Introduction
Dietary assessment is fraught with error among adults [1] and especially among children [2, 3]. As much as 50% of child reported 24 hour dietary recall of foods for the previous day’s breakfast and lunch had errors [4] as assessed against direct observation of consumption. Innovative technology may provide more accurate assessments of dietary intake [5].
One recently available innovative method is a camera worn on the chest (called an eButton) that takes images of whatever is in front of the wearer at brief intervals (2 sec to 10 sec) throughout the day [6–10]. Images of foods could minimize inaccurate recall of foods, but may have other limitations. These images can be clustered into images of a common single eating event [9–12]. Some of the foods in the food event image clusters can be automatically identified, but most must be identified by observers, usually dietitians [9, 10]. Food image portion size can be estimated using an innovative digital wire mesh procedure [9, 10, 13–16]. While the eButton has been tested among adults [14–16], adapting it for use by children requires understanding of its acceptance and procedural use. Two formative studies were conducted for using the eButton with children.
Study 1
Methods
Sample and Recruitment
In the Summer of 2014, a sample of 21 healthy 8–13 year old children and their parents were recruited from the Children’s Nutrition Research Center’s volunteer participant database, flyers posted throughout the Texas Medical Center in Houston, Texas, and online announcements on the Baylor College of Medicine and Children’s Nutrition Research Center web sites. Of those 21 children 5 were siblings having a total of 16 parents. Saturation is a criterion for sample size in qualitative research. In our experience 16 would be ample to reach saturation. Inclusionary criteria were children between 8–13 years old (to extend our previous work [4, 17]), willing to eat one meal while wearing the eButton, and parent and child willing to answer questions about the eButton. In our previous research [4, 17], 8 to 13 years encompasses ages when children had difficulty reporting intake (8–9 years) to when no unusual difficulties were encountered (12–13 years). A detailed feasibility study protocol was approved by the Baylor College of Medicine Institutional Review Board. Signed informed child assent and parent consent were obtained. The parent received a stipend of $20 and the child received $15 for participating in this study.
Procedures
Two eButtons were tested: one light weight (about 42–45 grams) with an 8 hour battery life, and a heavier one (about 70 grams) with a 12–14 hour battery life. First, the heavier eButton was attached with a cloth strap on the front of the child’s shirt at chest height and the child was asked to walk and run around the room. The same procedure was then followed with the lighter eButton. The child was then seated at a dining table. Height of the eButton camera to top of the table was measured. We asked if the child would wear the eButton for 2–3 days at a time and any concerns the child or parent might have wearing it. Lunch or dinner foods chosen by the child from a menu were then placed on a standard dinner plate (diameter 26cm, depth 2.25 cm) or bowl (diameter 15.5 cm, depth 5cm) in front of the child. Eighteen menu specified items included, for example, a breakfast meal like oatmeal with fruit and yogurt; or a lunch selection like ham sandwich with a side of fruit and a drink. Once the child finished the meal, the child’s thoughts about wearing the camera were queried.
A second staff person in a separate room interviewed the parent concerning the child wearing the eButton. Interviews were audio recorded.
Portion Size Estimation.
