute of Mental Health, Award: R25MH083620; Principal Investigator: Amy S Nunn, ScD).
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: All protocols have been approved by the institutional review boards at the Lifespan health system representing the two clinical sites (Approval Number: 212418).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Rudd RA, Seth P, David F, et al. Increases in Drug and Opioid-Involved Overdose Deaths - United States, 2010-2015. MMWR Morb Mortal Wkly Rep 2016;65:1445–52. 10.15585/mmwr.mm655051e1 [DOI] [PubMed] [Google Scholar]
- 2. Rudd RA, Aleshire N, Zibbell JE, et al. Increases in drug and opioid overdose deaths — United States, 2000–2014. MMWR Morb Mortal Wkly Rep 2016;64:1378–82. 10.15585/mmwr.mm6450a3 [DOI] [PubMed] [Google Scholar]
- 3. Scholl L, Seth P, Kariisa M, et al. Drug and Opioid-Involved overdose deaths — United States, 2013–2017. MMWR Morb Mortal Wkly Rep 2018;67:1419–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Seth P, Scholl L, Rudd RA, et al. Overdose deaths involving opioids, cocaine, and psychostimulants — United States, 2015–2016. MMWR Morb Mortal Wkly Rep 2018;67:349–58. 10.15585/mmwr.mm6712a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chen Q, Larochelle MR, Weaver DT, et al. Prevention of prescription opioid misuse and projected overdose deaths in the United States. JAMA Netw Open 2019;2:e187621 10.1001/jamanetworkopen.2018.7621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kiang MV, Basu S, Chen J, et al. Assessment of changes in the geographical distribution of opioid-related mortality across the United States by opioid type, 1999-2016. JAMA Netw Open 2019;2:e190040 10.1001/jamanetworkopen.2019.0040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Springer YP, Gladden RM, O’Donnell J, et al. Fentanyl drug submissions – United States, 2010–2017. MMWR Morb Mortal Wkly Rep 2019;68:41–2. [DOI] [PubMed] [Google Scholar]
- 8. Mercado-Crespo MC, Sumner SA, Spelke MB, et al. Increase in fentanyl-related overdose deaths - Rhode Island, November 2013–March 2014. MMWR Morb Mortal Wkly Rep 2014;63. [PMC free article] [PubMed] [Google Scholar]
- 9. Somerville NJ, O’Donnell J, Gladden RM, et al. Characteristics of fentanyl overdose - Massachusetts, 2014–2016. MMWR Morb Mortal Wkly Rep 2017;66:383–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tomassoni AJ, Hawk KF, Jubanyik K, et al. Multiple fentanyl overdoses — new Haven, Connecticut, June 23, 2016. MMWR Morb Mortal Wkly Rep 2017;66:107–11. 10.15585/mm6604a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Weiss AJ, Elixhauser A, Barrett ML, et al. Opioid-related inpatient stays and emergency department visits by state, 2009-2014. Rockville, Maryland: Agency for Healthcare Research and Quality, 2016. [PubMed] [Google Scholar]
- 12. Hasegawa K, Espinola JA, Brown DFM, et al. Trends in U.S. emergency department visits for opioid overdose, 1993–2010. Pain Med 2014;15:1765–70. 10.1111/pme.12461 [DOI] [PubMed] [Google Scholar]
- 13. Mazer-Amirshahi M, Sun C, Mullins P, et al. Trends in emergency department resource utilization for poisoning-related visits, 2003–2011. J. Med. Toxicol. 2016;12:248–54. 10.1007/s13181-016-0564-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yokell MA, Delgado MK, Zaller ND, et al. Presentation of prescription and nonprescription opioid overdoses to US emergency departments. JAMA Intern Med 2014;174:2034–47. 10.1001/jamainternmed.2014.5413 [DOI] [PubMed] [Google Scholar]
- 15. Vivolo-Kantor AM, Seth P, Gladden RM, et al. Vital Signs : Trends in Emergency Department Visits for Suspected Opioid Overdoses — United States, July 2016–September 2017. MMWR Morb Mortal Wkly Rep 2018;67:279–85. 10.15585/mmwr.mm6709e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Brady JE, DiMaggio CJ, Keyes KM, et al. Emergency department utilization and subsequent prescription drug overdose death. Ann Epidemiol 2015;25:613–9. 10.1016/j.annepidem.2015.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pavarin RM, Berardi D, Gambini D. Emergency department presentation and mortality rate due to overdose: a retrospective cohort study on nonfatal overdoses. Substance Abuse 2016;37:558–63. 10.1080/08897077.2016.1152342 [DOI] [PubMed] [Google Scholar]
- 18. Daly ER, Dufault K, Swenson DJ, et al. Use of emergency department data to monitor and respond to an increase in opioid overdoses in New Hampshire, 2011-2015. Public Health Rep 2017;132:73S–9. 10.1177/0033354917707934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bohnert ASB, Bonar EE, Cunningham R, et al. A pilot randomized clinical trial of an intervention to reduce overdose risk behaviors among emergency department patients at risk for prescription opioid overdose. Drug Alcohol Depend 2016;163:40–7. 10.1016/j.drugalcdep.2016.03.018 [DOI] [PubMed] [Google Scholar]
