Abstract
Nearly 50% of physicians report symptoms of clinical burnout. Occupational factors and personal health play substantial roles in physician burnout. The role of sleep in physician burnout is not well understood. Burnout is at epidemic levels in health care, with research suggesting nearly one in two physicians experience clinical burnout as defined according to the Maslach Burnout Index. Sleep deprivation, burnout, and clinician health are intricately intertwined. The relation between sleep deprivation and burnout is not only suggested in hypothetical models but also confirmed in observational studies of workers of all types. Models describing the relation between burnout and sleep suggest as potential causative mechanisms of sleep disturbances the following: (1) a chronic depletion of energy stores; or (2) activation of the hypothalamic-pituitary-adrenal axis and increasing levels of bodily stress. Sleep deprivation and burnout are widespread in health-care workers, affecting not only nurses but also medical students, physicians-in-training, and practicing physicians. Although sleep deprivation is associated with clinical burnout, direct studies showing that sleep extension can improve burnout recovery are lacking. Early detection and early intervention to improve both sleep deprivation and burnout are warranted in health-care professionals. Interventions should be directed not only at individuals but also at the entire health system. This review highlights the latest developments and emerging concepts concerning the role of sleep and circadian disorders in physician burnout.
Key Words: burnout, physician health, sleep deprivation, sleep medicine
Abbreviations: MBI, Maslach Burnout Inventory; REM, rapid eye movement
Burnout among physicians is at epidemic levels and is now an area of widespread focus. In large studies, nearly one in two trainee physicians1, 2 and practicing physicians3, 4, 5 have reported symptoms of burnout, suggesting that factors leading to burnout are rooted in the daily environment of physicians.4 Consequences of physician burnout include medical errors,2, 6, 7 patient outcomes,8 and compromised clinician general health.9, 10, 11 Burnout is defined via the Maslach Burnout Inventory (MBI) as the triad of depersonalization, emotional exhaustion, and decreased sense of personal accomplishment; this entails not just perception but also reduced performance.12, 13 When > 7,000 US physicians were sampled by using the MBI, 37.9% reported high emotional exhaustion, 29.4% reported high rates of depersonalization, and 12.4% reported a low sense of personal accomplishment.4
Physicians with duties at the front lines of patient care (family medicine, general internal medicine, and emergency medicine) report the highest rates of burnout.4 Likewise, critical care physicians and critical care nurses report burnout rates close to 60%. Of great concern, compared with a probability-based adult sample, physicians were more likely to experience symptoms of burnout (37.9% vs 27.8%; P < .001) and be disgruntled with their current work/life balance (40.2% vs 23.2%; P < .001).
Adverse health effects of burnout have been reported in the literature, including depression, substance abuse, suicidal ideation, and insomnia.4, 7, 14, 15 Because patient outcomes are also at risk, the effects of physician burnout go one step further. For example, Fahrenkopf et al6 discovered that physicians-in-training who reported clinical burnout based on the MBI also reported 6.2 times more medical errors compared with their non-burned out counterparts.
Given these high rates of physician burnout and the deleterious effects on both health of physicians and their patients, occupational risk factors for burnout among physicians are essential to consider. Job stressors, including emotionally demanding clinical experiences, exposure to death and dying on a frequent basis, time pressures, and increasing work demands, are all associated with an increased risk for clinical burnout.16, 17 In addition to the aforementioned occupational risk factors, sleep deprivation and circadian disorders are inherent occupational risks for physicians and could have a major impact in perpetuating high rates of physician burnout.
Sleep Deprivation/Circadian Disorders Among Physicians
The health effects associated with sleep deprivation are similar to findings of burnout. These health consequences include mood changes, increased sleepiness, fatigue, irritability, difficulty concentrating, and disorientation.18 Although few adults achieve 8 h per night of recommended sleep, physicians only average 6.5 h nightly.19 In a national survey by the American College of Chest Physicians Sleep Institute, physician members reported that they were not receiving the amount of sleep needed to function as peak performers. Almost one-half (43%) of the practicing physicians surveyed reported that their work schedules were to blame for their inadequate sleep.19 Practicing physicians also reported making up for missed weekday sleep on weekends or days off, sleeping on average 7.5 h. One in five physician respondents also reported missing out on family/leisure activities due to sleep problems. This scenario can be especially challenging for physicians who naturally have an advanced sleep phase (the “early bird”) or a delayed sleep phase (the “night owl”) circadian rhythm. Not surprisingly, physicians also reported increased caffeine use compared with the general population.
In addition to long shifts, one reason for the high rates of sleep loss/circadian disorders in physicians is the culture of medical training.20 Physicians-in-training receive the message that sleep is dispensable, as they continue to work long extended shifts even with restricted duty hours. As a result, trainees may become desensitized to their physiological need for adequate sleep. Given the 24-h nature of medical care, circadian disorders such as delayed sleep-wake phase disorder, advanced sleep-wake disorder, irregular sleep-wake rhythm disorder, and jet lag disorder may further compound physician sleep disturbances but remain largely unexplored. Due to the high prevalence of sleep deprivation and circadian disorders and epidemic rates of burnout in physicians, it is important to better understand how they are conceptually linked.
