Abstract
Infant and young child feeding has been recognised as an essential element to improve growth of children, especially in developing countries where malnutrition among children and its dire consequences are very prevalent. However, little attention has been paid on the influence of fathers on child feeding practices, although fathers are very important in raising well‐adjusted, happy and successful children. Therefore, this study aimed to assess the influence of fathers' child feeding knowledge and practice on children's dietary diversity. A community‐based comparative cross‐sectional study was conducted among 850 eligible urban and rural households with children of 6–23 months. The father and mother of the child were interviewed on children's dietary diversity and fathers' knowledge and practice of child feeding. Nearly half (46%) of the children in the rural district did not meet the minimum dietary diversity, and in the urban district, the rate was even worse (72%). Grains were the common food group given to the children in both districts, whereas flesh food was the least commonly consumed food group. Additionally, low vitamin A‐rich food and other fruit and vegetable consumption seem to be a problem in both districts. Almost all dimensions of fathers' knowledge and practice were significantly related to children's minimum dietary diversity; especially, fathers' knowledge of food groups was an important predictor (P‐value < 0.001) in both districts. Interventions that focus on the fathers' knowledge of child feeding, especially about food groups, are recommended to improve children's dietary diversity in the study communities.
Keywords: IYCF, dietary diversity, fathers' knowledge, fathers' practice
Introduction
Numerous efforts have been made to alleviate children's malnutrition in developing countries where poor socio‐economic status, food insecurity and poor child feeding practices are still common (Ghosh & Shah 2004; Bhutta et al. 2008; Saul et al. 2008; Uauy et al. 2009; Shetty 2009; Remans et al. 2011; Wuehler & El Hafed Ould Dehah 2011). Since the early 2000s, infant and young child feeding (IYCF) has been issued as an essential element to improve growth of children (United Nations 2000; WHO 2000, 2001, 2002; Nguyen et al. 2011). Implementation of the guiding principles of IYCF is essential in developing countries where the consequences of children's malnutrition, such as stunting, underweight and wasting, are very prevalent (Michael 2006; Black et al. 2008; UNICEF 2008; Shetty 2009; Willey et al. 2009; Asres & Eidelman 2011; Central Statistical Agency 2011; Beiersmann et al. 2012). One of the core indicators of IYCF is dietary diversity, which is a proxy for adequate micronutrient density of foods and liquids other than breast milk. According to a recent study conducted in 21 developing and developed countries, less than half of the countries met the minimum dietary diversity (MDD) (Onyango et al. 2013). Similarly, the 2011 Ethiopian Demographic and Health Survey showed that only 5% of children were fed according to minimum standards with respect to dietary diversity (Central Statistical Agency 2011). A recent Oxfam report showed that, Ethiopia's diet is one of the least nutritious diets in the world (Oxfam 2014). Again, other study in developing country confirmed this fact (WHO 2008).
Most of the studies and interventions on the parents' role in IYCF have focused on mothers, not fathers (Pryer et al. 2003). Despite the fact that fathers are primary care givers, like mothers, and are very important in raising well‐adjusted, happy and successful children, most of the studies are superficial and only showed the positive impact of fathers' educational and economic status on child health and nutrition status (Kikafunda & Tumwine 2006; Willey et al. 2009; Nahar et al. 2010; Jesmin et al. 2011). Even in the developed world, where child obesity is evident, only a few studies engage fathers in areas of child care and health (Anderson et al. 2010; Dearden et al. 2013).
Along with the fathers' socio‐economic status, their knowledge on child feeding and related practices needs to be assessed to develop more successful interventions in the future. This is especially relevant in developing countries where household income generation and decision‐making are mainly controlled by fathers. Therefore, we assessed fathers' knowledge and practices of child care and feeding among Ethiopian fathers from both urban and rural districts, and investigated the association with children's dietary diversity. We chose to select both urban and rural districts in our study because we expected that there might be important differences between these settings.
Key messages.
Nearly half of the children in the rural district did not meet the minimum dietary diversity, and in the urban district, the rate was even worse.
Flesh food, vitamin A‐rich food and other fruits and vegetables were the least food groups fed to the children.
Fathers' knowledge of food groups was an important predictor of children's dietary diversity.
Interventions that enhance the fathers' knowledge and practice of child feeding, especially about food groups, are recommended to improve children's dietary diversity.
Materials and methods
Setting and subjects
We conducted the study in two different districts: one rural district, Atsibi, and one urban district, Adigrat, located in Tigray Region in Northern Ethiopia. More than three‐fourths of the population in Tigray region are farmers. However, centuries of erosion, deforestation and overgrazing have left the region with dry and treeless plains, hills and plateau. The communities are served by health centres that provide primary health care to children through health extension workers and volunteer health development army. The primary health care activities include immunisation, growth monitoring (measuring weights and height on a regular basis) and educating mothers about breastfeeding and complementary feeding based upon World Health Organization (WHO)'s recommendations and few curative services (WHO 2010a, 2010b). Considering that the child's first two years of life are a ‘critical window of opportunity’ for prevention of growth faltering (UNICEF 2008). The participants were fathers of children in the age of 6–23 months. In order to assess children's dietary diversity in 24‐h recall, mothers also participated in this study. There were more than 5000 children of 6–23 months in each of the two districts (Tigray Regional Health Bureau 2011).
