Abstract
We report a case of invasive dermatophytosis mimicking vasculitis. A patient consulted the Department of Dermatology, Zealand University Hospital, Roskilde, Denmark for the assessment of violaceous/erythematous lesions thought to be vasculitis. She had prior to this been treated with the immunosuppressive drug teriflunomid. Due to the lesion's erythematous scaling boarder invasive dermatophytosis was suspected. By using direct microscopy a mycological diagnosis was confirmed. We underline the utility of direct microscopy in the diagnosis.
Keywords: Vasculitis, Invasive dermatophytosis, Fungal infection, Trichophyton rubrum, Ulcer
1. Introduction
The clinical presentation of vasculitis can range from cutaneous vasculitis to life threating internal organ involvement [1]. Several conditions can mimic the presentation of vasculitis and the range of differential diagnosis is therefore broad [1]. One differential diagnosis is invasive dermatophytosis, which is associated with immunodeficiency. A tool that can be used in making the diagnosis is direct microscopy. We report a case of invasive dermatophytosis mimicking vasculitis in an immunocompromised patient and underline the practical utility of direct microscopy in the diagnosis.
2. Case
A 55-year old woman known with multiple sclerosis and onychomycosis consulted the Department of Dermatology, Zealand University Hospital, Roskilde, Denmark, for the assessment of lesions thought to represent vasculitis (day 0). She had a one year history of scaly, itching sores on the lower right leg. The lesions were exacerbated during treatment with clobetasolpropionate under zinkoxide bandage. The patient had been treated with the immunosuppressive drug teriflunomid for multiple sclerosis for two years.
A physical examination revealed scaly violaceous/erythematous skin with sharply demarcated lesions primarily on the right foot and anterior aspect on the lower right leg (Fig. 1). Deep <1 cm diameter ulcers were also observed.
Fig. 1.

Violaceous, haemorrhagic and scaly erythematous skin with deep sores. Right foot.
Due to the ulcers the patient was referred for vasculitis, but because of erythematous scaling border of the lesions, dermatophytosis was suspected as a differential diagnosis. Direct microscopy was performed using blanchophor and fluorescence microscopy and showed numerous hyphae (day 0) (Fig. 2). A skin scraping was performed for further mycological examination. The patient was started on a combination of oral terbinafine 250 mg daily combined with topically terbinafine (day 0) for the treatment of tinea incognito due to the usage of teriflunomid and clobetasolpropionate.
Fig. 2.
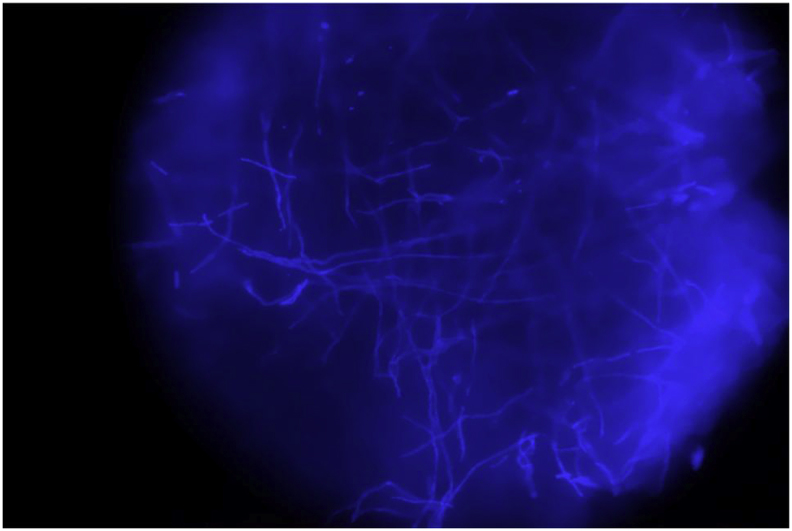
Direct microscopy revealing numerous hyphae.
