Abstract
Background: Madelung deformity is a congenital wrist condition characterized by volar subluxation of the wrist caused by premature growth arrest of the distal radius. Progressive symptoms can necessitate surgical intervention, yet optimal treatment strategy remains unknown. The aim of this study is to determine treatment options, surgical indications, and operative outcomes for Madelung deformity. Methods: This study adhered to the Meta-Analyses of Observational Studies in Epidemiology (MOOSE) guidelines. A comprehensive systematic review was performed to identify all studies describing surgical interventions for Madelung deformity. All studies were evaluated by level of evidence and a self-developed quality assessment tool. Results: Twenty-five studies met inclusion criteria; all case series with type IV level of evidence. Studies assessed pain, range of motion, aesthetic deformity, and grip strength. The primary indication for surgery was the presence of wrist pain. Various surgical procedures exist and could be categorized as radial lengthening, ulnar shortening, or a combination of both. All studies report postoperative pain reduction and most studies report an improved range of motion. Conclusions: A variety of surgical procedures reportedly have satisfactory outcomes. However, outcomes are reported in an inconsistent manner, prohibiting pooling of studies and comparisons of surgical procedures and their outcomes. We propose several methodological changes for implementation in future studies, increasing the quality of evidence to compensate for small patient numbers.
Keywords: Madelung deformity, osteotomy, congenital hand, wrist, hand surgery
Introduction
In 1878, Otto W. Madelung reported on a rare disease of the wrist, now known as Madelung deformity.36 Although the first case was presented years before, Madelung was the first to provide an overview even before the discovery of radiographs.6 In his clinical observations, he describes a palmar subluxation of the hand, a prominent distal ulna, and volar angulation of the distal radial epiphysis.36 Currently, we know that the deformity is caused by an abnormal growth arrest of the distal radial epiphysis leading to volar and ulnar tilting of the radial articular surface, and palmar bowing of the distal radius.5,38 Studies have also identified an abnormally thickened volar ligament, the so-called “Vickers ligament,” that tethers the lunate to the radius and is hypothesized to hinder growth by compressing the epiphyseal plate.50 Because of its progressive nature, the deformity can lead to wrist pain, restricted range of motion (ROM), and loss of grip strength, heavily interfering with daily activities.18,21,30 In addition, patients can complain about the visible deformity caused by prominence of the distal ulna.30 Madelung deformity often occurs bilaterally,46 is most often diagnosed in adolescent females,40 and has been associated with genetic disorders such as Léri-Weill dyschondrosteosis (LWD) and Turner syndrome.7,11
Representing less than 2% of pediatric hand deformities,22 our current understanding of this condition is limited. Despite the small number of affected patients, studies have tried to shed light on various clinical aspects of the deformity, prompting the rise of multiple classification systems28,40 and various radiographic criteria to be used in the diagnostic process.14,38 However, the consistency with which these classification systems are applied remains unclear. This is also reflected in patient care, as multiple surgical procedures have been proposed to correct the deformity, without a current consensus.19,23,32 Therefore, nearly 200 years after its original description, a significant knowledge gap remains, with respect to the surgical management of Madelung deformity,19 compromising patients’ access to optimal care.
The purpose of this systematic review is to evaluate the current body of literature on Madelung deformity, to identify available surgical treatment options, criteria utilized for surgical decision making, as well as clinical outcomes. The following questions will be addressed:
Which criteria are assessed in the preoperative workup?
What surgical procedures are available to correct the deformity?
What is the primary indication for surgical treatment?
What are the outcomes in regard to pain and ROM?
Materials and Methods
Search Strategy
The study protocol adhered to the Meta-Analyses of Observational Studies in Epidemiology (MOOSE) guidelines (Supplemental File 1).49 A comprehensive electronic search strategy was developed and reviewed by a senior Harvard Medical School research librarian. On September 12, 2017, an online search was performed using Medline, Embase, and the Cochrane Collaboration Library to identify all original citations that addressed surgical approaches for Madelung deformity. The search was conducted using both Medical Subject Heading (MeSH) and free-text using the following search terms: “Madelung Deformity,” “Leri-Weill Syndrome,” and “Dyschondrosteosis.” In addition, a manual reference check of all articles meeting inclusion criteria was performed to capture additional references not yielded in the initial search. The search was limited to articles published in English, Chinese, Dutch, French, and German from inception to September 2017. Articles published in languages other than English were translated by native speakers in the research team whenever applicable.
Eligibility Criteria
Studies eligible for inclusion described a corrective operative procedure for Madelung deformity and included postoperative outcomes. Studies ineligible for inclusion were case reports, case series including fewer than 3 patients, studies detailing a surgical technique only, and studies including patients with prior corrective procedures of the same wrist. In addition, literature reviews and studies that did not report patient follow-up and outcomes were excluded. If a study described a patient cohort that was used in a previous study, the study with shorter follow-up time was excluded to capture the most current long-term outcomes. Abstracts and unpublished studies were not eligible for inclusion.
Study Selection
After completion of an initial electronic database search, all citations were identified and imported into EndNote X7.7.1 (Thomas Reuters, New York, NY). After removal of duplicates, all studies were subject to title and abstract screening by 2 independent reviewers (A.P., A.R.J). Subsequently, these 2 reviewers obtained and screened full-text articles using the eligibility criteria outlined above to obtain the final list of articles. Disagreement was resolved by consensus from a third evaluator (S.D.S.). When full-text articles were not available, efforts were made to obtain these through correspondence with study authors.
