Abstract
Researchers trialing behavioral interventions often use attention control groups, but few publish details on attention control activities or perceived benefit. Attention control groups receive the same dose of interpersonal interaction as intervention participants but no other elements of the intervention, to control for the benefits of attention that may come from behavioral interventions. Because intervention success is analyzed compared to control conditions, it is useful to examine attention control content and outcomes. The purpose of this study is to report on attention control visit activities and their perceived benefit in a randomized control trial. The trial tested an aging-in-place intervention comprised of a series of participant goal-directed visits facilitated by an occupational therapist, nurse, and handyman. The attention control group participants received visits from a lay person. We report on the number and length of visits received, types of visit activities that participants chose, and how much visit time was spent on each activity, based on the attention visitor’s records. We report on participant perceptions of benefit based on a 10-item Likert-scale survey. The attention control group participants (n = 148) were cognitively intact, at least 65 years old, with at least one Activities of Daily Living limitation. Attention control group participants most often chose conversation (20.1% of visit time), and playing games (18.7%), as visit activities. The majority of attention control group participants (63.4%) reported “a great deal” of perceived benefit. Attention control group visits may be an appropriate comparison in studies of behavioral interventions for community-dwelling older adults.
Keywords: attention control, behavioral intervention, community-dwelling older adults
Introduction
Behavioral interventions demonstrate efficacy in improving depression, improving the experience of dementia caregiving, and reducing functional decline in community-dwelling older adults (Szanton et al., 2019; Gitlin et al., 2016). Behavioral intervention trials examine whether those who receive the intervention benefit more than a similar group who receives no care, or a similar group who receives a comparison of interest. Behavioral interventions include not just the elements of the interventions themselves but also inherently include attention from the intervention facilitators which itself may benefit participants. This can make it challenging to determine the benefits of the content of the intervention.
One strategy for addressing comparison challenges in behavioral interventions is to provide control group study participants with attention control visits. In an attention control group, participants receive social attention equivalent in dose and timing to that provided by the intervention (Aycock, Hayat, Helvig, Dunbar, & Clark, 2018). Attention and interpersonal interactions alone may influence depression, pain, anxiety and other health outcomes (Popp & Schneider, 2015; Stice, Burton, Bearman, & Rhode, 2007; Seers, Crichton, Tutton, Smith, & Saunders, 2008; Hedman et al., 2011). Attention control groups help researchers disentangle the benefits of attention from the impacts of the intervention itself. This allows researchers to assess whether the intervention being tested is effective beyond the benefits of social interaction alone.
Many behavioral trials use attention control groups as a comparison, but few publications provide detail about the attention control group, such as who facilitated the attention control group and what activities were facilitated (Aycock et al., 2018). This results in a lack of literature to guide future researchers on employing an attention control group in behavioral trials. Therefore, the purpose of this study is to report on attention control visit activities and what their perceived benefit was in a randomized control trial. The trial tested an aging-in-place intervention comprised of a series of participant goal-directed visits facilitated by an occupational therapist, nurse, and handyman. The team provided participants with support in enhancing individual functional capacity and with home modifications to improve the home environment. We analyze data from the attention control group participants in a randomized trial of the CAPABLE intervention (Szanton et al., 2019). CAPABLE is designed to improve function among low-income community-dwelling older adults by providing time-limited services focused on functional goals as determined by the older adult participants (Szanton, Leff, Wolff, Roberts, & Gitlin, 2016). Examples of services provided by the team include the occupational therapist developing and facilitating a tailored physical activity program, the registered nurse completing a medication review to reduce fall risk, or the handyman installing handrails to facilitate improved navigation of the home environment. CAPABLE has been widely studied and shows both therapeutic benefits and cost-effectiveness as an intervention to promote successful aging in place (Szanton et al., 2019; Szanton et al., 2017; Szanton et al., 2014; Szanton et al., 2015; Szanton et al., 2011; Szanton & Gitlin, 2016; Szanton et al., 2016).
