Abstract
Background
Wearable sensors are acquiring more and more influence in diagnostic and rehabilitation field to assess motor abilities of people with neurological or musculoskeletal impairments. The aim of this systematic literature review is to analyze the wearable systems for monitoring shoulder kinematics and their applicability in clinical settings and rehabilitation.
Methods
A comprehensive search of PubMed, Medline, Google Scholar and IEEE Xplore was performed and results were included up to July 2019. All studies concerning wearable sensors to assess shoulder kinematics were retrieved.
Results
Seventy-three studies were included because they have fulfilled the inclusion criteria. The results showed that magneto and/or inertial sensors are the most used. Wearable sensors measuring upper limb and/or shoulder kinematics have been proposed to be applied in patients with different pathological conditions such as stroke, multiple sclerosis, osteoarthritis, rotator cuff tear. Sensors placement and method of attachment were broadly heterogeneous among the examined studies.
Conclusions
Wearable systems are a promising solution to provide quantitative and meaningful clinical information about progress in a rehabilitation pathway and to extrapolate meaningful parameters in the diagnosis of shoulder pathologies. There is a strong need for development of this novel technologies which undeniably serves in shoulder evaluation and therapy.
Keywords: Shoulder kinematics, Upper limb, Wearable system, Inertial sensors, Smart textile
Background
Shoulder kinematics analysis is a booming research field due to the emergent need to improve diagnosis and rehabilitation procedures [1]. The shoulder complex is the human joint characterized by the greatest range of motion (ROM) in the different planes of space.
Commonly, several scales and tests are used to evaluate shoulder function, e.g., the Constant-Murley score (CMS), the Simple Shoulder test (SST), the Visual Analogue Scale (VAS) and the Disability of the Arm, Shoulder, and Hand (DASH) score [2–4]. However, despite their easy-to-use and wide application in clinical settings, these scores conceal an intrinsic subjectivity [2–4], inaccuracy in approaching diagnosis, follow-up and treatment of the pathologies. Quantitative and objective analyses are rapidly developing as a valid alternative to evaluate shoulder activity level, to gauge its functioning and to provide information about movement quality, e.g., velocity, amplitude and frequency [5, 6]. This interest in the use of measuring systems is growing in many medical fields to record information of clinical relevance. For example, electromyography (EMG), force sensors, inertial measurement units (IMU), accelerometers, fiber optic sensors and strain sensors are employed for human motion analysis, posture and physiological parameters monitoring [7–10]. From a technological viewpoint, the monitoring of shoulder motion is challenging due to the complexity of joint kinematic which require the development of protocols exploiting sensing technology as much as possible reliable and unobtrusive. In the last years, a great number of human motion analysis systems have been largely employed for objective monitoring. These systems can be classified into two main categories: wearable and non-wearable [11]. The last one includes electromagnetic tracking systems (e.g., Fastrak) [12], ultrasound-based motion analysis systems (e.g., Zebris) [13], stereo-photogrammetric and optoelectronic systems (e.g., VICON, Optotrak, BTS SMART-D) often used as gold standard [14–17]. These systems based on magnetic field, ultrasound and cameras are effectively suitable for 3D motion tracking and analysis due to their accuracy, precision and reliability [18]. On the other hand, such systems require expensive equipment, frequent calibration and, overall, they restrict measurements in structured environment [19]. Wearable systems overcome these shortcomings and they are a promising solution for continuous and long-term monitoring of human motion in daily living activities. Gathering data in unstructured environment continuously (e.g., home environment) provide additional information compared to those obtainable inside a laboratory [20].
Wearable sensor-based systems, intended for kinematics data extraction and analyses, are acquiring more and more influence in diagnostic applications, rehabilitation follow-up, and treatments of neurological and musculoskeletal disorders [21, 22]. Such systems comprise accelerometers, gyroscopes, IMU, among others [23]. Patients’ acceptance of monitoring systems that should be worn for long-time relies on sensors’ features whose must be lightweight, unobtrusive and user-friendly [24]. The increasing trend to adopt such wearable systems has been promoted by the innovative technology of micro-electro-mechanical systems (MEMS). MEMS technology has fostered sensors’ miniaturization, paving the way for a revolutionary technology suited to a wide range of applications, including extraction of clinical-relevant kinematics parameters. In recent years, there has been growth in the use of smart textile-based systems which integrate sensing units directly into garments [11, 25, 26]. Moreover, in the era of big data, machine learning technical analysis can improve home rehabilitation thanks to the recognition of the quality level of performed physical exercises and the possibility to prevent disorders in patients’ movement [27].
The aim of this systematic literature review is to describe the wearable systems for monitoring shoulder kinematics. The authors want to summarize the main features of the current wearable systems and their applicability in clinical settings and rehabilitation for shoulder kinematics assessment.
Methods
Literature search strategy and study selection process
A systematic review was executed applying the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [28]. Full-text articles and conference proceedings were selected from a comprehensive search of PubMed, Medline, Google Scholar and IEEE Xplore databases. The search strategy included free text terms and Mesh (Medical Subject Headings) terms, where suited. These terms were combined using logical Boolean operators. Keywords and their synonyms were combined in each database as follows: (“shoulder biomechanics” OR “upper extremit*” OR “shoulder joint” OR “scapular-humeral” OR “shoulder kinematics” OR “upper limb”) AND (“wearable system*” OR “wearable device*” OR “wearable technolog*” OR “wearable electronic device*” OR “wireless sensor*” OR “sensor system” OR “textile” OR “electronic skin” OR “inertial sensor”). No filter was applied on the publication date of the articles, and all results of each database were included up to July 2019. After removal of duplicates, all articles were evaluated through a screening of title and abstract by three independent reviewers. The same three reviewers performed an accurate reading of all full-text articles assessed for eligibility to this study and they performed a collection of data to minimize the risk of bias. In case of disagreement among investigators regarding the inclusion and exclusion criteria, the senior investigator made the final decision.
Inclusion criteria were:
-
i)
The studies concern wearable systems as a tool to assess upper limb kinematics;
-
ii)
The studies used sensors directly stuck on the human skin by means of adhesive, embedded within pockets, straps or integrated into fabrics;
-
iii)
Systems intended for motion recognition and rehabilitation;
-
iv)
Articles are written in English language;
-
v)
Papers are published in a peer-reviewed journal or presented in a conference;
Exclusion criteria were:
-
i)
Use of prosthetics, exoskeleton or robotic systems;
-
ii)
Wearable system not directly worn or tested on human;
-
iii)
The study concerns wearable systems for full-body motion tracking;
-
iv)
Shoulder joint is not included;
-
v)
Reviews, books.
Data extraction process
Data extraction was executed on 73 articles. Data was extracted on the base of the following checklist: authors, year and type of publication (i.e., conference or full-text); typology, number, brand and placement of the sensors used to measure or track the kinematic of the interested joint, wearability of the system, target parameters with regard to the shoulder; system used as gold standard to assess the wearable systems’ performance; tasks executed in the assessment protocol; characteristics of the participants involved in the study and aim of the study.
Results
The literature search returned 1811 results and additional 14 studies were identified through other sources. A total of 73 studies fulfilled the inclusion criteria (Fig. 1), of which 27% were published on conference proceedings and the remaining 73% on peer-reviewed journal.
Fig. 1.
PRISMA 2009 flow diagram
Three levels of analysis have been emphasized in this survey: A. application field and main aspects covered, B. the typology of sensors exploited to measure kinematic parameters, C. the placement of the single measurement units on the body segment of interest and how sensing modules are integrated into the wearable system from a wearability viewpoint.
Application field
Fifteen out of the 73 studies focused on evaluating upper limbs motion in case of musculoskeletal diseases (e.g., osteoarthritis, rotator cuff tear, frozen shoulder), 26 on neurological diseases and ap-plication in neurorehabilitation (e.g., stroke, multiple sclerosis), 15 on general rehabilitation aspects (e.g., home rehabilitation, physiotherapy monitoring) and 17 focusing on validation and development of systems and algorithm for monitoring shoulder kinematics. Tables 1, 2, 3 and 4 include, for each of the identified application fields, data listed in the previous data extraction process section.
Table 1.
Shoulder motion monitoring for application in patients with musculoskeletal disorders
| Reference, Year, Type of publication | Sensors, Brand | Placement and wearability | Target shoulder parameters, Performance | Gold standard | Task executed | Participants | Aim |
|---|---|---|---|---|---|---|---|
|
Coley 2007, [29] Full-Text |
IMU (n = 2), Analog Device (gyr: ADXRS 250, acc: ADXL 21 0) |
Bilateral: humeri (posteriorly, distally) Adhesive patch |
Sh ROM (HT joint angles), RMSE =5.81° Mean = 1.80° |
Zebris CMS-HS |
Sh FLX-EXT Sh AB-AD Sh IER |
HS (n = 10), 25.1 ± 4.1 Y P (n = 10), 7 RC, 3 OA, 4 F, 6 M, 62.4 ± 10.4 Y |
Find objective scores to assess shoulder function; to validate such scores comparing healthy and affected shoulders |
|
Coley 2008, [30] Full-Text |
IMU (n = 4), Analog Device (gyr: ADXRS 250, acc: ADXL 21 0) |
Bilateral: humeri (posteriorly, distally), thorax Adhesive patch |
Sh ROM (HT joint angles) |
– | Daily activities (8 h) |
HS (n = 35) 32 ± 8 Y |
Quantify usage of shoulder and the contribution of each shoulder in daily life activities |
|
Jolles 2011, [31] Full.Text |
IMU (n = 4), Analog Device (gyr: ADXRS 250, acc: ADXL 21 0) |
Bilateral: Humeri (distally, posteriorly), thorax (× 2) Adhesive patch |
Sh ROM (HT joint angles), r = 0.61–0.80 |
– | 7 activities of SST |
P (n = 34) 27 RC, 7 OA 25 M, 9 F 57.5 ± 9.9 CG (n = 31) 17 M, 14 F 33.3 ± 8.0 |
Validate clinically shoulder parameters in patients after surgery for GH OA and RC disease |
|
Duc 2013, [5] Full-Text |
IMU (n = 3), Analog Device (gyr: ADXRS 250, acc: ADXL 210) |
Bilateral: Humeri (distal, posterior), sternum Adhesive patch |
Sh ROM (HT joint angles), r2 = 0.13-0.52 (CMS) r2 = 0.06-0.30 (DASH) r2 = 0.03-0.31 (SST) |
– | Free movements, daily activities |
HS (n = 41) 34 ± 9 Y P (n = 21) 53 ± 9 Y RC (unilateral) |
Validate a method to detect movement of the humerus relative to the trunk and to provide outcomes parameters after shoulder surgery (frequency of arm movement and velocity) |
