Abstract
This study aimed to assess the iodine status of pregnant women in each trimester and to compare the pregnancy outcomes between groups with iodine insufficiency and iodine sufficiency. Longitudinal study on urinary iodine concentration (UIC) in each trimester as well as comparison between women with iodine insufficiency (<150 mcg L−1) and iodine sufficiency was conducted. Pregnant women without thyroid diseases who had not received iodine supplementation were recruited for UIC measurements in each trimester and were followed up for pregnancy outcomes. In the analysis of 384, 325 and 221 samples in the first, second and third trimester, the medians of UICs were 147.39, 157.01 and 153.07 mcg L−1, respectively. Of 399 women, 174 (43.6%) had a UIC less than 150 mcg L−1 (suggesting iodine insufficiency) and 225 (56.4%) had a UIC greater than or equal to 150 mcg L−1 (suggesting iodine sufficiency). Of 390 women with availability of the final outcomes, 171 and 219 in the insufficiency and sufficiency group, respectively, the rates of preterm birth and low birthweight were significantly higher in the insufficiency group, 17.5% vs. 10.0% (P = 0.031) and 19.9% vs. 12.3% (P = 0.042), respectively. Logistic regression analysis showed that iodine status was an independent risk of preterm birth and low birthweight. Finally, women with a UIC <100 mcg L−1 had a significantly higher rate of fetal growth restriction, 13/68 vs. 30/322 (P = 0.031). In northern Thailand, a great number of pregnant women had a median UIC less than 150 mcg L−1 and they had a higher risk of preterm birth and low birthweight. Finally, those with a median UIC of less than 100 mcg L−1 had a higher risk of fetal growth restriction.
Keywords: iodine, pregnancy, outcomes
Introduction
Iodine deficiency has been a significant health problem worldwide and affects both industrialized and developing countries. The ongoing monitoring of iodine status in the population remains essential, and special attention needs to be paid to monitor the status of vulnerable population, such as pregnant women and infants. Recent data on urinary iodine excretion in adults as well as newborns indicate a high prevalence of iodine insufficiency in many countries (Hetzel 1983; Zimmermann & Andersson 2012; Pearce 2013). These cases may manifest as subclinical hypothyroidism in neonates, or as goitre in adolescents and adults. Iodine insufficiency causes not only goitre but also mental deficiency, hearing loss and other neurological impairments, as well as short stature secondary to thyroid insufficiency. Although iodinated salt should be available in most countries where it is needed, its quality and share of the market are often unsatisfactory. Dietary iodine requirement is increased during pregnancy due to increased thyroid hormone production, increased renal iodine loss and fetal iodine requirements. Adequate amount of iodine is essential for fetal neurological development immediately after conception, and such abnormalities are dependent on the degree of insufficiency. The degree of insufficiency varied from countries to countries. Therefore, each geographical area should have its own baseline data of the status of iodine intake. The World Health Organization (WHO) has estimated that at least 50 million people worldwide have varying degrees of preventable brain damage due to iodine deficiency (WHO, UNICEF, ICCIDD 2007). Although it is doubtful whether mild insufficiency causes intellectual impairment or not, iodine supplementation does prevent fetal goitre (Stagnaro‐Green et al. 2012). Severe insufficiency, on the other hand, is frequently associated with damage typically encountered with endemic cretinism (Delange 2001). It is presumed that moderate insufficiency has intermediate and variable effects.
Although several reports have documented the effects of iodine insufficiency on fetal neurodevelopment and some authors have observed a potential risk of fetal growth restriction (FGR) or low birthweight (LBW) among pregnancies with iodine insufficiency (Boyages 1993; Zimmermann 2009), little has been known about the effects of iodine insufficiency on pregnancy outcomes such as preterm birth (PTB), growth restriction or pre‐eclampsia. Furthermore, very few studies have assessed iodine status in each trimester of pregnancy. In our practice, we have not routinely supplemented iodine to pregnant women, although some hospitals and clinics have. Only iron supplementation has been routinely prescribed to pregnant women, and folic acid supplementation is optional. Currently, national policy has been developed to support routine iodine supplementation. However, before implementation, we need to determine the baseline iodine status in our obstetric population. Therefore, we conducted this study to assess the iodine status of pregnant women in each trimester and to compare the pregnancy outcomes between women with iodine insufficiency and iodine sufficiency.