The study we report on here was a controlled study in which participants were randomized to the CAPABLE treatment group or to receive one-on-one, in-home, visits from an attention visitor. The goal of the attention control group was to match the amount of attention time provided to the treatment group in order to determine if CAPABLE provides benefit to intervention participants beyond the benefit of the attention provided by the nurse, occupational therapist and handyman. The results of the randomized control trial are provided in a different manuscript (Szanton et al., 2019). Here, we focus on describing and analyzing the attention control group. The aims of this analysis are to report on the number and length of visits received, types of activities that older adult participants chose, how much visit time was spent on each type of activity, and perceived benefit among the attention control group participants in a randomized control trial of the CAPABLE behavioral intervention.
Methods
Study Setting and Recruitment
The study took place in Baltimore, Maryland between 2012 and 2016. Participants were recruited through direct mailings (35%), government program referrals (19%), community-based organizations (16%), ambassador referrals by CAPABLE participants from previous trials (15%), and media (4%). More details on recruitment are provided in a separate manuscript (Nkimbeng et al., 2018). The study was approved through the Johns Hopkins University Institutional Review Board.
Study Sample
Participants were required to be aged 65 or older, report difficulty with at least 1 Activity of Daily Living (ADL) (Katz et al., 1963) or 2 Instrumental Activities of Daily Living (IADL) (Lawton & Brody, 1969), have a self-reported income at or below 200% of Federal Poverty Level, and be able to stand with or without assistance. Participants were excluded if they had a cognitive impairment, had been hospitalized more than 3 times in the past year, if they were currently receiving in-home nursing, occupational therapy or physical therapy, if they were receiving cancer treatment, if they lived in an apartment, if they had a terminal diagnosis, or if they planned to move from their current residence within the year. Baseline participant characteristics are presented in Table 1. The control group was similar to the intervention group in terms of age, sex, race, education, and whether or not the participant lived alone (Szanton et al., 2019).
Table 1:
Baseline Attention Control Group Participant Characteristics
| Attention control Participants (n = 148) | ||
|---|---|---|
| Age, years | Mean | SD |
| 75.4 | 7.4 | |
| Sex (female) | No. | % |
| 129 | 87.2 | |
| Race | No. | % |
| White | 14 | 9.5 |
| Black | 133 | 89.9 |
| Asian | 1 | 0.7 |
| Education | No. | % |
| < 12 years | 54 | 36.7 |
| ≥ 12 years | 93 | 63.3 |
| Live Alone | No. | % |
| 70 | 47.3 | |
A total of 300 participants were randomized to the intervention group (152) or the attention control group (148). Participants received a mailed letter stating whether they had been randomized to the intervention or to the attention control group. The attention control group letter provided a brief description of the attention control group, explaining that a member of the research team would make visits to converse, play cards/board games, listen to music, create scrapbooks or to facilitate other activities the person found appealing.
Attention Control Group Design
Whereas participants assigned to the intervention group received the CAPABLE intervention, those assigned to the control group received attention visits. All attention control group visits were provided by one attention visitor who was hired for this role and was otherwise not involved in the study implementation.
The researchers asked the attention visitor to facilitate activities with participants that the participants identified as meaningful or enjoyable. The research team asked the attention visitor to limit attention control group activities to sedentary activities that could take place in the participants’ homes. Otherwise, the team provided the attention visitor with minimal guidance as to what activities to initiate on his visits.
The attention visitor was asked to visit each participant for the same number of hours and visits as were provided by the nurse, handyman and occupational therapist to the intervention group. The attention visitor encouraged each participant to choose an enjoyable activity for each visit. He provided the participants with examples of appropriate activities, such as playing games or listening to music together, but also encouraged the participant to identify activities other than the examples provided. The attention visitor was asked to visit each attention control group participant 10 times over the course of the five-month study. If a participant received between 8–10 visits, that was considered a full dose. The study team administered a 10-item survey regarding perception of benefit to each participant at 5 months.
Measures
Duration and number of visits.
The attention visitor recorded the date, type of activity and duration of each visit.
Perception of benefit.
