Abstract
Objective
Few studies have examined the sleep behaviors associated with a caregiver-reported sleep problem beyond early childhood and across different age groups. This study examined sleep behaviors associated with a caregiver-reported sleep problem from birth to middle childhood.
Methods
Participants were 5,107 children from the Longitudinal Study of Australian Children—Birth Cohort. Caregiver-reported child sleep problems and sleep behaviors were assessed biennially from ages 0–1 to 10–11 years. Logistic regressions were used to examine associations between three child sleep behaviors (waking overnight, difficulty falling asleep, and difficulty sleeping alone) and the odds of having a caregiver-reported sleep problem at each age.
Results
Caregiver-reported child sleep problems were most prevalent in infancy (17.1%) and decreased through middle childhood (7.7%). All three sleep behaviors were associated with a sleep problem at each age. Whereas waking overnight was the most common sleep behavior and was associated with the highest odds of having a sleep problem from infancy to age 6–7 years (ORs = 5.78–8.29), difficulty falling asleep was the most common sleep behavior and was associated with the highest odds of having a sleep problem at ages 8–9 and 10–11 years (ORs =10.65 and 17.78, respectively).
Conclusion
Caregivers’ endorsement of a child sleep problem is associated with developmentally-relevant sleep behaviors, with night awakenings most relevant during infancy and difficulty falling asleep most relevant in middle childhood. Study findings have implications for targeted and developmentally-focused sleep problem screening questions in child healthcare settings. Future research examining additional indicators of caregiver-defined sleep problems is required.
Keywords: development, longitudinal, pediatric, sleep behaviors, sleep problems
1. Introduction
Caregiver-reported child sleep problems are common in infancy, early, and middle childhood,1–3 and are frequently assessed using a single caregiver-rated item,4–6 particularly in routine clinical practice.7 However, few studies have examined which sleep behaviors are associated with caregiver-reported sleep problems beyond the preschool years. In a large sample of 29,287 infants and toddlers up to 36 months of age from 17 different countries, Sadeh et al.2 found that greater night awakenings and a prolonged sleep onset latency were among the variables most strongly associated with a small to severe caregiver-reported sleep problem in both predominantly Caucasian and predominantly Asian cultural contexts. Another study8 that examined the prevalence of sleep problems and sleep behaviors over time (6 to 36 months) found frequent night awakenings, prolonged sleep onset latency, and shortened nighttime sleep duration were consistently associated with a caregiver-reported sleep problem across timepoints.
Given that help-seeking for child sleep problems is likely driven by primarily caregiver-reported concerns,2 it is important to identify which sleep behaviors are associated with caregiver perceptions of a child sleep problem. This research can provide guidance for clinicians about common problematic sleep behaviors, which is especially helpful as clinicians are rarely able to administer detailed diagnostic sleep surveys in routine practice due to the need to assess multiple child domains in a short amount of time.9 Furthermore, it is important identify whether there are developmental shifts in which sleep behaviors are perceived as problematic by caregivers across child age groups to guide more targeted sleep screening approaches in clinical practice. Thus, the purpose of this study was to examine the prevalence of caregiver-reported child sleep behaviors and identify associations between these behaviors and a global caregiver rating of child sleep problems from infancy through middle childhood.
2. Methods
2.1. Participants and Procedure
We examined the first 6 waves of the prospective Growing up in Australia: The Longitudinal Study of Australian Children (LSAC)—Birth Cohort (B-cohort), which has been described elsewhere.10 Briefly, LSAC used a two-stage cluster sampling design to enroll a nationally representative cohort. A total of 5,107 infants aged 0–1 years were enrolled in the B-cohort, began data collection in 2004 (Wave 1), and were sampled biennially through ages 10–11 years (Wave 6, 2014). A total of 3,764 children (73.7%) were retained in the study at Wave 6, with children who had less highly educated caregivers and those from non-English speaking backgrounds being marginally more likely to drop out of the study.11 Data were collected at each wave via a home-based face-to-face interview with the primary caregiver, which was usually the mother; both mothers and fathers were interviewed when possible. The Australian Institute of Family Studies Ethics Committee approved this study and caregivers provided written informed consent.
