Abstract
Throughout the industrialized world, nearly one in five employees works some form of nontraditional shift. Such shift work is associated with numerous negative health consequences, ranging from cognitive complaints to cancer, as well as diminished quality of life. Furthermore, a substantial percentage of shift workers develop shift work disorder, a circadian rhythm sleep disorder characterized by excessive sleepiness, insomnia, or both as a result of shift work. In addition to adverse health consequences and diminished quality of life at the individual level, shift work disorder incurs significant costs to employers through diminished workplace performance and increased accidents and errors. Nonetheless, shift work will remain a vital component of the modern economy. This article reviews seminal and recent literature regarding shift work, with an eye toward real-world application in clinical and organizational settings.
Key Words: fatigue, occupational health, shift work disorder, sleep, workplace
Abbreviations: FRMP, fatigue risk management program; MSLT, multiple sleep latency test; SWD, shift work disorder
Throughout the industrialized world, 24-h operations are necessary for public safety and health and are frequently economically advantageous. As a result, in many nations, approximately one in five working adults works a nontraditional shift outside “regular” 9:00 am to 5:00 pm hours. A subset of shift workers develops shift work disorder (SWD), a condition that is triggered by circadian misalignment and which results in insomnia and/or excessive sleepiness. These individuals experience significant negative health consequences and diminished quality of life as a result of shift work. Furthermore, at the societal level, SWD is associated with dramatically increased accident risk and thus financial costs borne by employers and the public.
Recent scientific discoveries have advanced understanding of individual differences in tolerance to shift work and expanded treatment options for individuals with SWD. However, efforts to reduce the burden of shift work in the workplace remain in their infancy. Although data remain scant, from an organizational perspective, reducing the costs associated with shift work has the potential to realize significant financial gain. The purpose of the present article therefore was to synthesize the available evidence regarding shift work from clinical and organizational perspectives. We first present the general characteristics of shift work. The etiology and consequences of shift work disorder are then reviewed. Finally, recommendations are made for both clinicians and occupational health leaders in industries with 24-h or shift work operations.
Definition and Prevalence of Shift Work
Although the term “shift work” lacks a consistent definition,1 shift work has been defined as occurring when at least a portion of the shift occurs between 7:00 pm and 6:00 am.2 In the United States, the work schedules of nearly 20% of employed adults meet this definition, with 18% to 26% of workers beginning their shift between 2:00 pm and 6:30 am.3 Shift work is similarly common across nations on multiple continents, including the United Kingdom (22%), Greece and Finland (25%), the Czech Republic (24%), Chile (15%), China (17.5%), and Senegal (20%).4, 5 The US Bureau of Labor Statistics has recognized certain Standard Occupational Classification groups that require overnight hours or early start times (Table 1).6, 7
Table 1.
Shift Work Occupations According to US Bureau of Labor Statistics Standard Occupational Classifications
| Occupation | Classification |
|---|---|
| 11-0000 Management occupations | Industrial production managers; transportation managers, storage and distribution managers; farmers, ranchers and other agricultural managers; construction managers; food service managers; gaming managers; lodging managers; computer and information systems managers; medical and health services managers; emergency management directors |
| 15-0000 Computer and mathematical operations | Information security analysts; computer support specialists |
| 17-0000 Architecture and engineering occupations | Aerospace engineers; chemical engineers; civil engineers; industrial engineers, including health and safety; mechanical engineers; mining safety engineers; nuclear engineers; petroleum engineers; aerospace engineering and operations technicians; civil engineering technicians; electrical and electronics engineering technicians; industrial engineering technicians; mechanical engineering technicians |
| 19-0000 Life, physical, and social sciences | Astronomers and physicists; atmospheric and space scientists; clinical and counseling psychologists; biological technicians; chemical technicians; geological and petroleum technicians; nuclear technicians; forensic science technicians; forest and conservation technicians |
| 21-0000 Community and social service occupations | Substance abuse and behavioral disorder counselors; marriage and family therapists; mental health counselors; rehabilitation counselors; child, family and school social workers; healthcare social workers; mental health and substance abuse social workers; probation officers and correctional treatment specialists; social and human service assistants; clergy; directors of religious activities and education |
| 23-0000 Legal occupations | Lawyers and judicial law clerks; judges, magistrates and other judicial workers; legal support workers |
| 25-0000 Education, training, and library occupations | Postsecondary teachers; adult basic and secondary education and literacy teachers and instructors; librarians and library technicians |
| 27-0000 Arts, design, entertainment, sports, and media occupations | Actors, producers, directors; athletes, coaches, umpires, and related workers; dancers and choreographers; musicians, singers, and related workers; other entertainers and performers, sports, and related workers; announcers; news analysts, reporters, and correspondents; public relations specialists; writers and editors; other media and communications workers; broadcast and sound engineering technicians and radio operators; photographers; television, video, and motion picture camera operators and editors |
| 29-0000 Health-care practitioners and technical operations | Chiropractors; pharmacists; physicians and surgeons; physicians assistants; podiatrists; respiratory therapists; veterinarians; registered nurses; nurse anesthetists; nurse midwives; nurse practitioners; miscellaneous health diagnosing and treating practitioners; health technologists; clinical laboratory technologists and technicians; diagnostic related technologists and technicians; emergency medical technicians and paramedics; health practitioner support technologists and technicians; licensed practical and vocational nurses; medical records and health information technologists; occupational health and safety specialists and technicians; athletic trainers; other health care practitioners and technical workers |
| 31-0000 Health-care support occupations | Nursing, psychiatric and home health aides; occupational and physical therapy assistants; massage therapists; medical equipment preparers; pharmacy aides; veterinarian assistants and laboratory animal caretakers; phlebotomists |
| 33-0000 Protective service occupations | Supervisors of protective service workers; fire-fighting and prevention workers; fire inspectors and investigators; forest fire firefighters, inspectors; bailiffs, correctional officers, and jailers; detectives and criminal investigators; police officers; animal control workers; private detectives and investigators; security guards and gaming surveillance officers; transportation security screeners |
| 35-0000 Food preparation and serving related occupations | Chefs and cooks; bartenders; waiters and servers; dishwashers; hosts and hostesses |
| 37-0000 Building and grounds cleaning and maintenance occupations | Building cleaning workers and supervisors |
| 39-0000 Personal care and service occupations | Gaming and slot service workers and supervisors; Nonfarm animal caretakers; motion picture projectionists; ushers, lobby attendants, and ticket takers; amusement and recreation attendants; costumers; locker room, coatroom, and dressing room attendants; funeral service workers- embalmers, morticians, and funeral attendants; baggage, porters, bellhops, and concierges; child care workers; personal care aides; fitness trainers and fitness workers |
| 41-0000 Sales and related occupations | Cashiers; counter and rental clerks; telemarketers |
| 43-0000 Office and administrative support occupations | Switchboard operators including answering service; Telephone operators; gaming cage workers; hotel, motel, and resort desk clerks; cargo and freight agents; dispatchers for police, fire, and ambulance; stock clerks and order fillers; insurance claim and policy clerks |
| 45-0000 Farming, fishing, and forestry occupations | Farm workers and laborers; fishers and related fishing workers; logging workers |
| 47-0000 Construction and extraction occupations | Construction laborers and supervisors; construction equipment operators; highway maintenance workers; extraction workers (derrick, earth, explosive, mining, and quarry) |
| 49-0000 Installation, maintenance, and repair occupations | Computer, automated teller, and office machine repairers; avionics technicians; electrical and electronic repairers, substations, powerhouse, and relay; aircraft maintenance and service technicians; bus and truck mechanics and diesel engine specialists |
| 51-0000 Production occupations | Bakers; food processing workers; metal and plastics workers; printing workers; operators of power plants, nuclear plants, boilers, chemical and gas, petroleum |
| 53-0000 Transportation and material moving occupations | Aircraft cargo handlers; airline pilots, copilots and flight engineers; traffic controllers and airfield operations specialists; flight attendants; ambulance drivers and attendants; bus drivers; tractor trailer drivers; locomotive engineers and operators; railroad brake, signal, and switch operators; railroad conductors and yardmasters; subway and streetcar operators; sailors and marine oilers; ship and boat captains, mates, and pilots; bridge and lock tenders; parking lot attendants |
| 55-0000 Military-specific occupations | Air crew, aircraft launch, and recovery officers; armored assault vehicle officers; artillery and missile officers; command and central officers; infantry officers; special forces officers; enlisted tactical operations and air/weapon specialists and crew members |
Rates of shift work are particularly high in service occupations.6, 7 Nearly one-half of protective service (eg, law enforcement and fire safety) and food preparation/food service employees work shifts, as do one-quarter of transportation (eg, airline pilots and train and bus drivers) and health-care workers.3 Shift schedules frequently vary by industry and include permanent night shifts starting between 6:00 pm and 4:00 am, early morning shifts starting between 4:00 am and 7:00 am, and afternoon/evening shifts starting between 2:00 pm and 6:00 pm.8 Importantly, between 2.7% and 4.3% of US workers work rotating shifts, which can be classified as rapid shifting (eg, multiple schedule changes per week) or slow shifting (eg, multiple weeks per schedule).9 Other common shift alternatives include split shifts (ie, when some hours are worked during the nighttime) and irregular shifts in which the employee’s hours are not predictable.10
Shift Work and Sleep Physiology
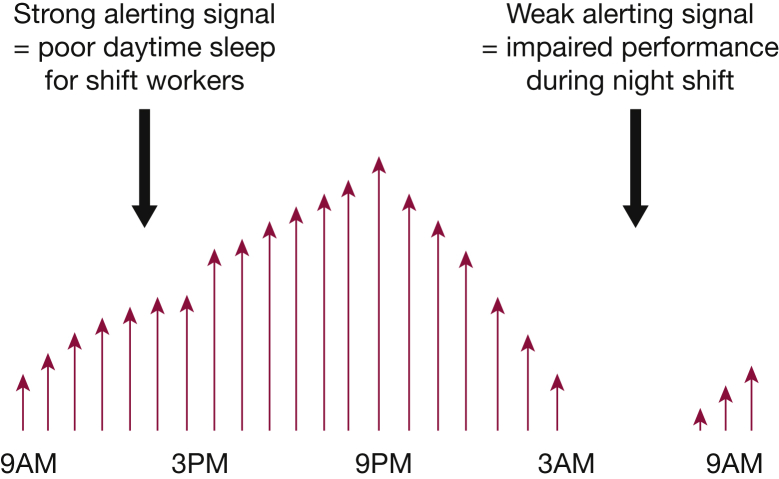
From a physiologic perspective, shift work requires a sleep-wake schedule that regularly conflicts with the natural, endogenous rhythm of sleep and wakefulness. As a result, a subset of shift workers experience impairments in both sleep and wakefulness that stem from the desynchronization of the two processes that regulate these physiologic functions. Current ideas of determinants of sleep/wakefulness revolve around the “two-process” model.11 In this model, the tendency to sleep is regulated by the interaction between a “homeostatic pressure” to sleep and a “circadian alerting signal” that encourages wakefulness. The homeostatic pressure for sleep increases with each hour of wakefulness and dissipates with sleep. The circadian alerting signal is regulated primarily in the suprachiasmatic nucleus of the anterior hypothalamus. This intrinsic pacemaker confers circadian rhythmicity of approximately 24.2 h not only to sleep and wakefulness but also to many physiologic functions that vary across the day, such as body temperature, blood pressure, and hormone secretion, including cortisol and melatonin.12, 13 As the homeostatic pressure for sleep rises during the day, the circadian alerting signal also rises to facilitate wakefulness.14 After the onset of sleep, as homeostatic sleep pressure decreases, the circadian alerting signal also then subsides. Figure 1 presents the mismatch between the biologically regulated circadian alerting signal and sleep and work performance among night shift workers.15
Figure 1.