Study design and sampling
A community‐based comparative cross‐sectional study was conducted. To calculate the required sample size, we used the two population proportion formula for comparative studies (Rigby & Vail 1998). We wanted to be able to detect at least a difference of 10% in a positive outcome (good dietary diversity), between fathers with good and poor knowledge/practice, with α = 0.05 and 1 − β = 0.8, in urban and rural districts. We figured that dietary diversity had improved in Ethiopia since the last measurements, so we estimated the prevalence of good dietary diversity in the poor knowledge/practice group to be close to 10%. To be able to detect a difference of 10% (minimum 20% good dietary diversity), we calculated that we would need 380 subjects per group. As we wanted to investigate the urban and rural population separately, and taking into account possible non‐response, we aimed to include 425 households per district, hence a total of 850 households. Then, a systematic random sampling technique was applied to select eligible households of mothers and fathers of children 6–23 months old, 425 households in each (rural and urban) category, out of the list of children within this age range prepared by the local health workers in these districts.
Data collection and quality control
Data collectors, who had completed at least 10th grade education, were trained using the local language, Tigrigna, before the data collection; intense training was given on the questionnaire and the ethical issues. Regarding the questionnaire, each question in the questionnaire was explained to the data collectors and unclear things were discussed. Regarding ethics, confidential and anonymous and, getting the signed consent papers from participants before the interview, were explained for the data collectors. There was continuous supervision throughout the data collection.
The interview questionnaire was developed based upon a qualitative study we conducted in 2011, which was about the practice and challenges on one of the nutrition programmes, growth monitoring and promotion, for infant and young children in Ethiopia and the WHO report on indicators for assessing infant and young child feeding practices (WHO 2010b). Then, a pre‐test was conducted before the actual data collection, in a similar setting as the study communities. During pre‐testing, the questions to fathers were adjusted to open‐ended questions based upon findings that fathers almost exclusively answered positively to yes/no questions about what they knew. After the data collection, the collected data were checked out for the completeness, accuracy and clarity by the principal investigators and supervisors.
The interview questionnaire had two parts. The first part of the interview questionnaire focused upon the socio‐demographic characteristics of mothers and children's dietary diversity (WHO 2010b) based upon 24‐h recall, and mothers were interviewed about it. The second part focused upon the socio‐demographic characteristics of fathers and fathers' knowledge and practice of child care and child feeding. A general description of all independent variables measured can be found in Table 1. To avoid socially desirable answers, possible answers were not mentioned to the fathers, but instead fathers had to mention the items spontaneously.
Table 1.
Description and the median (measurement scale) for each independent variable
| Variable (number of options) | Description of answer options (median) |
|---|---|
| Fathers' knowledge of the consequences of malnutrition (number of options = 11, median = 1) | Refers to weight loss, increased susceptibility to infectious diseases(illness), delayed development (stunting or low height for age), reduced intellectual development and learning, attention deficit disorder, impaired school performance, memory deficiency, learning disabilities, reduced social skills, reduced language development and reduced problem‐solving abilities |
| Fathers' knowledge of important things to keep the child healthy (number of options = 11, median = 2) | Refers to breastfeeding soon after birth, exclusive breastfeeding up to 6 months of age, beginning supplementary food at 6 months, timely and full immunisations, going to a doctor if the child gets sick, supplementary vitamins, clean house, clean water, clean food, adequate food, balanced diet, washing hands with soap before eating, more money to buy food and keeping the child clean |
| Fathers' knowledge of food groups (number of options = 7, median = 4) | Refers to grains (barley, wheat, corn), roots and tubers (potato, sweet potato), legumes and nuts (lentils, peas, beans), dairy products (milk, yoghurt, cheese), flesh foods (meat, fish, poultry and organ meats like: liver, kidney, heart), eggs, vitamin A‐rich fruits (ripe mango, ripe papaya, pumpkins) and vegetables (which comes from green leafy vegetables like carrot, tomato) and other fruits and vegetables |
| Fathers' knowledge of child care (number of options = 8, median = 2) | Refers to appropriate child feeding (breastfeeding, complimentary feeding), keeping the child clean (keeping the child's hygiene), spending time with the child (playing with the child, looking after the child when the mother is not around), helping mothers in child care (changing cloths, bathing the child, putting the child to sleep), taking the child to health facilities (for vaccination, growth monitoring, in case of illness), giving money to the mother to purchase necessary things for the child (food, cloths, any materials), buying/bringing necessary things (meat, fruits, cloth) for the child from the market/town/and discussing the child's health‐related issues with the mother |
| Fathers' practice in routine childcare activities (number of options = 7, median = 4) | Refers to if they changed their children's clothes on the previous day; if they bathed their children on the previous day; if they put their children to sleep on the previous day; if they played with their children at home on the previous day; if they took out their children on the previous day; if they took part in monitoring (watching) while their children played, moved, sat, stood, slept, etc., on the previous day; and if they took part in teaching their children how to behave and disciplining them on the previous day |
| Fathers' practice in child provision (number of options = 7, median = 5) | Refers to if the fathers quieten their children when crying or calmed them after the children fell or had pain; if they discussed their children's feeding with the mothers; if they discussed their children's health, hygiene, growth and appetite with the mothers; if they looked after their children when the mothers were not around (working in the kitchen, going out), all within a week time; if they took their children to health facilities for vaccination, growth monitoring and other related services in the previous month; if they gave money to the mothers to purchase the necessary food for the children during the last week; and finally, if they checked, asked, were concerned about and attentive about their children's growth during the last month |
| Fathers' participation in child feeding (number of options = 7, median = 5) | Refers to if fathers bought necessary food items for their children like eggs, meat, milk, fruits and vegetables during the last weekday from market/town; if they checked upon, asked or attended to the amount of food their children took on the previous day; whether they checked upon/asked about or attended to their children's frequency of meal on the last day; whether they tried to encourage their children to take food while the mothers were feeding them during the last day; if they checked, asked about or attended to the diversity of the food their children took during the last day; and if they checked, asked about or attentively observed their children's appetite on the last day |
Minimum dietary diversity was assessed as the proportion of children 6–23 months of age who receive food from four or more food groups out of the seven food groups: grains, roots and tubers; legumes and nuts; dairy products (milk, yogurt, cheese); flesh foods (meat, fish, poultry and liver/organ meats); eggs; vitamin A‐rich fruits and vegetables; other fruits and vegetables (WHO 2010b).