On a separate blinded data collection visit that was at five months post-baseline, participants reported to a trained data collector on their perceived benefit of the study in response to Likert scale questions on a 10-item survey. The study team administered the same perception of benefit survey to the attention control group participants as we administered to the intervention participants. The survey was adapted from previous trials of behavioral interventions (Gitlin, Winter, Dennis, Hodgson, & Hauck, 2010). The response to each question on the survey was analyzed separately. The survey asked participants to report their perception of the extent to which participation in the study 1) was beneficial overall, 2) made life easier, 3) made home safer, 4) kept the participant living at home, 5) helped with gaining confidence, 6) helped with caring for self, 7) helped with caring for others, 8) lessened distress, and 9) would help others. The tenth question asked participants whether they felt that participating in the study required too much work. The Likert scale for all ten questions included three responses: not at all, some, or a great deal.
Data Analysis
Duration and number of visits.
We analyzed the duration and number of visits for each participant and averaged them across the group to provide a mean.
Attention control group visit content.
Two members of the study team, including a non-intervention Occupational Therapist with activity expertise, coded each attention control group visit activity into categories. The categories were developed by three members of the study team based on initial review of the visit activities. After two coders had coded all activities, a third member reconciled any category coding disagreements. Because all attention control group visits contained conversation at least as a secondary activity, when a visit was coded both as “conversation” as well as another activity such as “play games,” the visit time was linked to the non-conversation activity. Therefore, time allocated to “conversation” only accounts for those visits in which “conversation” was the only activity. For visits on which two other types of activities were tracked, half of the visit time was allocated to each of the two activities, because it was unknown what portion of the visit was allocated to each activity.
Perception of benefit.
Responses to each question on the 10-item participant survey were aggregated and analyzed based on percentage of participants who responded, “not at all,” “some,” or “a great deal.”
Results
Number and Length of Visits
Of the 148 participants randomized to the attention control group, 73 (49%) received the full dose of 8–10 visits. Fifty-six (37.8%) attention control group participants received fewer than 3 visits. Of the attention control group participants, 123 (83.1%) completed the 5-month survey. The mean number of visits received by the group was 6.8. The mean visit length was 60.1 minutes. Additional details about visits are provided in Table 2.
Table 2:
Attention Control Group Visit Details
| Visit Length (minutes) | Minimum: 10 | Mean: 60.1 | Maximum: 200 |
|---|---|---|---|
| Number of Attention Control Group Visits by Visit Length | |||
| < 30 mins | 33 (4.23%) | ||
| 30–60 mins | 535 (68.5%) | ||
| > 60 mins | 201 (25.74%) | ||
| Visit length missing from tracking sheet | 12 (1.54%) | ||
| Number of Visits Per Participant | Minimum: 1 | Mean: 6.8 | Maximum: 10 |
| Number of Attention Control Group Participants Receiving Full Dose of Visits | |||
| 1 – 3 visits | 35 (30.4%) | ||
| 4 – 7 visits | 14 (12.2%) | ||
| 8 – 10 visits (full dose) | 66 (57.4%) | ||
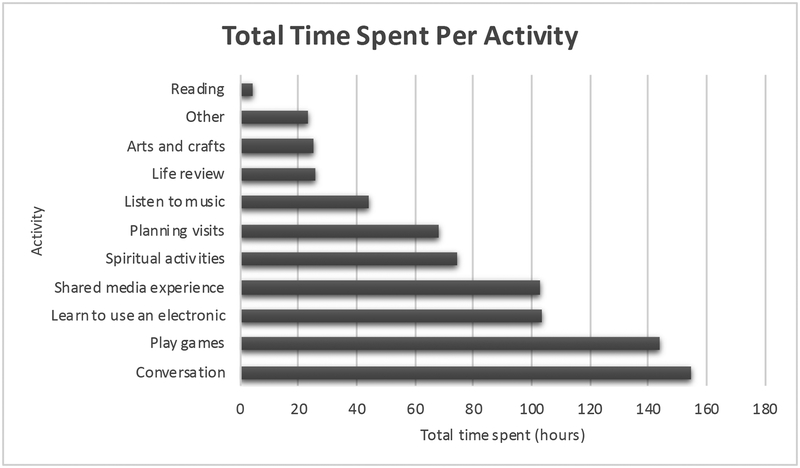
Types of Activities and Time Spent Per Activity
The visit activity most commonly reported was conversation, followed by playing games. The next most common preferred activities were learning to use an electronic device or a shared media experience. The fewest visits were spent reading aloud, conducting life review, or doing arts and crafts. Activities coded as “arts and crafts” included activities such as creating scrapbooks and drawing together. Visits coded as “learn to use an electronic” included activities such as setting up an email account or learning to send text messages. “Life review” included things like “remembering old times” or “learning about participant’s life.” “Listening to music” included all types of listening to music except those that specified that they listened to spiritual music. Spiritual music listening was coded as “spiritual activities” along with other spiritual activities such as reading and discussing the bible together. “Play games” included card games, Monopoly, dominoes, bingo, and others. “Reading” included any time spent reading aloud to each other besides spiritual reading. “Planning” included time spent by the participant and the attention visitor determining how they would spend their future visits together. Planning also included time finding supplies and time that the attention visitor spent showing participants how to do the activities, when necessary.