Key messages.
Iodine insufficiency is prevalent in many regions of the world. Pregnant women in the northern part of Thailand have a median urinary iodine concentration (UIC) less than 150 mcg L−1.
A maternal UIC less than 150 mcg L−1 significantly increases the risk of preterm birth and low birthweight.
A maternal UIC less than 100 mcg L−1 significantly increases the risk of fetal growth restriction.
In this population, the median UIC is relatively constant over the three trimesters of normal pregnancy.
Subjects and methods
This study, including longitudinal measurements of urinary iodine concentrations (UICs) throughout pregnancy and comparison of pregnancy outcomes between women with iodine insufficiency and iodine sufficiency, was carried out at the Department of Obstetrics and Gynecology, Faculty of Medicine, Chiang Mai University, Thailand, with ethical approval granted by the institutional review boards. Pregnant women who are attending our antenatal care clinic during 1 September 2013 and 31 October 2014 were invited to participate in the study with written informed consent. The inclusion criteria were (1) singleton pregnancy; (2) Thai ethnicity; (3) reliable gestational age based on certain and regular menstrual period consistent with clinical estimation on early gestation or fetal sonographic biometry in the first half of pregnancy; and (4) no thyroid diseases. To avoid heterogeneity of study population, only Thai ethnic women were included. Exclusion criteria consisted of (1) multifetal pregnancies; (2) previously or currently diagnosed for any thyroid diseases or history of thyroid treatment; (3) receiving iodine‐containing supplements; and (4) loss to follow‐up or unavailability of the pregnancy outcomes.
The main outcome measures were (1) median of UICs in each trimester and patterns of UIC changes among the three trimesters; (2) iodine status among our obstetric population, categorized as insufficiency, adequacy, above requirement and excessive levels, as well as the proportion of women with iodine insufficiency among non‐supplemented pregnant women. The criteria of insufficiency, adequate, above requirement and excessive in this study, were defined as a median UIC of less than 150, 150–249 and 250–449 μg L−1, and more than 500 μg L−1, respectively, based on the international WHO, UNICEF, ICCIDD (2007) criteria; and (3) a comparison of pregnancy outcomes between women with iodine insufficiency and iodine sufficiency, including rates of FGR, PTB, LBW, pre‐eclampsia or pregnancy‐induced hypertension (PIH), antepartum haemorrhage (placenta previa and placental abruption), low Apgar scores at 1 and 5 min, and caesarean section. The maternal baseline characteristics and obstetric outcomes were also evaluated. The following variables were assessed: parity, number of antenatal visits, gestational age at delivery, route of delivery, pregnancy outcomes including abortion (defined as ending up before 24 weeks), PTB (delivery before 259 days of gestation), LBW (birthweight of less than 2500 g), FGR (birthweight of less than 10th percentile for gestation age), gestational diabetes, pre‐eclampsia or PIH, post‐partum haemorrhage, low Apgar scores (less than 7) at 1 and 5 min, and stillbirth.
A 30‐mL sample of early morning urine was collected from each women using a screw‐capped plastic bottle and then frozen at −70°C in the laboratory until analysis. Samples were analysed in batches of 20 samples at a time. The analysis was carried out using inductively coupled mass spectrometry (WHO, UNICEF, ICCIDD 2007). External quality control monitoring was performed by regular participation in Ensuring the Quality of Urinary Iodine Procedures, Centers of Disease Control and Prevention, United States of America.
Women recruited in the study were treated in routine standard antenatal care. The results of iodine status were not disclosed until the end of the study and were not used for any clinical decisions.