Models Linking Sleep Deprivation/Circadian Disorders to Burnout
To understand better the link between sleep deprivation/circadian disorders and physician burnout, it is first essential to understand the underlying biological mechanisms that would link the two. It is well understood that sleep is an essential biological purpose and has a major responsibility in recovery, energy conservation, and survival.18, 21 Rodent studies by Everson and Crowley22 reported reductions in circulating hormones and failed negative feedback loops, pointing to hypothalamic mechanisms in sleep deprivation. Metabolic and immunologic consequences of sleep deprivation in the form of altered enzymatic levels in the heart, liver, and lung have also been noted in sleep-deprived rodents.23 Sleep not only plays a key role in learning, memory consolidation, and motor learning but also in emotional regulation and cardiovascular metabolism.24, 25, 26 Restorative effects of adequate sleep include driving neurotoxic wastes out of the CNS which accumulate during waking hours.18, 26 Insufficient sleep or circadian misalignment can lead to a decline in cognitive function, memory, and performance and the blunting of the cardiovascular autonomic response system.18, 24
Disturbed sleep has been hypothesized as a mechanism that contributes to burnout and the chronic depletion of energy stores.27 According to this conceptual model, burnout is a syndrome encompassing feelings of physical, emotional, and mental depletion, and it is considered a consequence of employment environment stressors, without adequate recovery.28, 29 Another model suggests that a hyperactive/stress state may be integral in burnout and may involve an increased activation of the hypothalamic-pituitary-adrenal axis, resulting in a chronic increased allostatic load.30 Melamed et al31 suggest that this increase in hypothalamic-pituitary-adrenal axis activation and chronic stress are mediators for both burnout and sleep deprivation.
Sleep consequences of burnout include a hyperarousal state and an inability to settle down due to worries, concerns, self-depreciation, and anxiety.24, 32 These factors all lead to an increase in sleep initiation insomnia and sleep maintenance insomnia, along with effects on the structure and architecture of sleep. This scenario leads to insufficient sleep quality and to the underlying cyclical dilemma of sleep disturbance and its role in burnout. However, it is equally important to remember that insufficient sleep itself is a potential cause of burnout and may facilitate the emergence of burnout as a syndrome in vulnerable individuals.
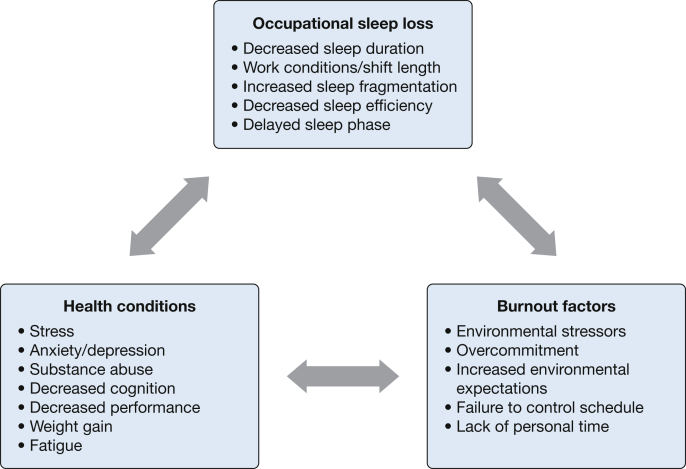
A model in which incomplete burnout/stress recovery mediates a relationship between stressful employment conditions and chronic health problems has been described by Geurts and Sonnentag.33 These authors suggest situations in which prolonged exposure to work-related stressors leads to rumination and anticipation regarding potential future stressors, which lead to sustained psychological and physiological activation. Perseverative cognition, such as rumination over past stressors and anticipatory stress, has been associated with an increased psychosomatic load, prolonged and sustained physiologic stress, and insomnia.18, 34, 35 Chronic stress is the primary cause of persistent psychophysiological insomnia.18 Even modest amounts of daily stress can affect sleep architecture. Sleep loss, factors leading to burnout, and the health conditions associated with both are intricately interwoven (Fig 1).
Figure 1.
The multidimensional association of occupational sleep loss, health conditions, and burnout factors.
Given this theoretical framework, it is not surprising that several studies have implicated sleep problems in the development of burnout in the general population.36, 37, 38 In a study among nonmedical working professionals, respondents reported that < 6 h of sleep nightly was the main risk factor for developing burnout.39 Moreover, other studies found that sleep physiology improves with recovery from burnout.38 Ekstedt et al38 and Söderström et al40 reported that among white collar workers on “sick leave” compared with population control subjects, improving burnout symptoms was associated with shortened sleep latency, increased sleep efficiency, reduced number of arousals, reduced sleep fragmentation rate, and reduced time awake following sleep onset. In contrast, slow wave sleep (important in memory consolidation and processing)41, 42 did not completely recover with burnout resolution.37, 38, 40 Together, these findings suggest that certain aspects of sleep take longer to recover to normal levels once burnout occurs.
There are also a variety of expert opinions and studies showing an association between sleep loss and increased stress. Because sleep is a restorative bodily function, sleep restriction makes the body more sensitive to emotional and stressful stimuli.43 Likewise, daytime emotional stress has been shown to influence sleep physiology, dream patterns, and dream content. Exaggerated startle response, increased levels of awakening thresholds from rapid eye movement (REM) sleep, increased and decreased sleep-onset latency to REM, REM sleep duration, and arousal occurrences are all noted effects of stress. Because restorative sleep seems to be a buffer for the negative effects of stress, it is hypothesized that reduced sleep leads to burnout-like symptoms such as impaired cognitive functioning, fatigue, and sleepiness.44 In support of this hypothesis, Bonnet and Arand45 along with Fahlén et al46 determined that fragmented sleep has similar effects on burnout-like symptoms.
