Abstract
Objective:
Emotional distress has been posited as a key underlying mechanism in the development and maintenance of substance use disorder (SUD), and patients seeking SUD treatment are often experiencing high levels of negative emotion and/or low levels of positive emotion. But the extent to which SUD interventions impact emotional outcomes among general SUD populations is yet unquantified. The current meta-analysis aims to fill this gap.
Method:
A total of 11,754 records were screened for randomized controlled trials examining the effect of behavioral SUD interventions on emotion outcomes. Our search yielded a total of 138 effect sizes calculated based on data from 5,146 individuals enrolled in 30 independent clinical trials. Random-effects meta-analysis was used to calculate pooled effect sizes, and meta-regression analyses examined study-level moderators (e.g., intervention type).
Results:
Findings indicated a small but significant effect of SUD interventions on emotion outcomes, d=0.157, 95%CI= 0.052–0.262 (k=30). The effect size for negative emotion was nominally bigger, d=0.162, 95%CI= 0.056–0.269 (k=30), whereas the effect for positive emotion did not reach statistical significance, d=0.062, 95%CI= −0.089–0.213 (k=7). Studies featuring SUD interventions designed to specifically target emotions (i.e., affect-regulation, mindfulness-based treatments) produced larger reductions in negative emotion compared with studies featuring interventions that did not contain specific emotion modules (e.g., contingency management).
Conclusions:
Findings suggest that SUD interventions—especially mindfulness-based and affect-regulation treatments—indeed significantly reduce negative emotion, although relatively small effect sizes indicate potential room for improvement. Conclusions regarding positive emotion should be considered preliminary due to limited numbers of samples assessing these outcomes.
Keywords: emotion, substance use disorder, intervention, randomized controlled trials, meta-analysis
Emotional distress is believed to play a key role in the development and maintenance of substance use disorder (SUD; T. B. Baker, Piper, McCarthy, Majeskie, & Fiore, 2004; Kassel, 2010). More specifically, emotional distress has long been of interest to SUD researchers as a central underlying mechanism in the etiology of SUD (T. B. Baker et al., 2004; Sinha et al., 2009; Stasiewicz & Maisto, 1993), and also as a factor driving relapse among those seeking to abstain from using substances (Cook, Spring, McChargue, & Doran, 2010; Cooney, Litt, Morse, Bauer, & Gaupp, 1997). In light of the key role posited for emotional distress in SUD, the reduction of negative emotions (e.g., sadness, anxiety) and, to a certain extent, the enhancement of positive emotions (e.g., happiness, excitement) have been a target change mechanism of many prominent SUD interventions (Carmody, 1989; Kober, 2014; Riper et al., 2014). However, previous reviews and meta-analyses have not assessed the broad efficacy of SUD interventions on emotion outcomes among individuals with SUD. Although emotional distress has long been a central focus of many SUD interventions, there is little sense for the overall efficacy of these interventions for reducing this distress. The current meta-analysis aims to fill this gap.
Emotional Processes and SUD Treatment Outcomes
The term emotional distress has been conceptualized in a variety of ways (Drapeau, Marchand, & Beaulieu-Prevost, 2012; Leventhal & Everhart, 1979). Generally characterized as a state (rather than a trait) construct (Martínez-Sánchez, Ato-García, & Ortiz-Soria, 2003), and so potentially varying over time within a given individual (Dahlquist, Czyzewski, & Jones, 1996), emotional distress has been characterized by some as involving the specific experience of anxiety and/or depression (Catanzaro, 1993), whereas in other cases it has been conceptualized more broadly to also encompass a range of other non-specific, distressing emotional experiences including high levels of negative emotion or low levels of positive emotion (Orlando, Ellickson, & Jinnett, 2001). Clark and Watson (1991)’s tripartite model suggests that measures of non-specific distress (e.g., PANAS; Denollet & De Vries, 2006) are highly correlated with measures of specific distress (i.e., anxiety/stress scales, depression scales) and thus the two types of measures are inseparable in assessing emotional distress in general. In sum, emotional distress may be used to refer to experiences assessed not only via measures of non-specific emotional distress (e.g., PANAS), but also those assessing specific internalizing symptoms (e.g., symptoms of depression and anxiety; Catanzaro, 1993; Tschann et al., 2005), which might also encompass physiological and other states in addition to emotional states (L. A. Clark & Watson, 1991). In the current paper, we use the term “negative emotion” to refer to emotional states characterized by symptoms of anxiety/stress and depression (Joiner, Catanzaro, & Laurent, 1996) as well as unpleasantness (Watson, Clark, & Tellegen, 1988), and “positive emotion” to refer to any emotion with positive valence (Watson et al., 1988). In addition, we use the term emotional distress as an umbrella term to reflect a continuous (vs. binary) construct characterized by higher levels of negative emotions (e.g., sadness) and/or internalizing symptoms (e.g., anxiety/stress or depressive symptoms) as well as by lower levels of positive emotions (e.g., anhedonia).
Multiple theories have been proposed to explain the association between emotional distress and SUD (Cooper, 1994; Cooper, Frone, Russell, & Mudar, 1995; Lee, Greely, & Oei, 1999; Marlatt & Witkiewitz, 2005). According to many of these models, using substances to cope with negative emotion and to enhance positive emotion represent psychologically distinct behaviors with differential implications for the development of SUD (Cooper et al., 1995; Marlatt & Witkiewitz, 2005). Concerning the former of these constructs, negative emotion has been thought to have strong motivational consequences, prompting both cognitive and behavioral efforts to manage or eliminate the source of the problem or the negative emotional states themselves (Cooper et al., 1995). Thus, negative emotion has been viewed as particularly important in the development and maintenance of SUD (Cooper et al., 1995; Kang, Bresin, & Fairbairn, 2018; Marlatt & Witkiewitz, 2005). Longitudinal studies indicate that high levels of negative emotion predict SUD development as well as relapse (Lowman et al., 1996; Marlatt & Donovan, 2008), and laboratory studies also provide support for a causal relationship between lab-manipulations of negative emotion and substance craving (Bresin, Mekawi, & Verona, 2018). The relationship between SUD and negative emotion is also thought to be bidirectional, with chronic substance use leading to higher baseline levels of negative emotion in substance users over time (Chaiton, Cohen, O’Loughlin, & Rehm, 2009; Pacek, Martins, & Crum, 2013).
In contrast, the role of positive emotion in SUD has been less widely researched, yielding mixed conclusions from the associated literature. Some research has indicated that high levels of positive emotion protect against the development of problematic substance use (Levine, Marcus, Kalarchian, Houck, & Cheng, 2010; Wills, 1996) and low levels of positive emotion predict both higher cravings for substances (Cook et al., 2010; Hatzigiakoumis, Martinotti, Giannantonio, & Janiri, 2011) and also relapse among those in treatment for SUD (Marlatt & Witkiewitz, 2005). On the other hand, some research has suggested that experimentally induced positive emotion is associated with higher cravings for alcohol among individuals with alcohol use disorders (Mason, Light, Escher, & Drobes, 2008). In addition, one review indicated a differential relationship between positive emotion and substance use depending on the stage of disorder progression, with high levels of positive emotion predicting the initial onset of SUD and low levels of positive emotion being associated with SUD maintenance (Cheetham, Allen, Yücel, & Lubman, 2010). The subjective experience of positive emotion may be less likely to elicit attributional searches and behavioral responding (Cooper et al., 1995; Robinson & Berridge, 1993), so one possibility is that positive emotion is in fact less relevant for understanding SUD development (Cooper, 1994; Cooper et al., 1995; Lee et al., 1999; Marlatt & Witkiewitz, 2005). It is important to note, however, that relatively few studies have examined positive emotion as a factor in the development and maintenance of SUD, and so more research is needed before conclusions can be drawn.
Although emotions have been thought to play a key role in SUD etiology and maintenance, little is known about whether emotions change during SUD treatment. An examination of how SUD interventions impact emotion may be critical for several reasons. First, many theories of SUD consider emotional distress as the true underlying mechanism driving SUD, whereas the substance use itself is merely a manifest symptom (T. B. Baker et al., 2004; Kassel, 2010; Khantzian, 1987; Nolen-Hoeksema & Watkins, 2011; Stasiewicz & Maisto, 1993). In recent decades, many clinical researchers have moved away from traditional diagnostic approaches that consider disorders as discrete entities and more towards transdiagnostic approaches that consider common underlying mechanisms and multifinality in clinical manifestation (Nolen-Hoeksema & Watkins, 2011). Therefore, even among non-comorbid SUD populations, implementing SUD interventions that are successful at diminishing substance use but leave underlying sub-clinical emotional symptoms unaddressed may raise concerns for (a) the development of emotional disorders or other harmful behaviors (e.g., self-harm, aggression; Arendt et al., 2007; Dhossche, Meloukheia, & Chakravorty, 2000) in place of SUD and/or (b) relapse to substance use. In other words, implementing a SUD intervention that has no impact on emotional distress might be thought similar to administering paracetamol to a patient presenting with a kidney infection––it will bring down the fever but leave the underlying pathology untreated.
Second, and importantly, an examination of the efficacy of SUD treatments for emotion outcomes is necessary because individuals entering treatment programs for SUD are typically experiencing high levels of emotional distress (Sinha et al., 2009) and SUD interventions may often be administered as a frontline intervention for these individuals (Aharonovich, Nguyen, & Nunes, 2001; Rosenblum, 2003; Watts et al., 2014). Although approaches for the simultaneous treatment of SUD with specific comorbid disorders have been developed (e.g., Seeking Safety and CTAP for post-traumatic stress disorder; Back, 2015; Najavits, 2002), such approaches may not be available and/or applicable for many patients (McGovern et al., 2009). In addition, although the pairing of psychotherapy and medication or Medication-Assisted Treatments (MAT) have become a more prevalent practice in SUD treatment, some pharmacotherapies (e.g., anxiolytic medications; Lader, 1994) may be contraindicated in people with active SUD (Merlo, Arana, & Stone, 2010). As a result, in many settings, substance use behaviors are often treated before symptoms of emotional distress (Donald, Dower, & Kavanagh, 2005; Torchalla, Nosen, Rostam, & Allen, 2012) and, in some cases, treatment for substance use behaviors may be the only psychological treatment these individuals receive (Volkow, 2011). In sum, since SUD patients experience high levels of emotional distress (Sinha et al., 2009) and SUD interventions are often the primary intervention administered to these individuals (Aharonovich et al., 2001; Rosenblum, 2003; Watts et al., 2014), a systematic evaluation of the efficacy of SUD interventions for dealing with the symptoms of emotional distress is overdue.
Although some previous literature reviews have examined the impact of SUD interventions on emotion outcomes, these reviews have focused exclusively on SUD populations who also meet criteria for a co-occurring depression or anxiety disorder at the time of intake (A. L. Baker, Thornton, Hiles, Hides, & Lubman, 2012; Hides, Samet, & Lubman, 2010; Secades-Villa, González-Roz, García-Pérez, & Becoña, 2017). Further, the only one of these systematic reviews to employ meta-analytic methods—methods which, in contrast to narrative approaches, allow for the precise quantification of pooled effect sizes—focused only on interventions for populations of smokers with depression, and excluded individuals with other substance use disorders and those without a depression diagnosis (Secades-Villa et al., 2017). No review to date has examined the effect of SUD interventions on emotion outcomes among general SUD populations.
Moderators of the Effect of SUD Intervention on Emotional Distress
A number of factors might potentially impact the extent to which SUD interventions mitigate emotional distress. One potentially important factor is the specific type of SUD intervention implemented, as SUD interventions have varied widely in the degree to which they have incorporated change processes intended to specifically target emotional distress (NIDA, 2019). For example, SUD interventions such as cue-exposure therapy (Germeroth et al., 2017; Marissen, Franken, Blanken, van den Brink, & Hendriks, 2007), family therapy (Azrin et al., 2008), motivational enhancement (Kropp, Winhusen, Lewis, Hague, & Somoza, 2010), and contingency management (Petry, Alessi, & Rash, 2013) seek to reduce substance use by focusing on a variety of processes not directly related to emotion, such as cognitive, social, motivational, and incentive/structural processes. Thus, traditional applications of such interventions do not typically include components aimed at directly impacting emotional processes.