|
Körver 2014, [32] Full-Text |
IMU (n = 2), Inertia-Link-2400-SKI, MicroStrain |
Bilateral: Humerus (distal, posterior) Adhesive |
Sh ROM (HT joint angles), r = 0.39 (DASH) r = 0.32 (SST) |
– |
Hand to the back, Hand behind the head |
HS (n = 100) 37 M, 63 F 40.6 ± 15.7 Y P (n = 15) 5 M, 10 F 57.7 ± 10.4 Y, Subacromial impingement |
Investigate about the correlation between subjective (clinical scale) and objective (IMU) assessment of shoulder ROM during a long-term period of follow-up |
|
Van Den Noort 2014, [33] Full-Text |
M-IMU (n = 4), Xsens MTw |
Unilateral: Thorax, scapula, UA, FA Straps, skin tape |
Sh ROM (HT and ST joint angles) |
– | FLX (sagittal plane) and AB (frontal plane) with elb extended and thumb pointing up |
HS (n = 20) 3 M, 17 F 36 ± 11 Y |
Evaluate the intra- and inter-observer reliability and precision of 3D scapula kinematics |
|
Pichonnaz 2015, [34] Full-Text |
IMU (n = 3), Analog Device (acc: ADXL 210, gyr: ADXRS 250) |
Bilateral: Sternum, Humeri (posterior, distal) Skin tape |
Sh ROM (HT joint angles) |
– |
Free movements (7 h) |
HS (n = 41) 23 M, 18 F 34.1 ± 8.8 Y P (n = 21) 14 M, 7 F 53.3 ± 9 Y RC |
Explore dominant and non-dominant arm usage as an indicator of UL function after rotator cuff repair during the first year after surgery |
|
Roldán-Jiménez e Cuesta-Vargas 2015, [35] Full-Text |
M-IMU (n = 4), InterSense InertiaCube3 |
Unilateral: Sternum, humerus, scapula, FA (near wrist) adhesive tape and bandage |
Sh ROM (HT and ST joint angles) |
– | 180° sh AB and EXT with wri in neutral position and elb extended |
HS (n = 11) 8 M, 3 F 24.7 ± 4.2 Y |
Analyse UL angular mobility and linear acceleration in three anatomical axes |
|
Van Den Noort 2015, [36] Full-Text |
M-IMU (n = 4), Xsens MTw |
Unilateral: Thorax, Scapula, UA, FA Straps, skin tape |
Sh ROM (ST joint angles) |
– | Humeral FLX (sagittal plane) and AB (frontal plane) with elb extended and thumb pointing up |
P (n = 10) 8 M, 2 F 24–63 Y SD |
Evaluate the change in 3D scapular kinematics using a single and double anatomical calibration with a scapular locator versus standard calibration; evaluate difference in 3D scapular kinematics between static posture and dynamic humeral elevation |
|
Roldán-Jiménez e Cuesta-Vargas 2016, [38] Full-Text |
M-IMU (n = 3), InterSense, InertiaCube3 |
Unilateral: Humerus (middle third, slightly posterior), scapula, sternum Double-sided tape, elastic bandage |
Sh ROM (GH and ST joint angles) |
– |
Sh AB (frontal plane) Sh FLX (sagittal plane) Wri in neutral position and elb extended |
Young HS (n = 11), 18–35 Y 3 M, 8 F Adult HS (n = 14) > 40 Y 5 M, 9F |
Analyze differences in shoulder kinematics in terms of angular mobility and linear acceleration related to age |
|
Wang 2017, [26] Full-Text |
M-IMU (n = 3), Adafruit FLORA 9-DOF |
Unilateral: Shoulder (flat part of acromion), spine (C7-T1, T4-T5) Zipped vest, elastic strap with Velcro |
Sh ROM (ST joint angles), RMSE ~ 3.57° |
PST-55/110 series | 60 ° sh FLX with elb extended and thumb pointing up, place a cooking pot on a shelf, 40 ° sh EL in the scapular plane with elb extended and thumb pointing up, place a bottle of water on a shelf |
P with musculoskeletal shoulder pain (n = 8) 3 M, 5 F 50 ± 6.44Y Physiotherapist (n = 5) |
Evaluate usability of a smart garment-supported postural feedback scapular training in patients with musculoskeletal shoulder pain and in physiotherapists who take care patients with shoulder disorders |
|
Aslani 2018, [39] Full-Text |
M-IMU (n = 1), Bosh Sensortec BNO055 EMG, MyoWare Muscle Sensor |
Unilateral: UA, deltoid (2 surface electrodes on each deltoid section) Band |
Sh ROM (azimuthal and elevation angles) | – | Arm EL (medially, anteriorly, cranially, posteriorly, laterally) with elb fully extended |
HS (n = 6) 4 M, 2 F 27.3 ± 3.4Y P (n = 1), M Frozen Sh 42 Y |
Evaluate a measurements protocol to assess the performance of the shoulder by combining both ROM and electromyography measurements |
|
Carbonaro 2018, [40] Conference |
M-IMU (n = 3), Xsens MTw |
Unilateral: Sternum, FA (distal), scapula (similar to the configuration in [37]) Elastic bands |
Sh ROM (GH and ST joint angles) |
– |
Extra-rotation, Arm AB (with different load) |
HS (n = 5) | Test a digital application intended for tele-monitoring and tele-rehabilitation of the shoulder muscular-skeletal diseases |
|
Hurd 2018, [41] Full-Text |
Acc buil.in ActiGraph (n = 2), ActiGraph GT3XP-BLE |
Unilateral: Wrist, UA (mid-biceps level) Velcro strap |
Sh ROM | – | ADL |
P (n = 14) 7 M, 7 F 73 ± 6Y GH OA, RC disease |
Evaluate changes in pain, self-reported function and objective measurement of upper limb activity after RSA |
|
Langohr 2018, [6] Full-Text |
IMU (n = 5), YEI Technology |
Bilateral: Sternum, UA (lateral aspects of the midhumerus), FA (dorsal aspect of the wrist) Shirt |
Sh ROM (humeral elevation and plane of elevation angles) | – |
Daily activities (1 day, monitoring of 11 ± 3 h) |
P (n = 36) 73 ± 10 Y TSA, RTSA |
Determine the total daily shoulder motion of patients after TSA and RTSA, compare the motion of the arthroplasty shoulder with that of the contralateral asymptomatic joint and compare the daily motion of TSA and RTSA shoulders |
acc accelerometer, gyr gyroscope, magn magnetometer, IMU Inertial Measurement Unit, M-IMU Magneto and Inertial Measurement Unit, UA Upper Arm, FA Forearm, ROM Range of motion, HT humerothoracic, ST scapulothoracic, GH glenohumeral, Sh shoulder, wri wrist, elb elbow, FLX-EXT flexion-extension, AB-AD abduction-adduction, IER internal-external rotation, RMSE root mean square error, r = correlation, r2, coefficient of determination, HS Healthy subject, CG Control Group, P patient, M male, F female, RC Rotator Cuff, OA Osteoarthritis, Y Years old, SST Simple Shoulder test, DASH Disability of the Arm, Shoulder and Hand, CMS Constant Murley Score
Table 2.
Shoulder motion monitoring for application in patients with neurological disorders
| Reference, Year, Type of publication | Sensors, Brand | Placement and wearability | Target shoulder parameters, Performance | Gold standard | Task executed | Participants | Aim |
|---|---|---|---|---|---|---|---|
|
Bartalesi 2005, [8] Conference |
Strain sensor, WACKER Ltd. (ELASTOSIL LR 3162 A/B) |
Unilateral: Sensors’ segment series along right upper limb Shirt |
Sh ROM | – | – | HS | Wearable garment able to reconstruct shoulder, wrist and elbow movement to correct stroke patients’ rehabilitation exercises |
|
Hester 2006, [42] Conference |
Acc (n = 6) |
Unilateral: thumb, index, back of the hand, FA and UA (medially), thorax Adhesive |
Sh ROM | – | Reaching, prehension, manipulation | SP (n = 12) | Predict clinical scores of stroke patients’ motor abilities |
|
Zhou 2006, [43] Full-Text |
IMU (n = 2), Xsens MT9B |
Unilateral: Wrist (inwards), elbow (outwards) - |
Sh orientation and position | – |
FA FLX-EXT FA PR-SU, reach test |
HS (n = 1, M) | Propose a data fusion algorithm to locate the shoulder joint without drift |
|
Willmann 2007, [44] Conference |
M-IMU (n = 4), Philips |
Unilateral: Torso, shoulder, UA, FA Garment |
Sh ROM | – | – | HS | Provide a home system for upper limb rehabilitation in stroke patients |
|
Zhou 2008, [45] Full-Text |
M-IMU (n = 2), Xsens MT9B |
Unilateral: FA (distally, near the wrist center), UA (laterally, on the line between the lateral epicondyle and the acromion process) Velcro straps |
Sh orientation and position, RMSE = 2.5°-4.8° |
CODA |
reaching shrugging FA rotation |
HS (n = 4, M) 20–40 Y |
Validate data fusion algorithm |
|
Giorgino 2009, [46] Full-Text |
Strain sensor (n = 19), WACKER Ltd. (ELASTOSIL LR 3162 A/B) |
Unilateral: Sensors’ sensing segments distributed over the UA, FA, shoulder, elbow, wrist Shirt |
Sh ROM | – |
GH FLX (sagittal plane) Lateral AB ER |
HS (n = 1) | Describe a sensing garment for posture recognition in neurological rehabilitation |
|
Lee 2010, [47] Full-Text |
Acc (n = 2), Freescale MMA7261 QT |
Unilateral: UA, FA Velcro strap |
Sh ROM, Mean error~0°-3.5° |
gon | FLX-EXT (sagittal plane) | HS (n = 1) | Validate performance and accuracy of the system |
|
Chee Kian 2010, [48] Conference |
OLE (n = 1) Acc (n = 1) |
Unilateral: UA, elbow Adhesive patch |
Sh ROM | IGS-190 | Cyclic movements with arm exerciser | HS (n = 1) | Validate feasibility and performance (accuracy, repeatability) of the proposed sensing system designed to assist stroke patients in upper limb home rehabilitation |
|
Patel 2010, [49] Full-Text |
Acc (n = 6) |
Unilateral: thumb, index, back of the hand, FA, UA, trunk - |
Sh ROM | – | 8 activities of FAS |
SP (n = 24) 57.5 ± 11.8 Y |
Evaluate accuracy of FAS score obtained via analysis of the accelerometers data comparing such estimates with scores provided by an expert clinician using this scale |
|
Pérez 2010, [15] Full-Text |
M-IMU (n = 4), Xsens MTi |
Unilateral: UA (18 cm from acromion), FA (25 cm from epicondyle), hand (5.5 cm from distal radio-cubital joint), back (position is not relevant) Strap |
Sh ROM, r = 0.997 (for sh IR, after calibration) |
BTS SMART-D |
Sh FLX-EXT Sh horizontal AB-AD Sh IR Elb FLX Elb PR-SU Wri FLX-EXT Serving water from a jar |
HS (n = 1, F) | Validate the system |
|
Bento 2011, [50] Conference |
M-IMU (n = 4) |
Bilateral: Shoulder, UA, wrist (affected and unaffected side) Strap |
Sh orientation and position | – |
FA to Table FA to box Extend elbow Hand to table Hand to box |
SP (n = 5, M) 35–73 Y |
Preliminary validation of a system able to quantify upper limb motor function in patients after neurological trauma |
|
Nguyen 2011, [51] Full-Text |
OLE (n = 3) Acc (n = 3) |
Unilateral: Shoulder, elbow, wrist Clothing module fixed with Velcro straps |
Sh ROM, Test2: RMSE = 3.8° (gon), RMSE = 3.1° (SW) Test3: ICC = 0.975 (sh) |
Test2: gon, Shape- Wrap |
Test2: Bend and Flex elbow Test3: reaching task |
Test2: HS (n = 3, M); Test3: HS (n = 5) |
Validation of the proposed motion capture system |
|
Ding 2013, [52] Full-Text |
M-IMU (n = 2), Analog Device (acc: ADXL320), HoneyWell (magn: HMC1 053), Silicon Sensing System (gyr) |
Unilateral: UA (distal, near elbow), FA (distal, near wrist) Velcro strap |
Sh ROM | – | Replication of 10 reference arm posture |
HS (n = 5) 20–27 Y |
Check the feasibility of the proposed system which measures orientation and corrects upper limb posture using vibrotactile actuators |
|
Lee 2014, [53] Full-Text |
M-IMU (n = 7), Analog Device (acc:ADXL 345) InvenSense (gyr: ITG3200) Honeywell (magn: HMC5883L) |
Bilateral: Back, UA, FA and hand Strap |
Sh ROM, Test1: r = 0.963 Test2: RMSE< 5° |
Test1: gon Test2: VICON |
Sh FLX-EXT Sh AB Arm IER Elb FLX FA PR-SU Wri FLX-EXT Wri radial-ulnar deviation |
SP (n = 5) 2 M, 3 F Mean age: 68 Y |
Introduce a smartphone centric wireless wearable system able to automate joint ROM measurements and detect the type of activities in stroke patients |
|
Bai 2015, [54] Full-Text |
M-IMU (n = 4 or n = 1), Xsens MTx |
Unilateral Scapula, UA, FA, back of the hand or only on UA Velfoam, Velcro straps |
Sh ROM (upper limb segments orientation and position) |
Test1: gon Test2: gon, VICON |
Sh FLX-EXT Sh IER Sh AB-AD Elb FLX-EXT FA PR-SU Wri FLX-EXT Wri radial-ulnar deviation |
HS (n = 10) 8 M, 2 F 20–38 Y P (n = 1), F 41 Y |
Evaluate a four-sensor system and a one-sensor system, investigate whether these systems are able to obtain quantitative motion information from patients’ assessment during neurorehabilitation |
|
Ertzgaard 2016, [55] Full-Text |
IMU (n = 5), Analog Device, Adis 16,350 |
Bilateral: Back (upper body), UA and FA Strap |
Sh ROM (HT joint angles), ICC = 0.768–0.985 |
Coda | Movements that mimic activities of daily life |
HS (n = 10) 2 M, 8 F 34.3 ± 13.1Y SP (n = 1), F, 43 Y |