Data Collection
The final list of articles was independently evaluated by 2 authors (A.P., A.R.J) and the following variables were extracted: type of study, number of patients, number of operated wrists, gender, age at surgery, etiology, criteria used in clinical examination, radiographic criteria used in the diagnostic process, surgical procedure, indication for surgical intervention, intraoperative identification of Vickers ligament, and patient follow-up time. Whenever available, data for the following clinical outcome variables were extracted: pain, ROM, grip strength, and presence of aesthetic deformity. For patients who underwent bilateral wrist surgery, age at the time of the first operation was selected for the “age at surgery” variable, as this would best represent the age at which patients undergo surgical intervention. The majority of surgical procedures were categorized as: (1) radial lengthening (eg, wedge osteotomy, Ilizarov technique); (2) ulnar shortening (eg, resection, excision, osteotomy); or (3) a combination of (1) and (2).
Study Quality and Bias Assessment
Each study was evaluated by the level of evidence as proposed by the Centre for Evidence-Based Medicine (Oxford, UK). This classification scheme assigns a level of evidence ranging from I (highest) to V (lowest).
We were unable to find a published and validated scale to assess case series for use in subsequent statistical analyses. Therefore, a novel quality assessment tool was developed in accordance with MOOSE guidelines to accurately reflect important factors in the surgical decision making process (Supplemental Table 1). The scoring system used the following parameters: (1) sample size; (2) disease etiology; (3) preoperative clinical exam; (4) radiographic criteria; (5) postoperative outcomes; (6) follow-up time; and (7) patient-reported outcome measures. One point was awarded if the sample size was greater than 10 patients, follow-up time was greater than 1 year, and etiology was defined for all patients. For pre- and postoperative assessment, a range of 0 to 2 points were awarded based on reporting of 2 parameters: pain and ROM. No points were awarded if any of these parameters was not described. One point was awarded if pain and ROM were described subjectively and 2 points were awarded if both parameters were quantified. Radiographic criteria were assessed using a 0- to 2-point scale: no points if criteria were missing, 1 point for self-defined criteria, and 2 points for standardized criteria (eg, Dannenberg or McCarroll). Finally, if authors assessed patient-reported outcome measures using a validated tool, 1 point was awarded.
Two authors (A.P., A.R.J) independently scored each study (Supplemental Table 2). The intraclass correlation coefficient (ICC) was determined using a reliability analysis (IBM SPSS Statistics 25) indicating excellent interrater agreement (ICC = 0.802). Due to the wide variety of surgical procedures and the nature of included studies (exclusively case series), it was not possible to perform bias assessments, heterogeneity assessments, or meta-analyses.
Results
Search Results
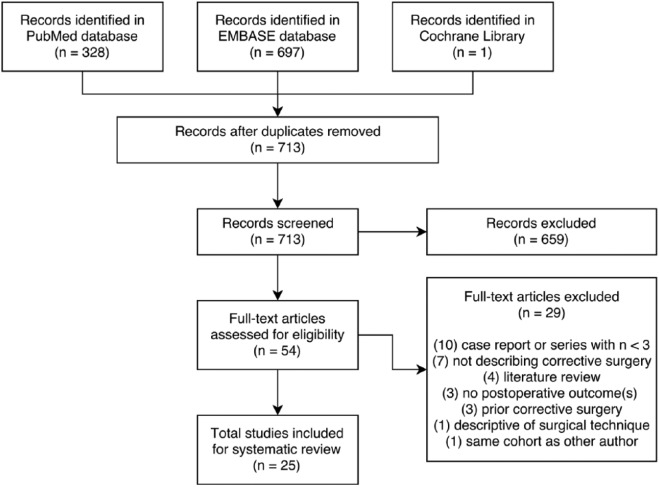
A total of 1026 citations were identified for potential inclusion after initial electronic database search, with 713 citations remaining after removal of duplicates (Figure 1). Of these, 54 were available for full-text review after title and abstract screening. Twenty-five studies met eligibility criteria and were included in the study. The 29 studies that did not meet eligibility criteria were excluded for reasons including case report or case series with fewer than 3 patients (n = 10), studies not describing corrective surgery (n = 7), literature review (n = 4), lack of postoperative outcomes (n = 3), prior corrective surgery performed on the same wrist (n = 3), and descriptive study of surgical technique (n = 1). In addition, 1 study was excluded26 as the same patient cohort was used by another author that provided longer follow-up time.48
Figure 1.
Flow diagram.
Study Characteristics
The 25 included studies are listed in Table 1. All studies were case series with type IV level of evidence. Our self-developed quality assessment tool provided a median quality score of 5 (range, 2-8). The mean sample size was 9 (range, 3-19). Mean follow-up time was 6.3 years and was available for 20 studies.
Table 1.