Cross-sectional studies in the general public report a connection between job strain, stress, and overcommitment with sleep disturbances.46, 47, 48, 49 In a study by Williamson and Feyer50 among employees at a transportation company, moderate levels of sleep deprivation produced impairment in cognitive and motor function similar to alcohol intoxication, with response speeds < 50% of expected. Although there are few prospective studies on the relation of sleep and burnout, one analysis by Linton51 showed that a “poor psychosocial work environment” nearly doubled the risk of sleep-related issues over the course of 1 year. One study on burnout and insomnia predicted the intertwining development of these issues over time, suggesting that one is a risk factor for the other.36
Relation Between Sleep Disorders and Clinicians
Given this conceptual framework linking burnout and sleep deprivation, as well as evidence from the general population, it is especially important to evaluate the relation between sleep deprivation and burnout among health-care professionals.
Sleep Disturbances in Medical Students
Although the majority of trainee literature focuses on residency trainees, medical students also experience sleep loss and burnout. Among two preclinical medical student cohorts at a large academic US institution, more than one-third of students reportedly received less than the suggested 7 h of sleep nightly, and nearly 10% reported sleepiness while driving.52 In another study in preclinical medical students, pathologic sleepiness correlated with a higher prevalence of burnout.53
Sleep Disturbances in House Officers
In a national duty hour trial among internal medicine interns and residents, trainee physicians experience a substantial degree of sleep deprivation and fatigue.54 They frequently have extended on-call shifts or night shifts as a routine aspect of their duties. There has been increasing importance placed on improving sleep loss and fatigue as well as high rates of burnout for physicians-in-training, particularly residents.
In a single-institution study among intern physicians prior to duty hour reform, prevalence of chronic sleep deprivation (9% to 43%; P = .0001), moderate depression (4.3%-29.8%; P = .0002), and clinical burnout (4.3%-55.3%; P < .0001) were significantly increased when baseline was compared with year-end.55 A prospective study of critical care fellows prior to duty hour reform reported increased levels of stress, increased levels of dehydration, arrhythmias, and decreased amount of consecutive sleep.56 Another study pre-duty hour reform evaluated the impact of eliminating extended duty periods for interns, and noted increased sleep and decreased attention failures.57 Due to the growing concerns regarding duty hours, regulations attempting to improve trainee education and well-being along with patient care ensued.
Despite initial duty hour reforms in 2003, studies regarding trainee fatigue and burnout were vague and hampered by suboptimal study design and conduct.58 A systematic review by Fletcher et al59 in 2005 examined quality of life factors in the post-duty hour era, including amount of sleep achieved among trainees. Interventions resulted in mixed effects but suggesting “that there may not be uniform benefits for residents from these changes” and the use of nonvalidated instruments made further conclusions challenging. Although trainees commonly cite sleep deprivation as one of several factors leading to burnout, a statistically significant correlation was not observed between hours slept, hours worked, or sleep deprivation.55 Elimination of extended work hour shifts for interns did show an increase in sleep along with decreased attentional failures during night work hours in the ICU.57
Studies of the 2011 duty hour restrictions on resident well-being have been conducted. The Flexibility in Duty Hour Requirements for Surgical Trainees (FIRST) trial in 2016 evaluated standard duty hours vs flexible duty hours, both with an 80-h work week maximum; no differences were recorded in patient safety or resident well-being, but sleep was not evaluated with the use of objective measures.60 In another pivotal duty hours trial, The Individualized Comparative Effectiveness of Models Optimizing Patient Safety and Resident Education (iCOMPARE) study evaluated flexible duty hour programs compared with standardized Accreditation Council for Graduate Medical Education duty-hour policies across multiple indices.61 Interns in flexible duty hour programs (longer shifts) were more likely to report dissatisfaction with overall well-being (OR, 2.47; 95% CI, 1.67- 3.65). However, burnout rates were notably high in both groups: 79% in flexible duty hour programs vs 72% in standard duty hour programs (OR, 1.43; 95% CI, 0.96-2.13). Although there are no studies directly evaluating whether improvements in sleep lead to burnout recovery in physicians, the evidence suggests this topic should be an area for future investigation. This is particularly important because studies show that even with recent duty hour limits, trainees, especially those who work night shifts, are still receiving inadequate sleep.62
Sleep Disturbances in Practicing Physicians
Practicing physicians are subjected to long working hours and nighttime hours. Physicians also face demanding clinical situations, high clinical loads, emotionally charged patient encounters, and often critical decision-making, all of which can lead to a heighted level of stress.63 Extended-hour night shifts disrupt the pattern of sleep from a circadian rhythm standpoint. Specialties that require on-call or shift work such as emergency medicine or critical care are especially susceptible to sleep deprivation and sleep disorders. These specialties routinely require on-call shifts and shifts outside of the normal circadian rhythm.