Validation study to characterize elbow and shoulder motion during functional task using a modified Exposure Variation Analysis (EVA) |
|
Lorussi 2016, [56] Full-Text |
M-IMU (n = 2), Xsens MTw Strain sensor (n = 1), Smartex |
Unilateral: M-IMU sensors on sternum and UA Textile-based strain sensor on the back (from the spine to scapula) Shirt |
Sh ROM (HT joint angle and scapular translation) |
BTS SMART-DX |
UA FLX (sagittal plane) UA AB (frontal plane) |
HS (n = 5) | Validate sensors and data fusion algorithm to reconstruct scapular-humeral rhythm |
|
Mazamenos 2016, [57] Full-Text |
M-IMU (n = 2), Shimmer2r |
Unilateral: UA (distal, near elbow), FA (distal, near wrist) Straps |
Sh ROM (segments’ orientation and position) | – |
EXP1: Reach and retrieve, lift object to mouth, rotate an object EXP2: preparing a cup of tea |
HS (n = 18) M, F 25–50 Y SP (n = 4) M, F 45–73 Y |
Evaluate the performance and robustness of a detection and discrimination algorithm of arm movements |
|
Jiang 2017, [58] Conference |
Acc (n = 4), Analog Device ADXL362 EMG (n = 4), Analog Device AD8232 Temperature (n = 1) |
Unilateral: along upper limb Shirt |
Sh ROM | – | 4 typical joint actions performed in clinical assessment | HS (n = 1), M | Introduce an IoT-Bases upper limb rehabilitation assessment system for stroke patients |
|
Li 2017, [59] Full-Text |
IMU (n = 2), InvenSense, MPU-9250 EMG (n = 10), American Imex, Dermatrode |
Unilateral: IMU: UA, wrist EMG: FA (n = 8), UA (n = 2) Stretchable belt |
Sh ROM | – |
11 tasks including: Sh FLX, Sh AB Wri FLX-EXT, Fetch and hold a ball or a cylindric roll, finger to nose, touch the back of the sh, FA PR-SU |
HS (n = 16) 10 M, 6 F 36.25 ± 15.19Y SP (n = 18) 11 M, 7 F 55.28 ± 12.25 Y |
Propose data fusion from IMU and surface EMG for quantitative motor function evaluation in stroke subjects |
|
Newman 2017, [60] Full-Text |
IMU (n = 3), Gait Up SA Physilog4 |
Bilateral: sternum, UA (posterior) Velcro straps, adhesive patch |
Sh ROM (HT joint angles) |
– | Reaching movements (lateral, forward, upward) |
Children (n = 30) 10.6 ± 3.4 Y 17 boys, 13 girls |
Test an IMU-based system to measure upper limb function in children with hemiparesis and its correlation with clinical scores |
|
Yang e Tan 2017, [61] Conference |
M-IMU (n = 4), APDM Opal |
Unilateral: Waist, thorax, UA (distal, near elbow), FA (distal, near elbow) Straps |
Sh ROM (HT joint angles) |
Optitrack | Movements related with waist joint, sh joint and elb joints to achieve joint rotation | HS (n = 2) | Validate the proposed motion tracking system |
|
Daunoraviciene 2018, [62] Full-Text |
M-IMU (n = 6), Shimmer |
Bilateral: UA, FA, hand (on centres of mass) Strap |
Sh ROM | – | FNT test (Sh EXT, sh AB, elb FLX, hand SU) |
CG (n = 24) 7 M 31.14 ± 5.67 17 F 28 ± 3.97 MS-P (n = 34) 13 M 36.46 ± 13.07 21 F 42.19 ± 12.55 |
Test a M-IMU based system to identify quantitative parameters for evaluation of UL disability and relate it to clinical scores |
|
Jung 2018, [63] Conference |
M-IMU (n = 5), Xsens MTw Awinda |
Bilateral: UA and FA, trunk Velcro straps |
Sh ROM (HT join angles), RMSE = 0.32 for the estimation of movements qualities using data of the entire duration of movements |
Quality of movements’ label provided by the therapist | Reaching exercise |
SP (n = 5), F 66.6 ± 15.9 Y |
Evaluate movements quality regarding compensation and inter-joint coordination; exploiting a supervised machine learning approach, validate the hypothesis that therapists’ evaluation can be made considering only the beginning movement data |
|
Lin 2018, [64] Full-Text |
IMU (n = 2) |
Unilateral: UA (distal, near elbow), FA (dorsal aspect of the wrist) Strap |
Sh ROM | – |
Sh FLX-EXT Sh AB Sh ER Elb FLX FA PR-SU |
SP (n = 18): n = 9, control group (62.6 ± 7.1) n = 9, device group (52.2 ± 10.2 Y) |
Evaluate the feasibility and efficacy of an IMU-based system for upper limb rehabilitation in stroke patients and compare the intervention effects with those in a control group |
|
Repnik 2018, [7] Full-Text |
M-IMU (n = 7), Myo armband, n = 2_ with n = 8 EMGs built-in, Thalamic labs |
Bilateral: -M-IMU: Back of the hand, wrist, UA (distal, near elbow), sternum -MYO: FA (in the proximity of elbow joint) Straps, armband |
Sh ROM (HT joint angles) |
– | ARAT tasks: 19 movements divided in 4 subtests (grasp, grip, pinch, gross arm movement) |
SP (n = 28) 18 M, 10 F 57 ± 9.1 Y HS (n = 12) 9 M, 3 F 36 ± 8 Y |
Quantify UL and trunk movement in stroke patients |
acc accelerometer, gyr gyroscope, magn magnetometer, OLE Optical Linear Encoder, IMU Inertial Measurement Unit, M-IMU Magneto and Inertial Measurement Unit, UA Upper Arm, FA Forearm, ROM Range of motion, HT humerothoracic, GH glenohumeral, Sh shoulder, wri wrist, elb elbow, FLX-EXT flexion-extension, PR-SU pronation-supination, AB-AD abduction-adduction, IER internal-external rotation, RMSE root mean square error, r = correlation, ICC Intraclass Correlation Coefficients, gon goniometer, HS Healthy subject, CG control group, SP Stroke Patient, MS-P Multiple Sclerosis Patient, P patient, M male, F female, Y Years old, FAS Functional Ability Scale, ARAT Action research arm test
Table 3.
Shoulder motion monitoring for application in patients undergoing rehabilitation
| Reference, Year, Type of publication | Sensors, Brand | Placement and wearability | Target shoulder parameters, Performance | Gold standard | Task executed | Participants | Aim |
|---|---|---|---|---|---|---|---|
|
Cutti 2008, [37] Full-Text |
M-IMU (n = 4), Xsens MT9B |
Unilateral: Thorax (flat portion of the sternum), Scapula (central third, aligned with the cranial edge of the scapular spine), humerus (central third, slightly posterior), FA (distal) Double-sided tape, elastic cuff |
Sh ROM (HT and ST joint angles) RMSE = 0.2°-3.2° |
VICON |
Exp 1: elb FLX-EXT, PR-SU sh FLX-EXT, IER, sh EL-DE and P-R Exp 2: tasks in Exp1 + sh IER (arm abducted 90°), sh AB-AD (frontal plane), HTN (sagittal and frontal plane) |
HS (n = 1, M) | Develop a protocol to measure humerothoracic, scapulothoracic and elbow kinematics |
|
Parel 2012, [65] Full-Text |
M-IMU (n = 3), Xsens MTx |
Unilateral: thorax, scapula, humerus Elastic cuff, adhesive |
Sh ROM (HT and ST joint angles) |
– | Humerus FLX-EXT (sagittal plane) and AB-AD (scapular plane) |
HS (n = 20) 7F, 13 M 28.3 ± 5.5 Y P (n = 20) 8F, 12 M 43.9 ± 19.9 Y |
Assess the inta- and inter-operator agreement of ISEO protocol in measuring scapulohumeral rhythm |
|
Daponte 2013a, [66] Conference |
M-IMU (n = 2), Zolertia Z1 |
Unilateral: UA, FA Brace |
Sh ROM | – |
Sh AB-AD Elb FLX |
HS (n = 1) | Discuss design and implementation of a home rehabilitation system |
|
Daponte 2013b, [67] Conference |
M-IMU (n = 2), Zolertia Z1 |
Unilateral: UA, FA Brace |
Sh ROM, Test1: max gap = 6.5° (roll) 5.2° (pitch) 11.6° (yaw) |
Test 1: Tecno Body MJS Test 2: BTS |
Test 1: shoulder IR, EL-DE and horizontal FLX-EXT Test 2: elbow FLX-EXT (along sagittal and horizontal plane) |
HS (n = 1, M) | Validation of a home rehabilitation system |
|
Pan 2013, [68] Full-Text |
Acc (n = 2), LIS3LV02DQ Acc built-in a Smartphone (n = 1) |
Unilateral: -acc: UA, thorax -Smartphone: wrist Strap, Armband |
Sh ROM (HT joint angles) |
– |
Touch ear Use fingers to climb wall Pendulum clockwise and counter clockwise Active-assisted stretch fore and side, raises hand from back |
HS (n = 10) 3 M, 7 F 20-25Y P (n = 14) 5 M, 9 F 44–67 Y |
Describe design and implementation of a shoulder joint home-based rehabilitation monitoring system |
|
Thiemjarus 2013, [69] Conference |
Acc (n = 1), Analog Device (acc: ADXL330) Magn (n = 1), Honeywell (magn: HMC5843) |
Unilateral: UA (proximal) or wrist, left or right Strap |
Sh ROM, RMSE = 0.86°-5.05° |
– | Sh FLX-EXT, AB-AD, horizontal AB-AD, IER |
HS, (n = 23) 20–55 Y |
Evaluate the effect of sensor placement on the estimation accuracy of shoulder ROM |
|
Rawashdeh 2015, [70] Conference |
M-IMU (n = 1), InvenSense (gyr: ITG-3200) Analog Device (acc: ADXL 345) Honeywell (magn: HMC5883L) |
Unilateral: UA (lateral) Strap |
Sh ROM | – |
7 sh rehabilitation exercises 2 sports activities |
HS (n = 11) | Describe a detection and classification method of shoulder motion gestures that can be used to prevent shoulder injury |
|
Álvarez 2016, [71] Full-Text |
M-IMU (n = 4), Xsens MTx |
Unilateral: Back of the hand, FA (near wrist), UA (near elbow), back Wristband, Velcro strap, elastic band |
Sh ROM, Lab test: mean error = 0.06° (FLX) 1.05° (lateral deviation) |
Lab test: robotic wrist |
Test1: Mounting of a shock dumper system Test2: holding a tablet for long periods Test3: elbow FLX-EXT |
Test1: Mechanical worker (n = 1) Test2: worker of a commercial centre (n = 1) Test3: patient (n = 1) |
Demonstrate the feasibility of an IMU-based system to measure upper limb joint angles in occupational health |
|
Lee 2016, [72] Conference |
Strain sensor (n = 2), MWCNT, Hyosung: multi-walled carbon nanotubes, EcoFlex0030, Smooth-On: silicon rubber |
Unilateral: Shoulder Skin adhesive |
Sh ROM, RMSE<10° | OptiTrack |
Sh FLX-EXT Sh AB-AD |
HS (n = 1) | Validate sensors and calibration method estimating two shoulder joint angles |
|
Tran e Vajerano 2016, [73] Conference |
M-IMU (n = 2), Shimmer2r |
Unilateral: UA (distal, near elbow), FA (distal, near wrist) Straps |
Sh ROM (HT joint angles) |
– | Periodic arm movements | HS (n = 1) | Validate an algorithm to predict the received signal strength indicator (RSSI) and the future joint-angle values of the user |
|
Rawashdeh 2016, [74] Full-Text |
M-IMU (n = 1), InvenSense (gyr: ITG-3200) Analog Device (acc: ADXL 345) Honeywell (magn: HMC5883L) |
Unilateral: UA (central third) Straps |
Sh ROM (HT motion) |
Visual observation | 7 sh rehabilitation exercises, baseball throws, volley serves |
HS (n = 11) 25 ± 7 Y |
Validate a detection and classification algorithm of upper limb movements |
|
Wu 2016, [75] Full-Text |
M-IMU (n = 3), Bluetooth 3-Space Sensor, YEI |
Unilateral: FA (near wrist), UA (near elbow), thorax (shifted to the right) Strap, bandage |
Sh ROM (HT joint angles) |
– | 12 gestures common in daily life: 3 static and 9 dynamic |
HS (n = 10) 9 M, 1 F 22–24 Y |
Evaluate accuracy, recall and precision of a gesture recognition system |
|
Burns 2018, [27] Full-Text |
Acc and gyr built-in a smartwatch (n = 1), Apple Watch (Series 2 &3) |
Unilateral: Wrist Wristband |
Sh ROM | – |
Pendulum AB Forward EL IR ER Trapezius EXT Upright row |
HS (n = 20) 14 M, 6 F 19–56 Y |
Evaluate performance of a commercial smartwatch to perform home shoulder physiotherapy monitoring |
|
Esfahani e Nussbaum 2018, [11] Full-Text |
Textile sensors (printed) n = 11 |
Bilateral: Shoulder (n = 6), low back (n = 5) Undershirt |
Sh ROM, mean error = 9.6° for sh angle estimation | M-IMU (Xsens MTw Awinda) |
Sh AB Sh FLX-EXT Sh IER Left/right side bending Trunk FLX-EXT Trunk rot left/right |
HS (n = 16), 10 M, 6 F 21.9 ± 3.3 |
Describe a smart undershirt and evaluate its accuracy in task classification and planar angle measures in the shoulder joints and low back |
|
Ramkumar 2018, [76] Full-Text |
Acc,gyr and magn built-in a smartphone, Apple iPhone |
Unilateral: UA, FA Armband |
Sh ROM <5° | gon |
AB (coronal plane) forward FLX (sagittal plane) IER (elbow fixed to the body flexed to 90°) |
HS (n = 10) 5 M, 5 F Mean 27 Y |
Validate a motion-based machine learning software development kit for shoulder ROM |
acc accelerometer, gyr gyroscope, magn magnetometer, IMU Inertial Measurement Unit, M-IMU Magneto and Inertial Measurement Unit, UA Upper Arm, FA Forearm, ROM Range of motion, HT humerothoracic, ST scapulothoracic, Sh shoulder, elb elbow, FLX-EXT flexion-extension, AB-AD abduction-adduction, IER internal-external rotation, P-R protraction-retraction, RMSE root mean square error, HS Healthy subject, P patient, M male, F female, Y Years old
Table 4.
