Abstract
Purpose
This study aims to describe and characterize the spatial and temporal clustering patterns of suicide in the ten states with the greatest suicide burden in the United States from 1999 to 2016.
Methods
All suicide deaths from January 1, 1999 to December 31, 2016 in the United States were identified using data from the Wide-ranging Online Data for Epidemiologic Research (WONDER) dataset. The ten states with the highest age-adjusted suicide rates were Montana, Alaska, Wyoming, New Mexico, Nevada, Utah, Idaho, Colorado, Arizona, and Oklahoma. A spatiotemporal scan statistic using a discrete Poisson model was employed to retrospectively detect spatiotemporal suicide clusters.
Results
From 1999 to 2016, a total of 649,843 suicides were recorded in the United States. Nineteen statistically significant spatiotemporal suicide mortality clusters were identified in the states with the greatest suicide rates, and 13.53% of the suicide cases within these states clustered spatiotemporally. The risk ratio of the clusters ranged from 1.45 to 3.64 (p < 0.001). All states had at least one cluster, with three clusters spanning multiple states, and four clusters were found in Arizona. While there was no clear secular trend in the average size of suicide clusters, the number of clusters increased from 1999 to 2016.
Conclusions
Hot spots for suicidal behavior in the United States warrant public health intervention and continued surveillance. As suicide rates in the US continue to increase annually, public health efforts could be maximized by focusing on regions with substantial clustering.
Keywords: Suicide, Suicide clusters, Epidemiology, Spatial statistics, Cluster analysis
Introduction
Suicide in the United States has increased by an average of 25.4% from 1999 to 2016 [1], and is currently the tenth leading cause of mortality overall and the second leading cause of mortality among youth and young adults [2]. Risk factors for suicide death include previous suicide attempts, psychiatric and substance abuse disorders, as well as adverse and stressful life events and family history of psychiatric disorders and suicide [3, 4]. Further, those who complete suicide are more likely to be male, and use a lethal means of death such as a firearm [5]. Additional demographic risk factors include being non-Hispanic White or Native American [3], as well as being an adolescent or older adult [3]. It is also well established that suicide spatially and temporally correlates; however, relatively little has been done to examine suicide clusters across space and time in the United States during the past decade, a time period in which suicide has increased. Previous studies have shown that suicide clusters represent about 5–10% of suicides, and clustering has been found to be especially prevalent among adolescents and young adults [6–8].
Two main kinds of suicide clusters exist: mass and point clusters. More research has been conducted on mass clusters, which are suicide clusters that aggregate in time following, for example, media reports on suicide [9, 10]. Studies have demonstrated that suicide rates rise after increased media reporting on suicide, with a corresponding greater increase in suicide rates with increased coverage [11]. Recent evidence indicates an excess of 1841 suicides (9.85%) in the United States in the months following the death of Robin Williams [12]. On the other hand, point clusters, or spatiotemporal clusters that are localized in both geographic space and time, are less understood [13].
To our knowledge, no recent large-scale epidemiological study of spatiotemporal suicide clusters across multiple states or the national population in the United States has been conducted, despite an unprecedented suicide rate increase of over 25%. In the past 6 years, a few smaller studies using spatiotemporal cluster analysis methods have been carried out in the United States; however, all these studies examined clusters within one state. Additionally, most studies have examined spatial clusters, which are geographic areas with high or low suicide rates relative to other regions, as opposed to spatiotemporal clusters which are identified across both space and time [14–16].
Several social and psychological mechanisms have been suggested to contribute to the formation of spatiotemporal clusters of suicide. Environmental factors such as sunlight, seasonality, and altitude contribute to suicidal behavior and underlie some degree of spatial correlation [17–19]; further, clustering of socio-economic deprivation and marginalization [20–22], as well as greater local person-to-person transmission of suicidal thoughts and behavior also contribute [13, 23]. Local transmission can occur through imitation, suggestion, social learning, and assortative relating [23]. More sophisticated statistical methods and techniques, such as methods derived from geographical information systems and spatial epidemiology, may be able to detect significant clustering effects during surveillance. Such detection of suicide clusters is essential for effective prevention of suicides and may allow medical professionals and policymakers to identify potential high-risk areas and intervene to prevent suicide deaths and injuries from attempted suicide.
This study aims to fill in gaps in the current literature on spatiotemporal suicide clustering in the United States. First, we examined demographic and county-level differences in overall suicide mortality in the United States. Second, we examined spatiotemporal clustering from 2009 through 2016 within the ten states in the United States with the highest suicide burden. We focused on states with the highest burden to determine whether suicide cluster analysis would generate additional information that can inform suicide prevention and monitoring efforts. Third, we estimated temporal trends in the number of clusters identified in the United States, as well as the size of (i.e., number of cases within) the clusters. Lastly, we assessed whether there were any significant demographic differences between the counties included and not included in the suicide clusters.
Methods
Data source
Suicide count and age-adjusted suicide rates (from January 2009 to December 2016) were obtained from the Centers for Disease Control and Prevention Wide-ranging Online Data for Epidemiologic Research (CDC WONDER). The CDC WONDER Underlying Cause of Death database contains mortality and population counts for all US counties. The data are based on death certificates for US residents. Each death certificate identifies a single underlying cause of death and demographic data. During the study period, changes to county boundaries may have occurred, including the wholesale addition or deletion of counties. Additional information on the WONDER database is described elsewhere [24]. County-level demographic characteristics were obtained from the US Census Bureau 2010 Profile of General Population and Housing Characteristics (DP-1) [25]. The data are publicly available, de-identified, and were deemed to be without human subjects risk by the Columbia University institutional review board.
Study population and case ascertainment
All suicide deaths identified through WONDER database were included in the study. Suicides in WONDER were selected if they endorsed any one of the following ICD-10 codes: U03 Terrorism intentional—Suicide (n = 4), X60–X84 Intentional self-harm (n = 648,635), and Y87.0 Sequelae of intentional self-harm (n = 1204). In WONDER, deaths in 1999 and beyond were classified using ICD-10; however, category U03 was added in 2001.
Statistical analysis
We began by estimating suicide rates by state across all 50 states. Age-adjusted mortality rates (number of deaths/100,000 persons) were calculated by age, gender, census division, state, and county for the years 1999–2016. We used the midyear 2000 US standard population to estimate age-adjusted rates and account for changes in the age distribution of the population over time. Descriptive statistics were used to characterize the sample demographics and describe trends and variations in suicides across different demographic groups.