Statistical analysis
All statistical analyses were performed using SPSS version 21.0 (released 2012; IBM SPSS Statistics for Windows, IBM Corp., Armonk, NY, USA). The baseline characteristics of the pregnant women were compared using Student's t‐test for quantitative data and chi‐square for categorical variables. UICs in each trimester were compared using analysis of variance (repeated measures) test using linear mixed models: UIC as a dependent variable and trimester as a factor or repeated variable that was also used in fixed effect model. The associations of iodine status and adverse pregnancy outcomes were analysed using Pearson's chi‐square test. Multivariate binary logistic regression was performed to control the potential confounders such as age, parity, body mass index and the number of antenatal care visits, on unweighted data, to assess the amount to which iodine status might affect the odds of main pregnancy outcomes identified. In comparison with the gestational age at delivery between group with iodine sufficiency and insufficiency, given a mean difference of 1 week with standard deviation (SD) of 3 weeks, at 95% confidence interval (CI) and 80% power of test, the study needed at least 142 women per group. A P‐value of <0.05 was considered statistically significant.
Results
Of all 410 women recruited, 11 were excluded because of unavailability of the final outcomes (four cases) and receiving iodine supplementation (seven cases). The remaining 399 women with a total of 930 urinary samples were analysed for UICs. Median with interquartile range and mean (±SD) for each trimester are presented in Table 1. Notably, UICs were relatively low compared with the reference levels of adequacy (250–499 mcg L−1), and not significantly different among the three trimesters, although UICs had a tendency to be higher in the second and third trimester when compared with those in the first trimester (Fig. 1). The median of UICs throughout pregnancy was only 150.67 mcg L−1. The adequacy of iodine status in each trimester, categorized by WHO criteria, is presented in Table 2. Interestingly, based on the total number of collected samples, nearly half of all samples indicated iodine insufficiency and only approximately 2% showed excessive urinary iodine levels. Of 399 cases, if iodine status of each patient was represented by the means of their UICs derived from each trimester, 43.6% (174 women) had iodine insufficiency and 56.4% (225 women) had iodine sufficiency. The group with iodine sufficiency included a group of proper adequacy 43.4% (173), above requirement 12.0% (48) and excessive levels 1.0% (4). The complete data of pregnancy outcomes were available in 390 women, 171 in the group with iodine insufficiency and 219 in the group with iodine sufficiency. The baseline characteristics of women in the two groups were comparable as shown in Table 3. Frequencies of most pregnancy outcomes were not significantly different as presented in Table 4. Nevertheless, the rate of PTB was slightly but significantly higher among women with iodine insufficiency, 17.5% vs. 10.0%, relative risk of 1.75, P = 0.031. Consequently, the rate of LBW was significantly higher in the group with iodine insufficiency, 19.9% vs. 12.3%, relative risk of 1.61, P = 0.042. Accordingly, mean gestational age at delivery of women in the group with iodine insufficiency was slightly but significantly lower than in the group with iodine sufficiency (37.66 vs. 38.73 weeks, P < 0.001). Likewise, mean birthweight in the group with iodine insufficiency was significantly lower (2833 ± 565 vs. 3007 ± 620 g, P = 0.005). Interestingly, the rate of FGR was not significantly associated with iodine status. However, if severe iodine insufficiency was defined as UIC of lower than 100 mcg L−1, the rate of FGR was significantly higher in the group with iodine insufficiency, 13/68 (19.1%) vs. 30/322 (9.3%), relative risk 2.05 (95% CI: 1.13–3.72), P = 0.031.
Table 1.
Median (interquartile range: IQR) and mean (±SD) of the urinary iodine concentrations in each trimester derived from 930 samples of 399 women
| Trimester | n | Median | IQR | Mean | Standard deviation | ANOVA (repeated measures) |
|---|---|---|---|---|---|---|
| 1 | 384 | 147.39 | 99.42–202.26 | 164.37 | 98.16 | 0.092 |
| 2 | 325 | 157.01 | 99.83–224.13 | 181.83 | 138.07 | |
| 3 | 221 | 153.07 | 106.10–225.85 | 180.50 | 133.09 | |
| Total | 930 | 150.67 | 101.54–213.74 | 174.30 | 122.00 |
ANOVA, analysis of variance; SD, standard deviation.
Figure 1.
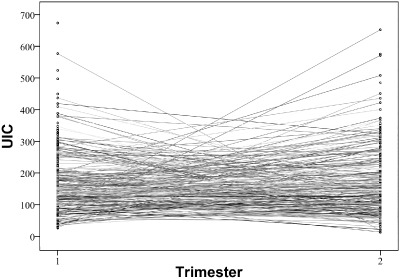
Scatter lines of urinary iodine levels of patients in the first and second trimester. UIC, urinary iodine concentration.