Ethics
Before the study began, ethical clearance was obtained from the Ethical Committee of Mekelle University and approval letter from the Regional Health Bureau. Then, the Atsibi and Adigrat district health offices were informed through formal letters. After informing the participants about the aim of the project, written information about the benefits and confidentiality of the research was given to those who were able to read and write, and verbal information was given otherwise. Then, written informed consent and verbal informed were obtained.
Data analysis
The collected data were entered and analysed using SPSS version 19 (IBM Corp 2010). The data were cleaned by the principal investigator, and after cleaning the data, frequencies were generated and associations were tested. For the knowledge and practice questions in the questionnaire, we did not set an absolute minimum to distinguish between good and poor knowledge. Instead, we used a relative cut‐off point by calculating the median for each variable for all participants and then applied it to the urban and rural districts. All our independent variables consisted of several sub‐questions, so we had to decide how to use the independent variables in our regression models: continuous or in two or more categories. We chose to make them dichotomous, firstly because the outcomes would be easier to interpret; odds ratios (ORs) for good knowledge/practice against poor knowledge/practice, instead of ORs for one more item answered correctly for that independent variable. In addition, the fact that the answers were highly skewed also made the median the best option in our view. In Table 1, we give a short description and the median for each knowledge and practice variables in the questionnaire.
A chi‐square followed by binary logistic regression was used to investigate which factors predicted dietary diversity. In addition, we entered all variables into a multivariate logistical regression model, using forward stepwise methods at a 95% confidence interval (CI) to determine the predictors of the minimum dietary diversity. P‐values less than 0.05 were considered statistically significant and the result was presented with OR and 95% CI.
Results
Descriptive characteristics
Demographic characteristics of fathers, mothers and children are presented in Table 2. A total of 850 households, with at least one child between 6 and 23 months, participated in the study: 425 households from the rural district and 425 from the urban district. The response rate was 100%, but 10 (1%) questionnaires were excluded from the analysis because of major errors or incompleteness.
Table 2.
Descriptive characteristics of the children and their fathers and mothers
| Variables | Urban (n = 420) | Rural (n = 420) | |
|---|---|---|---|
| Age of the last child [Mean (SD)] | Months | 14 (5) | 14 (5) |
| Age of the last child | 6–8 months | 48 (12%) | 60 (14%) |
| 9–23 months | 371 (88%) | 359 (86%) | |
| Sex of the last child [n (%)] | Male | 200 (48%) | 231 (55%) |
| Female | 216 (52%) | 188 (45%) | |
| Number of children in each household | <4 | 321 (77%) | 168 (40%) |
| ≥4 | 99 (23%) | 252 (60%) | |
| Mothers' education level [n (%)] | No education | 60 (15%) | 310 (75%) |
| Primary (Grade 1–8) | 165 (40%) | 91 (22%) | |
| Secondary (Grade 9–12) | 163 (39%) | 10 (2%) | |
| >Secondary (12+) | 25 (6%) | 2 (0.4%) | |
| Fathers' education level [n (%)] | No education | 19 (5%) | 215 (51%) |
| Primary (Grade 1–8) | 135 (32%) | 146 (35%) | |
| Secondary (Grade 9–12) | 198 (47%) | 25 (6%) | |
| >Secondary (12+) | 64 (15%) | 2 (0.4%) | |
| Mothers' occupation [n (%)] | House wife | 342 (82%) | 10 (2%) |
| Farmer | 0 (0%) | 407 (97%) | |
| Merchant | 38 (9%) | 1 (0.2%) | |
| Government worker | 38 (9%) | 1 (0.2%) | |
| Fathers' occupation [n (%)] | Farmer | 2 (0.2%) | 398 (95%) |
| Daily labour | 160 (38%) | 6 (1%) | |
| Merchant | 85 (20.3%) | 4 (1%) | |
| Government worker | 172 (41%) | 10 (2%) | |
| Average monthly income [Mean birr (dollar)] | 1415 birr (76$) | 1290 birr (69$) | |
Dietary diversity
One quarter of the urban children (28%) were fed on four or more food groups out of the seven food groups the day before the interview. In the rural district, more than half of the children (54%) met the minimum dietary diversity (MDD). Figure 1 shows the common food groups fed to the children the day before the survey, and out of the seven food groups, grains (urban – 91%, rural – 99%), legumes and nuts (urban – 62%, rural – 94%) were the common food groups fed in both districts. Flesh foods (urban – 3%, rural – 5%) was the least common food groups fed to the children in both urban and rural districts. Additionally, vitamin A‐rich and fruits and vegetables were uncommonly eaten food groups in both districts.