Shift workers struggle to sleep during the day and experience impaired workplace performance at night. Vertical arrows depict the circadian alerting signal, which rises throughout the day and decreases during the biological night.
(Based on Wickwire.15 Used with permission.)
The synchronization of circadian rhythms to the 24-h cycle is largely maintained by external and environmental cues. The natural light/dark cycle is the strongest of these circadian regulators. When light enters the eyes (or transmits through closed eyelids), photic stimuli are transmitted via retinohypothalamic and retino-geniculo-hypothalamic pathways to the suprachiasmatic nucleus. This action results in suppression of melatonin from the pineal gland.16, 17 In turn, central and peripheral melatonin receptors regulate the aforementioned physiologic functions. Melatonin levels are low during the day, then rise in the evening to suppress CNS arousal and set the stage for sleep onset.18 The onset of melatonin secretion under conditions of low light (ie, dim-light melatonin onset) is the single most accurate marker for assessing circadian phase. The onset of daylight suppresses melatonin secretion, thus signaling to the internal clock that it is day and time to arise.
In shift workers, these two opponent processes become uncoupled, negatively affecting both sleep and wakefulness; that is, external “day” is no longer synchronized with high alerting and low melatonin secretion. For example, night shift workers frequently sleep during the day, precisely when the circadian alerting signal is strongest. As a result, daytime sleep is short and fragmented, leading to homeostatic sleep debt and blunted circadian arousal at nighttime. Furthermore, night work is expected to occur precisely at a time when circadian alerting signals are at their lowest, and sleepiness is at its greatest. In such instances, shift workers experience the consequences of excessive sleepiness at work, when wakefulness is required. Lower stimulation (eg, dimmer light, quieter, less bustle) frequently present at night further unmasks a high propensity for sleep. Indeed, unintended sleep does occur during night shift, with 7% of workers falling asleep at work several times per month,19 a particular concern in safety-sensitive environments.20
Individual Differences in Shift Workers
Shift workers exhibit significant variability in their tolerance for and adaptation to shift work.21 Individual differences have been identified in the degree of sleepiness during the night,22 ability to sleep during the daytime, and degree of performance impairment.23, 24 The mechanisms for this variation in individual workers’ ability to sustain alertness during shift work and to obtain adequate sleep during nonworking times are complex and not completely understood. For example, even though it is well established that shift workers obtain about 10 fewer hours of sleep per week than day shift workers,19 this sleep deficiency does not fully explain the observed variability in nighttime sleepiness among shift workers. One possible genetically linked trait is “morningness/eveningness.” This trait refers to periods during the day when individuals are most awake and active. “Morning larks” are individuals who are most awake and functional in the early morning hours; other individuals (eg, “night owls”) may be more awake and functional during the late afternoon or evening hours. Morning vs evening preference is at least partially linked to the period of the circadian clock and a length polymorphism of the PER3 “clock” gene that regulates sleep and wakefulness. Circadian preference or tendency (ie, morningness-eveningness) has been hypothesized to modulate tolerance to shift work.25 Morning types exhibit reduced tolerance for shift work.26 Furthermore, polymorphisms in the coding region of the PER3 gene might explain resistance to sleepiness as well as performance decrements resulting from sleep deficiency,27 which is ubiquitous among shift workers.28
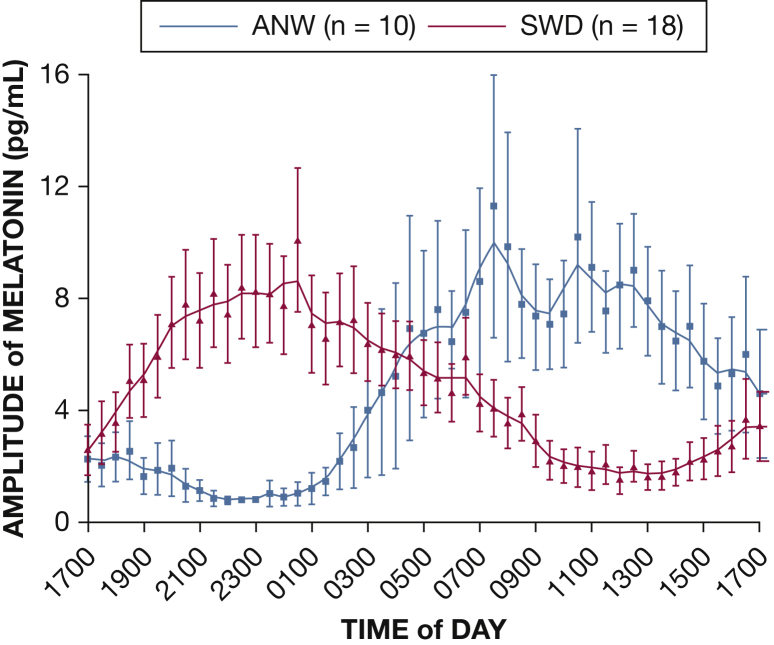
In addition to genetic polymorphisms, melatonin profiles and dim-light melatonin onset have been shown to discriminate between asymptomatic shift workers and those who develop SWD,29, 30 suggesting differences in adaptability of the internal circadian clock (Fig 2). Finally, multiple work-related and person-level factors have been found to moderate the effects of shift work, including time of shift, duration of shift, and constancy of shift schedule. Person-level factors that influence adaptability to shift work include shift work history, concomitant sleep disorders and/or medical and psychiatric conditions, medication use, and amount of time in bed over the past several weeks, as well as social and family responsibilities.24
Figure 2.
Melatonin profiles of night workers with and without shift work disorder (SWD). Shift workers demonstrate remarkable diversity in degree of circadian adaptation to shift work schedules. A study62 evaluated the dim light salivary melatonin profiles of 10 asymptomatic night workers (ANW) and 18 workers with SWD during a 25-h sleep deprivation protocol. Notably, the melatonin profiles of those with SWD were similar to those of healthy day workers (20:27 ± 5.0 h), suggesting minimal circadian adaptation to shift work. However, the ANW group exhibited significantly delayed dim-light melatonin onset (5:00 ± 3.4 h), indicating better circadian adaptation to the shift work schedule.
(Reproduced from Gumenyuk et al29 with permission from the Associated Professional Sleep Societies, Inc.)
SWD: Diagnostic Criteria, Prevalence, and Consequences
Not surprisingly, a percentage of shift workers develop SWD, a circadian rhythm sleep-wake disorder recognized in all major diagnostic nosologies. SWD is characterized by excessive sleepiness during the desired waking period and/or insomnia when sleep is allowed. Furthermore, symptoms must not be attributable to another sleep disorder, medical condition, or medication effect. Table 2 presents diagnostic criteria from the Diagnostic and Statistical Manual for Mental Disorders, Fifth Edition,31 and International Classification of Sleep Disorders, 3rd Edition.8
Table 2.
Diagnostic Criteria for Shift Work Sleep Disorder
| International Classification of Sleep Disorders, Third Edition: general criteria for any circadian rhythm sleep disorder (ICD-10 G47.26) |
| A. A persistent or recurrent pattern of sleep disturbance is present and due primarily to the following: |
| i. Alterations in the circadian time-keeping system; and/or |
| ii. Misalignment between the endogenous circadian rhythm and exogenous factors that affect the timing and/or duration of sleep |
| B. The circadian-related sleep disturbance results in insomnia and/or excessive sleepiness |
| C. Sleep disturbance is associated with impairment of social, occupational, and/or other waking functioning |
| Specific criteria for circadian rhythm sleep disorder, shift work type (ICD-10 G47.26) |
| A. Insomnia and/or excessive sleepiness is present and temporally associated with a work schedule that regularly overlaps the usual time for sleep |
| B. Symptoms are associated with the shift work schedule for duration ≥ 1 month |
| C. Sleep log or actigraphy monitoring (with sleep diaries) for ≥ 7 days demonstrates circadian and sleep-time misalignment |
| D. Symptoms are not better explained by another sleep, medical, neurologic, or mental disorder, medication use, or substance use |
| Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition: diagnostic criteria for circadian rhythm sleep disorder (307.45) |
| A. Recurrent pattern of sleep disruption that is primarily due to alteration of the circadian system or to a misalignment between the endogenous circadian rhythm and the sleep-wake schedule required by an individual’s physical environment or social or professional schedule |
| B. Sleep disturbance results in insomnia and/or excessive sleepiness |
| C. Sleep disturbance results in clinically significant distress or impairment in social, occupational, and/or other waking functioning |
| Shift work type: 307.45 (G47.26) |
| Insomnia during the major sleep period and/or excessive sleepiness (including unintentional sleep) during the major wake period is associated with a shift work schedule |
ICD-10 = International Classification of Diseases, 10th Revision.
Although the true prevalence of SWD is understudied, evidence suggests that more than one in five shift workers experiences SWD. A seminal population-based, random-digit dialed telephonic community sample of day shift, night shift, and rotating shift workers found that 14.1% to 32% of night workers (n = 174) and 8.1% to 26% of rotating shift workers (n = 360) met Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, criteria for SWD.24 An investigation of oil rig workers working shifts in the North Sea (N = 103) yielded a similar prevalence rate of 23%.32 Although not a population-based study, Barger et al33 reported higher prevalence rates of 39.2% to 43.0% for sleep physician-diagnosed “definite” SWD and an additional 26.7% to 22.8% for “probable” SWD among a sample of shift workers (N = 311). Notably, these investigators did not control for insomnia in day shift workers, which might partially explain the increased prevalence of SWD. In aggregate, these studies suggest a population prevalence of SWD in the United States of 2% to 5%.8
Person-level variables and demographic characteristics also affect SWD. The most well studied of these factors is age. Evidence suggests that older shift workers accrue more sleep loss than younger shift workers,34 are less able to adapt to the altered circadian requirements of shift work,35 report higher levels of excessive sleepiness and more disturbed sleep as a result of shift work,28, 35, 36 and are less responsive to the phase-shifting effects of light.37 Insomnia also increases with age, which might increase vulnerability to SWD in this population. Although the exact neurophysiologic mechanisms remain unclear, it seems that increased vulnerability with age is due to changes affecting the homeostatic and circadian sleep-wake systems. For example, well-documented neurodegeneration in the suprachiasmatic nucleus has been associated with the shortened circadian phase among older adults.38 It is possible that older adults’ preferences for morningness might particularly explain their increased vulnerability to SWD.39
In addition to age, the role of sex has been evaluated in relation to SWD. Although most SWD research has been conducted among male subjects, female shift workers report relatively more sleep loss, daytime sleepiness, and psychological distress.40, 41 Nonetheless, it is unclear whether these differences are due to sex-related differences in sleep, job assignment, expected roles on returning home, or some other reason.