2.2. Measures
At each time point, child sleep problems were defined using the primary caregiver-reported question, How much is your child’s sleeping pattern or habits a problem for you?12 Caregivers indicated whether their child’s sleep was a large problem, a moderate problem, a small problem, no problem at all or not sure/don’t know. Responses were dichotomized according to previous longitudinal and intervention research,4–6 with a sleep problem defined as those who had a moderate or large problem, and no sleep problem defined as no problem or a small problem. Not sure/don’t know responses were coded as missing. Three sleep behaviors were measured via caregiver report: difficulty getting off to sleep at night; not happy to sleep alone; and waking during the night. Caregivers rated each item individually, indicating whether the behavior occurred 4 or more nights per week (yes or no), or more than half of the week.
Demographic variables, including child sex and indigenous status, were assessed at birth. The LSAC dataset also includes a composite socioeconomic position (SEP) variable consisting of caregiver income, education, and occupational prestige that were standardized and combined to index family socioeconomic status.13
2.3. Statistical Analyses
Survey methods were used in analyses to address the unequal probability of participant selection into the sample and sample attrition, and the multi-stage, clustered sampling design.14,15 Interrelations between sleep problems and specific sleep behaviors were examined using logistic regressions, accounting for child sex, indigenous status, and SEP in Stata version 15.0.
3. Results
3.1. Demographics
There were similar proportions of male (51.1%) and female children enrolled in the study, with a mean age of 8.8 months (SD = 2.5 months, range = 3–19 months) at Wave 1. A total of 10.5% of children lived in single parent homes and 4.9% of children were of Aboriginal or Torres Strait Islander origin. Most participating caregivers were married (90.6%), spoke primarily English in the home (85.6%), and were born in Australia or New Zealand (81.4%). The majority of primary caregivers were the child’s biological mother (96.1%), had completed at least high school (68.3%) and had a mean age of 31.0 years (SD = 5.5 years, range = 15–63 years) at Wave 1. A total of 25% of families were characterized as having low SEP.13
3.2. Prevalence of sleep problems and sleep behaviors by age
Figure 1 describes the prevalence of caregiver-reported overall sleep problem and sleep behaviors at each age. The prevalence of overall sleep problems was highest during infancy (17.1%), gradually declining during early childhood and stabilizing from ages 6–7 (7.8%) to ages 10–11 years (7.7%). Waking overnight was the most prevalent behavior during infancy (40.8%) and steadily decreased through ages 10–11 years (5.7%). Difficulty sleeping alone peaked at ages 2–3 years (20.0%), while problems with falling asleep fluctuated over time, with the highest prevalence at ages 10–11 years (17.6%).
Figure 1.
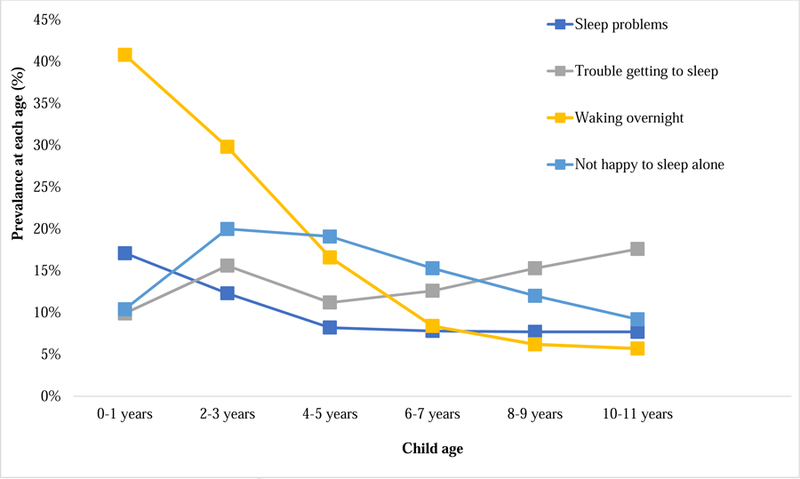
Prevalence of caregiver-reported sleep problems and sleep behaviors by age birth to age 10–11 years.