Figure 1.
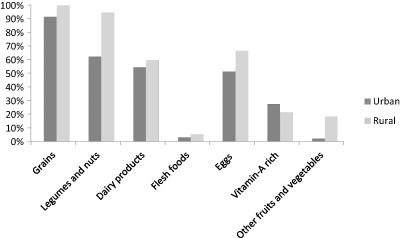
Percentage of each food group that consumed by urban children vs. rural children.
Fathers' knowledge and practice of child care and feeding
Except fathers' knowledge of the consequences of malnutrition, all fathers' knowledge predictors seem to be related to dietary diversity in both urban and rural districts (Table 3). Fathers' knowledge of the important things to keep the child healthy was significantly associated with dietary diversity with OR of 3.43 (95% CI: 2.19–5.37) and 2.58 (95% CI: 1.59–4.19); fathers who had a good knowledge of food groups, the dietary diversity of their children was much higher, with an OR of 5.28 (95% CI: 3.32–8.38) and 8.38 (95% CI: 5.32–13.2); and fathers' knowledge of child care activities was significantly associated with minimum dietary diversity with OR of 4.62 (95% CI: 2.86–7.48) and 2.88 (95% CI: 1.94–4.29) in the urban and rural district, respectively.
Table 3.
The relationship of fathers' knowledge and practices of child care and feeding with children's minimum dietary diversity in the urban and rural districts
| Variables | Urban | Rural | ||||||
|---|---|---|---|---|---|---|---|---|
| N = 420 | N = 420 | |||||||
| Frequency | Minimum dietary diversity | Frequency | Minimum dietary diversity | |||||
| <MDD | ≥MDD | <MDD | ≥MDD | |||||
| n (%) | n (%) | n (%) | OR (95% CI) | n (%) | n (%) | n (%) | OR (95% CI) | |
| Fathers' knowledge of the consequences of malnutrition | ||||||||
| Poor | 154 (37%) | 114 (74%) | 40 (26%) | 340 (81%) | 157 (46%) | 183 (54%) | ||
| Good | 266 (63%) | 189 (71%) | 77 (29%) | 1.16 (0.74–1.81) | 80 (19%) | 37 (46%) | 43 (54%) | 0.99 (0.61–1.62) |
| Fathers' knowledge of the important things to keep the child healthy | ||||||||
| Poor | 286 (68) | 230 (80%) | 56 (20%) | 91 (21%) | 58 (64%) | 32 (36%) | ||
| Good | 134 (32%) | 73 (54%) | 61 (46%) | 3.34 (2.19–5.37)*** | 330 (79%) | 136 (41%) | 194 (59%) | 2.58 (1.59–4.19)*** |
| Fathers' knowledge of the important food groups | ||||||||
| Poor | 252 (60%) | 215 (85%) | 37 (15%) | 160 (38%) | 122 (76%) | 38 (24%) | ||
| Good | 168 (40%) | 88 (52%) | 80 (48%) | 5.28 (3.32–8.38)*** | 260 (62%) | 72 (28%) | 188 (72%) | 8.38 (5.32–13.2)*** |
| Fathers' knowledge of child care | ||||||||
| Poor | 321 (76%) | 257 (80%) | 64 (20%) | 197 (47%) | 118 (60%) | 79 (40%) | ||
| Good | 99 (24%) | 46 (46%) | 53 (54%) | 4.62 (2.86–7.48)*** | 223 (53%) | 76 (34%) | 147 (66%) | 2.88 (1.94–4.29)*** |
| Fathers' practice in routine child care activities | ||||||||
| Poor | 253 (61%) | 200 (79%) | 53 (21%) | 92 (22%) | 52 (57%) | 40 (43%) | ||
| Good | 160 (39%) | 99 (62%) | 61 (38%) | 2.32 (1.49–3.61)*** | 320 (78%) | 137 (43%) | 183 (57%) | 1.73 (1.08–2.77)* |
| Fathers' practice in child provision | ||||||||
| Poor | 209 (52%) | 175 (84%) | 34 (16%) | 153 (38%) | 58 (38%) | 95 (62%) | ||
| Good | 195 (48%) | 117 (60%) | 78 (40%) | 3.43 (2.15–5.46)*** | 255 (62%) | 128 (50%) | 127 (50%) | 0.60 (0.40–0.91)* |
| Fathers' practice in child feeding | ||||||||
| Poor | 191 (48%) | 161 (84%) | 30 (16%) | 199 (49%) | 94 (47%) | 105 (53%) | ||
| Good | 208 (52%) | 127 (61%) | 81 (39%) | 3.42 (2.12–5.52)*** | 211 (51%) | 95 (45%) | 116 (55%) | 1.09 (0.74–1.61) |
| Educational status of father | ||||||||
| Primary | 135 (34%) | 110 (82%) | 25 (18%) | 146 (84%) | 75 (51%) | 71 (49%) | ||
| Secondary | 198 (50%) | 139 (70%) | 59 (30%) | 1.86 (1.09–3.17) | 25 (15%) | 9 (36%) | 16 (64%) | 1.87 (0.78–4.52) |
| >Secondary | 64 (16%) | 35 (54%) | 29 (46%) | 3.64 (1.89–7.01)*** | 2 (1%) | 1 (50%) | 1 (50%) | 1.05 (0.06–17.2) |
| Occupation of father | ||||||||
| Farmer and labourer | 162 (39%) | 140 (86%) | 22 (14%) | 404 (97%) | 184 (46%) | 220 (55%) | ||
| Merchant | 85 (20%) | 56 (66%) | 29 (34%) | 3.29 (1.74–6.21) | 4 (1%) | 3 (75%) | 1 (25%) | 0.27 (0.02–2.70) |
| Government worker | 172 (41%) | 106 (62%) | 66 (38%) | 3.96 (2.29–6.83)*** | 10 (2%) | 6 (60%) | 4 (40%) | 0.55 (0.15–2.00) |
| Monthly income | ||||||||
| Low | 123 (30%) | 104 (85%) | 19 (15%) | 129 (31%) | 57 (44%) | 72 (56%) | ||
| Middle | 117 (28%) | 90 (77%) | 27 (23%) | 1.64 (0.856–3.15) | 31 (7%) | 16 (52%) | 15 (48%) | 0.74 (0.34–1.68) |
| High | 24 (6%) | 10 (42%) | 14 (58%) | 7.66 (2.971–19.8)*** | 146 (35%) | 65 (45%) | 81 (55%) | 0.99 (0.62–1.59) |