We then focused the cluster analysis on the ten states with the highest age-adjusted suicide rates over the study period (Montana, Alaska, Wyoming, New Mexico, Nevada, Utah, Idaho, Colorado, Arizona, and Oklahoma). Spatiotemporal clusters of suicides in these ten states were retrospectively assessed using cluster analysis with the spatiotemporal SaTScan v.9.4.4 program [26]. Due to WONDER data suppression for sparse cells, we used completed suicide information aggregated every 6 months, which was the most granular time scale without substantial county-level data suppression. The ten states with the highest age-adjusted suicide rate were selected for the cluster analysis, as this also limited the overall amount of data suppression: 65.3% of suicides were not suppressed and remained available for analysis. In contrast, this percentage dropped to 61.9% and 55.2% for the top 15 and 20 states, respectively. SaTScan is commonly used in infectious disease cluster analysis, but has also been previously used in the identification of suicide clusters [27, 28], typically in a specific geographic region or institutional setting within the US, or in population-level analysis in other countries [27, 29–31]. We define a suicide spatiotemporal cluster as a group of suicides that occur (based on place of residence) closer together in space and time than would be expected by chance.
A spatiotemporal scan statistic was obtained using a cylindrical scan window that is moved through space and time, and each window reflects a possible cluster. A discrete Poisson model was used, and the likelihood of each possible cluster was assessed using Monte Carlo simulations. A likelihood ratio test was used to compare the risk of suicides within the scan relative to outside the scan. Statistical significance was reached when a higher than expected risk within the scan window was found compared to the outside. Because the scan window uses longitude and latitude to assess for clusters in the spatial dimension, changes in county boundaries during the study period did not affect the cluster analysis.
Previous research has shown that the time period during which suicide clusters are expected to occur ranges from 24 h to 5 years [32]; our study focus was point clusters more localized in space and time, thus the maximum temporal cluster size was a priori set to 15% of the study period or around 2.5 years, and the minimum temporal cluster size was set to 12 months. The maximum proportion of the population that a cluster could contain was a priori set at 10% of the study population. We then compared the cluster analysis results with state-level, county-level, and group-specific descriptive statistics to evaluate which additional distinct information could be gleaned from the spatiotemporal cluster analysis. Subsequently, we linked these counties with county-level demographic information (age, sex, race, and ethnicity) from the US Census Bureau to determine whether associations exist between these characteristics and suicide clustering.
Further, we stratified the study period into 3-year increments to test whether there was a trend over time in the number and size of suicide clusters, while accounting for overall increasing suicide rates. Because the analysis was conducted on 3-year segments, the maximum temporal cluster size was set to 1.5 years and the minimum temporal cluster size was set to 6 months. This stratified cluster analysis determines clusters relative to the cases and population size within the 3-year time period of interest and yields different clusters. Therefore, the total number of clusters in the overall time period (1999–2016) is not expected to equal the sum of the clusters within each 3-year period. Additionally, we identified purely spatial clusters in the data, and compared whether these spatial clusters overlapped with the spatiotemporal clusters.
All analyses, except the cluster analysis, were conducted in R version 3.4.1 [33]. The geocode function of the ggmap package of R determined each county’s geocoordinates using Google Map APIs. The spatiotemporal cluster analysis was conducted in the spatiotemporal SaTScan v.9.4.4 program [26].
Results
Age-adjusted suicide death rates by gender, age group, and census division
In the United States, 649,843 deaths due to suicide were recorded between 1999 and 2016. The overall age-adjusted suicide rate was 11.74/100,000 persons (95% CI 11.71–11.77). The suicide rate (per 100,000 persons) was highest for those in the 85 + age group (18.07, 95% CI 17.79–18.34), males (19.26, 95% CI 19.20–19.31), and the Mountain State census division (18.06, 95% CI 17.92–18.19) (Table 1). Males were almost four times more likely than females to die from suicide (3.84, 95% CI 3.82–3.87). Furthermore, the rate of suicide mortality increased within the study period; the age-adjusted death rate during 2016 was 1.29 times (95% CI 1.27–1.31) the age-adjusted death rate in 1999.
Table 1.
Characteristics of suicides in the United States, January 1999 to December 2016
| Characteristic | 1999–2004 |
2005–2010 |
2011–2016 |
Overall |
||||
|---|---|---|---|---|---|---|---|---|
| No. | Age-adjusted rate | No. | Age-adjusted rate | No. | Age-adjusted rate | No. | Age-adjusted rate | |
| Total | 184,749 | 10.74 | 211,843 | 11.45 | 253,251 | 12.88 | 649,843 | 11.75 |
| Age group | ||||||||
| 5–14 years | 1629 | 0.66 | 1436 | 0.59 | 2277 | 0.92 | 5337 | 0.72 |
| 15–24 | 24,180 | 9.98 | 25,810 | 9.96 | 30,876 | 11.74 | 80,866 | 10.58 |
| 25–34 | 30,153 | 12.70 | 31,608 | 13.15 | 39,551 | 15.25 | 101,312 | 13.75 |
| 35–44 | 39,754 | 14.84 | 39,814 | 15.66 | 40,589 | 16.69 | 120,157 | 15.70 |
| 45–54 | 36,155 | 15.31 | 47,879 | 18.13 | 52,303 | 19.95 | 136,337 | 17.88 |
| 55–64 | 20,630 | 13.13 | 31,519 | 15.62 | 43,622 | 18.30 | 95,771 | 16.03 |
| 65–74 | 14,272 | 12.89 | 15,859 | 13.08 | 23,059 | 14.95 | 53,190 | 13.77 |
| 75–84 | 13,084 | 17.25 | 12,617 | 16.09 | 14,180 | 17.35 | 39,881 | 16.90 |
| 85 + | 4826 | 18.50 | 5255 | 17.14 | 6763 | 18.53 | 16,844 | 18.07 |
| Gender | ||||||||
| Female | 36,823 | 4.21 | 44,543 | 4.70 | 56,530 | 5.66 | 137,769 | 4.98 |
| Male | 147,926 | 18.08 | 167,300 | 18.83 | 196,721 | 20.64 | 511,947 | 19.16 |
| Census division | ||||||||
| New England | 7023 | 8.11 | 8138 | 9.03 | 9900 | 10.60 | 25,061 | 9.28 |
| Middle Atlantic | 18,612 | 7.62 | 20,900 | 8.27 | 25,328 | 9.68 | 64,840 | 8.56 |
| East North Central | 27,631 | 10.12 | 30,896 | 10.97 | 35,838 | 12.49 | 94,365 | 11.21 |
| West North Central | 13,148 | 11.26 | 15,055 | 12.34 | 18,495 | 14.60 | 46,698 | 12.78 |
| South Atlantic | 37,430 | 11.54 | 42,893 | 11.88 | 51,020 | 13.00 | 131,343 | 12.20 |
| East South Central | 12,803 | 12.36 | 15,017 | 13.64 | 17,232 | 14.93 | 45,052 | 13.69 |
| West South Central | 21,392 | 11.39 | 24,385 | 11.78 | 30,423 | 13.33 | 76,200 | 12.24 |
| Mountain | 18,382 | 16.67 | 22,158 | 17.51 | 27,359 | 19.64 | 67,899 | 18.05 |
| Pacific | 28,222 | 10.46 | 32,305 | 10.93 | 37,625 | 11.73 | 98,152 | 11.09 |
County-level age-adjusted suicide death rates within age groups and states
When examined within the same age groups and states, there were variations in suicide rates among counties, particularly within the 15–24 and 25–34 age groups. The overall age-adjusted suicide mortality rate (per 100,000 persons) among the 15–24 age group was 10.58 (95% CI 10.51–10.65), which was the second lowest death rate among the age groups. However, a county in Alaska, one in South Dakota, and another in Alaska had age-adjusted death rates (per 100,000 persons) of 254.67 (95% CI 197.36–323.42), 206.08 (95% CI 132.04–306.63), and 196.14 (95% CI 147.76–255.31) among that age group, respectively. These mortality rates were 24.07, 19.48, and 18.54 times the overall age-adjusted death rate among the 15–24 age group.