Table 2.
Adequacy of iodine status in each trimester based on the total number of 930 collected samples from 399 women
| Pattern of adequacy in each trimester | Number of cases (%) |
|---|---|
| Insufficiency in all trimesters | 82 (20.55%) |
| Insufficiency in the first two trimesters with dropout in the third trimester | 50 (12.53%) |
| Insufficiency in the first trimesters with dropout in the last two trimesters | 34 (8.52%) |
| Sufficiency in all trimesters | 103 (25.81%) |
| Sufficiency in the first two trimesters with dropout in the third trimester | 72 (18.05%) |
| Sufficiency in the first trimesters with dropout in the last two trimesters | 35 (8.77%) |
| Other patterns (sufficiency in one or two trimesters and insufficiency in the others, sufficiency in one trimester/insufficiency in another one and dropout in the other) | 23 (5.76%) |
Table 3.
Comparisons of baseline characteristics of pregnant women with iodine insufficiency and those with iodine sufficiency
| Insufficiency (n: 171) | Sufficiency (n: 219) | P‐value | |
|---|---|---|---|
| Maternal age (years) mean ± SD | 28.26 ± 5.50 | 28.13 ± 4.86 | 0.812 |
| Maternal BMI mean ± SD | 23.56 ± 2.98 | 23.34 ± 3.31 | 0.494 |
| Number of ANC visits mean ± SD | 10.64 ± 2.65 | 10.31 ± 3.42 | 0.288 |
| Gestational age (days) mean ± SD (first sampling) | 11.58 ± 4.36 | 11.30 ± 4.32 | 0.473 |
| Gestational age (week) mean ± SD (second sampling) | 18.68 ± 4.33 | 18.19 ± 4.05 | 0.063 |
| Gestational age (week) mean ± SD (third sampling) | 29.82 ± 5.34 | 29.43 ± 6.11 | 0.609 |
| Parity (nulliparous/multiparous) | 98/73 | 130/89 | 0.683 |
| Income (high/low) | 107/64 | 129/90 | 0.462 |
| Education (high/low) | 108/63 | 141/78 | 0.803 |
| Religion (Buddhism/others) | 165/6 | 202/17 | 0.077 |
| Medical disease (absence/presence) | 159/12 | 206/13 | 0.665 |
ANC, antenatal care; BMI, body mass index; SD, standard deviation.
Table 4.
Associations between iodine sufficiency and adverse pregnancy outcomes
|
Sufficiency n = 219; n (%) |
Insufficiency n = 171; n (%) |
RR (95% CI) |
P‐value | |
|---|---|---|---|---|
| Gestational week at birth (mean ± SD) | 38.73 ± 3.01 | 37.66 ± 2.35 | – | <0.001 |
| Birthweight (g) mean ± SD | 3006.64 ± 620.44 | 2833.15 ± 564.92 | – | 0.005 |
| Stillbirth |
7 (3.2%) |
2 (1.2%) |
0.37 (0.08–1.74) |
0.186 |
| IUGR |
20 (9.1%) |
23 (13.5%) |
1.47 (0.84–2.59) |
0.177 |
| Preterm birth |
22 (10.0%) |
30 (17.5%) |
1.75 (1.05–2.92) |
0.031 |
| LBW |
27 (12.3%) |
34 (19.9%) |
1.61 (1.02–2.57) |
0.042 |
| Low Apgar score 1 min |
29 (13.2%) |
15 (8.8%) |
0.66 (0.37–1.19) |
0.166 |
| Low Apgar score 5 min |
11 (5.0%) |
5 (2.9%) |
0.58 (0.21–1.64) |
0.300 |
| Antepartum haemorrhage |
4 (1.8%) |
6 (3.5%) |
1.92 (0.55–6.70) |
0.297 |
| PIH |
16 (7.3%) |
7 (4.1%) |
0.56 (0.24–1.33) |
0.181 |
| GDM |
15 (6.8%) |
21 (12.3%) |
1.79 (0.95–3.37) |
0.066 |
| Caesarean delivery |
53 (24.2%) |
41 (24.0%) |
0.99 (0.69–1.41) |
0.959 |
CI, confidence interval; GDM, gestational diabetes mellitus; IUGR, intrauterine growth restriction; LBW, low birthweight; PIH, pregnancy‐induced hypertension; RR, risk ratio; SD, standard deviation.
