Abstract
With an emphasis on systems analyses, the VSV-EBOVAC project harnesses state-of-the-art technologies that illuminate mechanisms behind the observed immunogenicity and reactogenicity of the rVSV-ZEBOV vaccine and ensures that such information is shared among stakeholders.
In August 2014, after the Ebolavirus disease (EVD) outbreak hit six West African countries, the World Health Organization (WHO) created an African and European VSV-Ebola consortium (VEBCON) to initiate dose-escalation phase 1 clinical trials with a vesicular stomatitis virus (VSV)–Zaire Ebola virus vaccine candidate (rVSV-ZEBOV). When used at high doses in humans, the rVSV-ZEBOV Ebola vaccine elicited antibodies against the Ebola virus but also triggered an undesirable “reactogenic” response—including the development of viral oligoarthritis in multiple joints within the second week after vaccination—at discrepant frequencies across phase 1 clinical study sites. Lower doses reduced vaccine immunogenicity but did not prevent induction of arthritis. High doses of rVSV-ZEBOV proved to be efficacious in preventing Ebola virus disease within a few days after vaccination in a Guinea phase 3 clinical trial.
Now, the VSV-EBOVAC project on “Vaccine safety and immunogenicity signatures of human responses to VSV-ZEBOV” aims to acquire in-depth knowledge of the innate and adaptive immune responses elicited by the rVSV-ZEBOV vaccine during the WHO-initiated phase 1 trials being conducted in Switzerland, Kenya, and Gabon. Here, we describe these efforts to fill the knowledge gaps in Ebola virus (EBOV) research and development (R&D).
Unmet Need: Ebola Vaccine
Named after the Ebola river in the Democratic Republic of Congo (DRC), EBOV first appeared in 1976 in simultaneous outbreaks in DRC and Sudan (1). The 2014 outbreak was first recognized in Guinea in March, with cases and deaths reported in six West African countries: Guinea, Liberia, Nigeria, Senegal, Mali, and Sierra Leone (www.cdc.gov) (2). The known-case rate has exceeded the largest prior EVD outbreak, which occurred in Uganda in 2000 to 2001, with more than 26,000 confirmed or probable cases and more than 10,000 deaths (3). The scale of this outbreak has led to extraordinary efforts from the WHO and other institutions in an attempt to treat victims and contain the spread of disease. Outbreaks manifest through person-to-person transmission, with infection resulting from direct contact with blood or other bodily fluids or organs of infected people, and indirect contact with environments contaminated by such fluids (1). The EVD incubation period is between 2 and 21 days (7 to 10 days on average) (4), followed by severe acute illness. Death can occur 6 to 16 days after the onset of symptoms, and mortality rate has been reported in some outbreaks to be as high as 90% (1, 4). Such high infectivity of blood and secretions puts health care workers at particularly high risk during outbreaks. No effective therapies or licensed vaccines exist for any member of the Filoviridae family of viruses, and an effective vaccine would maximize safety for those at greatest risk of disease during outbreaks.
A primary antibody response [immunoglobulin M (IgM)] can be detected in the blood of infected persons 2 to 9 days after infection, whereas appearance of virus-specific IgG antibodies occurs ~17 to 25 days after infection and coincide with the recovery phase. Both humoral and cellular immunity are detected in EVD survivors (5), but the mechanisms at play and their relative contributions to protection in humans remain unknown.
A vaccination strategy capable of rapidly eliciting protective immunity in most recipients through a single vaccination is needed, in particular, for populations in areas of the world where EVD is endemic and outbreaks occur sporadically. A promising Ebola vaccine candidate, a replication-competent version of VSV that expresses a surface glyco-protein of Zaire Ebolavirus (rVSV-ZEBOV) (6, 7), was developed by the Public Health Agency of Canada in collaboration with several international partners (8) and licensed to NewLink Genetics and subsequently to Merck. The international consultation led by the WHO in September 2014 concluded that rVSV-ZEBOV was one of the only two candidates that had shown 100% protection in nonhuman primates and had clinical-grade material ready for testing in people (9–11). Researchers assessed the rVSV-ZEBOV vaccine’s potential for protection against newly emerging, phylogenetically related strains by immunizing macaques prior to challenge with Bundibugyo ebolavirus (BEBOV), a newly emerged Ebolavirus species (12). A single vaccination with rVSV-ZEBOV provided significant cross-protection (75% survival), suggesting that monovalent rVSV-based vaccines can be useful against newly emerging species. Thus, VEBCON initiated dose-escalation phase 1 clinical trials in Germany, Kenya, Gabon, and Switzerland.
