Abstract
Perinatal depression is associated with infant undernutrition. We hypothesised that perinatal depression was associated with early cessation of exclusive breastfeeding and reduced quantity of breast milk in rural Pakistan. We used a prospective cohort design to study a population‐based sample of 132 depressed and 147 non‐depressed women from the third trimester of pregnancy to 6 months post‐natal. Current major depressive episode was measured in the third trimester and 6 months post‐natal using the Structured Clinical Interview for DSM‐IV Diagnosis. In a convenience sample of 24 depressed and 31 non‐depressed exclusively breastfeeding mothers, breast milk quantity was assessed (mL kg−1 infant weight per 24 h) at 4 months using the dose‐to‐mother deuterium dilution method. We administered also the Perception of Insufficient Milk questionnaire at 6 months post‐natal. Depression was associated with fewer days of exclusive breastfeeding (91.8 (SD = 47.1) vs. 108.7 days (SD = 54.3) (95% CI: 3.4 to 30.3 P = 0.014). Women with persistent depression ceased exclusive breastfeed earliest. There was no difference in the quantity of breast milk produced by depressed and non‐depressed mothers: 89.3 (SD = 38.1) vs. 83.9 (29.0) ml/kg infant wt/24 hours, P = 0.57. Depressed mothers were significantly more likely to report insufficient milk: PIM scores were 34.4 (SD = 14.3) for depressed and 39.7 (SD = 10.4) for non‐depressed women (P = 0.004). In Cox regression PIM score mediated the association between depression and early cessation of breastfeeding. In this area of rural Pakistan, perinatal depression is associated with early cessation of exclusive breastfeeding and this is associated with mothers' perceptions of insufficiency of breast milk but not reduced milk production.
Keywords: perinatal depression, maternal depression, breastfeeding, exclusive breastfeeding, breast milk, deuterium dilution method
Introduction
Depression in the perinatal period is associated with infant undernutrition in South Asia (Stewart 2007; Surkan et al. 2011). Such perinatal depression has been associated also with early cessation of breastfeeding (Dennis & McQueen 2009; Feldens et al. 2012; Ystrom 2012; de Jager et al. 2013) but there are few high‐quality studies concerning exclusive breastfeeding in low‐income countries where the prevalence of perinatal depression is high (Feldens et al. 2012; Fisher et al. 2012). The rates of exclusive breastfeeding in Pakistan are among the lowest in the world and the prevalence of perinatal depression is high – approximately 25% (Rahman et al. 2004, 2008). It is plausible, therefore, that depression is associated with reduced rates of exclusive breastfeeding in Pakistan.
It is also possible that the quantity of breast milk is actually reduced in depressed mothers (Gatti 2008) and one study did show that objectively measured milk inadequacy is a predictor of early breastfeeding cessation (Hill et al. 2007). An alternative possibility is that early cessation of breastfeeding may result from the mother's perception that she is producing insufficient milk, even though the milk supply is adequate (Dennis 2002; Gatti 2008; Meedya et al. 2010). We have shown that such a negative perception is common among women in rural Pakistan (Rahman et al. 2012). In Western cultures, it has been shown that the perception of inadequate breast milk is associated with depressive symptoms so perception of insufficient milk may mediate the association between depression and early cessation of breastfeeding (Dennis & McQueen 2009; Zubaran & Foresti 2013).
Current research findings are limited by a paucity of prospective studies, which assess the time relationship between depression and cessation of breastfeeding and few have examined correlates of exclusive breastfeeding up to 6 months post‐partum (Bland et al. 2003; Ystrom 2012; de Jager et al. 2013). Many studies have used self‐report measures of depression rather than a research clinical interview (Dennis & McQueen 2009).
In this study, we aimed to test the hypotheses that perinatal depression is associated with both early cessation of exclusive breastfeeding and reduction in the quantity of breast milk in Pakistani mothers. We assessed also whether the association between depression and early cessation of exclusive breastfeeding might be mediated through a psychological perception of insufficient breast milk.
Key messages.
In Pakistan, perinatal depression is associated with early cessation of breastfeeding.
Depression is not associated with a reduction of breast milk.
Depression is associated with perception of insufficient breast milk production.
Interventions to improve rates of exclusive breastfeeding should detect and manage depressive disorder as an adjunct to changing perceptions of adequacy of breast milk.