Because watching television was not considered providing attention, the attention visitor did not spend time passively watching television with participants. However, on some visits, he did watch and discuss YouTube videos or television shows with participants. These types of activities were included in the category “Shared media experience.” Less common activities such as researching coins together and creating an address list were coded as “Other.” Time spent by activity type is summarized in Figure 1.
Figure 1:
Total Time Spent Per Activity (Hours)
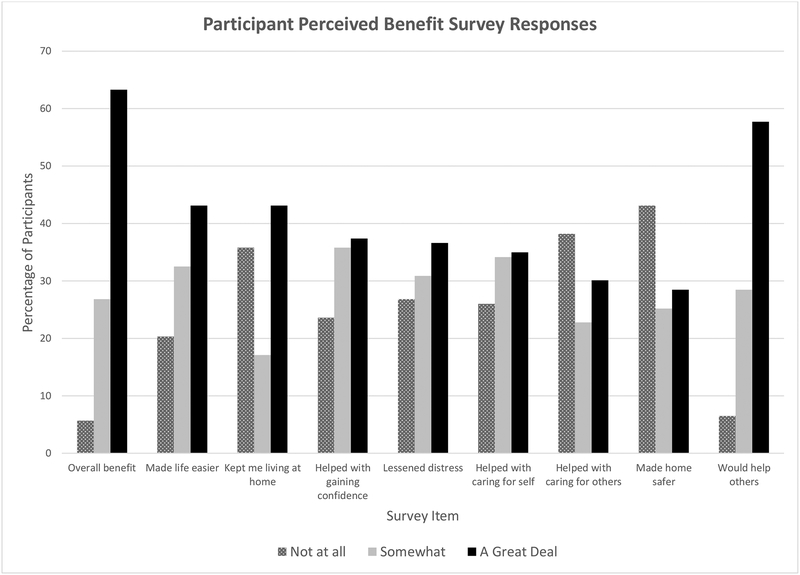
Perceived Participant Benefit
Of the attention control group participants, 5.7% perceived no overall benefit from their participation in the study, 26.8% perceived some benefit, and 63.4% perceived a great deal of benefit. For six of the eight specific benefits, the largest fraction of participants reported the perceived benefit as “a great deal;” this ranged from 35.0% for “helped with caring for self” to 57.7% for “would help others.” The two benefits that the largest fraction of participants rated as “not at all” were “helped with caring for others” (38.2%) and “made home safer” (43.1%). Nevertheless, for these latter benefits, 30.1% and 28.5% of participants, respectively, rated their benefit as “a great deal.” In response to the question asking whether participating in the study required too much work, 87.8% of attention control group participants responded “not at all,” 6.5% responded “somewhat” and 1.63% responded “a great deal.” Perceived participant benefit results for the attention control group are reported in Figure 2.
Figure 2:
Attention Control Group Participants’ Perceived Benefit
Discussion
The attention control group employed in this trial of the CAPABLE intervention provides an example of the types of activities that can be included in an attention control group for a community-based aging in place intervention. Attention control group participants generally perceived benefit from chosen activities, so researchers may want to include these activities as possible options for future older adult attention control group participants. Conversation was the most popular activity among attention control group participants in this study. This is valuable information for researchers designing attention control groups for community-dwelling older adults. Future analysis of attention control group activities in studies of aging in place interventions should further examine older adult preferences for conversation versus more structured activities like arts and crafts.
