Abstract
Published literatures report controversial results about the association of folic acid–containing multivitamins with gestational hypertension and pre‐eclampsia. A comprehensive search was performed to identify related prospective studies to assess the effect of folic acid fortification on gestational hypertension and pre‐eclampsia. The Q test and I2 statistic were used to examine between‐study heterogeneity. Fixed or random effects models were selected based on study heterogeneity. A funnel plot and modified Egger linear regression test were used to estimate publication bias. Eleven studies conformed to the criteria. Pooled results indicated that folic acid fortification alone was not associated with the occurrence of gestational hypertension [relative risk (RR) = 1.03, 95% confidence interval (CI): 0.98–1.09, P = 0.267] and pre‐eclampsia (RR = 0.99, 95% CI: 0.90–1.08, P = 0.738). However, supplementation of multivitamins containing folic acid could prevent gestational hypertension (RR = 0.57, 95% CI: 0.43–0.76, P < 0.001) and pre‐eclampsia (RR = 0.64, 95% CI: 0.48–0.84, P = 0.001). The difference between folic acid fortification alone and multivitamins containing folic acid was significant. This meta‐analysis suggests that periconceptional multivitamin supplementation with appropriate dose, not folic acid alone, is an appropriate recommendation for pregnant women. The effect should be further confirmed by conducting large‐scale randomised controlled trials.
Keywords: folic acid, multivitamins, gestational hypertension, pre‐eclampsia, meta‐analysis
Introduction
Gestational hypertension and pre‐eclampsia are the most common hypertensive disorders associated with pregnancy. Ten per cent of women have high blood pressure during pregnancy, and pre‐eclampsia complicates 2–8% of pregnancies (Duley 2009). They are also major causes of maternal and perinatal morbidity and mortality worldwide (World Health Organization 2005). Hypertension in pregnancy is also associated with an increased risk for subsequent cardiovascular disease or diabetes mellitus later in life (Feig et al. 2013; Charlton et al. 2014; Cusimano et al. 2014). Identifying and characterising modifiable risk factors of gestational hypertension and pre‐eclampsia remain important for public health and clinical medicine.
In the past decades, many research studies have focused on periconceptional folic acid fortification as a gestational hypertension or pre‐eclampsia preventive factor. Further findings from these studies showed that there is a significant elevation in plasma or serum homocysteine among women with gestational hypertension or pre‐eclampsia in pregnancy; thus, homocysteine may be an independent risk factor for these disorders (Cotter et al. 2003; Makedos et al. 2007; Dodds et al. 2008; Murphy & Fernandez‐Ballart 2011; Bergen et al. 2012). Hyperhomocysteinaemia can usually be ameliorated by folic acid supplementation (Maron & Loscalzo 2009; Scorsatto et al. 2011; Sudchada et al. 2012; Yamamoto et al. 2012). Thus, a research hypothesis was formed on that administering of folic acid–containing multivitamins can help prevent the occurrence of gestational hypertension or pre‐eclampsia. In addition, a number of extensive evidence have demonstrated that adequate folate intake protects against neural tube defects; hence, folic acid fortification became a general recommendation for pregnant women (Ray & Mamdani 2002; Ray et al. 2002; De Wals et al. 2007). The associations between folic acid fortification and other pregnancy outcomes, such as gestational hypertension and pre‐eclampsia, has become a research hot spot. Numerous epidemiological studies have explored the influence of folic acid supplementation on gestational hypertension and pre‐eclampsia. However, their reported results are inconsistent (Bukowski et al. 2009; Catov et al. 2009; Timmermans et al. 2011; Li et al. 2013; Vanderlelie et al. 2014). Individual studies could not draw solid conclusions, and no meta‐analysis to explore the effect of folic acid fortification on gestational hypertension and pre‐eclampsia has been conducted. Thus, we performed this meta‐analysis of prospective studies to assess whether periconceptional folic acid fortification for pregnant women is associated with a decreased risk of subsequent gestational hypertension and pre‐eclampsia.
Key messages.
Folic acid fortification alone did not prevent gestational hypertension.
Multivitamins containing folic acid were associated with reduced risk of gestational hypertension.
Folic acid fortification alone did not prevent pre‐eclampsia.
Multivitamins containing folic acid were associated with reduced risk of pre‐eclampsia.
The stable result and optimal dose for multivitamins should be further estimated.
Materials and methods
The meta‐analysis of observational studies in epidemiology (MOOSE) guidelines were followed (Stroup et al. 2000).
Search strategy
Studies were identified using a search strategy in the PubMed, Scopus, Web of Science and Cochrane library to 8 December 2014. Search items were listed as follows: (gestational hypertension OR pregnancy‐induced hypertension OR hypertension of pregnancy OR preeclampsia OR pre‐eclampsia OR eclampsia) AND (folic acid OR folate OR micronutrient* OR vitamin* OR multivitamin*). Moreover, we reviewed the reference lists from retrieved articles to search for further relevant studies. When same data were reported in more than one publication, only studies with more complete data and more extensive interval of enrolment were included in the study.