Preliminary results from the phase 1 trials indicated that a single high dose of rVSV-ZEBOV was immunogenic but also reactogenic (13, 14); high doses [3 × 106 and 5 × 107 plaque-forming units (PFU)] provoked mild to moderate, early-onset, transient symptoms such as fever, myalgia, chills, fatigue, and headaches in most subjects and were associated with viremia and hematological changes indicative of vaccine replication (14). EBOV–glycoprotein (GP)–specific IgG antibody responses were detected in all participants, with significantly higher titers of EBOV neutralizing antibodies at higher vaccine doses. However, oligoarthritis was reported in the second week after injection in 11 of the 51 Geneva trial participants, occasionally accompanied by vesicular dermatitis. The identification of rVSV-ZEBOV in synovial fluid and skin vesicles confirmed viral dissemination and replication in peripheral tissues (15). Only two similar cases of arthritis were observed at other trial sites, which suggests an influence of the vaccine dose, host factors, or reporting and investigative approaches.
After a safety-driven study hold, the Geneva randomized clinical trial resumed at the markedly lower dose of 3 × 105 PFU and the Gabon trials at the same or lower doses—providing a singular opportunity to assess the relative influence of vaccine dose on vaccine safety and immunogenicity in the same patients. Reducing the vaccine dose stemmed acute reactogenicity, but did not prevent arthritis, dermatitis, or cutaneous vasculitis, and also decreased the magnitude of antibody responses (15). Nevertheless, no vaccine-associated severe adverse events were reported in any of the rVSV-ZEBOV phase 1 trials. Hence, the vaccine was selected for further phase 2/3 trials by WHO (Guinea), the U.S. Centers for Disease Control and Prevention (CDC) (Sierra Leone), and the U.S. National Institute of Health (NIH) (Liberia), along with the National Health Authorities in the host countries.
The Guinea trial was conducted by vaccinating all eligible and willing persons with an identified or potential contact with an EBOV-infected person, thus creating a potential protective “ring” to stop the virus from further spreading. The interim analysis included a total population of 7651 people, which was divided in two groups and vaccinated either immediately or after a 21-day delay. Recent results showed that at a high dose (2 × 107 PFU), rVSV-ZEBOV was highly effective: No new cases of EVD were diagnosed in vaccinees from 6 days after vaccination (16).
These promising results call for in-depth studies to assess the induction and duration of immune memory responses and to identify the signatures of immunogenicity and reactogenicity—challenges that the VSV-EBOVAC project aims to address.
Goals: Knowledge and Harmonization
The VSV-EBOVAC project (www.vsv-ebo-vac.eu) is a transdisciplinary, multinational collaboration with a public health–oriented strategy that fills a translational gap in Ebola vaccine R&D and informs rational development of efficacious live vaccines with acceptable safety profiles for other life-threatening infections for which vaccines are not currently available. Supported by the European Commission Innovative Medicines Initiative 2 Joint Undertaking (IMI2 JU), the project brings together 12 leading international vaccine research institutes from six EU countries and the United States, as well as two African clinical sites (tables S1 and S2) and thus contributes to capacity building at the African sites by intimately involving scientists from these institutions and exchanging critical information. Several of the VSV-EBOVAC partners participate in the High Impact FP7 Project on Advanced Immunization Technologies (ADITEC; www.aditecproject.eu), a collaborative research program that involves 42 institution from 12 EU countries and the United States and aims to accelerate the development of new immunization technologies for next-generation human vaccines (17, 18).