Robust evidence illustrates the adverse health consequences of shift work. Relative to non-shift work control subjects, shift workers experience more sleep loss, excessive sleepiness, and insomnia.24 Medical complications include increased risk for cardiovascular disease,42 cerebrovascular events and stroke,43 obesity2 and metabolic disorders,44, 45 GI complaints,46 poor sexual health (including reduced fertility and problems during pregnancy),47 and multiple forms of cancer.48, 49, 50 From a mental health perspective, shift workers experience more psychiatric disease and greater psychosocial distress, including depression,24 anxiety,51 alcohol abuse,52 and work stress spillover as well as poorer quality of life. More recent neuroimaging data suggest altered neurophysiologic function in attention and memory domains associated with SWD relative to non-SWD night shift workers.53
The most immediate adverse consequences of shift work are related to impaired neurocognitive performance and subsequent increased risk for accidents and errors. Sleep loss dramatically impairs neurobehavioral performance, with 24 h of sustained wakefulness resulting in performance decrements equal to a blood-alcohol concentration of 0.10, which is over the legal limit in most states.54 At the same time, many shift workers commute to and from home during the early morning hours, when the circadian alerting signal is at its lowest.12, 55 It is thus perhaps not surprising that shift work greatly increases the risk for motor vehicle crashes.56, 57, 58, 59 To address these risks and others, recent efforts have sought to increase public awareness and prevention of drowsy driving by establishing consensus standards for minimal sleep within the past 24 h.60 In addition to motor vehicle crashes, workplace accidents have been found to be 60% higher among shift workers, resulting in a total cost of $71 to $93 billion per annum.59
Clinical Recommendations
Assessment
As with all circadian rhythm sleep disorders, the cornerstone of SWD assessment is the clinical interview, including careful review of the general and psychiatric medical history and medication profile. A careful sleep history is essential to the evaluation of the shift work patient. Clinicians should not only elucidate the temporal nature and antecedents of sleep-wake complaints but also seek to discern the regularity, duration, and timing of sleep. Unfortunately, it is well documented that sleep assessment is generally not emphasized in medical education.61 Table 3 presents the basic elements of a sleep history as conducted by a fictitious nurse, Ms BAMS-RN. In addition, because hypersomnolence can be a core characteristic of SWD, it is essential to rule out other causes of observed sleepiness, including sleep disorders such as OSA and narcolepsy. Clinical assessment of circadian desynchrony, sleepiness, sleep disturbance, and the multiple comorbidities known to be associated with shift work are reviewed here.
Table 3.
Elements of Sleep History
| B | Bedtime | Time in bed |
| Time lights out | ||
| Perceived sleep latency | ||
| A | Awakenings | Number |
| Timing | ||
| Perceived duration | ||
| Reasons (eg, nocturia, rumination) | ||
| M | Maladaptive sleep behaviors | Alcohol within 2 h of bed |
| Caffeine within 6 h of bed | ||
| Inconsistent presleep routine or engaging in stimulating activities before bed: planning, worry, professional activities, housework, finances, computer | ||
| Television/electronics in bed or bedroom | ||
| S | Snoring | Loud snoring |
| Snorting/gasping | ||
| Witnessed apneas | ||
| R | Rise time | Time awake |
| Time out of bed | ||
| Feel refreshed | ||
| Dry mouth | ||
| Headache | ||
| N | Naps | Timing |
| Duration | ||
| Other daytime sleepiness |
Patient Preferences and Goals for Treatment
Successful adaptation to shift work requires lifestyle change. Thus, because motivation and adherence are central to SWD outcomes, patient preferences should be assessed in detail. Clinicians should assess patient goals for treatment, including not only sleep but also specific and measurable quality of life outcomes (eg, social or recreational engagement) that the patient hopes to gain from treatment. Clinicians should be aware that even preferred shifts can be associated with adverse outcomes. For example, among health-care professionals, 12-h shifts have become popular and are standard in many institutions. Indeed, 12-h shifts are often preferred by workers because they allow for a shorter workweek of 3 days. However, in a study using sleep diaries, actigraphy findings, and objective test results of cognition and sleepiness, Geiger-Brown et al62 found progressive sleep debt and performance deficits in nurses working 12-h night shifts in critical care units. Furthermore, the results suggest that sleep deficits during the day contributed to these adverse outcomes.
Circadian Dysregulation
A central criterion to establish a diagnosis of SWD is that sleepiness and/or sleep disturbance are the result of circadian dysregulation due to shift work. It is thus necessary to conduct a detailed assessment of the patient’s sleep-wake schedule using (at a minimum) subjective sleep diaries. In some cases, objective evidence of sleep-wake activities can be obtained by using actigraphy.63 A minimum of 7 days’ sleep monitoring is required for a diagnosis of SWD, which should include both work and nonwork days.64 Clinicians should pay particular attention to consistency of sleep/wake schedule across workdays and nonwork days. Assessment of melatonin secretion, especially dim-light melatonin onset using salivary or plasma melatonin measured hourly, can provide valuable insight into the degree of circadian misalignment. However, in clinical practice, salivary or plasma melatonin assays are typically not feasible due to cost and time constraints. Despite the absence of clinically useful assessment of melatonin secretion, other measures of circadian phase can be nonetheless be considered. For example, in our professional experience, both direct and indirect measures of core body temperature (eg, asking a patient to record rectal or oral temperature every 2 h for three consecutive 24-h periods) can provide valuable clinical insight.
Sleepiness
The measurement standard for objective sleepiness is the multiple sleep latency test (MSLT). Among US adults, the mean sleep-onset latency during the MSLT is 11.4 min, with a mean sleep-onset latency < 8 min often used to indicate abnormal sleepiness.8, 65 Among patients with SWD, mean sleep-onset latency during MSLT ranges from approximately 2 min to 3.6 min.66, 67, 68 Nonetheless, there are currently no evidence-based norms for sleepiness in shift workers. Due to this limitation and the high cost of the MSLT, sleepiness is commonly assessed in clinical practice via self-report measures such as the Epworth Sleepiness Scale,69 which measures general or trait sleepiness. More than four in 10 night shift workers (44%)24 and nearly one-third of day workers (24%-33%)70, 71 report pathologic levels of sleepiness on the Epworth Sleepiness Scale (ie, score > 10). For assessing real-time or state sleepiness on the job, other measures such as the Karolinska Sleepiness Scale can also be used.72 Because sleepiness is often a core symptom of SWD, it is essential to first rule out other organic causes of sleepiness (eg, OSA, narcolepsy) during assessment and second to monitor and document sleepiness throughout treatment as an important outcome metric.
Sleep Disturbance
Patients with SWD are likely to report insufficient sleep, difficulty staying asleep, and/or poor quality sleep on both workdays and nonwork days. As mentioned earlier, detailed sleep history and monitoring via sleep diaries and/or actigraphy is essential.64 Two characteristics of sleep among shift workers bear mention. First, most shift workers seek to return to their “normal” schedule on off days73 so that they are able to spend time with friends and family and engage in recreational activities. As such, nearly all shift workers endure rapidly shifting schedules, which worsen sleep and sleepiness. Second, many shift workers are able to fall asleep quickly, but after several hours of daytime sleep are awoken by the increasing circadian alerting signal. They are thus unable to maintain sleep, and they develop acute and chronic insufficient sleep. Validated psychometric measures such as the Insomnia Severity Index74 and the Pittsburgh Sleep Quality Index75 can help quantify the severity of sleep disturbance and associated consequences. However, it is important to note that without modification, these questionnaire measures cannot discriminate nighttime and daytime sleep disturbance. Careful and comprehensive clinical assessment is essential.
Medical and Psychiatric Comorbidities
Shift workers are at increased risk for cardiovascular disease, cancer, depression, and poor cognitive performance. Therefore, these conditions should be evaluated at regular intervals by using standardized risk assessments where possible (eg, standard age-specific cancer screening). In addition, it can be important to differentiate sleepiness from fatigue, which is also common among shift workers. Practically, one straightforward way to discern sleepiness from fatigue is to ask patients how long it would take to fall asleep if the clinician left the room and turned out the light. In addition, questionnaires such as the Fatigue Severity Scale76, 77 can help quantify subjective fatigue. Furthermore, lifestyle factors such as alcohol use, cigarette smoking, and dietary practices should be assessed, as shift workers have demonstrated unhealthy lifestyle choices in each of these domains.24, 78, 79 Indeed, the evaluation of alcohol and substance use is of particular importance because alcohol is one of the most common self-medication strategies for managing sleep disturbance.80 Barger et al33 developed a standardized SWD questionnaire based on International Classification of Sleep Disorders, Second Edition, diagnostic criteria. Although this battery has been frequently used, several subscales will benefit from further psychometric refinement.81, 82
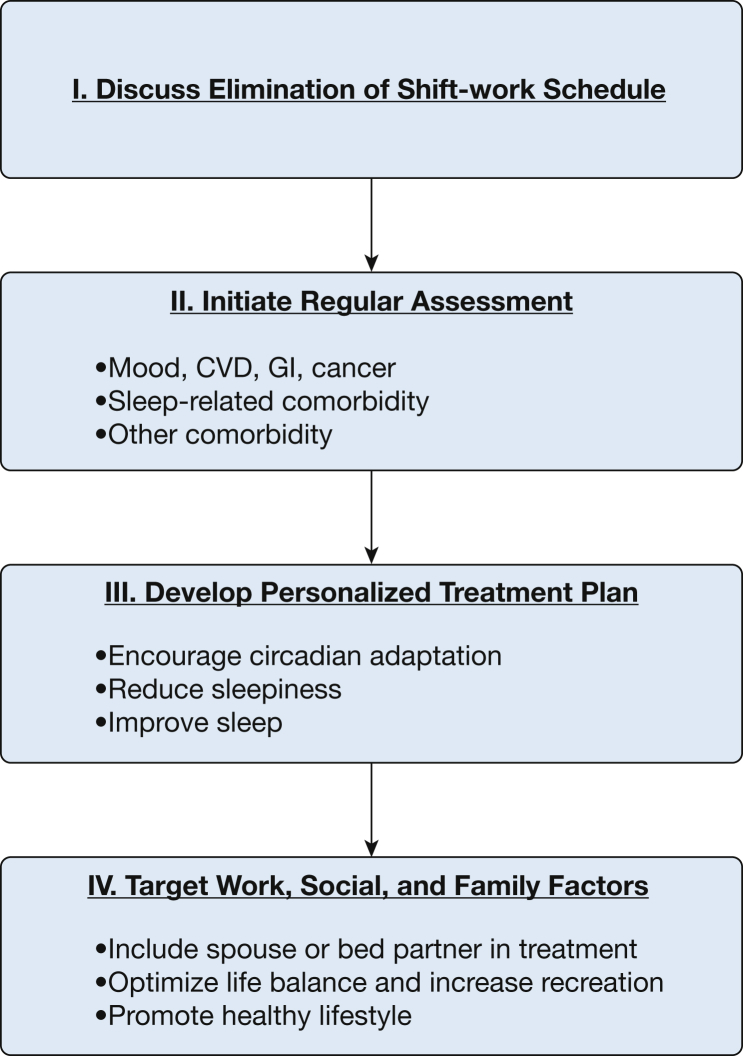
Treatment
Shift work is and will remain a vital component of the modern workplace. Thus, although there is no cure for SWD, a number of treatment efforts have targeted the core features of shift work: circadian misalignment, sleepiness, and sleep disturbances. Figure 3 presents step-by-step clinical guidelines that have emerged in the literature (reviewed in the following text), and Table 4 offers specific clinical recommendations for patients.83
Figure 3.