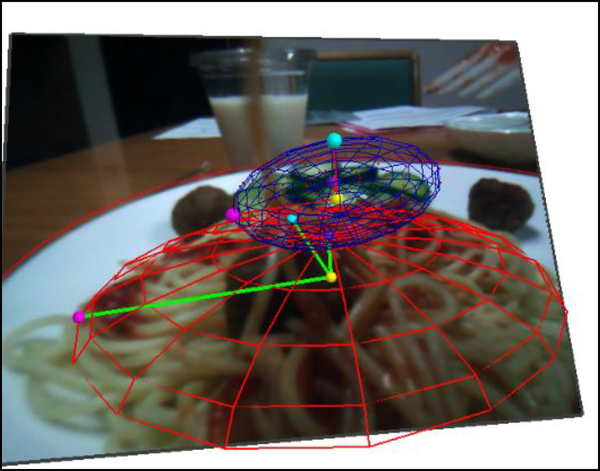
Portion size was estimated using wire-mesh software and images before and after intake from the pre-chosen meal. Technical details about portion measurement have been described [14–16]. True portion size before consumption was known from the detailed menu. Four analysts (one expert engineer from the University of Pittsburgh, who was facile in use of the wire mesh procedure, two research dietitians, and one undergraduate research assistant) estimated the foods portion sizes independently to assess interobserver reliability. The pictures were downloaded and imported to the specialized software (see Figure 1) [9]. Clear pictures were identified within the software before the foods had been eaten. The foods in the pictures were specified in the Food and Nutrition Database for Dietary Studies (FNDDS) food database embedded in the software. A 3-dimensional wire mesh, which best matched the shape of food, was selected, resized and deformed to fit the food (see Figure 1). After fitting, the volume of the wire mesh (in cm3) provided a measure of portion size. The diameter of the dinnerware (circular plate) on which the food was served was previously measured, providing a reference for the mesh. A total of 138 food items were analyzed. The portion sizes of 88 food items were estimated using the 3-dimensional wire mesh and 50 through visual estimation. Foods that were not able to be analyzed through the mesh software were either foods that were one whole piece with an irregular shape (e.g. individual pizza, hot dog) or the shape of a mesh was not available (e.g. meatballs in spaghetti, condiment packs). For these types of foods, a visual estimate of the portion size was entered directly in the software using the appropriate FNDDS options.
Figure 1.
Half ellipse wire mesh for image volume estimation.
Data Analysis
Audio-recordings were transcribed; transcriptions were checked against audio-recordings; and imported into NVivo software (QSR NVivo 10.0, 2012, Doncaster, Victoria, Australia). Responses were thematically classified by question in the interview guide; codes were derived as the classification proceeded. Two coders coded all transcripts; differences in code assignment were adjudicated by consensus. Agreement on the portion size estimates among the four analysts and the known value were assessed using the intra-class correlation, which took into account observers nested within food items, nested within participants. The USDA’s Food and Nutrient Database for Dietary Studies (5.0, 2012) was used to code dietary intake data and calculate calories and portion intakes [18].
Results
The average age of the 21 child participants was 10.4 (SD= 1.2) years. Other sample characteristics are in Table 1. Children reported neither consistent perceived difference nor preference between the lighter and heavier eButtons. The most common themes (20% or more of respondents) on the positive and negative aspects of wearing the eButton from children and parents are found in Table 2. The most common responses were the absence of perceived problems, but a few concerns were raised about comfort, wear during sports, attracting negative attention, and privacy.
Table 1.
Demographics characteristics of children for Studies 1 and 2.
| Study 1 | Study 2 | |||
|---|---|---|---|---|
| n=21 | n= 12 | |||
| Mean | SD | Mean | SD | |
| Age (yrs) | 10.48 | 1.24 | 10.67 | 1.5 |
| Frequency | Percent | Frequency | Percent | |
| Gender | ||||
| Boy | 16 | 76.2% | 5 | 41.7% |
| Girl | 5 | 23.8% | 7 | 58.3% |
| Highest Education Completed by participating parent | ||||
| 6th grade or less | 1 | 4.8% | 0 | 0% |
| High School graduate or GED | 2 | 9.5% | 1 | 8.3% |
| Technical school | 2 | 9.5% | 0 | 0% |
| Some college | 7 | 33.3% | 4 | 33.3% |
| College graduate | 6 | 28.6% | 2 | 16.7% |
| Post Graduate Study | 3 | 14.3% | 5 | 41.7% |
| Highest Education Completed in your household | ||||
| 8th grade or less | 1 | 4.8% | 1 | 8.3% |
| High School graduate or GED | 2 | 9.5% | 0 | 0% |
| Technical school | 4 | 19% | 0 | 0% |
| Some college | 5 | 23.8% | 2 | 16.7% |
| College graduate | 4 | 19% | 4 | 33.3% |
| Post Graduate Study | 5 | 23.8% | 5 | 41.7% |
| Annual Household Income | ||||
| Less than $20,000 | 2 | 9.5% | 0 | 0% |
| $20,000 to $39,000 | 3 | 14.3% | 3 | 25% |
| $40,000 to $59,999 | 6 | 28.6% | 3 | 25% |
| $60,000 to $79,999 | 3 | 14.3% | 2 | 16.7% |
| $80,000 to $100,000 | 6 | 28.6% | 1 | 8.3% |
| More than $100,000 | 1 | 4.8% | 3 | 25% |
| Ethnicity | ||||
| Hispanic | 10 | 47.6% | 2 | 16.7% |
| African American | 7 | 33.3% | 9 | 75% |
| White | 3 | 14.3% | 1 | 8.3% |
| Asian-Non Vietnamese | 1 | 4.8% | 0 | 0% |
| Weight Status | ||||
| Underweight | 1 | 8.3% | ||
| Healthy Weight | 7 | 33.3% | 6 | 50% |
| Overweight | 6 | 28.6% | 1 | 8.3% |
| Obese | 8 | 38.1% | 4 | 33.3% |
| Residence Type | ||||
| Single family house | 16 | 76.2% | 10 | 83.3% |
| Townhouse | 1 | 4.8% | 2 | 16.7% |
| Apartment | 3 | 14.3% | 0 | 0% |
| Other | 1 | 4.8% | 0 | 0% |
Table 2.