Eligibility criteria
Each selected study was independently reviewed by two investigators (Yang and Chen) to determine whether it was eligible for inclusion in this meta‐analysis. The inclusion criteria were as follows: (1) prospective study; (2) exposure of interest was folic acid or multivitamins containing folic acid; (3) outcome of interest was gestational hypertension or pre‐eclampsia; (4) results with 95% confidence interval (CI; or data to calculate them) adjusted for confounding factors were provided; (5) no restriction in publication date, publication language and publication status; and (6) animal studies, reviews, comments and editorials were excluded. Any disagreement was settled by discussion.
Data extraction and quality assessment
A data extraction sheet was developed that included first author, publication year, country where the study was conducted, characteristics of study population, number of total participants, number of total events, the folic acid fortification start time, study results with 95% CI for folic acid on gestational hypertension or pre‐eclampsia, and adjusted confounding factors. All data were extracted independently by two reviewers (Yang and Chen). In cases of disagreement between the two reviewers, a consensus was achieved through discussion among all of the authors. The 9‐star Newcastle–Ottawa Scale (Wells et al. 2000) was used to estimate the quality of each selected prospective study.
Statistical analysis
The type of folic acid fortification was categorised into two groups, namely folic acid fortification alone and multivitamins containing folic acid. Pooled measure was calculated as the inverse variance‐weighted mean of the logarithm of relative risks (RRs) with 95% CI to assess the effect of folic acid fortification on gestational hypertension and pre‐eclampsia. The Q test and I 2 were used to assess heterogeneity among the included studies (Higgins & Thompson 2002). In the presence of substantial heterogeneity (I 2 > 50%) (Higgins et al. 2003), the DerSimonian and Laird random effect model (REM) was adopted as the pooling method; otherwise, the fixed effect model (FEM) was used as the pooling method. Meta‐regression with restricted maximum likelihood estimation was performed to assess the potentially important covariates exerting substantial impact on between‐study heterogeneity. Subgroup analysis for the type of folic acid fortification was further explored. The ‘leave one out’ sensitive analysis was carried out using I 2 > 50% as the criteria to evaluate the key studies with substantial impact on between‐study heterogeneity (Patsopoulos et al. 2008). An influence analysis was conducted to describe how robust the pooled estimator was (Tobias 1999). Publication bias was estimated using Egger's regression asymmetry test (Egger et al. 1997). All statistical analyses were performed with STATA version 13.1 (Stata Corporation, College Station, TX, USA). All reported probabilities (P‐value) were two‐sided, and less than 0.05 was considered statistically significant.
Results
Study characteristics
The detailed selection process was illustrated in Fig. 1 and we ultimately identified 11 eligible articles (Hernandez‐Diaz et al. 2002; Ray & Mamdani 2002; Merchant et al. 2005; Oken et al. 2007; Wen et al. 2008; Bukowski et al. 2009; Catov et al. 2009; Timmermans et al. 2011; Li et al. 2013; Vanderlelie et al. 2014) out of 3942 articles for this meta‐analysis. Among them, one was a prospective clinical trial (Merchant et al. 2005) and the rest were prospective observational studies. The total eligible pregnant women numbered 1 276 063 persons, out of which 78 105 cases of gestational hypertension and 44 608 cases of pre‐eclampsia occurred during pregnancy. Two studies (Catov et al. 2009; Timmermans et al. 2011) reported separate outcomes for folic acid fortification start time. General characteristics of the included studies were shown in Table 1. Of these studies, six were conducted in North America, two in Europe, one in China, one in Australia and one in Tanzania. All included studies met the quality criteria with scores ranging from 7 to 9 stars.
Figure 1.

Flow diagram of studies selection in the meta‐analysis.
Table 1.
