Abstract
The primary premature ejaculation (PPE) is a common male sexual disorder. We proposed a novel behavioral therapy for PPE through regular penis-root masturbation (PRM). Nine heterosexual men with PPE completed the self-controlled study. After a 3-month PRM training, the median intravaginal ejaculatory latency time (IELT) increased from 60 s to 180 s (P = 0.018), and the mean Premature Ejaculation Diagnostic Tool (PEDT) score decreased from 14.8 ± 3.7 to 12.8 ± 4.1 (P = 0.074). Five out of eight patients had the prolonged dorsal nerve somatosensory evoked potential (DNSEP). The results suggest that PRM has a short-term therapeutic effect. Randomized controlled trials are needed to validate the efficacy.
Premature ejaculation (PE) is a common male sexual disorder characterized by short ejaculatory latency, weak ability to control ejaculation, and PE-associated negative psychological and relational consequences.1 A variety of treatments have been recommended in the management of PE, such as pharmacotherapy, behavioral therapy (BT), and a combined behavioral and drug therapy.2 Although the pharmacotherapy is considered as a first-line treatment for primary PE (PPE), the associated deficiencies, including the side effects, variable effectiveness, and relatively high dropout rate, have hindered the adoption of this therapy.3 For patients who are unwilling to accept or do not respond to pharmacotherapy, BT is a viable therapeutic option. The typical techniques in behavioral therapy include the stop–start technique developed by Semans and the squeeze technique proposed by Masters and Johnson.4 Pelvic floor muscle rehabilitation exercises may also be helpful in treating PE.5 Although the overall success rates are reported to reach 50%–60%, the conventional BTs in the treatment of PPE are still controversial in terms of the intravaginal ejaculatory latency time (IELT).6 Maybe we need to find a new BT technique to improve the curative effect.
In a sense, the stop–start technique is thought to be a “typical” masturbatory style because the front two-thirds of the penis receives stimulation in the vagina, and it has limited effect on prolongation of the IELT.7 In addition, delayed ejaculation (DE) can be caused by “atypical” (idiosyncratic) masturbation that is a masturbation technique not easily duplicated by the partner's hand, mouth, or vagina.8 PE and DE are seemingly unrelated two extremities of ejaculatory disorder; however, there is a relationship between them that the idiosyncratic masturbatory style can cause DE, thereby suggesting that this kind of unusual masturbation has the potential to treat PE. The specific mode of idiosyncratic masturbation is prone masturbation.9 In our clinic, we also found that some patients complained the delayed ejaculation during penis-root masturbation. Therefore, we attempted to verify the hypothesis that regular penis-root masturbation as a behavior therapy had a therapeutic effect in patients with primary PE.
PATIENTS AND TECHNIQUE
The protocol and written informed consent used in this study were reviewed and approved by the Institutional Review Board of the Third Affiliated Hospital of Sun Yat-sen University, Guangzhou, China (trial registration number: (2018)02-209-01).
Male patients with PE were recruited from the outpatient clinic at the Third Affiliated Hospital of Sun Yat-sen University according to the following inclusion criteria: (1) patients' age varied from 18 to 45 years; (2) patients met the 2014 International Society for Sexual Medicine (ISSM) definition criteria for PPE;1 (3) patients had a stable, heterosexual relationship with a single sexually active female partner for at least 6 months and with at least two sexual intercourses a week and kept stable during the study period; (4) patients were identified if their scores were higher than 9 on the Chinese version of Premature Ejaculation Diagnostic Tool (PEDT); and (5) patients had no history of any previous therapies for PE or had recently stopped the therapies for at least 3 months.
Patients were not permitted to enroll in the study if they met any of the following exclusion criteria: (1) patients were diagnosed with secondary PE, variable PE, and subjective PE; (2) patients were diagnosed with erectile dysfunction (ED) if their scores were <21 on the abridged five-item International Index of Erectile Function (IIEF-5), unless the low IIEF-5 score was completely related to symptoms of PE; (3) patients were using medications for endocrinological, metabolic, chronic systemic, or psychiatric diseases; (4) patients were diagnosed with sexual hormone abnormalities, hyperthyroidism, hypothyroidism, Peyronie's disease, prostatitis, urethritis, or urinary tract infection; and (5) patients were abusing alcohol or illegal drugs. During the treatment period, the use of any other therapies for PE was inhibited.