Laboratory investigations including PCR confirmed a mycological diagnosis and revealed a growth of Trichophyton (T.) rubrum (day +2). PCR diagnostics were performed by Statens Serum Institut (SSI) using an in house PCR [6] Treatment assessment (day + 30) revealed improvement and no growth of T. rubrum.
3. Discussion
Dermatophytes are fungal pathogens that infect the keratinized layers of the skin, hair and nails [3]. T. rubrum is one of the most prevalent species [4]. Invasive dermatophytosis is a rare condition in which dermatophytes invade the deep dermis or internal organs [2,5]. It can present in two clinical forms: Majocchi's granuloma and deep dermatophytosis. A biopsy for histopathology is often required to differentiate between Majocchis granuloma/deep dermatophytosis.
One clue to the diagnosis of invasive dermatophytosis is the presence of associated typical superficial dermatophytosis lesions. Our patient had clinical signs of tinea pedis and onychomycosis. Furthermore, invasive dermatophytosis is typically unilateral whereas vasculitis is often bilateral.
In a review by Boral et al. [5] of 33 published cases of Majocchis granuloma 6/33 (17%) of the cases received immunosuppressive therapy, 6/33 (17%) systemically prednisolone and 18/33 (55%) topical corticosteroid treatment, respectively.
To the best of our knowledge, this is the first report of invasive dermatophytosis mimicking vasculitis. In our case direct microscopy was used to confirm a mycological diagnosis, thus confirming that it is still a highly useful bedside tool that should be used as a first step to help guide the use of other often more time-consuming diagnostic procedures.
Funding statement
None.
Declaration of competing interest
The authors have the following conflicts of interests to declare: GB Jemec has received honoraria from AbbVie, Coloplast, Pfizer, Pierre Fabre, Inflarx, MSD, Novartis and UCB for participation on advisory boards, and grants from Abbvie, Leo Pharma, Novartis, Janssen-Cilag, Regeneron, UCB, and Sanofi for participation as an investigator, and received speaker honoraria from AbbVie, Galderma, and Leo Pharma. DMLS was paid as a consultant for advisory board meeting by AbbVie, Janssen, Sanofi and received speaker's honoraria and/or received grants from the following companies: Bayer, Abbvie, Desitin, Pfizer, Galderma, Astellas, Novartis and Leo Pharma during the last 5 years.
Acknowledgments
We wish to thank Unit of Mycology, Department of Bacteria, Parasites and Fungi, Statens Serum Institut, Copenhagen, Denmark for performing the PCR analysis.
References
- 1.Suresh E. Diagnostic approach to patients with suspected vasculitis. Postgrad. Med. J. 2006;82:483–488. doi: 10.1136/pgmj.2005.042648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Warycha M.A., Leger M., Tzu J., Kamino H., Stein J. Deep dermatophytosis caused by Trichophyton rubrum. Dermatol. Online J. 2011;17:21. [PubMed] [Google Scholar]
- 3.Hay R.J., Baran R. Deep dermatophytosis: rare infections or common, but unrecognised, complications of lymphatic spread? Curr. Opin. Infect. Dis. 2004;17:77–79. doi: 10.1097/00001432-200404000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Matsuzaki Y., Ota K., Sato K., Nara S., Yagushi T., Nakano H., Sawamura D. Deep pseudocystic dermatophytosis caused by Trichophyton rubrum in a patient with myasthenia gravis. Acta Derm. Venereol. 2013 May;93(3):358–359. doi: 10.2340/00015555-1452. [DOI] [PubMed] [Google Scholar]
- 5.Boral H., Durdu M., Ilkit M. Majocchi's granuloma: current perspectives. 1. Infect. Drug Resist. 2018 May 22;11:751–760. doi: 10.2147/IDR.S145027. eCollection 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brillowska-Dabrowska A., Nielsen S.S., Nielsen H.V., Arendrup M.C. Optimized 5-hour multiplex PCR test for the detection of tinea unguium: performance in a routine, PCR laboratory. Med. Mycol. 2010 Sep;48(6):828–831. doi: 10.3109/13693780903531579. PubMed PMID: 20105101. [DOI] [PubMed] [Google Scholar]