To further evaluate the association between iodine status and the rate of PTB as well as LBW, logistic regression analysis was performed to control other confounders as presented in Table 5. It was found that iodine status was an independent factor accounting for an increased risk of preterm delivery and LBW. Additionally, the number of antenatal care visits and occurrences of PIH was also a significant risk factor of PTB and LBW.
Table 5.
Adjusted odd ratios for the risk of preterm birth and low birthweight derived from logistic regression analysis
| Outcomes | Preterm birth (<37 week) | Low birthweight | |||
|---|---|---|---|---|---|
| Potential risk factors | n | P‐value | Adjusted odd ratios (95% CI) | P‐value | Adjusted odd ratios (95% CI) |
| Maternal age | 0.992 | 1.00 (0.934–1.07) | 0.083 | 0.95 (0.89–1.01) | |
| Number of ANC | <0.001 | 0.79 (0.71–0.87) | <0.001 | 0.78 (0.70–0.86) | |
| Inadequate | |||||
| Adequate | |||||
| Income | 0.570 | 0.81 (0.40–1.67) | 0.892 | 1.05 (0.53–2.08) | |
| High | 236 | ||||
| Low | 154 | ||||
| Education | 0.701 | 0.87 (0.42–1.80) | 0.688 | 1.15 (0.58–2.29) | |
| High | 249 | ||||
| Low | 141 | ||||
| Religion | 0.827 | 1.15 (0.32–4.19) | 0.517 | 1.52 (0.43–5.32) | |
| Buddhism | 367 | ||||
| Others | 23 | ||||
| Medical disease | 0.947 | 0.96 (0.26–3.52) | 0.282 | 0.43 (0.09–1.99) | |
| Present | 25 | ||||
| Absent | 365 | ||||
| PIH | 0.025 | 3.56 (1.17–10.80) | <0.001 | 7.19 (2.39–21.60) | |
| Present | 23 | ||||
| Absent | 367 | ||||
| APH | 0.621 | 1.53 (0.29–8.21) | 0.829 | 0.83 (0.14–4.73) | |
| Present | 10 | ||||
| Absent | 380 | ||||
| Iodine status | 0.004 | 2.69 (1.38–5.24) | 0.003 | 2.66 (1.40–5.05) | |
| Insufficiency | 171 | ||||
| Sufficiency | 219 | ||||
| Parity | 0.185 | 0.60 (0.29–1.27) | 0.005 | 0.35 (0.17–0.73) | |
| Nulliparous | 228 | ||||
| Multiparous | 162 | ||||
| BMI | 0.392 | 1.05 (0.94–1.16) | 0.337 | 1.05 (0.95–1.16) | |
ANC, antenatal care; APH, antepartum haemorrhage; BMI, body mass index; CI, confidence interval; PIH, pregnancy‐induced hypertension.
Discussion
Unlike other previous studies that focused on an association between maternal iodine status and fetal or neonatal thyroid function and neurological development, this study was aimed at identifying the prevalence of iodine insufficiency and its effect on adverse pregnancy outcomes. Based on this study, the prevalence of iodine insufficiency was higher than expected and it seemed unethical not to supplement iodine during pregnancy in this geographical area and it might be impossible to further conduct a study like this as we could not keep them un‐nourished ethically. The policy of universal salt iodization has been launched in Thailand for many years (ICCIDD 2009, 2013). However, our data indicated that the policy had not perfectly worked, although the reasons for such an observation remain unclear, and attention to this problem must be paid seriously.