In contrast, several other prominent SUD interventions have incorporated modules that aim to reduce emotional distress as a central targeted change mechanism (e.g., Stasiewicz et al., 2013; Witkiewitz & Bowen, 2010). For example, Cognitive-Behavioral Therapy (CBT) was among the first empirically supported SUD interventions to integrate elements intended to reduce negative emotion and/or increase positive emotion, including modules aimed at helping patients identify and evaluate maladaptive cognitions and their impact on emotional states (Herzog et al., 2002; Lovejoy et al., 1995; O’Connor & Stewart, 2010). In addition, the behavioral activation component of CBT is designed to encourage patients to engage in pleasurable activities across a variety of life areas, thus offering patients a means of reducing negative emotion and also enhancing positive emotion independent of substance use (Lejuez, Hopko, LePage, Hopko, & McNeil, 2001). More recently, mindfulness-based interventions have been developed, focusing on facilitating the nonjudgmental acceptance and awareness of present moment experience as opposed to avoidance or suppression of this experience (Hayes, Follette, & Linehan, 2004; Witkiewitz & Bowen, 2010). Within such interventions, patients are encouraged to observe their cravings for substances and accept them non-judgmentally, thus regulating highly valent emotional states pertaining to their urges to use substances (Adams et al., 2014; Brewer et al., 2009; Garland, Gaylord, Boettiger, & Howard, 2010). Finally, affect-regulation interventions include mindfulness components intended to increase awareness and acceptance of internal experience (Stasiewicz et al., 2013). However, unlike mindfulness-based interventions, these interventions incorporate additional modules intended to help patients moderate these emotions, including modules that encourage patients to capitalize on positive events in their everyday lives (Berking et al., 2011; Berking, Meier, & Wupperman, 2010) and help instill skills to adaptively cope with various kinds of emotional distress (e.g., anxiety, depression, anhedonia; Lin et al., 2004; Worden et al., 2017). In the current review, we predicted that SUD interventions incorporating modules aimed at modulating emotion (CBT, mindfulness-based interventions, and affect-regulation interventions) would be significantly more effective than other SUD interventions at reducing emotional distress.
Another factor that might potentially impact the extent to which SUD interventions reduce emotional distress is the specific type of substance used/misused (e.g., alcohol, illicit drugs, nicotine). For example, when compared with individuals seeking treatment for smoking cessation, individuals seeking treatment for misuse of alcohol or illicit substances have been observed to report experiencing more diffuse and sometimes more extreme negative consequences of their substance use at treatment initiation (i.e., legal issues such as driving under the influence, drug-related offenses, family violence and disillusionment, etc.; Schottenfeld, 1989). Therefore, it is possible that individuals presenting with alcohol and illicit substance dependence may begin treatment with more extreme levels of emotional distress, and so might potentially be poised to receive more reduction in emotional distress as a result of intervention. At the same time, however, some researchers have argued that nicotine has particularly potent and targeted effects on negative emotional states when compared with other substances (Brandon, 1994; Kassel, Stroud, & Paronis, 2003). Further, research has indicated longitudinal associations between emotional distress and smoking (Orlando et al., 2001; Patton et al., 1998), and that regular smoking is associated with increased risk of emotional disorders (Mojtabai & Crum, 2013). Thus, the literature does not support firm predictions concerning the role of the type of substance as it relates to emotion outcomes of SUD intervention.
The Current Review
In sum, emotional distress is thought to be a key underlying mechanism driving SUDs, and SUD interventions are often implemented as a frontline psychological intervention for individuals experiencing high levels of negative emotion and/or low levels of positive emotion. Yet we currently have no sense for the efficacy of SUD interventions in reducing emotional distress among general SUD populations. The current meta-analysis is thus the first to examine the broad efficacy of SUD interventions on both negative and positive emotions among individuals with SUD.
The aims of the current review are as follows: (a) to examine whether there exists a significant effect of SUD interventions on emotion outcomes and to estimate the magnitude of this effect; (b) to examine the magnitude of the effect of SUD interventions on emotion outcomes across different sub-categories of emotion (e.g., positive emotion vs. negative emotion; measures of depression vs. stress/anxiety) and across post-treatment (end of treatment) vs. follow-up (N weeks after the end of treatment) stage of intervention; (c) to examine various moderators of the effect of SUD intervention on emotion outcomes, including type of intervention (i.e., CBT, affect-regulation interventions, mindfulness-based interventions) and type of substance targeted in the intervention (i.e., alcohol, nicotine, etc.).
Methods
Search Strategy
The search included studies published prior to January 2019. The following strategies were used to search for relevant studies: (a) The databases PsycINFO and PubMed were searched using the following parameters: (“alcohol” OR “substance” OR “drug” OR “addict*” OR “abus*”) AND (“treatment” OR “intervention” OR “therapy”) AND (“emotion*” OR “affect*” OR “mood” OR “stress” OR “anxi*” OR “depress*”). Methodological limits: “clinical trials.” An asterisk (*) was added next to the words “addict,” “abus,” “emotion,” “affect”, “anxi,” and “depress” to capture all variations in the ending of the words (for instance: addiction, abuse, emotional, affective, anxious, or depressive). In light of the large number of results produced by PubMed1, search terms were required to appear in either the title or abstract for the PubMed search. (b) Once a study was identified as meeting inclusion criteria, all studies that had cited that study since its publication were reviewed for eligibility. Furthermore, the reference list of each eligible study was scanned for other potential candidate studies. A total of 11,754 abstracts were scanned for potential inclusion in this review.
Inclusion Criteria
Characteristics of studies:
The study was required to include at least one behavioral (i.e., non-pharmacological) intervention for SUD and at least one control intervention. All types of SUD interventions and all levels of control interventions were eligible (see “Data Extraction”). The interventions included in this meta-analysis could have targeted any type of substance including—but not necessarily limited to—alcohol, marijuana/cannabis, nicotine/tobacco, stimulants (e.g., cocaine/amphetamine/methamphetamine), and opioids (e.g., heroin, prescription pain killers). Treatment conditions were required to be randomly assigned.
Characteristics of participants:
SUD populations were defined inclusively, encompassing populations meeting specific criteria for SUD set forth by the Diagnostic and Statistical Manual of Mental Disorders (DSM; e.g., American Psychiatric Association, 1994) as well as populations identified as meeting SUD criteria according to alternative tests/criteria delineated by the study authors (e.g., according to Alcohol Use Disorders Identification Test; Saunders, Aasland, Babor, de la Fuente, & Grant, 1993). Both treatment-seeking and non-treatment-seeking2 SUD samples were included. Studies were excluded if they used non-clinical samples (e.g., college student social drinkers). In addition, since the aim of this review was to examine the impact of behavioral interventions on general SUD populations, samples were excluded if all participants in the sample were required to also meet criteria for other psychological disorders (i.e., emotional disorders, schizophrenia, etc.). Note that the effect of interventions among exclusively comorbid SUD populations has been reviewed elsewhere (A. L. Baker et al., 2012; Hides et al., 2010; Secades-Villa et al., 2017). No age restrictions were placed on participants.
Characteristics of outcome:
Studies were required to include at least one outcome targeting emotional states measured at post-treatment (at the end of treatment) and/or follow-up (N weeks after the end of treatment). A range of emotional state types were acceptable, including negative emotion, positive emotion, symptoms of anxiety/stress, and depressive symptoms (see Table 1 for the complete list of measures). Measures were not included if they assessed levels of ‘regulation’ of emotion, e.g. the Distress Tolerance Scale (Simons & Gaher, 2005) and Difficulties in Emotion Regulation (Gratz & Roemer, 2004), as individuals’ emotion regulation skills are usually conceptualized as a stable construct (Gross, 2015) and may not always reflect their emotional state (MacIntyre, Ruscio, Brede, & Waters, 2018); for example, individuals who report similar levels of negative emotion may have different emotion regulation skills (MacIntyre et al., 2018). In addition, measures were not included if they assessed emotion as a ‘trait’ (e.g., Anxiety Sensitivity Index; Reiss, Peterson, Gursky, & McNally, 1986).
Table 1.
Characteristics of RCTs
| Study (Year) | N | Age | Intervention type | Control type | Substancetype | Time point(s)* | Emotion measures** | Time frame*** | Risk of bias**** |
|---|---|---|---|---|---|---|---|---|---|
| Boß et al. (2018) | 434 | 47.47 | Affect-regulation | ST/TAU | Alcohol | PT | Anx/strs (DASS) | Week | Unclear |
| Dep (DASS) | Week | ||||||||
| FU (18w) | Anx/strs (DASS) | Week | |||||||
| Dep (DASS) | Week | ||||||||
| Bornovalova et al. (2012) | 52 | 42.01 | Affect-regulation | Non-specific | Others/all | PT | Dep (CES-D) | Week | Low |
| Carrico et al. (2015) | 21 | 41.1 | Affect-regulation | Non-specific | Others/all | PT | NE (DES) | Day | Unclear |
| PE (DES) | Day | ||||||||
| FU (16w) | NE (DES) | Day | |||||||
| PE (DES) | Day | ||||||||
| Lin et al. (2004) | 14 | 36.6 | Affect-regulation | Specific | Others/all | PT | Anx/strs (STAI) | Moment | Unclear |
| Dep (BDI) | Month | ||||||||
| Anx/strs (STAI) | Moment | ||||||||
| FU (16w) | Dep (BDI) | Month | |||||||
| Stasiewicz et al. (2013) | 77 | 45.7 | Affect-regulation | Non-specific | Alcohol | PT | NE (PANAS) | N/I | Low |
| Worden et al. (2017) | 41 | 38.5 | Affect-regulation | ST/TAU | Others/all | PT | Anx/strs (DASS) | Week | Unclear |
| FU (12w) | Anx/strs (DASS) | Week | |||||||
| Brewer et al. (2009) | 36 | 38.2 | Mindfulness | Active comparator | Others/all | PT | Anx/strs (DES) | Day | High |
| Garland et al. (2010) | 53 | 40.3 | Mindfulness | Non-specific | Alcohol | PT | Anx/strs (PSS) | Month | Unclear |
| Garland et al. (2014) | 115 | 48.34 | Mindfulness | Non-specific | Other/all | PT | NE (SOSI) | Week | Unclear |
| Anx/Strs (SOSI) | Week | ||||||||
| Dep (SOSI) | Week | ||||||||
| Glasner et al. (2017) | 63 | 45.3 | Mindfulness | Non-specific | Others/all | PT | Anx/strs (BAI) | Month | Low |
| Dep (BDI) | Month | ||||||||
| FU (4w) | Anx/strs (BAI) | Month | |||||||
| Dep (BDI) | Month | ||||||||
| Marcus et al. (2009) | 459 | 34.98 | Mindfulness | ST/TAU | Others/all | PT | Anx/strs (SOSI) | Week | High |
| FU (32w) | Anx/strs (SOSI) | Week | |||||||
| Price et al. (2012) | 46 | 39 | Mindfulness | ST/TAU | Others/all | PT | Anx/strs (PSS) | Month | Unclear |
| Dep (BSI) | Week | ||||||||
| NE (PANAS) | N/I | ||||||||
| PE (PANAS) | N/I | ||||||||
| FU (24w) | Anx/strs (PSS) | Month | |||||||
| Dep (BSI) | Week | ||||||||
| NE (PANAS) | N/I | ||||||||
| PE (PANAS) | N/I | ||||||||
| Rogojanski et al. (2011) | 61 | 40.34 | Mindfulness | Specific | Nicotine | FU (1w) | NE (PANAS) | N/I | Low |
| Dep (DASS) | Week | ||||||||
| Ruscio et al. (2015) | 44 | 52.27 | Mindfulness | Specific | Nicotine | PT | NE (PANAS) | N/I | Low |
| PE (PANAS) | N/I | ||||||||
| FU (2w) | NE (PANAS) | N/I | |||||||
| PE (PANAS) | N/I | ||||||||
| Spears et al. (2017) | 257 | 48.7 | Mindfulness | ST/TAU | Nicotine | PT | NE (PANAS) | N/I | Low |
| PE (PANAS) | N/I | ||||||||
| FU (23w) | Dep (CES-D) | ||||||||
| NE (PANAS) | |||||||||
| PE (PANAS) | |||||||||
| Witkiewitz et al. (2011) | 776 | 44 | Mindfulness | Non-specific | Alcohol | PT | NE (POMS) | Moment | Unclear |
| Witkiewitz & Bowen (2010) | 168 | 40.45 | Mindfulness | ST/TAU | Others/all | PT | Dep (BDI) | Month | Low |
| Week | |||||||||
| N/I | |||||||||
| N/I | |||||||||
| Hooten et al. (2014) | 60 | 42.7 | CBT | ST/TAU | Nicotine | PT | Dep (CES-D) | Week | Unclear |
| Lanza et al. (2014) | 32 | 34.35 | CBT | Waitlist | Others/all | PT | NE (ASI) | Month | Unclear |
| FU (24w) | NE (ASI) | Month | |||||||
| Magura et al. (1995) | 62 | 36.68 | CBT | ST/TAU | Others/all | PT | NE (PANAS) | N/I | Unclear |
| NE (POMS) | Moment | ||||||||
| PE (PANAS) | N/I | ||||||||
| Sundström et al. (2016) | 80 | 42.3 | CBT | Non-specific | Alcohol | PT | Anx/strs (HAD) | Week | Unclear |
| Dep (HAD) | Week | ||||||||
| Germeroth et al. (2017) | 87 | 47.51 | Other (Cue-exposure) | Specific | Nicotine | PT | NE (MF) | 3 weeks | Low |
| FU (4w) | NE (MF) | 3 weeks | |||||||
| Horigian et al. (2013) | 480 | 15.4 | Other (Family therapy) | ST/TAU | Others/all | PT | Anx/strs (DISC) | Month | Unclear |
| Dep (DISC) | Month | ||||||||
| Kahler et al. (2011) | 236 | 41.5 | Other (Brief alcohol intervention) | Non-specific | Nicotine | PT | Dep (CES-D) | Week | Unclear |
| FU (24w) | Dep (CES-D) | Week | |||||||
| Kropp et al. (2010) | 200 | 26.08 | Other (Motivational enhancement) | ST/TAU | Others/all | PT | Anx/Strs (own measure) | Week | Unclear |
| Marissen et al. (2007) | 127 | 33.6 | Others (Cue-exposure therapy) | Non-specific | Others/all | PT | NE (POMS) | Moment | Unclear |
| PE (POMS) | Moment | ||||||||
| Dep (POMS) | Moment | ||||||||
| Anx/Strs (POMS) | Moment | ||||||||
| Petry et al. (2013) | 393 | 35.71 | Other (Contingency management) | ST/TAU | Others/all | PT | Anx/strs (BSI) | Week | Unclear |
| Dep (BSI) | Week | ||||||||
| FU (24w) | Anx/strs (BSI) | Week | |||||||
| Dep (BSI) | Week | ||||||||
| Adams et al. (2014) | 399 | 42.44 | Other (Computer-based) | ST/TAU | Nicotine | PT | NE (PANAS) | Week | Unclear |
| PE (PANAS) | Week | ||||||||
| Dep (CES) | Week | ||||||||
| Azrin et al. (2008) | 56 | 15.4 | Other (Family therapy) | Active | Others/all | PT | Dep (BDI) | Month | Unclear |
| comparator | FU (24w) | Dep (BDI) | Month | ||||||
| Polcin et al. (2014) | 217 | 38.4 | Other (Motivational Interviewing) | Specific | Others/all | PT | Anx/strs (ASI) | Month | Unclear |
| Dep (ASI) | Month | ||||||||
| FU (16w) | Anx/strs (ASI) | Month | |||||||
| Dep (ASI) | Month |
Time point(s): information in parentheses refers to the length of time from the end of treatment to the final follow-up assessment; w: week
Emotion measures: ST/TAU: Standard Treatment/Treatment-As-Usual; Specific: Specific factors component control group; Non-specific: Non-specific factors component control group; PT: Post-Treatment; FU: Follow-Up; Anx/Strs: Anxiety/Stress; Dep: Depressive Symptoms; NE: Negative Emotion; PE: Positive Emotion; ASI: Addiction Severity Index––Psychiatric symptoms; BAI: Beck Anxiety Inventory; BDI: Beck Depression Inventory; BSI: Brief Symptom Inventory; CES-D: Center for Epidemiological Studies-Depression; DASS: Depression Anxiety Stress Scale; DES: Differential Emotions Scale; DISC: the Diagnostic Interview Schedule for Children; HAD: Hospital Anxiety and Depression; PANAS: Positive Affect and Negative Affect Schedule; POMS: Profile Of Mood States; PSS: Perceived Stress Scale; SOSI: Symptoms of Stress Inventory; STAI: the State-Trait Anxiety Inventory; SSTAEI: State-Trait Anger Expression Inventory; N/I: not indicated.