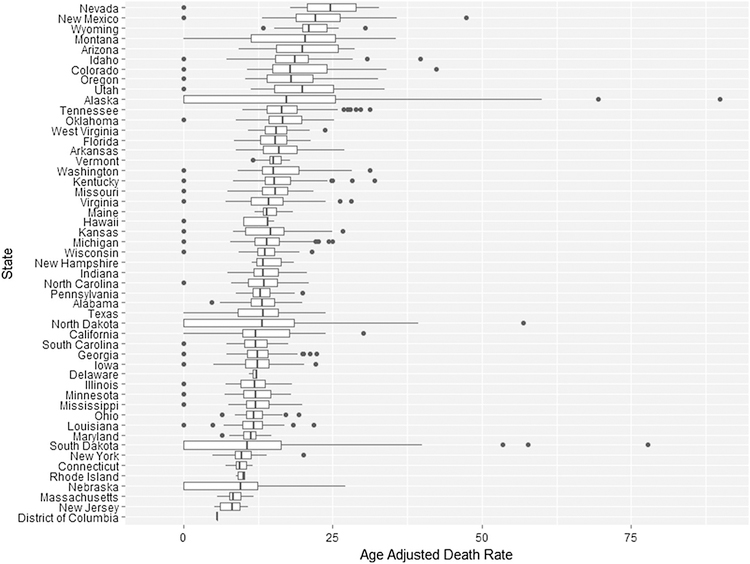
Furthermore, increased suicide mortality rates in certain counties were observed when county-level rates were examined by state, particularly in Alaska, South Dakota, and North Dakota. Figure 1 presents box and whiskers plots of county age-adjusted suicide rates stratified by state, where counties with suicide rates greater than 1.5 times the interquartile range are outliers (marked as dots). These outliers represent counties with much greater or less than average age-adjusted suicide rates throughout the study period. The age-adjusted death rate (per 100,000 persons) in a county in Alaska (89.86, 95% CI 73.35–106.36), a county in South Dakota (77.83, 95% CI 50.84–114.05), a second county in Alaska (69.52, 95% CI 56.75–82.30), a third county in Alaska (60.08, 95% CI 47.79–74.58), and a county in North Dakota (56.96, 95% CI 41.22–76.72) were 7.65, 6.63, 5.92, 5.12, and 4.85 times the overall age-adjusted death rate of 11.74 (95% CI 11.71–11.77) in the study sample (Fig. 1). There was less variation when county death rates were stratified by year and gender; there were no counties with mortality rates significantly higher relative to the stratified death rate by year and gender group.
Fig. 1.
County-level age-adjusted suicide death rates (per 100,000 persons) by state
Cluster analysis
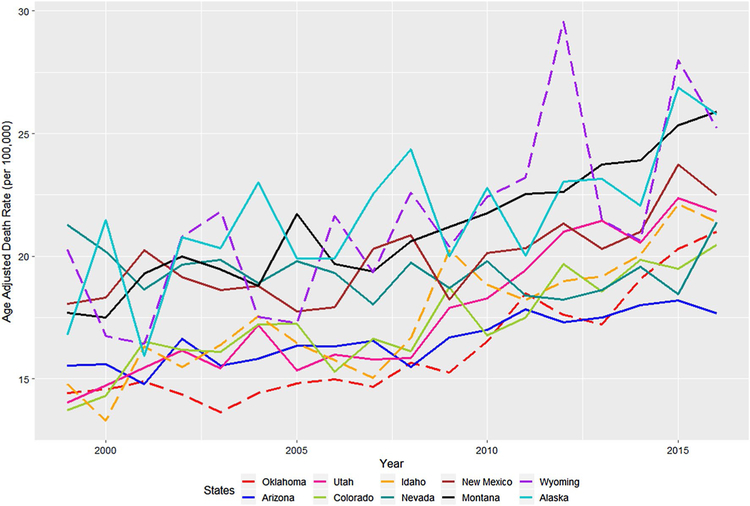
The Mountain Census Division had the greatest overall age-adjusted suicide rate during 1999–2016, and eight out of the ten states with the highest rate of suicides were included in this Census Division. The states with the greatest overall age-adjusted suicide mortality rates (per 100,000 persons) for all the study years were Montana (21.26, 95% CI 20.57–21.95), Alaska (21.65, 95% CI 20.80–22.49), Wyoming (21.49, 95% CI 20.56–22.42), New Mexico (19.95, 95% CI 19.48–20.42), Nevada (19.32, 95% CI 18.92–19.73), Utah (18.02, 95% CI 17.61–18.43), Idaho (17.73, 95% CI 17.22–18.25), Colorado (17.39, 95% CI 17.11–17.67), Arizona (16.70, 95% CI 16.46–16.95), and Oklahoma (16.33, 95% CI 16.01–16.64). Figure 2 shows the age-adjusted suicide rates by year among these states from 1999 to 2016.