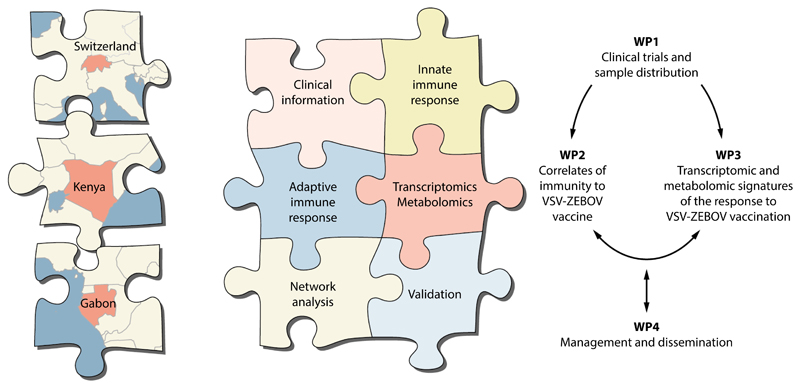
VSV-EBOVAC’s key goal is to comprehensively characterize the molecular signatures of immune responses elicited by the rVSV-ZEBOV vaccine in humans. VSV-EBOVAC thus extends and enriches the dose-escalating phase 1 trials of the rVSV-ZEBOV vaccine conducted in Switzerland, Kenya, and Gabon by harnessing state-of-the-art technologies for systems analyses (transcriptomic and metabolomics profiling) of the human innate and adaptive immune responses to vaccination and by subsequently integrating these data with clinical findings (safety and immunogenicity) (Fig. 1). The project benefits from having access to the clinical samples of subjects who were vaccinated with different doses of the VSV-ZEBOV vaccine and assessed at numerous early and subsequent time points (Table 1). The sharing of clinical samples collected at multiple time points from ~300 participants immunized with rVSV-ZEBOV ensures sufficient power to decipher the influence of numerous demographic determinants, including gender and age, on vaccine safety and immune responses. Systems biology approaches have been used to pinpoint signatures of immunogenicity for only a few human vaccines (19). Integration of multiple layers of information derived from distinct “-omics” analyzed with clinical immunological measures might provide a better understanding of the complex mechanisms of protective immunity induced by vaccines than is possible with only conventional clinical and immunological readouts. For example, systems analyses might identify early gene signatures or other biomarkers predictive of magnitude, quality, and duration of vaccine-induced adaptive immune responses as well as surrogate markers of potential vaccine-induced adverse events. The VSV-EBOVAC project provides an opportunity to study molecular biomarkers of live-vaccine reactogenicity and immunogenicity. Results from this project could inform rational development of new live vaccines for other diseases with acceptable safety and immunogenicity profiles.
Fig. 1. Project plan form and functions.
Shown in schematic form is the VSV-EBOVAC structure of the project plan. Blood samples and clinical data are obtained throughout the study, and clinical, immunological, and -omics data are integrated in order to identify molecular signatures associated with the rVSV-ZEBOV vaccine. The project is overseen by a management team consisting of the project coordinator, the scientific coordinator, and the work-package (WP) leaders. (Inset, right) The project is organized and carried out in four WPs. WP1 extends the clinical trials to 12 months and organizes sample distribution between partners.
Table 1. Clinical trials studied in VSV-EBOVAC.
| Trial reference | Clinical site | Study start date | Vaccine* (PFU) | Number of participants | Visits (days) |
|---|---|---|---|---|---|
| NCT02287480 | Geneva (Switzerland) | November 2014 | 5 × 107† | 16 | (-90, -1) 0, 1, 3, 7, 14, 28, 84, 168 |
| 1 × 107 | 35 | ||||
| 3 × 105‡ | 56 | ||||
| Placebo | 8 | ||||
| NCT02296983 | Kilifi (Kenya) | December 2014 | 3 × 106 | 20 | 0, 1, 3, 7, 14, 28, 60, 90, 180 |
| 1 × 107 | 20 | ||||
| PACTR201411000919191 | Lambaréné (Gabon) | November 2014 | 2 × 107 | 20 | 0, 1, 2, 7, 14, 28, 56, 84, 180 |
| 3 × 106 | 20 | ||||
| 3 × 105 | 20 |
One single administration on Day 0 for each subject.
Arm interrupted on January 2015.
Started on January 2015.
One of the intriguing features of VSV-ZEBOV is that no EVD cases were reported in vaccinees later than 6 days after immunization. This implies that innate or very early adaptive immune responses support viral clearance and control. Given that plasma and blood samples were retrieved from the volunteers of these trials early after vaccination—that is, days 0, 3, 7, and 14—VSV-EBOVAC project offers a distinct opportunity to profile innate and adaptive immune responses induced by the vaccine at these very early time points when the protective response is in play. Such findings could then be bridged with parallel data to be generated from nonhuman primates after VSV-ZEBOV vaccination and ZEBOV challenge for cross validation.