Time frame: time frame refers to the specific amount of time indicated by emotion measures employed in each study for the reporting of emotions (e.g., “I have felt sad over the past month” vs. “I have felt sad over the past week”).
Risk of bias: RCTs were rated as having the following overall risk of bias using Cochrane Risk of Bias assessment tool: (a) low risk of bias if all domains were assessed as having low risk of bias; (b) unclear risk of bias if all domains were assessed as low or unclear risk of bias; and (c) high risk of bias if 1 or more domains were assessed as high risk of bias.
Data Extraction
Study characteristics and effect sizes were coded by the first author and the third author. The following characteristics of studies were coded: (a) sample size; (b) average age of participants at study initiation; (c) gender composition of participants; (d) type of substance (alcohol, nicotine/tobacco, other); (e) experimental intervention type; (f) control intervention type; (g) treatment duration; and (h) emotion outcome measures assessed.
Experimental interventions were divided into four groups: (a) affect-regulation interventions; (b) mindfulness-based interventions; (c) CBT-based interventions; and (d) other interventions (interventions which do not involve a specific component targeting emotion). Where researchers examined more than one intervention within the context of a single study, the intervention judged to most directly targeted emotion was selected for inclusion. In addition, control interventions were divided into five groups (Mohr et al., 2014, 2009): (a) Treatment-As-Usual (TAU)/standard treatment; (b) waitlist; (c) non-specific factors component control; (d) specific factors component control; and (e) active comparators. TAUs were conducted in a clinic where patients had access to some form of baseline treatment; in other words, patients in the experimental intervention condition would receive an additional treatment in addition to TAU. Standard treatments were delivered in a research setting, and participants received a treatment comparable to TAU. Waitlist conditions did not provide any treatment but offered delayed access to the experimental treatment. Non-specific factors component control treatment provided a therapy equivalent to the experimental treatment but only provided non-specific factors of the experimental treatment. Specific factors component control treatment provided a therapy equivalent to the experimental condition, but a different or lower intensity of specific factors in addition to the non-specific factors provided in the experimental condition. Finally, active comparator treatments were alternative evidence-based treatments that would not be expected to differ from the experimental treatment in terms of their impact on SUD outcomes. See Mohr et al. (2009; 2014) for more details of control group categorizations used here. Emotion outcome measures were subdivided into “Positive Emotion” and “Negative Emotion” outcomes, and “Anxiety/Stress” and “Depressive Symptoms” outcomes were categorized as subtypes of Negative Emotion outcomes (see Table 1 for a complete list of measures). Lastly, if researchers employed more than one control group within a single study, the most stringent level of control was selected for analysis (e.g., if a study used both waitlist and active comparator, then the active comparator was chosen).
Effect sizes were coded as Hedges’ g coefficients by both the first author and the third author. All effect sizes were coded such that higher effect sizes indicate higher levels of positive emotion and lower levels of negative emotion in treatment vs. control conditions. If a report did not include sufficient information for the calculation of intervention effect sizes for at least one emotion outcome, authors were contacted directly. Of 19 authors contacted, 63% responded with the requested data (4 reports were excluded for author non-response, Davis et al., 2015; Decker, Morie, Hunkele, Babuscio, & Carroll, 2016; Holzhauer & Gamble, 2017; Minami, Bloom, Reed, Hayes, & Brown, 2015; 3 reports were excluded because the authors responded but no longer had access to the data; Johnson, Farris, Schmidt, & Zvolensky, 2012; Luthar, Suchman, & Altomare, 2007; Seidman et al., 2010).
The study codes and effect size codes of the two coders were compared, and any differences were resolved through discussion. The average intraclass correlation (ICC) between the coders was 1.00 for variables coded on a continuous scale (i.e., sample size, age, gender composition, and treatment duration) —the two coders had perfect agreement on the continuous variables. Cohen’s kappa was used to score agreement for the categorical variables (i.e., type of substance, treatment type, control group type, and type of emotion outcomes measured), and interrater agreement for these variables was also high, κ=0.97.
Study Quality Assessment
We assessed the quality of eligible studies by using the criteria described in the “Risk of Bias Assessment Tool” developed by the Cochrane Collaboration (Higgins et al., 2011). These assessments did not impact study inclusion. Each eligible study was examined by two research assistants for the following domains: “random sequence generation,” “allocation concealment,” “blinding on outcome assessment,” “incomplete outcome data,” and “selective outcome reporting” (see Higgins et al., 2011 for details of the assessment). “Blinding of participants and personnel” was not included in the current risk of bias assessment because concealment of treatment group is not applicable in behavioral treatments (Munder & Barth, 2018). For each domain, the risk of bias was scored as low, unclear, or high based on the criteria specified in the assessment tool. Studies were rated as having the following overall risk of bias (see Table 1): (a) low risk of bias if all domains were assessed as having low risk of bias; (b) unclear risk of bias if all domains were assessed as low or unclear risk of bias; and (c) high risk of bias if one or more domains were assessed as high risk of bias. For the five domains of bias, interrater agreement ranged from κ = 0.25 to 0.67. The overall interrater agreement was κ = 0.51, which is comparable to agreement achieved in past studies (Bilandzic, Fitzpatrick, Rosella, & Henry, 2016; Couto, Pike, Torkilseng, & Klemp, 2015). Discrepancies were resolved through discussion until consensus was reached.
Data Analytic Plan
Analyses were completed in Comprehensive Meta-Analysis 2.0 software (CMA 2.0; Borenstein et al., 2005). As the studies included in the current review were not functionally identical, all models were conducted using a random-effects model rather than a fixed-effects model (Hedges & Vevea, 1998; Moses, Mosteller, & Buehler, 2002). We present results in stages (or sections) as defined by time point, first presenting results of models that aggregate effects across post-treatment and follow-up time points included in studies reviewed, and then subdividing effects and presenting them separately for post-treatment and follow-up time points. Within each of these sections, results are first presented for aggregate emotional outcomes, followed by results that subdivide effects into Negative Emotion and Positive Emotion outcomes as well as sub-types within the Negative Emotion category (Anxiety/Stress and Depressive Symptoms). When studies reported multiple follow-up points, the last follow-up time point was used to calculate effect sizes. Moreover, if the study assessed multiple measures of the same outcome construct, we applied CMA formulas for calculating a mean value of the selected outcomes.3 Effect sizes were interpreted based on guidelines proposed by Cohen (1988), with 0.20 interpreted as indicating a “small” effect size, 0.50 indicating “medium,” and 0.80 and above indicating a “large” effect size. A 95-percent confidence interval (CI) was calculated for each study’s effect size measure (Lipsey & Wilson, 2001). To assess and quantify heterogeneity, the I2 statistic (Cochran, 1954), as well as the p-value associated with the Q-test, are reported for each pooled effect reported below. The Q-statistic and its associated p-value are common metrics but may be poor detectors of true heterogeneity in some cases, with statisticians noting that non-significant Q-statistics can sometimes emerge even in cases where underlying heterogeneity exists (Borenstein et al., 2005; Higgins et al., 2003). In contrast, the I2 metric is independent of the number of samples under examination and so is often a useful supplemental measure (Higgins et al., 2003). I2 values of 25% are interpreted as low heterogeneity, 50% as representing moderate heterogeneity, and 75% as representing high heterogeneity between studies (Higgins et al., 2003).
Finally, we employed random effects meta-regression models to identify sources of any variation in effect sizes, with effects aggregated across post-treatment and follow-up time points as well as all emotion outcomes included in reviewed studies (see above). Within meta-regression models, we examined treatment type, substance type, control group type, level of risk of bias, and length of treatment as moderators of the effect of SUD interventions on emotion outcomes. These variables were selected as factors for which there was either conceptual/theoretical (i.e., treatment type, substance type) or methodological (i.e., control group type, level of risk of bias, length of treatment) grounds to predict a moderating effect on emotion outcomes. With respect to these moderator analyses, we explore the robustness of results across various model structures, first entering moderators into univariate meta-regression models to examine bivariate relationships, and then entering all moderators into a single multivariate model in order to examine whether covariation among moderators might account for bivariate effects. The Q-statistic was used to test the overall significance of moderating effects for each categorical variable. The R2 analog was used to report the explained magnitude of between-study variance.
Results
Eligible Studies
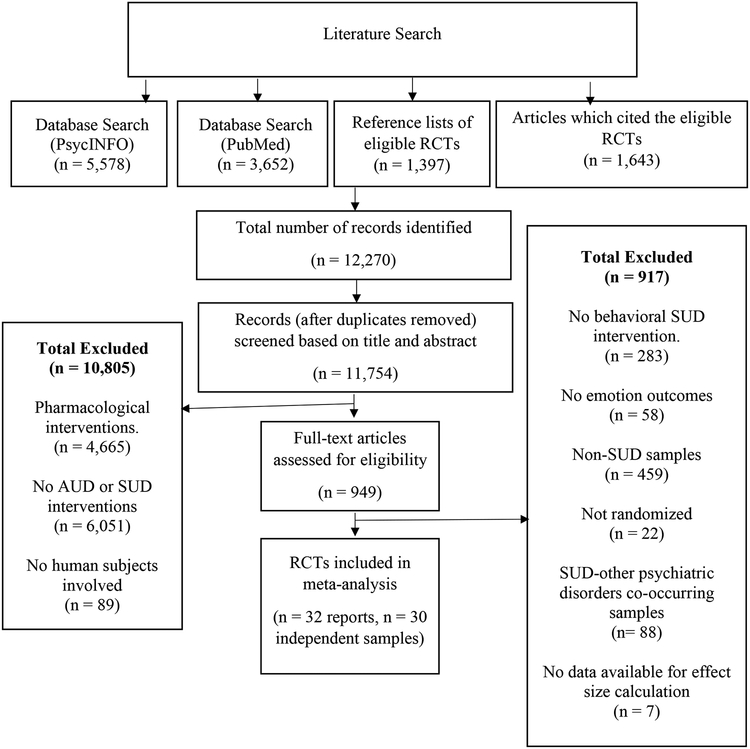
Of 11,754 papers reviewed, 10,805 were excluded based on the titles and abstracts. Full-text articles of 949 papers were further assessed for eligibility. Among the 949 papers, 283 were excluded because the interventions in the studies did not employ a behavioral SUD treatment (i.e., the study used a pharmacological intervention, acupuncture therapy, etc.). Fifty-eight studies were excluded for not reporting any emotion outcomes at post-treatment or follow-up time points. Four hundred and fifty-nine studies were excluded because the participants who engaged in the studies were non-SUD samples (i.e., healthy college student social drinkers, patients with other psychiatric disorders). Twenty-two studies were excluded because treatment groups were not randomly assigned (e.g., no comparison groups, matched-group design); 88 studies were excluded for recruiting exclusively comorbid samples; finally, 7 studies were excluded because we were not able to acquire information required for effect size calculation. As a result, a total of 32 reports, derived from 30 independent samples4, were included in the current analyses. The study selection process is illustrated in Figure 1 using the PRISMA flow diagram (Moher, Liberati, Tetzlaff, Altman, & The PRISMA Group, 2009).