Studies among physicians confirm a similar relationship between sleep and burnout. Among primary care physicians in Madrid, Spain, in those with high levels of burnout compared with low levels of burnout, high rates of insomnia and poorer sleep quality were noted (39.7% vs 7%, respectively) after controlling for sociodemographic factors.64 The cohort with higher burnout was also found to have poorer sleep quality in addition to noteworthy differences between sleep duration, sleep latency, and Pittsburgh Sleep Quality Index scores.64 These findings are consistent with other results reported by Melamed et al.65 In a survey among Japanese physicians working in stroke care in 2011, > 40% of respondents reported clinical burnout.66 Ninety percent of those reporting severe burnout were male, had a median age of 45 years, worked on average 72 hours per week, and slept on average slightly more than 5.5 h per night. In another study of practicing physicians in Japan, burnout and job discontent were directly related to short sleep time, although they were indirectly related to poor work control and high on-call duties.67 Physician control over work time can diminish the negative impact that working night shifts has on sleep quantity and sleep disturbances.68 Junior attendings in academic settings may be especially vulnerable due to the expectation of them not only to carry a higher clinical load but also to be able to be productive with grants or papers.69
Potential Solutions and Future Directions
The literature indicates that structural, organizational, and individual-focused strategies can result in reduction in burnout symptoms.70 However, these strategies have not yet translated into interventions targeting improvements in physician sleep. One reason for this is the failure to recognize the importance of improving sleep and sleep hygiene among practicing physicians, including trainees and early-career physicians. Thus, we do not yet know whether adequate sleep hygiene and safeguarding of sleep can prevent burnout syndrome among physicians and physicians-in-training. Exploring this topic further at the level of cellular metabolism may provide insight. In non-health-care workers, there is evidence that reduction of work hours not only improves sleep but also reduces stress.71
Interestingly, attention to early detection and early intervention of burnout symptoms could lead to minimization of the anxiety and stress associated with work that affect sleep, while simultaneously regularizing and optimizing sleep. Identifying sleep-associated features of burnout should be initiated by institutions, which can lead to identification of individuals at risk for circadian rhythm misalignment and clinical burnout. Programs introduced by the health system/organization to educate and promote healthy sleep practices may lead to minimization and mitigation of clinical burnout, and should be explored. Good sleep hygiene should be encouraged and celebrated within the health-care profession. Habit changes and lifestyle changes are challenging but imperative in this situation. Informing colleagues of burnout and the benefits of receiving adequate sleep is a pillar of improving health, and needs to be included within educational initiatives. Data show that sleep diaries and cognitive behavioral therapy aid in insomnia treatment, and light therapy and melatonin aid in the treatment of circadian disorders.72, 73
Findings suggest that reversibility of burnout syndrome may be contingent on more optimized sleep as a whole.69 Among individuals who have experienced burnout and stopped working subsequently to pursue self-care, in those who underwent treatment, not only were there sleep issues tremendously impaired, but through the process of sleep regularity, the individuals who recovered faster were those who were able to achieve recommended levels of sleep quality and quantity.71
Physician Level
The implementation of healthy sleep practices begins with clinicians. Multiple societies have released recommendations of healthy sleep practices.74, 75 Key recommendations include receiving adequate sleep, avoid drowsy driving, go to bed when tired and not before, set a fixed wake time, and avoid naps (Table 1). Kushner and Ruffin76 described findings in unhealthy practitioners, such as environmental and emotional fatigue, inadequate sleep, shift work disorder, and role strain, and listed these as areas for improvement. Physician control of work time is an important determinant of reduced workplace stress and diminishes the negative impact of night shift and long shifts worked on sleep quality.68 Optimization of schedule flexibility could augment physician empowerment, potentially leading to improved patient care.
Table 1.
Recommendations to Improve Sleep and Burnout in Medicine
| Clinician Level | Institutional Level (By Target) |
||
|---|---|---|---|
| Health Professionals | Culture and Oversight | Scheduling/Work Hygiene | |
|
|||
|
|
|
|
|
|||
|
|
||
|
|||
|
|
|
|
|
|||
|
|||
|
|
|
|
|
|
|
|
|
|
||
|
|||
Organizational Level
Utilization of hospital resources and encouragement of healthy practices can reduce burnout, improve clinician satisfaction, and improve clinician retention.76 A systematic review and meta-analysis of interventions to combat physician burnout suggested such interventions should be tailored not only at the individual level but also at the organizational level.70 Moreover, in a systematic review and meta-analysis by West et al,70 findings did not differ from randomized controlled trials vs observational studies (P = .6; I2 = 0%), and organizational interventions were more successful than individualized interventions (P = .3; I2 = 79%). One could conclude that interventions improving burnout would also lead to improved sleep. The CDC Workplace Health Resource Center recommends that employers provide employees with education, training and assessment, incorporate breaks and napping rooms, recognize fatigue and prevent drowsy driving, and modify the workplace to increase alertness, including changes to lighting, temperature, and noise.77 They have also introduced sleep and fatigue as part of their CDC Worksite Health ScoreCard to help employers provide safe and hazard-free worksites.78
Work Hours
Although reductions in work hours have been implemented for trainee physicians with the suggestion of improved sleep and well-being, these interventions do not extend to practicing physicians. There are reasons to believe that work hour reductions would improve sleep and burnout among practicing physicians. In a Swedish randomized controlled study using sleep diary data, a positive benefit on sleep and perceived stress was noted. These findings were noted following a 25% decrease in work hours, while maintaining a consistent salary.71 Randomization was performed at the workplace level, with participants representing four different working sectors: social services, technical services, care and welfare (including physicians), and call center. During days off, the intervention group reported improved subjective sleep quality, sleepiness, and stress but not sleep duration.
Light Exposure
Most individuals use smartphones throughout the day, every day, and even prior to going to sleep. This scenario is also likely true for physicians, who face heavy documentation requirements in electronic health records.79 Even a small amount of light exposure, depending on timing, can delay or advance the circadian rhythm, potentially leading to insomnia.20, 69 Light exposure can lead to circadian misalignment and is also used in therapy for circadian rhythm disorders.18 It is worth exploring whether reducing nighttime light exposure can improve sleep as well as burnout among physicians.