Fig. 2.
Suicide rates over time in states with the greatest mortality burden
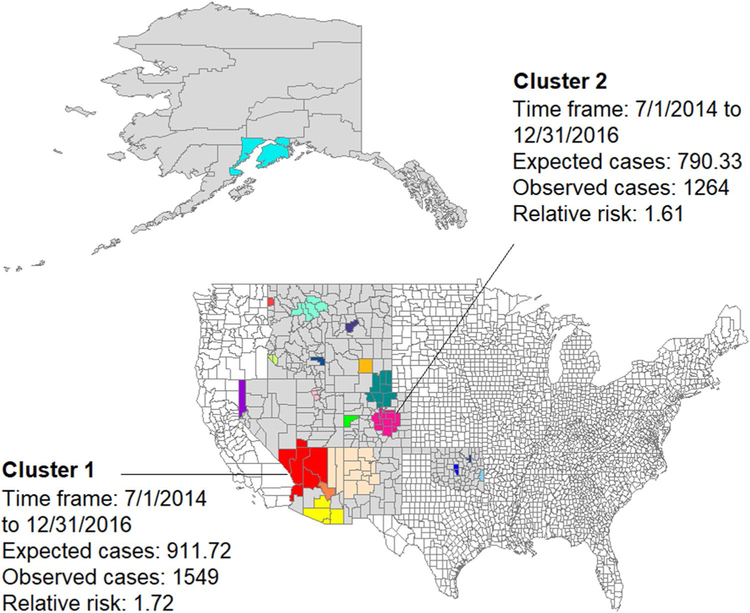
Spatiotemporal analysis was conducted among counties within the states with the highest age-adjusted suicide rates. We found 19 statistically significant spatiotemporal clusters. The rate of suicide in the counties where the clusters occurred was up to 3.64 times higher than in areas outside the clusters, and the risk ratio ranged from 1.45 to 3.64 (p < 0.001). Four clusters were found in Arizona, three each in Idaho, Colorado, and Oklahoma, two in Nevada, Wyoming, Utah, and Montana, and one each in New Mexico and Alaska. There were three clusters that spanned multiple states (Table 2).
Table 2.
Spatiotemporal suicide cluster characteristics
| State | No. of Counties | Observed cases | Expected cases | RR | p value | Dates | |
|---|---|---|---|---|---|---|---|
| 1 | Arizona, Nevada and Utah | 6 | 1549 | 911.72 | 1.72 | < 0.001 | 7/1/2014–12/31/2016 |
| 2 | Colorado | 11 | 1264 | 790.33 | 1.61 | < 0.001 | 7/1/2014–12/31/2016 |
| 3 | Utah | 3 | 913 | 537.69 | 1.71 | < 0.001 | 7/1/2014–12/31/2016 |
| 4 | New Mexico and Arizona | 14 | 761 | 487.17 | 1.57 | < 0.001 | 7/1/2014–12/31/2016 |
| 5 | Arizona | 4 | 730 | 502.87 | 1.46 | < 0.001 | 1/1/2014–6/30/2016 |
| 6 | Wyoming and Colorado | 8 | 537 | 350.04 | 1.54 | < 0.001 | 7/1/2014–12/31/2016 |
| 7 | Nevada | 1 | 265 | 142.48 | 1.86 | < 0.001 | 7/1/2014–12/31/2016 |
| 8 | Colorado | 1 | 118 | 46.6 | 2.54 | < 0.001 | 1/1/2011–6/30/2013 |
| 9 | Alaska | 2 | 212 | 112.85 | 1.88 | < 0.001 | 7/1/2014–12/31/2016 |
| 10 | Oklahoma | 1 | 321 | 201.37 | 1.6 | < 0.001 | 1/1/2014–6/30/2016 |
| 11 | Oklahoma | 2 | 483 | 334.34 | 1.45 | < 0.001 | 7/1/2014–12/31/2016 |
| 12 | Idaho | 2 | 255 | 164.7 | 1.55 | < 0.001 | 1/1/2015–12/31/2016 |
| 13 | Montana | 5 | 122 | 68.68 | 1.78 | < 0.001 | 7/1/2011–6/30/2013 |
| 14 | Montana | 1 | 95 | 49.95 | 1.9 | < 0.001 | 7/1/2014–12/31/2016 |
| 15 | Idaho | 1 | 75 | 37.85 | 1.98 | < 0.001 | 1/1/2014–12/31/2015 |
| 16 | Wyoming | 1 | 49 | 20.69 | 2.37 | < 0.001 | 1/1/2014–12/31/2015 |
| 17 | Oklahoma | 1 | 23 | 6.31 | 3.64 | < 0.001 | 7/1/2015–6/30/2016 |
| 18 | Arizona | 1 | 22 | 6.72 | 3.27 | < 0.001 | 7/1/2014–6/30/2015 |
| 19 | Idaho | 1 | 56 | 28.03 | 2 | < 0.001 | 7/1/2014–6/30/2016 |
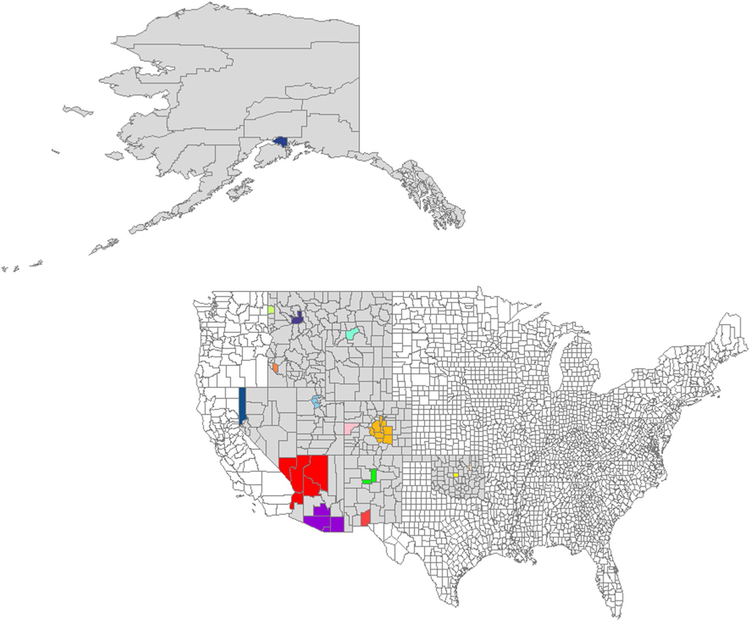
In total, 7850 suicides (13.53%) within these ten states clustered spatiotemporally, with the lowest percentage of clustered deaths in Montana (2.85%) and the highest in New Mexico (50.50%). Additionally, 66 counties (17.05%) within these ten states were included in the space–time clusters, with the lowest proportion of counties in Alaska (2 out of 32 counties, 6.25%) and the highest in Arizona (11 out of 15 counties, 73.33%). Figure 3 shows the map of the spatiotemporal clusters. We also conducted cluster analysis to detect purely spatial clusters; 15 clusters were found: 2 spatial clusters each were found in Arizona, Colorado, Idaho, Montana, New Mexico, and Oklahoma, and 1 cluster was detected in Kansas, Nevada, and Utah. There were no spatial clusters found in Wyoming, and none of the identified clusters spanned multiple states (Table 3 in Appendix). There was substantial overlap between spatial and spatiotemporal clusters; of 35 counties included in the spatial clusters, only 4 were not in the spatiotemporal clusters. On the other hand, 16 counties were included in the spatiotemporal clusters but not the spatial clusters. Figure 4 in Appendix provides a map of the clusters.