Study 1 themes identified and responses to key questions.
| Child (n=21) | n | Parent (n=16) | n |
|---|---|---|---|
| Undesirable Aspects Identified | Parents Concerns for using the eButton | ||
| Uncomfortable while wearing it, for example: | 6 | May fall or interfere while playing or during sports | 10 |
| - Straight pin on back was uncomfortable | Concern about attracting negative public’s attention and kids asking about it | 8 | |
| - Magnet feels on body | Privacy concerns while at home or school | 8 | |
| - Weight pulled the t-shirt down | Concern about loss or damage | 7 | |
| - Strap felt rough, itchy, tight around neck | |||
| - Strap didn’t match school uniform | Desirable Aspects | ||
| eButton bounced when running or skipping | 4 | Parent not having problem charging eButton or uploading pictures for 2–3 days | 15 |
| Uncomfortable while wearing it during the meal: | 9 | ||
| - Worry it’ll be damaged or get dirty while eating | Suggestions to improve eButton and overcome concerns | ||
| - Restricted movement while eating or come in way | Reduce size of eButton | 7 | |
| Desirable Aspects | Have clear instructions of the process using the eButton | 5 | |
| Wearing the eButton during a meal was comfortable and had no problems | 14 | ||
| Fine to wear the eButton for 2–3 days at a time | 15 | ||
| Suggestions to improve eButton | |||
| Reduce size of eButton | 6 |
Difficulty in obtaining pictures of foods was encountered with 7 of 21 children. For the three shortest children, a minimum height of 137 cm was needed to obtain images. Four children were too tall (≥156.7 cm) (camera to table measured 14 cm to 21.5 cm) since their images at their collarbone level were cut off. When the camera was lowered, the obtained images were acceptable.
Portion Size Estimation
Overall agreement on portion size estimation among the four analysts and the known value was moderate (ICC=0.60) when using 3-dimensional wire mesh and when estimating the portion size visually (ICC=0.57). The intra-class correlation was highest (ICC=0.97) for visual estimation when the engineer’s values were excluded, likely due to the dietitians having increased knowledge of foods, volumes and portion sizes.
Changes in Method
Based on these results the following were changed for Study 2: the heavier longer duration battery eButton was selected; a soft paracord lanyard with emergency breakaway buckles and an adjustable double barrel sliding cord lock were added (see Figure 2) allowing movement up and down in case someone pulled on the string; the eButton was placed just below the collar bone (see Figure 3) to maximize obtaining clear images; a magnet was placed inside the child’s t-shirt attached to the back side of the metallic eButton (to minimize bouncing); and the child was required to wear a t-shirt or high tank top to accommodate the magnet. No height restrictions were introduced since table heights at home would substantially vary. Given difficulties in identifying some foods and portions in the images (e.g. poor lighting, opaque packaging), a next day child food and portion verification procedure was added.
Figure 2.
eButton sliding cord lock.