The project represents a critical step forward through harmonization and in-depth integrated analyses of data generated through a variety of clinical, immunological, and molecular readouts—safety, immunogenicity, innate and adaptive immunity, immunological memory, transcriptomics, and metabolomics—and ensures that all information resulting from the ongoing first-in-humans clinical studies is exploited and shared. The results obtained from this project should enhance and accelerate the development of a safe and efficacious vaccine to counter Ebola infection in humans but also could provide a blueprint for the development of other future vaccines. The VSV-EBOVAC project will pursue interactions with other relevant Ebola vaccine efforts to ensure maximum coordination and harmonization, in order to enhance the worldwide capacity to respond swiftly to future EVD outbreaks.
Supplementary Material
Funding
The VSV-EBOVAC project is supported by IMI2 JU (www.imi.europa.eu), under grant agreement no. 115842, within the IMI Ebola+ program launched in response to the EVD outbreak in Western Africa in 2014. IMI2 receives support from the European Union’s Horizon 2020 research and innovation programme and EFPIA. The VSV-EBOVAC is coordinated by the Sclavo Vaccines Association (www.sclavo.org), a nonprofit organization devoted to support research and development of human vaccines. VEBCON trials: The Public Health Agency of Canada donated 800 vials of the rVSV-ZEBOV vaccine to WHO, which created VEBCON to initiate dose-escalation phase 1 clinical trials. These phase 1 trials were initiated in Germany (NCT02283099), Kenya (NCT02296983), Gabon (PACTR2014000089322), and Switzerland (a phase 1/2 randomized, controlled trial NCT02287480) and were supported financially through WHO by a grant from the Wellcome Trust Foundation, the Bill and Melinda Gates Foundation, and the German Center for Infection Research. Phase 2/3 Guinea trial: PACTR201503001057193.
References
- 1.WHO. Ebola Virus Disease. 2015 available at www.who.int/mediacentre/factsheets/fs103/en.
- 2.Dixon MG, Schafer IJ, Centers for Disease Control and Prevention (CDC) Ebola viral disease outbreak—West Africa, 2014. MMWR Morb Mortal Wkly Rep. 2014;63:548–551. [PMC free article] [PubMed] [Google Scholar]
- 3.Van Kerkhove MD, Bento AI, Mills HL, Ferguson NM, Donnelly CA. A review of epidemiological parameters from Ebola outbreaks to inform early public health decision-making. Sci Data. 2015;2 doi: 10.1038/sdata.2015.19. 150019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yan T, Mu J, Qin E, Wang Y, Liu L, Wu D, Jia H, Li Z, Guo T, Wang X, Qin Y, et al. Clinical characteristics of 154 patients suspected of having Ebola virus disease in the Ebola holding center of Jui Government Hospital in Sierra Leone during the 2014 Ebola outbreak. Eur J Clin Microbiol Infect Dis. 2015;34:2089–2095. doi: 10.1007/s10096-015-2457-z. [DOI] [PubMed] [Google Scholar]
- 5.McElroy AK, Akondy RS, Davis CW, Ellebedy AH, Mehta AK, Kraft CS, Lyon GM, Ribner BS, Varkey J, Sidney J, Sette A, et al. Human Ebola virus infection results in substantial immune activation. Proc Natl Acad Sci USA. 2015;112:4719–4724. doi: 10.1073/pnas.1502619112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang ZY, Duckers HJ, Sullivan NJ, Sanchez A, Nabel EG, Nabel GJ. Identification of the Ebola virus glycoprotein as the main viral determinant of vascular cell cytotoxicity and injury. Nat Med. 2000;6:886–889. doi: 10.1038/78645. [DOI] [PubMed] [Google Scholar]