Description of the prospective studies included in the meta‐analysis
| Author (year) | Country | Total samples | Mean age | Exposure | Time | Disease | Cases | RR (95% CI) | Quality | Adjusted factors |
|---|---|---|---|---|---|---|---|---|---|---|
| Hernandez‐Diaz et al. (2002) | United States and Canada | 2 151 | 29.3 | MvFa | Precon | GH | 157 | 0.53 (0.36–0.80) | 7 | Geographic region, family income, age, prepregnancy weight, parity, twin pregnancy, diabetes, smoking and education |
| PE | 47 | 0.63 (0.28–1.45) | ||||||||
| Ray et al. (2002) | Canada | 1 001 441 | 28.9 | Fa | Precon | GH | 58965 | 0.98 (0.95–1.01) | 7 | Age and year of delivery |
| PE | 37880 | 0.94 (0.91–0.97) | ||||||||
| Merchant et al. (2005) | Tanzania | 1 078 | 24.7 | MvFa | Postcon | GH | 89 | 0.62 (0.40–0.94) | 8 | Randomisation, adjusted for all possible confounders |
| Bodnar et al. (2006) | United States | 1 835 | 24.7 | MvFa | Pericon | PE | 75 | 0.55 (0.32–0.95) | 8 | Race, marital status, parity, preconceptional physical activity, and poverty index ratio |
| Oken et al. (2007) | United States | 1 718 | 31.2 | Fa | Postcon | GH | 119 | 1.02 (0.99–1.06) | 8 | Age, BMI, first‐trimester systolic blood pressure, race, education, and parity, total energy intake |
| PE | 59 | 0.96 (0.89–1.03) | ||||||||
| Wen et al. (2008) | Canada | 2 951 | 32.2 | Fa | Postcon | PE | 71 | 0.46 (0.16–1.31) | 8 | Age, ethnicity, education, parity, history of pre‐eclampsia, chronic hypertension, diabetes, BMI, household income, gestational age at recruitment and smoking |
| MvFa | 0.37 (0.18–0.75) | |||||||||
| Bukowski et al. (2009) | United States | 34 480 | 30.0 | Fa | Precon | PE | 883 | 1.04 (0.90–1.19) | 9 | Age, BMI, race and ethnicity, education, marital status, smoking, parity and history of prior preterm birth |
| Catov et al. (2009) | Denmark | 28 601 | 29.4 | MvFa | Precon | PE | 668 | 0.88 (0.70–1.10) | 9 | BMI, smoking, parity, chronic hypertension, gestational age at recruitment and partial multivitamin use |
| Postcon | 0.74 (0.56–0.98) | |||||||||
| Timmermans et al. (2011) | The Netherlands | 5 993 | 29.9 | Fa | Postcon | GH | 301 | 1.40 (0.90–2.10) | 8 | Age, gestational age at time of measurement, BMI, parity, ethnicity, education, smoking, alcohol antenatal care |
| Precon | 1.10 (0.70–1.70) | |||||||||
| Postcon | PE | 125 | 0.90 (0.50–1.30) | |||||||
| Precon | 0.80 (0.50–1.40) | |||||||||
| Li et al. (2013) | China | 193 554 | 24.9 | Fa | Postcon | GH | 18474 | 1.08 (1.04–1.11) | 9 | Age, BMI, education, occupation, parity and multiple births |
| PE | 4756 | 1.11 (1.04–1.18) | ||||||||
| Vanderlelie et al. (2014) | Australia | 2 261 | 28.2 | Fa | Postcon | PE | 44 | 0.42 (0.13–0.98) | 8 | Age, parity, gestational diabetes, indigenous status and maternal smoking |
| MvFa | 0.33 (0.14–0.75) |
BMI, body mass index; CI, confidence interval; Fa, folic acid fortification; GH; gestational hypertension; MvFa, multivitamins containing folic acid; PE, pre‐eclampsia; Pericon, periconception; Postcon, post‐conception; Precon, preconception; RR, relative risk; Time, the starting time of folic acid fortification.
Quantitative synthesis
Folic acid fortification on gestational hypertension
The association of folic acid fortification with gestational hypertension was presented in Fig. 2. Pooled results indicated that the improvement of folic acid alone was not associated with the occurrence of gestational hypertension (REM: RR = 1.03, 95% CI: 0.98–1.09, P = 0.267), but supplementation of multivitamins containing folic acid was associated with a decreased risk of gestational hypertension (FEM: RR = 0.57, 95% CI: 0.43–0.76, P < 0.001). The categorised difference was statistically significant (P = 0.012).
Figure 2.
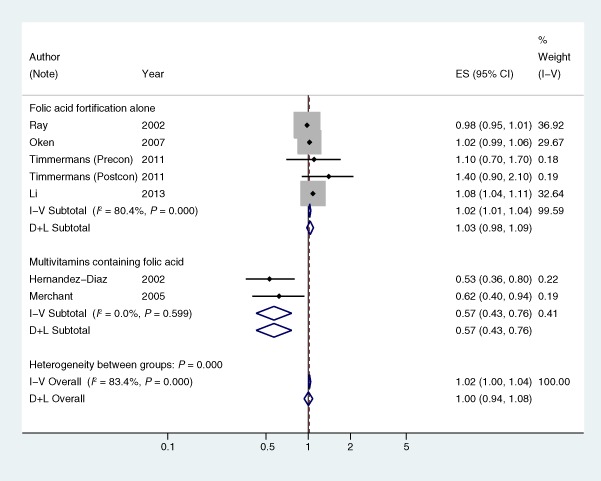
Forest plot of RR of the association between folic acid fortification and gestational hypertension. Postcon, post‐conception; Precon, preconception; RR, relative risk.