Studies focused on validation/development of systems/algorithms for monitoring shoulder motion
| Reference, Year, Type of publication | Sensors, Brand | Placement and wearability | Target shoulder parameters, Performance | Gold standard | Task executed | Participants | Aim |
|---|---|---|---|---|---|---|---|
|
Jung 2010, [77] Conference |
IMU (n = 6), ADXL 345 (acc) LPY51 50 AL (gyr) HMC5843 (magn) |
Bilateral: UA and FA (distal third), thorax and pelvis Strap |
Sh orientation and position | HDRT system |
Arms above head Bend arms Bend waist |
HS (n = 1) | Validate the motion tracking algorithm |
|
El-Gohary 2011, [78] Conference |
IMU (n = 2), APDM Opal |
Unilateral: FA (near wrist), UA (distal third) Strap |
Sh ROM, r = 0.91–0.97 |
Eagle Analog System |
Sh FLX-EXT Sh AB-AD Elb FLX-EXT Elb PR-SU |
HS (n = 1) | Validate data fusion algorithm |
|
Zhang 2011, [79] Full-Text |
M-IMU (n = 3), Xsens MTx |
Unilateral: UA (laterally, above the elbow), FA (lateral and flat side of the FA near the wrist), sternum Strap, clothing |
Sh ROM, RMSE = 2.4° (sh FLX-EXT) RMSE = 0.9° (sh AB-AD) RMSE = 2.9° (sh IER) |
BTS SMART-D | Free movements | HS (n = 4) | Validate sensor fusion algorithm |
|
El-Gohary 2012, [80] Full-Text |
IMU (n = 2), APDM Opal |
Unilateral: UA (middle third, slightly posterior), FA (distal, near wrist) Strap band |
Sh ROM, RMSE = 5.5° (sh FLX-EXT) RMSE = 4.4° (sh AB-AD) |
VICON |
Sh FLX-EXT Sh AB-AD Elb FLX-EXT FA PR-SU Touching nose Reaching for a doorknob |
HS (n = 8) | Validate data fusion algorithm |
|
Lee e Low 2012, [81] Full-Text |
Acc (n = 2), Freescale MMA7361 L |
Unilateral: UA (near elbow), FA (near wrist) - |
Sh ROM, RMSE = 2.12° (sh FLX-EXT) RMSE = 3.68° (sh rotation) |
IMU (Xsens MTx) |
UA FLX-EXT and medial/lateral rotation FA FLX-EXT and PR-SU (sagittal plane) |
HS (n = 1) | Validate the feasibility of the proposed algorithm |
|
Hsu 2013, [82] Conference |
M-IMU (n = 2), LSM303DLH (acc, magn) L3G4200D (gyr) |
Unilateral: UA, FA Velcro strap |
Sh ROM, RMSE = 1.34°-5.08° |
Xsens MTw, (n = 2) | Sh FLX, AB, EXT, ER and IR |
HS (n = 10) 8 M, 2 F 23.3 ± 1.33 Y |
Validate data fusion algorithm |
|
Lambrecht e Kirsch 2014, [16] Full-Text |
M-IMU (n = 4), InvenSense MPU-9150 chip |
Unilateral: Sternum, UA, FA and hand - |
Sh ROM, RMSE = 4.9° (sh azimuth) RMSE = 1.2° (sh elevation) RMSE = 2.9° (sh IR) |
Optotrack | Reaching movements | HS (n = 1) | Validate sensors’ accuracy and data fusion algorithm |
|
Ricci 2014, [83] Full-Text |
M-IMU (n = 5), APDM Opal |
Bilateral: Thorax, UA (latero-distally) and FA (near wrist) Velcro strap |
Sh ROM (HT joint angles) |
– |
UA FLX-EXT UA AB-AD FA PR-SU FA FLX-EXT Thorax rotation Thorax FLX-EXT |
Children (n = 40) 6.9 ± 0.65 Y |
Develop a calibration protocol for Thorax and upper limb motion capture |
|
Roldan-Jimenez 2015, [84] Full-Text |
Inertial sensors built-in a Smartphone (n = 1), LG Electronics INC, iPhone4 |
Unilateral: UA Neoprene arm belt |
Sh ROM | – | sh AB, EXT with wrist in neutral position and elb extended |
HS (n = 10) 7 M, 3 F 24.2 ± 4.04 Y |
Study humerus kinematics through six physical properties that correspond to angular mobility and acceleration in the three axes of space |
|
Fantozzi 2016, [17] Full-Text |
M-IMU (n = 7), APDM Opal |
Bilateral: Sternum, UA, FA, back of the hand Velcro strap |
Sh ROM (HT joint angles), RMSE <10° (sh FLX-EXT, AB-AD, IER) |
BTS SMART-DX | Simulated front-crawl and breaststroke swimming |
HS (n = 8), M 26.1 ± 3.4 Y |
Validate a protocol to assess the 3D joint kinematics of the upper limb during swimming |
|
Meng 2016, [85] Full-Text |
M-IMU (n = 2), Shimmer2r |
Unilateral: UA (distal, near elbow), FA (distal, near wrist) Straps |
Sh ROM, Test2: RMSE = from 2.20° to 0.87° |
VICON |
Sh FLX-EXT Sh AB-AD Sh IER Elb FLX-EXT Elb PR-SU |
Test1: HS (n = 15), M, 19–23 Y Test2: HS (n = 5) |
Validate an algorithm to improve accuracy on measurements of arm joint angles considering the properties of human tissue |
|
Crabolu 2017, [86] Full-Text |
M-IMU (n = 3), Xsens, MTw2 Awinda |
Unilateral: UA, scapula, Sternum Velcro strap, double-sided tape, elastic band |
GH joint center | MRI acquisition |
Cross and star motions (2 joint velocities, 2 range of motions) |
HS (n = 5) 3 M, 2 F 36 ± 4 Y |
Evaluate accuracy and precision of the GHJC estimation |
|
Kim 2017, [87] Conference |
MYO armband (n = 1): contains 8 EMG and 1 IMU, Thalamic Labs, MYO armband |
Unilateral: UA (near elbow) Armband |
Sh ROM | – |
Elb FLX (0°,45°,90°) with sh in neutral position, elb FLX (0°,45°,90°) with sh FLX 90° (sagittal plane) |
HS (n = 1) | Introduce an algorithm for upper arm and forearm motion estimation using MYO armband |
|
Morrow 2017, [88] Full-Text |
M-IMU (n = 6), APDM Opal |
Bilateral: FA and UA (lateral), head, sternum Velcro straps |
Sh ROM (HT joint angles), RMSE = 6.8° ± 2.7° (sh elevation) |
Raptor 12 Digital Real Time Motion Capture System |
Peg transfer (to mimic minimally invasive laparoscopy) |
Surgeon HS (n = 6) 3 M, 3 F 45 ± 7 Y |
Validate a M-IMU based protocol to measure shoulder EL, elbow FLX, trunk FLX-EXT and neck FLX-EXT kinematics |
|
Rose 2017, [89] Full-Text |
IMU (n = 6), APDM Opal |
Bilateral: UA (lateral), FA (dorsal), sternum, lumbar spine Straps |
Sh ROM (HT joint angles) |
– | Diagnostic arthroscopy simulation |
Surgeon HS (n = 14) |
Develop an IMU-based system to assess the performance of orthopaedic residents with different arthroscopic experiences |
|
Tian 2017, [90] Conference |
M-IMU (n = 2), Acc: LIS3LV02D, Magn: HMC5843, Gyr: ITG3200 |
Unilateral: UA, FA Straps |
Sh ROM | VICON | Sh FLX and elb FLX (sagittal plane) | HS (n = 1) | Validate data fusion algorithm |
|
Pathirana 2018, [91] Full-Text |
M-IMU (n = 1) |
Unilateral: Wrist Strap |
Sh ROM |
VICON, Kinect |
Forward FLX-EXT AB-AD Backward FLX-EXT Horizontal FLX-EXT |
HS (n = 14) 10 M, 4 F |
Validate accuracy and robustness of data fusion algorithm using a single sensor to measure shoulder joint angles |
acc accelerometer, gyr gyroscope, magn magnetometer, IMU Inertial Measurement Unit, M-IMU Magneto and Inertial Measurement Unit, UA Upper Arm, FA Forearm, ROM Range of motion, HT humerothoracic, GH glenohumeral, Sh shoulder, elb elbow, FLX-EXT flexion-extension, PR-SU pronation-supination, AB-AD abduction-adduction, IER internal-external rotation, RMSE root mean square error, r = correlation, HS Healthy subject, M male, F female, Y Years old
Sensing technology
Some studies combined different sensors in their measurements system. The most used sensors are accelerometers, gyroscopes and magnetometers, a combination of them (n = 55) or with other sensors (n = 8), or built-in into other devices (e.g., smartphones, smartwatch) (n = 6); additional studies (n = 4) utilized strain sensors for motion analysis.
B.1 wearable systems based on inertial sensors and magnetometers
An IMU allows estimating both translational and rotational movements. Such sensors comprise gyroscopes that measure angular velocity and accelerometers that measure proper acceleration, i.e. gravitational force (static) and force due to movements (dynamic) [92]. The main limitation of the gyroscopes is the issue bias due to drift. Gyroscopes do not have an external reference, as opposed to accelerometers that use gravity vector as reference; in the orientation estimation, gyroscopes suffer of drift during the integration procedures. To compensate such issue, these sensors are combined with magnetometers that measure magnetic field and use the Earth’s magnetic field as reference. The main limitation of magnetometers is the interference due to the presence of ferromagnetic materials in the surrounding environment [92]. We refer to these hybrid sensors as M-IMU (magnetic and inertial measurement unit). By integrating the information derived from each sensor (i.e., acceleration, angular velocity and magnetic field) through sensor-fusion algorithms, M-IMUs provide an accurate estimation of the 3D-position and 3D-orientation of a rigid body. The upper limb can be modelled as a kinematic chain constituted by a series of rigid segments, i.e., thorax, upper arm, forearm and hand, linked to each other by joints that allow relative motion among consecutive links [17]. In the kinematic chain, the shoulder joint consists of three degrees of freedom (DOFs) correspondent to abduction-adduction (AB-AD), internal-external rotation (IER), and flexion-extension (FLX-EXT) [15, 54, 57, 71, 79]. Shoulder rotations can be described using Euler angles that identify the anatomical DOFs with the roll-pitch-yaw angles [17, 33, 37, 88]. Sensor-fusion algorithms can exploit two main approaches, deterministic or stochastic. The deterministic approach includes the complementary filter that merges a high pass filter for gyroscope data (to avoid drift) and a low pass filter for accelerometer and magnetometer data [64, 82, 90, 92]. The stochastic approach includes the Kalman Filter and its more sophisticated versions [7, 55, 66, 67, 78–80, 91, 92]. The Kalman filter (KF) is the most used algorithm to process M-IMU and IMU data due to its accuracy and reliability [15, 38, 54, 75, 83, 93].
Wearable systems based on IMU or M-IMU include a variable number of sensor nodes that, properly distributed on each body segment of interest, provide kinematic parameters such as joint ROM, position, orientation, and velocity. Fifty-one out of the included studies used exclusively IMUs (n = 15) or M-IMUs (n = 36). Systems performances were analyzed in terms of the agreement between results obtained from the M-IMU or IMU-based systems and those collected by a gold standard system. Several types of systems were used as gold standard, such as ultrasound-based system (e.g., Zebris CMS-HS [29]), diagnostic imaging (e.g., Magnetic Resonance [86]), optical-based systems (e.g., VICON [37, 53, 54, 80, 85, 90, 91], BTS Bioengineering [15, 17, 56, 67, 79], Eagle Analogue System [78], Optotrack [16], Optitrack [61], CODA [45, 55]), goniometer [53, 54]. Results from an inertial system were benchmarked against an ultrasound-based reference system, showing a root mean square error (RMSE) of 5.81° and a mean error of 1.80° in the estimation of shoulder angles of FLX-EXT, AB-AD and IER evaluated in the sagittal, frontal and transversal planes, respectively [29]. Accuracy of a protocol based on commercial inertial sensors (MT9B, Xsens) was tested and compared to a VICON system to measure humerothoracic, scapulothoracic joint angles and elbow kinematics [37]. Results demonstrated high accuracy in the estimation of upper limb kinematics with an RMSE lower than 3.2° for 97% of data pairs. A BTS reference system was used to validate accuracy of a wearable system comprised of commercial sensors (Xsens) and results showed a mean error difference of 13.82° for FLX-EXT, 7.44° for AB-AD, 28.88° for IR [15]. In a protocol-validation study, commercial Opal sensors were compared to a BTS system to assess upper limb joint kinematics during simulated swimming movements. Data showed a median RMSE always better than 10° considering movements of AB-AD, IER and FLX-EXT in front-crawl and breaststroke [17]. Opal wearable sensors were compared to optical motion capture systems to estimate shoulder and elbow angles [78, 80]. Planar shoulder FLX-EXT and AB-AD were performed showing an RMSE of 5.5° and 4.4°, respectively [80]; a good correlation between the measurements performed on shoulder motion with the two systems was also found in [78] (no data regarding measurements error were proposed).