Fig. 3.
Graphical representation of 19 suicide spatiotemporal clusters within the 10 states with the greatest age-adjusted suicide rates. Each color represents a different cluster
Table 3.
Spatial suicide cluster characteristics
| State | No. of counties | Observed cases | Expected cases | RR | p value | |
|---|---|---|---|---|---|---|
| 1 | Arizona | 5 | 8389 | 5364.28 | 1.66 | < 0.001 |
| 2 | Colorado | 10 | 6684 | 5136.49 | 1.34 | < 0.001 |
| 3 | Utah | 3 | 4663 | 3440 | 1.39 | < 0.001 |
| 4 | New Mexico | 3 | 2678 | 1799.08 | 1.51 | < 0.001 |
| 5 | Nevada | 1 | 1531 | 918.26 | 1.69 | < 0.001 |
| 6 | Arizona | 4 | 4254 | 3230.98 | 1.34 | < 0.001 |
| 7 | Colorado | 1 | 575 | 311.99 | 1.85 | < 0.001 |
| 8 | Oklahoma | 1 | 1825 | 1352.36 | 1.36 | < 0.001 |
| 9 | Oklahoma | 1 | 2019 | 1618.68 | 1.26 | < 0.001 |
| 10 | Alaska | 1 | 895 | 644.8 | 1.39 | < 0.001 |
| 11 | Idaho | 1 | 1031 | 849.29 | 1.22 | < 0.001 |
| 12 | Idaho | 1 | 408 | 299.77 | 1.36 | < 0.001 |
| 13 | Montana | 1 | 426 | 326.72 | 1.31 | < 0.001 |
| 14 | Montana | 1 | 321 | 241.37 | 1.33 | < 0.001 |
| 15 | New Mexico | 1 | 533 | 450.48 | 1.18 | < 0.001 |
Fig. 4.
Graphical representation of 15 suicide spatial clusters within the 10 states with the greatest age-adjusted suicide rate. Each color represents a different cluster
Association between county-level demographic data and suicide clusters
Significant associations were found between county-level demographic characteristics (age group, race, and ethnicity) and suicide clustering. The percentages of 15–24 years old (13.50% vs 12.37%, p < 0.01) and 25–34 years old (12.51% vs 11.75%, p = 0.026) among the cluster counties were greater than in the counties not included in the clusters. In contrast, the percentages of older adults 45–54 years old (14.38% vs 15.07%, p < 0.01), 75–84 (4.29% vs 4.78%, p = 0.012), and above 85 (1.53% vs 1.84%, p < 0.0001) within cluster counties were less than in remaining counties. For counties in suicide clusters compared to the non-cluster counties, significant differences were also noted in the percentage of Native Hawaiians and other Pacific Islander (19.22% vs. 10.26%, p = 0.017), other race (6.04% vs 4.52%, p = 0.025), and Hispanic ethnicity (16.68% vs. 12.59%, p = 0.032).
Temporal trends in number and size of suicide clusters
We also stratified the study period into 3-year increments to test whether there was a trend over time in the number and size of suicide clusters, while accounting for the overall increasing suicide rate. The number of spatiotemporal clusters varied across the study period; overall, the number of clusters observed across the study period increased by greater than 50% between the first and last 3 years of the study, 1999–2001 and 2014–2016. During the first 3 years of the study, 15 spatiotemporal clusters were found, with an average cluster size of 168.8 people. The number of clusters increased to 20, 21, 20, and 23 in the next five 3-year time periods and to 24 during the final 3 years. On the other hand, there was no trend in the average size of identified suicide spatiotemporal clusters.
Discussion
We investigated the spatiotemporal distribution of suicides in the United States, with a focus on the ten states with the highest age-adjusted rate of suicides between 1999 and 2016. The results demonstrate that a considerable number of suicides cluster in space and time, and that spatiotemporal cluster analysis contributes valuable information to the surveillance of suicides beyond general state-level trends. Monthly state-level time series plots are unable to account for the spatiotemporal suicide clusters identified in cluster analysis. Based on our findings, suicide prevention efforts that focus on geographic areas with high suicide risk, in addition to individual risk factors, may achieve greater public health benefits than focusing on individual risk factors alone.
Sub-state-level heterogeneity in suicide death rates and clustering was evident in the WONDER record. These deviations from state-level rates produced some interesting findings. For example, some counties with significantly higher suicide rates, such as several counties in Alaska, did not provide evidence of suicide clustering; whereas other counties with extremely high suicide rates were found in South Dakota and North Dakota, which are states with the 13th and 21st highest state-level suicide rates in the United States (Fig. 1). This finding adds evidence to the inadequacy of aggregated state-level, county-level, or group-specific rates to assess suicide patterns, and points to the need to identify clusters in space and time with few predetermined boundaries. Clusters may represent locations that have the greatest need for targeted interventions and suicide prevention strategies. Additional studies are needed to identify suicide clusters given the finding here that cluster numbers have increased since 1999. The increase in number of suicide clusters in the United States demonstrates greater spatiotemporal suicide rate heterogeneity in recent years. This trend represents a greater than expected increase in suicide rates in specific counties and should be examined further in future studies.