3.3. Associations between sleep problems and sleep behaviors by age
All three sleep behaviors were significantly associated with increased odds of a caregiver-reported sleep problem at each age (see Table 1). However, associations between specific sleep behaviors and sleep problems varied in magnitude by age. Whereas night awakenings were consistently associated with the highest odds of having a caregiver-reported sleep problem from ages 0–1 years through ages 6–7 years, difficulty falling asleep was associated with the highest odds of having a caregiver-reported sleep problem at ages 8–9 and 10–11 years. Difficulty sleeping alone had the lowest odds of being linked to a caregiver-rated sleep problem relative to other sleep behaviors at age, with the exception of ages 2–3 years and 4–5 years, when it was associated with a slightly higher odds of having a sleep problem compared to difficulty falling asleep.
Table 1.
Associations between caregiver-reported child sleep problems and sleep behaviors at each wave
| Wave | Sleep problem (% | |||
|---|---|---|---|---|
| No | Yes | OR (95% CI)* | p-value | |
| 0−1 years | n = 4225 | n = 871 | ||
| Trouble getting to sleep | 5.68 | 30.20 | 4.26 (3.32 to 5.45) | <0.001 |
| Not happy to sleep alone | 6.82 | 27.78 | 3.10 (2.42 to 3.96) | <0.001 |
| Waking over night | 32.21 | 82.32 | 8.29 (6.74 to 10.21) | <0.001 |
| 2−3 years | n = 4041 | n = 564 | ||
| Trouble getting to sleep | 11.19 | 46.99 | 3.55 (2.83 to 4.45) | <0.001 |
| Not happy to sleep alone | 14.63 | 58.51 | 4.29 (3.45 to 5.33) | <0.001 |
| Waking over night | 23.46 | 75.00 | 6.29 (5.02 to 7.86) | <0.001 |
| 4−5 years | n = 4024 | n = 361 | ||
| Trouble getting to sleep | 8.20 | 44.04 | 4.44 (3.37 to 5.86) | <0.001 |
| Not happy to sleep alone | 15.13 | 63.71 | 4.45 (3.42 to 5.78) | <0.001 |
| Waking over night | 12.57 | 60.94 | 5.78 (4.46 to 7.48) | <0.001 |
| 6−7 years | n = 3905 | n = 331 | ||
| Trouble getting to sleep | 9.68 | 46.83 | 5.59 (4.23 to 7.37) | <0.001 |
| Not happy to sleep alone | 12.22 | 51.36 | 3.71 (2.81 to 4.87) | <0.001 |
| Waking over night | 5.43 | 42.90 | 7.96 (5.91 to 10.70) | <0.001 |
| 8−9 years | n = 3732 | n = 313 | ||
| Trouble getting to sleep | 11.07 | 65.18 | 10.65 (8.10 to 14.00) | <0.001 |
| Not happy to sleep alone | 9.27 | 44.41 | 3.76 (2.77 to 5.08) | <0.001 |
| Waking over night | 3.91 | 33.23 | 5.54 (3.88 to 7.89) | <0.001 |
| 10−11 years | n = 3401 | n = 284 | ||
| Trouble getting to sleep | 12.50 | 78.87 | 17.78 (12.95 to 24.40) | <0.001 |
| Not happy to sleep alone | 6.70 | 39.44 | 4.06 (2.89 to 5.71) | <0.001 |
| Waking over night | 3.47 | 32.04 | 5.56 (3.75 to 8.25) | <0.001 |
Multivariate logistic regression, model includes all sleep behaviors; CI = confidence interval.
4. Discussion
Study findings indicate developmental shifts in the prevalence of sleep behaviors and sleep problems, as well as how caregivers characterize sleep problems by child age. In line with previous studies,1–3,8 caregiver-perceived sleep problems were the most prevalent in infancy and declined from early to middle childhood, although sleep problems still impacted nearly 1 in 10 children between ages 6 and 11 years. Waking overnight was the most common sleep behavior during infancy and early childhood, reflecting normative patterns of child sleep consolidation.16 Waking overnight was also associated with the highest odds of a caregiver-reported sleep problem in early development, as in other studies of early childhood sleep problems,2,8 followed by difficulty sleeping independently. These findings correspond with manifestations of insomnia disorder in early development, including problematic sleep onset associations (e.g., feeding or parental presence at bedtime) and the common emergence of nighttime fears and bedtime refusal in early childhood.17,18 Unlike in earlier development, difficulty falling asleep was more prevalent between ages 6 and 11 years, and was associated with the highest odds of having a caregiver-reported sleep problem at these ages, which aligns with population-based research showing that difficulty falling asleep is the most frequent symptom of insomnia in middle childhood.19 This particular symptom may be attributable to increased sleep-related anxiety or hyperarousal at bedtime,20 or to emerging or concurrent mood or anxiety disorders.1,21
Study findings collectively show the most common sleep behaviors that caregivers identify as being problematic at different child ages. Many of these behaviors correspond with developmentally-linked patterns of sleep consolidation in early development and symptoms of insomnia disorder from early to middle childhood. These findings have implications for the use of targeted screening questions for specific sleep behaviors in usual child healthcare settings, such as primary care, and for anticipatory guidance for caregivers and pediatric providers about common sleep problems by age. For example, specific questions about sleep consolidation (night awakenings) are more relevant when screening for sleep problems in very young patients, whereas questions about difficulties with sleep onset are more appropriate for school-aged children.
