Abstract
Mobile health (mHealth) interventions have the potential to improve infant and young child feeding (IYCF) practices; however, gaps in the literature remain regarding their design, implementation, and effectiveness. The aims of this study were to design an mHealth voice messaging intervention delivered to mothers and fathers targeting IYCF practices and examine its implementation and impact in households with children 6–23 months in three rural villages in Senegal. We conducted focus groups (n = 6) to inform the intervention development. We then conducted a pilot study (n = 47 households) to examine the impact of the intervention on IYCF practices of children 6–23 months. Voice messages were sent to the children's mothers and fathers over a period of 4 weeks (two messages per week; eight messages in total), and 24‐hr dietary recalls and food frequency questionnaires (FFQs) were conducted before and immediately after the implementation of the mHealth intervention to examine its impact on IYCF practices. Overall, three of the eight behaviours increased and one decreased. There was a significant increase in the number of children that consumed fish (60% vs. 94%; p = .008) as measured by the 24‐hr recall after the completion of the intervention. We also found significantly higher frequency of egg (p = .026), fish (p = .004), and thick porridge (p = .002) consumption in the previous 7 days measured by the FFQ. Our findings suggest that voice messaging IYCF interventions in Senegal have the potential to improve IYCF behaviours among young children in the short term. Future research should entail scaling‐up the intervention and examining its sustainability over the long‐term.
Keywords: behaviour change communication, infant and young child feeding, mHealth
Key messages.
Our formative research informed the design of our voice messaging intervention in two main ways: (a) We included both mothers and fathers as recipients of the intervention given that men were making food purchasing decisions, and (b) we used voice rather than text messages given the low literacy levels in the study communities.
We found improvements in three of the eight behaviours (i.e., fish, thick porridge, and eggs) targeted in the voice messages, which were aligned with changes in mothers' attitudes towards feeding these foods to their children.
There were some implementation challenges related to ensuring that the phone numbers provided by participants were correct and that there was adequate network coverage in some areas, signalling the need to invest time prior to implementing the intervention to verify all phone numbers.
Both mothers and fathers viewed the voice messaging intervention favourably, with nearly all of them (97%) rating it as good or excellent.
1. INTRODUCTION
The use of appropriate, evidence‐based infant and young child feeding (IYCF) practices, including breastfeeding and complementary feeding from 6 to 23 months, is essential for preventing malnutrition (Smith & Haddad, 2000; WHO, 2015). According to global recommendations, infants should be exclusively breastfed for the first 6 months of life. Thereafter, they should receive a combination of continued breastfeeding and complementary feeding of nutrient‐rich and safe complementary foods until the age of two or beyond (WHO, 2015). The peak period for growth faltering and micronutrient deficiencies in low‐ and middle‐income countries (LMICs) is between 6 and 23 months, which coincides with the introduction of complementary feeding (Bhutta et al., 2013; Dewey & Adu‐Afarwuah, 2008; WHO, 2015). Improving complementary feeding has the potential to prevent malnutrition among young children in the first 1,000 days.
Behaviour change communication (BCC) interventions aimed at improving IYCF practices in the first 1,000 days have shown promising results (Graziose, Downs, O'Brien, & Fanzo, 2018; Lee et al., 2016; Naugle & Hornik, 2014). BCC differs from traditional nutrition education by going beyond simply providing the target populations with knowledge about best practices but also provides them with the reasoning for the importance of adopting specific behaviours, as well as targeted actions to operationalize the messaging. It also places a strong emphasis on behaviour change through the cultural lens of the target population. BCC campaigns that promote recommended IYCF practices have shown promise in improving IYCF outcomes in several countries in Asia and Africa (Graziose et al., 2018).
Mobile health (mHealth) messaging interventions have shown potential in changing health behaviours, but much of the evidence has been from developed countries (Gurman, Rubin, & Roess, 2012; Hurt, Walker, Campbell, & Egede, 2016). The majority of mHealth interventions in LMICs have targeted HIV/AIDs and family planning/pregnancy, with inconsistent results (Gurman et al., 2012). Very few mHealth IYCF interventions have been conducted in LMICs to date (Graziose et al., 2018), and those that have been conducted have primarily focused on exclusive breastfeeding (Flax et al., 2014; Jiang et al., 2014; Sellen et al., 2014).
Gaps in the literature remain in terms of the design, implementation, and effectiveness of using mHealth interventions to improve other feeding practices that make up the continuum of IYCF practices, including complementary feeding. Given the low cost of using mobile phone delivery platforms, as well as the widespread cellphone ownership in most LMICs, mHealth interventions have the potential to be scaled up at the population level, removing barriers to access for traditionally hard to reach populations.
In Senegal, 20% of children 6–23 months of age are stunted, 7% are wasted, and 71% are anaemic (ANSD, 2016). Moreover, only 7% of children 6–23 months of age are fed according to global IYCF recommendations (ANSD, 2016). Given the high rates of malnutrition, interventions aimed at improving IYCF practices have the potential to lead to substantial gains in both health and productivity. Although Senegal has a network of community health workers and Bajenu gox (meaning “community grandmothers” in Wolof) who support community maternal and child health initiatives, their reach is often limited (Kristen Devlin & Pandit‐Rajani, 2016). Using mHealth delivery platforms could accelerate the dissemination of knowledge related to recommended IYCF practices and complement the existing activities of community health workers and Bajenu gox. Thus, the aims of this study were to (a) design an mHealth voice messaging intervention aimed at improving IYCF practices and (b) examine its implementation by conducting a pilot study of its impact and implementation in households with children 6–23 months in three rural villages in Senegal.
2. METHODS
2.1. Overview of study
This study includes formative research (i.e., focus groups) to inform the development of a voice messaging intervention as well as a pilot evaluation of its implementation. The study was approved by the Columbia University and Johns Hopkins University institutional review boards. It was also approved by the Comité National D'éthique pour la Recherche en Santé (National Ethics Committee for Health Research) within the Senegalese Ministry of Health.