Our results demonstrate that some county-level demographic features associated with suicide clusters are similar to previously reported individual-level demographic correlates for suicide. The positive associations of Native Hawaiians and other Pacific Islander [34] and other race [34] with suicide have been previously demonstrated; our results indicate that areas with cluster suicides have a higher concentration of individuals with such demographic risk factors. Additionally, previous research has reported disproportionately high rates of suicides among American Indians and Alaskan Natives [35, 36]; suicide clusters in the current study, however, do not have higher concentrations of American Indians and Alaskan Natives. Published research on Hispanic ethnicity and suicide in the United States are inconsistent [37], but our findings identify higher concentrations of Hispanic ethnicity in areas with suicide clusters. Relationships between age groups at risk for completed suicide versus counties with different concentrations of various older and younger adults are also heterogenous. In sum, while some individual-level risk factors for suicide demonstrate similar aggregate relationships with suicide clusters, many do not. However, area-level factors are a different unit of analysis than individual-level factors, with different potential mechanisms for influencing suicide clusters versus individual risk of suicide. Further studies examining these multi-level ecological and individual-level effects simultaneously would allow for more rigorous disentanglement of individual and ecological risks.
There are several strengths in this study. To our knowledge, this is the first epidemiological study that has applied spatiotemporal scan statistics to county-level data from multiple states in the US in the last decade. The examination of recent suicide trends and clustering is extremely valuable given that suicide rates have increased considerably in the US, and half of states had an increase of more than 30% [1]. Consistent with previous research in similar large-scale studies in other countries, our findings show the potential of suicides to cluster in space and time. We also found considerable overlap between spatial and spatiotemporal clusters; in situations where longitudinal suicide data are unavailable, cross-sectional data could instead be used to detect spatial clusters amenable to geographically targeted interventions. An additional strength of the study is the comparison of the cluster analysis to descriptive statistics, which has not been examined before. This feature allowed explicit examination of the unique information each approach adds to the surveillance of suicide clusters. This study also illustrates the potential of leveraging publicly available epidemiologic datasets that are conventionally not used for spatial analysis.
Spatiotemporal clusters were also found in recent studies in Australia [29, 30], Brazil [31], United Kingdom [27], and Spain [28]. The inherent propensity of suicides to cluster in both space and time adds further credibility to the notion that the clustering effect is not only due to area or group characteristics, but rather that temporally varying social and psychological mechanisms may underlie the formation of these spatiotemporal clusters. Indeed, by detecting spatiotemporal suicide clusters rather than purely spatial ones, the present study provides greater evidence for complex and poorly understood suicide cluster mechanisms [29]. Such mechanisms might suggest a transmission effect; however, it is important to note that the size of the clusters identified here are much larger than the typical cluster sizes associated with direct transmission of suicidal behaviors. This larger size may be due to the county-level spatial resolution of the WONDER data, which is likely not granular enough to characterize smaller clusters that are socially transmitted. The large geographic area of some counties in the cluster analysis could also have obscured smaller clusters, and future studies with smaller geographic units of analysis are needed. Moreover, both risk (media coverage) and protective (prevention program) factors associated with suicide clustering need to be further examined to link data at geographic scales with individual-level data on suicide decedents. The demographics and topology of the cluster areas identified here suggest a variety of other possible underlying mechanisms may also play a role, including deprivation and isolation, such as might occur in rural areas of Alaska, as well as potential environmental factors, such as altitude and weather. Public health efforts to reduce suicide in these high burden areas should therefore take account of the social and environmental dynamics of the local areas in which high suicide rates are observed.
One of the main limitations of the present study was the data suppression in the WONDER dataset. An aim of the study was to conduct cluster analysis at the county level and at a granular time scale; however, WONDER data from counties with less than 10 reported suicides within a given time interval are suppressed. Consequently, steps were taken to limit the effects of this data suppression. Six months was the most granular time scale employed, and the ten states with the highest age-adjusted suicide mortality rates were selected for analysis as data suppression was less substantial in these states. Moreover, our findings are only generalizable to the ten states included in the study, since clusters in high rate areas may be very different from those in low rate areas. Given that the identification of suicide clusters provides vital information to inform the allocation of resources for suicide prevention and monitoring efforts, future spatiotemporal cluster analysis needs to be conducted in all states, regardless of suicide rates and without any data suppression.
Another possible limitation is the potential erroneous identification of cause of death. Depending on state law, death investigations are conducted by either a coroner system or a medical examiner system organized at the state, district, or county level. In coroner systems, coroners generally do not need to be physicians, whereas medical examiners are usually required to be physicians and often pathologists [38, 39]. States included in the cluster analysis employ different death investigation systems: Alaska, New Mexico, Utah, Oklahoma, and Montana utilize state medical examiners; in addition, Montana also has county coroners. In contrast, Nevada, Idaho, Wyoming, and Colorado have county-based coroners, and Arizona has county medical examiners [40]. The differences in these systems both at the state and county level could potentially introduce differential bias among states or counties, which could affect the results of the cluster analysis. To the extent that suicide deaths are generally undercounted or misclassified as unintentional deaths, we would anticipate that the number of clusters and cluster sizes would be greater than what is reported in our analysis. Lastly, another possible limitation is that our analysis only examines clustering in space and time, and we are only able to count suicides where the decedent resides, not other areas in which he/she interacts. We were not able to observe cases linked by anything other than time and space such as social networks (e.g., close loved one dying from a different state).
Given that suicides cluster in space and time, coupled with the overall increase in suicides in the US, there is great need for effective interventions to prevent suicide clustering. Previous research on suicide mass clusters found that media portrayals of suicide play a role in the formation of clusters [6], and this finding may also extend to spatiotemporal clusters. The media depiction of suicides—more specifically local sources in the case of spatiotemporal clusters—needs to adhere to appropriate guidelines to minimize subsequent suicides [10, 41]. Further, the advent of social media and new electronic media requires additional research to assess the impact of the transmission of information regarding completed suicides within one’s social network [10, 42]. In the wake of a death by suicide of someone in the community or a suicide that receives media attention, additional resources need to be allocated to postvention efforts with vulnerable groups, as it has been suggested that this may contain the effects of suicide contagion [43, 44]. Further research needs to examine the risk factors that lead to the formation of suicide clusters, with the goal of implementing multifactorial suicide prevention and postvention strategies. A 2016 systematic review found that there are numerous effective methods for prevention of suicidal behavior, such as psychotherapy, pharmacological interventions, and community and family-based interventions. A tailored approach using a combination of evidence-based strategies at both the individual and population level would be most effective for each risk group [45]. Additionally, screening for suicide risk is useful for identifying individuals with high susceptibility to suicide contagion [46].