There are a number of limitations with the current study. First, this study did not examine other sleep behaviors that have been associated with a caregiver-reported sleep problem, such as shortened sleep duration, restless sleep, or parasomnias.8 Thus, future research should examine a range of sleep behaviors that could characterize a child sleep problem. Second, the use of a global, caregiver-reported single-item to assess child sleep problems provides limited information, given that endorsement of this item could reflect heterogeneous sleep concerns. However, it should be noted that a single item continues to be commonly used to assess sleep problems in the context of both research4–6 and clinical practice,7 highlighting the need to continue to assess the utility of this approach. Third, caregiver perspectives on early childhood child sleep problems have been found to vary according to caregiver sleep-related cognitions22 and socio-cultural factors, including caregiver behaviors at bedtime and family sleep arrangement.2 These factors, as well as caregivers’ expectations about and tolerance for various child sleep behaviors, should be examined in relation to sleep problems through middle childhood. Fourth, this study did not investigate other factors that could contribute to a child sleep problem, such as feeding and co-sleeping practices in infancy and early childhood,2 as well as child temperament23 and comorbid physical or behavioral health conditions1,6 over time. Finally, additional study limitations include the use of an Australian sample that may not generalize to other cultural contexts, and the use of subjective caregiver ratings for study outcomes, which introduces shared method variance.
Despite these limitations, the findings from this study provide preliminary information about developmental shifts in linkages between a caregiver-endorsed child sleep problem and modifiable sleep behaviors. These findings can help to inform developmentally tailored screening for sleep problems in usual care settings, although future research on additional socio-cultural factors and other sleep behaviors that contribute to a caregiver-identified sleep problem is needed.
Highlights.
Sleep problems decrease from 17.1% in infancy to 7.7% in middle childhood.
Waking overnight is most common in infancy and associated with a sleep problem.
Difficulty falling asleep was most linked with middle childhood sleep problems.
Links between sleep behaviors and a caregiver-reported sleep problem vary by age.
Acknowledgments
Funding Source:
Ariel A. Williamson was supported during this study by T32HL007953-17 from the National Heart, Lung, and Blood Institute, by a career development award from the Sleep Research Society Foundation and by K23HD094905-01A1 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Harriet Hiscock is supported by a National Health and Medical Research Council Practitioner Fellowship (1136222).
Research at the Murdoch Childrens Research Institute is supported by the Victorian Government’s Operational Infrastructure Support Program. The funding bodies had no role in relation to the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Abbreviations:
- LSAC
Longitudinal Study of Australian Children
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest:
The authors have no conflicts of interest relevant to this article.