Figure 1.
PRISMA flow diagram illustrating the process of identifying eligible RCTs
Descriptive Statistics
In total, 138 effect sizes calculated based on data from 5,146 individuals enrolled in 30 independent randomized controlled trials (RCTs) were included in this review. On average, samples were 48.03% female with an average age of 38.39 at treatment initiation. RCTs included in the current review compared psychological interventions for addiction with TAU/standard treatment (k=12), waitlist (k=1), active comparator (k=2), non-specific factors component control (k=10), and specific factors component control (k=5). Eleven RCTs examined mindfulness-based interventions, 6 examined affect-regulation interventions, 4 examined CBT-based interventions, and 9 examined “other” interventions. All 30 RCTs reported a measure of Negative Emotion, and 7 also reported a measure of Positive Emotion. Twenty-nine RCTs reported emotion outcomes at post-treatment, and 16 reported emotion outcomes at follow-up time points. Altogether, all 30 RCTs reported at least one emotion measure at post-treatment or follow-up (see inclusions). See Table 1 for a full report of RCT characteristics.
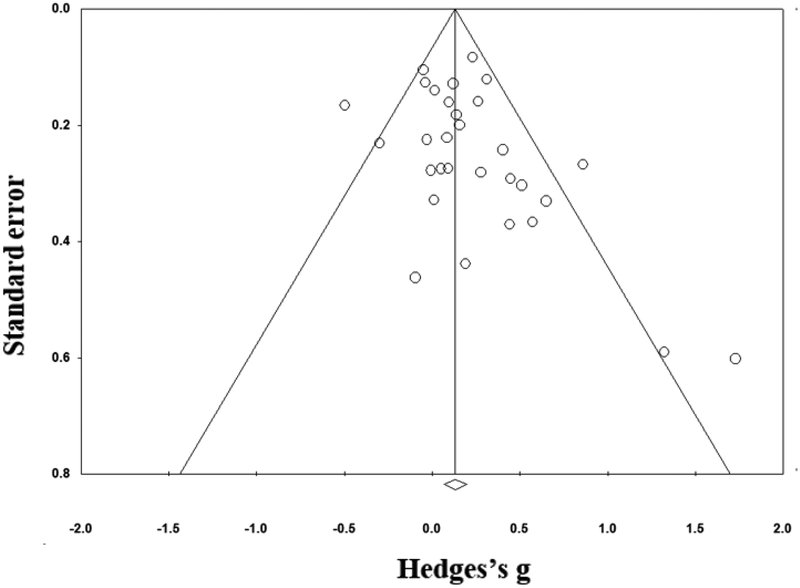
Publication Bias
We used two strategies to assess for publication bias. First, Rosenthal’s fail-safe N was calculated to determine whether publication bias might have influenced the size of the effect of addiction treatments on emotion outcomes (Rosenthal, 1979). Results indicated that 184 unpublished null results would be required to offset the significant finding, a figure that exceeds Rosenthal’s criteria of 5*k + 10 (5*30+10=160). Second, we visually inspected funnel plots of the data. Funnel plots depict the effect size for each sample against its standard error. When there is no publication bias, funnel plots approximate the shape of a funnel, with larger samples clustered around the average effect size at the top of the graph and smaller samples being more spread out along the bottom of the graph. When publication bias is present, the bottom of the plot appears asymmetrical (Sutton, 2009). Visual inspection of the funnel plot indicated that effects were reasonably evenly distributed around the mean (Figure 2). Taken as a whole, these tests indicate that publication bias was unlikely to have had a major influence on results.
Figure 2.
Funnel Plot of Standard Error by Hedges’s g
Main Effect of SUD Interventions on Substance Use Outcomes
Note that the effect of SUD interventions on substance use behaviors has been reviewed and quantified exhaustively elsewhere (e.g., Gierisch et al., 2012; Secades-Villa et al., 2017) and was not the main aim of the current review. However, given potential connections between emotion and substance use, we did want to examine the overall effect of SUD interventions on substance use outcomes in the specific sample of RCTs reviewed here. Substance use outcomes measured in our sample of RCTs included standard self-report measures of abstinence, frequency, and quantity of alcohol and drug use. Twenty out of thirty RCTs reported substance use outcomes at post-treatment or follow-up time points. As might be expected, there was a significant effect of SUD interventions on substance use outcomes measured at all time points (post-treatment and follow-up time points examined together), indicating that SUD interventions do tend to broadly decrease the frequency and quantity of substance use and increase levels of abstinence in our sample of RCTs, d=0.166, 95% CI=0.038 to 0.295 (I2=45.70, p=0.01; k=20).5
Main Effect of SUD Interventions on Emotion Outcomes
All time points.
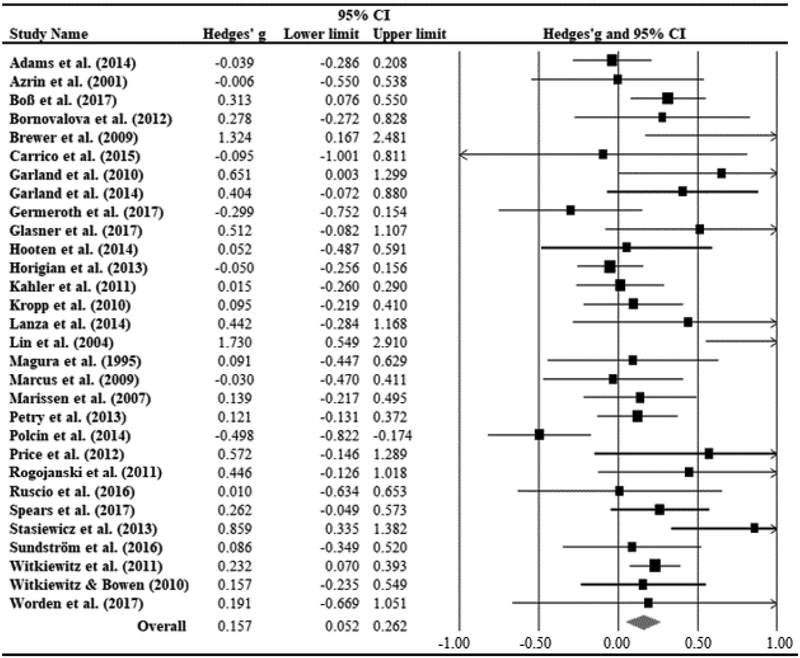
We first examined the main effect of SUD intervention on emotion outcomes measured at all time points (post-treatment and follow-up time points examined together). The purpose of these analyses was to look at the broad (“omnibus”) efficacy of SUD intervention at all time points after the completion of treatment. There was a small but significant effect of SUD intervention on emotion outcomes, d=0.157, 95% CI=0.052 to 0.262 (I2=48.82, p<0.01; k=30; see Figure 3).6 In order to further parse this finding, we next subdivided emotion outcomes into Positive Emotion and Negative Emotion outcomes. The effect size for Negative Emotion was nominally bigger, indicating a small but significant effect of SUD interventions in reducing negative emotions, d=0.162, 95% CI=0.056 to 0.269 (I2=49.97, p<0.01; k=30). In contrast, the effect for Positive Emotion was smaller and did not reach statistical significance, d=0.062, 95% CI= −0.089 to 0.213 (I2=0.00, p=0.82; k=7). Although the effects for Positive Emotion were smaller, it is important to note that the sample size for Positive Emotion was relatively limited, so these results should be considered preliminary. Next, to get a sense for different Negative Emotion subcategories, we conducted analyses examining “Anxiety/Stress” and “Depressive Symptoms” outcomes. The effect size for Anxiety/Stress emerged as significant, d=0.353, 95% CI=0.131 to 0.574 (I2=77.04, p<0.01; k=15), whereas the effect size for Depressive Symptoms was smaller and non-significant, d=0.122, 95% CI= −0.153 to 0.397, (I2=90.06, p<0.01; k=18).
Figure 3.
Forest Plot of the Effect Sizes of SUD Interventions on Emotion Outcomesª ª Hedge’s g with 95% confidence intervals (bars). The diamond is the average of the effect sizes.
Post-treatment.
We next conducted analyses separating post-treatment from follow-up time points. There was a significant main effect of SUD intervention on overall emotion outcomes at post-treatment that was small in magnitude, d= 0.158, 95% CI=0.032 to 0.283 (I2=66.06, p<0.01; k=29). The effect size for Negative Emotion was statistically significant, d=0.161, 95% CI=0.034 to 0.287 (I2=66.63, p<0.01; k=29), whereas the effect for Positive Emotion again did not reach statistical significance, d=0.082, 95% CI= −0.069 to 0.232 (I2=0.00, p=0.81; k=7). The effect of SUD intervention on Anxiety/Stress outcomes emerged as significant, d=0.275, 95% CI=0.097 to 0.453 (I2=68.04, p<0.01; k=15), whereas the effect for Depressive Symptoms was not significant and smaller in magnitude, d=0.031, 95% CI= −0.317 to 0.379 (I2=93.33, p<0.01; k=16).
Follow-up.
In analyses looking at effects of SUD intervention at follow-up, we still found a significant overall effect of SUD intervention on emotion outcomes, d=0.149, 95% CI=0.011 to 0.310 (I2=46.30, p=0.02; k=16). The effect for Negative Emotion was significant, d=0.155, 95% CI=0.007 to 0.318 (I2=47.84, p=0.02; k=16), whereas the effect for Positive Emotion was again non-significant, d=0.131, 95% CI= −0.230 to 0.491 (I2=32.39, p=0.22; k=4). When different types of Negative Emotion were subdivided, we found a significant effect of SUD interventions on Anxiety/Stress that was moderate in magnitude, d=0.617, 95% CI=0.193 to 1.042 (I2=85.68, p<0.01; k=8), whereas the effect was again not significant for Depressive Symptoms, d=0.251, 95% CI= −0.192 to 0.695 (I2=92.35, p<0.01; k=10).
In sum, analyses including measures taken at both post-treatment and follow-up revealed a small but significant effect of SUD treatment on reducing Negative Emotion, with this effect emerging as non-significant for Positive Emotion. In addition, the effect was especially strong for Anxiety/Stress outcomes. Models parsing these effects by time point indicated effects at post-treatment were retained into the follow-up stage.
Moderators of the Treatment Effects on Emotion Outcomes
Given the significant heterogeneity between RCTs, we first present the results of univariate meta-regression models examining bivariate associations between moderators and treatment effects (see data analytic plan). Results indicated that type of intervention employed significantly moderated effect sizes, Q(3) =18.29, p<0.01 (R2 analog=0.71). Specifically, the average effect size for RCTs employing affect-regulation interventions, d=0.458, 95% CI=0.115 to 0.801 (I2=49.49, p=0.08; k=6), as well as mindfulness-based treatments, d=0.265, 95% CI=0.152 to 0.379 (I2=0.00, p=0.49; k=11), were significantly larger than the effect size for RCTs employing “Other” interventions (see footnote 2), d= −0.037, 95% CI= −0.135 to 0.061 (I2=35.18, p=0.14; k=9). The average effect size for CBT interventions, d=0.127, 95% CI= −0.140 to 0.393 (I2=0.00, p=0.84; k=4), was not significantly larger than “Other” interventions7. No other moderator reached significance. Specifically, neither control intervention type8, Q(4) =4.37, p=0.36 (R2 analog=0.00), type of substance, Q(3)=4.11, p=0.13 (R2 analog=0.13), level of risk of bias, Q(2)=1.22, p=0.54 (R2 analog=0.00), nor treatment duration, b= −0.001, p=0.99 (R2 analog=0.00), significantly moderated the effect size for SUD intervention on emotion outcomes.