Our work adds to the body of evidence demonstrating the tendency of suicides to cluster spatiotemporally. Studies utilizing aggregated state-level or group-specific statistics alone are inadequate for examining trends in suicides and miss an essential epidemiological component of suicidality that can assist in the identification of regions of increased suicidal risk. The identification of these clusters is crucial to perform targeted interventions and inform public policy decisions. Future studies need to integrate spatial analysis in the epidemiological investigation of suicides at granular spatial and temporal scales.
Acknowledgements
Support for this work was provided by the National Institute of Alcohol Abuse and Alcoholism (K01AA021511, Keyes), the Center for Injury Epidemiology and Prevention at Columbia University, and the National Institute of General Medical Science (R01GM110748, Shaman).
Appendix
Footnotes
Conflict of interest JS and Columbia University disclose partial ownership of SK Analytics. SK has consulted for SK Analytics. The other authors report no conflicts of interest and have no financial relationships with commercial interests.
References
- 1.Centers for Disease Control and Prevention (2018) Suicide rates rising across the US. Vital signs morbidity and mortality weekly report, June 2018 https://www.cdc.gov/vitalsigns/pdf/vs-0618-suicide-H.pdf. Accessed 19 May 2018
- 2.National Center for Health S (2017) Health, United States. In: Health, United States, 2016: With Chartbook on Long-term Trends in Health National Center for Health Statistics (US), Hyattsville (MD) [PubMed] [Google Scholar]
- 3.Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S (2008) Suicide and suicidal behavior. Epidemiol Rev 30:133–154. 10.1093/epirev/mxn002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krug EG, Mercy JA, Dahlberg LL, Zwi A (2002) World report on violence and health World Health Organization, Geneva [Google Scholar]
- 5.Denning DG, Conwell Y, King D, Cox C (2000) Method choice, intent, and gender in completed suicide. Suicide Life Threat Behav 30(3):282–288 [PubMed] [Google Scholar]
- 6.Gould MS, Kleinman MH, Lake AM, Forman J, Midle JB (2014) Newspaper coverage of suicide and initiation of suicide clusters in teenagers in the USA, 1988–96: a retrospective, population-based, case–control study. Lancet Psychiatry 1(1):34–43. 10.1016/S2215-0366(14)70225-1 [DOI] [PubMed] [Google Scholar]
- 7.Gould MS, Wallenstein S, Kleinman M (1990) Time-space clustering of teenage suicide. Am J Epidemiol 131(1):71–78 [DOI] [PubMed] [Google Scholar]
- 8.Johansson L, Lindqvist P, Eriksson A (2006) Teenage suicide cluster formation and contagion: implications for primary care. BMC Fam Pract 7:32 10.1186/1471-2296-7-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Niederkrotenthaler T, Fu KW, Yip PS, Fong DY, Stack S, Cheng Q, Pirkis J (2012) Changes in suicide rates following media reports on celebrity suicide: a meta-analysis. J Epidemiol Community Health 66(11):1037–1042. 10.1136/jech-2011-200707 [DOI] [PubMed] [Google Scholar]
- 10.Pirkis J, Nordentoft M (2011) International handbook of suicide prevention: research, policy and practice. In: O’Connor R, Platt S, Gordon J (eds) Media influences on suicide and attempted suicide Wiley, Chichester, pp 531–544 [Google Scholar]
- 11.Stack S (2003) Media coverage as a risk factor in suicide. J Epidemiol Community Health 57(4):238–240. 10.1136/jech.57.4.238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fink DS, Santaella-Tenorio J, Keyes KM (2018) Increase in suicides the months after the death of Robin Williams in the US. PLoS One 13(2):e0191405 10.1371/journal.pone.0191405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Joiner TE (1999) The clustering and contagion of suicide. Curr Dir Psychol Sci 8(3):89–92. 10.1111/1467-8721.00021 [DOI] [Google Scholar]
- 14.Johnson AM, Woodside JM, Johnson A, Pollack JM (2017) Spatial patterns and neighborhood characteristics of overall suicide clusters in florida from 2001 to 2010. Am J Prev Med 52(1):e1–e7. 10.1016/j.amepre.2016.07.032 [DOI] [PubMed] [Google Scholar]
- 15.Saman DM, Walsh S, Borowko A, Odoi A (2012) Does place of residence affect risk of suicide? A spatial epidemiologic investigation in Kentucky from 1999 to 2008. BMC Public Health 12:108 10.1186/1471-2458-12-108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fontanella CA, Saman DM, Campo JV, Hiance-Steelesmith DL, Bridge JA, Sweeney HA, Root ED (2018) Mapping suicide mortality in Ohio: a spatial epidemiological analysis of suicide clusters and area level correlates. Prev Med 106:177–184. 10.1016/j.ypmed.2017.10.033 [DOI] [PubMed] [Google Scholar]
- 17.Brenner B, Cheng D, Clark S, Camargo CA Jr (2011) Positive association between altitude and suicide in 2584 US counties. High Alt Med Biol 12(1):31–35. 10.1089/ham.2010.1058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.White RA, Azrael D, Papadopoulos FC, Lambert GW, Miller M (2015) Does suicide have a stronger association with seasonality than sunlight? BMJ Open 10.1136/bmjopen-2014-007403 [DOI] [PMC free article] [PubMed]
- 19.Vyssoki B, Kapusta ND, Praschak-Rieder N, Dorffner G, Willeit M (2014) Direct effect of sunshine on suicide. JAMA Psychiatry 71(11):1231–1237. 10.1001/jamapsychiatry.2014.1198 [DOI] [PubMed] [Google Scholar]