The prevalence of maternal iodine insufficiency greatly varied from countries to countries. Therefore, each geographical area should have its own data that can lead to different approaches for widely control or national policy. For example, our study suggests the necessity of urgent solution for such a high rate of iodine insufficiency among pregnant women in the northern part of Thailand. This is due to the fact that other than adverse impact on pregnancy outcomes it has been established that maternal iodine insufficiency can have long‐term adverse impact on fetal neurological development (Cao et al. 1994; Delange 2001; Zimmermann 2011, 2012; Hynes et al. 2013), which could not be ameliorated by iodine supplementation during childhood. Note that our conventional antenatal care did not routinely supplement iodine to pregnant women and the women who took iodine supplementation were excluded from analysis. Therefore, the iodine status in this study might not represent the true status of all our obstetric population. Nevertheless, high percentage of women with iodine insufficiency in this study could reflect the baseline of iodine status in our population and indicates that guidelines for iodine intake and monitoring during pregnancy are needed.
Some previous studies indirectly suggested that iodine insufficiency may adversely affect birthweight or fetal growth (Zimmermann 2011; Pearce 2012). In China, Cao et al. (1994) reported reduction in the rate of microcephaly from 27% to 11% with iodine repletion of pregnant women with severe iodine insufficiency. In Algeria, Chaouki & Benmiloud (1994) reported that oral administration of lipiodol before or during the first trimester of pregnancy normalized thyroid function in newborn babies and mothers, increased placental and birthweight, and reduced the frequency of iodine insufficiency. In Spain, Alvarez‐Pedrerol et al. (2009) suggested that iodine status during pregnancy might be related to prenatal growth in healthy women, in particular the babies of mothers with urinary iodine below 50 mcg L−1. Nevertheless, there have been some conflicting data. Mason et al. (2002) reported that the use of iodated salt was related to birthweight in Sri Lanka and in the Philippines, where iodized oil capsules given during pregnancy had a negative effect when used with high levels of iodine in salt. To the best of our knowledge, the impact of maternal iodine insufficiency on adverse pregnancy outcomes other than thyroid problems is still inconclusive. Unlike previous reports, this study suggested that iodine insufficiency might have minimal effect on fetal growth but it could rather predispose to PTB and LBW. We have noted that a significantly higher rate of FGR was observed only when UIC was lower than 100 mcg L−1. However, it is possible that insufficiency of other nutritional factors, which possibly tended to be more prevalent among women with iodine insufficiency, might have confounded and accounted for such adverse outcomes.
The weakness of this study might include (1) no evaluation of other nutritional factors apart from iodine, which could have been confounders for adverse pregnancy outcomes; (2) neither assessment of fetal and neonatal thyroid function nor long‐term follow‐up for neurological development. The strength of this study included (1) adequate sample size of the cases with iodine insufficiency to assess the adverse pregnancy outcomes, although the total number of cases did not seem to be large; (2) prospective nature of the cohort study, together with the fact that the results of iodine status were blinded to the doctors who assessed the pregnancy outcomes; and (3) the measurement of the UIC was based on a highly reliable laboratory methods.
In conclusion, this study provides insights on iodine status during pregnancy as follows: (1) in northern Thailand, a great number of pregnant women who were not taking iodine supplements had a median UIC less than 150 mcg L−1; (2) urinary iodine levels had a tendency to increase during the second trimester, when compared with those in the first trimester, although not significantly different; (3) iodine insufficiency was associated with an increased risk of PTB as well as LBW; (4) severe iodine insufficiency (<100 mcg L−1) increased the risk of FGR, although such an effect was probably minimal; and finally (5) iodine insufficiency was unlikely to increase the risk of other common adverse pregnancy outcomes such as PIH or antepartum haemorrhage.
Source of funding
This study was funded by the National Research University Project under Thailand's Office of the Higher Education Commission and the Diamond Research Grant of Faculty of Medicine, Chiang Mai University.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
CC: Proposal development, Data collection, Manuscript writing. PL: Laboratory analysis (urinary iodine concentration measurements). KT: Proposal development, Data collection. TT: Data analysis, Manuscript editing.
Charoenratana, C. , Leelapat, P. , Traisrisilp, K. , and Tongsong, T. (2016) Maternal iodine insufficiency and adverse pregnancy outcomes. Maternal & Child Nutrition, 12: 680–687. doi: 10.1111/mcn.12211.