Study Characteristics.
| Study | N (wrists) | Age, y (range) | Etiology | Radiographic criteria | Follow-up, mo (range) | Qualitya |
|---|---|---|---|---|---|---|
| Burrows9 | 3 (3) | 14 (10-17) | Idiopathic (2) Posttraumatic (1) |
Other | 16 (8-34) | 4/10 |
| Ranawat et al42 | 8 (13) | 17 (12-26) | Idiopathic (8) | Other | 96 (12-192) | 5/10 |
| Nielsen40 | 13 (15) | 22 (14-57) | LWD (5) | NS | 102 (6-240) | 4/10 |
| Vickers and Nielsen50 | 17 (24) | N/A | LWD (17) | Other | NS (15-180) | 5/10 |
| Watson et al51 | 10 (15) | 17 (NS) | LWD (9) Posttraumatic (1) |
NS | 48 (3-132) | 4/10 |
| Angelini et al4 | 15 (25) | 18 (16-23) | Idiopathic (15) | Dannenberg | 67 (24-120) | 7/10 |
| Murphy et al39 | 11 (12) | 16 (9-31) | LWD (7) Posttraumatic (2) |
Dannenberg | 48 (13-97) | 7/10 |
| de Billy et al15 | 3 (5) | 13 (13-13) | Idiopathic (3) | Other | NS | 4/10 |
| Dos Reis et al18 | 18 (25) | 23 (16-35) | Idiopathic (18) | Other | 53 (22-76) | 6/10 |
| Salon et al45 | 7 (11) | 15 (11-19) | LWD (2) | Other | 116 (18-264) | 5/10 |
| Schmidt-Rohlfing et al46 | 5 (6) | 21 (NS) | NS | Dannenberg | NS | 5/10 |
| Ahmed Mir et al2 | 7 (7) | 13 (12-15) | Idiopathic (7) | Other | NS | 4/10 |
| Bruno et al9 | 9 (9) | 34 (29-45) | LWD (2) | Other | 42 (6-112) | 8/10 |
| Houshian et al30 | 7 (8) | 19 (9-44) | LWD (4) Posttraumatic (3) |
Other | 30 (18-66) | 7/10 |
| Dagregorio and Saint-Cast13 | 3 (5) | 22 (15-33) | NS | NS | NS | 2/10 |
| Aharoni et al1 | 3 (4) | 29 (27-32) | NS | Other | 24 (NS) | 6/10 |
| de Paula et al16 | 4 (6) | 16 (12-22) | NS | Other | 24 (3-53) | 4/10 |
| Glard et al24 | 3 (4) | 29 (27-32) | NS | Other | 24 (NS) | 6/10 |
| Potenza et al41 | 5 (8) | 13 (11-13) | Idiopathic (5) | Other | 408 (NS) | 5/10 |
| Laffosse et al33 | 11 (14) | 13 (9-16) | LWD (2) | McCarroll | 61 (48-105) | 7/10 |
| Kampa et al31 | 4 (5) | 34 (26-45) | LWD (3) | McCarroll | 55 (14-113) | 7/10 |
| El-Gafary and El-adly20 | 7 (7) | 10 (5-17) | NS | Other | 24 (NS) | 4/10 |
| Mallard et al37 | 5 (10) | 27 (NS) | NS | McCarroll | 95 (7-227) | 6/10 |
| Steinman et al48 | 18 (26) | 13 (9-17) | LWD (4) Posttraumatic (4) |
McCarroll | 132 (84-168) | 8/10 |
| Saffar and Badina44 | 19 (21) | 27 (8-51) | NS | McCarroll | 51 (7-228) | 8/10 |
Note. LWD = Léri-Weill dyschondrosteosis; NS = not specified.
Score calculated using self-designed quality assessment tool.
Patient Characteristics
We identified 215 patients with 288 operated wrists. The majority of patients (90%) were female with a mean age at surgery of 18.5 years (range, 5-57 years). Disease etiology was reported for 166 patients (77%). Most patients were classified as idiopathic Madelung deformity (100 patients; 60%), 55 patients (33%) had a diagnosis of LWD, and 11 patients (7%) had a posttraumatic deformity.
Preoperative Evaluation
In the clinical examination process, all studies assessed pain, ROM, and presence of aesthetic deformity. In addition, 8 studies assessed grip strength.1,4,8,13,18,20,44,48 As part of the diagnostic process, 14 studies used their own radiographic criteria, 5 studies used the McCarroll criteria,38 and 3 studies used the Dannenberg criteria.14 The remaining 3 studies did not specify criteria used.
Surgical Procedures and Outcomes
The primary surgical procedures and outcomes for each study are provided in Table 2. The most commonly performed procedure was a combination of radial lengthening and ulnar shortening. Other procedures in order of decreasing frequency included radial lengthening, ulnar shortening, the Sauvé-Kapandji procedure, and the Langenskiöld procedure. Seventeen studies described the primary indication for surgical intervention, with the occurrence of pain being the decisive factor in 14 studies. Three studies intraoperatively identified and resected Vickers ligament.39,48,50
Table 2.