2.2. Overview of the development and piloting of the mHealth voice messaging intervention
The design and piloting of the voice messaging intervention were conducted in several steps: (1) informal (n = 8) and formal (n = 6) focus groups with men and women, (2) design of the voice messaging content, and (3) a pilot and process evaluation to examine the implementation of the intervention, its impact on IYCF practices, and potential for scale‐up. We describe these steps in additional detail below.
2.3. Formative focus group discussions
Informal information gathering focus groups were conducted in November–December 2014 in order to gain information related to cultural norms and how these relate to food, household dynamics, and preliminary insight into existing IYCF practices in the three study regions in Senegal. This step was important given that it provided insight into the questions that should be asked in the formal focus groups. In June–July 2015, we conducted three formal focus groups with men and three with women (n total = 6) in order to ascertain information about current perceptions surrounding IYCF practices. The topics discussed in the focus groups included food production, food procurement, IYCF practices, seasonal variation, and sources of nutrition information.
2.4. Design of the mHealth voice messages
The findings from the formal focus groups were then used to identify the key behaviours to target in the voice messaging intervention. We used the key messages booklets for IYCF practices from UNICEF (2012) as well as the Senegalese version of the key messages booklet developed by the Cellule de Lutte contre la Malnutrition (CLM, 2015; unit for the fight against malnutrition) to develop the content related to each of the target behaviours in order to ensure that the messages were consistent with both global and local recommendations.
The theory of planned behaviour was used as the theoretical underpinning of the voice messages (Ajzen, 1991). The theory of planned behaviour posits that the intentions to perform behaviours can be predicted based on an individual's beliefs, their attitudes towards the behaviour, subjective norms, and their perceived behavioural control. Behavioural beliefs associate a behaviour with specific outcomes and attributes (Ajzen, 1991). They are the underlying reasons for engaging in a given behaviour (Contento, 2007). The stronger the belief and the more favourable or unfavourable the outcome, the larger the impact of those beliefs on an individual's attitudes (Ajzen, 1991). Attitudes are favourable or unfavourable judgements about a given behaviour and are strongly influenced by beliefs about the behaviour's expected outcome or consequences (Contento, 2007). Distinguishing between beliefs and attitudes is important when considering food choice and IYCF behaviour, given that it can help to provide insight into the decision‐making process and the underlying reasons for action (or inaction).
The messaging used for the voice messaging addresses these theoretical components as does the survey tool to examine its impact. More specifically, each message was designed to target the underlying beliefs, attitudes, or norms of the targeted behaviours as well as provide advice as to how to change the specific behaviour. The underlying beliefs and attitudes were identified through the formative research in these communities. For example, a common belief among this population is that a runny or thin porridge should be fed to young children. However, these porridges tend to provide little nutrition beyond calories. We therefore designed a message that describes why the consistency of the porridge is important for their baby's nutrition and how to improve its nutritional quality.
Table S1 outlines the eight key messages sent to both mothers and fathers of young children. The average voice message was approximately 90 s in duration. After the messages were finalized, they were then translated into Wolof and Serer—the two local languages spoken by our study participants. The messages were recorded in a single female voice and subsequently uploaded into a voice messaging platform operated by a social enterprise specializing in the use of mobile technology, called Viamo (formerly VOTOmobile). The voice messaging platform allowed for the automated delivery of messages to the study sample at prespecified dates and times. The platform also allowed us to obtain real‐time information about whether or not the participants answered the voice messaging call and the length of time that they listened to the messages. In addition, two “yes or no” keypad response questions were included after each message was completed in order to ascertain information about: (a) whether the participant understood the message and (b) whether they found the message helpful. If the participant indicated that they did not understand the message, the voice message would be repeated.
2.5. Pilot and process evaluation of voice messaging intervention
2.5.1. Surveys
In order to examine the implementation of the voice messaging intervention and its potential for impact, we piloted the intervention in April–May 2017. A before and after study was conducted in three villages in Thies and Fatick. All households in the villages' farming group with a child 6 to 24 months (n = 48) were recruited to participate in the pilot study; however, one of the households did not complete the follow‐up data collection and was therefore not included in the analyses. In total, 47 households participated in the intervention and both data collection timepoints. Two voice messages per week for a period of 4 weeks were sent to the mothers and fathers of the young child.
In order to examine the impact of the voice messaging intervention on IYCF beliefs, attitudes intentions, and practices, a survey was conducted before and after the intervention was implemented. The beliefs, attitudes, and intentions survey included sociodemographic information (age, wealth, education, and literacy), questions related to IYCF beliefs, attitudes, intentions, and behaviours as well exposure to the intervention. The beliefs, attitudes, and intentions questions were based on those previously published by Monterrosa et al. (2013) and were tailored to our intervention. Questions aimed at assessing beliefs were operationalized as whether or not participants agreed or disagreed with the expected nutrition or growth outcome associated with the IYCF behaviour whereas questions to assess attitudes were framed as whether or not the participants perceived the IYCF behaviour to be good or not (i.e., favourable or unfavourable).
Both mothers and fathers answered questions related to IYCF beliefs and attitudes before and after the intervention implementation as well as questions related to exposure to the intervention and programme satisfaction, at the completion of the survey. In order to assess exposure to the intervention, participants conducted an unprompted recall of the different messages included in the intervention as part of the postintervention survey. Enumerators asked participants about the content of the messages they received with an open‐ended question and recorded all of the messages that the participant recalled. In addition, women also answered questions related to IYCF intentions and behaviours both before and after the implementation of the voice messaging intervention. In order to ascertain feeding behaviours, women were asked how many times they fed their child the specific foods targeted in the intervention over the previous 7 days. A structured 24‐hr recall was also conducted with women to assess their child's consumption over the previous day. The 24‐hr recall was used to calculate minimum dietary diversity, minimum meal frequency, and minimum acceptable diet indicators (WHO/UNICEF, 2010). Children who consumed four or more of the seven food groups (grains, roots, and tubers; legumes and nuts; dairy products; flesh foods; eggs; Vitamin A‐rich fruits and vegetables; and other fruit and vegetables) were defined as consuming a minimally diverse diet. Children who met both minimum dietary diversity and minimum meal frequency (2× for breastfed infants 6–8.9 months, 3× for breastfed children 9–23.9 months, and 4× for nonbreastfed children 6–23.9 months) were defined as consuming a minimum acceptable diet (WHO/UNICEF, 2010).