| Very high | 151 (36%) | 95 (63%) | 56 (37%) | 3.23 (1.789–5.82)*** | 111 (27%) | 54 (49%) | 57 (51) | 0.84 (0.50–1.39) |
OR, odds ratio; CI, confidence interval. For the outcome variable, <MDD refers to children who got less than four food groups in their diet the day before the survey and ≥MDD refers to children who got four or more food groups in their the day before the survey. On educational status of the father and mother, the category primary refers to grade 1–8, secondary refers to grade 9–12, >secondary refers to diploma and above. Statistically significant at *P < 0.05; **P < 0.01; ***P < 0.001. For knowledge and practice variables, the median was calculated for all participants and then applied to both rural and urban. The relative cut‐off point that was used to differentiate fathers with good knowledge/practice vs. poor knowledge/practice, fathers who answered the median and above were considered as good knowledge/practice. The income classification was based upon quantile calculation.
Regarding practice, children whose fathers had a good practice of routine child care activities, better dietary diversity was reported with OR of 2.32 (95% CI:1.49–3.61) and 1.73 (95% CI:1.08–2.77) in the urban and rural district, respectively (Table 3). Again, for both the urban and the rural districts, a significant association was found between provision of necessary things and dietary diversity with OR of 3.43 (95% CI: 2.15–5.46) and 1.73 (95% CI: 1.08–2.77), respectively. For fathers who had a meaningful participation in child feeding activities, a significant association was found with dietary diversity in the urban district with an OR of 3.42 (95% CI: 2.12–5.52), but not for the rural district. Lastly, the stepwise logistic regression showed that in both urban and rural districts, fathers' knowledge of food groups became the most important determinant of children's minimum dietary diversity with ORs of 6.50 (95% CI: 3.89,–10.9) and 8.65 (95% CI: 3.10–18.9), respectively.
Discussion
Our study showed that dietary diversity was a serious problem in the urban district when compared to the rural district and that grains were the most common food groups fed to the children in both districts. Legumes and nuts were also commonly reported food groups. The majority of children were not given flesh foods. Additionally, vitamin A‐rich food and other fruits and vegetables were also less commonly consumed food groups in both districts. Almost all dimensions of fathers' knowledge and practice that we measured and also the socio‐economic characteristics were significantly related to children's minimum dietary diversity, indicating the strong influence of the father on child nutrition. Especially, fathers' knowledge of food groups was the main and independent predictor of child food diversity in both districts.
In this study, almost half of the children in the rural district did not meet the minimum dietary diversity of four food groups per day, and in the urban district, the rate was even worse. We expected better report in the urban district, but the result showed that children's dietary diversity in the rural district is much better. One possible reason could be that special attention has been given to the rural people, considering that the rural people have poor access to health care. Therefore, for the past decade, health educations have been provided house to house by the community health workers for the people in the rural area but not for the urban people. In general, our finding is consistent with other observational studies that calculated the percentage of children that had minimum dietary diversity in other developing countries, such as India (24.4%) (Khanal et al. 2013), Nepal (30.4%) (Mukhopadhyay et al. 2013) and Bangladesh (42%) (Kabir et al. 2012). Although this illustrates that dietary diversity is a big concern in Ethiopia and other developing countries, it is a big improvement considering the result of a study conducted in 2010 in Ethiopia where only 5% of the children met the minimum dietary diversity (Central Statistical Agency 2011). It seems that a lot of work is still needed to improve children's dietary diversity. Our study showed that improving fathers' knowledge and practice could be a prerequisite to meet children's dietary diversity. However, more studies are needed to investigate the influence of the fathers' role in children nutrition.