In this trial, we found that attention control participants perceived less benefit than the intervention group, both in terms of overall benefit from participating in the study, and in response to each of the eight survey questions about specific benefit (Szanton et al., 2019). For example, 28.5% of the attention control group participants compared to 82.3% of the intervention group participants reported that the study helped to make their homes safer (Szanton et al., 2019). This provides valuable information when comparing the attention control group results to the intervention group results. These compared results allowed us to more confidently interpret that the intervention did improve participants’ perception of benefit beyond the general benefit of increased attention, than if we had compared the intervention group to a waitlist control group (Aycock et al., 2018). For full results comparing the attention control group to the intervention group in terms of number and length of visits and perception of benefit, please see Szanton et al., 2019.
This attention control group provided an opportunity to rigorously test a behavioral aging in place intervention, by offering a beneficial alternative to non-intervention group participants. Participants in this attention control group, like their peers in the intervention group, were asked to select visit activities rather than the facilitator dictating them. Many behavioral interventions, including the CAPABLE intervention, are individually tailored to meet participant needs and priorities. In trials of goal-directed or individually tailored interventions, asking attention control group participants to choose their activities should be considered as a design element in order to make the experience of attention control groups as similar as possible to that of the intervention participants. Most importantly, in order to improve the rigor of the comparison, activities should be selected that attention control group participants perceive to be interesting and enjoyable (Aycock et al., 2018).
It is also important to consider the benefit that participants perceived from the attention control group visits. Although the benefits of aging in one’s own environment, neighborhood, and home are tremendous, it is important to critically consider the impact that aging in place may have on an older adult’s social connections, and how aging in place models can mitigate the risks of perpetuating loneliness. The evidence on the effectiveness of one-to-one attention interventions for older adults is mixed (Ong, Uchino, & Wethington, 2016). However, most one-to-one attention interventions for older adults do not allow the older adult to control the activities or structure of attention visits (Cattan, White, Bond, & Learmouth, 2005). The results from this study indicate that some community-dwelling older adults may find benefit from participant-directed attention visits. Allowing older adults to choose activities may be an important consideration when designing one-to-one loneliness interventions or attention control groups for community-dwelling older adults.
The majority of attention control group participants reported that the study was beneficial and that it may benefit others. Given that for six of eight specific perceived benefits the largest fraction of participants rated the benefit as “a great deal,” the benefits of the attention control group were wide-ranging. It is possible that attention control group participants perceived benefit because they felt less lonely due to the visits from the attention control group attention visitor. Future studies should continue to explore the value of participant-directed attention visits for improving community-dwelling older adults’ loneliness.
Unsurprisingly, studies that use a placebo or wait list control group consistently conclude that the studied intervention was more impactful than do studies that use an attention or active control group (Karlsson & Bergmark, 2015). Most studies and systematic reviews fail to thoroughly acknowledge the rationale behind control group design, or to adequately account for control group design when discussing study limitations or concluding about an intervention’s impact (Karlsson & Bergmark, 2015). Failure to appropriately choose the appropriate control group design, or to adequately acknowledge control group design in the literature, likely influences accurate evaluation of interventions. Researchers should provide information about attention control group design, such as is provided in this article, in trial manuscripts. There may be value in editors or reviewers specifically calling for this information in submission requirements, especially in protocol papers.
A limitation of this study is that it took place in one city with low-income older participants with disabilities and thus may not be generalizable. Additionally, the attention control group visits were facilitated by just one individual. The attention visitor was a long-time resident of Baltimore and was an older adult himself. However, he was a white man and most participants were African American women. Future studies should explore the impact of racial and gender concordance of attention control group facilitators with participants. It is also a limitation of this study that conversation was not tracked by type; for example, some conversation might have been more superficial (“small talk”) whereas other conversation was more meaningful. In future studies, researchers should consider developing more discrete activity categories including conversation types. These efforts will help to improve the body of knowledge on what activities are most relevant to include as control in studies of behavioral interventions for older adults. Another limitation is that we did not assess or report psychometrics of the perceived benefit survey so we cannot attest to the reliability of the instrument.