Materials and methods
Study area and participants
The study was carried out in two rural sub‐districts near Rawalpindi city in the northwest of Pakistan, where agriculture is the main economy. This area consists of 40 union councils, which formed units of randomisation for a cluster randomised controlled trial (RCT) of a psychological intervention for perinatal depression (Rahman et al. 2008). The present study was performed in the 20 union council clusters in the control arm of the RCT. Over recent years, there have been no food shortages, precluding the possibility of epidemic malnutrition due to deficient food supply. Male and female literacy rates are 79% and 48%, respectively. The average household consists of 6.2 members. The infant mortality rate is about 80 per 1000 live births and over a third of children under the age of five show stunted growth (Bhutta et al. 2004). Primary health care is delivered through a network of Basic Health Units, each providing care to 15 000–20 000 individuals. Each Basic Health Unit is staffed by a doctor, midwife, vaccinator and 15–20 village‐based community health workers called Lady Health Workers (LHWs).
For the purpose of the trial, all physically healthy women aged 16–45 years in their third trimester of pregnancy and living in one of the relevant 20 union councils were screened for depression between September 2004 and December 2005. Potential participants were identified from official registers kept by the LHWs with an additional door‐to‐door survey to identify those few women not registered with the LHW. Women were excluded if they had learning disability, any form of psychosis, severe depression or active suicidal ideas. We also excluded those women who subsequently gave birth prematurely (<37 weeks according to gestational age calculated by LHWs), or if their infant had a low birthweight (<2.5 kg), was stillborn, died before 6 months of age or had a congenital abnormality hindering breastfeeding.
In order to gain a representative sample of depressed and non‐depressed pregnant women for this study, we selected the first eight eligible depressed women in each of the relevant 20 union councils. For each depressed woman, we selected a non‐depressed woman from the immediate neighbourhood as a control. Thus, we approached 160 depressed and 160 non‐depressed women to allow for 10% non‐recruitment and a 40% dropout rate at the follow‐up.
For the quantity of breast milk study, we recruited 55 women (a further five refused) from the main sample who were exclusively breastfeeding at 4 months post‐natal and who lived in the four union councils nearest to Rawalpindi, so that samples could be transported to the lab within 1 h.
Measures
Depressive episode in mothers
Current major depressive episode was assessed by experienced psychiatrists (AM and SS) trained to administer the Structured Clinical Interview for DSM‐IV Diagnosis (SCID; First et al. 1994). The section for major depressive episode was translated and culturally adapted into Urdu using a rigorous procedure developed in Pakistan for earlier studies (Rahman et al. 2003). Interviews were conducted after high inter‐rater reliability (kappa = 0.91) between interviewers had been established. Baseline assessments were conducted during the third trimester of pregnancy and all women were reassessed at 6 months post‐natally. The interviewers were blind to the breastfeeding practice of the women as required for the trial (Rahman et al. 2008).
Duration of exclusive breastfeeding
We used two measures of duration of exclusive breastfeeding. In all 243 mothers, we assessed feeding pattern cross‐sectionally when the infant was 6 months old by interview. With the help of the community‐based LHWs, we were able to measure duration of exclusive breastfeeding prospectively from birth to 6 months in 223 of these women. Each participating mother was given a specially developed pictorial ‘breastfeeding calendar’. On days that the infant was exclusively breastfed, the mother placed a mark next to a picture of a breastfeeding mother. If any top‐up feed (water, formula milk or semi‐solids) was added, a mark was placed against another representative picture. The LHW visited weekly to monitor the calendar and verify the recorded information by asking another member of the family. Thus, even if the mother failed to mark the calendar, recall was kept to a maximum of 1 week (Bland et al. 2003). The LHWs were blind to the psychiatric diagnosis of the mothers. For this study, exclusive breastfeeding was defined as only breastfeeding being practised with no other semi‐solid or liquid foods (other than medication and/or oral rehydration solutions).
Breast milk quantity
The volume of breast milk produced was estimated at 4 months, using the dose‐to‐mother deuterium dilution method (Coward et al. 1982) in a convenience subsample of 30 depressed and 30 non‐depressed mothers who were exclusively breastfeeding at 4 months post‐delivery. The method has been validated in Pakistan (Wells et al. 2007). The method consists of oral administration of a fixed dose of deuterium to the mother, the fate of which is traced in the body water pool of mothers and infants by analysing their saliva and/or urine samples. At baseline, samples of saliva and urine were collected from each mother and a sample of urine collected from their infants, after which the mother received a dose of 7 mL of 99.9% deuterium oxide. Samples of saliva and urine were collected again on days 1, 2, 3, 4, 5, 13 and 14. The samples were stored at −15°C and transported to the Radiation and Isotope Applications Division, Pakistan Institute of Science and Technology Islamabad, for analysis. The detailed methods for this are described elsewhere (Wells et al. 2007). The mean 24 h volume of breast milk for 14 days (thus adjusting for day to day variation) was calculated using computer software and expressed as mL per 24 h as well as mL kg−1 body weight per 24 h.