2.5.2. Focus groups
In addition to the surveys, we also conducted three focus groups (one per village) to better understand the process of the intervention implementation. We asked process evaluation questions related to the intervention's fidelity, dose delivered and received, reach, and context. We had anticipated doing separate focus groups with mothers and fathers (two per village); however, many of the men were working in nearby cities and were unable to participate in the in‐village focus groups. A total of 24 women and two men participated in the focus groups.
2.6. Analyses
Descriptive statistics were used to examine programme satisfaction and recall of the voice messages as part of the pilot. Paired t tests (for continuous variables) and the McNemar's test (for categorical variables) were used to examine whether IYCF beliefs, attitudes, intentions, and behaviours improved after the intervention implementation. We used SPSS (Version 24) to conduct these analyses and used a p value of <.05 to denote significant differences.
All focus groups were recorded in Wolof, translated to English, and transcribed verbatim.
Focus group transcripts were open coded by one researcher (S. M. D.) using NVivo software (Version 11.4). The codes from the focus groups conducted as part of the formative research were subsequently organized based on key themes related to IYCF knowledge and practices as well as potential barriers and facilitators to implementing an mHealth IYCF intervention.
The focus groups conducted as part of the process evaluation were also open coded and subsequently organized based on key themes related to the intervention implementation process, including fidelity, dose delivered and received, reach, and context.
3. RESULTS
3.1. Formative research for the development of voice messages
3.1.1. Formative data to inform logistics of intervention design
Low literacy levels, lack of electricity in some villages, and the role of men as key food purchasing decision‐makers influenced the way in which the voice messaging programme was designed. Although our original plans were to conduct the intervention via text message, our formative work led us to shift from text to voice messaging to ensure better comprehension of the IYCF messages given that some focus group participants indicated that they would need to “have someone read the messages for [them]” if they were sent via text message. The lack of electricity in some villages also influenced the design of the intervention. One focus group participant said they “would like to receive messages everyday but we don't have electricity power in the village.” As another focus group participant stated they “generally charge [their] mobile phones once or twice a week,” leading us to align the delivery of the voice messages with the days of the weekly markets in villages without electricity so that we could increase the likelihood that mobile phones would be charged at the time that we sent the messages. The participants in both the male and female focus groups indicated that men were key decision‐makers related to household food expenditure: “It's the husband who decides to purchase the food” and “the wife only goes to the market.” However, there was also a recognition that women have some input into the nonstaple foods that are purchased. As one woman said: “Generally men decide in terms of basic food (millet, rice, oil) but when we go to the market, we buy condiments.” For this reason, we decided to include the fathers, in addition to mothers, in the intervention with the intent to improve buy‐in for messages related to increasing the purchase and consumption of specific foods (e.g., animal sourced foods).
3.1.2. Formative data to inform content of voice messages
Breastfeeding was viewed favourably by all focus group participants. However, many participants mentioned providing newborns with holy water rather than exclusively breastfeeding. As one participant said: “They are given holy water before anything else and then breast milk.” There was also a lack of clarity regarding the recommended length of time that a baby should be breastfed. One of the participants distinguished the breastfeeding length based on sex: “male infants breast 1 year and 6 months and female 2 years.” This was attributed to the belief that “when a male child breasts a lot he will not be clever.”
Focus group participants were aware of some locally produced nutrient rich foods (e.g., millet) that should be fed to children; however, a combination of cultural beliefs as well as a lack of knowledge related to the nutritional quality of some nutrient‐rich foods led to their avoidance in the initial stages of complementary feeding. As one woman stated: “When the child is 6 months, he/she eats porridge millet, and from 1 year, he/she starts eating heavy food such as Dakhine, and from 1 year and 6 months … you serve the child with rice and fish and some vegetables.” In terms of the avoidance of specific foods, there was a reluctance to feed young children “heavy” foods such as rice and root vegetables as well as some greens given the children's small stomachs. Moreover, feeding fish in the early stages of complementary feeding was reportedly avoided due to its bones. There were also cultural reasons for not feeding children eggs, yet some scepticism over these beliefs, “some say that children eating eggs will not be able to talk … but there are examples of many children eating eggs and yet are talking without any problem.” Lastly, focus group participants identified specific foods that they would like to feed their children to improve their nutrition, but their lack of availability or affordability limited their purchase. This included “meat, chicken and sardines” and “oranges, bananas and mandarins.”
3.2. Piloting of voice messaging intervention
3.2.1. Beliefs, attitudes, and intentions
We asked mothers and fathers about their beliefs about the expected outcomes of feeding their babies according to the IYCF practices targeted in the intervention both before and after its implementation (Table S2). The only significant difference in mothers' IYCF beliefs after the completion of the intervention was related to the nourishment that young children receive from “thin” porridge, where fewer women believed it was nourishing after the intervention completion. There were no other significant differences in the beliefs of mothers, or of fathers, after the intervention completion.
Table 1 provides an overview of mothers' and fathers' attitudes (i.e., favourable or unfavourable judgements about specific behaviours) related to IYCF before and after the intervention. Overall, mothers' attitudes related to feeding their child leafy greens, eggs, fish, and thin porridge changed over the course of the intervention. Fathers' attitudes towards feeding their child a variety of foods at each meal, feeding them fruits and vegetables and thin porridge, were also significantly different after the completion of the intervention.
Table 1.