Folic acid fortification on pre‐eclampsia
The REM was applied because I 2 of between‐study heterogeneity was more than 50%. The association between folic acid fortification and pre‐eclampsia was presented in Fig. 3. Pooled results indicated that the improvement of folic acid alone was not associated with pre‐eclampsia (REM: RR = 0.99, 95% CI: 0.90–1.08, P = 0.738), but supplementation of multivitamins containing folic acid could decrease the risk of pre‐eclampsia (REM: RR = 0.64, 95% CI: 0.48–0.84, P = 0.001). The categorised difference was significant (P = 0.020).
Figure 3.
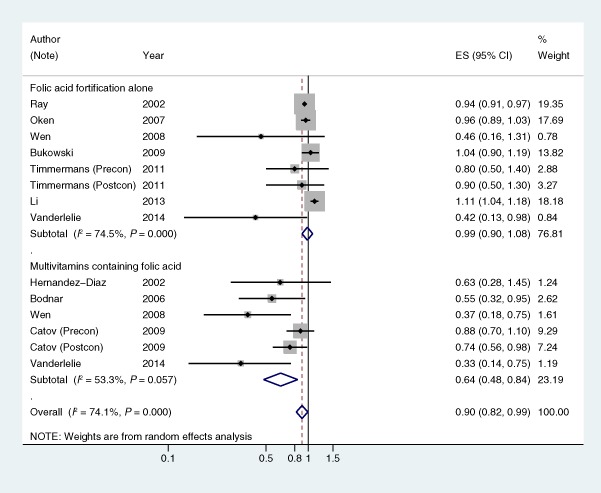
Forest plot of RR of the association between folic acid fortification and pre‐eclampsia. Postcon, post‐conception; Precon, preconception; RR, relative risk.
Sources of heterogeneity and sensitivity analysis
The between‐study heterogeneity (I 2 > 50%) could be found among nearly all analyses except for multivitamins containing folic acid and gestational hypertension. The univariate meta‐regression, with the covariates of folic acid fortification start time (preconception and post‐conception), published year, location (categorised as North America, European and Other), maternal body mass index (BMI) (adjusted and non‐adjusted), mean age, sample size and study quality, showed that no aforementioned covariates had a significant impact on between‐study heterogeneity.
In the sensitivity analysis, Li et al.'s (2013) study was the key contributor to between‐study heterogeneity for folic acid fortification alone on gestational hypertension and pre‐eclampsia, and Catov et al.'s (2009) study for multivitamins containing folic acid on pre‐eclampsia. After excluding the two studies, the meta‐analysis showed a modest protective effect of folic acid intake on pre‐eclampsia (FEM: RR = 0.95, 95% CI: 0.92–0.97, P < 0.001). The other two pooled results did not change substantially.
Influence and publication bias analyses
Both before and after excluding the two studies as the key contributors to between‐study heterogeneity, no individual study was found to have excessive influence on the pooled effect. Before excluding the Catov's study, significant publication bias was found in the multivitamins containing folic acid on pre‐eclampsia studies (P = 0.014). The trim and fill analysis showed that multivitamins containing folic acid still reduced the risk of pre‐eclampsia (REM: RR = 0.67, 95% CI: 0.51–0.89, P = 0.006). No significant publication bias was observed in any other analyses, both before and after excluding the two studies identified as the key contributors to between‐study heterogeneity.
Discussion
To the best of our knowledge, this study is the first meta‐analysis conducted to specifically investigate the association of folic acid fortification with incidence of gestational hypertension and pre‐eclampsia. The results of this study indicated that folic acid fortification alone did not prevent the occurrence of gestational hypertension and pre‐eclampsia. However, the results suggested that supplementation of multivitamins containing folic acid could reduce the risk of gestational hypertension and pre‐eclampsia.
In this meta‐analysis, between‐study heterogeneity was found among some groups based on the tentative categorisation of I 2 values (Higgins et al. 2003). An indeterminate number of characteristics that varied among studies (such as starting time of folic acid fortification, maternal BMI, published year, ethnicity, age, sample size and quality) could be the sources of between‐study heterogeneity. Therefore, we applied meta‐regression and ‘leave one out’ sensitivity analysis to explore the potential important causes of between‐study heterogeneity for both covariates and studies. Our meta‐analysis did not identify any of the aforementioned covariates as being an important contributor to between‐study heterogeneity. The aetiology of gestational hypertension and pre‐eclampsia is complex and unclear (Roberts et al. 2003). Although the aforementioned covariates were not found to be important sources of disease–effect heterogeneity across the studies in this meta‐analysis, other variables, as well as their possible interaction, may well be potential contributors to this disease–effect unconformity. In this respect, the lack of relevant study‐level covariates in the reported articles precluded a more robust assessment of sources of this heterogeneity.