Clinical recommendations for the treatment of SWD. CVD = cardiovascular disease. See Figure 2 legend for expansion of other abbreviation.
(Approach based on Drake and Wright Jr.83)
Table 4.
Clinical Recommendations for Shift Work Disorder (Night Shift Example)
| Time | Recommendation |
|---|---|
| Before shift | 30- to 60-min planned nap |
| 300 mg of caffeine or consider stimulant or wake-promoting medication | |
| First half of shift | Bright or blue wavelength light |
| Second half of shift | Avoid psychostimulants |
| After shift | Avoid bright light, consider light goggles |
| Avoid driving while sleepy | |
| Home | Bedroom environment conducive to sleep: cool, dark, quiet, uncluttered |
| Consider melatonin | |
| Nonwork days | “Anchor” sleep: maintain partially delayed sleep schedule so that some sleep always overlaps |
| Family and social supports | Include bed partner and family members in treatment planning, especially to accommodate shift worker prescribed sleep schedule |
Circadian Adaptation
The core feature of SWD is misalignment between the endogenous and exogenous circadian schedules. Hence, a central objective of SWD treatments is to reduce this misalignment to enhance adaptation to the shift work schedule. The most powerful external time cue (ie, zeitgeber) of circadian rhythmicity is light, and multiple studies have examined bright light exposure as an approach to “shift” the endogenous clock. In laboratory studies, 15-min exposure to bright (2,000-10,000 lux) light 3 to 6 hours prior to the circadian nadir have demonstrated substantial shifts in circadian phase.84, 85 Unfortunately, translation of these laboratory findings to real-world settings remains a challenge as shift workers’ circadian phases can be anywhere across the 24-h day. Thus, it is difficult for clinicians to determine the appropriate timing for light exposure.29
It is also worth noting that complete circadian re-entrainment is only adaptive if shift workers maintain a consistent sleep-wake schedule 7 days per week. When shift workers revert to a diurnal schedule on nonwork days, circadian misalignment and associated difficulties resume. To compromise between these two extremes, a consistent partial phase delay has demonstrated clinical utility.86, 87 When workers follow this consistent schedule on both work and nonwork days, the nadir of circadian alertness occurs within a few hours after the shift ends. Evidence suggests that intermittent bright light exposure during the night (ie, 15-min increments of bright light exposure per hour for 5 consecutive hours) and light avoidance during the day (ie, wearing dark goggles) produce large phase delays (ie, 7.5 h), enhanced sleep, and improved psychomotor outcomes.87
In addition to bright light therapy, researchers have explored other zeitgebers as potentially modifiable regulators of circadian rhythmicity. For example, exogenous melatonin administration (0.5-3 mg) can enhance circadian adaptation among shift workers, and the American Academy of Sleep Medicine recommends 3 mg of melatonin before bed for shift workers.64 However, clinical effectiveness is directly related to control of exposure to other zeitgebers, especially light, and effects have not been assessed in SWD. Unplanned or poorly timed light exposure can easily override the potential therapeutic effects of exogenous melatonin. In terms of magnitude of effect, it is important to recognize limitations of melatonin. For example, 3 mg of melatonin and 1, 2, and 4 mg of the melatonin agonist ramelteon have been found to produce approximately 1.5-h phase shifts among young adults.88 When contrasted to the large phase-shifting effects of bright light therapy, these results suggest that melatonin might be better suited for other circadian rhythm disorders such as jet lag and delayed sleep phase syndrome, in which even modest phase shifts can be highly therapeutic. Furthermore, because even low doses (eg, 0.5 mg) of melatonin can produce performance impairments, cognitively intensive tasks such as operating machinery should be avoided for several hours following administration.89
Finally, although the phase-shifting properties of exercise are generally weak and unlikely to provide substantive chronobiotic benefit, the overall health benefits of exercise might help reduce morbidity associated with SWD.90 Exercise should thus be encouraged and, if possible, scheduled at the time of light exposure or desired phase shift.
Improving Sleep
Many but not all shift workers experience difficulties with sleep onset during daytime sleep. Conversely, sleep maintenance is consistently disrupted due to circadian misalignment,91 resulting in poor quality sleep and acute and chronic sleep loss. As a result, several strategies have been evaluated to increase sleep time and to improve daytime sleep quality in shift workers. A critical first step in any treatment approach is that patients should practice good sleep hygiene, including avoiding alcohol and caffeine close to bedtime. Because shift workers often sleep during the day, it is essential to ensure a bedroom environment that is conducive to sleep. The sleeping environment should be cool, dark, quiet, and uncluttered. Air conditioning, blackout shades or an eye mask, and ear plugs or white noise generator can all be cost-effective tools to create an optimal sleeping environment.24, 90 Clinicians are encouraged to enlist patient family and social support, which can be invaluable to help protect the worker’s sleep period.
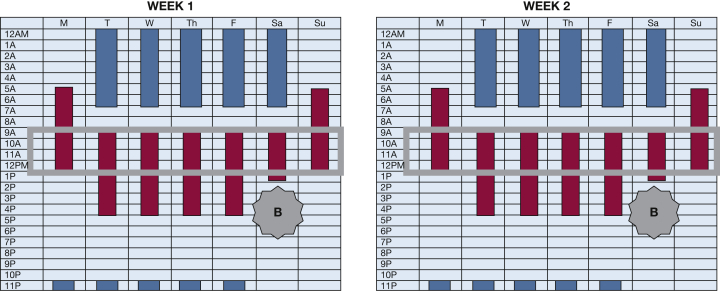
Another effective behavioral strategy is to “anchor” sleep by creating a sleep period that overlaps on both work and nonwork days (Fig 4). Sleep anchoring not only helps stabilize circadian rhythms and increases sleep duration but also makes it easier for shift workers to maintain social and recreational engagement on off days.91, 92 Including family members and social supports in the treatment plan are likely to enhance acceptability, increase adherence, and improve outcomes.
Figure 4.
Sample 2-week anchored work and sleep schedule for a night worker. Blue bars represent consistent work hours (11:00 pm-7:00 am), and red bars represent the scheduled sleep period. In this example, a night worker maintains a partially delayed sleep-wake schedule even on off days. This way, some period of sleep always overlaps, thus helping to “anchor” the circadian clock. “B” represents the so-called “light brake,” which can facilitate phase advance following the last night of a series of night shifts.82
(Based on Wickwire.15 Used with permission.)
In addition to improving sleep during the primary sleep period, planning strategic naps can help increase total sleep time, as well as increase alertness and improve performance in shift workers. Indeed, napping prior to and during shifts decreases reaction time, increases alertness, and reduces fatigue.93, 94, 95 However, it is important for clinicians to note that napping during shift had no impact on subsequent alertness during the commute home following the shift.95 All shift workers and particularly night shift workers should be consistently and strongly cautioned regarding the risks of drowsy driving. Furthermore, the effects of sleep inertia are worsened during the middle of the night relative to other periods of the circadian cycle.96 Thus, naps should be closely monitored,97 and shift workers should be advised to avoid driving or operating machinery until their post-nap sleep inertia has dissipated.
In addition to naps in isolation, empirical data and clinical experience suggest that naps can be effectively combined with other fatigue countermeasures, resulting in additive beneficial effect. For example, combining a pre-shift nap (30 min prior to shift) with caffeine (250-300 mg) can improve alertness and performance.98 Similarly, among professional drivers working shifts, two 20-min naps followed by 10 min of bright light (approximately 5,000 lux) exposure reduced the risk of sleep onset during a simulated driving task.94
There is a paucity of empirical data regarding the efficacy of circadian or insomnia treatments in patients with SWD. Although many clinical approaches to SWD can be considered broadly behavioral, it is difficult to generalize from insomnia studies to SWD due to the severe circadian dysregulation characteristic of shift work. In terms of sedative-hypnotic agents and insomnia pharmacotherapies, performance and safety concerns are paramount among patients with SWD. For example, benzodiazepines such as triazolam and temazepam improve sleep but have minimal impact on alertness.64, 73 Newer nonbenzodiazepine sedative-hypnotic agents such as zolpidem also improve sleep and can enhance nocturnal performance, but they can be associated with side effects such as anxiety and irritable mood.99 Exogenous melatonin (in doses ranging from 1-10 mg) has been found to improve daytime sleep in shift work simulation studies.89, 100, 101, 102
As mentioned earlier, the American Academy of Sleep Medicine recommends 3 mg of exogenous melatonin prior to the post-shift daytime sleep period.64 The melatonin-receptor agonists ramelteon and tasimelteon approved by the US Food and Drug Administration have also been shown to improve sleep in shift-work simulation studies. However, data from SWD samples are rare,89, 100, 101, 102 and clinicians must strive to control exposure to other zeitgebers, especially light. In addition, common side effects of ramelteon include dizziness, fatigue, and nausea, and melatonin and melatonin agonists might also increase prolactin levels.90
Reducing Sleepiness
Among shift workers and healthy volunteers, psychostimulants (including low-dose amphetamine and caffeine) have been shown to enhance alertness and improve psychomotor performance during prolonged periods of wakefulness.103, 104 However, such stimulants are associated with tolerance and withdrawal (ie, physiologic dependence),65 and amphetamines and methylphenidate present with high abuse potential.105 Although commercial energy drinks are common among shift workers and the general public, the psychostimulating effects of these beverages are not yet well understood. Among shift workers, two doses (250-mL can [includes 80 mg of caffeine, 1,000 mg of taurine, and 600 mg of glucuronolactone]) administered at 1:30 am and 5:30 am improved nocturnal alertness but decreased sleep duration and worsened sleep quality during the subsequent sleep episode.106
In addition to these options, modafinil and armodafinil are medications approved by the US Food and Drug Administration for improving nocturnal wakefulness in patients with SWD. Among patients with SWD who exhibited excessive nocturnal sleepiness (MSLT < 6 min), regular use of modafinil (200 mg) over 3 months resulted in improved alertness.65 Psychomotor vigilance was also increased, and self-reported motor vehicle crashes and near-misses were reduced. Although no adverse effects on subsequent daytime sleep were detected, clinicians are advised that careful timing of medication dosage is essential to minimize a potential negative impact on subsequent sleep. Furthermore, although nighttime sleepiness was reduced, participants remained pathologically sleepy (MSLT mean, 3.77 ± 0.5 min). More recent studies have examined armodafinil, the R-isomer of modafinil with the same half-life (approximately 15 h) but different elimination profile (higher plasma concentrations about 4-6 h following administration).107 Results have been similar to those of modafinil, with armodafinil (150 mg) reducing objective sleepiness during the night (MSLT = 2.3 ± 1.6 min to 5.3 ± 5.0 min) and improving neurocognitive performance, including both memory and attention. Similar to modafinil, armodafinil is generally well tolerated and has not been found to affect subsequent daytime sleep with appropriately timed administration. Common side effects of these medications include headache, nausea, dizziness, and anxiety, with headaches being the most common complaint.66, 67
Organizational Recommendations
From an organizational perspective, shift work must be conceptualized within the broader context of a multicomponent fatigue risk management program (FRMP). FRMPs are comprehensive approaches to fatigue-related risks that have been developed in response to regulatory and business demands. For example, Table 5 summarizes current hours of rest regulation and legislation, and readers are also referred to the excellent review put forth by the American College of Occupational and Environmental Physicians.108 A comprehensive FRMP should not only meet regulatory requirements in safety-sensitive industries but should also protect stakeholders from sleepiness-related harm. Even in nonsafety-sensitive industries, FRMPs can provide direct benefit by reducing costs associated with lost workplace productivity and increased risk for errors, accidents, and injuries. Although a detailed discussion of FRMPs is beyond the scope of the present review, several organizational recommendations regarding shift work can be made.