Some studies (n = 11) compared data obtained from wearable sensors, custom or commercial, with a gold standard to validate their own sensors data fusion algorithm (for more details see Table 4). Two different algorithms were compared to a customized KF [79]. Comparing the results derived from the BTS system and the inertial-based system (Xsens), the proposed algorithm showed a smaller error than the other two methods for computing shoulder FLX-EXT (RMSE = 2.4°), AB-AD (RMSE = 0.9°), IER (RMSE = 2.9°) [79]. The addition of the magnetometer-based heading correction in the sensor data fusion algorithm was investigated to test the accuracy of an inertial-based motion tracking system using the Optotrak Certus (Northern Digital Inc., Waterloo, ON, Canada) as reference. Results showed a RMSE of 4.9°, 1.2° and 2.9° for shoulder azimuth, elevation and internal rotation, respectively [16].
Four studies used only accelerometers [42, 47, 49, 81]. Systems performance analysis in measurement of arm motion, showed a RMSE lower than 3.5° and 3.68° for shoulder ROM when results from the accelerometers-based systems were benchmarked against a goniometer and commercial M-IMUs, respectively [47, 81]. Evaluation of upper limbs’ physical activity was performed recording data of accelerometers built-in wearable device as ActiGraph (Pensacola, Florida, Model GT3XP-BTLE) to obtain objective outcomes in patients after reverse shoulder arthroplasty [41].
Shoulder ROM has been also estimated by means of a single sensor node which integrated an accelerometer and a magnetometer [69]. Sensor fusion algorithms of accelerometers and magnetometers data provide accurate orientation estimation in static or semi static condition, e.g., in a rehabilitation session in which patients perform slow movements [81]. M-IMUs comprised of a 3D accelerometer, 3D gyroscope and 3D magnetometer are the most appropriate choice for motion tracking either in static that in dynamic condition.
Two accelerometer-based sensors were combined with those built-in a smartphone to realize a smart rehabilitation platform for shoulder home-rehabilitation [68]. Mobile phone or a smartwatch, with their built-in inertial sensor units, were used as mobile monitoring devices [27, 76, 84]. These results give proof of the growing trend in the application of commercial devices in clinical setting for rehabilitation purposes. Data has been processed using machine learning algorithms to extract salient features and for gesture recognition related to shoulder motion. In these techniques, the main steps are the data collection, followed by segmentation process, feature extraction and classification [27, 49]. For instance, the identification of different types of RC physiotherapy exercises has been performed processing data from inertial sensors built-in a wrist-worn smartwatch [27]. Data from inertial sensors built-in a smartphone were benchmarked against a manual goniometer. Angular differences between a machine learning-based application and goniometer measurements resulted less than 5° for all shoulder ROM (i.e., AD, forward FLX, IR, ER) [76].
Two studies combined accelerometer(s) with Optical Linear Encoder (OLE) [68, 84]. An OLE-based system acts as a goniometer providing measures of joint angles. Despite of the simplicity and low cost of the proposed systems, differences in shoulder ROM estimation resulted not negligible when data collected by the wearable systems were compared against an inertial-based motion capture (i.e., IGS-190 [54]) and a fiber optics-based system (i.e., ShapeWrap [71]).
Three studies included EMG sensors in their assessment tool in combination with accelerometers [58], IMUs [59] and M-IMU [39]. EMG sensors placed on the biceps, triceps [59] and deltoid muscles [39] provide additional information about upper limb motor function and shoulder assessment, evaluating muscles activity. Quantification of upper limb motion was executed through a wearable device, MYO armband by Thalamic labs, that combines EMG sensors to record electrical impulses of the muscles [7, 87].
B.2 wearable systems based on strain sensors
Four studies used smart-textiles instrumented by strain sensors with piezoresistive properties to estimate kinematic parameters and to perform motion analysis [8, 11, 46, 56]. Such sensing elements are stretched or compressed during movements of the examined body segments, with consequent variation of their electrical resistance [94, 95]. Using a M-IMU system as reference, accuracy evaluation of a smart-textile with printed strain sensors showed a mean error of 9.6° in planar motions measurements of shoulder joint [11]. Shoulder kinematics was assessed combining a strain sensor for scapular sliding detection with two M-IMUs for HT orientation measure [56].
Piezoresistive strain sensors directly adhered to the skin were used to estimate shoulder ROM; the comparison between reference data from an optical-based system (i.e., Optitrack) and strain sensors showed a RMSE less than 10° in shoulder FLX-EXT and AB-AD estimation [72].
Sensors placement and wearability
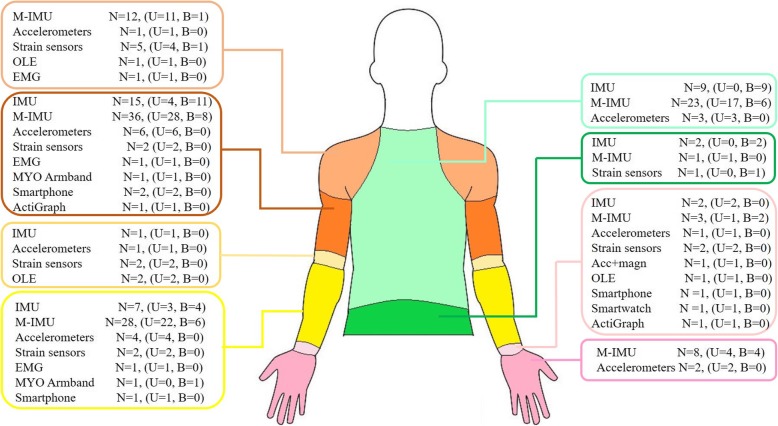
Placement of the sensing technology on the body landmarks has shown a heterogeneous distribution linked to the different nature of the employed technology and to the purpose for which monitoring system was designed. With respect to the monitored upper limb, 53 out of the 73 studies included in this review showed a unilateral distribution of the sensing elements while the remaining studies utilized a bilateral placement. Several configurations using different number of sensors and placements have been investigated as reported in detail in each table and Fig. 2.
Fig. 2.
Placement of sensing units (NOTE One study [90] is not included because the specific position of each sensor nodes is not so clear. Legend: N = number of studies, U = Unilateral, B = Bilateral)
Regarding the wearability, we classified the systems in terms of how the sensors were fixed to the human body: i) by adhesive patch, ii) by means of straps or embedded within pocket, iii) the sensing element is physically integrated into the fabric. Four studies did not specify the method of attachment, 12 studies have stuck sensors directly on human skin by means of adhesive patch, 52 studies have attached sensors through straps or embedding them in modular clothing, and 5 studies have integrated sensors directly into garments. For more details refers to Tables 1, 2, 3 and 4.
Discussion
This paper summarizes the main features of wearable systems that have been employed in clinical setting and research field to evaluate upper limb functional performance and particularly for shoulder ROM assessment. Shoulder complex is characterized by the greatest mobility among all human joints and, due to its complexity, reviewed articles evidenced heterogeneity on the more suitable protocol for capturing joint ROM [96].
Wearable technology
Although 73% of the reviewed papers use commercial products for tracking joint angles, many of these personalize the positioning of the sensors, the calibration methodology and the algorithms used to process the recorded data. This customization makes strenuous a direct comparison among protocols, especially if sensing units of different nature (e.g., M-IMU vs. strain sensors) are used to measure the same kinematic parameters, leaving still open the issue of the protocols’ definition with general validity.
About studies using inertial-based motion tracking systems, most in this summary (88%), calibration procedures before data acquisition and data processing represent a relevant issue about accuracy and reliability of the system. Typically, the M-IMUs are attached on the segment of interest to estimate its orientation, so the calibration is necessary to relate sensors’ measurements to movements of the tracked body segment. Sometimes the manufacturer suggests how to perform calibration, e.g., positioning sensors on a flat surface [15, 35] to align coordinate system or assuming static anatomical position [65], as N-pose [79], to compute orientation differences between segments and sensors coordinates in order to obtain sensor-to-segment alignment [56]. Dynamic or functional anatomical calibration has also been performed in some studies, but the sequence of movements executed varied among these [17, 33, 55, 83]. One interesting improvement that may be done to have a positive impact on the accuracy of inertial-based motion tracking systems, is to define a standard set of movements for the initial calibration and a standard method of data processing by which extrapolate kinematic parameters of high clinical relevance.
Some works have reported remarkable results in human motion tracking using e-textile sensors [8, 46]. Technological improvements in the development of conductive elastomers allowed to integrate such strain sensors directly into garments making them comfortable and unobtrusive [11, 56]. Although conductive elastomers ensure flexibility and performances comparable with those of the M-IMU sensors, the main limitations are the hysteresis, uniaxial measurements and non-negligible transient time [56]. Wearable systems based on strain sensors are a promising technology for kinematics analysis that may overcome the main M-IMUs drawbacks, as interferences due to surrounding ferromagnetic materials, gyroscopes’ error drift and long-term use. On the other hand, errors may occur with strain sensors-based systems in the estimation of shoulder kinematics for their inherent hysteresis behaviour.
Among wearable systems reviewed in this summary, differences resulted in terms of sensors typology, number and size, placement, and wearability features. Sensors placement and method of attachment must be carefully investigated as they could influence the outcomes reliability (e.g., effects of soft tissues’ artefacts). Human skeleton is covered by skin tissue and muscles. The combination of skin’s elasticity and muscle activity may cause negative effects in the measurement of the bones’ movement. In studies where M-IMU sensors were used to track shoulder kinematics, soft tissue properties were opportunely included in mathematical models to reduce soft tissue artifacts [79, 85]. The body fat percentage was found the main influencing factor that negatively affects the inertial sensors’ orientation [85]. To reduce such source of error, either when sensors are directly adherent to the skin that embedded in a textile, sensing units should be placed as near as possible to the bone segment to reduce soft tissue artifacts [97, 98]. Wearability is a key factor to consider because it can influence the level of patients’ acceptance [26].There are several relevant requirements that wearable systems must meet to encourage their applications in continuous monitoring of patient status. Indeed, execution of movements, either in home environments or in clinical settings, should not be hindered by measurements systems so they must be non-invasive, modular, lightweight, unobtrusive and include a minimal number of sensors [33, 40, 51, 56, 66, 67, 91]. Most studies have employed magneto and inertial-based tracking systems in which sensors were attached to the upper limb through Velcro straps or including them in modular brace and garments [26, 45, 67, 82, 88].
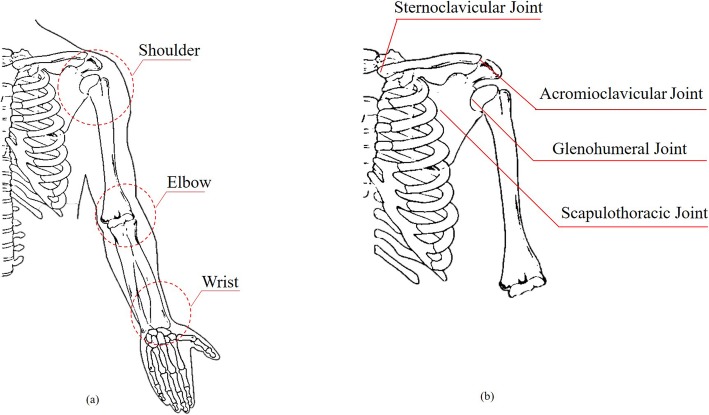
Upper limb includes the shoulder, elbow and wrist joints (Fig. 3a). Humerus, scapula, clavicle, and thorax constitute the shoulder complex: humeral head articulates in the glenoid fossa of the scapula to form GH joint, the AC joint is the articulation between the lateral end of the clavicle and the acromion process, the SC joint articulates the medial end of the clavicle and the sternum and the functional ST joint allows rotational and translational movements of the scapula with respect to the thorax [96] (Fig. 3b). The ST joint and GH joint act togheter in arm elevation according to scapular-humeral rhythm described in [99]. From a biomechanical point of view, shoulder complexity is justified by the high degree of coupling and coordination between shoulder joints (i.e., shoulder rhythm) and the action of more than one muscles over more than one joints in the execution of a movement. Data extraction of shoulder kinematics is frequently based on movements pattern in the sagittal, frontal and transversal planes, so monitoring of complex movements (e.g., daily activities) in multiple planes, performed through wearable sensors, requires a more stringent evaluation and accurate interpretation. As resulted in the review, the shoulder is generally approximated as a ball-and-socket joint [56]. This assumption provides an approximate representation of the whole shoulder girdle (e.g., it neglects the contribution of scapular movements). A standardized protocol has been proposed (i.e., The ISEO®, INAIL Shoulder and Elbow Outpatient protocol) to improve the performance of M-IMUs in the estimation of scapular kinematics, by locating inertial sensors on the back in correspondence of scapula [33, 35–38, 40, 65]. An adequate investigation of scapular motions may be beneficial to assess shoulder disorders [100].