In the ‘leave one out’ sensitivity analysis, two studies (Catov et al. 2009; Li et al. 2013) were identified as being possible key contributors to between‐study heterogeneity. After carefully evaluating the two studies, they were entirely appropriate for the current meta‐analysis, except for the potential ethnic difference. We did not advise excluding the two studies.
Although publication bias was detected in the multivitamins containing folic acid on pre‐eclampsia studies, the trim and fill analysis showed that multivitamins containing folic acid still reduced the risk of pre‐eclampsia. No significant influence and publication bias were observed in the other analyses.
The mechanism in folic acid preventing cardiovascular disease focuses on its critical role in lowering plasma homocysteine, which is found to be associated with a higher risk of cardiovascular disease from epidemiological studies (Moat et al. 2004). Many studies in the past decades show that women with gestational hypertension or pre‐eclampsia have a significant elevation of homocysteine post‐partum, in the third trimester, in the second trimester or even in early pregnancy (Cotter et al. 2003; Makedos et al. 2007; Dodds et al. 2008; Murphy & Fernandez‐Ballart 2011; Bergen et al. 2012). Taking this emerging evidence into consideration, in combination with other data implicating hyperhomocysteinaemia as an independent risk factor for vascular disease, some researchers hypothesised that hyperhomocysteinaemia may be an independent risk factor for gestational hypertension (Roberts & Cooper 2001). However, recent trials have failed to demonstrate a benefit of lowering homocysteine for cardiovascular disease (Albert et al. 2008; Ebbing et al. 2010). Steegers‐Theunissen et al. (2004) contend that, in most cases, hyperhomocysteinaemia may be a consequence rather than a cause of hypertensive disorders in pregnancy. Folic acid fortification can effectively decrease homocysteine (Maron & Loscalzo 2009; Scorsatto et al. 2011; Sudchada et al. 2012; Yamamoto et al. 2012). Thus, theoretically, if elevated homocysteine is a cause of gestational hypertension or pre‐eclampsia, periconceptional folic acid fortification may significantly decrease the incidence of these outcomes. However, our study results did not find a protective effect of folic acid supplementation alone on gestational hypertension or pre‐eclampsia, but rather, multivitamins containing folic acid could reduce the risk of gestational hypertension and pre‐eclampsia.
Some possible reasons for the current outcome include the following. Firstly, some ingredients in multivitamins may play important roles in preventing gestational hypertension and pre‐eclampsia. For instance, either maternal vitamin B6 or vitamin D deficiency is an independent risk factor for pre‐eclampsia (Thaver et al. 2006; Hovdenak & Haram 2012; Bodnar et al. 2014; Brodowski et al. 2015). Secondly, the joint effect of multivitamins, such as folic acid, vitamins B6 and B12, may synergistically affect the development of hypertension. For example, a recent meta‐analysis indicated that folic acid supplementation has no significant effect on revascularisation, but a combination of folic acid and vitamin B6 may be beneficial for revascularisation (Qin et al. 2014). Thirdly, with the development of modern society and the implementation of mandatory folic acid fortification since 1998, the folic acid demand during pregnancy may be supplied adequately from dietary intake of folic acid (Lawrence et al. 1999, Global Progress 2013). A dose–response study showed that the decrease of plasma homocysteine achieved with more than 600 μg day–1 folic acid was not obvious (Van Oort et al. 2003). Thus, when folic acid supplement is adequate, its effect for gestational hypertension and pre‐eclampsia may be not significant. Although our study implied that periconceptional multivitamins containing folic acid supplementation could reduce the risk of gestational hypertension and pre‐eclampsia, the potential adverse effects, such as early fetal death (Nohr et al. 2014), should be considered in clinical application for multivitamin supplementation. Therefore, large‐scale randomised controlled trials with appropriate dose at appropriate times during pregnancy are recommended to estimate the impact of multivitamins containing folic acid supplement on pregnant women.
Strengths and weaknesses
This meta‐analysis had several strengths. This study included prospective studies to determine the risk of gestational hypertension and pre‐eclampsia over time. It also had a large sample size and our included studies were adjusted for potential confounding, which increased the accuracy of the effect estimate. However, the potential limitations of this meta‐analysis should be considered. Firstly, exposures cited by the included studies were mainly folic acid supplement rather than the real folic acid intake and the vitamins' dose varied in each study, which may influence the pooled estimated value. Secondly, although significant protective function of multivitamin containing folic acid on gestational hypertension and pre‐eclampsia was found, the recurring result should be confirmed in the future, for a few samples included. Thirdly, strong heterogeneity was observed in our study. Although we applied meta‐regression and sensitive analysis to explore it, the source of heterogeneity was not determined. Fourthly, due to our inability to obtain raw data, we could only perform a study‐level but not a patient‐level meta‐analysis, which would have enabled us to control some confounders, such as maternal BMI, smoking, physical activity. Lastly, the different subtypes and definitions of gestational hypertension or pre‐eclampsia may affect the pooled estimated result.