Table 5.
Federal HOS Regulations in the United States
| HOS Regulation | Rest Periods | Examples of Workers Covered by Regulations |
|---|---|---|
| 14 CFR §135.261-135.273 and 14 CFR CFR §121.465-121.525 | Required length of rest periods between flights are determined by the length of the flight, the number of pilots, time aloft, time on the flight deck, and sleeping facilities. HOS are specified for year, calendar quarter, month, and day. Regulations are complex | Aviation: Airplane pilots, passenger carrying Airplane pilots, Alaska nonscheduled flights Airplane pilots, overseas and international flights Airplane pilots, nonpassenger commercial and deadhead flights Medical evacuation helicopter pilots Airplane crew |
| 49 CFR pt. 395 | Required length of rest periods are determined by short vs long haul, whether passengers or loads are carried, hours on duty on consecutive days, time of use of sleeper berth, and working during “breaks.” Regulations are complex | Trucking: Long-haul truck drivers Long-haul drivers with passengers |
| 49 U.S.C. § 21103 and 49 C.F.R. pt. 228 | Required HOS depend on duty hours per month, waiting for deadhead transportation or transport back from duty assignment to final release, number of consecutive hours of work or number of consecutive rest hours, or number of days per week worked in past 7 days, and collective bargaining agreement stipulations. Regulations are complex | Railroad: Train employees Signal employees Dispatch employees |
| 46 U.S.C. § 8104 and 46 CFR §§ 15.705, 15.710, and 15.1111 | Required length of rest periods are determined based on type of watch, type of vessel and purpose of mission, and duration of rest over past 24 h and past 7 days. Overrides in place for safety of persons, ship, and cargo. Regulations are complex | Maritime: Ship captain Navigator Engineer Crew member |
| 10 C.F.R. §§ 26.205 and 26.211 | Required length of duty periods depend on rest in the past 24, 48, and 72 h, and 7 days, 9 days, and 60 days; whether the plant is active or on outage, emergency preparedness exercise, or drill. Regulations are complex | Nuclear power: Plant operators Engineers |
HOS = hours of service.
Prevention of SWD: Shared Responsibility
From an employer perspective, the overall objective of a shift work program within an FRMP is to encourage a culture of sleep health to support employee productivity and business outcomes, including reduced accident risk. Prevention and early recognition of problems associated with shift work are central to this mission. This approach requires ensuring fitness for duty, identifying employees at highest risk for SWD, and either insourcing occupational sleep health care or ensuring availability of external sleep health providers. In “just culture” companies, employers and employees share responsibility for ensuring fitness for duty. Thus, this partnership should begin as early as personnel selection and employee onboarding processes. For example, each job category, work schedule, and location within an employment setting should be graded for risk of fatigue-related errors and adverse outcomes, and these grades should be discussed with potential employees. Employers are responsible for ensuring adequate sleep opportunity between shifts, and employees are responsible for arriving to work rested. When workplace accidents, errors, and injuries do occur, labor and management (ie, employees and employers) should jointly examine events to determine whether sleepiness or fatigue was a contributing cause. Due to substantial interindividual variability in adaptability to shift work, a “one-rule fits all” approach is unlikely to maximize outcomes for either employees or employers. At minimum, standard operating procedures surrounding sleep and fatigue should be clearly defined and articulated to optimize organizational performance and reduce risk of fatigue-related harm.
Top-down Sleep Management
In addition to shared responsibilities in just culture organizations, certain efforts must be directed by employers, who develop and oversee standard operating procedures. Among the most important of these measures are staffing and scheduling policies, which operate in tandem and influence sleepiness and fatigue. In terms of schedule design, allowing employees to choose their own shifts does not increase operational costs yet increases perceived control and satisfaction among employees.109 Furthermore, self-scheduling is associated with additional health benefits and increased quality of life. When night shifts are unavoidable, permanent nights or clockwise or forward-rotating nights (ie, from day to evening to night) with a noncompressed pattern of shift rotation are then preferable.110 In addition to allowing for more time between shifts, rotations in this direction are consistent with the tendency of the circadian clock to delay sleep.111 It is thus surprising that empirical evidence regarding clockwise or counter-clock wise shift rotation has been mixed, with one study supporting clockwise rotation,112 but others demonstrating no impact on risks of SWD.113, 114 Fast rotations have been associated with improved outcomes such as better sleep quality and reduced fatigue.115, 116 Finally, when early start times cannot be avoided, employers should then schedule later start times (eg, 5:00 am, 5:00 am, 10:00 am) on successive days to allow for extended morning sleep, as every hour of delayed start times increases total sleep time by 0.7 h.117
In addition to shift scheduling, physical work environment is also an important and modifiable determinant of sleepiness on the job. Fortunately, physical environment is frequently highly supportive of fatigue countermeasures among shift workers. For example, ensuring a well-lighted workspace, maintaining an appropriate temperature, and reducing fatigue-inducing noise can help maximize performance among shift workers. Despite the availability of these environmental controls, there are bona fide challenges associated with implementing evidence-based interventions such as bright light therapy and napping in real-world settings.
Sleep Organizational Change Management
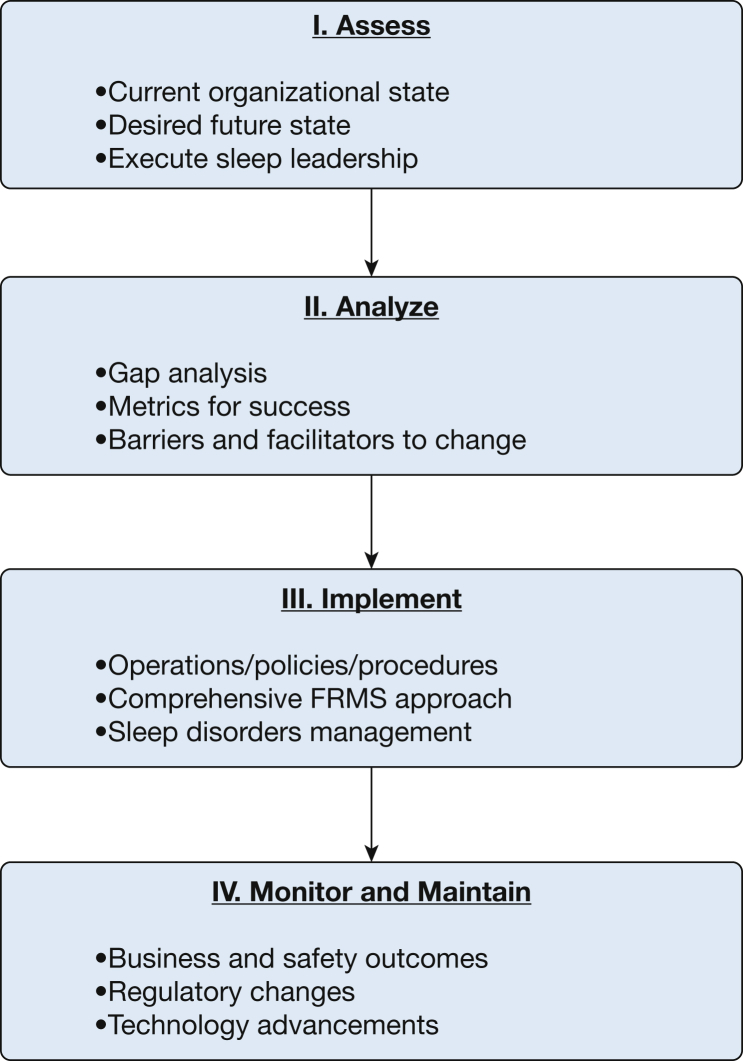
Successful organizational change efforts require clear delineation of project objectives and strategic alignment with overall business objectives. Project rationale must be articulated and disseminated in a way that ensures clarity regarding benefits to the organization and individual employees. Identifying and leveraging internal exemplars is essential,118 and clear rewards for adherence and punishment for nonadherence are required. Furthermore, preexisting culture is an important determinant of the success of such efforts and thus requires careful assessment during project planning. For example, napping is increasingly encouraged in “nap rooms” and frequently required in safety-sensitive industries (eg, long-distance pilots) but considered “sleeping on the job” in others. Figure 5 presents a process overview of organizational change initiatives.
Figure 5.
Process overview for organization change intervention. FRMP = fatigue risk management program.
From an occupational health perspective, sleep should be included prominently within workplace health promotion initiatives. Sleep disorders screening can be used to triage employees to an appropriate level of care based on risk (eg, general wellness education or clinical assessment). Relatedly, employers should provide health-related services at times when night shift workers will participate. It is essential to ensure the presence of health providers who can correctly diagnose SWD. Many employers in nonregulated industries are surprised to learn that employees diagnosed with SWD qualify for reasonable accommodations under the Americans With Disabilities Act.119 When other accommodations are impossible, it is best to assign these workers to evening shifts so that longer sleep durations can be achieved.19 Similarly, the number of consecutive shifts should be reduced, with a maximum of 3 to 4 consecutive days of shift work. Although not preferred by most employees, reducing work hours can also allow more time for sleep and thus reduce symptoms of SWD.