Possible reasons for the very low consumption of flesh foods among children could be affordability and a tradition of having flesh only for special occasions. Further research seems needed to dig‐out the reasons behind. Although assessing vitamin A and fruit and vegetable intakes is complicated, compared with previous studies conducted in Ethiopia and other African countries (Getaneh et al. 2000; MacKeown & Faber 2004), a big improvement has been reported. However, it is still below the recommendation line and it seems a common problem in both developing and developed countries (Blissett 2011; de Lauzon‐Guillain et al. 2013). According to a recent review, the problem of low fruits and vegetable consumption seem multifactorial, but include at least product accessibility, availability, and distribution and consumers' behaviours (Rekhy & McConchie 2014).
Our study confirmed the hypothesis that the fathers' knowledge and practice about food diversity is significantly associated with meeting the minimum dietary diversity. Although we could not find studies using the same concepts of father's knowledge and practice, our findings are in line with other observational studies on the fathers' involvement in breastfeeding, such as attending breastfeeding sessions with mothers, involvement in decision‐making and helping the mother in the household, showed much better breastfeeding practice than families with fathers who were less involved (Ingram et al. 2002; Moestue & Huttly 2008; Pontes et al. 2009; Sasaki et al. 2010). Similarly, better cognitive and language competence and nutrition status were reported among young children whose fathers were involved in child playing and child care activities (Tran 2008).
These findings from observational studies are also supported by intervention studies. A recent systematic literature review showed that involving fathers actively in the child's life, such as father's participation child care, enhanced a positive father–child interaction, which also had a positive effect on child development (Magill‐Evans et al. 2006). Another community‐based participatory intervention study highlighted that empowering both parents to play an active and equal role with the research team in intervention design and implementation of child feeding was reported as a promising approach to child obesity prevention (Davison et al. 2013).
Certain limitations of this study require mentioning. Firstly, to avoid social desirable answers, open‐ended knowledge and practice questions were used. This might however lead to recall bias, but we do not expect the recall bias to be differential, and thus we do not expect that the observed associations would be changed. Another limitation of this study could be that we developed the knowledge and practice questions and the cut‐off points ourselves, especially because for few questions, the median number was 1 or 2 good answers out of 10 or more options. We needed to do this because validated questionnaires on the concepts that we wanted to measure were not available. To give better insight into the questions we asked in this study, we provided a description of all the variables and answer categories. The final limitation of this study is of course that this study was a cross‐sectional study. Whether there is really a causal relationship between fathers' knowledge and practice and dietary diversity should preferably be investigated in cohort studies and randomised trials.
Considering our results and the results of other observational and intervention studies, it seems reasonable to assume that interventions should be designed to involve the father in the process of child feeding in order to improve dietary diversity in small children in developing countries. Based upon our findings, the knowledge and practices have an impact over and above the ‘usual suspects’, i.e. educational status and occupation. Therefore, interventions that enhance the fathers' knowledge of the important things to keep the child healthy, especially about food groups, could be a priority. Concurrently, participatory interventions that increase the fathers' practice in any child care activities from the very beginning could be effective to increase fathers' understanding towards children's needs. In general, interventions that improve both child feeding knowledge and practice of fathers are probably crucial to improve children's dietary diversity.
Source of funding
The research is funded by an AECID PhD Scholarship from Spain, the street of los Reyes, Catolicus, 428040 Madrid, Spain.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
All authors contributed extensively to the work presented in this paper. SMB, M.S, RC and AM designed the method. SMB gathered the data. SMB and MS analyze, interpreted the data and wrote the manuscript. GD and RB participated in designing and paper drafting process.
Acknowledgements
We would like to thank the mothers and fathers who shared their time and information with us, thereby contributing to the success of the data collection, and Atsibi and Adigrat district health offices for the support they gave us during the data collection. Finally, we would like to extend our appreciation to our colleagues and staff in the College of Health Sciences, Department of Public Health of Mekelle University for allowing us to use their facilities, for their expert consultations and participation in the data collection.
Bilal, S. M. , Dinant, G. , Blanco, R. , Crutzen, R. , Mulugeta, A. , and Spigt, M. (2016) The influence of father's child feeding knowledge and practices on children's dietary diversity: a study in urban and rural districts of Northern Ethiopia, 2013. Maternal & Child Nutrition, 12: 473–483. doi: 10.1111/mcn.12157.