Psychological perception of insufficient milk
We used the Perception of Insufficient Milk (PIM) questionnaire (McCarter‐Spaulding & Kearney 2001) after focus groups with the local population indicated that this was suitable for the target population. The questionnaire was translated and adapted into the local language using methods developed for earlier studies (Rahman et al. 2003). It is a self‐report, 6‐item scale with items such as ‘my breasts seem to have enough milk’, and ‘my baby generally appears satisfied after feedings’ rated on a 10‐point Likert‐type scale ranging from 0 = strongly disagree to 10 = strongly agree (min 0; max 50), with higher numbered responses indicating higher perceived adequacy of breast milk.
The PIM was administered to 243 women at 6 months post‐natally by assessors blinded to the pattern of infant‐feeding practices.
Socio‐demographic variables
Data were collected on the following sociodemographic variables and dichotomised on the basis of a priori criteria. (1) Socio‐economic status was assessed by inquiring if the household was in debt and by asking LHWs, who lived in the same locality and had intimate knowledge of the families being studied, to rate the household on a 5‐point Likert scale ranging from 1 (richest) to 5 (poorest); (2) mother financially empowered to manage household expenses (answered yes to both questions: ‘Does the head of the family give you money to run the household?’ and ‘Can you make independent decisions on how you spend it?’; (3) three or more children under the age of 7 years; (4) literacy of the mother, defined as the ability to read and write a simple text in Urdu; (5) maternal age 30 or over; (6) nuclear family (husband and children only) vs. joint family (husband, children and maternal or paternal grandparents); (7) sex of infant.
Sample size calculation
The study was designed to detect a twofold increase in risk with a precision of 0.05% and 80% statistical power. Assuming a 20% prevalence of exclusive breastfeeding (National Institute of Population Studies) among non‐depressed mothers and a 1:1 exposed to non‐exposed ratio, sample size requirements were 91 depressed and 91 non‐depressed subjects.
The sample size for breast milk quantity was calculated to detect a difference of 100 mL (about 15% of mean 24‐h production) in breast milk quantity between the two groups. For 80% power, significance of 95% and an estimated standard deviation (SD) of +100 mL, 30 mothers in each group were required.
Statistical analysis
All the analyses were carried out using SPSS for windows version 20 (SPSS Inc., Chicago, IL, USA). Characteristics of mother, family and child were compared for non‐depressed and depressed women using Fisher's exact test for dichotomous variables and t‐tests for continuous measures.
The duration of exclusive breastfeeding was censored for several mothers because they were still breastfeeding at their 6‐month interview, and therefore, this data was analysed using log‐rank tests and Cox regression analyses for survival data. In order to determine significant correlates of the duration, univariate analyses were carried out using log‐rank tests for dichotomous variables, and Spearman correlation coefficients for continuous measures. Cox regression analysis was carried out with duration of exclusive breastfeeding as the dependent variable. The independent variables were those variables found to be significant or nearly significant with P < 0.2 in the univariate analyses (age of mother, grandmother in the home, three or more children, husband's employment status, prosperity rating by LHW), mother depressed or have been associated previously with early cessation of breastfeeding (years of formal education of parents; Rahman et al. 2012). Missing values were replaced with the mean. A second Cox regression (model 2) was carried out including the same list of independent variables, but also including PIM score.
On the basis of outcome of depression over the 6‐month period, it was possible to identify three groups of mothers: (1) not depressed at either baseline or follow‐up, (2) depressed antenatally only, (3) depressed both antenatally and at follow‐up. In order to determine which factors were related to depression and persistent depression, analysis of variance and Bonferroni adjusted pairwise comparisons were carried out to compare the means of these three groups on the baby's length and weight at 6 months and PIMS score. Similar analyses using the log‐rank test were carried out for days of exclusive breastfeeding and quantity of milk in mL kg−1.
Prior to recruitment, informed verbal and written consent was obtained. Ethical approval for the study was granted by committees of the University of Manchester, UK, and the Institute of Psychiatry, Pakistan.
Results
Five hundred and ninety‐three mothers in their last trimester of pregnancy were identified in 20 union councils and interviewed using the SCID (Fig. 1). Of 160 depressed women, 132 (82.5%) were successfully recruited to the study; 10 were subsequently excluded or lost to follow‐up (Fig. 1) so 122 (92.4% of those recruited) were reassessed at follow‐up. One hundred and forty‐seven (91.8%) non‐depressed mothers were recruited; 26 were excluded or lost to follow‐up so 121 (82.3% of those were recruited) were reassessed at follow‐up (Fig. 1).
Figure 1.