Conclusions
Physician burnout is well documented in the literature. The role of sleep in the development and implications of burnout demands further investigation. Although multiple studies have noted the relationship between increased stress, burnout, and the consequences of decreased sleep, no studies have yet evaluated the concept of whether improved sleep improves burnout symptoms and clinician health. Because these symptoms can begin in training, no study has evaluated carryover effects of these symptoms into clinical practice. These areas are ripe for future investigation. Investigation into the mechanisms underlying the development of shift work disorder and other circadian rhythm disorders, as well as health and safety consequences, is also warranted. Interventions focused at increasing physician schedule control and improving clinician sleep are needed. An increase in health system awareness of the impact of sleep deprivation and meaningful interventions promoting change are essential.
Acknowledgments
Financial/nonfinancial disclosures: None declared.
References
- 1.Dyrbye L.N., Harper W., Durning S.J. Patterns of distress in US medical students. Med Teach. 2011;33(10):834–839. doi: 10.3109/0142159X.2010.531158. [DOI] [PubMed] [Google Scholar]
- 2.West C.P., Tan A.D., Habermann T.M., Sloan J.A., Shanafelt T.D. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302(12):1294–1300. doi: 10.1001/jama.2009.1389. [DOI] [PubMed] [Google Scholar]
- 3.Shanafelt T.D., Hasan O., Dyrbye L.N. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613. doi: 10.1016/j.mayocp.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 4.Shanafelt T.D., Boone S., Tan L. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377–1385. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 5.Shanafelt T.D., Balch C.M., Bechamps G.J. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250(3):463–471. doi: 10.1097/SLA.0b013e3181ac4dfd. [DOI] [PubMed] [Google Scholar]
- 6.Fahrenkopf A.M., Sectish T.C., Barger L.K. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336(7642):488–491. doi: 10.1136/bmj.39469.763218.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shanafelt T.D., Bradley K.A., Wipf J.E., Back A.L. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136(5):358–367. doi: 10.7326/0003-4819-136-5-200203050-00008. [DOI] [PubMed] [Google Scholar]
- 8.Moss M., Good V.S., Gozal D., Kleinpell R., Sessler C.N. An Official Critical Care Societies collaborative statement: burnout syndrome in critical care healthcare professionals: a call for action. Crit Care Med. 2016;44(7):1414–1421. doi: 10.1097/CCM.0000000000001885. [DOI] [PubMed] [Google Scholar]
- 9.West C.P., Shanafelt T.D., Kolars J.C. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306(9):952–960. doi: 10.1001/jama.2011.1247. [DOI] [PubMed] [Google Scholar]
- 10.Dyrbye L.N., Thomas M.R., Massie F.S. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149(5):334–341. doi: 10.7326/0003-4819-149-5-200809020-00008. [DOI] [PubMed] [Google Scholar]
- 11.Mateen F.J., Dorji C. Health-care worker burnout and the mental health imperative. Lancet. 2009;374(9690):595–597. doi: 10.1016/S0140-6736(09)61483-5. [DOI] [PubMed] [Google Scholar]
- 12.Lee R.T., Ashforth B.E. A meta-analytic examination of the correlates of the three dimensions of job burnout. J Appl Psychol. 1996;81(2):123–133. doi: 10.1037/0021-9010.81.2.123. [DOI] [PubMed] [Google Scholar]
- 13.Maslach C., Jackson S.E., Leiter M.P. CPP Incorporated; Sunnyvale, CA: 1996. MBI: Maslach Burnout Inventory. [Google Scholar]
- 14.Mion G., Libert N., Journois D., Burnout-associated factors in anesthesia and intensive care medicine 2009 survey of the French Society of anesthesiology and intensive care [in French] Ann Fr Anesth Reanim. 2013;32(3):175–188. doi: 10.1016/j.annfar.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 15.Goldberg R., Boss R.W., Chan L. Burnout and its correlates in emergency physicians: four years’ experience with a wellness booth. Acad Emerg Med. 1996;3(12):1156–1164. doi: 10.1111/j.1553-2712.1996.tb03379.x. [DOI] [PubMed] [Google Scholar]
- 16.Wu S., Zhu W., Wang Z., Wang M., Lan Y. Relationship between burnout and occupational stress among nurses in China. J Adv Nurs. 2007;59(3):233–239. doi: 10.1111/j.1365-2648.2007.04301.x. [DOI] [PubMed] [Google Scholar]
- 17.Demerouti E., Bakker A.B., Nachreiner F., Schaufeli W.B. A model of burnout and life satisfaction amongst nurses. J Adv Nurs. 2000;32(2):454–464. doi: 10.1046/j.1365-2648.2000.01496.x. [DOI] [PubMed] [Google Scholar]
- 18.Sheldon S.H., Kryger M.H., Ferber R., Gozal D. Elsevier Health Sciences; Amsterdam, The Netherlands: 2014. Principles and Practice of Pediatric Sleep Medicine: Expert Consult-Online and Print. [Google Scholar]
- 19.American College of Chest Physicians. Most physicians sleep fewer hours than needed for peak performance, report says. ScienceDaily. March 5, 2008. www.sciencedaily.com/releases/2008/03/080304075723.htm. Accessed December 14, 2018.