Upon enrollment, all participants completed the questionnaires including PEDT and IIEF-5. The genital examinations were performed to check if the participants had urogenital abnormality. Penile dorsal nerve somatosensory evoked potential (DNSEP) that is an electroencephalographic response after stimulating the somatic sensory area of penile dorsal nerve was measured.10 The therapeutic efficacy of PRM was evaluated through comparison of the mean PEDT score and self-reported IELT value before and after a 3-month PRM training. DNSEP was retested after 3 months of PRM.
PRM was performed in a private setting. Briefly, the penis was fully erected through various sexual stimuli instead of directly stimulating the glans, frenulum, and distal penile shaft. It is required to avoid stimulating the distal penile shaft because the stimulation could probably affect the frenulum simultaneously. Then, one thumb or two thumbs were placed on the dorsal surface of the penile root (within the rear one-third of the penis) (Figure 1), and the penile root was massaged circularly or along the proximal penile shaft firmly to allow the patients to feel sexual pleasure and keep erection. When the patients felt the urge to ejaculate, the stimulation was stopped immediately. When the sensation subsided, the stimulation was resumed. During the training session, the partner's touch, kiss, and audiovisual sexual stimulation were permitted. Each training session was required to last 10–15 min. After the training session, ejaculation was permitted. Unlike precoital masturbation that requires ejaculation before a formal intercourse, PRM was not prepared for a formal intercourse. The vaginal intercourse was permitted after the training session. The training was conducted three times a week for 3 months and could be done by the patient himself or his partner.
Figure 1.
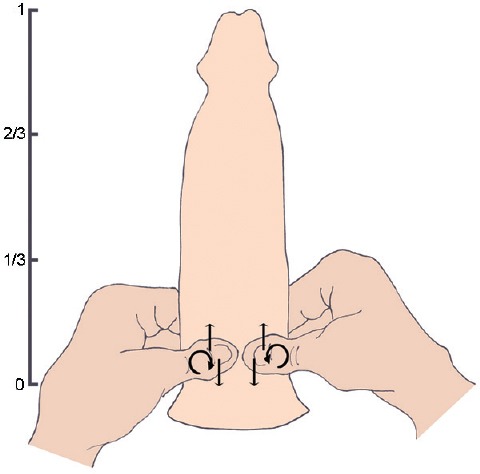
Diagram of regular PRM: the PRM was performed by placing the thumb (one hand) or thumbs (two hands) on the root of the penis (no more than 1/3 of the erect penis) and rubbing the penile root up and down (straight arrow) or circularly (curve arrow) with a certain degree of friction. PRM: penis-root masturbation.
Statistical analysis was conducted using IBM SPSS software version 19 (SPSS, Inc., Chicago, IL, USA). Data were normally distributed according to the Shapiro–Wilk test. Differences of the mean PEDT scores and mean DNSEP in patients before and after a 3-month training were compared using the paired t-test. Differences of the self-reported IELT in patients before and after a 3-month training were compared using the Wilcoxon signed-rank test. Differences were considered statistically significant at P < 0.05.
During the period of May through November 2018, a total of 16 patients met the enrollment criteria and volunteered to participate. During the study period, four patients declined to continue the treatment without any reasons, and three could not stick to the treatment plan. All of these seven patients quitted the study in less than a month. Finally, nine patients completed the entire treatment regimen. The characteristics of the participants are listed in Table 1. The mean age of nine participants was 30.2 ± 5.1 years, the mean frequency of sexual intercourse was 3.0 ± 1.3 times a week, and the mean duration of PE was 6.3 ± 5.2 years.
Table 1.