The attitudesa of mothers and fathers regarding IYCF practices
| Mothers' attitudes (n = 47) | Fathers' attitudes (n = 47) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preintervention | Postintervention | p value | Preintervention | Postintervention | p value | |||||||||
| Attitudes towards IYCF practices | 1 = Good (%) | 2 = Not good (%) | 3 = Not sure (%) | 1 = Good (%) | 2 = Not good (%) | 3 = Not sure (%) | 1 = Good (%) | 2 = Not good (%) | 3 = Not sure (%) | 1 = Good (%) | 2 = Not good (%) | 3 = Not sure (%) | ||
| Continuing breastfeeding after 6 months | 100 | 0 | 0 | 97.8 | 2.2 | 0 | .32 | 91.7 | 0 | 8.3 | 97.2 | 0 | 2.8 | .32 |
| Feeding a variety of foods at each meal | 89.1 | 10.9 | 0 | 95.7 | 4.3 | 0 | .26 | 62.2 | 2.7 | 35.1 | 91.9 | 8.1 | 0 | .001* |
| Feeding multiple times per day | 91.5 | 8.5 | 0 | 95.7 | 4.3 | 0 | .41 | 89.2 | 2.7 | 8.1 | 83.8 | 13.5 | 2.7 |
1.00 |
| Feeding leafy greens | 70.2 | 10.6 | 19.2 | 89.4 | 6.4 | 4.3 | .01* | 83.8 | 5.4 | 10.8 | 89.2 | 5.4 | 5.4 | .43 |
| Feeding eggs | 77.3 | 22.7 | 0 | 93.2 | 6.8 | 0 | .04* | 75.7 | 10.8 | 13.5 | 83.8 | 13.5 | 2.7 | .18 |
| Feeding fish | 80.9 | 8.5 | 10.6 | 95.8 | 2.1 | 2.1 | .03* | 91.7 | 0 | 8.33 | 94.4 | 0 | 5.6 | .66 |
| Feeding yogurt | 89.3 | 6.4 | 4.3 | 85.1 | 12.8 | 2.1 | .78 | 100 | 0 | 0 | 89.2 | 8.1 | 2.7 | .06 |
| Feeding cow pea | 97.9 | 2.1 | 0 | 97.9 | 2.1 | 0 | 1.00 | 100 | 0 | 0 | 100 | 0 | 0 | 1.00 |
| Feeding peanuts | 51.1 | 38.3 | 10.6 | 53.2 | 40.4 | 6.4 | .61 | 56.8 | 27.0 | 16.2 | 46 | 35.1 | 18.9 | .47 |
| Feeding orange F&V | 100 | 0 | 0 | 100 | 0 | 0 | 1.00 | 100 | 0 | 0 | 100 | 0 | 0 | 1.00 |
| Feeding other F&V | 76.1 | 0 | 23.9 | 87 | 0 | 13 | .17 | 39 | 0 | 61 | 82.1 | 0 | 17.9 | .001* |
| Feeding thin porridge | 97.8 | 2.2 | 0 | 76.1 | 23.9 | 0 | .004* | 100 | 0 | 0 | 86.5 | 13.5 | 0 | .03* |
| Feeding thick porridge | 93.6 | 4.3 | 2.1 | 100 | 0 | 0 | .39 | 97.3 | 0 | 2.7 | 91.9 | 8.1 | 0 | .71 |
| Feeding meat | 66 | 21.3 | 12.8 | 74.5 | 17 | 8.5 | .38 | 44.2 | 39.5 | 16.3 | 59 | 28.2 | 12.8 | .12 |
| Feeding milk | 93.6 | 4.3 | 2.1 | 100 | 0 | 0 | .39 | 100 | 0 | 0 | 100 | 0 | 0 | 1.00 |
| Feeding cheese | 89.4 | 2.1 | 8.5 | 100 | 0 | 0 | .17 | 97.3 | 0 | 2.7 | 97.3 | 2.7 | 0 | .66 |
| Feeding organ meat | 85.1 | 6.4 | 8.5 | 91.4 | 4.3 | 4.3 | .28 | 91.4 | 0 | 8.6 | 94.3 | 0 | 5.7 | .66 |
| Feeding homegrown F&V | 97.9 | 2.1 | 0 | 100 | 0 | 0 | .32 | 100 | 0 | 0 | 100 | 0 | 0 | 1.00 |
Abbreviations: IYCF, infant and young child feeding; F&V, fruits and vegetables.
Attitudes refer to the favourable or unfavourable judgements that participants made regarding infant and young child feeding (IYCF) behaviours. Participants were asked whether they thought each IYCF practice or behaviour was good, bad, or they were unsure.
Denotes significance at p < .05.
In addition to asking mothers and fathers about their beliefs and attitudes related to IYCF practices, we also asked mothers about their intentions for feeding their child within the next 3 days (Table S3). We found that mothers were significantly more likely to have the intention to feed their babies orange fruits and vegetables. However, they were less likely to have the intention to feed their child porridge mixed with other foods, which contrasts the messaging delivered.
3.2.2. Behaviours
Overall, there was a significant increase in the number of children that consumed fish (60% vs. 94%; p = .008) as measured by the 24‐hr dietary recall after the completion of the intervention (Figure 1). We also found significant increases in the frequency of eggs (p = .026), fish (p = .004), and thick porridge (p = .002; porridge that has a consistency that is thick enough that it does not fall off the spoon) consumption in the previous 7 days measured by the food frequency questionnaire (Figure 2). Alongside the increases in the consumption of targeted foods, there was also a significant reduction in the frequency of consuming organ meat postintervention (p = .033) over the past 7 days, which is contradictory to the messaging delivered through the intervention. There were no differences in organ meat consumption in the 24‐hr recall.
Figure 1.