- 20.National Sleep Foundation. Annual sleep in America poll exploring connections with communications technology use and sleep. March 7, 2011. https://www.sleepfoundation.org/press-release/annual-sleep-america-poll-exploring-connections-communications-technology-use-and. Accessed December 14, 2018.
- 21.Rechtschaffen A., Bergmann B.M., Everson C.A., Kushida C.A., Gilliland M.A. Sleep deprivation in the rat: X. Integration and discussion of the findings. Sleep. 1989;12(1):68–87. [PubMed] [Google Scholar]
- 22.Everson C.A., Crowley W.R. Reductions in circulating anabolic hormones induced by sustained sleep deprivation in rats. Am J Physiol Endocrinol Metab. 2004;286(6):E1060–E1070. doi: 10.1152/ajpendo.00553.2003. [DOI] [PubMed] [Google Scholar]
- 23.Everson C.A., Laatsch C.D., Hogg N. Antioxidant defense responses to sleep loss and sleep recovery. Am J Physiol Regul Integr Comp Physiol. 2005;288(2):R374–R383. doi: 10.1152/ajpregu.00565.2004. [DOI] [PubMed] [Google Scholar]
- 24.Cincin A., Sari I., Oğuz M. Effect of acute sleep deprivation on heart rate recovery in healthy young adults. Sleep Breath Schlaf Atm. 2015;19(2):631–636. doi: 10.1007/s11325-014-1066-x. [DOI] [PubMed] [Google Scholar]
- 25.Davies S.K., Ang J.E., Revell V.L. Effect of sleep deprivation on the human metabolome. Proc Natl Acad Sci U S A. 2014;111(29):10761–10766. doi: 10.1073/pnas.1402663111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xie L., Kang H., Xu Q. Sleep drives metabolite clearance from the adult brain. Science. 2013;342(6156):373–377. doi: 10.1126/science.1241224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Toker S., Shirom A., Shapira I., Berliner S., Melamed S. The association between burnout, depression, anxiety, and inflammation biomarkers: C-reactive protein and fibrinogen in men and women. J Occup Health Psychol. 2005;10(4):344–362. doi: 10.1037/1076-8998.10.4.344. [DOI] [PubMed] [Google Scholar]
- 28.Cherniss C. Praeger; New York, NY: 1980. Professional Burnout in the Human Service Organization. [Google Scholar]
- 29.Shirom A. Job-Related Burnout; Washington, DC: 2003. Handbook of Occupational Health Psychology. [Google Scholar]
- 30.McEwen B.S. Protection and damage from acute and chronic stress: allostasis and allostatic overload and relevance to the pathophysiology of psychiatric disorders. Ann N Y Acad Sci. 2004;1032:1–7. doi: 10.1196/annals.1314.001. [DOI] [PubMed] [Google Scholar]
- 31.Melamed S., Shirom A., Toker S., Berliner S., Shapira I. Burnout and risk of cardiovascular disease: evidence, possible causal paths, and promising research directions. Psychol Bull. 2006;132(3):327–353. doi: 10.1037/0033-2909.132.3.327. [DOI] [PubMed] [Google Scholar]
- 32.Jarral O.A., Baig K., Shetty K., Athanasiou T. Sleep deprivation leads to burnout and cardiothoracic surgeons have to deal with its consequences. Int J Cardiol. 2015;179:70–72. doi: 10.1016/j.ijcard.2014.10.020. [DOI] [PubMed] [Google Scholar]
- 33.Geurts S.A.E., Sonnentag S. Recovery as an explanatory mechanism in the relation between acute stress reactions and chronic health impairment. Scand J Work Environ Health. 2006;32(6):482–492. doi: 10.5271/sjweh.1053. [DOI] [PubMed] [Google Scholar]
- 34.Brosschot J.F., Pieper S., Thayer J.F. Expanding stress theory: prolonged activation and perseverative cognition. Psychoneuroendocrinology. 2005;30(10):1043–1049. doi: 10.1016/j.psyneuen.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 35.Brosschot J.F. Markers of chronic stress: prolonged physiological activation and (un)conscious perseverative cognition. Neurosci Biobehav Rev. 2010;35(1):46–50. doi: 10.1016/j.neubiorev.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 36.Armon G., Shirom A., Shapira I., Melamed S. On the nature of burnout-insomnia relationships: a prospective study of employed adults. J Psychosom Res. 2008;65(1):5–12. doi: 10.1016/j.jpsychores.2008.01.012. [DOI] [PubMed] [Google Scholar]
- 37.Ekstedt M., Fagerberg I. Lived experiences of the time preceding burnout. J Adv Nurs. 2005;49(1):59–67. doi: 10.1111/j.1365-2648.2004.03264.x. [DOI] [PubMed] [Google Scholar]
- 38.Ekstedt M., Söderström M., Akerstedt T. Sleep physiology in recovery from burnout. Biol Psychol. 2009;82(3):267–273. doi: 10.1016/j.biopsycho.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 39.Söderström M., Jeding K., Ekstedt M., Perski A., Akerstedt T. Insufficient sleep predicts clinical burnout. J Occup Health Psychol. 2012;17(2):175–183. doi: 10.1037/a0027518. [DOI] [PubMed] [Google Scholar]
- 40.Söderström M., Ekstedt M., Akerstedt T., Nilsson J., Axelsson J. Sleep and sleepiness in young individuals with high burnout scores. Sleep. 2004;27(7):1369–1377. doi: 10.1093/sleep/27.7.1369. [DOI] [PubMed] [Google Scholar]
- 41.Walker M.P. Sleep-Dependent Memory Processing. Harv Rev Psychiatry. 2008;16(5):287–298. doi: 10.1080/10673220802432517. [DOI] [PubMed] [Google Scholar]
- 42.Carey B. Aging in brain found to hurt sleep needed for memory. New York Times. Section A. January 27, 2013. https://www.nytimes.com/2013/01/28/health/brain-aging-linked-to-sleep-related-memory-decline.html. Accessed December 14, 2018.