Characteristics of nine participants in the study
| Case | Age (year) | Weight (kg) | Height (cm) | BMI (kg m−2) | Smoking history | Drinking history | Educational background | PE history (year) | Frequency of intercourse (time per week) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 31 | 56 | 165 | 20.6 | No | Yes | TSS | 8 | 4 |
| 2 | 28 | 68 | 172 | 23.0 | No | Yes | TSS | 13 | 3 |
| 3 | 41 | 52 | 150 | 23.1 | No | Yes | JHS | 15 | 2 |
| 4 | 28 | 68 | 170 | 23.5 | No | Yes | Undergraduate | 5 | 2 |
| 5 | 28 | 62 | 173 | 20.7 | No | No | SHS | 1 | 2 |
| 6 | 26 | 62 | 172 | 21.0 | No | Yes | SHS | 1 | 3 |
| 7 | 29 | 78 | 173 | 26.1 | Yes | Yes | TSS | 5 | 2 |
| 8 | 36 | 60 | 165 | 22.0 | No | Yes | JHS | 1 | 6 |
| 9 | 25 | 55 | 160 | 21.5 | No | No | JHS | 8 | 3 |
| Mean±s.d. | 30.2±5.1 | 62.3±8.0 | 166.7±7.7 | 22.4±1.8 | - | - | - | 6.3±5.2 | 3.0±1.3 |
BMI: body mass index; JHS: junior high school; s.d.: standard deviation; SHS: senior high school; TSS: technical secondary school; PE: premature ejaculation; -: not applicable
The therapeutic effectiveness of PRM was assessed in terms of the mean PEDT score, self-reported IELT value, and DNSEP, as listed in Table 2. Before the penis-root masturbatory training, the mean baseline PEDT score in participants was 14.8 ± 3.7, and the median self-reported IELT was 60 s ranging from 30 s to 60 s. Here, it is noted that the IELT was recorded as 60 s when the patient just said the IELT was <1 min without telling the exact time. The mean baseline latency time of DNSEP was 38.73 ± 2.63 ms in nine participants. The levels of serum fasting blood glucose, thyroid hormones, and sexual hormones in the blood samples obtained from patients were tested, and all of the values were within the normal range (data not shown). No symptom of urinary tract infection was found in participants by urinalysis. The IIEF-5 scores were normal. No abnormality was found in participants by genital examinations.
Table 2.
Results of premature ejaculation evaluation using Premature Ejaculation Diagnostic Tool, intravaginal ejaculatory latency time, and dorsal nerve somatosensory evoked potential at baseline and after 3 months of the penis-root masturbatory training
| Case | PEDT score | IELT (s) | DNSEP (ms) | |||
|---|---|---|---|---|---|---|
| Baseline | 3 months | Baseline | 3 months | Baseline | 3 months | |
| 1 | 10 | 10 | 60 | 300 | 37.4 | 39.5 |
| 2 | 14 | 10 | 60 | 240 | 39.0 | 40.0 |
| 3 | 19 | 18 | 30 | 60 | 34.4 | 34.6 |
| 4 | 16 | 17 | 60 | 60 | 37.0 | 37.6 |
| 5 | 13 | 16 | 60 | 60 | 42.9 | 42.1 |
| 6 | 20 | 14 | 60 | 300 | 37.6 | 34.9 |
| 7 | 17 | 14 | 60 | 180 | 40.0 | 38.2 |
| 8 | 15 | 11 | 60 | 120 | 42.1 | NA |
| 9 | 9 | 5 | 60 | 240 | 38.2 | 41.6 |
| Mean±s.d. | 14.8±3.7 | 12.8±4.1 | 56.7±10.0 | 173.3±101.5 | 38.31±2.47 (8 cases) 38.73±2.63 (9 cases) |
38.56±2.80 |
| Median (range) | 15 (9–20) | 14 (5–18) | 60 (30–60) | 180 (60–300) | 38.20 (34.40–42.90) | 38.85 (34.60–42.10) |
| P | 0.074 | 0.018 | 0.734 | |||
Differences in the mean PEDT scores and DNSEP in patients before and after a 3-month training were compared using the paired t-test. Differences in the self-reported IELT in patients before and after a 3-month training were compared using the Wilcoxon signed-rank test. Differences were considered statistically significant at P<0.05. DNSEP: dorsal nerve somatosensory evoked potential; IELT: intravaginal ejaculation latency time; PEDT: Premature Ejaculation Diagnostic Tool; NA: not available; s.d.: standard deviation
After the 3-month penis-root masturbatory training, the median IELT was 180 s (range: 60–300 s) that was significantly longer than 60 s at baseline (range: 30–60 s, P = 0.018). Seven (77.8%) out of nine participants reported that the IELT was prolonged by about 120 s. The mean PEDT score decreased from 14.8 ± 3.7 at baseline to 12.8 ± 4.1 after 3-month PRM (P = 0.074). Eight participants were retested for DNSEP after 3-month PRM, and the mean latency time was 38.56 ± 2.80 ms that was longer than 38.31 ± 2.47 ms at baseline, but the difference was not statistically significant (P = 0.734).