Conclusion
This meta‐analysis suggested that periconceptional multivitamins containing folic acid supplementation could reduce the risk of gestational hypertension and pre‐eclampsia, whereas folic acid fortification alone did not prevent the occurrence of gestational hypertension and pre‐eclampsia. Large‐scale randomised controlled trials are recommended to confirm the impact of multivitamins containing folic acid supplement on the incidence rates of gestational hypertension and pre‐eclampsia during pregnancy.
Source of funding
None.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
XY performed the literature searches, study selection, data extraction, data analyses, data interpretation and wrote the initial draft of the manuscript. HC involved in literature searches, study selection, data extraction, data analyses. YD and SW solved disagreements regarding study selection and risk of bias assessment, and critically revised the article. ZW contributed to the study design, interpreted the data and revised the initial draft. All authors contributed to the editing of the final version of the manuscript.
Yang, X. , Chen, H. , Du, Y. , Wang, S. , and Wang, Z. (2016) Periconceptional folic acid fortification for the risk of gestational hypertension and pre‐eclampsia: a meta‐analysis of prospective studies. Maternal & Child Nutrition, 12: 669–679. doi: 10.1111/mcn.12209.
References
- Albert C.M., Cook N.R., Gaziano J.M., Zaharris E., MacFadyen J., Danielson E. et al (2008) Effect of folic acid and B vitamins on risk of cardiovascular events and total mortality among women at high risk for cardiovascular disease: a randomized trial. JAMA: The Journal of the American Medical Association 299, 2027–2036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergen N.E., Jaddoe V.W.V., Timmermans S., Hofman A., Lindemans J., Russcher H. et al (2012) Homocysteine and folate concentrations in early pregnancy and the risk of adverse pregnancy outcomes: the Generation R study. British Journal of Obstetrics and Gynaecology 199, 739–751. [DOI] [PubMed] [Google Scholar]
- Bodnar L.M., Tang G., Ness R.B., Harger G. & Roberts J.M. (2006) Periconceptional multivitamin use reduces the risk of preeclampsia. American Journal of Epidemiology 164, 470–477. [DOI] [PubMed] [Google Scholar]
- Bodnar L.M., Simhan H.N., Catov J.M., Roberts J.M., Platt R.W., Diesel J.C. et al (2014) Maternal vitamin D status and the risk of mild and severe preeclampsia. Epidemiology (Cambridge, Mass.) 25, 207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodowski L., Burlakov J., Hubel C.A. & von Versen‐Höynck F. (2015) [256‐POS]: vitamin D restores functional abilities of fetal endothelial progenitor cells from pregnancies complicated by preeclampsia. Pregnancy Hypertension 5, 129. [Google Scholar]
- Bukowski R., Malone F.D., Porter F.T., Nyberg D.A., Comstock C.H., Hankins G.D. et al (2009) Preconceptional folate supplementation and the risk of spontaneous preterm birth: a cohort study. PLoS Medicine 6, e1000061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catov J.M., Nohr E.A., Bodnar L.M., Knudson V.K., Olsen S.F. & Olsen J. (2009) Association of periconceptional multivitamin use with reduced risk of preeclampsia among normal‐weight women in the Danish National Birth Cohort. American Journal of Epidemiology 169, 1304–1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlton F., Tooher J., Rye K.A. & Hennessy A. (2014) Cardiovascular risk, lipids and pregnancy: preeclampsia and the risk of later life cardiovascular disease. Heart, Lung and Circulation 23, 203–212. [DOI] [PubMed] [Google Scholar]
- Cotter A.M., Molloy A.M., Scott J.M. & Daly S.F. (2003) Elevated plasma homocysteine in early pregnancy: a risk factor for the development of nonsevere preeclampsia. American Journal of Obstetrics and Gynecology 189, 391–394, discussion 394–396. [DOI] [PubMed] [Google Scholar]
- Cusimano M.C., Pudwell J., Roddy M., Cho C.K. & Smith G.N. (2014) The maternal health clinic: an initiative for cardiovascular risk identification in women with pregnancy‐related complications. American Journal of Obstetrics and Gynecology 210, 438.e1–438.e9. [DOI] [PubMed] [Google Scholar]
- De Wals P., Tairou F., Van Allen M.I., Uh S.H., Lowry R.B., Sibbald B. et al (2007) Reduction in neural‐tube defects after folic acid fortification in Canada. The New England Journal of Medicine 357, 135–142. [DOI] [PubMed] [Google Scholar]
- Dodds L., Fell D.B., Dooley K.C., Armson B.A., Allen A.C., Nassar B.A. et al (2008) Effect of homocysteine concentration in early pregnancy on gestational hypertensive disorders and other pregnancy outcomes. Clinical Chemistry 54, 326–334. [DOI] [PubMed] [Google Scholar]
- Duley L. (2009) The global impact of pre‐eclampsia and eclampsia. Seminars in Perinatology 33, 130–137. [DOI] [PubMed] [Google Scholar]
- Ebbing M., Bonaa K.H., Arnesen E., Ueland P.M., Nordrehaug J.E., Rasmussen K. et al (2010) Combined analyses and extended follow‐up of two randomized controlled homocysteine‐lowering B‐vitamin trials. Journal of Internal Medicine 268, 367–382. [DOI] [PubMed] [Google Scholar]
- Egger M., Davey Smith G., Schneider M. & Minder C. (1997) Bias in meta‐analysis detected by a simple, graphical test. BMJ (Clinical Research Ed.) 315, 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feig D.S., Shah B.R., Lipscombe L.L., Wu C.F., Ray J.G., Lowe J. et al (2013) Preeclampsia as a risk factor for diabetes: a population‐based cohort study. PLoS Medicine 10, e1001425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global Progress (2013) Flour Fortification Initiative website. Flour Fortificatoin Initiative. Available at: http://www.ffinetwork.org/global_progress/ (Accessed 30 December 2014).