- 43.Vandekerckhove M., Cluydts R. The emotional brain and sleep: an intimate relationship. Sleep Med Rev. 2010;14(4):219–226. doi: 10.1016/j.smrv.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 44.Harrison Y., Horne J.A. One night of sleep loss impairs innovative thinking and flexible decision making. Organ Behav Hum Decis Process. 1999;78(2):128–145. doi: 10.1006/obhd.1999.2827. [DOI] [PubMed] [Google Scholar]
- 45.Bonnet M.H., Arand D.L. Clinical effects of sleep fragmentation versus sleep deprivation. Sleep Med Rev. 2003;7(4):297–310. doi: 10.1053/smrv.2001.0245. [DOI] [PubMed] [Google Scholar]
- 46.Fahlén G., Knutsson A., Peter R. Effort-reward imbalance, sleep disturbances and fatigue. Int Arch Occup Environ Health. 2006;79(5):371–378. doi: 10.1007/s00420-005-0063-6. [DOI] [PubMed] [Google Scholar]
- 47.Ota A., Masue T., Yasuda N., Tsutsumi A., Mino Y., Ohara H. Association between psychosocial job characteristics and insomnia: an investigation using two relevant job stress models—the demand-control-support (DCS) model and the effort-reward imbalance (ERI) model. Sleep Med. 2005;6(4):353–358. doi: 10.1016/j.sleep.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 48.Urponen H., Vuori I., Hasan J., Partinen M. Self-evaluations of factors promoting and disturbing sleep: an epidemiological survey in Finland. Soc Sci Med 1982. 1988;26(4):443–450. doi: 10.1016/0277-9536(88)90313-9. [DOI] [PubMed] [Google Scholar]
- 49.Akerstedt T., Knutsson A., Westerholm P., Theorell T., Alfredsson L., Kecklund G. Sleep disturbances, work stress and work hours: a cross-sectional study. J Psychosom Res. 2002;53(3):741–748. doi: 10.1016/s0022-3999(02)00333-1. [DOI] [PubMed] [Google Scholar]
- 50.Williamson A.M., Feyer A.M. Moderate sleep deprivation produces impairments in cognitive and motor performance equivalent to legally prescribed levels of alcohol intoxication. Occup Environ Med. 2000;57(10):649–655. doi: 10.1136/oem.57.10.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Linton S.J. Does work stress predict insomnia? A prospective study. Br J Health Psychol. 2004;9(Pt 2):127–136. doi: 10.1348/135910704773891005. [DOI] [PubMed] [Google Scholar]
- 52.Johnson K.M., Simon N., Wicks M., Barr K., O’Connor K., Schaad D. Amount of sleep, daytime sleepiness, hazardous driving, and quality of life of second year medical students. Acad Psychiatry. 2017;41(5):669–673. doi: 10.1007/s40596-017-0668-6. [DOI] [PubMed] [Google Scholar]
- 53.Wolf M.R., Rosenstock J.B. Inadequate sleep and exercise associated with burnout and depression among medical students. Acad Psychiatry. 2017;41(2):174–179. doi: 10.1007/s40596-016-0526-y. [DOI] [PubMed] [Google Scholar]
- 54.Fletcher K.E., Nickoloff S., Whittle J., Jackson J.L., Frank M., Schapira M.M. Why residents consider working beyond the duty hour limits: implications of the ACGME 2011 duty hour standards. J Grad Med Educ. 2011;3(4):571–573. doi: 10.4300/JGME-D-11-00069.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rosen I.M., Gimotty P.A., Shea J.A., Bellini L.M. Evolution of sleep quantity, sleep deprivation, mood disturbances, empathy, and burnout among interns. Acad Med. 2006;81(1):82–85. doi: 10.1097/00001888-200601000-00020. [DOI] [PubMed] [Google Scholar]
- 56.Parshuram C.S., Dhanani S., Kirsh J.A., Cox P.N. Fellowship training, workload, fatigue and physical stress: a prospective observational study. CMAJ. 2004;170(6):965–970. doi: 10.1503/cmaj.1030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lockley S.W., Cronin J.W., Evans E.E. Effect of reducing interns’ weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351(18):1829–1837. doi: 10.1056/NEJMoa041404. [DOI] [PubMed] [Google Scholar]
- 58.5. Impact of duty hours on resident well-being. In: Institute of Medicine (US) Committee on Optimizing Graduate Medical Trainee (Resident) Hours and Work Schedule to Improve Patient Safety; Ulmer C, Miller Wolman D, Johns MME, eds. Resident Duty Hours: Enhancing Sleep, Supervision, and Safety. Washington, DC: National Academies Press (US); 2009. https://www.Ncbi.Nlm.Nih.Gov/Books/NBK214939/. Accessed February 5, 2019. [PubMed]
- 59.Fletcher K.E., Underwood W., Davis S.Q., Mangrulkar R.S., McMahon L.F., Saint S. Effects of work hour reduction on residents’ lives: a systematic review. JAMA. 2005;294(9):1088–1100. doi: 10.1001/jama.294.9.1088. [DOI] [PubMed] [Google Scholar]
- 60.Bilimoria K.Y., Chung J.W., Hedges L.V. National cluster-randomized trial of duty-hour flexibility in surgical training. N Engl J Med. 2016;374(8):713–727. doi: 10.1056/NEJMoa1515724. [DOI] [PubMed] [Google Scholar]