Fig. 3.
a Anatomy of the Upper limb; b Anatomy of the Shoulder complex
For long-term monitoring of shoulder kinematics considering also scapular motions, the combination of M-IMUs and smart-textile with embedded strain sensors is a perfect balancing of accuracy, flexibility and wearability (i.e., strain sensors positioned on the scapula could increase the portability and acceptance of the wearable system for long-term monitoring of ADLs) [86].
Applicability in clinical setting and rehabilitation
Alterations in the complex shoulder kinematics can derive by both neurological or musculoskeletal disorders and result in pain and limited movements [68]. Compensatory movements in patients with shoulder disorders are the most common consequential responses to pain or to difficulty in performing free-pain movements. In such situations, information retrieved by posture monitoring may be beneficial in clinical application and rehabilitation [26]. In the last years, the application of wearable devices for gathering motion data outside the laboratory settings is growing. Avoiding complex laboratory set-up, wearable systems employed to assess upper limb kinematics have proven to be a well-founded alternative to obtain quantitative motions parameters. Quantitative outcomes about shoulder motions recorded by wearable sensors are beneficial in clinical practice in terms of time-saving and they are becoming a promising alternative to improve assessment accuracy overcoming the subjectivity of clinical scales. The automatic assessment of motor abilities can also provide therapists a tangible and, therefore, measurable awareness of the effectiveness of the treatment and the recovery path chosen.
In clinical practice, the severity level of patients’ condition with musculoskeletal disease is usually assessed through questionnaire-based scores [36, 42]. Algorithms for kinematic scores computing were developed to evaluate shoulder functional performance after surgery in subjects with GH osteoarthritis and RC diseases, elaborating data obtained from IMU sensors [29, 31]. High correlation (0.61–0.8) between shoulder kinematic scores (i.e., power score, range of angular velocity score and moment score) and clinical scales (e.g., DASH, SST, VAS) was found [31]. Unlike clinical scores, kinematic scores showed greater sensitivity in detecting significant functional changes in shoulder activity at each post-operative follow-up with respect to the baseline status [29, 31]. In a five-year follow-up study, asymmetry in shoulder movements was evaluated in patients with subacromial impingements syndrome. Asymmetry scores, derived from an IMU-based system, showed post-treatment improvements with greater sensitivity than clinical scores and only a weak correlation was found with DASH (r = 0.39) and SST (r = 0.32) [32]. Quantitative evaluation of arm usage and quality of movements in every kind of shoulder impairment contributes to outline a clinical picture about the functional recovery and the effectiveness of the treatment [30, 49]. Using the same number of IMU (n = 3) and the same placement on both humeri and sternum, the shoulder function was evaluated before and after treatment, in patients underwent surgery for RC tear [5, 34]. Results showed significative differences in movements frequency between patients and control group during activities of daily life [5], with limited use of arm at 3 months after surgery [34]. With a bilateral configuration based on 5 IMU, shoulder motion was assessed to extrapolate relevant clinical outcomes about Total Shoulder Arthroplasty (TSA) and Reverse Total Shoulder Arthroplasty (RTSA) [6]. Patients underwent either TSA or RTSA showed shoulder ROM below 80° of elevation, indiscriminately; but, on average, patients treated with RTSA performed movements above 100° less frequently [6]. Objective measurements (i.e., mean activity value and activity frequency) of limb function after RTSA did not show significant improvements 1 year after surgery, despite DASH scores and pain perception have improved compared to preoperative outcomes [41].
In patient with neurological impairments (e.g., stroke), assessments of motor abilities performed through wearable sensors showed a time saving compared to clinical scores (e.g., Fugl-Meyer Assessment Test) measured by the clinician [50, 53]. Data from accelerometers-based systems demonstrated accurate capability in the estimation of clinical scores for quality of movement (e.g., FAS score) and in prediction of shoulder features about shoulder portion of Fugl-Meyer scale with errors near 10% [42, 49]. Generally, the main evaluated features comprise coordination, smoothness, presence of compensatory movements, speed, amplitude of ROM. Quantitative measurements, such as movement time and smoothness, showed a strong correlation with Action research arm test scores in patients after stroke [7]. Spatiotemporal parameters (e.g., ROM, movement time) extracted from inertial sensors’ data provided an accurate evaluation of patients with multiple sclerosis and they distinguished affected and unaffected upper limbs in children with hemiparesis significantly [60, 62].
Digital simulations and virtual reality implementation in upper limb rehabilitation context aim to reproduce accurately limb movements processing data from wearable sensors and give a direct feedback about the adequacy or not of the executed movements [40]. The long-term monitoring, associated with suitable feedback strategy (e.g., visive, auditory, vibrational), can foster the correction of wrong postures [40, 52]. In addition, wearable systems allows a more supervised home-rehabilitation giving substantial improvements to patient healing: total patient involvement in rehabilitation programs can advantage the motor learning process and, at the same time, providing a direct feedback (e.g., visual, auditory) about performance level can increase patient interest and motivation [44, 48]. A new trend is the use of smartphone as monitoring systems or user-interface [53, 76, 84]. Implementation of suitable application (i.e., App) can provide a direct feedback to the patients and therapists about the progress in motor performance [26]. Gathered data could be remotely evaluated by the therapists [64]. Remote monitoring can provide useful information about patients’ status at every stage of rehabilitation pathway and, at the same time, it implies a greater centralization of patients role in the management of their own health associated to a more direct clinician control [101]. A typical architecture of remote monitoring systems includes: i) wearable sensing unit to gather movements data; ii) data storage and management in cloud computing; iii) software to analyse data and extract relevant clinical parameters [58, 66]. This approach implies collection of big amounts of data regarding personal information that requires ethical considerations and the definition of legal responsibility [102].
Most of the reviewed articles limited the application of wearable systems in short-time session for shoulder motion evaluation; only few studies performed longer monitoring periods of ADLs until 7 or 11 monitoring hours of 1 day [5, 6, 34].
Conclusion
This review reveals that wearable systems are becoming an efficient and promising tool to evaluate shoulder health after neurological trauma or musculoskeletal injuries. Wearable systems have the potential to provide quantitative and meaningful clinical information about movement quality and progress in a rehabilitation pathway. The magneto-inertial measurements systems resulted the most used in clinical and research settings, followed by the growing application of smart-textiles for joint angles assessment. Despite of the accuracy of the current wearable systems in shoulder kinematics assessment, additional investigation needs to be executed to ensure long-term applicability in clinical settings and rehabilitation.
Acknowledgements
Not applicable.
Abbreviations
- AB-AD
abduction-adduction
- AC
acromioclavicular
- CMS
Constant-Murley score
- DASH
Disability of the Arm, Shoulder, and Hand
- DOFs
degrees of freedom
- EMG
electromyography
- ER
external rotation
- FLX-EXT
flexion-extension
- GH
glenohumeral
- HT
humerothoracic
- IE
internal rotation
- IER
internal-external rotation
- IMU
inertial measurement unit
- KF
Kalman filter
- MEMS
micro-electro-mechanical systems
- M-IMU
magnetic and inertial measurement unit
- OLE
Optical Linear Encoder
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RC
rotator cuff
- RMSE
root mean square error
- ROM
range of motion
- RTSA
Reverse Total Shoulder Arthroplasty
- SC
sternoclavicular
- SST
Simple Shoulder test
- ST
scapulothoracic
- TSA
Total Shoulder Arthroplasty
- VAS
Visual Analogue Scale
Authors’ contributions
UGL and ES conceived and supervised the study. AC carried out the search process and data collection, UGL, ES and VD assessed the quality of the study. AC and ES drafted the manuscript. All the authors have read and approved the final manuscript.
Funding
This work has been funded by the Italian Ministry of Health in the framework of RICERCA FINALIZZATA 2016 (PE-2016-02364894).
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
UGL and AB are members of the Editorial Board of BMC Musculoskeletal Disorders. The remaining authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Arianna Carnevale, Email: arianna.carnevale@unicampus.it.
Umile Giuseppe Longo, Phone: +39-06-2254-1613, Email: g.longo@unicampus.it.
Emiliano Schena, Email: e.schena@unicampus.it.
Carlo Massaroni, Email: c.massaroni@unicampus.it.
Daniela Lo Presti, Email: d.lopresti@unicampus.it.
Alessandra Berton, Email: a.berton@unicampus.it.
Vincenzo Candela, Email: v.candela@unicampus.it.
Vincenzo Denaro, Email: denaro.cbm@gmail.com.
References
- 1.Cutti AG, Veeger HE. Shoulder biomechanics: today’s consensus and tomorrow’s perspectives. Med Biol Eng Comput. 2009;47(5):463–466. doi: 10.1007/s11517-009-0487-3. [DOI] [PubMed] [Google Scholar]
- 2.Longo UG, Vasta S, Maffulli N, Denaro V. Scoring systems for the functional assessment of patients with rotator cuff pathology. Sports Med Arthrosc Rev. 2011;19(3):310–320. doi: 10.1097/JSA.0b013e31820af9b6. [DOI] [PubMed] [Google Scholar]
- 3.Longo UG, Berton A, Ahrens PM, Maffulli N, Denaro V. Clinical tests for the diagnosis of rotator cuff disease. Sports Med Arthrosc Rev. 2011;19(3):266–278. doi: 10.1097/JSA.0b013e3182250c8b. [DOI] [PubMed] [Google Scholar]
- 4.Longo UG, Saris D, Poolman RW, Berton A, Denaro V. Instruments to assess patients with rotator cuff pathology: a systematic review of measurement properties. Knee Surg Sports Traumatol Arthrosc. 2012;20(10):1961–1970. doi: 10.1007/s00167-011-1827-z. [DOI] [PubMed] [Google Scholar]
- 5.Duc C, Farron A, Pichonnaz C, Jolles BM, Bassin JP, Aminian K. Distribution of arm velocity and frequency of arm usage during daily activity: objective outcome evaluation after shoulder surgery. Gait Posture. 2013;38(2):247–252. doi: 10.1016/j.gaitpost.2012.11.021. [DOI] [PubMed] [Google Scholar]
- 6.Langohr GDG, Haverstock JP, Johnson JA, Athwal GS. Comparing daily shoulder motion and frequency after anatomic and reverse shoulder arthroplasty. J Shoulder Elb Surg. 2018;27(2):325–332. doi: 10.1016/j.jse.2017.09.023. [DOI] [PubMed] [Google Scholar]
- 7.Repnik E, Puh U, Goljar N, Munih M, Mihelj M. Using Inertial Measurement Units and Electromyography to Quantify Movement during Action Research Arm Test Execution. Sensors (Basel) 2018;18:9. doi: 10.3390/s18092767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bartalesi R, Lorussi F, Tesconi M, Tognetti A, Zupone G, Rossi DD: Wearable kinesthetic system for capturing and classifying upper limb gesture. In: First Joint Eurohaptics Conference and Symposium on Haptic Interfaces for Virtual Environment and Teleoperator Systems World Haptics Conference: 18–20 March 2005 2005; 2005: 535–536.
- 9.Massaroni C, Di Tocco J, Presti DL, Schena E, Bressi F, Bravi M, Miccinilli S, Sterzi S, Longo UG, Berton A: Influence of motion artifacts on a smart garment for monitoring respiratory rate. In: 2019 IEEE International Symposium on Medical Measurements and Applications (MeMeA): 2019: IEEE; 2019: 1–6.
- 10.Presti DL, Massaroni C, Di Tocco J, Schena E, Formica D, Caponero MA, Longo UG, Carnevale A, D’Abbraccio J, Massari L: Cardiac monitoring with a smart textile based on polymer-encapsulated FBG: influence of sensor positioning. In: 2019 IEEE International Symposium on Medical Measurements and Applications (MeMeA): 2019: IEEE; 2019: 1–6.