Attrition after randomization is a limitation in this study as it is in many evaluations of behavioral interventions. Although attention control groups can help address attrition by offering something of value to control participants, participants may still prefer the intervention of interest and therefore not choose to accept the attention control group visits, as some did in this trial. In this study, participants were offered the same number and length of visits, regardless of group allocation, but more of the intervention group participants received the full dose than did attention control group participants (Szanton et al. 2019). To address this issue, researchers could consider using a waitlist attention control group design in which participants allocated to the attention control group later receive the intervention. A waitlist attention control group may be useful, unless researchers intend to look at long-term outcomes, in which case it may be necessary to compare the intervention group against a control group that is never exposed to the intervention. Additionally, some participants within the attention control group had longer or more visits than others (see Table 2) which may have impacted results. Those participants who received more visits or longer visits may have perceived that the study was more beneficial because they had received more attention. They also may have wanted more visits than the ones who received a smaller dose because they found them beneficial. In future studies, efforts should be made to make the length of visits more uniform based on an attention control group protocol. Lastly, participant baseline social connections and level of family/social support were not included as variables and may have impacted results in this study.
Despite its limitations, this study has many strengths. The findings provide valuable information for future trials of behavioral interventions. Some community-dwelling older adults may perceive general benefit from participant-directed social interaction with an attention visitor, making it an appropriate comparison to behavioral interventions aimed at improving function and ability to age in place. The study primarily included African American women, an underrepresented group in research. In addition, the study only included low-income adults with activity limitations, a group that is also underrepresented in research due to recruitment challenges.
Conclusion
This manuscript reports on the activities that were selected by attention control group participants in a trial of the CAPABLE intervention. Researchers should consider publishing manuscripts specific to attention control group activities and results so that other researchers can use the information to improve the rigor of future studies. The participants in our study most often chose to participate in conversation and playing games so researchers may want to consider employing these attention control group activities in future studies of behavioral interventions. Attention control group participants in this trial generally perceived benefit from the study, indicating that attention control groups may be a useful comparison in studies of in-home behavioral interventions with community-dwelling older adults.
Acknowledgment of financial and other support:
This project was supported by the National Institute on Aging, NIA AG040100.
Footnotes
The authors declare no conflicts of interest.
References
- Aycock DM, Hayat MJ, Helvig A, Dunbar SB, & Clark PC (2018). Essential considerations in developing attention control groups in behavioral research. Research in Nursing and Health, 41, 320–328. doi: 10.1002/nur.21870 [DOI] [PubMed] [Google Scholar]
- Cattan M, White M, Bond J, & Learmouth A (2005). Preventing social isolation and loneliness among older people: A systematic review of health promotion interventions. Aging & Society, 25, 41–67. doi: 10.1017/S0144686X04002594 [DOI] [PubMed] [Google Scholar]
- Gitlin LN, Hodgson NA, & Choi SSW (2016). Home-based interventions targeting persons with dementia: What is the evidence and where do we go from here? In Boltz M & Galvin J (Eds.), Dementia Care. Springer. doi: 10.1007/978-3-319-18377-0_11 [DOI] [Google Scholar]
- Gitlin LN, Winter L, Dennis MP, Hodgson H, & Hauck WW (2010). A biobehavioral home-based intervention and the well-being of patients with dementia and their caregivers: the COPE randomized Trial. Journal of the American Medical Association, 304(9), 983–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedman E, Andersson G, Andersson E, Ljotsson B, Ruck C, Asmundson GJG, & Lindefors N Internet-based cognitive-behavioural therapy for severe health anxiety: randomised controlled trial. (2011). British Journal of Psychiatry, 198(3), 230–236. doi: 10.1192/bjp.bp.110.086843. [DOI] [PubMed] [Google Scholar]