- 7.Garbutt M, Liebscher R, Wahl-Jensen V, Jones S, Möller P, Wagner R, Volchkov V, Klenk HD, Feldmann H, Ströher U. Properties of replication-competent vesicular stomatitis virus vectors expressing glycoproteins of filoviruses and arenaviruses. J Virol. 2004;78:5458–5465. doi: 10.1128/JVI.78.10.5458-5465.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jones SM, Feldmann H, Ströher U, Geisbert JB, Fernando L, Grolla A, Klenk HD, Sullivan NJ, Volch-kov VE, Fritz EA, Daddario KM, et al. Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses. Nat Med. 2005;11:786–790. doi: 10.1038/nm1258. [DOI] [PubMed] [Google Scholar]
- 9.Kanapathipillai R, Henao Restrepo AM, Fast P, Wood D, Dye C, Kieny MP, Moorthy V. Ebola vaccine—An urgent international priority. N Engl J Med. 2014;371:2249–2251. doi: 10.1056/NEJMp1412166. [DOI] [PubMed] [Google Scholar]
- 10.Stanley DA, Honko AN, Asiedu C, Trefry JC, Lau-Kilby AW, Johnson JC, Hensley L, Ammendola V, Abbate A, Grazioli F, Foulds KE, et al. Chimpanzee adenovirus vaccine generates acute and durable protective immunity against ebolavirus challenge. Nat Med. 2014;20:1126–1129. doi: 10.1038/nm.3702. [DOI] [PubMed] [Google Scholar]
- 11.Geisbert TW, Daddario-Dicaprio KM, Lewis MG, Geisbert JB, Grolla A, Leung A, Paragas J, Matthias L, Smith MA, Jones SM, Hensley LE, et al. Vesicular stomatitis virus-based ebola vaccine is well-tolerated and protects immunocompromised nonhuman primates. PLOS Pathog. 2008;4:e1000225. doi: 10.1371/journal.ppat.1000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mire CE, Geisbert JB, Marzi A, Agans KN, Feldmann H, Geisbert TW. Vesicular stomatitis virus-based vaccines protect nonhuman primates against Bundibugyo ebolavirus. PLOS Negl Trop Dis. 2013;7:e2600. doi: 10.1371/journal.pntd.0002600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agnandji ST, Huttner A, Zinser ME, Njuguna P, Dahlke C, Fernandes JF, Yerly S, Dayer JA, Kraehling V, Kasonta R, Adegnika AA, et al. Phase 1 Trials of rVSV Ebola Vaccine in Africa and Europe—Preliminary Report. N Engl J Med. 2015 doi: 10.1056/NEJMoa1502924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Regules JA, Beigel JH, Paolino KM, Voell J, Castellano AR, Muñoz P, Moon JE, Ruck RC, Bennett JW, Twomey PS, Gutiérrez RL, et al. A Recombinant Vesicular Stomatitis Virus Ebola Vaccine—Preliminary Report. N Engl J Med. 2015 doi: 10.1056/NEJMoa1414216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huttner A, Dayer JA, Yerly S, Combescure C, Auderset F, Desmeules J, Eickmann M, Finckh A, Goncalves AR, Hooper JW, Kaya G, et al. The effect of dose on the safety and immunogenicity of the VSV Ebola candidate vaccine: A randomised double-blind, placebo-controlled phase 1/2 trial. Lancet Infect Dis. 2015;15:1156–1166. doi: 10.1016/S1473-3099(15)00154-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Henao-Restrepo AM, Longini IM, Egger M, Dean NE, Edmunds WJ, Camacho A, Carroll MW, Doumbia M, Draguez B, Duraffour S, Enwere G, et al. Efficacy and effectiveness of an rVSV-vectored vaccine expressing Ebola surface glycoprotein: Interim results from the Guinea ring vaccination cluster-randomised trial. Lancet. 2015;386:857–866. doi: 10.1016/S0140-6736(15)61117-5. [DOI] [PubMed] [Google Scholar]
- 17.Rappuoli R, Medaglini D. Big science for vaccine development. Vaccine. 2014;32:4705–4707. doi: 10.1016/j.vaccine.2014.06.071. [DOI] [PubMed] [Google Scholar]
- 18.Rappuoli R, Medaglini D. ADITEC: Joining forces for next-generation vaccines. Sci Transl Med. 2012;4 doi: 10.1126/scitranslmed.3003826. 128cm4. [DOI] [PubMed] [Google Scholar]
- 19.Hagan T, Nakaya HI, Subramaniam S, Pulendran B. Systems vaccinology: Enabling rational vaccine design with systems biological approaches. Vaccine. 2015;33:5294–5301. doi: 10.1016/j.vaccine.2015.03.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.