- 20. Banta-Green CJ, Coffin PO, Merrill JO, et al. Impacts of an opioid overdose prevention intervention delivered subsequent to acute care. Inj Prev 2019;25:191–8. 10.1136/injuryprev-2017-042676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ramchand R, Ahluwalia SC, Xenakis L, et al. A systematic review of peer-supported interventions for health promotion and disease prevention. Prev Med 2017;101:156–70. 10.1016/j.ypmed.2017.06.008 [DOI] [PubMed] [Google Scholar]
- 22. Eddie D, Hoffman L, Vilsaint C, et al. Lived experience in new models of care for substance use disorder: a systematic review of peer recovery support services and recovery coaching. Front Psychol 2019;10:1052 10.3389/fpsyg.2019.01052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Waye KM, Goyer J, Dettor D, et al. Implementing peer recovery services for overdose prevention in Rhode island: an examination of two outreach-based approaches. Addict Behav 2019;89:85–91. 10.1016/j.addbeh.2018.09.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Luthra S. States see peer-recovery coaches as a way to break the addiction epidemic [Web]. San Francisco, California: Kaiser Health News, 2016. Available: https://khn.org/news/states-see-peer-recovery-coaches-as-a-way-to-break-the-addiction-epidemic/
- 25. United States Department of Health and Human Services 2-year Restricted Use Data Analysis System (2016-2017) [Internet]. Rockville, Maryland: Substance Abuse and Mental Health Services Administration, 2018. Available: https://rdas.samhsa.gov/#/survey/NSDUH-2016-2017-RD02YR
- 26. Centers for Disease Control and Prevention Multiple Cause of Death, 1999-2017 [Internet]. Hyattsville, Maryland: National Center for Health Statistics, 2019. Available: https://wonder.cdc.gov/mcd-icd10.html
- 27. State of Rhode Island. Reporting Requirements - RI BHOLD [Internet] Providence, Rhode island: department of behavioral healthcare, developmental disabilities, and hospitals, 2019. Available: http://www.bhddh.ri.gov/sections/reporting.php
- 28. State of Rhode Island Prescription Drug Monitoring Program [Internet]. Providence, Rhode Island: Department of Health, 2019. Available: http://health.ri.gov/healthcare/medicine/about/prescriptiondrugmonitoringprogram/
- 29. Adams LL. The role of health information technology in improving quality and safety in RI: can new money solve old problems? R I Med J 2009;98:267–8. [PubMed] [Google Scholar]
- 30. Rowe C, Vittinghoff E, Santos G-M, et al. Performance measures of diagnostic codes for detecting opioid overdose in the emergency department. Acad Emerg Med 2017;24:475–83. 10.1111/acem.13121 [DOI] [PubMed] [Google Scholar]
- 31. Ellison J, Walley AY, Feldman JA, et al. Identifying patients for overdose prevention with ICD-9 classification in the emergency department, Massachusetts, 2013-2014. Public Health Rep 2016;131:671–5. 10.1177/0033354916661981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. McCormick M, Koziol JA, Sanchez K. Development and use of a new opioid overdose surveillance system, 2016. R I Med J 2017;100:37–9. [PubMed] [Google Scholar]
- 33. Samuels EA, Bernstein SL, Marshall BDL, et al. Peer navigation and take-home naloxone for opioid overdose emergency department patients: preliminary patient outcomes. J Subst Abuse Treat 2018;94:29–34. 10.1016/j.jsat.2018.07.013 [DOI] [PubMed] [Google Scholar]
- 34. Moerbeek M, van Breukelen GJ, Berger MP. A comparison between traditional methods and multilevel regression for the analysis of multicenter intervention studies. J Clin Epidemiol 2003;56:341–50. 10.1016/S0895-4356(03)00007-6 [DOI] [PubMed] [Google Scholar]
- 35. State of Rhode Island Rhode Island’s Strategic Plan on Addiction and Overdose: Four Strategies to Alter the Course of an Epidemic. Providence, Rhode Island: Governor’s Overdose Prevention and Intervention Task Force, 2015. [Google Scholar]
- 36. Marshall BDL, Yedinak JL, Goyer J, et al. Development of a statewide, publicly accessible drug overdose surveillance and information system. Am J Public Health 2017;107:1760–3. 10.2105/AJPH.2017.304007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. McClellan C, Lambdin BH, Ali MM, et al. Opioid-Overdose laws association with opioid use and overdose mortality. Addict Behav 2018;86:90–5. 10.1016/j.addbeh.2018.03.014 [DOI] [PubMed] [Google Scholar]
- 38. Koester S, Mueller SR, Raville L, et al. Why are some people who have received overdose education and naloxone reticent to call emergency medical services in the event of overdose? Int J Drug Policy 2017;48:115–24. 10.1016/j.drugpo.2017.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