- Karlsson P, & Bergmark A (2015, January 15). Compared with what? An analysis of control-group types in Cochrane and Campbell reviews of psychosocial treatment efficacy with substance abuse disorders. Addiction, 110(3), 420–428. doi: 10.1111/add.12799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz S, Ford AB, Moskowitz RW, Jackson BA, & Jaffe MW (1963) Studies of illness in the aged. The index of ADL: A Standardized measure of biological and psychosocial function. JAMA, 185, 914–919. [DOI] [PubMed] [Google Scholar]
- Lawton MP, & Brody EM (1969). Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist, 9, 179–186. [PubMed] [Google Scholar]
- Nkimbeng M, Roberts L, Thorpe RJ, Gitlin LN, Delaney A, Tanner EK, & Szanton SL (2018). Recruiting older adults with functional difficulties into a community-based research study: Approaches and costs. Journal of Applied Gerontology. 10.1177/0733464818786612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong AD, Uchino BN, & Wethington E (2016). Loneliness and health in older adults: A mini-review and synthesis. Gerontology, 62, 443–449. doi: 10.1159/000441651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popp L, & Schneider S (2015, April 11). Attention placebo control in randomized controlled trials of psychosocial interventions: theory and practice. Trials, 16(150). doi: 10.1186/s13063-015-0679-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seers K, Crichton N, Tutton L, Smith L, & Saunders T (2008, June). Effectiveness of relaxation for postoperative pain and anxiety: randomized controlled trial. Journal of Advanced Nursing,62(6), 681–688. doi: 10.1111/j.1365-2648.2008.04642.x. [DOI] [PubMed] [Google Scholar]
- Stice E, Burton E, Bearman S, & Rohde P (2007, May). Randomized trial of a brief depression prevention program: An elusive search for a psychosocial placebo control condition. Behavior Research and Therapy, 45(5), 863–876. doi: 10.1016/j.brat.2006.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szanton SL, Alfonso YN, Leff B, Guralnik J, Wolff JL, Stockwell I, Gitlin LN & Bishai D (2017, November 22). Medicaid cost savings of a preventive home visit program for disabled older adults. Journal of the American Geriatrics Society, 66(3), 614–620. doi: 10.1111/jgs.15143 [DOI] [PubMed] [Google Scholar]
- Szanton SL & Gitlin LN (2016, January 1). Meeting the health care financing imperative through focusing on function: The CAPABLE studies. Public Policy & Aging Report, 26(3), 106–110. 10.1093/ppar/prw014 [DOI] [Google Scholar]
- Szanton SL, Leff B, Wolff JL, Roberts L, & Gitlin LN (2016). Home-based care program reduces disability and promotes aging in place. Health Affairs, 35(9), 1558–1563. 10.1377/hlthaff.2016.0140 [DOI] [PubMed] [Google Scholar]
- Szanton SL, Thorpe RJ, Boyd C, Tanner EK, Leff B, Agree E, … Gitlin LN (2011). Community Aging in Place, Advancing Better Living for Elders (CAPABLE): A bio-behavioral-environmental intervention to improve function and health-related quality of life in disabled, older adults. Journal of the American Geriatrics Society, 59(12), 2314–2320. 10.1111/j.1532-5415.2011.03698.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szanton SL, Wolff JL, Leff B, Roberts L, Thorpe RJ, Tanner EK, Boyd C, Xue QL, Guralnik J, Bishai D & Gitlin LN (2015, January 30). Preliminary data from Community Aging In Place, Advancing Better Living For Elders, a patient-directed, team-based intervention to improve physical function and decrease nursing home utilization: The first 100 individuals to complete a centers for Medicare and Medicaid services innovation project. Journal of the American Geriatrics Society, 63(2), 371–374. doi: 10.1111/jgs.13245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szanton SL, Wolff JW, Leff B, Thorpe RJ, Tanner EK, Boyd C, Xue Q, Guralnik J, Bishai D & Gitlin LN (2014, May). CAPABLE trial: a randomized controlled trial of nurse, occupational therapist and handyman to reduce disability among older adults: rationale and design. Contemporary Clinical Trials, 38(1), 102–112. doi: 10.1016/j.cct.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szanton SL, Xue QL, Leff B, Guralnik J, Wolff JL, Tanner EK, Boyd C, Thorpe RJ, Bishaii D, & Gitlin LN (2019). Effect of a biobehavioral environmental approach on disability among low-income older adults: A randomized clinical trial. JAMA Internal Medicine, 179(2). doi: 10.1001/jamainternmed.2018.6026 [DOI] [PMC free article] [PubMed] [Google Scholar]