We next present the results of multivariate meta-regression models, examining the effects of all moderators (treatment type, type of substance, control group type, level of risk of bias, and length of treatment) entered into a single analysis (see data analytic plan). Results of multivariate meta-regression analyses revealed that intervention type remained a significant moderator of effects, even after controlling for the effects of all other moderators, Q(3) =8.71, p=0.03 (Table 2). The average effect sizes for both affect-regulation interventions, d=0.458, 95% CI=0.115 to 0.801 (I2=49.49, p=0.08; k=6), and mindfulness-based interventions d=0.265, 95% CI=0.152 to 0.379 (I2=0.00, p=0.49; k=11), were significantly larger than “Other” interventions, d= −0.037, 95% CI = −0.135 to 0.061 (I2=35.18, p=0.14; k=9). As in the univariate models, the difference between the average effect sizes for CBT, d=0.127, 95% CI= −0.140 to 0.393 (I2=0.00, p=0.84; k=4), and “Other” interventions did not reach significance. A repetition of these moderator analyses subdividing by emotion outcome categories indicated that these effects were likely driven by Negative Emotion outcomes, with the moderating effect of treatment type emerging as statistically significant even when Negative Emotion outcomes were examined alone, Q(3)=7.73, p=0.04. Further, in these multivariate models, the effects of treatment duration, b=−0.005, p=0.49, control intervention type, Q(4)=7.66, p=0.10, level of risk of bias, Q(2)=0.70, p=0.70, and type of substance, Q(2)=0.31, p=0.86, did not reach significance.
Table 2.
Multivariate Meta-Regression Analysis for the Effects of SUD Interventions on Emotion Outcomes.
| Moderators | Coefficient | p-value | |
|---|---|---|---|
| Intercept | 0.2565 | 0.6206 | |
| Treatment durationa | −0.0050 | 0.4862 | |
| Main Intervention Type | Q=8.71, df=3, p=0.0334* | ||
| Others (k=9) | (reference) | ||
| Affect-regulation (k=6) | 0.5217 | 0.0047** | |
| Mindfulness-based (k=11) | 0.3094 | 0.0340* | |
| CBT (k=4) | 0.0478 | 0.7958 | |
| Control Intervention Type | Q=7.66, df=4, p=0.1049 | ||
| Waitlist (k=1) | (reference) | ||
| Active Comparator (k=2) | −0.1302 | 0.7965 | |
| ST/TAU (k=12) | −0.4153 | 0.3287 | |
| Non-specific component control (k=10) | −0.4522 | 0.3070 | |
| Specific component control (k=5) | −0.7704 | 0.0951 | |
| Substance Type | Q=0.31, df=2, p=0.8572 | ||
| Others/all (k=18) | (reference) | ||
| Alcohol (k=5) | 0.0909 | 0.5949 | |
| Nicotine (k=7) | 0.0289 | 0.8033 | |
| Risk of Bias | Q=0.70, df=2, p=0.7050 | ||
| High (k=2) | (reference) | ||
| Unclear (k=8) | 0.2182 | 0.4407 | |
| Low (k=20) | 0.2232 | 0.4090 |
p < 0.05
p<0.01
The unit of analysis for treatment duration is week.
Proportion of total between-study variance explained by the model: R2 analog=0.67
Discussion
With the emergence of transdiagnostic and transtheoretical approaches to understanding clinical disorders, researchers have increasingly pointed to the importance of evaluating the success of psychological interventions on not only target symptoms but also on underlying mechanisms. Although links between emotional distress and SUD have been firmly established within longitudinal (Marlatt & Witkiewitz, 2005) and also laboratory research (Bresin et al., 2018), the extent to which SUD interventions address emotional distress among general SUD populations has not yet been estimated and quantified. The current meta-analysis, which was the first to synthesize and quantify the evidence supporting the effect of SUD interventions on emotion outcomes, revealed a small but statistically significant effect of SUD interventions in reducing emotional distress. Specifically, results indicated a significant effect of SUD intervention in reducing subjective feelings of negative emotion, an effect that appeared to emerge as especially pronounced with respect to symptoms of anxiety/stress. In contrast, there was no significant effect of SUD interventions on positive emotion, although sample size was a limiting factor with respect to these analyses. These findings were consistent across post-treatment and follow-up stages of interventions. Finally, moderator analyses indicated that specific classes of SUD interventions (i.e., mindfulness-based and affect-regulation interventions) were associated with a significantly greater reduction in emotional distress compared to interventions that did not include explicit modules for targeting emotional distress.
There are several notable implications for the results of this review. First and foremost, results suggest that SUD interventions––which often serve as a frontline treatment for SUD populations with co-occurring symptoms of emotional distress (Donald et al., 2005; Torchalla et al., 2012)––are indeed effective in reducing negative emotion. This finding is, to some extent, surprising because past studies have suggested that, among substance dependent populations, abstinence may often lead to increases in negative emotion, at least in the shorter term (Koob, 2015; Koob & Le Moal, 1997). Given that the primary goal of most SUD interventions is to diminish substance use, these interventions could easily be implicated in increases in negative emotion and decreases in positive emotion, at least in the short term. In this regard, the findings of the current meta-analysis––that SUD interventions do significantly reduce negative emotion—seem to offer some hopeful implications for SUD treatment. It is also notable that the size of the effect of SUD interventions on emotion outcomes is, perhaps unsurprisingly, smaller than effect sizes estimated for many treatments designed to specifically target emotional symptoms (Cohen’s d’s range 0.7 to 0.85; Acarturk et al., 2009; Vøllestad et al., 2012). Moreover, these SUD interventions are not only producing small effects for emotion outcomes but for substance use outcomes as well. Thus, there appears to be room for improvement when it comes to designing behavioral interventions for SUD and ensuring that these treatments are effectively addressing emotional symptoms.
Second, these results indicate that, while SUD interventions are associated with significant reductions in negative emotion, positive emotion does not change substantially during SUD treatment. This may be because many SUD interventions focus explicitly on negative emotion (e.g., Bornovalova et al., 2012; Brewer et al., 2009; Witkiewitz & Bowen, 2010), or because the number of studies on SUD and positive emotion (k=7) was smaller than the number assessing negative emotion (k=30). Further research is needed to better understand whether psychosocial SUD interventions influence positive emotions.
Third, the effect sizes for anxiety/stress emerged as significant, whereas the effect sizes for depressive symptoms were smaller and non-significant, at both post-treatment and follow-up stages of intervention. This finding may reflect the fact that the interventions included in the current meta-analysis had specific treatment components pertaining to symptoms of anxiety and stress (e.g., distress tolerance skills in Stasiewicz et al., 2013 and Bornovalova et al., 2012; anxiety sensitivity protocol in Worden et al., 2017) rather than depression. In addition, craving for substance use has long been associated with symptoms of anxiety and stress in the addiction literature (Sinha, 2001), thus it is perhaps not surprising that many existing treatment components for SUD interventions focus on anxiety/stress regulation. Nonetheless, further research is needed to better understand the differences in the effects of SUD interventions on anxiety/stress and depressive symptoms.
Fourth, the results of this review did indicate that RCTs employing certain types of interventions (i.e., mindfulness-based and affect-regulation interventions) produced significantly larger reductions in emotional distress compared with RCTs employing other types of interventions (i.e., contingency management, family therapy, etc.). This finding may reflect the fact that affect-regulation and mindfulness-based interventions include components designed specifically to help patients modulate emotion (e.g., acceptance and tolerance with affect-regulation interventions, non-judgmental acceptance with mindfulness-based interventions). In addition, it is worth noting that the effect sizes for CBT-based interventions were nominally––but not significantly––bigger than those of “other” interventions. These findings are perhaps not surprising, given that affect-regulation and mindfulness-based treatments are built upon the foundation of CBT and likely include the CBT components targeting emotion (e.g., cognitive restructuring, analyzing/modifying emotion; Berking & Whitley, 2014a; Jimenez et al., 2010) as well as additional components, beyond those included in CBT, aimed at helping patients regulate emotions (Berking & Whitley, 2014b; Jimenez et al., 2010). It is worth noting, however, that our sample included a relatively small number of RCTs implementing CBT-based interventions, and so further research is needed to replicate these findings. Nonetheless, by indicating specific types of SUD interventions that may be more effective than others at reducing emotional distress, results of the current review might have implications for clinical practice. For example, in cases where symptoms of emotional distress are of particular concern in a SUD patient, clinicians might consider selecting a mindfulness-based or affect-regulation intervention. Future research might also look to transdiagnostic theory to identify other SUD treatment approaches likely to be effective at reducing emotional distress. For example, approaches such as the Unified Protocol for Transdiagnostic Treatment of Emotional Disorders (UP; Farchione et al., 2012) have been found to be particularly useful in reducing emotional distress among patients with not only co-occurring emotional disorders (Wilamowska et al., 2010) but also other disorders such as borderline personality disorder (Sauer-Zavala, Bentley, & Wilner, 2016). Given that feelings of anxiety and depression are potent predictors of relapse among substance users (Shiffman & Waters, 2004; Witkiewitz & Villarroel, 2009), future treatment-based research may consider implementing such treatments in SUD populations.
Limitations and directions for future work should be noted. First, we were able to examine the effect of moderators (e.g., treatment type, control group type) only at the between-study level, and not within-studies. Such between-study comparisons are necessarily limited, since a variety of factors may vary across studies and thus confound effects (Fairbairn et al., 2018). Future research should further examine the effect of these moderators (e.g., treatment type) within a single sample of participants. Second, although we had excellent power for our main analyses examining the impact of SUD interventions on emotion outcomes, we had lower power for some of our subgroup analyses (e.g., analyses parsing Positive Emotion outcomes at follow-up). These subgroup analyses should be replicated in larger samples of studies. Third, although the current meta-analysis revealed a significant effect of SUD interventions on both substance use outcomes and emotion outcomes, explicit links between emotion outcomes and substance use outcomes were not examined in the current review. The direction of causality among these factors—whether changes in patterns of substance use led to subsequent changes in emotional outcomes, or vice versa—could not be determined on the basis of studies reviewed here. Future research might productively explore more nuanced questions, including the correlation between SUD and emotion outcomes in SUD intervention studies, the strength of emotion as a statistical mediator of SUD outcomes, and temporal precedence in the emotion-substance use link. Importantly, however, such questions are best addressed through individual-level data, and not through between-study comparisons. More empirical research reporting on participant-level correlations between emotion and substance use outcomes within samples, and the strength of emotion as a mediator of substance use outcomes within samples, would be required before a meta-analysis on these questions would be feasible.9
Fourth, it was unexpected that control group type emerged as a non-significant moderator of the impact of SUD intervention on emotion outcomes. One possible explanation is that, although our sample of studies did include a range of control group types, varying from “waitlist” to “active comparator,” some of the more minimal/extreme control group categories (e.g., waitlist) featured very low numbers of samples (k=1). Therefore, our power to detect an effect of control group type may have been limited. Fifth, it is worth noting that time frames for measuring emotion can vary across questionnaires with some assessing emotion experienced in the current moment (e.g., Profile of Mood States; McNair, Lorr, & Droppleman, 1971), while others request information on emotions over a larger time scale (e.g., Perceived Stress Scale; S. Cohen, Kamarck, & Mermelstein, 1983). Future research might explicitly examine the impact of such variability on effect sizes. Sixth, note that it is possible that emotional processes differ across adolescent vs. adult samples (Chassin et al., 2013; D. B. Clark, Kirisci, & Tarter, 1998). Our review, which included only two adolescent samples, had only limited power to examine such effects. In addition, although two samples included in this review featured individuals involved in the criminal justice system (Azrin et al., 2008; Lanza et al., 2014), most of our studies recruited voluntary samples, and so results of this review might generalize best to populations of treatment-seeking adults. These restrictions on generalizability notwithstanding, it is also worth observing that a specific strength of this meta-analysis is the relatively high base rates of female participation in studies reviewed (compared to many studies of SUD populations), indicating unusually strong potential for generalization across genders. Finally, all measures of emotions were based on self-reports, which are capable of measuring consciously accessible emotions only (Mauss & Robinson, 2009). Future research might explore other ways to measure emotions such as behavioral (Sayette et al., 2012) and psychophysiological measures (Kang et al., 2018).
In sum, researchers have increasingly pointed to the importance of evaluating the efficacy of psychological interventions for not only target symptoms but also underlying mechanisms (T. B. Baker et al., 2004). Numerous theories of SUD have posited emotional dysregulation as a core underlying mechanism driving SUD (Cooper et al., 1995; Orlando et al., 2001; Witkiewitz & Villarroel, 2009), and so evaluating the effect of SUD interventions on emotion outcomes may be crucial for establishing the long-term efficacy of such interventions. The results of the current review provide evidence for the efficacy of SUD interventions in reducing emotional distress among SUD patients and indicate several promising directions for future research into emotional processes in SUD treatment.
Public Health Significance Statement:
Individuals seeking treatment for addiction often experience high levels of emotional distress and leaving these emotional symptoms untreated can lead to relapse or to the emergence of other psychological symptoms. Results of this review indicate a small but significant effect of behavioral SUD interventions in reducing negative emotion. No significant effects of SUD interventions emerged for positive emotion, although conclusions regarding positive emotion are preliminary due to limited numbers of samples.
Acknowledgments
This research was supported by National Institutes of Health Grant R01AA025969 to Catharine E. Fairbairn. Thanks to Sara Mei, Zoe Lee, and Eddie Caumiant for their assistance in coding research reports and to Howard Berenbaum and Joseph Cohen for helpful comments on the manuscript.
Footnotes
Without the search field restrictions, the PubMed search yielded 21,089 results.
Participants recruited within Lanza et al. (2014) were incarcerated women in a state prison who met the diagnostic criteria for SUD. In addition, participants recruited within Azrin et al., (2008) were teenagers who were referred to the study by juvenile detention center staff, judges, probation officers, and school administrators.