Surgical Procedures and Outcomes.
| Study | Surgical procedures | Primary indication | Pain reduced | ROM improved | Complications |
|---|---|---|---|---|---|
| Burrows9 | RL/US | Deformity | NS | 50% | NS |
| Ranawat et al42 | RL/US, USa | Pain | 100% | 100% | 1 revision surgery |
| Nielsen40 | RL/US, US | Pain | 69% | 8% | 3 revision surgeries |
| Vickers and Nielsen50 | LP | Pain | 100% | 100% | 1 iatrogenic injury |
| Watson et al51 | RL, RL/US | Pain | 100% | NS | 8 revision surgeries |
| Angelini et al4 | SK | Pain | 87% | 87% | 1 CRPS |
| Murphy et al39 | RL | NS | 100% | 100% | 2 revision surgeries 1 hardware removal |
| de Billy et al15 | RLb | Pain | 100% | 100% | 1 transient neurological injury |
| Dos Reis et al18 | RL/US | Deformity | 80% | 100% | 1 wound infection 1 CRPS requiring revision surgery |
| Salon et al45 | RL/US | Pain | 100% | 100% | 1 revision surgery |
| Schmidt-Rohlfing et al46 | RL, US | Pain | 100% | 20% | None |
| Ahmed Mir et al2 | RLb | Pain | 100% | 100% | None |
| Bruno et al8 | US | Pain | 100% | 100% | 1 revision surgery |
| Houshian et al30 | RLb | Pain | 100% | 100% | 2 infection 2 revision surgery |
| Dagregorio and Saint-Cast13 | RL | Pain | 100% | 100% | None |
| Aharoni et al1 | US | NS | 100% | NS | NS |
| de Paula et al16 | RL | NS | 100% | 100% | None |
| Glard et al24 | US | NS | 100% | 100% | NS |
| Potenza et al41 | RL/US | NS | 100% | 100% | None |
| Laffosse et al33 | RL/US | Pain | 82% | 100% | 2 neurological deficits (transient) |
| Kampa et al31 | RL/USa | Pain | 100% | 100% | 1 hardware removal |
| El-Gafary and El-adly20 | RLb | Deformity | 100% | 100% | NS |
| Mallard et al37 | RL | NS | 100% | 100% | 7 hardware removal 1 persistent neurological deficit |
| Steinman et al48 | RL | NS | 83% | 83% | 6 revision surgeries |
| Saffar and Badina44 | RL, RL/US | NS | 75% | 100% | 16 hardware removal 1 revision surgery 1 CRPS |
Note. ROM = range of motion; RL = radial lengthening; US = ulnar shortening; NS = not specified; LP = Langenskiöld procedure; SK = Sauvé-Kapandji procedure; CRPS = complex regional pain syndrome.
Ulnar shortening through Darrach procedure.
Radial lengthening through Ilizarov technique.
All studies reported postoperative pain reduction in the majority of patients and 20 studies reported an improved ROM. Patient-reported outcomes were assessed in 4 studies,8,31,37,48 of which 3 used the Disabilities of the Arm, Shoulder and Hand score. One study used a visual analog scale (VAS) to assess pre- and postoperative pain.30
The majority of studies reported complications. Revision procedures were reported in 10 studies (40%), with varying indications, including complex regional pain syndrome, recurrence of deformity, and need for additional reconstructive procedures.
Discussion
In this review, we evaluated the available literature describing surgical interventions in patients with Madelung deformity, with respect to disease etiology, clinical examination parameters, radiographic criteria, choice and type of intervention, and surgical outcomes. Pain, ROM, aesthetic deformity, and occasionally grip strength were assessed in clinical examination, with pain being the most common indication for surgery. A variety of surgical procedures exist to treat Madelung deformity, with reportedly satisfactory outcomes in terms of pain and ROM. However, the heterogeneity of surgical techniques described, diversity of radiographic criteria used, and inconsistencies in reporting the etiology of the deformity and outcomes did not allow for quantitative comparisons. These factors, combined with the lack of patient-reported outcome measures, compromised our ability to make recommendations regarding optimal treatment.
Strengths and Limitations
A major strength of our study is that it is the first systematic review assessing surgical management of Madelung deformity. Our study is largely limited by the nature of included studies: All 25 studies were low-powered case series of low-quality evidence (IV). Also, the possibility of publication bias could weaken the overwhelmingly positive reported outcomes in terms of pain and ROM.
Etiology
Madelung deformity is often classified into 4 groups based on etiology: (1) posttraumatic; (2) bone dysplasia; (3) chromosome abnormalities; and (4) idiopathic occurrence.28 Existing literature supports the association between Madelung deformity and skeletal dysplasias or genetic syndromes,7,11 with mutations or deletions in the short stature homeobox (SHOX) gene identified as key factors.43 Some studies even suggest that most Madelung deformity patients have an underlying genetic condition.29,52 In contrast, the majority of patients in our review were classified as idiopathic, yet none of the included studies mentioned genetic testing as part of their clinical management. This could imply that patients described as idiopathic” in origin were potentially misclassified due to lack of genetic workup. Furthermore, mutations of the SHOX gene have also been associated with idiopathic presentations of the deformity.25 These factors support that the absence of genetic testing could skew our understanding of the true etiology of Madelung deformity.
In addition, there was no clear rationale for selection of the surgical approach based on etiology. Different etiologies can present with unique anatomic deformities which can influence treatment choice. Prior research has shown that LWD patients were more likely to have a deformity involving the entire radius.52 This is clinically relevant, as this could result in more severe functional and aesthetic manifestations, in turn requiring more complex surgical interventions.