Figure 3.
eButton location below the collar bone.
Study 2
Methods
Sample and Recruitment
Study 2 was conducted in winter of 2014–2015 having the child wear the eButton for one day at home and school and pilot testing the food and portion verification process. The same process was used to recruit 10 8–13 year old children (no siblings) and their parents. Ten was considered enough to encounter and identify the main problems in wearing an eButton all day. Inclusionary criteria were children between 8–13 years old, willing to wear the eButton for one day, and parent and child willing to answer questions about the eButton and send images via internet. Exclusionary criterion was participation in Study 1. A detailed study protocol was approved by Baylor College of Medicine Institutional Review Board, and written parent consent and child assent were obtained. Both staff were trained dietitians, who processed the Study 1 images, and passed all Baylor College of Medicine courses on human subjects and HIPAA confidentiality. Participating children were reimbursed $20 and parents $30.
Procedures
A full explanation was given to both child and parent in our Center on how to wear the eButton including type of shirt, specific location on the chest, turning it on/off, and charging the eButton. Staff provided a standard white plate (diameter 26cm, depth 2.25 cm), two size bowls (diameter 13.5cm and 15.5cm, depth 3.5 cm and 5cm respectively), and a small measuring tape; explained and demonstrated how to measure other dinnerware height and diameter (measures needed for volume estimation); demonstrated how to remove the Secure Digital card with the pictures to upload and send the pictures through bigfile; and how to complete a log of usage and problems. A food amount booklet (paper copy) was provided for the food and portion verification interview.
All images taken by the eButton were automatically encrypted, and unencrypted only by trained staff. Images with foods were identified and drawn into a separate file. All images with people in the file were de-identified by blurring faces or identifying information. Images not related to food events were deleted from the food analysis computer. After identifying food events, images were selected for before and after eating based on quality of the image, and whether the food could be clearly identified. When no clear image was available the best one was selected. Images with foods were uploaded to the volume estimation software. All the food items were searched in Food and Nutrition Database for Dietary Studies by dietitians within the volume estimation software and added to a list created by the software. When no exact food was found in the database a judgment of closest equivalent was made to identify the food. For example, “oatmeal not specified” was chosen versus “oatmeal with sugar, prepared with milk” since from the picture it was not possible to assess if it was prepared with milk or water or any additions to the oatmeal. Details on food preparation were asked at the food verification interview. Any unidentified food item, for example liquid in a colored cup or picture not clear, was flagged for food identification by the child. All the food and portion verification images were grouped in a file and sent via email to the parent before the verification phone call. On the same day the pictures were processed (the day after the images were obtained), a research dietitian conducted an audio-recorded phone-conducted food verification interview, where all the unidentified pictures were clarified, and the portion sizes were verified by the child. Food items recalled by the child as consumed, but not in the pictures, were also included. These data were collected and analyzed using Nutrition Data System for Research (NDSR) software version 2015, developed by the Nutrition Coordinating Center (NCC), University of Minnesota, Minneapolis, MN [18]. After the food verification interview, child and parent interviews were conducted about their experience with the eButton.
Portion Size Estimation
Before the interview, portion size estimation using the 3-dimensional wire mesh software was conducted on the images able to be estimated. Foods that could not be software analyzed (e.g. plate size not measured) were visually estimated, and child-confirmed during the food and portion verification interview. After the interview, the list of food items was updated, and transferred back into the Food and Nutrition Database for Dietary Studies eButton software component.
Data Analysis
The data analysis procedures from Study 1 were used. The dietitians estimated portions independently.
Results
Twelve 8–12 yo children participated in this study. Average participant age was 10.7 (SD= 1.49) years. Details are in Table 1. Two children were dropped from the sample: for one the camera battery did not work properly and the family did not follow protocol procedures; the other did not have internet access at home and did not follow the wear time schedule. There was an average of 9 hours of images (minimum 4 hours; maximum 13 hours) from these 10 participants.
Food Identification and Portion Size Estimation
A total of 118 (84.2%) food items were identified before the food and portion verification interview (see Table 3). Twenty two (15.7%) additional food items were identified in the food and portion verification interview. Characteristics of these images are detailed in Table 3. After the food verification one food item was not recalled by the child even when the picture was available. This item was removed from the intra-class correlation analysis.