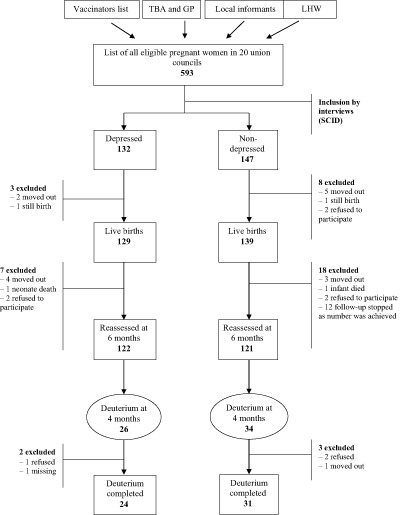
Study subjects' recruitment and attrition flow chart. TBA = Traditional Birth Attendant; GP = General Practitioner; LHW = Lady Health Worker.
Socio‐demographic characteristics of the sample
The socio‐demographic characteristics are shown in Table 1. The average age of participating women was 27.8 years (SD = 6) and all were married. The mean number of years of formal education was 4.6 (SD = 4.1) for the mothers (37% had received no formal education and 25.5% had 2–5 years) and 7.2 years (SD = 4.0) for their husband; 113 (46.5%) had three or more children, 168 (69%) were financially empowered to manage household expenses, 70 (29%) lived in nuclear families (parents and children only) while the remaining lived in extended families (three generations, or one or both parents with married sons, their wives and children). One hundred and sixty‐six (69%) of the fathers were employed by an outside agency and half of these were resident at work in a city far from home. One hundred and forty‐eight (61%) had no debt to pay, and the mean scoring of the families on the 5‐point Likert socio‐economic scale by the LHWs was 3.4 (SD = 0.8).
Table 1.
Socio‐demographic characteristics of depressed and non‐depressed mothers
| Characteristic | Whole group (n = 243) | Non‐depressed (n = 121) | Depressed (n = 122) | P * |
|---|---|---|---|---|
| Mother's characteristics mean (SD) | ||||
| Age in years | 27.8 (6.0) | 27.5 (6.0) | 28.1 (6.1) | 0.43 |
| Weight (kg) | 55.6 (11.6) | 54.5 (10.2) | 56.7 (12.8) | 0.15 |
| Height (cm) | 156.1 (5.5) | 156.4 (5.5) | 155.8 (5.5) | 0.40 |
| Body mass index | 22.8 (4.4) | 22.3 (3.8) | 23.3 (4.9) | 0.062 |
| Education and prosperity | ||||
| Mother's years of schooling | 4.6 (4.1) | 5.0 (4.1) | 4.2 (4.1) | 0.13 |
| Husband's years of schooling | 7.2 (4.0) | 7.3 (4.2) | 7.1 (3.9) | 0.69 |
| Rating of household prosperity by lady health workers | 3.4 (0.8) | 3.0 (0.6) | 3.7 (0.8) | <0.001 |
| Family characteristics n (%) | ||||
| Three or more children | 113 (46%) | 64 (53%) | 49 (40%) | 0.054 |
| Nuclear family structure | 70 (28%) | 32(26%) | 38 (31%) † | 0.48 |
| Educated person living in household/neighbourhood | 57 (24%) | 52(43%) † | 5 (4%) † | <0.001 |
| Grandmother lives in household | 129 (53%) | 75(62%) | 54 (44%) | 0.007 |
| Mother financially empowered | 168 (69%) | 112 (93%) | 56 (46%) † | <0.001 |
| Household in debt | 93 (39%) | 23 (19%) † | 70 (58%) † | <0.001 |
| Husband works for outside agency | 166 (69%) | 66 (55%) † | 100 (82%) | <0.001 |
| Baby variables n (%) | ||||
| Home delivery | 90 (37%) | 35 (29%) | 55 (45%) | 0.012 |
| Male gender | 144 (60%) | 73 (61%) † | 71 (58%) | 0.70 |
| Immunisation complete | 218 (90%) | 110 (91%) | 108 (89%) † | 0.83 |
| Baby variables mean (SD) | ||||
| Age of infant in months | 6.01 (0.59) | 5.98 (0.59) | 6.04 (0.58) | 0.44 |
| Birthweight (kg) | 2.80 (0.39) | 2.80 (0.39) | 2.80 (0.39) | 0.99 |
| Weight at 6 months (kg) | 6.93 (0.92) | 7.10 (0.88) | 6.77 (0.93) | 0.005 |
| Pattern of breastfeeding at 6 months interview n (%) | ||||
| Exclusive breastfeeding | 36 (15%) | 26 (21%) | 10 (8%) | χ 2 = 8.6 |
| Partial breastfeeding | 195 (80%) | 89 (74%) | 106 (87%) | d.f. = 2 |
| No breastfeeding | 12 (5%) | 6 (5%) | 6 (5%) | P = 0.014 |
*Comparison used t‐test for continuous variables and Fisher's exact test for dichotomous variables. †Missing data for one patient in this group.