Radiographic Criteria and Imaging
There were multiple radiographic criteria used across studies. Radiographic criteria based on common findings in Madelung deformity have been described to aid in the diagnostic workup.14,38,50 However, most studies in our review used their own radiographic criteria. This heterogeneity underscores existing inconsistencies in the radiographic assessment of Madelung deformity. This could be explained by the limitations inherent to 2-dimensional assessment and its inability to capture the 3-dimensional (3D) nature of Madelung deformity. We anticipate that the application of 3D imaging will revolutionize our understanding of Madelung deformity by providing a roadmap for the development of new morphological parameters for more objective diagnosis and classification. This new spatial assessment could also facilitate the use of innovative techniques such as 3D preoperative planning for osteotomies,17 with the goal to more accurately restore normal anatomic and functional relationships.
Surgical Intervention
A variety of procedures exist to treat Madelung deformity. In our review, it appeared that surgeons almost exclusively chose any of the following approaches for surgical correction: lengthening of the radius, shortening of the ulna, or a combination of both. Vickers and Nielsen were the first to use the Langenskiöld procedure in 17 patients (24 wrists) with Madelung deformity.50 The procedure consists of resecting the affected part of the radial physis and interposing fat to prevent recurrence of a bony bridge,34 enabling radius growth in a more normal fashion. The Sauvé-Kapandji procedure was used primarily in 1 study.4
The main indication for surgical intervention in this review was pain. This is interesting, provided the significance placed on radiographic parameters and degree of deformity as important considerations for operative intervention. Instead, these parameters could be considered as essential components of successful surgical planning.
In this review, most studies reported objective outcome measures such as pain and ROM. However, we were unable to make comparisons across studies because of the diversity of surgical interventions and poor specification of ROM and pain for individual participants. This eliminated the ability to link surgical procedures to postoperative outcomes, in turn compromising our ability to evaluate efficacy of surgical techniques.
Complications occurred in the majority of studies, and the need for a revision procedure was the most common postoperative complication. A prior review of 15 studies23 did not provide information regarding the general incidence of postoperative complications. In our review, there was no identifiable surgical intervention associated with a higher complication rate. This finding may be misleading, as studies often did not specify complications according to the surgical procedure.
Studies have confirmed the presence of Vickers ligament in multiple Madelung deformity patients undergoing magnetic resonance imaging.12,47 One study even suggested that all congenital cases of Madelung deformity are characterized by the presence of this ligament.3 This abnormal ligament has been thought to contribute to developmental arrest of the distal radius through compression, and early identification and removal may have significant prophylactic potential.50 However, underlying etiology and identification of this ligament were not consistently reported. With only 3 of our included studies describing Vickers ligament, this precluded any discussion about its influence on the anatomical changes seen in Madelung deformity.
Recommendations for Future Research and Practice
We were unable to conduct a meta-analysis due to the low quality of studies as reflected by the scores from our self-developed assessment tool. Therefore, we propose several changes in the methodology of future studies which we deem necessary considering the rarity of Madelung deformity. During clinical evaluation, a thorough history and physical exam is imperative and includes family history of disorder, existing medical conditions, and prior trauma. An interdisciplinary approach, including coordination with a genetic counselor, should be considered as part of the routine workup. Genetic testing could be particularly helpful in patients with an obscure etiology or lack of preceding wrist trauma to identify potential chromosomal aberrancies.
The pre- and postoperative physical examination should include uniform, quantified measurements of all clinically relevant variables. Pain is quantified using a VAS, a validated instrument commonly used for measuring pain intensity. ROM measurements of the affected and contralateral wrist should include flexion, extension, pronation, supination, radial, and ulnar deviation. Patient satisfaction with the aesthetic appearance could be quantified using patient-reported outcome measures such as the Michigan Hand Outcomes Questionnaire10 or the Patient-Rated Wrist Evaluation questionnaire.35 A routine grip strength measurement should be considered, as it may indicate postoperative improvement.4 In addition, a standardized imaging protocol needs to be developed and uniformly adapted, possibly using a 3D assessment of the deformity. Surgeons should aim to identify and report on the presence of Vickers ligament intraoperatively, as prevalence and existing etiologic association are still unknown and require investigation.
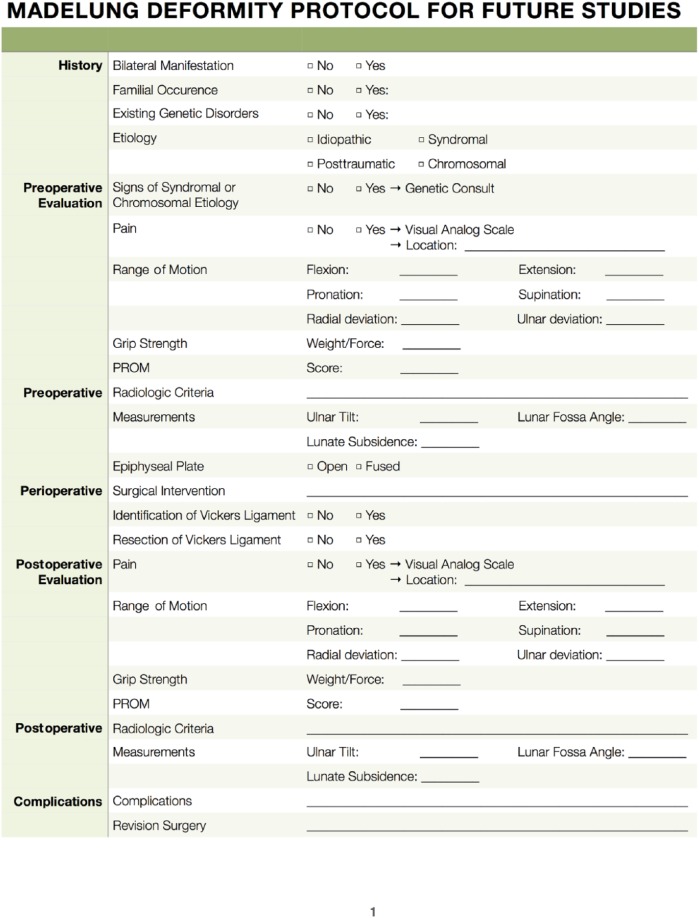
Multiple algorithms have been proposed for the surgical management of Madelung deformity, selecting appropriate treatment based on a variety of factors such as patient age, pain location, skeletal maturity, and the presence of secondary arthritis.19,27 Yet these algorithms are based on low-quality evidence. Future studies should implement data collection protocols to increase study homogeneity and evidence quality. A suggested template can be found in Figure 2.