- Hernandez‐Diaz S., Werler M.M., Louik C. & Mitchell A.A. (2002) Risk of gestational hypertension in relation to folic acid supplementation during pregnancy. American Journal of Epidemiology 156, 806–812. [DOI] [PubMed] [Google Scholar]
- Higgins J.P. & Thompson S.G. (2002) Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine 21, 1539–1558. [DOI] [PubMed] [Google Scholar]
- Higgins J.P., Thompson S.G., Deeks J.J. & Altman D.G. (2003) Measuring inconsistency in meta‐analyses. BMJ (Clinical Research Ed.) 327, 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovdenak N. & Haram K. (2012) Influence of mineral and vitamin supplements on pregnancy outcome. European Journal of Obstetrics, Gynecology, and Reproductive Biology 164, 127–132. [DOI] [PubMed] [Google Scholar]
- Lawrence J.M., Petitti D.B., Watkins M. & Umekubo M.A. (1999) Trends in serum folate after food fortification. Lancet 354, 915–916. [DOI] [PubMed] [Google Scholar]
- Li Z., Ye R., Zhang L., Li H., Liu J. & Ren A. (2013) Folic acid supplementation during early pregnancy and the risk of gestational hypertension and preeclampsia. Hypertension 61, 873–879. [DOI] [PubMed] [Google Scholar]
- Makedos G., Papanicolaou A., Hitoglou A., Kalogiannidis I., Makedos A., Vrazioti V. et al (2007) Homocysteine, folic acid and B12 serum levels in pregnancy complicated with preeclampsia. Archives of Gynecology and Obstetrics 275, 121–124. [DOI] [PubMed] [Google Scholar]
- Maron B.A. & Loscalzo J. (2009) The treatment of hyperhomocysteinemia. Annual Review of Medicine 60, 39–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merchant A.T., Msamanga G., Villamor E., Saathoff E., O'Brien M., Hertzmark E. et al (2005) Multivitamin supplementation of HIV‐positive women during pregnancy reduces hypertension. The Journal of Nutrition 135, 1776–1781. [DOI] [PubMed] [Google Scholar]
- Moat S.J., Lang D., McDowell I.F., Clarke Z.L., Madhavan A.K., Lewis M.J. et al (2004) Folate, homocysteine, endothelial function and cardiovascular disease. The Journal of Nutritional Biochemistry 15, 64–79. [DOI] [PubMed] [Google Scholar]
- Murphy M.M. & Fernandez‐Ballart J.D. (2011) Homocysteine in pregnancy. Advances in Clinical Chemistry 53, 105–137. [DOI] [PubMed] [Google Scholar]
- Nohr E.A., Olsen J., Bech B.H., Bodnar L.M., Olsen S.F. & Catov J.M. (2014) Periconceptional intake of vitamins and fetal death: a cohort study on multivitamins and folate. International Journal of Epidemiology 43, 174–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oken E., Ning Y., Rifas‐Shiman S.L., Rich‐Edwards J.W., Olsen S.F. & Gillman M.W. (2007) Diet during pregnancy and risk of preeclampsia or gestational hypertension. Annals of Epidemiology 17, 663–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patsopoulos N.A., Evangelou E. & Ioannidis J.P. (2008) Sensitivity of between‐study heterogeneity in meta‐analysis: proposed metrics and empirical evaluation. International Journal of Epidemiology 37, 1148–1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin X., Fan F., Cui Y., Chen F., Chen Y., Cheng X. et al (2014) Folic acid supplementation with and without vitamin B6 and revascularization risk: a meta‐analysis of randomized controlled trials. Clinical Nutrition (Edinburgh, Scotland) 33, 603–612. [DOI] [PubMed] [Google Scholar]
- Ray J.G. & Mamdani M.M. (2002) Association between folic acid food fortification and hypertension or preeclampsia in pregnancy. Archives of Internal Medicine 162, 1776–1777. [DOI] [PubMed] [Google Scholar]
- Ray J.G., Meier C., Vermeulen M.J., Boss S., Wyatt P.R. & Cole D.E. (2002) Association of neural tube defects and folic acid food fortification in Canada. Lancet 360, 2047–2048. [DOI] [PubMed] [Google Scholar]