Conclusions and Future Directions
Twenty-four-hour operations are a practical necessity for the modern industrialized economy. To accommodate this societal need, approximately 20% of employees work some sort of nontraditional shift. There is substantial variability in tolerance for and adaptation to shiftwork, and roughly one of five shift workers develops SWD. This circadian rhythm sleep disorder is associated with significant adverse consequences to individuals, employers, and society. Treatments that focus on increasing circadian adaptation, reducing sleepiness, and improving sleep can improve quality of life in patients with SWD. Clinicians are strongly advised to incorporate family and social supports to maximize patient adherence. However, despite these promising clinical approaches, efforts to implement SWD prevention and treatment programs in real-world settings are in their infancy. Table 6 summarizes current and future research needs.
Table 6.
High Impact Future Directions in SWD
| Domain | Recommendation |
|---|---|
| Economic impact of SWD and treatment | Clarification is needed regarding impact of SWD on economic costs borne by employers, including lost workplace productivity, increased health-care utilization, and increased accident risk. Similarly, cost-benefit and cost-effectiveness analyses of FRMP and SWD programs are needed |
| Measurement and employer-specific end points | Enhanced measurement of sleep and sleepiness (fatigue) are essential among shift workers. Linking these sleep-wake measures to identified organization-specific end points (including missed work; accidents, injuries, and errors; motor vehicle crashes; work performance including coworker relationships, customer satisfaction, and organizational productivity) will be critical |
| Technology | Actigraphy and activity monitors can be used to assess sleep-wake patterns and circadian rhythmicity, and to determine their predictive value in terms of accident risk and schedule optimization. Development and evaluation of fail-safe override systems linked to physiologic measures of operator sleepiness are needed to prevent accidental harm |
| Telehealth and increased access to care | Mobile applications and online interventions have the potential to provide cost-effective prevention and treatment. Telehealth can be used to provide direct to patient care or connect occupational health professionals with sleep health specialists |
| Circadian measurement techniques | Further development of practical circadian assessment techniques using validated objective markers (eg, melatonin, core body temperature) is required for widespread implementation of circadian approaches to treatment |
| Implementation of FRMP and occupational sleep health programs | Investment in human resource capital is required, including staffing and scheduling to prevent fatigue, training in fatigue risks and fatigue risk management, and resourcing of occupational health providers to ensure access of staff to occupational health beyond ED visits. Incorporation of environmental modifications such as adapted lighting, temperature, and air quality improvements are required and should be rigorously evaluated |
FRMP = fatigue risk management program; SWD = shift work disorder.
Shift work is particularly amenable to occupational health approaches, and the integration of shift scheduling software, activity monitoring, mobile health, and telemedicine will likely be fruitful for forward-thinking organizations. Future studies will benefit from close collaboration with employers to identify occupational specific end points of interest, such as days missed and annual performance evaluations.
Acknowledgments
Financial/nonfinancial disclosures: The authors have reported to CHEST the following: E. M. W. has moderated noncommercial scientific discussions for Merck and is an equity shareholder in WellTap. E. M. W. and S. M. S.'s institution has received research support from Merck and ResMed. C. L. D. has received grants from TEVA, Merck, Jazz, Pernix, Robert Wood Johnson Foundation, and Aladdin Dreamer and has served on the speaker bureau for Merck. None declared (J. G.-B.).
Other contributions: The authors thank Donna Brighton, PhD, for her valuable input regarding organizational change.
References
- 1.Knutsson A. Methodological aspects of shift-work research. Chronobiol Int. 2004;21(6):1037–1047. doi: 10.1081/cbi-200038525. [DOI] [PubMed] [Google Scholar]
- 2.Caruso C.C. Negative impacts of shiftwork and long work hours. Rehabil Nurs. 2014;39(1):16–25. doi: 10.1002/rnj.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McMenamin T, Holden R, Bahls D. A time to work: recent trends in shift work and flexible schedules. Monthly Labor Review. 2007;130:3-14.
- 4.Boisard P, Cartron D, Gollac M, Valeyre A. Time and Work: Duration of Work. Luxembourg: Publications Office of the European Union; 2003.
- 5.Messenger JC, Lee S, McCann D. Working Time Around the World: Trends in Working Hours, Laws, and Policies in a Global Comparative Perspective. New York, NY: Routledge; 2007.
- 6.Bureau of Labor Statistics. Standard occupational classification groups. http://www.bls.gov/soc/major_groups.htm. Accessed July 10, 2016.
- 7.Tucker P, Folkard S. Working Time, Health and Safety: A Research Synthesis Paper. ILO; 2012.
- 8.International Classification of Sleep Disorders: Diagnostic and Coding Manual, 3rd Edition. Darien, IL: American Academy of Sleep Medicine; 2014.
- 9.Office of Technology Assessment, US Congress . University Press of the Pacific; Honolulu, HI: 2005. Biological Rhythms—Implications for the Worker: New Developments in Neuroscience. [Google Scholar]
- 10.Bureau of Labor Statistics. Shift usually worked: full-time wage and salary workers by selected characteristics. http://www.bls.gov/news.release/flex.t04.hm. Accessed July 10, 2016.
- 11.Borbély A.A., Daan S., Wirz-Justice A., Deboer T. The two-process model of sleep regulation: a reappraisal. J Sleep Res. 2016;25(2):131–143. doi: 10.1111/jsr.12371. [DOI] [PubMed] [Google Scholar]
- 12.Czeisler C.A., Duffy J.F., Shanahan T.L. Stability, precision, and near-24-hour period of the human circadian pacemaker. Science. 1999;284(5423):2177–2181. doi: 10.1126/science.284.5423.2177. [DOI] [PubMed] [Google Scholar]
- 13.Rosenwasser A.M. Neurobiology of the mammalian circadian system: oscillators, pacemakers, and pathways. Progress Psychobiol Physiol Psychol. 2003;18:1–38. [Google Scholar]
- 14.Edgar D.M., Dement W.C., Fuller C.A. Effect of SCN lesions on sleep in squirrel monkeys: evidence for opponent processes in sleep-wake regulation. J Neurosci. 1993;13(3):1065–1079. doi: 10.1523/JNEUROSCI.13-03-01065.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wickwire E.M. self-published; Baltimore, MD: 2016. Shift work survival guide. [Google Scholar]
- 16.Czeisler C.A., Buxton O.M. The human circadian timing system and sleep-wake regulation. In: Kryger M.H., Roth T., Dement W.C., editors. Principles and Practice of Sleep Medicine, Fifth Edition. WB Saunders; Philadelphia, PA: 2011. pp. 402–419. [Google Scholar]
- 17.Guardiola-Lemaitre B., Quera-Salva M. Melatonin and the regulation of sleep and circadian rhythms. In: Kryger M.H., Roth T., Dement W.C., editors. Principles and Practice of Sleep Medicine, Fifth Edition. WB Saunders; Philadelphia, PA: 2011. pp. 420–430. [Google Scholar]
- 18.Shanahan T.L., Kronauer R.E., Duffy J.F., Williams G.H., Czeisler C.A. Melatonin rhythm observed throughout a three-cycle bright-light stimulus designed to reset the human circadian pacemaker. J Biol Rhythms. 1999;14(3):237–253. doi: 10.1177/074873099129000560. [DOI] [PubMed] [Google Scholar]
- 19.Akerstedt T. Shift work and disturbed sleep/wakefulness. Occup Med (Lond) 2003;53(2):89–94. doi: 10.1093/occmed/kqg046. [DOI] [PubMed] [Google Scholar]
- 20.Ohayon M.M., Smolensky M.H., Roth T. Consequences of shiftworking on sleep duration, sleepiness, and sleep attacks. Chronobiol Int. 2010;27(3):575–589. doi: 10.3109/07420521003749956. [DOI] [PubMed] [Google Scholar]
- 21.Saksvik I.B., Bjorvatn B., Hetland H., Sandal G.M., Pallesen S. Individual differences in tolerance to shift work—a systematic review. Sleep Med Rev. 2011;15(4):221–235. doi: 10.1016/j.smrv.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 22.Akerstedt T., Wright K.P., Jr. Sleep loss and fatigue in shift work and shift work disorder. Sleep Med Clin. 2009;4(2):257–271. doi: 10.1016/j.jsmc.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Axelsson J., Åkerstedt T., Kecklund G., Lowden A. Tolerance to shift work—how does it relate to sleep and wakefulness? Int Arch Occup Environ Health. 2004;77(2):121–129. doi: 10.1007/s00420-003-0482-1. [DOI] [PubMed] [Google Scholar]
- 24.Drake C.L., Roehrs T., Richardson G., Walsh J.K., Roth T. Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers. Sleep. 2004;27(8):1453–1462. doi: 10.1093/sleep/27.8.1453. [DOI] [PubMed] [Google Scholar]
- 25.Taniyama Y., Yamauchi T., Takeuchi S., Kuroda Y. PER1 polymorphism associated with shift work disorder. Sleep Biol Rhythms. 2015;13(4):342–347. [Google Scholar]
- 26.Hilliker N.A., Muehlbach M.J., Schweitzer P.K., Walsh J.K. Sleepiness/alertness on a simulated night shift schedule and morningness-eveningness tendency. Sleep. 1992;15(5):430–433. doi: 10.1093/sleep/15.5.430. [DOI] [PubMed] [Google Scholar]
- 27.Viola A.U., Archer S.N., James L.M. PER3 polymorphism predicts sleep structure and waking performance. Curr Biol. 2007;17(7):613–618. doi: 10.1016/j.cub.2007.01.073. [DOI] [PubMed] [Google Scholar]
- 28.Sack R., Auckley D., Auger R. Circadian rhythm sleep disorders: part I, basic principles, shift work and jet lag disorders. An American Academy of Sleep Medicine review. Sleep. 2007;30(11):1460–1483. doi: 10.1093/sleep/30.11.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gumenyuk V., Howard R., Roth T., Korzyukov O., Drake C.L. Sleep loss, circadian mismatch, and abnormalities in reorienting of attention in night workers with shift work disorder. Sleep. 2014;37(3):545–556. doi: 10.5665/sleep.3494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gumenyuk V., Belcher R., Drake C.L., Roth T. Differential sleep, sleepiness, and neurophysiology in the insomnia phenotypes of shift work disorder. Sleep. 2015;38(1):119–126. doi: 10.5665/sleep.4336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, fifth edition. Arlington, VA: American Psychiatric Association; 2013.