Figure 2.
Madelung deformity protocol for use in future studies.
Note. PROM = Patient Reported Outcome Measures.
Conclusion
Despite nearly 200 years of experience with Madelung deformity, there remains a paucity of evidence-based algorithms regarding the surgical decision-making process. Outcomes are reported in an inconsistent manner, prohibiting pooling of studies and comparisons of surgical procedures and their outcomes. We propose multiple changes to serve as the basis for new clinical guidelines that will increase the quality of evidence in future studies, compensating for small sample sizes.
Supplemental Material
Supplemental material, DS_10.1177_1558944718793179 for Surgical Management of Madelung Deformity: A Systematic Review by Abbas Peymani, Anna Rose Johnson, Arriyan S. Dowlatshahi, Johannes G. G. Dobbe, Samuel J. Lin, Joseph Upton, Geert J. Streekstra and Simon D. Strackee in HAND
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: This article did not require the use of informed consent.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: A.P. received a PhD scholarship (2017) from the Academic Medical Center (Amsterdam, The Netherlands) supporting this research.
ORCID iD: A Peymani  https://orcid.org/0000-0002-3312-0469
https://orcid.org/0000-0002-3312-0469
References
- 1. Aharoni C, Glard Y, Launay F, et al. Maladie de Madelung: ostéotomie isolée de l’ulna. Chir Main. 2006;25(6):309-314. doi: 10.1016/j.main.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 2. Ahmed Mir N, Ahmed Kawoosa A, Mir GR. Ilizarov’s technique for treatment of Madelung’s deformity by lengthening and re-axation of the distal extremity of the radius. JK Sci. 2003;5(3):118-121. doi: 10.1055/s-2008-1071176. [DOI] [Google Scholar]
- 3. Ali S, Kaplan S, Kaufman T, et al. Madelung deformity and Madelung-type deformities: a review of the clinical and radiological characteristics. Pediatr Radiol. 2015;45(12):1856-1863. doi: 10.1007/s00247-015-3390-0. [DOI] [PubMed] [Google Scholar]
- 4. Angelini LC, Leite VM, Faloppa F. Surgical treatment of Madelung disease by the Sauvé-Kapandji technique. Ann Chir Main Memb Super. 1996;15(4):257-264. doi: 10.1016/S0753-9053(96)80035-4. [DOI] [PubMed] [Google Scholar]
- 5. Anton JI, Reitz GB, Spiegel MB. Madelung’s deformity. Ann Surg. 1938;108(3):411-439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Arora AS, Chung KC, Otto W. Madelung and the recognition of Madelung’s deformity. J Hand Surg Am. 2006;31(2):177-182. doi: 10.1016/j.jhsa.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 7. Belin V, Cusin V, Viot G, et al. SHOX mutations in dyschondrosteosis (Leri-Weill syndrome). Nat Genet. 1998;19(1):67-69. doi: 10.1038/ng0198-67. [DOI] [PubMed] [Google Scholar]
- 8. Bruno RJ, Blank JE, Ruby LK, et al. Treatment of Madelung’s deformity in adults by ulna reduction osteotomy. J Hand Surg Am. 2003;28(3):421-426. doi: 10.1053/jhsu.2003.50073. [DOI] [PubMed] [Google Scholar]
- 9. Burrows HJ. An operation for the correction of Madelung’s deformity and similar conditions. Proc R Soc Med. 1937;30(5):565-572. doi: 10.1177/003591573703000518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chung KC, Hamill JB, Walters MR, et al. The Michigan Hand Outcomes Questionnaire (MHQ): assessment of responsiveness to clinical change. Ann Plast Surg. 1999;42(6):619-622. doi: 10.1097/00000637-199906000-00006. [DOI] [PubMed] [Google Scholar]
- 11. Clement-Jones M, Schiller S, Rao E, et al. The short stature homeobox gene SHOX is involved in skeletal abnormalities in Turner syndrome. Hum Mol Genet. 2000;9(5):695-702. doi: 10.1093/hmg/9.5.695. [DOI] [PubMed] [Google Scholar]
- 12. Cook PA, Yu JS, Wiand W, et al. Madelung deformity in skeletally immature patients: morphologic assessment using radiography, CT, and MRI. J Comput Assist Tomogr. 1996;20(4):505-511. doi: 10.1097/00004728-199607000-00001. [DOI] [PubMed] [Google Scholar]
- 13. Dagregorio G, Saint-Cast Y. [Reorientation of the distal radial articular surface in Madelung’s deformity by a reversed cuneiform osteotomy]. Chir Main. 2005;24(2):109-112. doi: 10.1016/j.main.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 14. Dannenberg M, Anton JI, Spiegel MB. Madelung’s deformity: consideration of its roentgenological diagnostic criteria. Am J Roentgenol. 1939;42:671-676. [Google Scholar]