There were no significant differences between depressed and non‐depressed women in terms of age, physical characteristics, education or family structure (Table 1). Compared with the non‐depressed group, depressed women were less likely to have an educated person or grandmother in the household, to be financially empowered and were less prosperous (Table 1). They were more likely to be in debt and to have a husband employed by an outside agency (often away from home).
The depressed mothers were more likely to have had a home delivery than the non‐depressed mothers and their babies were significantly lighter at 6 months but there were no differences in other characteristics of the infant.
At 6 months of age, infants of depressed mothers were less likely to be exclusively breastfed than infants of non‐depressed mothers (8% vs. 21%, P = 0.014).
Prospective data collected from 223 women (110 depressed and 113 non‐depressed) showed that the mean duration of exclusive breastfeeding was 100 days, standard deviation = 52 days, range 2 to 205 days, skewness = 0.06. The duration was 17 days shorter in the depressed mothers compared to non‐depressed mothers [91.8 (SD = 47.1) vs. 108.7 days (SD = 54.3); 95% CI 3.4 to 30.3; P = 0.014].
Quantity of milk in the deuterium subsample
There was no difference in the quantity of breast milk at 4 months of age between the depressed and non‐depressed mothers. The mean for the 31 depressed mothers was 89.3 mL kg−1 weight of the infant (SD = 38.1) compared with 83.9 (SD = 29.0) for the 24 non‐depressed mothers, P = 0.57. The mean kg day−1 for depressed mothers was 0.61 (SD = 0.26) compared with 0.60 (SD = 0.23) for the non‐depressed mothers, P = 0.86. The quantity of milk was not associated with any of the social factors we measured, including those associated with depression.
Multiple regression‐mediating role of perception of inadequate milk
In univariate analysis, the log‐rank test showed that the duration of exclusive breastfeeding was longer for mothers with fewer than three children (P = 0.024) and for those with a lower household prosperity rating (P = 0.012). Spearman's correlation between duration of exclusive breastfeeding and total PIMS score was 0.42, P < 0.001.
Women with depressive disorder were significantly more likely to report insufficient milk: PIM scores were 34.4 (SD = 14.3) for depressed and 39.7 (SD = 10.4) for non‐depressed women (log‐rank P = 0.004).
Cox regression, which adjusted for depression, mother's education, father's education and all the variables, which had P < 0.2, except PIMS score, showed that depression was a significant correlate of duration of exclusive breastfeeding (Table 2, model 1). The hazard ratio suggests that depressed mothers were 1.66 times as likely as non‐depressed mothers to cease exclusive breastfeeding at any point in time. The variable ‘husband employed’ was also significant in this model, suggesting that mothers whose husband was employed were 0.68 times as likely as those whose husband was not employed to cease exclusive breastfeeding at any time. Addition of PIM score to the regression analysis meant that depression was no longer a significant predictor of duration of exclusive breastfeeding (Table 2, model 2). Therefore, PIM score at 6 months appears to be an intervening variable between depression and duration of exclusive breastfeeding.
Table 2.
Cox regression analysis with dependent variable, duration of exclusive breastfeeding (n = 223)
| Maternal variable | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| Hazard ratio | 95% CI | P | Hazard ratio | 95% CI | P | |
| Age of mother | 0.99 | 0.97, 1.02 | 0.64 | 1.0 | 0.97, 1.03 | 0.93 |
| Mother's years of education | 1.02 | 0.98, 1.06 | 0.30 | 1.02 | 0.98, 1.06 | 0.28 |
| Husband's years of education | 0.98 | 0.95, 1.02 | 0.40 | 0.98 | 0.94, 1.01 | 0.18 |
| Presence of grandmother in the household | 1.03 | 0.75, 1.41 | 0.85 | 1.03 | 0.76, 1.40 | 0.85 |
| Husband employed | 0.68 | 0.49, 0.93 | 0.018 | 0.67 | 0.49, 0.93 | 0.017 |
| Rating of household prosperity by LHW | 1.17 | 0.93, 1.47 | 0.17 | 1.10 | 0.88, 1.38 | 0.41 |
| Three or more children | 1.50 | 1.07, 2.10 | 0.018 | 1.38 | 0.99, 1.93 | 0.055 |
| Mother depressed | 1.66 | 1.16, 2.38 | 0.006 | 1.42 | 0.98, 2.06 | 0.064 |
| Perception of insufficient milk | – | – | 0.97 | 0.96, 0.98 | <0.001 | |
LHW, Lady Health Workers.
Persistence of depression
Of the participants in our study, 121 women were not depressed either ante‐ or post‐natally; 69 were depressed antenatally only, and 53 were depressed at both time points. Table 3 shows significant differences between these three groups in terms of duration of exclusive breastfeeding and PIM score. In each case, the women with persistent depression had the worst outcomes; those with only antenatal depression had intermediate outcomes between the non‐depressed and persistent depressed groups.