COMMENTS
Ejaculation is a complex physiological process involving a variety of biological, psychological, and social factors, and it is challenging to understand the neurophysiopharmacology of ejaculatory disorders.11 Many researches have focused on the pathophysiology and pharmacological treatments of PE, but little attention was paid to BT, as well as its underlying mechanism.12 The ultimate goal of BT is to develop sexual skills over time to control or delay ejaculation, thereby improving sexual confidence.6,13 Although BT has also been used to treat PE, the mechanism underlying the treatment of PE remains to be elucidated. The mechanism of delayed ejaculation (DE) includes both psychogenic and physical factors. Xia et al.14 reported that patients with primary DE have penile shaft rather than glans hyposensitivity, though it is not stated if the patients have unusual masturbation. Through unusual masturbation, patients with DE may develop the autosexual patterns that produce different types of orgasm from what they experience with a partner.15
In this study, we found that five out of eight patients had prolonged ejaculation time when they were retested for DNSEP after regular PRM. There are multiple possible mechanisms for the acquired prolonged IELT, however, the most plausible mechanism might be attributed to autosexual orientation that could enable the patients to develop a specialized synergistic ability of the peripheral and central nervous systems to control the ejaculation.8,11,15,16 It can be described as follows: (1) the sensate focus is shifted to the penile root which might reduce the feeling of irritation to the glans or decrease glans sensitivity during vaginal intercourse, and (2) the patients are getting used to this uncommon stimulation style that cannot be easily duplicated by their partner's vagina.
Despite the prospective nature of the study, there are still some limitations. Self-estimation rather than a stopwatch was used to measure the IELT in this work. Although the self-estimation may be an inaccurate measure of actual IELT, some studies have demonstrated that patient self-report of ejaculatory latency has a good correlation with objective stopwatch latency.17 Compared to a rapid-acting pharmacological treatment, most BTs require a willingness of the patients to engage in practicing the relatively dull techniques, which may explain the higher attrition rate in our study. The current study only evaluated the short-term therapeutic effect of regular PRM in patients with primary PE immediately after a 3-month training session, and little is known about the long-term effects. In addition, we had a relatively small sample size and uncontrolled and nonblinded assessment of primary outcome. Therefore, it is needed to conduct a new multicenter, large-scale, randomized, comparative clinical trial to validate the efficacy and explore the underlying mechanism of regular PRM as a novel BT.
CONCLUSION
Regular PRM, as a novel BT, is a promising therapeutic approach for PPE. However, it is still required to be further verified in randomized controlled trials, and the underlying mechanism is also needed to be elucidated.
AUTHOR CONTRIBUTIONS
YZ developed the original content and drafted the manuscript. GCM contributed to the clinical trial design, data acquisition, and data interpretation. ZJZ contributed to data acquisition, statistical analysis, and data interpretation and drafted the manuscript. YFL and XZ contributed to data acquisition. YZ, ZJZ, and GCM contributed to the critical revision of the manuscript. All authors read and approved the final manuscript.
COMPETING INTERESTS
All authors declared no competing interests.
ACKNOWLEDGMENTS
This work was supported by the National Natural Science Foundation of China (Grant No. 81571424 and No. 81771565).