- 15. de Billy B, Gastaud F, Repetto M, et al. Treatment of Madelung’s deformity by lengthening and relaxation of the distal extremity of the radius by Ilizarov’s Technique. Eur J Pediatr Surg. 1997;7(5):296-298. doi: 10.1055/s-2008-1071176. [DOI] [PubMed] [Google Scholar]
- 16. de Paula EJL, Cho AB, Junior RM, et al. Madelung’s deformity: treatment with radial osteotomy and insertion of a trapezoidal wedge. J Hand Surg Am. 2006;31(7):1206-1213. doi: 10.1016/j.jhsa.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 17. Dobbe JGG, Strackee SD, Streekstra GJ. Minimizing the translation error in the application of an oblique single-cut rotation osteotomy: where to cut? IEEE Trans Biomed Eng. 2018;65(4):821-827. [DOI] [PubMed] [Google Scholar]
- 18. dos Reis FB, Katchburian MV, Faloppa F, et al. Osteotomy of the radius and ulna for the Madelung deformity. J Bone Joint Surg Br. 1998;80(5):817-824. doi: 10.1302/0301-620X.80B5.8691. [DOI] [PubMed] [Google Scholar]
- 19. Dubey A, Fajardo M, Green S, et al. Madelung’s deformity: a review. J Hand Surg Eur Vol. 2010;35(3):174-181. doi: 10.1177/1753193409346070. [DOI] [PubMed] [Google Scholar]
- 20. El-Gafary K, El-adly W. Forearm lengthening using Ilizarov external fixator. Eur Orthop Traumatol. 2013;4(4):217-224. doi: 10.1007/s12570-013-0161-y. [DOI] [Google Scholar]
- 21. Fagg PS. Wrist pain in the Madelung’s deformity of dyschondrosteosis. J Hand Surg Br. 1988;13(1):11-15. doi: 10.1016/0266-7681(88)90042-3. [DOI] [PubMed] [Google Scholar]
- 22. Flatt AE. The Care of Congenital Hand Anomalies. St. Louis, MO: Mosby; 1994. [Google Scholar]
- 23. Ghatan AC, Hanel DP. Madelung deformity. J Am Acad Orthop Surg. 2013;21(6):372-382. doi: 10.5435/JAAOS-21-06-372. [DOI] [PubMed] [Google Scholar]
- 24. Glard Y, Gay A, Launay F, et al. Isolated wedge osteotomy of the ulna for mild Madelung’s deformity. J Hand Surg Am. 2007;32(7):1037-1042. doi: 10.1016/j.jhsa.2007.05.015. [DOI] [PubMed] [Google Scholar]
- 25. Grigelioniene G, Eklöf O, Ivarsson SA, et al. Mutations in short stature homeobox containing gene (SHOX) in dyschondrosteosis but not in hypochondroplasia. Hum Genet. 2000;107(2):145-149. doi: 10.1007/s004390000352. [DOI] [PubMed] [Google Scholar]
- 26. Harley BJ, Brown C, Cummings K, et al. Volar ligament release and distal radius dome osteotomy for correction of Madelung’s deformity. J Hand Surg Am. 2006;31(9):1499-1506. doi: 10.1016/j.jhsa.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 27. Hawkes DH, Nixon MF. Evidence-based treatment of Madelung’s deformity. In: Alshryda S, Huntley JS, Banaszkiewicz PA. eds. Paediatric Orthopaedics. Basel, Switzerland: Springer International Publishing AG; 2017:317-321. [Google Scholar]
- 28. Henry A, Thorburn MJ. Madelung’s deformity. A clinical and cytogenetic study. J Bone Joint Surg Br. 1967;49(1):66-73. [PubMed] [Google Scholar]
- 29. Herdman RC, Langer LO, Good RA. Dyschondrosteosis. The most common cause of Madelung’s deformity. J Pediatr. 1966;68(3):432-441. [DOI] [PubMed] [Google Scholar]
- 30. Houshian S, Schrøder H, Weeth R. Correction of Madelung’s deformity by the Ilizarov technique. J Bone Joint Surg Br. 2004;86(4):536-540. [PubMed] [Google Scholar]
- 31. Kampa R, Al-Beer A, Axelrod T. Madelung’s deformity: radial opening wedge osteotomy and modified Darrach procedure using the ulnar head as trapezoidal bone graft. J Hand Surg Eur Vol. 2010;35(9):708-714. doi: 10.1177/1753193410375778. [DOI] [PubMed] [Google Scholar]
- 32. Kozin SH, Zlotolow DA. Madelung deformity. J Hand Surg Am. 2015;40(10):2090-2098. doi: 10.1016/j.jhsa.2015.03.033. [DOI] [PubMed] [Google Scholar]
- 33. Laffosse JM, Abid A, Accadbled F, et al. Surgical correction of Madelung’s deformity by combined corrective radioulnar osteotomy: 14 cases with four-year minimum follow-up. Int Orthop. 2009;33(6):1655-1661. doi: 10.1007/s00264-008-0711-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Langenskiold A. An operation for partial closure of an epiphysial plate in children, and its experimental basis. J Bone Joint Surg Br. 1975;57(3):325-330. [PubMed] [Google Scholar]