Table 3.
Dose response effect
| n | Mean (SD) | 95% Confidence interval for mean | (P‐value) | |||
|---|---|---|---|---|---|---|
| Lower bound | Upper bound | |||||
| Baby's current weight | Non‐depressed | 121 | 7.1 (0.88) | 6.9 | 7.3 | 0.011* |
| Antenatal depression only | 69 | 6.8 (1.02) | 6.6 | 7.1 | ||
| Depressed both points | 53 | 6.7 (0.80) | 6.4 | 6.9 | ||
| Baby's current length in cm | Non‐depressed | 121 | 66.1 (2.88) | 65.6 | 66.6 | 0.001* |
| Antenatal depression only | 69 | 65.4 (3.02) | 64.7 | 66.1 | ||
| Depressed both points | 53 | 64.3 (2.75) | 63.6 | 65.1 | ||
| PIM score | Non‐depressed | 114 | 39.7 (10.41) | 37.8 | 41.7 | <0.001*, † |
| Antenatal depression only | 65 | 37.1 (14.11) | 33.6 | 40.6 | ||
| Depressed both points | 49 | 30.8 (13.80) | 26.8 | 34.8 | ||
| Exclusive breastfeeding days | Non‐depressed | 113 | 108.7 (54.33) | 98.6 | 118.8 | 0.011* |
| Antenatal depression only | 61 | 95.5 (48.75) | 83.0 | 108.0 | ||
| Depressed both points | 49 | 87.3 (44.96) | 74.4 | 100.2 | ||
| Milk in mL kg−1 ‡ | Non‐depressed | 31 | 83.9 (28.96) | 71.7 | 96.1 | 0.13 |
| Antenatal depression only | 6 | 65.3 (47.59) | 15.3 | 115.2 | ||
| Depressed both points | 18 | 95.1 (34.17) | 81.0 | 109.2 | ||
PIM, Perception of Insufficient Milk; SD, standard deviation. *The mean is significantly greater in the non‐depressed group than in the group who were depressed at both time points (using Bonferroni adjusted pairwise comparisons). †The mean is significantly greater in the antenatal depressed only group than in the group who were depressed at both time points (using Bonferroni‐adjusted pairwise comparisons). ‡Measured in 45 women who were exclusively breastfeeding at 4 months.
Discussion
There are two main findings in this study. First, we have shown in a prospective study that perinatal depression is associated with shorter duration of exclusive breastfeeding in Pakistan. This effect was most pronounced when the depression was persistent. Secondly, we found that depression was not associated with actual reduction of milk production. Using a retrospective measure, it appears that the mother's perception of insufficient breast milk production may be an intervening variable in the association between depression and duration of exclusive breastfeeding.
Our study has a number of strengths. The selection of participants was from a population‐based sample so it is likely to be representative of the mothers in rural Pakistan. The diagnosis of depressive disorder was made prior to the birth using a gold standard research interview rather than a questionnaire. The measurement of exclusive breastfeeding used a prospective method with involvement of a LHW to increase accuracy. The measurement of milk production used the gold standard deuterium method. We were able to adjust for a wide range of confounders in our multiple regression analysis. Where relevant, all measures were adapted for the local population using rigorous methodology.
The main weakness of the study was the retrospective measure of perception of milk production. In order to assess mediation, the perception of milk production should have been made at an early stage of the study. Although the assessment of exclusive breastfeeding by keeping a daily calendar could have encouraged exclusive breastfeeding, our sample's rate of Exclusive breastfeeding (EBF) of 15% was not above the national figure of 23.1% (National Institute of Population Studies 2008).
One of the key results is the length of exclusive breastfeeding in the non‐depressed group was more than 17 days longer than that in the depressed group and 22 days longer than that of the persistently depressed group. Recent systematic reviews of studies, principally in high‐income countries, point to increasing evidence that perinatal depression is associated with early cessation of exclusive breastfeeding (Dennis & McQueen 2009; Grigordias et al. 2013). Our study adds to this growing body of evidence but is one of a few studies in lower and middle‐income countries. Two small studies from Pakistan suggested that both early cessation of breastfeeding and mothers' perception of insufficient milk were associated with depression, but these studies were retrospective (Taj & Sikander 2003; Nawaz et al. 2009). One prospective study in a low‐ and middle‐income country showed that maternal depression predicted cessation of breastfeeding during the first year of life and the effect was most pronounced in more severe depression (Feldens et al. 2012).