References
- Anderson K.E., Nicklas J.C., Spence M. & Kavanagh K. (2010) Roles, perceptions and control of infant feeding among low‐income fathers. Public Health Nutrition 13, 522–530. [DOI] [PubMed] [Google Scholar]
- Asres G. & Eidelman A.I. (2011) Nutritional assessment of Ethiopian Beta‐Israel children: a cross‐sectional survey. Breastfeeding Medicine 6 (4), 171–176. [DOI] [PubMed] [Google Scholar]
- Beiersmann C., Bountogo M., Tiendrébeogo J., Louis V.R., Gabrysch S., Yé M. et al (2012) Malnutrition in young children of rural Burkina Faso: comparison of survey data from with 2009. Tropical Medicine and International Health 17 (6), 715–721. [DOI] [PubMed] [Google Scholar]
- Bhutta Z.A., Ahmed T., Black R.E., Cousens S., Dewey K., Giugliani E. et al (2008) What works? Interventions for maternal and child under‐nutrition and survival. Lancet 371 (9610), 417–440. [DOI] [PubMed] [Google Scholar]
- Black M.M., Walker S.P., Wachs T.D., Ulkuer N., Gardner J.M., Grantham‐McGregor S. et al (2008) Policies to reduce under nutrition includes child development. Lancet 371, 454–455. [DOI] [PubMed] [Google Scholar]
- Blissett J. (2011) Relationships between parenting style, feeding style and feeding practices and fruit and vegetable consumption in early childhood. Appetite 57 (3), 826–831. [DOI] [PubMed] [Google Scholar]
- Central Statistical Agency (2011) Ethiopia Demographic and Health Survey. Addis Ababa.
- Davison K.K., Jurkowski J.M., Li K., Kranz S. & Lawson H.A. (2013) A childhood obesity intervention developed by families for families: results from a pilot study. The International Journal of Behavioral Nutrition and Physical Activity 10, 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dearden K., Crookston B., Madanat H., West J., Penny M. & Cueto S. (2013) What difference can fathers make? Early paternal absence compromises Peruvian children's growth. Maternal and Child Nutrition 9, 143–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Getaneh T., Assefa A. & Tadesse Z. (2000) Dietary practices and xerophthalmia in under‐fives in Jimma town, southwest Ethiopia. East African Medical Journal 77 (6), 313–315. [DOI] [PubMed] [Google Scholar]
- Ghosh S. & Shah D. (2004) Early childhood development in deprived urban settlements. Indian Pediatrics 41, 682–696. [PubMed] [Google Scholar]
- IBM Corp (2010) IBM SPSS Statistics for Windows, Version 19.0. Armonk, NY.
- Ingram J., Johnson D. & Greenwood R. (2002) Breastfeeding in Bristol: teaching good positioning, and support from fathers and families. Midwifery 18 (2), 87–101. [DOI] [PubMed] [Google Scholar]
- Jesmin A., Yamamoto S.S., Malik A.A. & Haque M.A. (2011) Prevalence and determinants of chronic malnutrition among preschool children: a cross‐sectional study in Dhaka City, Bangladesh. Journal of Health, Population, and Nutrition 29 (5), 494–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabir I., Khanam M., Agho K.E., Mihrshahi S., Dibley M.J. & Roy S.K. (2012) Determinants of inappropriate complementary feeding practices in infant and young children in Bangladesh: secondary data analysis of Demographic Health Survey 2007. Maternal and Child Nutrition 8 (1), 11–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanal V., Sauer K. & Zhao Y. (2013) Determinants of complementary feeding practices among Nepalese children aged 6–23 months: findings from demographic and health survey 2011. BMC Pediatrics 13 (1), 131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kikafunda J.K. & Tumwine J.K. (2006) Diet and socio‐economic factors and their association with the nutritional status of pre‐school children in a low income suburb of Kampala City, Uganda. East African Medical Journal 83 (10), 565–574. [DOI] [PubMed] [Google Scholar]
- de Lauzon‐Guillain B., Jones L., Oliveira A., Moschonis G., Betoko A., Lopes C. et al (2013) The influence of early feeding practices on fruit and vegetable intake among preschool children in 4 European birth cohorts. American Journal of Clinical Nutrition 98 (3), 804–812. [DOI] [PubMed] [Google Scholar]
- MacKeown J.M. & Faber W.M. (2004) Frequency of food items consumed by young rural and urban African children – essential knowledge to provide dietary advice in caries prevention. International Dental Journal 54 (5), 284–290. [DOI] [PubMed] [Google Scholar]
- Magill‐Evans J., Harrison M.J., Rempel G. & Slater L. (2006) Interventions with fathers of young children: systematic literature review. Journal of Advanced Nursing 55 (2), 248–264. [DOI] [PubMed] [Google Scholar]
- Michael W. (2006) Malnutrition and its effect in Ethiopian children. Global Citizenship: Ethiopia.