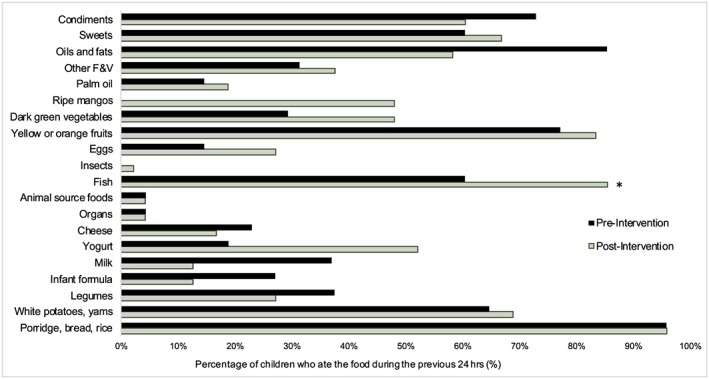
Consumption of food groups over the previous 24 hr before and after the intervention. *Significant at p < .05
Figure 2.
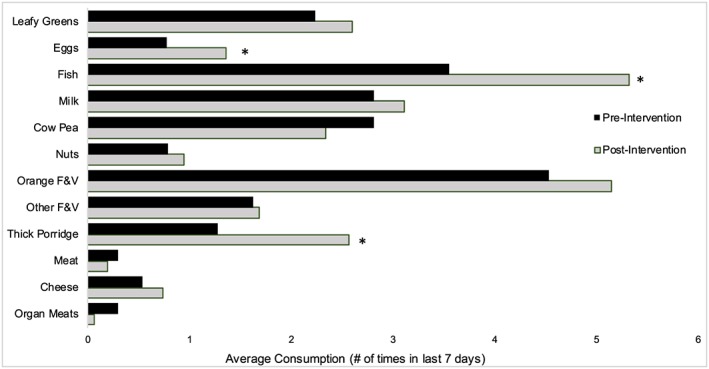
The mean frequency of consumption of foods over the past 7 days before and after the voice messaging intervention. *Significant at p < .05
We also examined minimum dietary diversity and minimum acceptable diet scores before and after the intervention implementation. A higher meal frequency (3.3 vs. 4.3 meals per day; p = .026), number of food groups (3.9 vs. 4.5 of the seven food groups; p = .067), minimum meal frequency (87% vs. 96%; p = .125), minimum dietary diversity (63% vs. 72%; p = .523), and minimum acceptable diet score (48% vs. 67%; p = .108) were observed after the intervention; however, only meal frequency was statistically significant. We did not find any significant differences in any of the IYCF behaviours between boys and girls.
3.3. Implementation process
3.3.1. Dose delivered and received and reach
Figure 3 depicts the number of voice messaging calls that were answered and completed. Overall, the majority of participants answered and completed the calls. Although only about a third of participants answered the automated keypad questions, for the most part, participants reported understanding the messages and finding them useful (Figure S1). One exception was the message related to providing infants and young children with a variety of foods during each meal—only half of the respondents to these questions reported understanding the message and about half of participants hung up prior to the message completion. A few participants indicated that some of the messages in the Serer language were spoken too quick.
Figure 3.
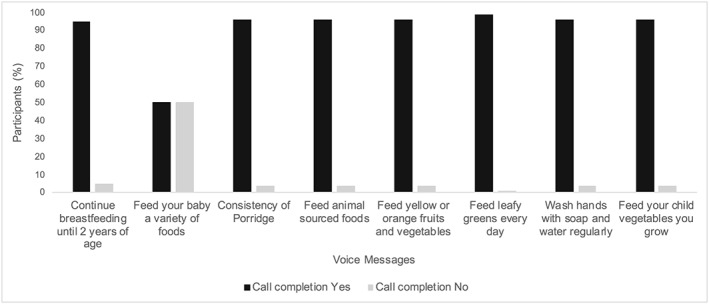
The percentage of participants that listened to the voice message in its entirety
Figure 4 provides an overview of the messages recalled by mothers and fathers as part of the open recall of the voice messages. The message related to feeding infants and young children orange fruits and vegetables was the most, and the breastfeeding message the least, commonly recalled message by both mothers and fathers.
Figure 4.
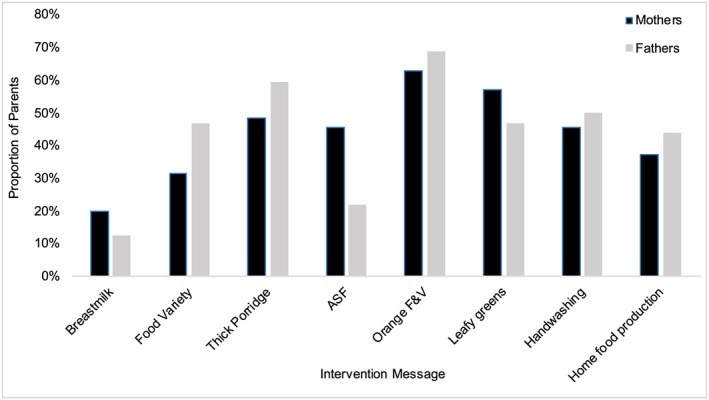
Mother and father recall of voice messages
There were some challenges in terms of the reach of the intervention that were identified through the focus group discussions. In one of the study villages, several women who participated in the focus group reported not receiving the messages due to providing incorrect phone numbers or providing the number of a family member given that they did not have their own mobile phone. Although mobile phone ownership is widespread in rural Senegal, there are still women who are unable to afford them. In the two other study villages, focus group participants indicated that they had received all, or nearly all, the messages and that they listened to the messages in their entirety.
Focus group participants reported some barriers in terms of receiving the voice messages. In two of the villages, there were problems with receiving cellphone service, and one village reported problems in terms of charging phones because the village did not have electricity. Focus group participants recalled the exact days and times that they received the messages and indicated that they were ready to receive the calls at those times—this was seen as being a crucial element of the voice messaging intervention's success.
3.3.2. Context
Focus group participants indicated that several of the messages contradicted their previous beliefs related to IYCF practices and led them to shift their behaviours, particularly in terms of feeding their children moringa (leafy green), fish, thicker porridge, and eggs. However, there were some participants that indicated that they had not yet started implementing changes. The main barrier to adopting these practices was “mostly financial.”