- Roberts J.M. & Cooper D.W. (2001) Pathogenesis and genetics of pre‐eclampsia. Lancet 357, 53–56. [DOI] [PubMed] [Google Scholar]
- Roberts J.M., Pearson G., Cutler J. & Lindheimer M. (2003) Summary of the NHLBI working group on research on hypertension during pregnancy. Hypertension 41, 437–445. [DOI] [PubMed] [Google Scholar]
- Scorsatto M., Uehara S.K., Luiz R.R., de Oliveira G.M. & Rosa G. (2011) Fortification of flours with folic acid reduces homocysteine levels in Brazilian women. Nutrition Research (New York, N.Y.) 31, 889–895. [DOI] [PubMed] [Google Scholar]
- Steegers‐Theunissen R.P., Van Iersel C.A., Peer P.G., Nelen W.L. & Steegers E.A. (2004) Hyperhomocysteinemia, pregnancy complications, and the timing of investigation. Obstetrics and Gynecology 104, 336–343. [DOI] [PubMed] [Google Scholar]
- Stroup D.F., Berlin J.A., Morton S.C., Olkin I., Williamson G.D., Rennie D. et al (2000) Meta‐analysis of observational studies in epidemiology: a proposal for reporting. Meta‐analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA: The Journal of the American Medical Association 283, 2008–2012. [DOI] [PubMed] [Google Scholar]
- Sudchada P., Saokaew S., Sridetch S., Incampa S., Jaiyen S. & Khaithong W. (2012) Effect of folic acid supplementation on plasma total homocysteine levels and glycemic control in patients with type 2 diabetes: a systematic review and meta‐analysis. Diabetes Research and Clinical Practice 98, 151–158. [DOI] [PubMed] [Google Scholar]
- Thaver D., Saeed M.A. & Bhutta Z.A. (2006) Pyridoxine (vitamin B6) supplementation in pregnancy. Cochrane Database of Systematic Reviews (2), Cd000179. [DOI] [PubMed] [Google Scholar]
- Timmermans S., Jaddoe V.W., Silva L.M., Hofman A., Raat H., Steegers‐Theunissen R.P. et al (2011) Folic acid is positively associated with uteroplacental vascular resistance: the Generation R study. Nutrition, Metabolism, and Cardiovascular Diseases 21, 54–61. [DOI] [PubMed] [Google Scholar]
- Tobias A. (1999) Assessing the influence of a single study in the meta‐analysis estimate. Stata Technical Bulletin 47, 15–17. [Google Scholar]
- Van Oort F.V., Melse‐Boonstra A., Brouwer I.A., Clarke R., West C.E., Katan M.B. et al (2003) Folic acid and reduction of plasma homocysteine concentrations in older adults: a dose‐response study. The American Journal of Clinical Nutrition 77, 1318–1323. [DOI] [PubMed] [Google Scholar]
- Vanderlelie J., Scott R., Shibl R., Lewkowicz J., Perkins A. & Scuffham P.A. (2014) First trimester multivitamin/mineral use is associated with reduced risk of pre‐eclampsia among overweight and obese women. Maternal and Child Nutrition. DOI: 10.1111/mcn.12133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells G., Shea B. & O'connell D. (2000) The Newcastle‐Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta‐analyses. pp. 3–5. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (Accessed 30 December 2014).
- Wen S.W., Chen X.K., Rodger M., Rennicks White R., Yang Q., Smith G.N. et al (2008) Folic acid supplementation in early second trimester and the risk of preeclampsia. American Journal of Obstetrics and Gynecology 198, 45.e1–45.e7. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2005) The World Health Report 2005: Make Every Mother and Child Count. World Health Organization: Geneva, Switzerland. [Google Scholar]
- Yamamoto K., Isa Y., Nakagawa T. & Hayakawa T. (2012) Folic acid fortification ameliorates hyperhomocysteinemia caused by a vitamin B(6)‐deficient diet supplemented with L‐methionine. Bioscience, Biotechnology, and Biochemistry 76, 1861–1865. [DOI] [PubMed] [Google Scholar]