- 32.Waage S., Moen B., Pallesen S. Shift work disorder among oil rig workers in the North Sea. Sleep. 2009;32(4):558–565. doi: 10.1093/sleep/32.4.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barger L.K., Ogeil R.P., Drake C.L., O'Brien C.S., Ng K.T., Rajaratnam S.M. Validation of a questionnaire to screen for shift work disorder. Sleep. 2012;35(12):1693–1703. doi: 10.5665/sleep.2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rosa R.R., Harma M., Pulli K., Mulder M., Nasman O. Rescheduling a three shift system at a steel rolling mill: effects of a one hour delay of shift starting times on sleep and alertness in younger and older workers. Occup Environ Med. 1996;53(10):677–685. doi: 10.1136/oem.53.10.677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harma M.I., Hakola T., Akerstedt T., Laitinen J.T. Age and adjustment to night work. Occup Environ Med. 1994;51(8):568–573. doi: 10.1136/oem.51.8.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith L., Mason C. Reducing night shift exposure: a pilot study of rota, night shift and age effects on sleepiness and fatigue. J Hum Ergol. 2001;30(1/2):83–87. [PubMed] [Google Scholar]
- 37.Duffy J.F., Zeitzer J.M., Czeisler C.A. Decreased sensitivity to phase-delaying effects of moderate intensity light in older subjects. Neurobiol Aging. 2007;28(5):799–807. doi: 10.1016/j.neurobiolaging.2006.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nakamura T.J., Takasu N.N., Nakamura W. The suprachiasmatic nucleus: age-related decline in biological rhythms. J Physiol Sci. 2016;66(5):367–374. doi: 10.1007/s12576-016-0439-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carrier J., Monk T.H., Buysse D.J., Kupfer D.J. Sleep and morningness-eveningness in the ‘middle’years of life (20–59y) J Sleep Res. 1997;6(4):230–237. doi: 10.1111/j.1365-2869.1997.00230.x. [DOI] [PubMed] [Google Scholar]
- 40.Ogińska H., Pokorski J., Ogińiski A. Gender, ageing, and shiftwork intolerance. Ergonomics. 1993;36(1-3):161–168. doi: 10.1080/00140139308967868. [DOI] [PubMed] [Google Scholar]
- 41.Shields M. Shift work and health. Health Reports. 2002;13(4):11. [PubMed] [Google Scholar]
- 42.Frost P., Kolstad H.A., Bonde J.P. Shift work and the risk of ischemic heart disease—a systematic review of the epidemiologic evidence. Scand J Work Environ Health. 2009;35(3):163–179. doi: 10.5271/sjweh.1319. [DOI] [PubMed] [Google Scholar]
- 43.Brown D.L., Feskanich D., Sanchez B.N., Rexrode K.M., Schernhammer E.S., Lisabeth L.D. Rotating night shift work and the risk of ischemic stroke. Am J Epidemiol. 2009;169(11):1370–1377. doi: 10.1093/aje/kwp056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Monk T.H., Buysse D.J. Exposure to shift work as a risk factor for diabetes. J Biol Rhythms. 2013;28(5):356–359. doi: 10.1177/0748730413506557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Karlsson B., Knutsson A., Lindahl B. Is there an association between shift work and having a metabolic syndrome? Results from a population based study of 27,485 people. Occup Environ Med. 2001;58(11):747–752. doi: 10.1136/oem.58.11.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Knutsson A., Bøggild H. Gastrointestinal disorders among shift workers. Scand J Work Environ Health. 2010;36(2):85–95. doi: 10.5271/sjweh.2897. [DOI] [PubMed] [Google Scholar]
- 47.Mahoney M.M. Shift work, jet lag, and female reproduction. Int J Endocrinol. 2010;2010:813764. doi: 10.1155/2010/813764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hansen J., Lassen C.F. Nested case-control study of night shift work and breast cancer risk among women in the Danish military. Occup Environ Med. 2012;69(8):551–556. doi: 10.1136/oemed-2011-100240. [DOI] [PubMed] [Google Scholar]
- 49.Jia Y., Lu Y., Wu K. Does night work increase the risk of breast cancer? A systematic review and meta-analysis of epidemiological studies. Cancer Epidemiol. 2013;37(3):197–206. doi: 10.1016/j.canep.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 50.Kubo T., Ozasa K., Mikami K. Prospective cohort study of the risk of prostate cancer among rotating-shift workers: findings from the Japan Collaborative Cohort Study. Am J Epidemiol. 2006;164(6):549–555. doi: 10.1093/aje/kwj232. [DOI] [PubMed] [Google Scholar]
- 51.Puca F.M., Perrucci S., Prudenzano M.P. Quality of life in shift work syndrome. Funct Neurol. 1996;11(5):261–268. [PubMed] [Google Scholar]
- 52.Morikawa Y., Sakurai M., Nakamura K. Correlation between shift-work-related sleep problems and heavy drinking in Japanese male factory workers. Alcohol Alcohol. 2013;48(2):202–206. doi: 10.1093/alcalc/ags128. [DOI] [PubMed] [Google Scholar]
- 53.Gumenyuk V., Roth T., Korzyukov O. Shift work sleep disorder is associated with an attenuated brain response of sensory memory and an increased brain response to novelty: an ERP study. Sleep. 2010;33(5):703–713. doi: 10.1093/sleep/33.5.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dawson D., Reid K. Fatigue, alcohol and performance impairment. Nature. 1997;388(6639) doi: 10.1038/40775. 235-235. [DOI] [PubMed] [Google Scholar]
- 55.Scheer F.A., Shea T.J., Hilton M.F., Shea S.A. An endogenous circadian rhythm in sleep inertia results in greatest cognitive impairment upon awakening during the biological night. J Biol Rhythms. 2008;23(4):353–361. doi: 10.1177/0748730408318081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Barger L.K., Cade B.E., Ayas N.T. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352(2):125–134. doi: 10.1056/NEJMoa041401. [DOI] [PubMed] [Google Scholar]
- 57.Ftouni S., Sletten T.L., Howard M. Objective and subjective measures of sleepiness, and their associations with on-road driving events in shift workers. J Sleep Res. 2013;22(1):58–69. doi: 10.1111/j.1365-2869.2012.01038.x. [DOI] [PubMed] [Google Scholar]
- 58.Smith L., Folkard S., Poole C. Increased injuries on night shift. Lancet. 1994;344(8930):1137–1139. doi: 10.1016/s0140-6736(94)90636-x. [DOI] [PubMed] [Google Scholar]
- 59.Rajaratnam S., Howard M.E., Grunstein R.R. Sleep loss and circadian disruption in shift work: health burden and management. Med J Aust. 2013;199(8):S11–S15. doi: 10.5694/mja13.10561. [DOI] [PubMed] [Google Scholar]
- 60.Czeisler C.A., Wickwire E.M., Barger L.K. Sleep-deprived motor vehicle operators are unfit to drive: a multidisciplinary expert consensus statement on drowsy driving. Sleep Health. 2016;2(2):94–99. doi: 10.1016/j.sleh.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 61.Gamaldo C.E., Salas R.E. Sleep medicine education: are medical schools and residency programs napping on the job? Nat Clin Pract Neurol. 2008;4(6):344–345. doi: 10.1038/ncpneuro0808. [DOI] [PubMed] [Google Scholar]
- 62.Geiger-Brown J., Rogers V.E., Trinkoff A.M., Kane R.L., Bausell R.B., Scharf S.M. Sleep, sleepiness, fatigue, and performance of 12-hour-shift nurses. Chronobiol Int. 2012;29(2):211–219. doi: 10.3109/07420528.2011.645752. [DOI] [PubMed] [Google Scholar]
- 63.Ancoli-Israel S., Martin J.L., Blackwell T. The SBSM guide to actigraphy monitoring: clinical and research applications. Behavioral Sleep Med. 2015;13(suppl 1):S4–S38. doi: 10.1080/15402002.2015.1046356. [DOI] [PubMed] [Google Scholar]
- 64.Morgenthaler T.I., Lee-Chiong T., Alessi C. Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report. Sleep. 2007;30(11):1445–1459. doi: 10.1093/sleep/30.11.1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Roehrs T., Roth T. Medication and Substance Abuse. In: Kryger M.H., Roth T., Dement W.C., editors. Principles and Practice of Sleep Medicine, Fifth Edition. WB Saunders; Philadelphia, PA: 2011. pp. 1512–1523. [Google Scholar]
- 66.Czeisler C.A., Walsh J.K., Roth T. Modafinil for excessive sleepiness associated with shift-work sleep disorder. N Engl J Med. 2005;353(5):476–486. doi: 10.1056/NEJMoa041292. [DOI] [PubMed] [Google Scholar]
- 67.Czeisler C.A., Walsh J.K., Wesnes K.A., Arora S., Roth T. Armodafinil for treatment of excessive sleepiness associated with shift work disorder: a randomized controlled study. Mayo Clin Proc. 2009;84(11):958–972. doi: 10.1016/S0025-6196(11)60666-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gumenyuk V., Roth T., Drake C.L. Circadian phase, sleepiness, and light exposure assessment in night workers with and without shift work disorder. Chronobiol Int. 2012;29(7):928–936. doi: 10.3109/07420528.2012.699356. [DOI] [PubMed] [Google Scholar]
- 69.Johns M.W. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14(6):540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 70.Punjabi N.M., Bandeen-Roche K., Young T. Predictors of objective sleep tendency in the general population. Sleep. 2003;26(6):678–683. doi: 10.1093/sleep/26.6.678. [DOI] [PubMed] [Google Scholar]
- 71.Walsleben J.A., Kapur V.K., Newman A.B. Sleep and reported daytime sleepiness in normal subjects: the Sleep Heart Health Study. Sleep. 2004;27(2):293–298. doi: 10.1093/sleep/27.2.293. [DOI] [PubMed] [Google Scholar]
- 72.Kaida K., Takahashi M., Akerstedt T. Validation of the Karolinska Sleepiness Scale against performance and EEG variables. Clin Neurophysiol. 2006;117(7):1574–1581. doi: 10.1016/j.clinph.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 73.Lowden A., Kecklund G., Axelsson J., Åkerstedt T. Change from an 8-hour shift to a 12-hour shift, attitudes, sleep, sleepiness and performance. Scand J Work Environ Health. 1998;24(suppl 3):69–75. [PubMed] [Google Scholar]
- 74.Bastien C.H., Vallières A., Morin C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 75.Buysse D.J., Reynolds C.F., Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 76.Krupp L.B., LaRocca N.G., Muir-Nash J., Steinberg A.D. The fatigue severity scale: application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46(10):1121–1123. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- 77.Valko P.O., Bassetti C.L., Bloch K.E., Held U., Baumann C.R. Validation of the fatigue severity scale in a Swiss cohort. Sleep. 2008;31(11):1601–1607. doi: 10.1093/sleep/31.11.1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Culpepper L. The social and economic burden of shift-work disorder. J Fam Pract. 2010;59(1) S3-S3. [PubMed] [Google Scholar]