3.3.3. Overall programme satisfaction
Table S4 provides an overview of the programme satisfaction among participants. Overall, both mothers and fathers viewed the intervention relatively positively. They indicated that it improved their knowledge, that they were able to take action on the recommendations made in the messages, and that they were confident in their ability to feed their child nutritious foods. Approximately, a third of mothers and 44% of fathers rated the programme as excellent, with the majority of the remaining respondents rating it as good. These data were supported by the qualitative focus group data.
Focus group participants reported enjoying receiving the voice messages and found it helpful that the examples of foods used in the messages were available in their local market, with the exception of a few fruits that are only available during specific seasons: “most foods are available, but some are seasonal and can be lacking at some periods of the year.” They provided very limited feedback in terms of how the messages could be improved. However, one focus group participant suggested that they could be more interactive and provide a phone number that could be called to get additional information about different topics. Given the role of elders in these communities, some participants also indicated that it may be helpful to send the messages to the grandmothers as well.
4. DISCUSSION
This study provides an overview of the design, pilot testing, and process evaluation of a voice messaging intervention aimed at improving IYCF practices in rural Senegal. We found formative work that influenced the intervention design to be critical in terms of ensuring that messages were relevant from a sociocultural perspective and based on the needs of the target population. The pilot study findings provide preliminary evidence to suggest that voice messaging interventions may have the potential to improve IYCF practices in rural Senegal. It also provides insight into the potential logistical challenges associated with the scale‐up of mHealth voice messaging interventions and ways to mitigate some of those challenges in future studies.
4.1. Intervention impact
Few of the interventions aimed at improving IYCF practices provide a detailed description of the theoretical underpinnings of their interventions, which makes it difficult to unpack the “black box” by which improvements in behaviours and practices occurred (Graziose et al., 2018). As part of our pilot study, we examined whether changes in the precursors to behaviour change, such as beliefs and attitudes related to IYCF practices, changed over the intervention period. Although we did not find significant differences in the IYCF beliefs of mothers and fathers following the intervention, with the exception of the thickness of porridge, we did find differences in the attitudes towards feeding children some of the targeted foods in the intervention, which also translated into changes in IYCF feeding behaviour. These shifts in attitudes may have been the impetus for behaviour change.
We found significant changes in mothers' attitudes and children's intakes of three of the eight targeted foods (i.e., fish, thick porridge, and eggs) following the voice messaging intervention's implementation. Based on our formative work, prior to commencing, the intervention community members had beliefs and attitudes related to feeding fish, thin rather than thick porridge, and eggs that would lead them to limit feeding these foods to young children. We found that the attitudes towards these targeted foods shifted over the course of the intervention, which may have been the impetus for behaviour change. It is possible that shifting these target behaviours was easier than some of the other targeted foods such as meat. Feeding thicker porridge would be relatively easy, even for households with little resources. Fish is consumed frequently in households, making it easier than meat (which is infrequently consumed) to incorporate into the diets of young children. Moreover, some households in these communities have chickens that could have facilitated increased consumption of eggs. Contrary to our expectations, we also found a decrease in organ meat consumption after the intervention, despite emphasizing its consumption in one of the voice messages. Given that organ meat may only be available in a given village at specific times, such as the day of weekly market, this may have been due to supply rather than demand given that beliefs, attitudes, and intentions related to feeding organ meat to their infants did not change following the intervention.
Our findings are consistent with other studies that have found a positive impact of mass media and BBC campaigns on IYCF practices (Graziose et al., 2018; Lee et al., 2016; Naugle & Hornik, 2014). Monterrosa et al. (2013) found increases in the consumption of leafy greens, thicker broth, and beef after the scripted message intervention, which was delivered by vaccination nurses and on local radios, was implemented in Mexico. Sun et al. (2018) found a 16.6% increase in dietary diversity and a 37.6% increase in feeding iron‐rich foods, following the implementation of an IYCF intervention consisting of individual education sessions along with a television and print campaign. Although we did not find any significant differences in minimum dietary diversity or minimum acceptable diet, our ability to detect significant differences was likely limited by our small sample size, given that we found a nearly 20% increase in minimum acceptable diet after the intervention implementation. Future research should involve scaling‐up the intervention to a larger number of households and conducting a rigorous evaluation of its impact on minimum dietary diversity and minimum acceptable diet, along with other nutrition outcomes (e.g., haemoglobin levels) in order to provide additional information regarding its effectiveness.
We targeted ASF consumption in our voice messages and found higher intakes of both eggs and fish at the completion of the intervention. Although egg consumption remained relatively low even after the completion of the intervention—likely attributable to their high cost (Headey, Hirvonen, & Hoddinott, 2017)—fish consumption was high with 85.4% of infants and young children consuming fish on the previous day. This is encouraging and will help provide key nutrients to children given that fish is an important source of protein in addition to several micronutrients (e.g., iron and zinc). Although other ASFs (e.g., red meat and chicken) were targeted in the intervention, their consumption remained low and unchanged after the intervention. Our focus group data suggested that although meat may be available in the marketplace, it is not perceived as being affordable. In order to increase its consumption, interventions will likely need to go beyond providing information about its potential to improve health but to provide complementary incentives for its purchase and consumption. Interventions that provide women with small livestock such as chickens may be one way to improve access to ASFs, while simultaneously increasing women's empowerment. These programmes have demonstrated a positive impact on nutrition and health outcomes among women and children (Olney et al., 2016; D. K. Olney, Pedehombga, Ruel, & Dillon, 2015), as well as increasing women's empowerment by improving their control over purchasing and health care decisions (Olney et al., 2016).
4.2. Intervention implementation
One of the challenges associated with assessing BCC interventions is that they often provide little information about the delivery and reach of the intervention (Graziose et al., 2018; Pelto, Martin, Van Liere, & Fabrizio, 2016). One of the benefits of conducting a voice messaging intervention, such as the one conducted in this study, is that we were able to receive real‐time feedback about whether participants answered the voice message calls and for how long they listened to them, through the monitoring of automated call logs via the voice messaging platform. This enabled us to identify problems in terms of reaching our participants early on in the intervention delivery period. This was important given that many of the phone numbers that participants had provided were incorrect. In these cases, we were able to contact the household (via the head of household's phone number) and make changes in the delivery platform early on in the study implementation period.