We found that perception of milk production (measured at 6 months) mediated the association between depressive disorder and duration of exclusive breastfeeding in multiple regression analysis. This suggests that the negative perceptions associated with depressive disorder affect the mother's perception of the adequacy of their breast milk. If so, it is important to manage the depressive disorder before expecting to change the mother's perception of her breast milk production. It is particularly important to treat persistent depression.
In Low and middle income countries (LMIC), exclusive breastfeeding during the first 6 months of life is advocated as the safest, most powerful and cost‐effective intervention to reduce infant morbidity and mortality (World Health Organization 2003, World Health Organization 2011). Furthermore, especially in South Asia, perinatal depression is associated with infant undernutrition, during the first 6 months of life (Stewart 2007; Surkan et al. 2011), which could result from early cessation of breastfeeding. In Pakistan, only 55% of infants are exclusively breastfed in the first month of their lives and this rate drops to 8% at 6 months (28–30; Agha et al. 2007; Kishore et al. 2007; National Institute of Population Studies 2008).
Our study has implications for interventions in LMIC that are aimed at changing maternal perception of breast milk production, such as the one we have developed incorporating the principles of cognitive behavioural therapy (Rahman et al. 2012).
The present study also underlines the importance of detecting and managing depressive disorder as this is so common in Pakistan and is associated with early cessation of breastfeeding.
Source of funding
The study was funded through a grant awarded by the Higher Education Commission of Pakistan.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
AR and AH conceived the study. AR, AH, RB and FC developed the research design. AR, AH, RB and FC supervised all aspects of study. FM, AH, AM and SS assisted with development of instruments and training material. AM and SS assisted in data collection. BT analysed the data and tabulated the results. AR and FC wrote the first draft of the report. All authors helped to interpret findings and review the report. All authors have seen and approved the final version of the report to be published.
Acknowledgements
We acknowledge the contributions of Dr Farhat, Dr Usman, Mr Ikhlaq and Mr Wajid who helped with the data collection. Our gratitude to all the mothers, infants and their families, who took part in the study, and the health workers who assisted us in the field.
Rahman, A. , Hafeez, A. , Bilal, R. , Sikander, S. , Malik, A. , Minhas, F. , Tomenson, B. , and Creed, F. (2016) The impact of perinatal depression on exclusive breastfeeding: a cohort study. Maternal & Child Nutrition, 12: 452–462. doi: 10.1111/mcn.12170.
References
- Agha A., White F., Younus M., Kadir M.M., Ali S. & Fatmi Z. (2007) Eight key household practices of Integrated management of childhood illnesses (IMCI) amongst mothers of children 6 to 59 months in Gambat, Sindh, Pakistan. The Journal of the Pakistan Medical Association 57, 288–293. [PubMed] [Google Scholar]
- Bhutta Z.A., Thaver D., Akram D.S. & Khan M. (2004) A situation and program analysis of malnutrition among women and children in Pakistan: can we break the time warp? In: Maternal and Child Health in Pakistan: Challenges and Opportunities (ed. Bhutta Z.A.), pp. 151–172. Oxford University Press: Oxford. [Google Scholar]
- Bland R.M., Rollins N.C., Solarsh G., Van den Broeck J. & Coovadia H.M. (2003) Child Health Group. Maternal recall of exclusive breastfeeding duration. Archives of Disease in Childhood 88, 778–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coward W.A., Cole T.J., Sawyer M.B. & Prentice A.M. (1982) Breast milk intake measurement in mixed fed infants by administration of deuterium oxide to their mothers. Human Nutrition. Clinical Nutrition 36, 141–148. [PubMed] [Google Scholar]
- Dennis C.L. (2002) Breastfeeding initiation and duration: a 1990–2000 literature review. Journal of Obstetric, Gynecologic, and Neonatal Nursing 31 (1), 12–32. [DOI] [PubMed] [Google Scholar]
- Dennis C.L. & McQueen K. (2009) The relationship between infant‐feeding outcomes and postpartum depression: a qualitative systematic review. Pediatrics 123 (4), e736–e751. [DOI] [PubMed] [Google Scholar]
- Feldens C.A., Vitolo M.R., Rauber F., Cruz L.N. & Hilgert J.B. (2012) Risk factors for discontinuing breastfeeding in southern Brazil: a survival analysis. Maternal and Child Health Journal 16 (6), 1257–1265. [DOI] [PubMed] [Google Scholar]
- First M.B., Spitzer R.L. & Gibbon M. (1994) Structured Clinical Interview for Axis I DSM‐IV Disorders. Biometrics Research: New York. [Google Scholar]