References
- Alvarez‐Pedrerol M., Guxens M., Mendez M., Canet Y., Martorell R., Espada M. et al (2009) Iodine levels and thyroid hormones in healthy pregnant women and birth weight of their offspring. European Journal of Endocrinology 160, 423–429. [DOI] [PubMed] [Google Scholar]
- Boyages S.C. (1993) Clinical review 49: iodine deficiency disorders. The Journal of Clinical Endocrinology and Metabolism 77, 587–591. [DOI] [PubMed] [Google Scholar]
- Cao X.Y., Jiang X.M., Dou Z.H., Rakeman M.A., Zhang M.L., O'Donnell K. et al (1994) Timing of vulnerability of the brain to iodine deficiency in endemic cretinism. The New England Journal of Medicine 331, 1739–1744. [DOI] [PubMed] [Google Scholar]
- Chaouki M.L. & Benmiloud M. (1994) Prevention of iodine deficiency disorders by oral administration of lipiodol during pregnancy. European Journal of Endocrinology 130, 547–551. [DOI] [PubMed] [Google Scholar]
- Delange F. (2001) Iodine deficiency as a cause of brain damage. Postgraduate Medical Journal 77, 217–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetzel B.S. (1983) Iodine deficiency disorders (IDD) and their eradication. Lancet 2, 1126–1129. [DOI] [PubMed] [Google Scholar]
- Hynes K.L., Otahal P., Hay I. & Burgess J.R. (2013) Mild iodine deficiency during pregnancy is associated with reduced educational outcomes in the offspring: 9‐year follow‐up of the gestational iodine cohort. The Journal of Clinical Endocrinology and Metabolism 98, 1954–1962. [DOI] [PubMed] [Google Scholar]
- ICCIDD (2009) Tracking Progress: Towards Sustainable Elimination of Iodine Deficiency Disorders in Thailand. International Council for the Control of Iodine Deficiency Disorders (ICCIDD), Keen Media (Thailand) Co., Ltd.: Thailand. [Google Scholar]
- ICCIDD (2013). Thailand Makes Progress in Elimination of IDD. Sona Printers Pvt. Ltd: New Delhi, India. [Google Scholar]
- Mason J.B., Deitchler M., Gilman A., Gillenwater K., Shuaib M., Hotchkiss D. et al (2002) Iodine fortification is related to increased weight‐for‐age and birthweight in children in Asia. Food and Nutrition Bulletin 23, 292–308. [DOI] [PubMed] [Google Scholar]
- Pearce E.N. (2012) Effects of iodine deficiency in pregnancy. Journal of Trace Elements in Medicine and Biology: Organ of the Society for Minerals and Trace Elements (GMS) 26, 131–133. [DOI] [PubMed] [Google Scholar]
- Pearce E.N. (2013) Monitoring and effects of iodine deficiency in pregnancy: still an unsolved problem? European Journal of Clinical Nutrition 67, 481–484. [DOI] [PubMed] [Google Scholar]
- Stagnaro‐Green A., Sullivan S. & Pearce E.N. (2012) Iodine supplementation during pregnancy and lactation. JAMA: The Journal of the American Medical Association 308, 2463–2464. [DOI] [PubMed] [Google Scholar]
- WHO, UNICEF, ICCIDD (2007) Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination, 3rd edn World Health Organization: Geneva. [Google Scholar]
- Zimmermann M.B. (2009) Iodine deficiency. Endocrine Reviews 30, 376–408. [DOI] [PubMed] [Google Scholar]
- Zimmermann M.B. (2011) The role of iodine in human growth and development. Seminars in Cell and Developmental Biology 22, 645–652. [DOI] [PubMed] [Google Scholar]
- Zimmermann M.B. (2012) The effects of iodine deficiency in pregnancy and infancy. Paediatric and Perinatal Epidemiology 26 (Suppl. 1), 108–117. [DOI] [PubMed] [Google Scholar]
- Zimmermann M.B. & Andersson M. (2012) Update on iodine status worldwide. Current Opinion in Endocrinology, Diabetes, and Obesity 19, 382–387. [DOI] [PubMed] [Google Scholar]