. Yj refers to the jth effect size from the outcomes to be averaged. Vj refers to the jth variance from the variances to be combined, j = 1, 2, 3, …, m (Borenstein et al., 2005).
Some of the studies identified in our review reported on overlapping RCTs (McHugh, Kaufman, Frost, Fitzmaurice, & Weiss, 2013 and Witkiewitz, Bowen, & Donovan, 2011; Price, Wells, Donovan, & Brooks, 2012; Price, Wells, Donovan, & Rue, 2012), and so the number of independent samples is slightly lower than the number of reports.
Given the significant moderate level of heterogeneity for the treatment effect on substance use outcomes, we examined treatment duration, experimental treatment type, control treatment type, level of risk of bias, and substance type as moderators of the effect sizes at all time points combined. None of the variables significantly moderated the effect of SUD interventions on substance use outcomes.
Some research suggests that emotion-related processes may operate differently among adolescent vs. non-adolescent samples. It is therefore worth noting that results excluding adolescent samples were consistent with those examining all samples together, d=0.178, 95%CI= 0.066 to 0.289, k=28.
As a secondary analysis, intervention type was dichotomized into interventions that include emotional components and those without emotional components. The effect size for interventions that target emotions remained significant, d=0.289, 95%CI= 0.182 to 0.397, and the effect size for interventions without emotional components was significantly smaller in magnitude, d=0.150, 95%CI= 0.068 to 0.231.
Given that “specific factors component control” and “non-specific factors component control” categories have shared characteristics, we also collapsed across the two control group categories. The result of this model was non-significant, Q(3) =0.89, p=0.83. In addition, we dichotomized the control type categories into “waitlist” and “other control treatment”; the result of this model was non-significant, b=0.289, p=0.49.
Among the 30 eligible RCTs included in the current meta-analysis, only two RCTs reported the effects of emotions as a statistical mediator of SUD outcomes (Witkiewitz & Bowen, 2010: B=−0.29, 95% CI= −0.70 to 0.03; Spears et al., 2017: B=−0.25, 95% CI= −0.33 to 0.83). A pooled effect size estimated on the results of these two studies did indicate a significant effect of reduced emotional distress in mediating reductions in substance use, d=−0.278, 95% CI= −0.41 to −0.13.
References
- Acarturk C, Cuijpers P, van Straten A, & de Graaf R (2009). Psychological treatment of social anxiety disorder: a meta-analysis. Psychological Medicine, 39(02), 241 10.1017/S0033291708003590 [DOI] [PubMed] [Google Scholar]
- Adams CE, Chen M, Guo L, Lam CY, Stewart DW, Correa-Fernández V, … Wetter DW (2014). Mindfulness predicts lower affective volatility among African Americans during smoking cessation. Psychology of Addictive Behaviors, 28(2), 580–585. 10.1037/a0036512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aharonovich E, Nguyen HT, & Nunes EV (2001). Anger and depressive states among treatment-seeking drug abusers: Testing the psychopharmacological specificity hypothesis. The American Journal on Addictions, 10(4), 327–334. 10.1111/j.1521-0391.2001.tb00522.x [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (Ed.). (1994). Diagnostic criteria from DSM-IV. Washington, D.C: The Association. [Google Scholar]
- Arendt M, Rosenberg R, Fjordback L, Brandholdt J, Foldager L, Sher L, & Munk-Jørgensen P (2007). Testing the self-medication hypothesis of depression and aggression in cannabis-dependent subjects. Psychological Medicine, 37(7), 935–945. 10.1017/S0033291706009688 [DOI] [PubMed] [Google Scholar]
- Azrin NH, Donohue B, Teichner GA, Crum T, Howell J, & DeCato LA (2008). A controlled evaluation and description of individual-cognitive problem solving and family-behavior therapies in dually-diagnosed conduct-disordered and substance-dependent youth. Journal of Child & Adolescent Substance Abuse, 11(1), 1–43. 10.1300/J029v11n01_01 [DOI] [Google Scholar]
- Back SE (2015). Concurrent treatment of PTSD and substance use disorders using prolonged exposure (COPE): Therapist guide. Oxford; New York: Oxford University Press. [Google Scholar]
- Baker AL, Thornton LK, Hiles S, Hides L, & Lubman DI (2012). Psychological interventions for alcohol misuse among people with co-occurring depression or anxiety disorders: A systematic review. Journal of Affective Disorders, 139(3), 217–229. 10.1016/j.jad.2011.08.004 [DOI] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, & Fiore MC (2004). Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review, 111(1), 33–51. 10.1037/0033-295X.111.1.33 [DOI] [PubMed] [Google Scholar]
- Berking M, Margraf M, Ebert D, Wupperman P, Hofmann SG, & Junghanns K (2011). Deficits in emotion-regulation skills predict alcohol use during and after cognitive–behavioral therapy for alcohol dependence. Journal of Consulting and Clinical Psychology, 79(3), 307–318. 10.1037/a0023421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berking M, Meier C, & Wupperman P (2010). Enhancing emotion-regulation skills in police officers: Results of a pilot controlled study. Behavior Therapy, 41(3), 329–339. 10.1016/j.beth.2009.08.001 [DOI] [PubMed] [Google Scholar]
- Berking M, & Whitley B (2014a). Module eight: Modifying emotions In Berking M & Whitley B, Affect Regulation Training (pp. 185–196). 10.1007/978-1-4939-1022-9_16 [DOI] [Google Scholar]
- Berking M, & Whitley B (2014b). Overview of current treatments that enhance emotion regulation skills In Berking M & Whitley B, Affect Regulation Training (pp. 47–51). 10.1007/978-1-4939-1022-9_5 [DOI] [Google Scholar]
- Bilandzic A, Fitzpatrick T, Rosella L, & Henry D (2016). Risk of bias in systematic reviews of non-randomized studies of adverse cardiovascular effects of thiazolidinediones and cyclooxygenase-2 inhibitors: Application of a new Cochrane Risk of Bias tool. PLOS Medicine, 13(4), e1001987 10.1371/journal.pmed.1001987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins J, & Rothstein H (2005). Comprehensive meta-analysis 2.0. Biostat. [Google Scholar]
- Bornovalova MA, Gratz KL, Daughters SB, Hunt ED, & Lejuez CW (2012). Initial RCT of a distress tolerance treatment for individuals with substance use disorders. Drug and Alcohol Dependence, 122(1–2), 70–76. 10.1016/j.drugalcdep.2011.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boß L, Lehr D, Schaub MP, Paz Castro R, Riper H, Berking M, & Ebert DD (2018). Efficacy of a web-based intervention with and without guidance for employees with risky drinking: Results of a three-arm randomized controlled trial. Addiction, 113(4), 635–646. 10.1111/add.14085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandon TH (1994). Negative affect as motivation to smoke. Current Directions in Psychological Science, 3(2), 33–37. [Google Scholar]
- Bresin K, Mekawi Y, & Verona E (2018). The effect of laboratory manipulations of negative affect on alcohol craving and use: A meta-analysis. Psychology of Addictive Behaviors, 32(6), 617–627. 10.1037/adb0000383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Sinha R, Chen JA, Michalsen RN, Babuscio TA, Nich C, … Rounsaville BJ (2009). Mindfulness training and stress reactivity in substance abuse: Results from a randomized, controlled stage I pilot study. Substance Abuse, 30(4), 306–317. 10.1080/08897070903250241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmody TP (1989). Affect regulation, tobacco addiction, and smoking cessation. Journal of Psychoactive Drugs, 21(3), 331–342. 10.1080/02791072.1989.10472175 [DOI] [PubMed] [Google Scholar]
- Carrico AW, Gómez W, Siever MD, Discepola MV, Dilworth SE, & Moskowitz JT (2015). Pilot randomized controlled trial of an integrative intervention with methamphetamine-using men who have sex with men. Archives of Sexual Behavior, 44(7), 1861–1867. 10.1007/s10508-015-0505-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catanzaro S (1993). Mood regulation expectancies, anxiety sensitivity, and emotional distress. Journal of Abnormal Psychology, 102(2), 327–330. 10.1037/0021-843X.102.2.327 [DOI] [PubMed] [Google Scholar]
- Chaiton MO, Cohen JE, O’Loughlin J, & Rehm J (2009). A systematic review of longitudinal studies on the association between depression and smoking in adolescents. BMC Public Health, 9(1). 10.1186/1471-2458-9-356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassin L, Hussong A, Barrera M, Molina BSG, Trim R, & Ritter J (2013). Adolescent substance use In Lerner RM & Steinberg L (Eds.), Handbook of Adolescent Psychology (pp. 665–696). 10.1002/9780471726746.ch21 [DOI] [Google Scholar]
- Cheetham A, Allen NB, Yücel M, & Lubman DI (2010). The role of affective dysregulation in drug addiction. Clinical Psychology Review, 30(6), 621–634. 10.1016/j.cpr.2010.04.005 [DOI] [PubMed] [Google Scholar]
- Clark DB, Kirisci L, & Tarter RE (1998). Adolescent versus adult onset and the development of substance use disorders in males. Drug and Alcohol Dependence, 49(2), 115–121. 10.1016/S0376-8716(97)00154-3 [DOI] [PubMed] [Google Scholar]
- Clark LA, & Watson D (1991). Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology, 100(3), 316–336. 10.1037/0021-843X.100.3.316 [DOI] [PubMed] [Google Scholar]
- Cochran WG (1954). The combination of estimates from different experiments. Biometrics, 10(1), 101 10.2307/3001666 [DOI] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed). Hillsdale, N.J: L. Erlbaum Associates. [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Cook J, Spring B, McChargue D, & Doran N (2010). Effects of anhedonia on days to relapse among smokers with a history of depression: A brief report. Nicotine & Tobacco Research, 12(9), 978–982. 10.1093/ntr/ntq118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooney NL, Litt MD, Morse PA, Bauer LO, & Gaupp L (1997). Alcohol cue reactivity, negative-mood reactivity, and relapse in treated alcoholic men. Journal of Abnormal Psychology, 106(2), 243–250. 10.1037/0021-843X.106.2.243 [DOI] [PubMed] [Google Scholar]
- Cooper ML (1994). Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment, 6, 117–128. 10.1037/1040-3590.6.2.117 [DOI] [Google Scholar]
- Cooper ML, Frone MR, Russell M, & Mudar P (1995). Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology, 69(5), 990–1005. 10.1037/0022-3514.69.5.990 [DOI] [PubMed] [Google Scholar]
- Couto E, Pike E, Torkilseng E, & Klemp M (2015). Inter-rater reliability of the Risk of Bias Assessment Tool: for Non-Randomized Studies of Interventions (ACROBAT-NRSI). Cochrane Colloquium. [Google Scholar]
- Dahlquist L, Czyzewski D, & Jones C (1996). Parents of children with cancer: A longitudinal study of emotional distress, coping style, and marital adjustment two and twenty months after diagnosis. Journal of Pediatric Psychology, 21(4), 541–554. 10.1093/jpepsy/21.4.541 [DOI] [PubMed] [Google Scholar]
- Davis ML, Powers MB, Handelsman P, Medina JL, Zvolensky M, & Smits JAJ (2015). Behavioral therapies for treatment-seeking cannabis users: A meta-analysis of randomized controlled trials. Evaluation & the Health Professions, 38(1), 94–114. 10.1177/0163278714529970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker SE, Morie K, Hunkele K, Babuscio T, & Carroll KM (2016). Emotion regulation strategies in individuals with cocaine use disorder maintained on methadone: Emotion regulation strategies in cocaine-dependent adults. The American Journal on Addictions, 25(7), 529–532. 10.1111/ajad.12439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denollet J, & De Vries J (2006). Positive and negative affect within the realm of depression, stress and fatigue: The two-factor distress model of the Global Mood Scale (GMS). Journal of Affective Disorders, 91(2–3), 171–180. 10.1016/j.jad.2005.12.044 [DOI] [PubMed] [Google Scholar]
- Dhossche DM, Meloukheia AM, & Chakravorty S (2000). The association of suicide attempts and comorbid depression and substance abuse in psychiatric consultation patients. General Hospital Psychiatry, 22(4), 281–288. 10.1016/S0163-8343(00)00085-2 [DOI] [PubMed] [Google Scholar]
- Donald M, Dower J, & Kavanagh D (2005). Integrated versus non-integrated management and care for clients with co-occurring mental health and substance use disorders: a qualitative systematic review of randomised controlled trials. Social Science & Medicine, 60(6), 1371–1383. 10.1016/j.socscimed.2004.06.052 [DOI] [PubMed] [Google Scholar]
- Drapeau A, Marchand A, & Beaulieu-Prevost D (2012). Epidemiology of psychological distress In LAbate L (Ed.), Mental Illnesses - Understanding, Prediction and Control. 10.5772/30872 [DOI] [Google Scholar]