- 11.Esfahani MIM, Nussbaum MA. A “smart” undershirt for tracking upper body motions: task classification and angle estimation. IEEE Sensors J. 2018;18(18):7650–7658. doi: 10.1109/JSEN.2018.2859626. [DOI] [Google Scholar]
- 12.Jordan K, Haywood KL, Dziedzic K, Garratt AM, Jones PW, Ong BN, Dawes PT. Assessment of the 3-dimensional Fastrak measurement system in measuring range of motion in ankylosing spondylitis. J Rheumatol. 2004;31(11):2207–2215. [PubMed] [Google Scholar]
- 13.Illyés A, Kiss RM. Method for determining the spatial position of the shoulder with ultrasound-based motion analyzer. J Electromyogr Kinesiol. 2006;16(1):79–88. doi: 10.1016/j.jelekin.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 14.Kuster RP, Heinlein B, Bauer CM, Graf ES. Accuracy of KinectOne to quantify kinematics of the upper body. Gait Posture. 2016;47:80–85. doi: 10.1016/j.gaitpost.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 15.Pérez R, Costa Ú, Torrent M, Solana J, Opisso E, Cáceres C, Tormos JM, Medina J, Gómez EJ. Upper limb portable motion analysis system based on inertial technology for neurorehabilitation purposes. Sensors (Basel) 2010;10(12):10733–10751. doi: 10.3390/s101210733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lambrecht JM, Kirsch RF. Miniature low-power inertial sensors: promising technology for implantable motion capture systems. IEEE Trans Neural Syst Rehabil Eng. 2014;22(6):1138–1147. doi: 10.1109/TNSRE.2014.2324825. [DOI] [PubMed] [Google Scholar]
- 17.Fantozzi S, Giovanardi A, Magalhães FA, Di Michele R, Cortesi M, Gatta G. Assessment of three-dimensional joint kinematics of the upper limb during simulated swimming using wearable inertial-magnetic measurement units. J Sports Sci. 2016;34(11):1073–1080. doi: 10.1080/02640414.2015.1088659. [DOI] [PubMed] [Google Scholar]
- 18.Presti DL, Massaroni C, Formica D, Saccomandi P, Giurazza F, Caponero MA, Schena E. Smart textile based on 12 fiber Bragg gratings array for vital signs monitoring. IEEE Sensors J. 2017;17(18):6037–6043. doi: 10.1109/JSEN.2017.2731788. [DOI] [Google Scholar]
- 19.Massaroni C, Carraro E, Vianello A, Miccinilli S, Morrone M, Levai IK, Schena E, Saccomandi P, Sterzi S, Dickinson JW, et al. Optoelectronic Plethysmography in clinical practice and research: a review. Respiration. 2017;93(5):339–354. doi: 10.1159/000462916. [DOI] [PubMed] [Google Scholar]
- 20.Massaroni C, Venanzi C, Silvatti AP, Lo Presti D, Saccomandi P, Formica D, Giurazza F, Caponero MA, Schena E. Smart textile for respiratory monitoring and thoraco-abdominal motion pattern evaluation. J Biophotonics. 2018;11(5):e201700263. doi: 10.1002/jbio.201700263. [DOI] [PubMed] [Google Scholar]
- 21.de Lucena DS, Stoller O, Rowe JB, Chan V, Reinkensmeyer DJ. Wearable sensing for rehabilitation after stroke: bimanual jerk asymmetry encodes unique information about the variability of upper extremity recovery. IEEE Int Conf Rehabil Robot. 2017;2017:1603–1608. doi: 10.1109/ICORR.2017.8009477. [DOI] [PubMed] [Google Scholar]
- 22.Patel S, Park H, Bonato P, Chan L, Rodgers M. A review of wearable sensors and systems with application in rehabilitation. Journal of neuroengineering and rehabilitation. 2012;9:21. doi: 10.1186/1743-0003-9-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muro-de-la-Herran A, Garcia-Zapirain B, Mendez-Zorrilla A. Gait analysis methods: an overview of wearable and non-wearable systems, highlighting clinical applications. Sensors (Basel) 2014;14(2):3362–3394. doi: 10.3390/s140203362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bergmann JH, Chandaria V, McGregor A. Wearable and implantable sensors: the patient's perspective. Sensors (Basel) 2012;12(12):16695–16709. doi: 10.3390/s121216695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Caldani L, Pacelli M, Farina D, Paradiso R. E-textile platforms for rehabilitation. Conf Proc IEEE Eng Med Biol Soc. 2010;2010:5181–5184. doi: 10.1109/IEMBS.2010.5626148. [DOI] [PubMed] [Google Scholar]
- 26.Wang Q, De Baets L, Timmermans A, Chen W, Giacolini L, Matheve T, Markopoulos P. Motor Control Training for the Shoulder with Smart Garments. Sensors (Basel) 2017;17:7. doi: 10.3390/s17071687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Burns DM, Leung N, Hardisty M, Whyne CM, Henry P, McLachlin S. Shoulder physiotherapy exercise recognition: machine learning the inertial signals from a smartwatch. Physiol Meas. 2018;39(7):075007. doi: 10.1088/1361-6579/aacfd9. [DOI] [PubMed] [Google Scholar]
- 28.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 29.Coley B, Jolles BM, Farron A, Bourgeois A, Nussbaumer F, Pichonnaz C, Aminian K. Outcome evaluation in shoulder surgery using 3D kinematics sensors. Gait Posture. 2007;25(4):523–532. doi: 10.1016/j.gaitpost.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 30.Coley B, Jolles BM, Farron A, Pichonnaz C, Bassin JP, Aminian K. Estimating dominant upper-limb segments during daily activity. Gait Posture. 2008;27(3):368–375. doi: 10.1016/j.gaitpost.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 31.Jolles BM, Duc C, Coley B, Aminian K, Pichonnaz C, Bassin JP, Farron A. Objective evaluation of shoulder function using body-fixed sensors: a new way to detect early treatment failures? J Shoulder Elb Surg. 2011;20(7):1074–1081. doi: 10.1016/j.jse.2011.05.026. [DOI] [PubMed] [Google Scholar]
- 32.Körver RJ, Senden R, Heyligers IC, Grimm B. Objective outcome evaluation using inertial sensors in subacromial impingement syndrome: a five-year follow-up study. Physiol Meas. 2014;35(4):677–686. doi: 10.1088/0967-3334/35/4/677. [DOI] [PubMed] [Google Scholar]
- 33.van den Noort JC, Wiertsema SH, Hekman KMC, Schönhuth CP, Dekker J, Harlaar J. Reliability and precision of 3D wireless measurement of scapular kinematics. Med Biol Eng Comput. 2014;52(11):921–931. doi: 10.1007/s11517-014-1186-2. [DOI] [PubMed] [Google Scholar]
- 34.Pichonnaz C, Duc C, Jolles BM, Aminian K, Bassin JP, Farron A. Alteration and recovery of arm usage in daily activities after rotator cuff surgery. J Shoulder Elb Surg. 2015;24(9):1346–1352. doi: 10.1016/j.jse.2015.01.017. [DOI] [PubMed] [Google Scholar]
- 35.Roldán-Jiménez C, Cuesta-Vargas AI. Studying upper-limb kinematics using inertial sensors: a cross-sectional study. BMC Res Notes. 2015;8:532. doi: 10.1186/s13104-015-1517-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van den Noort JC, Wiertsema SH, Hekman KM, Schönhuth CP, Dekker J, Harlaar J. Measurement of scapular dyskinesis using wireless inertial and magnetic sensors: importance of scapula calibration. J Biomech. 2015;48(12):3460–3468. doi: 10.1016/j.jbiomech.2015.05.036. [DOI] [PubMed] [Google Scholar]
- 37.Cutti AG, Giovanardi A, Rocchi L, Davalli A, Sacchetti R. Ambulatory measurement of shoulder and elbow kinematics through inertial and magnetic sensors. Med Biol Eng Comput. 2008;46(2):169–178. doi: 10.1007/s11517-007-0296-5. [DOI] [PubMed] [Google Scholar]
- 38.Roldán-Jiménez C, Cuesta-Vargas AI. Age-related changes analyzing shoulder kinematics by means of inertial sensors. Clin Biomech (Bristol, Avon) 2016;37:70–76. doi: 10.1016/j.clinbiomech.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 39.Aslani N, Noroozi S, Davenport P, Hartley R, Dupac M, Sewell P. Development of a 3D workspace shoulder assessment tool incorporating electromyography and an inertial measurement unit-a preliminary study. Med Biol Eng Comput. 2018;56(6):1003–1011. doi: 10.1007/s11517-017-1745-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Carbonaro N, Lucchesi I, Lorusssi F, Tognetti A: Tele-monitoring and tele-rehabilitation of the shoulder muscular-skeletal diseases through wearable systems. In: 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC): 18–21 July 2018 2018; 2018: 4410–4413. [DOI] [PubMed]
- 41.Hurd WJ, Morrow MM, Miller EJ, Adams RA, Sperling JW, Kaufman KR. Patient-reported and objectively measured function before and after reverse shoulder Arthroplasty. J Geriatr Phys Ther. 2018;41(3):126–133. doi: 10.1519/JPT.0000000000000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hester T, Hughes R, Sherrill DM, Knorr B, Akay M, Stein J, Bonato P: Using wearable sensors to measure motor abilities following stroke. In: International Workshop on Wearable and Implantable Body Sensor Networks (BSN'06): 3–5 April 2006 2006; 2006: 4 pp.-8.
- 43.Zhou H, Hu H, Harris ND, Hammerton J. Applications of wearable inertial sensors in estimation of upper limb movements. Biomedical Signal Processing and Control. 2006;1(1):22–32. doi: 10.1016/j.bspc.2006.03.001. [DOI] [Google Scholar]
- 44.Willmann RD, Lanfermann G, Saini P, Timmermans A, te Vrugt J, Winter S. Home stroke rehabilitation for the upper limbs. Conf Proc IEEE Eng Med Biol Soc. 2007;2007:4015–4018. doi: 10.1109/IEMBS.2007.4353214. [DOI] [PubMed] [Google Scholar]
- 45.Zhou H, Stone T, Hu H, Harris N. Use of multiple wearable inertial sensors in upper limb motion tracking. Med Eng Phys. 2008;30(1):123–133. doi: 10.1016/j.medengphy.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 46.Giorgino T, Tormene P, Lorussi F, Rossi DD, Quaglini S. Sensor evaluation for wearable strain gauges in neurological rehabilitation. IEEE Transactions on Neural Systems and Rehabilitation Engineering. 2009;17(4):409–415. doi: 10.1109/TNSRE.2009.2019584. [DOI] [PubMed] [Google Scholar]
- 47.Lee GX, Low KS, Taher T. Unrestrained measurement of arm motion based on a wearable wireless sensor network. IEEE Trans Instrum Meas. 2010;59(5):1309–1317. doi: 10.1109/TIM.2010.2043974. [DOI] [Google Scholar]
- 48.Chee Kian L, Chen I, Zhiqiang L, Yeo SH: A low cost wearable wireless sensing system for upper limb home rehabilitation. In: 2010 IEEE Conference on Robotics, Automation and Mechatronics: 28–30 June 2010 2010; 2010: 1–8.
- 49.Patel S, Hughes R, Hester T, Stein J, Akay M, Dy JG, Bonato P. A novel approach to monitor rehabilitation outcomes in stroke survivors using wearable technology. Proc IEEE. 2010;98(3):450–461. doi: 10.1109/JPROC.2009.2038727. [DOI] [PubMed] [Google Scholar]
- 50.Bento VF, Cruz VT, Ribeiro DD, Cunha JPS: Towards a movement quantification system capable of automatic evaluation of upper limb motor function after neurological injury. In: 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society: 30 Aug.-3 Sept. 2011 2011; 2011: 5456–5460. [DOI] [PubMed]
- 51.Nguyen KD, Chen I, Luo Z, Yeo SH, Duh HB. A wearable sensing system for tracking and monitoring of functional arm movement. IEEE/ASME Transactions on Mechatronics. 2011;16(2):213–220. doi: 10.1109/TMECH.2009.2039222. [DOI] [Google Scholar]
- 52.Ding ZQ, Luo ZQ, Causo A, Chen IM, Yue KX, Yeo SH, Ling KV. Inertia sensor-based guidance system for upperlimb posture correction. Med Eng Phys. 2013;35(2):269–276. doi: 10.1016/j.medengphy.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 53.Lee WW, Yen SC, Tay A, Zhao Z, Xu TM, Ling KK, Ng YS, Chew E, Cheong AL, Huat GK. A smartphone-centric system for the range of motion assessment in stroke patients. IEEE J Biomed Health Inform. 2014;18(6):1839–1847. doi: 10.1109/JBHI.2014.2301449. [DOI] [PubMed] [Google Scholar]
- 54.Bai L, Pepper MG, Yan Y, Spurgeon SK, Sakel M, Phillips M. Quantitative assessment of upper limb motion in neurorehabilitation utilizing inertial sensors. IEEE Trans Neural Syst Rehabil Eng. 2015;23(2):232–243. doi: 10.1109/TNSRE.2014.2369740. [DOI] [PubMed] [Google Scholar]
- 55.Ertzgaard P, Öhberg F, Gerdle B, Grip H. A new way of assessing arm function in activity using kinematic exposure variation analysis and portable inertial sensors--a validity study. Man Ther. 2016;21:241–249. doi: 10.1016/j.math.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 56.Lorussi F, Carbonaro N, De Rossi D, Tognetti A. A bi-articular model for scapular-humeral rhythm reconstruction through data from wearable sensors. J Neuroeng Rehabil. 2016;13:40. doi: 10.1186/s12984-016-0149-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mazomenos EB, Biswas D, Cranny A, Rajan A, Maharatna K, Achner J, Klemke J, Jöbges M, Ortmann S, Langendörfer P. Detecting elementary arm movements by tracking upper limb joint angles with MARG sensors. IEEE Journal of Biomedical and Health Informatics. 2016;20(4):1088–1099. doi: 10.1109/JBHI.2015.2431472. [DOI] [PubMed] [Google Scholar]
- 58.Jiang Y, Qin Y, Kim I, Wang Y: Towards an IoT-based upper limb rehabilitation assessment system. In: 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC): 11–15 July 2017 2017; 2017: 2414–2417. [DOI] [PubMed]
- 59.Li Y, Zhang X, Gong Y, Cheng Y, Gao X, Chen X. Motor Function Evaluation of Hemiplegic Upper-Extremities Using Data Fusion from Wearable Inertial and Surface EMG Sensors. Sensors (Basel) 2017;17:3. doi: 10.3390/s18010003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Newman CJ, Bruchez R, Roches S, Jequier Gygax M, Duc C, Dadashi F, Massé F, Aminian K. Measuring upper limb function in children with hemiparesis with 3D inertial sensors. Childs Nerv Syst. 2017;33(12):2159–2168. doi: 10.1007/s00381-017-3580-1. [DOI] [PubMed] [Google Scholar]
- 61.Yang X, Tan J: Tracking of Human Joints Using Twist and Exponential Map. In: 2017 IEEE 7th Annual International Conference on CYBER Technology in Automation, Control, and Intelligent Systems (CYBER): 31 July-4 Aug. 2017 2017; 2017: 592–597.