One of the other advantages to using this type of delivery platform is that we were able to incorporate process questions into the intervention delivery. Although we had conducted formative research in order to help develop the messages, we had not piloted the messages themselves prior to implementing the intervention. Thus, the feedback that was provided on whether or not participants understood the message, and whether they found it helpful, was informative with regard to any problems related to clarity of the messages. It also allowed for those who did not understand the message to listen to the message a second time. On the basis of this information, we are aware of a problem related to the interpretation of the “variety of foods” message that needs to be rectified prior to scaling‐up the intervention.
Although we were limited by a small sample size for this pilot study, the results were encouraging both in terms of IYCF practices but also in terms of programme satisfaction. The majority of both mothers (97.2%) and fathers (96.9%) rated the intervention as good or excellent. Fathers have most often not been included in interventions focused on IYCF, and their preferences for feeding their young children are often determined by cultural norms and the practices of their own mothers or relatives (Alive & Thrive, 2015). Although men reported enjoying the intervention, there were few significant differences in their beliefs and attitudes related to IYCF practices before and after the intervention. Unfortunately, we were unable to include enough men in the focus group discussions to be able to disentangle the reasoning for the lack of change. Accessing men in the pilot villages was difficult given that many of them are working from Dakar or other towns/cities during the dry season.
4.3. Lessons learned regarding the implementation of voice messaging interventions
There were several lessons learned through the piloting of the voice messaging intervention. The first was the importance, and difficulty, in ensuring that the mobile phone numbers participants provide to enumerators are accurate. This is often a challenge, especially given that many participants had multiple numbers through different service providers. Voice messaging interventions need to devote time to ensuring that the mobile phone numbers provided are accurate. Moreover, if voice messaging interventions include embedded questions related to the understanding and helpfulness of the message, enumerators need to demonstrate to participants how to key in their answers prior to the intervention beginning. We had low levels of responses to our process questions. Researchers should be cognizant that many participants will not be familiar with keypad responses, and thus, they need to be shown how to do this in order to increase their likelihood of response.
4.4. Limitations
This study has several limitations. Our pilot of the intervention is limited by its small sample size, lack of control group, and short follow‐up period. In order to ascertain the sustainability of the intervention, a longer follow‐up period would be necessary. Moreover, our primary outcomes of the pilot were focused on diets rather than on harder biological outcomes (e.g., anaemia). Future work should include additional outcome measures in order to examine the impact of the intervention on nutritional status. Lastly, the focus group discussions that we conducted as part of the process evaluation included predominantly women (24 of 26 participants), limiting our ability to gain in‐depth information regarding the implementation of the intervention from men.
5. CONCLUSIONS
This paper provides an overview of the process of designing an mHealth voice messaging intervention targeting IYCF practices in rural Senegal as well as its impact and implementation. Our findings suggest that voice messaging IYCF interventions have the potential to improve IYCF behaviours; they are viewed favourably by participants and are relatively easy to implement. Additional research is needed in order to assess the intervention's impact on IYCF and nutrition outcomes on a larger scale and over a longer period to assess the intervention's sustainability. Moreover, future work should examine the potential of including mHealth voice messaging interventions as part of a package of behavioural interventions aimed at targeting IYCF practices as well as interventions aimed at increasing agricultural production.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
SMD and JK performed the research. SMD, JF, and SS designed the research study. SMD, JK, and JS conducted the data analysis. SMD prepared the initial draft of the manuscript, and all authors provided feedback.
Supporting information
Table S1. Key Messages for Voice Messaging Intervention
Table S2. Beliefs related to IYCF practices of mothers and fathers before and after the intervention
Table S3. Mother's intentions for feeding their baby within the next 3 days
Figure S1. Overview of the participants’ understanding and perceived usefulness of the voice messages
Table S4. Overview of voice messaging intervention program satisfaction
ACKNOWLEDGMENT
We would like to acknowledge Patricia Welch for her assistance in developing the messages included in the voice messaging intervention. We are grateful for her contribution.
Downs SM, Kalaj J, Smith S, Sackey J, Fanzo J. An mHealth voice messaging intervention to improve infant and young child feeding practices in Senegal. Matern Child Nutr. 2019;15, e12825 10.1111/mcn.12825
REFERENCES
- Agence Nationale de la Statistique et de la Démographie (ANSD) (2016). Enquête Démographique et de Santé Continue. Dakar: Senegal. [Google Scholar]
- Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50(2), 179–211. 10.1016/0749-5978(91)90020-T [DOI] [Google Scholar]
- Alive & Thrive (2015). Fathers support infant and young child feeding: Their contributions to better outcomes. Retrieved from: https://www.aliveandthrive.org/wp-content/uploads/2018/07/Literature-Reivew-Dads.pdf
- Bhutta, Z. A. , Das, J. K. , Rizvi, A. , Gaffey, M. F. , Walker, N. , Horton, S. , … Black, R. E. (2013). Evidence‐based interventions for improvement of maternal and child nutrition: What can be done and at what cost? Lancet, 382(9890), 452–477. 10.1016/s0140-6736(13)60996-4 [DOI] [PubMed] [Google Scholar]