- Fairbairn CE, Briley DA, Kang D, Fraley RC, Hankin BL, & Ariss T (2018). A meta-analysis of attachment security and substance use. Psychological Bulletin, 144(5), 532–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Thompson-Hollands J, Carl JR, … Barlow DH (2012). Unified protocol for transdiagnostic treatment of emotional disorders: A randomized controlled trial. Behavior Therapy, 43(3), 666–678. 10.1016/j.beth.2012.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Gaylord SA, Boettiger CA, & Howard MO (2010). Mindfulness training modifies cognitive, affective, and physiological mechanisms implicated in alcohol dependence: Results of a randomized controlled pilot trial. Journal of Psychoactive Drugs, 42(2), 177–192. 10.1080/02791072.2010.10400690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Manusov EG, Froeliger B, Kelly A, Williams JM, & Howard MO (2014). Mindfulness-oriented recovery enhancement for chronic pain and prescription opioid misuse: Results from an early-stage randomized controlled trial. Journal of Consulting and Clinical Psychology, 82(3), 448–459. 10.1037/a0035798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Germeroth LJ, Carpenter MJ, Baker NL, Froeliger B, LaRowe SD, & Saladin ME (2017). Effect of a brief memory updating intervention on smoking behavior: A randomized clinical trial. JAMA Psychiatry, 74(3), 214 10.1001/jamapsychiatry.2016.3148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gierisch JM, Bastian LA, Calhoun PS, McDuffie JR, & Williams JW (2012). Smoking cessation interventions for patients with depression: A systematic review and meta-analysis. Journal of General Internal Medicine, 27(3), 351–360. 10.1007/s11606-011-1915-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasner S, Mooney LJ, Ang A, Garneau HC, Hartwell E, Brecht M-L, & Rawson RA (2017). Mindfulness-based relapse prevention for stimulant dependent adults: A pilot randomized clinical trial. Mindfulness, 8(1), 126–135. 10.1007/s12671-016-0586-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment, 30(4), 315–315. 10.1007/s10862-008-9102-4 [DOI] [Google Scholar]
- Gross JJ (2015). Emotion regulation: Current status and future prospects. Psychological Inquiry, 26(1), 1–26. 10.1080/1047840X.2014.940781 [DOI] [Google Scholar]
- Hatzigiakoumis DS, Martinotti G, Giannantonio MD, & Janiri L (2011). Anhedonia and substance dependence: Clinical correlates and treatment options. Frontiers in Psychiatry, 2 10.3389/fpsyt.2011.00010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC, Follette VM, & Linehan M (Eds.). (2004). Mindfulness and acceptance: expanding the cognitive-behavioral tradition. New York: Guilford Press. [Google Scholar]
- Hedges LV, & Vevea JL (1998). Fixed- and random-effects models in meta-analysis. Psychological Methods, 3(4), 486–504. 10.1037/1082-989X.3.4.486 [DOI] [Google Scholar]
- Herzog TA, Lazev AB, Irvin JE, Juliano LM, Greenbaum PE, & Brandon TH (2002). Testing for group membership effects during and after treatment: The example of group therapy for smoking cessation. Behavior Therapy, 33(1), 29–43. 10.1016/S0005-7894(02)80004-1 [DOI] [Google Scholar]
- Hides L, Samet S, & Lubman DI (2010). Cognitive behaviour therapy (CBT) for the treatment of co-occurring depression and substance use: Current evidence and directions for future research: CBT for depression and substance misuse. Drug and Alcohol Review, 29(5), 508–517. 10.1111/j.1465-3362.2010.00207.x [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, & Altman DG (2003). Measuring inconsistency in meta-analyses. BMJ (Clinical research ed.), 327(7414), 557–560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, … Cochrane Statistical Methods Group. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ, 343, d5928–d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holzhauer CG, & Gamble SA (2017). Depressive symptoms mediate the relationship between changes in emotion regulation during treatment and abstinence among women with alcohol use disorders. Psychology of Addictive Behaviors, 31(3), 284–294. 10.1037/adb0000274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooten WM, Townsend CO, Hays JT, Ebnet KL, Gauvin TR, Gehin JM, … Warner DO (2014). A cognitive behavioral smoking abstinence intervention for adults with chronic pain: A randomized controlled pilot trial. Addictive Behaviors, 39(3), 593–599. 10.1016/j.addbeh.2013.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horigian VE, Weems CF, Robbins MS, Feaster DJ, Ucha J, Miller M, & Werstlein R (2013). Reductions in anxiety and depression symptoms in youth receiving substance use treatment: Reductions in comorbidity in adolescent substance users. The American Journal on Addictions, 22(4), 329–337. 10.1111/j.1521-0391.2013.12031.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jimenez SS, Niles BL, & Park CL (2010). A mindfulness model of affect regulation and depressive symptoms: Positive emotions, mood regulation expectancies, and self-acceptance as regulatory mechanisms. Personality and Individual Differences, 49(6), 645–650. 10.1016/j.paid.2010.05.041 [DOI] [Google Scholar]
- Johnson KA, Farris SG, Schmidt NB, & Zvolensky MJ (2012). Anxiety sensitivity and cognitive-based smoking processes: Testing the mediating role of emotion dysregulation among treatment-seeking daily smokers. Journal of Addictive Diseases, 31(2), 143–157. 10.1080/10550887.2012.665695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner TE, Catanzaro SJ, & Laurent J (1996). Tripartite structure of positive and negative affect, depression, and anxiety in child and adolescent psychiatric inpatients. Journal of Abnormal Psychology, 105(3), 401–409. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Spillane NS, Busch AM, & Leventhal AM (2011). Time-varying smoking abstinence predicts lower depressive symptoms following smoking cessation treatment. Nicotine & Tobacco Research, 13(2), 146–150. 10.1093/ntr/ntq213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang D, Bresin K, & Fairbairn CE (2018). The impact of alcohol and social context on the startle eyeblink reflex. Alcoholism: Clinical and Experimental Research. 10.1111/acer.13838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassel JD (Ed.). (2010). Substance abuse and emotion. 10.1037/12067-000 [DOI]
- Kassel JD, Stroud LR, & Paronis CA (2003). Smoking, stress, and negative affect: Correlation, causation, and context across stages of smoking. Psychological Bulletin, 129(2), 270–304. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ (1987). The self-medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence In Allen DF (Ed.), The Cocaine Crisis (pp. 65–74). 10.1007/978-1-4613-1837-8_7 [DOI] [PubMed] [Google Scholar]
- Kober H (2014). Emotion regulation in substance use disorders. New York: Guilford: Handbook Of Emotion Regulation. 2nd. [Google Scholar]
- Koob GF (2015). The dark side of emotion: The addiction perspective. European Journal of Pharmacology, 753, 73–87. 10.1016/j.ejphar.2014.11.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF, & Le Moal M (1997). Drug abuse: Hedonic homeostatic dysregulation. Science, 278(5335), 52–58. [DOI] [PubMed] [Google Scholar]
- Kropp F, Winhusen T, Lewis D, Hague D, & Somoza E (2010). Increasing prenatal care and healthy behaviors in pregnant substance users. Journal of Psychoactive Drugs, 42(1), 73–81. 10.1080/02791072.2010.10399787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lader M (1994). Anxiolytic drugs: Dependence, addiction and abuse. European Neuropsychopharmacology: The Journal of the European College of Neuropsychopharmacology, 4(2), 85–91. [DOI] [PubMed] [Google Scholar]
- Lanza PV, García PF, Lamelas FR, & González-Menéndez A (2014). Acceptance and commitment therapy versus cognitive behavioral therapy in the treatment of substance use disorder with incarcerated women: drug abuse treatments to incarcerated women. Journal of Clinical Psychology, 70(7), 644–657. 10.1002/jclp.22060 [DOI] [PubMed] [Google Scholar]
- Lee NK, Greely J, & Oei TPS (1999). The relationship of positive and negative alcohol expectancies to patterns of consumption of alcohol in social drinkers. Addictive Behaviors, 24(3), 359–369. 10.1016/S0306-4603(98)00091-4 [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Hopko DR, LePage JP, Hopko SD, & McNeil DW (2001). A brief behavioral activation treatment for depression. Cognitive and Behavioral Practice, 8(2), 164–175. 10.1016/S1077-7229(01)80022-5 [DOI] [Google Scholar]
- Leventhal H, & Everhart D (1979). Emotion, pain, and physical illness In Izard CE (Ed.), Emotions in Personality and Psychopathology (pp. 261–299). 10.1007/978-1-4613-2892-6_10 [DOI] [Google Scholar]
- Levine MD, Marcus MD, Kalarchian MA, Houck PR, & Cheng Y (2010). Weight concerns, mood, and postpartum smoking relapse. American Journal of Preventive Medicine, 39(4), 345–351. 10.1016/j.amepre.2010.05.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin W-F, Mack D, Enright RD, Krahn D, & Baskin TW (2004). Effects of forgiveness therapy on anger, mood, and vulnerability to substance use among inpatient substance-dependent clients. Journal of Consulting and Clinical Psychology, 72(6), 1114–1121. 10.1037/0022-006X.72.6.1114 [DOI] [PubMed] [Google Scholar]
- Lipsey MW, & Wilson DB (2001). Practical meta-analysis. Thousand Oaks, Calif: Sage Publications. [Google Scholar]
- Lovejoy M, Rosenblum A, Magura S, Foote J, Handelsman L, & Stimmel B (1995). Patients’ perspective on the process of change in substance abuse treatment. Journal of Substance Abuse Treatment, 12(4), 269–282. 10.1016/0740-5472(95)00027-3 [DOI] [PubMed] [Google Scholar]
- Lowman C, Allen J, Stout RL, & THE RELAPSE RESEARCH GROUP. (1996). Replication and extension of Marlatt’s taxonomy of relapse precipitants: Overview of procedures and results. Addiction, 91(s12), S51–S71. 10.1111/j.1360-0443.1996.tb02327.x [DOI] [PubMed] [Google Scholar]
- Luthar SS, Suchman NE, & Altomare M (2007). Relational psychotherapy mothers’ group: A randomized clinical trial for substance abusing mothers. Development and Psychopathology, 19(01). 10.1017/S0954579407070137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacIntyre JM, Ruscio AC, Brede E, & Waters AJ (2018). Emotion dysregulation and negative affect: Laboratory and EMA investigations in smokers. Addictive Behaviors Reports, 7, 65–70. 10.1016/j.abrep.2018.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magura S, Rosenblum A, Lovejoy M, Handelsman L, Foote J, & Stimmel B (1995). Neurobehavioral treatment for cocaine-using methadone patients: A preliminary report. Journal of Addictive Diseases, 13(4), 143–160. 10.1300/J069v13n04_03 [DOI] [PubMed] [Google Scholar]
- Marcus MT, Schmitz J, Moeller G, Liehr P, Cron SG, Swank P, … Granmayeh LK (2009). Mindfulness-based stress reduction in therapeutic community treatment: A stage 1 trial. The American Journal of Drug and Alcohol Abuse, 35(2), 103–108. 10.1080/00952990902823079 [DOI] [PubMed] [Google Scholar]
- Marissen MAE, Franken IHA, Blanken P, van den Brink W, & Hendriks VM (2007). Cue exposure therapy for the treatment of opiate addiction: Results of a randomized controlled clinical trial. Psychotherapy and Psychosomatics, 76(2), 97–105. 10.1159/000097968 [DOI] [PubMed] [Google Scholar]
- Marlatt GA, & Donovan DM (Eds.). (2008). Relapse prevention: maintenance strategies in the treatment of addictive behaviors (2nd ed). New York London: Guilford. [Google Scholar]
- Marlatt GA, & Witkiewitz K (2005). Relapse prevention for alcohol and drug problems Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. 2nd ed (pp. 1–44.). NY US: Guilford Press. [Google Scholar]
- Martínez-Sánchez F, Ato-García M, & Ortiz-Soria B (2003). Alexithymia—state or trait? The Spanish Journal of Psychology, 6(01), 51–59. 10.1017/S1138741600005205 [DOI] [PubMed] [Google Scholar]
- Mason BJ, Light JM, Escher T, & Drobes DJ (2008). Effect of positive and negative affective stimuli and beverage cues on measures of craving in non treatment-seeking alcoholics. Psychopharmacology, 200(1), 141–150. 10.1007/s00213-008-1192-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauss IB, & Robinson MD (2009). Measures of emotion: A review. Cognition & Emotion, 23(2), 209–237. 10.1080/02699930802204677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGovern MP, Lambert-Harris C, Acquilano S, Xie H, Alterman AI, & Weiss RD (2009). A cognitive behavioral therapy for co-occurring substance use and posttraumatic stress disorders. Addictive Behaviors, 34(10), 892–897. 10.1016/j.addbeh.2009.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, Kaufman JS, Frost KH, Fitzmaurice GM, & Weiss RD (2013). Positive affect and stress reactivity in alcohol-dependent outpatients. Journal of Studies on Alcohol and Drugs, 74(1), 152–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNair DM, Lorr M, & Droppleman LF (1971). Manual for the profile of mood states (POMS). San Diego: Educational and Industrial Testing Service. [Google Scholar]
- Merlo LJ, Arana J, & Stone AM (2010). Pharmacological trials for the treatment of substance use disorders In Hertzman M & Adler L (Eds.), Clinical Trials in Psychopharmacology (pp. 207–232). 10.1002/9780470749180.ch11 [DOI] [Google Scholar]