References
- 1.Gregory AM, O’Connor TG. Sleep problems in childhood: a longitudinal study of developmental change and association with behavioral problems. Journal of the American Academy of Child & Adolescent Psychiatry 2002;41(8):964–971. [DOI] [PubMed] [Google Scholar]
- 2.Sadeh A, Mindell J, Rivera L. “My child has a sleep problem”: a cross-cultural comparison of parental definitions. Sleep medicine 2011;12(5):478–482. [DOI] [PubMed] [Google Scholar]
- 3.Wang B, Isensee C, Becker A, et al. Developmental trajectories of sleep problems from childhood to adolescence both predict and are predicted by emotional and behavioral problems. Frontiers in psychology 2016;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mindell JA, Du Mond CE, Sadeh A, Telofski LS, Kulkarni N, Gunn E. Efficacy of an internet-based intervention for infant and toddler sleep disturbances. Sleep 2011;34(4):451–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Quach J, Hiscock H, Ukoumunne OC, Wake M. A brief sleep intervention improves outcomes in the school entry year: a randomized controlled trial. Pediatrics 2011;128:692–701. [DOI] [PubMed] [Google Scholar]
- 6.Quach J, Mensah FK, Hiscock H. Differential outcomes of sleep problems in children with and without special health care needs: Australian population study. Journal of Developmental & Behavioral Pediatrics 2016;37(5):415–423. [DOI] [PubMed] [Google Scholar]
- 7.Owens JA. The practice of pediatric sleep medicine: results of a community survey. Pediatrics 2001;108(3):e51–e51. [DOI] [PubMed] [Google Scholar]
- 8.Byars KC, Yolton K, Rausch J, Lanphear B, Beebe DW. Prevalence, patterns, and persistence of sleep problems in the first 3 years of life. Pediatrics 2012;129(2):e276–e284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Honaker SM, Meltzer LJ. Sleep in pediatric primary care: a review of the literature. Sleep medicine reviews 2016;25:31–39. [DOI] [PubMed] [Google Scholar]
- 10.Soloff C, Lawrence D, Jonstone R. Longitudinal Study of Australian Children Technical Paper No. 1: Sample Design. Melbourne, Victoria: Australian Institute of Family Studies;2005. [Google Scholar]
- 11.Norton A, Monahan K. The Longitudinal Study of Australian Children: LSAC technical Paper No. 15, Wave 6 Weighting and Non-Response 2015.
- 12.Australian Government Department of Families, Housing, Community Services and Indigenous Affairs [AGDF]. Growing up in Ausralia: The Longitudinal Study of Australian Children 2009–10 Annual Report In. Australia: New Millennium Print; 2011. [Google Scholar]
- 13.Blakemore T, Strazdins L, Gibbings J. Measuring family socio-economic position. Australian Social Policy Journal 2009;8:121. [Google Scholar]
- 14.Soloff C, Lawrence D, Johnstone R. LSAC technical reference paper number 1: sample design Available at: www.aifs.gov.au/growingup/pubs/techpapers/tp1.pdf. 2005. Accessed May 22, 2008.
- 15.Misson S, Sipthorp M, Studies AIoF. Wave 2 weighting and non-response. Australian Institute of Family Studies; 2007.
- 16.Galland BC, Taylor BJ, Elder DE, Herbison P. Normal sleep patterns in infants and children: a systematic review of observational studies. Sleep medicine reviews 2012;16(3):213–222. [DOI] [PubMed] [Google Scholar]
- 17.Mindell JA, Kuhn B, Lewin DS, Meltzer LJ, Sadeh A. Behavioral treatment of bedtime problems and night wakings in infants and young children. Sleep: Journal of Sleep and Sleep Disorders Research 2006. [PubMed]
- 18.Muris P, Merckelbach H, Ollendick TH, King NJ, Bogie N. Children’s nighttime fears: parent–child ratings of frequency, content, origins, coping behaviors and severity. Behaviour research and therapy 2001;39(1):13–28. [DOI] [PubMed] [Google Scholar]
- 19.Calhoun SL, Fernandez-Mendoza J, Vgontzas AN, Liao D, Bixler EO. Prevalence of insomnia symptoms in a general population sample of young children and preadolescents: gender effects. Sleep medicine 2014;15(1):91–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vriend J, Corkum P. Clinical management of behavioral insomnia of childhood. Psychology research and behavior management 2011;4:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gregory AM, Sadeh A. Sleep, emotional and behavioral difficulties in children and adolescents. Sleep medicine reviews 2012;16(2):129–136. [DOI] [PubMed] [Google Scholar]
- 22.Sadeh A, Flint-Ofir E, Tirosh T, Tikotzky L. Infant sleep and parental sleep-related cognitions. Journal of family psychology 2007;21(1):74. [DOI] [PubMed] [Google Scholar]
- 23.Cremone A, Jong DM, Kurdziel LB, et al. Sleep Tight, Act Right: Negative Affect, Sleep and Behavior Problems During Early Childhood. Child Development 2017. [DOI] [PMC free article] [PubMed]