- 20.Oyesanya M, Lopez-Morinigo J, Dutta R (2015) Systematic review of suicide in economic recession. World J Psychiatry 5(2):243–254. 10.5498/wjp.v5.i2.243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Norström T, Grönqvist H (2015) The Great Recession, unemployment and suicide. J Epidemiol Community Health 69(2):110–116. 10.1136/jech-2014-204602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pollock NJ, Naicker K, Loro A, Mulay S, Colman I (2018) Global incidence of suicide among Indigenous peoples: a systematic review. BMC Med 16(1):145 10.1186/s12916-018-1115-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Haw C, Hawton K, Niedzwiedz C, Platt S (2013) Suicide clusters: a review of risk factors and mechanisms. Suicide Life Threat Behav 43(1):97–108. 10.1111/j.1943-278X.2012.00130.x [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention, National Center for Health Statistics (2017) Underlying Cause of Death 1999–2016 on CDC WONDER Online Database http://wonder.cdc.gov/ucd-icd10.html. Accessed 17 Jan 2018
- 25.US Census Bureau (2010) Profile of General Population and Housing Characteristics: 2010 (DP-1) using American FactFinder http://factfinder.census.gov. Accessed 25 March 2019
- 26.Kulldorff M (2006) Satscan: software for the spatial and space-time scan statistics http://www.satscan.org. Accessed 2 Dec 2017
- 27.Jones P, Gunnell D, Platt S, Scourfield J, Lloyd K, Huxley P, John A, Kamran B, Wells C, Dennis M (2013) Identifying probable suicide clusters in wales using national mortality data. PLoS One 8(8):e71713 10.1371/journal.pone.0071713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perez-Costillas L, Blasco-Fontecilla H, Benitez N, Comino R, Anton JM, Ramos-Medina V, Lopez A, Palomo JL, Madrigal L, Alcalde J, Perea-Milla E, Artieda-Urrutia P, de Leon-Martinez V, de Diego Otero Y (2015) Space-time suicide clustering in the community of Antequera (Spain). Rev Psiquiatr Salud Ment 8(1):26–34. 10.1016/j.rpsm.2014.01.007 [DOI] [PubMed] [Google Scholar]
- 29.Cheung YT, Spittal MJ, Williamson MK, Tung SJ, Pirkis J (2013) Application of scan statistics to detect suicide clusters in Australia. PLoS One 8(1):e54168 10.1371/journal.pone.0054168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Derek Cheung YT, Spittal MJ, Williamson MK, Tung SJ, Pirkis J (2014) Predictors of suicides occurring within suicide clusters in Australia, 2004–2008. Soc Sci Med (1982) 118:135–142. 10.1016/j.socscimed.2014.08.005 [DOI] [PubMed] [Google Scholar]
- 31.Dantas AP, Azevedo UN, Nunes AD, Amador AE, Marques MV, Barbosa IR (2018) Analysis of suicide mortality in Brazil: spatial distribution and socioeconomic context. Revista brasileira de psiquiatria (Sao Paulo, Brazil: 1999) 40(1):12–18. 10.1590/1516-4446-2017-2241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Niedzwiedz C, Haw C, Hawton K, Platt S (2014) The definition and epidemiology of clusters of suicidal behavior: a systematic review. Suicide Life Threat Behav 44(5):569–581. 10.1111/sltb.12091 [DOI] [PubMed] [Google Scholar]
- 33.R Development Core Team (2008) R: A language and environment for statistical computing R Foundation for Statistical Computing, Vienna, Austria: http://www.R-project.org. Accessed 18 Oct 2017 [Google Scholar]
- 34.Subica AM, Wu L-T (2018) Substance use and suicide in Pacific Islander, American Indian, and Multiracial Youth. Am J Prev Med 54(6):795–805. 10.1016/j.amepre.2018.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leavitt RA, Ertl A, Sheats K, Petrosky E, Ivey-Stephenson A, Fowler KA (2018) Suicides among American Indian/Alaska natives—National Violent Death Reporting System, 18 States, 2003–2014. MMWR Morb Mortal Wkly Rep 67:237–242. 10.15585/mmwr.mm6708a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.LeMaster PL, Beals J, Novins DK, Manson SM (2004) The prevalence of suicidal behaviors among Northern Plains American Indians. Suicide Life Threat Behav 34(3):242–254. 10.1521/suli.34.3.242.42780 [DOI] [PubMed] [Google Scholar]
- 37.Perez-Rodriguez MM, Baca-Garcia E, Oquendo MA, Blanco C (2008) Ethnic Differences in suicidal ideation and attempts. Prim Psychiatry 15(2):44–53 [PMC free article] [PubMed] [Google Scholar]
- 38.Hanzlick R (2007) The conversion of coroner systems to medical examiner systems in the United States: a lull in the action. Am J Forensic Med Pathol 28(4):279–283. 10.1097/PAF.0b013e31815b4d5a [DOI] [PubMed] [Google Scholar]
- 39.Hanzlick R (2006) Medical examiners, coroners, and public health: a review and update. Arch Pathol Lab Med 130(9):1274–1282. 10.1043/1543-2165(2006)130[1274:MECAPH]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- 40.Center for Disease Control and Prevention Public Health Law Program (2015) Coroner/medical examiner laws, by state https://www.cdc.gov/phlp/publications/topic/coroner.html. Accessed 5 Apr 2019
- 41.Gould MS (2001) Suicide and the media. Ann N Y Acad Sci 932:200–221 (discussion 221–204) [DOI] [PubMed] [Google Scholar]
- 42.Robertson L, Skegg K, Poore M, Williams S, Taylor B (2012) An adolescent suicide cluster and the possible role of electronic communication technology. Crisis 33(4):239–245. 10.1027/0227-5910/a000140 [DOI] [PubMed] [Google Scholar]
- 43.Poijula S, Wahlberg KE, Dyregrov A (2001) Adolescent suicide and suicide contagion in three secondary schools. Int J Emerg Ment Health 3(3):163–168 [PubMed] [Google Scholar]
- 44.Hacker K, Collins J, Gross-Young L, Almeida S, Burke N (2008) Coping with youth suicide and overdose: one community’s efforts to investigate, intervene, and prevent suicide contagion. Crisis 29(2):86–95. 10.1027/0227-5910.29.2.86 [DOI] [PubMed] [Google Scholar]
- 45.Zalsman G (2016) Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry 3(7):646–659. 10.1016/S2215-0366(16)30030-X [DOI] [PubMed] [Google Scholar]
- 46.Gould MS, Marrocco FA, Hoagwood K, Kleinman M, Amakawa L, Altschuler E (2009) Service use by at-risk youths after school-based suicide screening. J Am Acad Child Adolesc Psychiatry 48(12):1193–1201. 10.1097/CHI.0b013e3181bef6d5 [DOI] [PMC free article] [PubMed] [Google Scholar]