- Cellule de Lutte Contre la Malnutrition (CLM) (2015). Boite a images: Sur la survie de la mere, du nouveau‐ne et du jeune enfant. Pour les agents de sante et les relais communautaires. Retrieved from. Dakar: Senegal. [Google Scholar]
- Contento, I. (2007). Foundation in theory and research: Increasing awareness and enhancing motivation In Nutrition education: Linking research, theory, and practice (pp. 73–80). Boston: Jones and Bartlett Publishers. [Google Scholar]
- Dewey, K. G. , & Adu‐Afarwuah, S. (2008). Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Maternal & Child Nutrition, 4(Suppl 1), 24–85. 10.1111/j.1740-8709.2007.00124.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flax, V. L. , Negerie, M. , Ibrahim, A. U. , Leatherman, S. , Daza, E. J. , & Bentley, M. E. (2014). Integrating group counselling, cell phone messaging, and participant‐generated songs and dramas into a microcredit program increases Nigerian women's adherence to international breastfeeding recommendations. The Journal of Nutrition, 144(7), 1120–1124. 10.3945/jn.113.190124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graziose, M. M. , Downs, S. M. , O'Brien, Q. , & Fanzo, J. (2018). Systematic review of the design, implementation and effectiveness of mass media and nutrition education interventions for infant and young child feeding. Public Health Nutrition, 21(2), 273–287. 10.1017/s1368980017002786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurman, T. A. , Rubin, S. E. , & Roess, A. A. (2012). Effectiveness of mHealth behavior change communication interventions in developing countries: a systematic review of the literature. Journal of Health Communication, 17(Suppl 1), 82–104. 10.1080/10810730.2011.649160 [DOI] [PubMed] [Google Scholar]
- Headey, D. , Hirvonen, K. , & Hoddinott, J. (2017). Animal sourced foods and child stunting. IFPRI Discussion Paper 1695 Retrieved from. Washington, D.C.: International Food Policy Research Institute (IFPRI). [Google Scholar]
- Hurt, K. , Walker, R. J. , Campbell, J. A. , & Egede, L. E. (2016). mHealth interventions in low and middle‐income countries: A systematic review. Global Journal of Health Science, 8(9), 54429 10.5539/gjhs.v8n9p183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang, H. , Li, M. , Wen, L. M. , Hu, Q. , Yang, D. , He, G. , … Qian, X. (2014). Effect of short message service on infant feeding practice: Findings from a community‐based study in Shanghai, China. JAMA Pediatrics, 168(5), 471–478. 10.1001/jamapediatrics.2014.58 [DOI] [PubMed] [Google Scholar]
- Kristen Devlin, K. F. E. , & Pandit‐Rajani, T. (2016). Community health systems catalog country profile: Senegal. Retrieved from. Arlington, VA: Advancing Partners & Communities. [Google Scholar]
- Lee, S. H. , Nurmatov, U. B. , Nwaru, B. I. , Mukherjee, M. , Grant, L. , & Pagliari, C. (2016). Effectiveness of mHealth interventions for maternal, newborn and child health in low and middle–income countries: Systematic review and meta–analysis. Journal of Global Health, 6(1), xx–xx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monterrosa, E. C. , Frongillo, E. A. , Gonzalez de Cossio, T. , Bonvecchio, A. , Villanueva, M. A. , Thrasher, J. F. , & Rivera, J. A. (2013). Scripted messages delivered by nurses and radio changed beliefs, attitudes, intentions, and behaviors regarding infant and young child feeding in Mexico. The Journal of Nutrition, 143(6), 915–922. 10.3945/jn.112.169235 [DOI] [PubMed] [Google Scholar]
- Naugle, D. A. , & Hornik, R. C. (2014). Systematic review of the effectiveness of mass media interventions for child survival in low‐and middle‐income countries. Journal of Health Communication, 19(sup1), 190–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olney, D. K. , Bliznashka, L. , Pedehombga, A. , Dillon, A. , Ruel, M. T. , & Heckert, J. (2016). A 2‐year integrated agriculture and nutrition program targeted to mothers of young children in Burkina Faso reduces underweight among mothers and increases their empowerment: A cluster‐randomized controlled trial. The Journal of Nutrition, 146(5), 1109–1117. [DOI] [PubMed] [Google Scholar]
- Olney, D. K. , Pedehombga, A. , Ruel, M. T. , & Dillon, A. (2015). A 2‐year integrated agriculture and nutrition and health behavior change communication program targeted to women in Burkina Faso reduces anemia, wasting, and diarrhea in children 3–12.9 months of age at baseline: A cluster‐randomized controlled trial. The Journal of Nutrition, 145(6), 1317–1324. 10.3945/jn.114.203539 [DOI] [PubMed] [Google Scholar]
- Pelto, G. H. , Martin, S. L. , Van Liere, M. , & Fabrizio, C. S. (2016). The scope and practice of behaviour change communication to improve infant and young child feeding in low‐and middle‐income countries: Results of a practitioner study in international development organizations. Maternal & Child Nutrition, 12(2), 229–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sellen, D. , Mbugua, S. , Webb‐Girard, A. , Lou, W. , Duan, W. , & Kamau‐Mbuthia, E. (2014). Cell phone based peer counselling can support exclusive breastfeeding: A randomized controlled trial in Kenya (119.5). The FASEB Journal, 28(1_supplement), 119–115. [Google Scholar]
- Smith, L. , & Haddad, L. (2000). Explaining child malnutrition in developing countries: A cross country analysis. Retrieved from. Washington, DC: xxxx. [Google Scholar]
- Sun, J. , Zhang, L. , Cui, J. , Li, S. , Lu, H. , Zhang, Y. , … Baloch, Z. (2018). Effect of dietary intervention treatment on children with iron deficiency anemia in China: A meta‐analysis. Lipids in Health and Disease, 17(1), 108 10.1186/s12944-018-0749-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF (2012). Key messages booklet: The community infant and young child feeding counselling package. Retrieved from. New York: UNICEF, NY. [Google Scholar]
- WHO/UNICEF (2010). Indicators for assessing infant and young child feeding practices. Retrieved from. Geneva: WHO. [Google Scholar]
- World Health Organization (2015). Essential nutrition actions: Improving maternal, newborn, infant and child health and nutrition. Retrieved from. Geneva: WHO. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Key Messages for Voice Messaging Intervention
Table S2. Beliefs related to IYCF practices of mothers and fathers before and after the intervention
Table S3. Mother's intentions for feeding their baby within the next 3 days
Figure S1. Overview of the participants’ understanding and perceived usefulness of the voice messages
Table S4. Overview of voice messaging intervention program satisfaction