- Fisher J., Cabral de Mello M., Patel V., Rahman A., Tran T., Holton S. et al (2012) Prevalence and determinants of common perinatal mental disorders in women in low‐ and lower‐middle‐income countries: a systematic review. Bulletin of the World Health Organization 90, 139G–149G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatti L. (2008) Maternal perceptions of insufficient milk supply in breastfeeding. Journal of Nursing Scholarship 40 (4), 355–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grigordias S., VonderPorten E.H., Mamisashvili L., Tomlinson G., Dennis C.L., Koren G. et al (2013) The impact of maternal depression during pregnancy on perinatal outcomes: a systematic review and meta‐analysis. The Journal of Clinical Psychiatry 74 (4), e321–e341. #. [DOI] [PubMed] [Google Scholar]
- Hill P.D., Aldag J.C., Zinaman M. & Chatterton R.T. (2007) Predictors of preterm infant feeding methods and perceived insufficient milk supply at week 12 postpartum. Journal of Human Lactation 23 (1), 32–38. [DOI] [PubMed] [Google Scholar]
- de Jager E., Skouteris H., Broadbent J., Amir L. & Mellor K. (2013) Psychosocial correlates of exclusive breastfeeding: a systematic review. Midwifery 29 (5), 506–518. [DOI] [PubMed] [Google Scholar]
- Kishore S.M., Kumar P. & Aggarwal K.A. (2007) Breastfeeding knowledge and practices amongst mothers in a rural population of north India: a community‐based study. Journal of Tropical Pediatrics 55, 183–188. [DOI] [PubMed] [Google Scholar]
- McCarter‐Spaulding D.E. & Kearney M.H. (2001) Parenting self‐efficacy and perception of insufficient breast milk. Journal of Obstetric, Gynecologic, & Neonatal Nursing 30, 515–522. [DOI] [PubMed] [Google Scholar]
- Meedya S., Fahy K. & Kable A. (2010) Factors that positively influence breastfeeding duration to 6 months: a literature review. Women and Birth: Journal of the Australian College of Midwives 23 (4), 135–145. [DOI] [PubMed] [Google Scholar]
- National Institute of Population Studies (2008) Pakistan Demographic and Health Survey 2006–07. Government of Pakistan: Islamabad. [Google Scholar]
- Nawaz R., Ur Rehman S., Nawaz S. & Mohammad T. (2009) Factors causing non‐breastfeeding in children under six months of age in district Nowshera, Pakistan. Journal of Ayub Medical College, Abbottabad 21 (4), 93–95. [PubMed] [Google Scholar]
- Rahman A., Iqbal Z., Waheed W. & Hussain N. (2003) Translation and cultural adaptation of health questionnaires. Journal of the Pakistan Medical Association 53 (4), 142–147. [PubMed] [Google Scholar]
- Rahman A., Iqbal Z., Bunn J., Lovel H. & Harrington R. (2004) Impact of maternal depression on infant nutritional status and illness: a cohort study. Archives of General Psychiatry 61, 946–952. [DOI] [PubMed] [Google Scholar]
- Rahman A., Malik A., Sikander S., Roberts C. & Creed F. (2008) Cognitive behaviour therapy‐based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster‐randomised controlled trial. Lancet 372 (9642), 902–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A., Haq Z., Sikander S., Ahmad I., Ahmed M. & Hafeez A. (2012) Using cognitive‐behavioural techniques to improve exclusive breastfeeding in a low‐literacy disadvantaged population. Maternal & Child Nutrition 8, 57–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart R.C. (2007) Maternal depression and infant growth: a review of recent evidence. Maternal & Child Nutrition 3, 94–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surkan P.J., Kennedy C.E., Hurley K.M. & Black M.M. (2011) Maternal depression and early childhood growth in developing countries: systematic review and meta‐analysis. Bulletin of the World Health Organization 89 (8), 608–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taj R. & Sikander K.S. (2003) Effects of maternal depression on breast‐feeding. Journal of the Pakistan Medical Association 53 (1), 8–11. [PubMed] [Google Scholar]
- Wells J.C.K., Bilal R., Abbass K.A., Latif Z., Roohi S. & Hafeez A. (2007) Breast‐milk intake in exclusively breastfed Pakistani infants: an estimation by deuterium dilution method. Pakistan Pediatric Journal 31, 111–119. [Google Scholar]
- World Health Organization (2003) Global Strategy for Infant and Young Child Feeding. World Health Organization: Geneva. [Google Scholar]
- World Health Organization (2011) World Health Assembly.54.2 and A54/INF.DOC.4.
- Ystrom E. (2012) Breastfeeding cessation and symptoms of anxiety and depression: a longitudinal cohort study. BMC Pregnancy and Childbirth 12, 36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zubaran C. & Foresti K. (2013) The correlation between breastfeeding self‐efficacy and maternal postpartum depression in southern Brazil. Sexual & Reproductive Healthcare 4 (1), 9–15. [DOI] [PubMed] [Google Scholar]