- Moestue H. & Huttly S. (2008) Adult education and child nutrition: the role of family and community. Journal of Epidemiology and Community Health 62 (2), 153–159. [DOI] [PubMed] [Google Scholar]
- Mukhopadhyay D.K., Sinhababu A., Saren A.B. & Biswas A.B. (2013) Association of child feeding practices with nutritional status of under‐two slum dwelling children: a community‐based study from West Bengal, India. Indian Journal of Public Health 57 (3), 169–172. [DOI] [PubMed] [Google Scholar]
- Nahar B., Ahmed T., Brown K.H. & Hossain M.I. (2010) Risk factors associated with severe underweight among young children reporting to a diarrhea treatment facility in Bangladesh. Journal of Health, Population, and Nutrition 28 (5), 476–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen P.H., Menon P., Ruel M. & Hajeebhoy N. (2011) A situational review of infant and young child feeding practices and interventions in Viet Nam. Asia Pacific Journal of Clinical Nutrition 20 (3), 359–374. [PubMed] [Google Scholar]
- Onyango A.W., Borghi E., de Onis M., Casanovas M.D. & Garza C. (2013) Complementary feeding and attained linear growth among 6–23‐month‐old children. Public Health Nutrition 19, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxfam (2014) Netherlands is Country with Most Plentiful, Healthy Food. Available at: http://www.nytimes.com/reuters/2014/01/14/world/14reuters-food-countries.html?partner=rss&emc=rss&module=Search&mabReward=relbias%3Ar%2C{%222%22%3A%22RI%3A12%22} (Accessed 3 October 2014).
- Pontes C.M., Osorio M.M. & Alexandrino A.C. (2009) Building a place for the father as an ally for breast feeding. Midwifery 25 (2), 195–202. [DOI] [PubMed] [Google Scholar]
- Pryer J.A., Rogers S. & Rahman A. (2003) The epidemiology of good nutritional status among children from a population with a high prevalence of malnutrition. Public Health Nutrition 7 (2), 311–317. [DOI] [PubMed] [Google Scholar]
- Rekhy R. & McConchie R. (2014) Promoting consumption of fruit and vegetables for better health. Have campaigns delivered on the goals? Appetite 1 (79c), 113–123. [DOI] [PubMed] [Google Scholar]
- Remans R., Pronyk P.M., Fanzo J.C., Chen J., Palm C.A. & Nemser B., (2011) Multi‐sector intervention to accelerate reductions in child stunting: an observational study from 9 sub‐Saharan African countries. The American Journal of Clinical Nutrition 94 (6), 1632–1642. [DOI] [PubMed] [Google Scholar]
- Rigby A.S. & Vail A. (1998) Statistical methods in epidemiology. II: a common sense approach to sample size estimation. Disability and Rehabilitation 20 (11), 405–410. [DOI] [PubMed] [Google Scholar]
- Sasaki Y., Ali M., Kakimoto K., Saroeun O., Kanal K. & Kuroiwa C. (2010) Predictors of exclusive breast‐feeding in early infancy: a survey report from Phnom Penh, Cambodia. Journal of Pediatric Nursing 25 (6), 463–469. [DOI] [PubMed] [Google Scholar]
- Saul S.M., Bruce C., Ricardo U. & Maternal and Child Under nutrition Study Group (2008) Effective international action against undernutrition: why has it proven so difficult and what can be done to accelerate progress? Lancet 371, 608–621. [DOI] [PubMed] [Google Scholar]
- Shetty P. (2009) Community‐based approaches to address childhood under‐nutrition and obesity in developing countries. Nestle Nutrition Workshop Series. Paediatric Programme 63, 227–254. [DOI] [PubMed] [Google Scholar]
- Tigray Regional Health Bureau (2011) Tigray Regional Health Bureau Report. Ethiopia.
- Tran B.H. (2008) Relationship between paternal involvement and child malnutrition in a rural area of Vietnam. Food and Nutrition Bulletin 29 (1), 59–66. [DOI] [PubMed] [Google Scholar]
- Uauy R., Corvalan C. & Dangour AD. (2009) Conference on ‘Multidisciplinary approaches to nutritional problems’. Rank Prize Lecture Global nutrition challenges for optimal health and well‐being. Proceedings of the Nutrition Society 68, 34–42. [DOI] [PubMed] [Google Scholar]
- UNICEF Headquarters (2008) Recommendations from a Technical Consultation. Experts' consultation on growth monitoring and promotion strategies. Program guidance for a way forward: New York.
- United Nations (2000) Children's Fund. WHO organized a consultation: Geneva.
- WHO (2000) Global Strategy for Infant and Young Child Feeding. Fifty‐Third World Health Assembly. WHO: Geneva.
- WHO (2001) Global Strategy for Infant and Young Child Feeding. Fifty‐Fourth World Health Assembly. WHO: Geneva.
- WHO (2002) Global Strategy for Infant and Young Child Feeding. Fifty‐Fifth World Health Assembly. WHO: Geneva.
- WHO (2008) Strengthening Action to Improve Feeding of Infants and Young Children 6–23 months of Age in Nutrition and Child Health Programmes. WHO: Geneva.
- WHO (2010a) Indicators of Assessing Infant Young Child Feeding. Part II. WHO: Geneva.
- WHO (2010b) Indicators for Assessing Infant and Young Child Feeding Practices. Part III: Country Profiles. WHO: Geneva.
- Willey B.A., Cameron N., Norris S.A., Pettifor J.M. & Griffiths P.L. (2009) Socio‐economic predictors of stunting in preschool children – a population‐based study from Johannesburg and Soweto. South African Medical Journal 99 (6), 450–456. [PubMed] [Google Scholar]
- Wuehler S.E. & El Hafed Ould Dehah C.M. (2011) Situational analysis of infant and young child nutrition policies and programmatic activities in the Islamic Republic of Mauritania. Maternal and Child Nutrition 1, 113–132. [DOI] [PMC free article] [PubMed] [Google Scholar]