Table 3.
Food items before and after food verification in Study 2.
| Counts | % | |
|---|---|---|
| Total food items | 140 | 100 |
| Total of food items before food verification | 118 | 84.3 |
| Total of food items added from food verification | 22 | 15.7 |
| Before meal pictures available (numbers of food items) | ||
| Yes | 114 | 81.4 |
| No | 26 | 18.6 |
| After meal pictures available (numbers of food items) | ||
| Yes | 94 | 67.1 |
| No | 46 | 32.9 |
| Identification of foods (numbers of food items) | ||
| Foods accurately identified by dietitians | 71 | 50.7 |
| Blurry pictures | 6 | 4.3 |
| Dietitians not able to identify | 33 | 23.6 |
| More ingredient details needed for sandwich or mixed dish | 14 | 10.0 |
| More details needed for drink based on color | 7 | 5.0 |
| Not identified correctly (as determined by child interview) | 9 | 6.4 |
| Adequate placement of foods in the images (numbers of food items) | ||
| Correct placement to obtain image | 85 | 60.7 |
| Not correct placement | 47 | 33.6 |
| Images not available | 7 | 5.0 |
| Identification of portion size (numbers of food items) | ||
| Visual | 124 | 88.6 |
| Wire Mesh | 16 | 11.4 |
| Omission | ||
| Picture is available but was not recalled by child | 1 | 0.7 |
| Meals recorded for the day (numbers of children) | ||
| Complete meals (three meals + snacks) | 5 | 50 |
| Meals missing dinner pictures | 4 | 40 |
| Meals missing lunch & dinner pictures | 1 | 10 |
The intra-class correlation for portion size agreement between the two research dietitians using a consumed calories metric was moderate (0.53) with 3-dimensional wire mesh, but very good (0.98) when estimated visually. For the consumed servings metric, agreement was moderate when using the 3-dimensional wire mesh (0.59) and very good for visual estimation (0.99). When including the portion size verification data the agreement for consumed calories was both good using the 3-D wire mesh (0.62) and visual estimation (0.98). The approximate duration for the staff processing of the images for one day for one child was about 9 hours.
The most frequent child and parent themes about their experiences are summarized in Table 4. Again, the most common responses were in regard to ease and comfort of using the eButton.
Table 4.
Study 2 responses identified to key questions
| Child (n=12) | n | Parent (n=12) | n |
|---|---|---|---|
| Undesirable Aspects | Parents experience with eButton picture process | ||
| Attracted attention from other people (3 children felt uncomfortable about it and 3 didn’t mind the attention, they liked it) | 6 | Instructions for uploading pictures easy to follow | 9 |
| Average time to upload pictures = 30 min | 8 | ||
| Battery ran out or suddenly stopped | 5 | Parent thought the process for uploading was easy | 8 |
| Forgot to turn eButton back on | 5 | Desirable Aspects | |
| Difficult to wear it in school | 4 | Willing to do the upload process of pictures for 2–3days | 7 |
| Not secure enough | 4 | No concerns wearing for 2–3 days | 5 |
| Uncomfortable to wear | 3 | Concerns for wearing the eButton | |
| Desirable Aspects | Each concern mentioned by only one parent (unwanted attention, approval from school, size too big, child distraction, find appropriate clothes to wear eButton) | ||
| Comfortable to wear during the day and meals | 7 | ||
| No anticipated problems for wearing it 2–3 days | 7 |
Discussion
While image assisted dietary recalls have been used for some time and have been accepted among adults and adolescents [19], this was a first attempt at using all day camera images to directly assess diet among children. These two pilot studies investigated whether 8–13 yo children would accept using a wearable camera, provide images for one day, and follow the procedures needed for direct dietary assessment. The eButton was able to be used by these children, but some children turned off the camera and forgot to turn it back on; the lighting made it challenging to see some of the images; some children ate standing up which did not allow a clear image; minimal necessary heights were identified to obtain images from a camera placed on a child’s chest; and the battery lasted only 9 hours, so some of the meals were missed. Thus technical limitations persist in obtaining all day images.