REFERENCES
- 1.Althof SE, McMahon CG, Waldinger MD, Serefoglu EC, Shindel AW, et al. An update of the International Society of Sexual Medicine's Guidelines for the diagnosis and treatment of premature ejaculation (PE) J Sex Med. 2014;2:60–90. doi: 10.1002/sm2.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hatzimouratidis K, Giuliano F, Moncada I, Muneer A, Salonia A, et al. EAU Guidelines Panel on Male Sexual Dysfunction. EAU guidelines on Male Sexual Dysfunction. Edn. presented at the EAU Annual Congress Copenhagen. 2018 [Google Scholar]
- 3.Castiglione F, Albersen M, Hedlund P, Gratzke C, Salonia A, et al. Current pharmacological management of premature ejaculation: a systematic review and meta-analysis. Eur Urol. 2016;69:904–16. doi: 10.1016/j.eururo.2015.12.028. [DOI] [PubMed] [Google Scholar]
- 4.Melnik T, Althof S, Atallah AN, Puga ME, Glina S, et al. Psychosocial interventions for premature ejaculation. Cochrane Database Syst Rev. 2011;8:CD008195. doi: 10.1002/14651858.CD008195.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Pastore AL, Palleschi G, Leto A, Pacini L, Iori F, et al. A prospective randomized study to compare pelvic floor rehabilitation and dapoxetine for treatment of lifelong premature ejaculation. Int J Androl. 2012;35:528–33. doi: 10.1111/j.1365-2605.2011.01243.x. [DOI] [PubMed] [Google Scholar]
- 6.Cooper K, Martyn-St James M, Kaltenthaler E, Dickinson K, Cantrell A, et al. Behavioral therapies for management of premature ejaculation: a systematic review. Sex Med. 2015;3:174–88. doi: 10.1002/sm2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Semans JH. Premature ejaculation: a new approach. South Med J. 1956;49:353–8. doi: 10.1097/00007611-195604000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Perelman MA. Idiosyncratic masturbation patterns: a key unexplored variable in the treatment of retarded ejaculation by the practicing urologist. J Urol. 2005;173(4 Suppl):340. [Google Scholar]
- 9.Bronner G, Ben-Zion IZ. Unusual masturbatory practice as an etiological factor in the diagnosis and treatment of sexual dysfunction in young men. J Sex Med. 2014;11:1798–806. doi: 10.1111/jsm.12501. [DOI] [PubMed] [Google Scholar]
- 10.Xia JD, Zhou LH, Han YF, Chen Y, Wang R, et al. A reassessment of penile sensory pathways and effects of prilocaine-lidocaine cream in primary premature ejaculation. Int J Impot Res. 2014;26:186–90. doi: 10.1038/ijir.2014.5. [DOI] [PubMed] [Google Scholar]
- 11.Clement P, Giuliano F. Physiology and pharmacology of ejaculation. Basic Clin Pharmacol Toxicol. 2016;119(Suppl 3):18–25. doi: 10.1111/bcpt.12546. [DOI] [PubMed] [Google Scholar]
- 12.Gur S, Sikka SC. The characterization, current medications, and promising therapeutics targets for premature ejaculation. Andrology. 2015;3:424–42. doi: 10.1111/andr.12032. [DOI] [PubMed] [Google Scholar]
- 13.Althof SE. Psychosexual therapy for premature ejaculation. Transl Androl Urol. 2016;5:475–81. doi: 10.21037/tau.2016.05.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xia JD, Han YF, Pan F, Zhou LH, Chen Y, et al. Clinical characteristics and penile afferent neuronal function in patients with primary delayed ejaculation. Andrology. 2013;1:787–92. doi: 10.1111/j.2047-2927.2013.00119.x. [DOI] [PubMed] [Google Scholar]
- 15.Chen J. The pathophysiology of delayed ejaculation. Transl Androl Urol. 2016;5:549–62. doi: 10.21037/tau.2016.05.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lu J, Zhang X, Wang H, Qing Z, Han P, et al. Short- and long-range synergism disorders in lifelong premature ejaculation evaluated using the functional connectivity density and network property. Neuroimage Clin. 2018;19:607–15. doi: 10.1016/j.nicl.2018.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Althof SE, Abdo CH, Dean J, Hackett G, McCabe M, et al. International Society for Sexual Medicine's guidelines for the diagnosis and treatment of premature ejaculation. J Sex Med. 2010;7:2947–69. doi: 10.1111/j.1743-6109.2010.01975.x. [DOI] [PubMed] [Google Scholar]