- 35. MacDermid JC, Turgeon T, Richards RS, et al. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998;12(8):577-586. doi: 10.1097/00005131-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 36. Madelung OW. Die spontane Subluxation der Hand nach vorne. Verh Dtsch Ges Chir. 1878;7:259-276. [Google Scholar]
- 37. Mallard F, Jeudy J, Rabarin F, et al. Reverse wedge osteotomy of the distal radius in Madelung’s deformity. Orthop Traumatol Surg Res. 2013;99(4)(suppl):S279-S283. doi: 10.1016/j.otsr.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 38. McCarroll HR, James MA, Newmeyer WL, et al. Madelung’s deformity: quantitative assessment of x-ray deformity. J Hand Surg Am. 2005;30(6):1211-1220. doi: 10.1016/j.jhsa.2005.06.024. [DOI] [PubMed] [Google Scholar]
- 39. Murphy MS, Linscheid RL, Dobyns JH, et al. Radial opening wedge osteotomy in Madelung’s deformity. J Hand Surg Am. 1996;21(6):1035-1044. doi: 10.1016/S0363-5023(96)80312-1. [DOI] [PubMed] [Google Scholar]
- 40. Nielsen JB. Madelung’s deformity: a follow-up study of 26 cases and a review of the literature. Acta Orthop Scand. 1977;48(4):379-384. [DOI] [PubMed] [Google Scholar]
- 41. Potenza V, Farsetti P, Caterini R, et al. Isolated Madelung’s deformity: long-term follow-up study of five patients treated surgically. J Pediatr Orthop B. 2007;16(5):331-335. doi: 10.1097/BPB.0b013e3282ee9183. [DOI] [PubMed] [Google Scholar]
- 42. Ranawat CS, DeFiore J, Straub LR. Madelung’s deformity. An end-result study of surgical treatment. J Bone Joint Surg Am. 1975;57(6):772-775. [PubMed] [Google Scholar]
- 43. Rappold GA, Fukami M, Niesler B, et al. Deletions of the homeobox gene SHOX (short stature homeobox) are an important cause of growth failure in children with short stature. J Clin Endocrinol Metab. 2002;87(3):1402-1406. doi: 10.1210/jc.87.3.1402. [DOI] [PubMed] [Google Scholar]
- 44. Saffar P, Badina A. Treatment of Madelung’s deformity. Chir Main. 2015;34(6):279-285. doi: 10.1016/j.main.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 45. Salon A, Serra M, Pouliquen JC. Long-term follow-up of surgical correction of Madelung’s deformity with conservation of the distal radioulnar joint in teenagers. J Hand Surg Br. 2000;25(1):22-25. doi: 10.1054/jhsb.1999.0304. [DOI] [PubMed] [Google Scholar]
- 46. Schmidt-Rohlfing B, Schwobel B, Pauschert R, et al. Madelung deformity: clinical features, therapy and results. J Pediatr Orthop B. 2001;10(4):344-348. [PubMed] [Google Scholar]
- 47. Stehling C, Langer M, Nassenstein I, et al. High resolution 3.0 Tesla MR imaging findings in patients with bilateral Madelung’s deformity. Surg Radiol Anat. 2009;31(7):551-557. doi: 10.1007/s00276-009-0476-0. [DOI] [PubMed] [Google Scholar]
- 48. Steinman S, Oishi S, Mills J, et al. Volar ligament release and distal radial dome osteotomy for the correction of Madelung deformity: long-term follow-up. J Bone Joint Surg Am. 2013;95(13):1198-1204. doi: 10.2106/JBJS.L.00714. [DOI] [PubMed] [Google Scholar]
- 49. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-Analysis of Observational Studies in Epidemiology (MOOSE) Group. JAMA. 2000;283(15):2008-2012. [DOI] [PubMed] [Google Scholar]
- 50. Vickers D, Nielsen G. Madelung deformity: surgical prophylaxis (physiolysis) during the late growth period by resection of the dyschondrosteosis lesion. J Hand Surg Br. 1992;17(4):401-407. doi: 10.1016/S0266-7681(05)80262-1. [DOI] [PubMed] [Google Scholar]
- 51. Watson HK, Pitts EC, Herber S. Madelung’s deformity a surgical technique. J Hand Surg Am. 1993;18(5):601-605. doi: 10.1016/0266-7681(93)90013-6. [DOI] [PubMed] [Google Scholar]
- 52. Zebala LP, Manske PR, Goldfarb CA. Madelung’s deformity: a spectrum of presentation. J Hand Surg Am. 2007;32(9):1393-1401. doi: 10.1016/j.jhsa.2007.08.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, DS_10.1177_1558944718793179 for Surgical Management of Madelung Deformity: A Systematic Review by Abbas Peymani, Anna Rose Johnson, Arriyan S. Dowlatshahi, Johannes G. G. Dobbe, Samuel J. Lin, Joseph Upton, Geert J. Streekstra and Simon D. Strackee in HAND