- 61.Desai S.V., Asch D.A., Bellini L.M. Education outcomes in a duty-hour flexibility trial in internal medicine. N Engl J Med. 2018;378(16):1494–1508. doi: 10.1056/NEJMoa1800965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Basner M., Dinges D.F., Shea J.A. Sleep and alertness in medical interns and residents: an observational study on the role of extended shifts. Sleep. 2017;40(4) doi: 10.1093/sleep/zsx027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wallace J.E., Lemaire J.B., Ghali W.A. Physician wellness: a missing quality indicator. Lancet. 2009;374(9702):1714–1721. doi: 10.1016/S0140-6736(09)61424-0. [DOI] [PubMed] [Google Scholar]
- 64.Vela-Bueno A., Moreno-Jiménez B., Rodríguez-Muñoz A. Insomnia and sleep quality among primary care physicians with low and high burnout levels. J Psychosom Res. 2008;64(4):435–442. doi: 10.1016/j.jpsychores.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 65.Melamed S., Ugarten U., Shirom A., Kahana L., Lerman Y., Froom P. Chronic burnout, somatic arousal and elevated salivary cortisol levels. J Psychosom Res. 1999;46(6):591–598. doi: 10.1016/s0022-3999(99)00007-0. [DOI] [PubMed] [Google Scholar]
- 66.Nishimura K., Nakamura F., Takegami M. Cross-sectional survey of workload and burnout among Japanese physicians working in stroke care: the nationwide survey of acute stroke care capacity for proper designation of comprehensive stroke center in Japan (J-ASPECT) study. Circ Cardiovasc Qual Outcomes. 2014;7(3):414–422. doi: 10.1161/CIRCOUTCOMES.113.000159. [DOI] [PubMed] [Google Scholar]
- 67.Tokuda Y., Hayano K., Ozaki M., Bito S., Yanai H., Koizumi S. The interrelationships between working conditions, job satisfaction, burnout and mental health among hospital physicians in Japan: a path analysis. Ind Health. 2009;47(2):166–172. doi: 10.2486/indhealth.47.166. [DOI] [PubMed] [Google Scholar]
- 68.Tucker P., Bejerot E., Kecklund G., Aronsson G., Åkerstedt T. The impact of work time control on physicians’ sleep and well-being. Appl Ergon. 2015;47:109–116. doi: 10.1016/j.apergo.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 69.Sakshi D., Ayas N., Gozal D. Sleep and physician burnout. American Thoracic Society. November 1, 2018 www.thoracic.org/about/ats-podcasts/sleep-and-physicianburnout.php Accessed November 30, 2018. [Google Scholar]
- 70.West C.P., Dyrbye L.N., Erwin P.J., Shanafelt T.D. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet Lond Engl. 2016;388(10057):2272–2281. doi: 10.1016/S0140-6736(16)31279-X. [DOI] [PubMed] [Google Scholar]
- 71.Schiller H., Lekander M., Rajaleid K. The impact of reduced worktime on sleep and perceived stress—a group randomized intervention study using diary data. Scand J Work Environ Health. 2017;43(2):109–116. doi: 10.5271/sjweh.3610. [DOI] [PubMed] [Google Scholar]
- 72.Saddichha S. Diagnosis and treatment of chronic insomnia. Ann Indian Acad Neurol. 2010;13(2):94–102. doi: 10.4103/0972-2327.64628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dodson E.R., Zee P.C. Therapeutics for circadian rhythm sleep disorders. Sleep Med Clin. 2010;5(4):701–715. doi: 10.1016/j.jsmc.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mukherjee S., Patel S.R., Kales S.N. An official American Thoracic Society statement: the importance of healthy sleep. Recommendations and future priorities. Am J Respir Crit Care Med. 2015;191(12):1450–1458. doi: 10.1164/rccm.201504-0767ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Consensus Conference Panel. Watson N.F., Badr M.S. Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society on the recommended amount of sleep for a healthy adult: methodology and discussion. Sleep. 2015;38(8):1161–1183. doi: 10.5665/sleep.4886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kushner J., Ruffin T. Empowering a healthy practice environment. Nurs Clin North Am. 2015;50(1):167–183. doi: 10.1016/j.cnur.2014.10.013. [DOI] [PubMed] [Google Scholar]
- 77.Centers for Disease Control. Workplace Health Resource Center. Sleep: an important health and safety concern at work. January 2019. https://www.cdc.gov/Workplacehealthpromotion/Initiatives/Resource-Center/Pdf/WHRC-Brief-Sleep-508.pdf. Accessed February 5, 2019.
- 78.Centers for Disease Control. Worksite Health ScoreCard. January 2019. https://www.cdc.gov/workplacehealthpromotion/initiatives/healthscorecard/pdf/CDC-Worksite-Health-ScoreCard-Manual-Updated-Jan-2019-FINAL-rev-508.pdf. Accessed February 5, 2019.
- 79.Sinsky C., Colligan L., Li L. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med. 2016;165(11):753. doi: 10.7326/M16-0961. [DOI] [PubMed] [Google Scholar]