- 79.Trinkoff A.M., Storr C.L. Work schedule characteristics and substance use in nurses. Am J Ind Med. 1998;34(3):266–271. doi: 10.1002/(sici)1097-0274(199809)34:3<266::aid-ajim9>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 80.Ancoli-Israel S., Roth T. Characteristics of insomnia in the United States: results of the 1991 National Sleep Foundation Survey. I. Sleep. 1999;22(suppl 2):S347–S353. [PubMed] [Google Scholar]
- 81.Tucker P., Knowles S.R. Review of studies that have used the Standard Shiftwork Index: evidence for the underlying model of shiftwork and health. Appl Ergon. 2008;39(5):550–564. doi: 10.1016/j.apergo.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 82.Smith C., Gibby R., Zickar M. Measurement properties of the Shiftwork Survey and Standard Shiftwork Index. J Hum Ergol (Tokyo) 2001;30(1-2):191–196. [PubMed] [Google Scholar]
- 83.Drake C.L., Wright K.P., Jr. Shift work, shift-work disorder, and jet lag. In: Kryger M.H., Roth T., Dement W.C., editors. Principles and Practice of Sleep Medicine, Fifth Edition. 2011. pp. 784–798. [Google Scholar]
- 84.Boivin D.B., James F.O. Light treatment and circadian adaptation to shift work. Ind Health. 2005;43(1):34–48. doi: 10.2486/indhealth.43.34. [DOI] [PubMed] [Google Scholar]
- 85.Czeisler C.A., Allan J.S., Strogatz S.H. Bright light resets the human circadian pacemaker independent of the timing of the sleep-wake cycle. Science. 1986;233(4764):667–671. doi: 10.1126/science.3726555. [DOI] [PubMed] [Google Scholar]
- 86.Crowley S.J., Lee C., Tseng C.Y., Fogg L.F., Eastman C.I. Complete or partial circadian re-entrainment improves performance, alertness, and mood during night-shift work. Sleep. 2004;27(6):1077–1087. doi: 10.1093/sleep/27.6.1077. [DOI] [PubMed] [Google Scholar]
- 87.Smith M.R., Eastman C.I. Night shift performance is improved by a compromise circadian phase position: study 3. Circadian phase after 7 night shifts with an intervening weekend off. Sleep. 2008;31(12):1639–1645. doi: 10.1093/sleep/31.12.1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Richardson G.S., Zee P.C., Wang-Weigand S., Rodriguez L., Peng X. Circadian phase-shifting effects of repeated ramelteon administration in healthy adults. J Clin Sleep Med. 2008;4(5):456–461. [PMC free article] [PubMed] [Google Scholar]
- 89.Rajaratnam S.M., Polymeropoulos M.H., Fisher D.M. Melatonin agonist tasimelteon (VEC-162) for transient insomnia after sleep-time shift: two randomised controlled multicentre trials. Lancet. 2009;373(9662):482–491. doi: 10.1016/S0140-6736(08)61812-7. [DOI] [PubMed] [Google Scholar]
- 90.Wright K.P., Jr., Bogan R.K., Wyatt J.K. Shift work and the assessment and management of shift work disorder (SWD) Sleep Med Rev. 2013;17(1):41–54. doi: 10.1016/j.smrv.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 91.Dawson D., Campbell S.S. Timed exposure to bright light improves sleep and alertness during simulated night shifts. Sleep. 1991;14(6):511–516. doi: 10.1093/sleep/14.6.511. [DOI] [PubMed] [Google Scholar]
- 92.Minors D.S., Waterhouse J.M. Does ‘anchor sleep' entrain circadian rhythms? Evidence from constant routine studies. J Physiol. 1983;345:451–467. doi: 10.1113/jphysiol.1983.sp014988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Garbarino S., Mascialino B., Penco M.A. Professional shift-work drivers who adopt prophylactic naps can reduce the risk of car accidents during night work. Sleep. 2004;27(7):1295–1302. doi: 10.1093/sleep/27.7.1295. [DOI] [PubMed] [Google Scholar]
- 94.Leger D., Philip P., Jarriault P., Metlaine A., Choudat D. Effects of a combination of napping and bright light pulses on shift workers' sleepiness at the wheel: a pilot study. J Sleep Res. 2009;18(4):472–479. doi: 10.1111/j.1365-2869.2008.00676.x. [DOI] [PubMed] [Google Scholar]
- 95.Smith-Coggins R., Howard S.K., Mac D.T. Improving alertness and performance in emergency department physicians and nurses: the use of planned naps. Ann Emerg Med. 2006;48(5):596–604. doi: 10.1016/j.annemergmed.2006.02.005. 604.e1-3. [DOI] [PubMed] [Google Scholar]
- 96.Wertz A.T., Ronda J.M., Czeisler C.A., Wright K.P., Jr. Effects of sleep inertia on cognition. JAMA. 2006;295(2):163–164. doi: 10.1001/jama.295.2.163. [DOI] [PubMed] [Google Scholar]
- 97.Ruggiero J.S., Redeker N.S. Effects of napping on sleepiness and sleep-related performance deficits in night-shift workers: a systematic review. Biol Res Nurs. 2014;16(2):134–142. doi: 10.1177/1099800413476571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Schweitzer P.K., Randazzo A.C., Stone K., Erman M., Walsh J.K. Laboratory and field studies of naps and caffeine as practical countermeasures for sleep-wake problems associated with night work. Sleep. 2006;29(1):39–50. doi: 10.1093/sleep/29.1.39. [DOI] [PubMed] [Google Scholar]
- 99.Hart C.L., Ward A.S., Haney M., Foltin R.W. Zolpidem-related effects on performance and mood during simulated night-shift work. Exp Clin Psychopharmacol. 2003;11(4):259–268. doi: 10.1037/1064-1297.11.4.259. [DOI] [PubMed] [Google Scholar]
- 100.Hughes R.J., Badia P. Sleep-promoting and hypothermic effects of daytime melatonin administration in humans. Sleep. 1997;20(2):124–131. [PubMed] [Google Scholar]
- 101.Markwald R.R., Lee-Chiong T.L., Burke T.M., Snider J.A., Wright K.P., Jr. Effects of the melatonin MT-1/MT-2 agonist ramelteon on daytime body temperature and sleep. Sleep. 2010;33(6):825–831. doi: 10.1093/sleep/33.6.825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wyatt J.K., Dijk D.J., Ritz-de Cecco A., Ronda J.M., Czeisler C.A. Sleep-facilitating effect of exogenous melatonin in healthy young men and women is circadian-phase dependent. Sleep. 2006;29(5):609–618. doi: 10.1093/sleep/29.5.609. [DOI] [PubMed] [Google Scholar]
- 103.Hart C.L., Ward A.S., Haney M., Nasser J., Foltin R.W. Methamphetamine attenuates disruptions in performance and mood during simulated night-shift work. Psychopharmacology (Berl) 2003;169(1):42–51. doi: 10.1007/s00213-003-1464-4. [DOI] [PubMed] [Google Scholar]
- 104.Wyatt J.K., Cajochen C., Ritz-De Cecco A., Czeisler C.A., Dijk D. Low-dose repeated caffeine administration for circadian-phase-dependent performance degradation during extended wakefulness. Sleep. 2004;27(3):374–381. doi: 10.1093/sleep/27.3.374. [DOI] [PubMed] [Google Scholar]
- 105.Wood S., Sage J.R., Shuman T., Anagnostaras S.G. Psychostimulants and cognition: a continuum of behavioral and cognitive activation. Pharmacol Rev. 2014;66(1):193–221. doi: 10.1124/pr.112.007054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Jay S.M., Petrilli R.M., Ferguson S.A., Dawson D., Lamond N. The suitability of a caffeinated energy drink for night-shift workers. Physiol Behav. 2006;87(5):925–931. doi: 10.1016/j.physbeh.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 107.Darwish M., Kirby M., Hellriegel E.T., Robertson P. Armodafinil and modafinil have substantially different pharmacokinetic profiles despite having the same terminal half-lives: analysis of data from three randomized, single-dose, pharmacokinetic studies. Clin Drug Invest. 2009;29(9):613–623. doi: 10.2165/11315280-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 108.Lerman S.E., Eskin E., Flower D.J. Fatigue risk management in the workplace. J Occup Environ Med. 2012;54(2):231–258. doi: 10.1097/JOM.0b013e318247a3b0. [DOI] [PubMed] [Google Scholar]
- 109.Bambra C.L., Whitehead M.M., Sowden A.J., Akers J., Petticrew M.P. Shifting schedules: the health effects of reorganizing shift work. Am J Prev Med. 2008;34(5):427–434. doi: 10.1016/j.amepre.2007.12.023. [DOI] [PubMed] [Google Scholar]
- 110.Kecklund G., Eriksen C.A., Åkerstedt T. Police officers attitude to different shift systems: association with age, present shift schedule, health and sleep/wake complaints. Appl Ergon. 2008;39(5):565–571. doi: 10.1016/j.apergo.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 111.Czeisler C.A., Moore-Ede M.C., Coleman R.H. Rotating shift work schedules that disrupt sleep are improved by applying circadian principles. Science. 1982;217(4558):460–463. doi: 10.1126/science.7089576. [DOI] [PubMed] [Google Scholar]
- 112.Orth-Gomer K. Intervention on coronary risk factors by adapting a shift work schedule to biologic rhythmicity. Psychosom Med. 1983;45(5):407–415. doi: 10.1097/00006842-198310000-00004. [DOI] [PubMed] [Google Scholar]
- 113.Cruz C., Detwiler C., Nesthus T., Boquet A. Clockwise and counterclockwise rotating shifts: effects on sleep duration, timing, and quality. Aviat Space Environ Med. 2003;74(6):597–605. [PubMed] [Google Scholar]
- 114.Cruz C., Boquet A., Detwiler C., Nesthus T. Clockwise and counterclockwise rotating shifts: effects on vigilance and performance. Aviat Space Environ Med. 2003;74(6):606–614. [PubMed] [Google Scholar]
- 115.Hornberger S., Knauth P. Effects of various types of change in shift schedules: a controlled longitudinal study. Work Stress. 1995;9(2-3):124–133. [Google Scholar]
- 116.Hornberger S., Knauth P. Follow-up intervention study on effects of a change in shift schedule on shiftworkers in the chemical industry. Int J Industrial Ergonomics. 1998;21(3-4):249–257. [Google Scholar]
- 117.Ingre M., Kecklund G., Åkerstedt T., Söderström M., Kecklund L. Sleep length as a function of morning shift—start time in irregular shift schedules for train drivers: self-rated health and individual differences. Chronobiol Int. 2008;25(2-3):349–358. doi: 10.1080/07420520802110704. [DOI] [PubMed] [Google Scholar]
- 118.Gunia B.C., Sipos M.L., LoPresti M., Adler A.B. Sleep leadership in high-risk occupations: an investigation of soldiers on peacekeeping and combat missions. Mil Psychol. 2015;27(4):197–211. [Google Scholar]
- 119.EEOC Regulations To Implement the Equal Employment Provisions of the Americans With Disabilities Act, as Amended, 29 C.F.R. § 1630 (2011).