Diet assessment with 24 hour dietary recalls among children has encountered 50% + error (intrusions and omissions) in food identification and related problems in portion size assessment [17, 20]. Smartphones and related software have been designed to eliminate or minimize this error by taking images of the foods before and after meals to permit the assessment of dietary intake from images [21, 22]. This method, however, requires that picture taking be volitionally initiated before and after the meal, the camera be at a certain angle with proper lighting, and a fiducial marker be properly displayed in the image, all of which may pose problems for children. While there was early hope that the image review process could be completely automated, thereby providing a time efficient and low cost method of diet assessment, humans have since been involved in food identification and portion assessment with images [22]. The promise of the eButton, and other all day image taking cameras [23], has been that the non-volitional nature of all day recording of images would identify all foods consumed; portion size estimation procedures could be applied to the images taken; and thereby lead to minimal error in diet assessment, possibly even done by non-dietitians. At this time, however, children’s input is essential for food image verification to increase accuracy on food identification, especially on opaque cups for drinks and assembled foods, identification of missing foods (e.g. snacks), and portion estimation, especially for opaque packaged foods where volume can’t be estimated from images.
Although intrusions and omissions in children’s recall of foods eaten were no longer a problem when the images were visible, a number of technical problems existed. The size of the eButton needs to be smaller, thereby more discrete, so children can wear it comfortably. The resolution of the images needs to be improved in poor lighting since darker images are harder to identify. To make this system practical, the time to complete some of the image processing tasks needs to be reduced. Wire meshes for irregular, but common, food shapes (e.g. pizza slice, steak, hot dog) are needed. These problems are being studied by the engineers of our team who are designing new versions of eButton and software to improve performance.
The samples in both studies were small, self-selected, and unbalanced by gender, which are study limitations.
Conclusion
The eButton is a promising tool to minimize memory and portion size related error in child diet assessment, but poses new challenges. The eButton system for diet assessment may never be completely passive, requiring dietitian review of images and portions and child report of missing foods. Further development is needed to make the system practical and improve wearability and functionality among children.
Acknowledgments
Funding
This research was funded by a grant from the National Institutes of Health, National Cancer Institute (5 R21 CA172864), and institutional support from the U.S. Department of Agriculture, Agricultural Research Service (Cooperative Agreement 58–3092-5–001).
References
- 1.Thompson FE, Subar AF. (2013). Dietary assessment methodology Edited by Coulston AM, Boushey CJ, Ferruzzi MG. Nutrition in the Prevention and Treatment of Disease 3rd ed. San Diego, CA: Academic Press: 5–46. [Google Scholar]
- 2.Livingstone MBE, Robson PJ, Wallace JMW. (2004). Issues in dietary intake assessment of children and adolescents. British Journal of Nutrition 92, S213–222. [DOI] [PubMed] [Google Scholar]
- 3.McPherson RS, Hoelscher DM, Alexander M, Scanlon KS, Serdula MK. (2010). Dietary assessment methods among school-aged children: Validity and reliability. Preventive Medicine 31, S11–S33. [Google Scholar]
- 4.Baranowski T, Islam N, Baranowski J, Martin S, Beltran A, Dadabhoy H, Adame S, Watson KB, Thompson D, Cullen KW, Subar AF. (2012). Comparison of a web-based versus traditional dietary recall among children. Journal of the Academy of Nutrition and Dietetics 112, 527–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thompson FE, Subar AF, Loria CM, Reedy JL, Baranowski T. (2010). Need for technological innovation in dietary assessment. Journal of the American Dietetic Association 110, 48–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sun M, Fernstrom JD, Jia W, Hackworth SA, Yao N, Li Y, Li C, Fernstrom MH, Sclabassi RJ. (2010). A wearable electronic system for objective dietary