- 62.Daunoraviciene K, Ziziene J, Griskevicius J, Pauk J, Ovcinikova A, Kizlaitiene R, Kaubrys G. Quantitative assessment of upper extremities motor function in multiple sclerosis. Technol Health Care. 2018;26(S2):647–653. doi: 10.3233/THC-182511. [DOI] [PubMed] [Google Scholar]
- 63.Jung H, Park J, Jeong J, Ryu T, Kim Y, Lee SI: A wearable monitoring system for at-home stroke rehabilitation exercises: A preliminary study. In: 2018 IEEE EMBS International Conference on Biomedical & Health Informatics (BHI): 4–7 March 2018 2018; 2018: 13–16.
- 64.Lin LF, Lin YJ, Lin ZH, Chuang LY, Hsu WC, Lin YH. Feasibility and efficacy of wearable devices for upper limb rehabilitation in patients with chronic stroke: a randomized controlled pilot study. Eur J Phys Rehabil Med. 2018;54(3):388–396. doi: 10.23736/S1973-9087.17.04691-3. [DOI] [PubMed] [Google Scholar]
- 65.Parel I, Cutti AG, Fiumana G, Porcellini G, Verni G, Accardo AP. Ambulatory measurement of the scapulohumeral rhythm: intra- and inter-operator agreement of a protocol based on inertial and magnetic sensors. Gait Posture. 2012;35(4):636–640. doi: 10.1016/j.gaitpost.2011.12.015. [DOI] [PubMed] [Google Scholar]
- 66.Daponte P, Vito LD, Sementa C: A wireless-based home rehabilitation system for monitoring 3D movements. In: 2013 IEEE International Symposium on Medical Measurements and Applications (MeMeA): 4–5 May 2013 2013; 2013: 282–287.
- 67.Daponte P, Vito LD, Sementa C: Validation of a home rehabilitation system for range of motion measurements of limb functions. In: 2013 IEEE International Symposium on Medical Measurements and Applications (MeMeA): 4–5 May 2013 2013; 2013: 288–293.
- 68.Pan J-I, Chung H-W, Huang J-J. Intelligent shoulder joint home-based self-rehabilitation monitoring system. Int J Smart Home. 2013;7(5):395–404. doi: 10.14257/ijsh.2013.7.5.38. [DOI] [Google Scholar]
- 69.Thiemjarus S, Marukatat S, Poomchoompol P. A method for shoulder range-of-motion estimation using a single wireless sensor node. Conf Proc IEEE Eng Med Biol Soc. 2013;2013:5907–5910. doi: 10.1109/EMBC.2013.6610896. [DOI] [PubMed] [Google Scholar]
- 70.Rawashdeh SA, Rafeldt DA, Uhl TL, Lumpp JE: Wearable motion capture unit for shoulder injury prevention. In: 2015 IEEE 12th International Conference on Wearable and Implantable Body Sensor Networks (BSN): 9–12 June 2015 2015; 2015: 1–6.
- 71.Álvarez D, Alvarez JC, González RC, López AM. Upper limb joint angle measurement in occupational health. Comput Methods Biomech Biomed Engin. 2016;19(2):159–170. doi: 10.1080/10255842.2014.997718. [DOI] [PubMed] [Google Scholar]
- 72.Lee H, Cho J, Kim J: Printable skin adhesive stretch sensor for measuring multi-axis human joint angles. In: 2016 IEEE International Conference on Robotics and Automation (ICRA): 16–21 May 2016 2016; 2016: 4975–4980.
- 73.Tran TM, Vejarano G: Prediction of received signal strength from human joint angles in body area networks. In: 2016 International Conference on Computing, Networking and Communications (ICNC): 15–18 Feb. 2016 2016; 2016: 1–6.
- 74.Rawashdeh SA, Rafeldt DA, Uhl TL. Wearable IMU for Shoulder Injury Prevention in Overhead Sports. Sensors (Basel) 2016;16:11. doi: 10.3390/s16111847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wu Y, Chen K, Fu C. Natural gesture modeling and recognition approach based on joint movements and arm orientations. IEEE Sensors J. 2016;16(21):7753–7761. doi: 10.1109/JSEN.2016.2599019. [DOI] [Google Scholar]
- 76.Ramkumar PN, Haeberle HS, Navarro SM, Sultan AA, Mont MA, Ricchetti ET, Schickendantz MS, Iannotti JP. Mobile technology and telemedicine for shoulder range of motion: validation of a motion-based machine-learning software development kit. J Shoulder Elb Surg. 2018;27(7):1198–1204. doi: 10.1016/j.jse.2018.01.013. [DOI] [PubMed] [Google Scholar]
- 77.Jung Y, Kang D, Kim J: Upper body motion tracking with inertial sensors. In: 2010 IEEE International Conference on Robotics and Biomimetics: 14–18 Dec. 2010 2010; 2010: 1746-1751.
- 78.El-Gohary M, Holmstrom L, Huisinga J, King E, McNames J, Horak F. Upper limb joint angle tracking with inertial sensors. Conf Proc IEEE Eng Med Biol Soc. 2011;2011:5629–5632. doi: 10.1109/IEMBS.2011.6091362. [DOI] [PubMed] [Google Scholar]
- 79.Zhang Z, Wong W, Wu J. Ubiquitous human upper-limb motion estimation using wearable sensors. IEEE Trans Inf Technol Biomed. 2011;15(4):513–521. doi: 10.1109/TITB.2011.2159122. [DOI] [PubMed] [Google Scholar]
- 80.El-Gohary M, McNames J. Shoulder and elbow joint angle tracking with inertial sensors. IEEE Trans Biomed Eng. 2012;59(9):2635–2641. doi: 10.1109/TBME.2012.2208750. [DOI] [PubMed] [Google Scholar]
- 81.Lee GX, Low K. A factorized quaternion approach to determine the arm motions using Triaxial accelerometers with anatomical and sensor constraints. IEEE Trans Instrum Meas. 2012;61(6):1793–1802. doi: 10.1109/TIM.2011.2181884. [DOI] [Google Scholar]
- 82.Hsu Y, Wang J, Lin Y, Chen S, Tsai Y, Chu C, Chang C: A wearable inertial-sensing-based body sensor network for shoulder range of motion assessment. In: 2013 1st International Conference on Orange Technologies (ICOT): 12–16 March 2013 2013; 2013: 328–331.
- 83.Ricci L, Formica D, Sparaci L, Lasorsa FR, Taffoni F, Tamilia E, Guglielmelli E. A new calibration methodology for thorax and upper limbs motion capture in children using magneto and inertial sensors. Sensors (Basel) 2014;14(1):1057–1072. doi: 10.3390/s140101057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Roldan-Jimenez C, Cuesta-Vargas A, Bennett P. Studying upper-limb kinematics using inertial sensors embedded in Mobile phones. JMIR Rehabil Assist Technol. 2015;2(1):e4. doi: 10.2196/rehab.4101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Meng D, Shoepe T, Vejarano G. Accuracy improvement on the measurement of human-joint angles. IEEE J Biomed Health Inform. 2016;20(2):498–507. doi: 10.1109/JBHI.2015.2394467. [DOI] [PubMed] [Google Scholar]
- 86.Crabolu M, Pani D, Raffo L, Conti M, Crivelli P, Cereatti A. In vivo estimation of the shoulder joint center of rotation using magneto-inertial sensors: MRI-based accuracy and repeatability assessment. Biomed Eng Online. 2017;16(1):34. doi: 10.1186/s12938-017-0324-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kim HJ, Lee YS, Kim D: Arm Motion Estimation Algorithm Using MYO Armband. In: 2017 First IEEE International Conference on Robotic Computing (IRC): 10–12 April 2017 2017; 2017: 376–381.
- 88.Morrow MMB, Lowndes B, Fortune E, Kaufman KR, Hallbeck MS. Validation of inertial measurement units for upper body kinematics. J Appl Biomech. 2017;33(3):227–232. doi: 10.1123/jab.2016-0120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rose M, Curtze C, O'Sullivan J, El-Gohary M, Crawford D, Friess D, Brady JM. Wearable inertial sensors allow for quantitative assessment of shoulder and elbow kinematics in a cadaveric knee arthroscopy model. Arthroscopy. 2017;33(12):2110–2116. doi: 10.1016/j.arthro.2017.06.042. [DOI] [PubMed] [Google Scholar]
- 90.Tian Y, Li Y, Zhu L, Tan J: Inertial-based real-time human upper limb tracking using twists and exponential maps in free-living environments. In: 2017 2nd International Conference on Advanced Robotics and Mechatronics (ICARM): 27–31 Aug. 2017 2017; 2017: 552–557.
- 91.Pathirana PN, Karunarathne MS, Williams GL, Nam PT, Durrant-Whyte H. Robust and accurate capture of human joint pose using an inertial sensor. IEEE Journal of Translational Engineering in Health and Medicine. 2018;6:1–11. doi: 10.1109/JTEHM.2018.2877980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Filippeschi A, Schmitz N, Miezal M, Bleser G, Ruffaldi E, Stricker D. Survey of Motion Tracking Methods Based on Inertial Sensors: A Focus on Upper Limb Human Motion. Sensors (Basel) 2017;17:6. doi: 10.3390/s17061257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Madgwick SO, Harrison AJ, Vaidyanathan A. Estimation of IMU and MARG orientation using a gradient descent algorithm. IEEE Int Conf Rehabil Robot. 2011;2011:5975346. doi: 10.1109/ICORR.2011.5975346. [DOI] [PubMed] [Google Scholar]
- 94.Atalay O, Kennon W. Knitted strain sensors: impact of design parameters on sensing properties. Sensors. 2014;14(3):4712–4730. doi: 10.3390/s140304712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Holm R: Electric contacts: theory and application: Springer Science & Business Media; 2013.
- 96.Yang J, Feng X, Kim JH, Rajulu S. Review of biomechanical models for human shoulder complex. International Journal of Human Factors Modelling and Simulation. 2010;1(3):271–293. doi: 10.1504/IJHFMS.2010.036791. [DOI] [Google Scholar]
- 97.Liu Y, Zhang Y, Zeng M: Joint parameter estimation using Magneto and Inertial measurement units. In: 2017 36th Chinese Control Conference (CCC): 26–28 July 2017 2017; 2017: 2225–2230.
- 98.Chen X, Zhang J, Hamel WR, Tan J: An inertial-based human motion tracking system with twists and exponential maps. In: 2014 IEEE International Conference on Robotics and Automation (ICRA): 31 May-7 June 2014 2014; 2014: 5665–5670.
- 99.Sugamoto K, Harada T, Machida A, Inui H, Miyamoto T, Takeuchi E, Yoshikawa H, Ochi T. Scapulohumeral rhythm: relationship between motion velocity and rhythm. Clin Orthop Relat Res. 2002;401:119–124. doi: 10.1097/00003086-200208000-00014. [DOI] [PubMed] [Google Scholar]
- 100.Struyf F, Nijs J, Baeyens JP, Mottram S, Meeusen R. Scapular positioning and movement in unimpaired shoulders, shoulder impingement syndrome, and glenohumeral instability. Scand J Med Sci Sports. 2011;21(3):352–358. doi: 10.1111/j.1600-0838.2010.01274.x. [DOI] [PubMed] [Google Scholar]
- 101.Beckmann JS, Lew D. Reconciling evidence-based medicine and precision medicine in the era of big data: challenges and opportunities. Genome Med. 2016;8(1):134. doi: 10.1186/s13073-016-0388-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sikka RS, Baer M, Raja A, Stuart M, Tompkins M. Analytics in sports medicine: implications and responsibilities that accompany the era of big data. J Bone Joint Surg Am. 2019;101(3):276–283. doi: 10.2106/JBJS.17.01601. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.