- Minami H, Bloom EL, Reed KMP, Hayes SC, & Brown RA (2015). The moderating role of experiential avoidance in the relationships between internal distress and smoking behavior during a quit attempt. Psychology of Addictive Behaviors, 29(2), 400–407. 10.1037/adb0000030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, & The PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr DC, Ho J, Hart TL, Baron KG, Berendsen M, Beckner V, … Duffecy J (2014). Control condition design and implementation features in controlled trials: A meta-analysis of trials evaluating psychotherapy for depression. Translational Behavioral Medicine, 4(4), 407–423. 10.1007/s13142-014-0262-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr DC, Spring B, Freedland KE, Beckner V, Arean P, Hollon SD, … Kaplan R (2009). The selection and design of control conditions for randomized controlled trials of psychological interventions. Psychotherapy and Psychosomatics, 78(5), 275–284. 10.1159/000228248 [DOI] [PubMed] [Google Scholar]
- Mojtabai R, & Crum RM (2013). Cigarette smoking and onset of mood and anxiety disorders. American Journal of Public Health, 103(9), 1656–1665. 10.2105/AJPH.2012.300911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moses LE, Mosteller F, & Buehler JH (2002). Comparing results of large clinical trials to those of meta-analyses. Statistics in Medicine, 21(6), 793–800. 10.1002/sim.1098 [DOI] [PubMed] [Google Scholar]
- Munder T, & Barth J (2018). Cochrane’s risk of bias tool in the context of psychotherapy outcome research. Psychotherapy Research, 28(3), 347–355. 10.1080/10503307.2017.1411628 [DOI] [PubMed] [Google Scholar]
- Najavits L (2002). Seeking safety: A treatment manual for PTSD and substance abuse. New York: Guilford Press. [DOI] [PubMed] [Google Scholar]
- NIDA. (2019, January 17). Treatment approaches for drug addiction. Retrieved from https://www.drugabuse.gov/publications/drugfacts/treatment-approaches-drug-addiction
- Nolen-Hoeksema S, & Watkins ER (2011). A heuristic for developing transdiagnostic models of psychopathology: Explaining multifinality and divergent trajectories. Perspectives on Psychological Science, 6(6), 589–609. 10.1177/1745691611419672 [DOI] [PubMed] [Google Scholar]
- O’Connor RM, & Stewart SH (2010). Substance use disorders In McKay D, Abramowitz JS, & Taylor S (Eds.), Cognitive-behavioral therapy for refractory cases: Turning failure into success. (pp. 211–229). 10.1037/12070-010 [DOI] [Google Scholar]
- Orlando M, Ellickson PL, & Jinnett K (2001). The temporal relationship between emotional distress and cigarette smoking during adolescence and young adulthood. Journal of Consulting and Clinical Psychology, 69(6), 959–970. 10.1037//0022-006X.69.6.959 [DOI] [PubMed] [Google Scholar]
- Pacek LR, Martins SS, & Crum RM (2013). The bidirectional relationships between alcohol, cannabis, co-occurring alcohol and cannabis use disorders with major depressive disorder: Results from a national sample. Journal of Affective Disorders, 148(2–3), 188–195. 10.1016/j.jad.2012.11.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton GC, Carlin JB, Coffey C, Wolfe R, Hibbert M, & Bowes G (1998). Depression, anxiety, and smoking initiation: A prospective study over 3 years. American Journal of Public Health, 88(10), 1518–1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, & Rash CJ (2013). Contingency management treatments decrease psychiatric symptoms. Journal of Consulting and Clinical Psychology, 81(5), 926–931. 10.1037/a0032499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polcin DL, Bond J, Korcha R, Nayak MB, Galloway GP, & Evans K (2014). Randomized trial of intensive motivational interviewing for methamphetamine dependence. Journal of Addictive Diseases, 33(3), 253–265. 10.1080/10550887.2014.950029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price CJ, Wells EA, Donovan DM, & Brooks M (2012). Implementation and acceptability of mindful awareness in body-oriented therapy in women’s substance use disorder treatment. The Journal of Alternative and Complementary Medicine, 18(5), 454–462. 10.1089/acm.2011.0126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price CJ, Wells EA, Donovan DM, & Rue T (2012). Mindful awareness in body-oriented therapy as an adjunct to women’s substance use disorder treatment: A pilot feasibility study. Journal of Substance Abuse Treatment, 43(1), 94–107. 10.1016/j.jsat.2011.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, & McNally RJ (1986). Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behaviour Research and Therapy, 24(1), 1–8. 10.1016/0005-7967(86)90143-9 [DOI] [PubMed] [Google Scholar]
- Riper H, Andersson G, Hunter SB, de Wit J, Berking M, & Cuijpers P (2014). Treatment of comorbid alcohol use disorders and depression with cognitive-behavioural therapy and motivational interviewing: a meta-analysis: CBT/MI for comorbid alcohol use disorders and depression. Addiction, 109(3), 394–406. 10.1111/add.12441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson TE, & Berridge KC (1993). The neural basis of drug craving: An incentive-sensitization theory of addiction. Brain Research Reviews, 18(3), 247–291. [DOI] [PubMed] [Google Scholar]
- Rogojanski J, Vettese LC, & Antony MM (2011). Coping with cigarette cravings: Comparison of suppression versus mindfulness-based strategies. Mindfulness, 2(1), 14–26. 10.1007/s12671-010-0038-x [DOI] [Google Scholar]
- Rosenblum A (2003). Prevalence and characteristics of chronic pain among chemically dependent patients in methadone maintenance and residential treatment facilities. JAMA, 289(18), 2370 10.1001/jama.289.18.2370 [DOI] [PubMed] [Google Scholar]
- Rosenthal R (1979). The file drawer problem and tolerance for null results. Psychological Bulletin, 86(3), 638–641. 10.1037/0033-2909.86.3.638 [DOI] [Google Scholar]
- Ruscio AC, Muench C, Brede E, & Waters AJ (2015). Effect of brief mindfulness practice on self-reported affect, craving, and smoking: A pilot randomized controlled trial using ecological momentary assessment. Nicotine & Tobacco Research, ntv074. 10.1093/ntr/ntv074 [DOI] [PubMed] [Google Scholar]
- Sauer-Zavala S, Bentley KH, & Wilner JG (2016). Transdiagnostic treatment of borderline personality disorder and comorbid disorders: A clinical replication series. Journal of Personality Disorders, 30(1), 35–51. 10.1521/pedi_2015_29_179 [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, & Grant M (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption--II. Addiction (Abingdon, England), 88(6), 791–804. [DOI] [PubMed] [Google Scholar]
- Sayette MA, Creswell KG, Dimoff JD, Fairbairn CE, Cohn JF, Heckman BW, … Moreland RL (2012). Alcohol and group formation: A multimodal investigation of the effects of alcohol on emotion and social bonding. Psychological Science, 23(8), 869–878. 10.1177/0956797611435134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schottenfeld RS (1989). Involuntary treatment of substance abuse disorders: Impediments to success. Psychiatry: Interpersonal and Biological Processes, 52(2), 164–176. [DOI] [PubMed] [Google Scholar]
- Secades-Villa R, González-Roz A, García-Pérez Á, & Becoña E (2017). Psychological, pharmacological, and combined smoking cessation interventions for smokers with current depression: A systematic review and meta-analysis. PLOS ONE, 12(12), e0188849 10.1371/journal.pone.0188849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidman DF, Westmaas JL, Goldband S, Rabius V, Katkin ES, Pike KJ, … Sloan RP (2010). Randomized controlled trial of an interactive internet smoking cessation program with long-term follow-up. Annals of Behavioral Medicine, 39(1), 48–60. 10.1007/s12160-010-9167-7 [DOI] [PubMed] [Google Scholar]
- Shiffman S, & Waters AJ (2004). Negative affect and smoking lapses: A prospective analysis. Journal of Consulting and Clinical Psychology, 72(2), 192–201. 10.1037/0022-006X.72.2.192 [DOI] [PubMed] [Google Scholar]
- Simons JS, & Gaher RM (2005). The distress tolerance scale: Development and validation of a self-report measure. Motivation and Emotion, 29(2), 83–102. 10.1007/s11031-005-7955-3 [DOI] [Google Scholar]
- Sinha R (2001). How does stress increase risk of drug abuse and relapse? Psychopharmacology, 158(4), 343–359. 10.1007/s002130100917 [DOI] [PubMed] [Google Scholar]
- Sinha R, Fox HC, Hong KA, Bergquist K, Bhagwagar Z, & Siedlarz KM (2009). Enhanced negative emotion and alcohol craving and altered physiological responses following stress and cue exposure in alcohol dependent individuals. Neuropsychopharmacology, 34(5), 1198–1208. 10.1038/npp.2008.78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spears CA, Hedeker D, Li L, Wu C, Anderson NK, Houchins SC, … Wetter DW (2017). Mechanisms underlying mindfulness-based addiction treatment versus cognitive behavioral therapy and usual care for smoking cessation. Journal of Consulting and Clinical Psychology, 85(11), 1029–1040. 10.1037/ccp0000229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stasiewicz PR, Bradizza CM, Schlauch RC, Coffey SF, Gulliver SB, Gudleski GD, & Bole CW (2013). Affect regulation training (ART) for alcohol use disorders: Development of a novel intervention for negative affect drinkers. Journal of Substance Abuse Treatment, 45(5), 433–443. 10.1016/j.jsat.2013.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stasiewicz PR, & Maisto SA (1993). Two-factor avoidance theory: The role of negative affect in the maintenance of substance use and substance use disorder. Behavior Therapy, 24(3), 337–356. 10.1016/S0005-7894(05)80210-2 [DOI] [Google Scholar]
- Sundström C, Gajecki M, Johansson M, Blankers M, Sinadinovic K, Stenlund-Gens E, & Berman AH (2016). Guided and unguided internet-based treatment for problematic alcohol use – A randomized controlled pilot trial. PLOS ONE, 11(7), e0157817 10.1371/journal.pone.0157817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutton AJ (2009). Publication bias In Cooper H, Hedges LV, & Valentine JC (Eds.), The handbook of research synthesis and meta-analysis (Vol. 2, pp. 435–452). New York, NY: Russell Sage Foundation. [Google Scholar]
- Torchalla I, Nosen L, Rostam H, & Allen P (2012). Integrated treatment programs for individuals with concurrent substance use disorders and trauma experiences: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 42(1), 65–77. 10.1016/j.jsat.2011.09.001 [DOI] [PubMed] [Google Scholar]
- Tschann JM, Flores E, Pasch LA, & Marin BV (2005). Emotional distress, alcohol use, and peer violence among Mexican-American and European-American adolescents. Journal of Adolescent Health, 37(1), 11–18. 10.1016/j.jadohealth.2004.07.009 [DOI] [PubMed] [Google Scholar]
- Volkow ND (2011). Principles of drug addiction treatment: A research-based guide (2nd Ed.). DIANE Publishing. [Google Scholar]
- Vøllestad J, Nielsen MB, & Nielsen GH (2012). Mindfulness- and acceptance-based interventions for anxiety disorders: A systematic review and meta-analysis: Mindfulness- and acceptance-based interventions for anxiety disorders. British Journal of Clinical Psychology, 51(3), 239–260. 10.1111/j.2044-8260.2011.02024.x [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. [DOI] [PubMed] [Google Scholar]
- Watts R, Orr CA, Althoff RR, Artiges E, Banaschewski T, Barker GJ, … Garavan H (2014). Neuropsychosocial profiles of current and future adolescent alcohol misusers. Nature, 512(7513), 185–189. 10.1038/nature13402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilamowska ZA, Thompson-Hollands J, Fairholme CP, Ellard KK, Farchione TJ, & Barlow DH (2010). Conceptual background, development, and preliminary data from the unified protocol for transdiagnostic treatment of emotional disorders. Depression and Anxiety, 27(10), 882–890. 10.1002/da.20735 [DOI] [PubMed] [Google Scholar]
- Wills TA (1996). Handbook of coping: theory, research, applications (Zeidner M, Ed.). New York: Wiley. [Google Scholar]
- Witkiewitz K, & Bowen S (2010). Depression, craving, and substance use following a randomized trial of mindfulness-based relapse prevention. Journal of Consulting and Clinical Psychology, 78(3), 362–374. 10.1037/a0019172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S, & Donovan DM (2011). Moderating effects of a craving intervention on the relation between negative mood and heavy drinking following treatment for alcohol dependence. Journal of Consulting and Clinical Psychology, 79(1), 54–63. 10.1037/a0022282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, & Villarroel NA (2009). Dynamic association between negative affect and alcohol lapses following alcohol treatment. Journal of Consulting and Clinical Psychology, 77(4), 633–644. 10.1037/a0015647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worden BL, Genova M, & Tolin DF (2017). Randomized pilot of an anxiety sensitivity-based intervention for individuals in a substance use day program. Journal of Psychoactive Drugs, 49(4), 333–343. 10.1080/02791072.2017.1329570 [DOI] [PubMed] [Google Scholar]