assessment. Journal of the American Dietetic Association 110, 45–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bai Y, Li C, Yue Y, Jia W, Li J, Mao ZH, Sun M. (2012). Designing a wearable computer for lifestyle evaluation. Proceedings of the IEEE Annual Northeast Bioengeering Conference 2012, 93–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li Y, Jia W, Yu T, Luan B, Mao ZH, Zhang H, Sun M. (2015). A low power, parallel wearable multi-sensor system for human activity evaluation. Proceedings of the IEEE Annuals Northeast Bioengineering Conference 2015, [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sun M, Burke LE, Mao ZH, Chen Y, Chen HC, Bai Y, Li Y, Li C, Jia W. (2014). eButton: A wearable computer for health monitoring and personal assistance. Proceedings/Design Automation Conference 2014, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sun M, Burke LE, Baranowski T, Fernstrom JD, Zhang H, Chen HC, Bai Y, Li Y, Li C, Yue Y, Li Z, Nie J, Sclabassi RJ, Mao ZH, Jia W. (2015). An exploratory study on a chest-worn computer for evaluation of diet, physical activity and lifestyle. Journal of Healthcare Engineering 6, 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li Z, Wei Z, Jia W, Sun M. (2013). Daily life event segmentation for lifestyle evaluation based on multi-sensor data recorded by a wearable device. Conference Proceedings IEEE Engineering in Medicine and Biology Society 2013, 2858–2861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li Z, Wei Z, Yue Y, Wang H, Jia W, Burke LE, Baranowski T, Sun M. (2015). An adaptive hidden Markov model for activity recognition based on a wearable multi-sensor device. Journal of Medical Systems 39, 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yue Y, Jia W, Sun M. (2012). Measurement of food volume based on single 2-D image without conventional camera calibration. Conference Proceedings IEEE Engineering in Medicine and Biology Society 2012, 2166–2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jia W, Yue Y, Fernstrom JD, Yao N, Sclabassi RJ, Fernstrom MH, Sun M. (2012). Imaged based estimation of food volume using circular referents in dietary assessment. Journal of Food Engineering 109, 76–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen HC, Jia W, Yue Y, Li Z, Sun YN, Fernstrom JD, Sun M. (2013). Model-based measurement of food portion size for image-based dietary assessment using 3D/2D registration. Measurement Science and Technology 24, 105701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jia W, Chen HC, Yue Y, Li Z, Fernstrom J, Bai Y, Li C, Sun M. (2014). Accuracy of food portion size estimation from digital pictures acquired by a chest-worn camera. 17, 1671–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Diep CS, Hingle M, Chen TA, Dadabhoy HR, Beltran A, Baranowski J, Subar AF, Baranowski T. (2015). The Automated Self-Administered 24-Hour Dietary Recall for Children, 2012 version, for youth aged 9 to 11 years: A validation study. Journal of the Academy of Nutrition and Dietetics 115, 1591–1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feskanich D, Sielaff BH, Chong K, Buzzard IM. (1989). Computerized collection and analysis of dietary intake information. Computer Methods and Programs in Biomedicine 30, 47–57. [DOI] [PubMed] [Google Scholar]
- 19.Gemming L, Utter J, Ni Mhurchu C. (2015). Image-assisted dietary assessment: A systematic review of the evidence. Journal of the Academy of Nutrition and Dietetics 115, 64–77. [DOI] [PubMed] [Google Scholar]
- 20.Baranowski T, Islam N, Baranowski J, Cullen KW, Myres D, Marsh T, de Moor C. (2002). The Food Intake Recording Software System is valid among 4th grade children. Journal of the American Dietetic Association 102, 380–385. [DOI] [PubMed] [Google Scholar]
- 21.Schap TE, Zhu F, Delp EJ, Boushey CJ. (2014). Merging dietary assessment with the adolescent lifestyle. Journal of Human Nutrition and Dietetics 27 Suppl 1, 82–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martin CK, Nicklas T, Gunturk B, Correa JB, Allen HR, Champagne C. (2014). Measuring food intake with digital photography. Journal of Human Nutrition and Dietetics 27 Suppl 1, 72–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gemming L, Doherty A, Utter J, Shields E, Ni Mhurchu C. (2015). The use of a wearable camera to capture and categorise the environmental and social context of self-identified eating episodes. Appetite 92, 118–125. [DOI] [PubMed] [Google Scholar]