Abstract
The Baby‐friendly Hospital Initiative (BFHI) is a key component of the World Health Organization/United Nations Children's Fund Global Strategy for Infant and Young Child Feeding. The primary aim of this narrative systematic review was to examine the impact of BFHI implementation on breastfeeding and child health outcomes worldwide and in the United States. Experimental, quasi‐experimental and observational studies were considered eligible for this review if they assessed breastfeeding outcomes and/or infant health outcomes for healthy, term infants born in a hospital or birthing center with full or partial implementation of BFHI steps. Of the 58 reports included in the systematic review, nine of them were published based on three randomized controlled trials, 19 followed quasi‐experimental designs, 11 were prospective and 19 were cross‐sectional or retrospective. Studies were conducted in 19 different countries located in South America, North America, Western Europe, Eastern Europe, South Asia, Eurasia and Sub‐Saharan Africa. Adherence to the BFHI Ten Steps has a positive impact on short‐term, medium‐term and long‐term breastfeeding (BF) outcomes. There is a dose–response relationship between the number of BFHI steps women are exposed to and the likelihood of improved BF outcomes (early BF initiation, exclusive breastfeeding (EBF) at hospital discharge, any BF and EBF duration). Community support (step 10) appears to be essential for sustaining breastfeeding impacts of BFHI in the longer term.
Keywords: Baby‐Friendly Hospital Initiative, breastfeeding protection, promotion and support, child health
Introduction
Infant and young child feeding practices have a strong impact on the nutrition status of children under 2 years of age as well as on their risk for infectious diseases and mortality The World Health Organization (WHO) recommends that breastfeeding be initiated within 1 h after birth, that breastfeeding be practised exclusively for the first 6 months of life followed by the introduction of safe nutritious complementary foods and that breastfeeding be continued until the child is at least 2 years old (WHO 2002). The WHO guidelines are backed up by a strong body of evidence indicating that optimal breastfeeding behaviours are strongly associated with lower incidence of gastrointestinal and respiratory tract infections as well as with child survival (Sankar et al., 2015). Furthermore, breastfeeding may protect children against otitis media (Bowatte et al., 2015), malocclusions (Peres et al., 2015), dental caries (Tham et al., 2015), obesity and type 2 diabetes (Horta et al., 2015a) and has been consistently associated with improved cognitive development (Horta et al., 2015b). Benefits to the mother include prolonged lactational amenorrhea and a reduced risk of post‐partum (pp) haemorrhage, ovarian and breast cancer, and type 2 diabetes (Chowdhury et al. 2015). Thus, it is not surprising that the WHO Global Strategy on Infant and Young Child Nutrition specifically calls for strong government commitment to protecting, promoting and supporting breastfeeding (WHO/UNICEF 2003).
The Baby‐friendly Hospital Initiative (BFHI) launched in 1991 is a key component of the WHO/UNICEF Global Strategy for Infant and Young Child Feeding (de Oliveira et al., 2003, UNICEF 1990, WHO/UNICEF 2003). BFHI is based on adherence to the Ten Steps to Successful Breastfeeding (Ten Steps; WHO 1989) and the 1981 WHO Code for Marketing of Breast Milk Substitutes (Kyenkya‐Isabirye, 1992; Naylor, 2001, UNICEF/WHO 2009) and endorses the integration of facility‐level and community‐level services (UNICEF/WHO 2009).
The Ten Steps can be considered a quality assessment and improvement system based upon specific actions in five breastfeeding domains (Table 1; UNICEF/WHO 2009, WHO 1989). (1) Policy: includes written breastfeeding (BF) policies endorsing the Ten Steps and the 1981 WHO Code; not accepting infant formula for free or at reduced cost; and forbidding direct or indirect marketing of infant formula to mothers. (2) Development of human resources: BF training of maternity ward staff. (3) Promotion and support: prenatal BF education; in‐hospital support including early BF initiation and on demand BF; and community support including referrals and in‐house support groups. (4) Protection: no infant formula; avoiding teats or pacifiers. (5) Structural changes to maternity ward workflow in the form of rooming‐in throughout the hospital stay.
Table 1.
WHO/UNICEF Ten Steps to successful breastfeeding. Baby‐Friendly Hospital Initiative systematic review
| 1. Have a written breastfeeding policy that is routinely communicated to all health care staff. |
|---|
| 2. Train all health care staff in the skills necessary to implement this policy. |
| 3. Inform all pregnant women about the benefits and management of breastfeeding. |
| 4. Help mothers initiate breastfeeding within a half‐hour of birth. |
| 5. Show mothers how to breastfeed and how to maintain lactation even if they should be separated from their infants. |
| 6. Give newborn infants no food or drink other than breast milk, unless medically indicated. |
| 7. Practice rooming‐in: allow mothers and infants to remain together 24 h a day. |
| 8. Encourage breastfeeding on demand. |
| 9. Give no artificial teats or pacifiers to breastfeeding infants. |
| 10. Foster the establishment of breastfeeding support groups and refer mothers to them on discharge from the hospital or clinic. |
WHO, World Health Organization; UNICEF, United Nations Children's Fund.
The Ten Steps can be considered a quality assessment and improvement system based upon specific actions in five breastfeeding domains. (1) Policy: includes written BF policies endorsing the Ten Steps and the 1981 WHO Code, not accepting infant formula for free or at reduced cost and forbidding direct or indirect marketing of infant formula to mothers. (2) Development of human resources: BF training of maternity ward staff. (3) Promotion and support: prenatal BF education, in‐hospital support including early BF initiation and on demand BF and community support including referrals and in‐house support groups. (4) Protection: no infant formula, avoiding teats or pacifiers. (5) Structural changes to maternity ward workflow in the form of rooming‐in throughout the hospital stay. The Ten Steps are highly interrelated with each other. If the maternal‐newborn dyad is separated immediately after birth, it is not possible to comply with step 4 (early skin‐to‐skin contact and initiation of BF). If the maternal‐newborn dyad is not rooming‐in 24 h a day (step 7), it becomes very difficult to adhere to step 6 (no breast milk supplements) and step 8 (BF on demand). If adequate prenatal education (step 3) and BF support in the maternity ward (step 5) are not available, it is unreasonable to expect that women will be able to breastfeed exclusively and on demand throughout the hospital stay. If direct or indirect marketing of infant formula is allowed, it may become extremely difficult for women to remain motivated to follow optimal BF practices even if several measures supportive of BF are in place. If there is no community support for BF once the mothers leave the maternity facility (step 10), it is unlikely that they will be able to breastfeed exclusively once they are back home and when many return work. Ten Steps implementation relies on having a well‐qualified workforce in place (step 2), and this is unlikely to happen unless there are clear written policies in place (step 1).
It is estimated that as of 2010 there were 21 328 maternity hospitals or birthing centres that had ever received the Baby‐friendly Hospital (BFH) designation worldwide (Labbok, 2012, UNICEF/WHO 2009, Baby Friendly USA, 2010). The BFHs are distributed across 160 countries with approximately 31% of maternity facilities in developing countries and 8.5% in developed countries having ever received the BFH certification (Labbok, 2012). Currently, the United States has 166 hospitals and birthing centres with the baby‐friendly designation, distributed across 41 states and the District of Columbia and accounting for 7% of annual births nationwide (Baby Friendly USA 2012).
Key messages.
The Ten Steps that form the basis of Baby‐friendly Hospital Initiative (BFHI) serve as a quality assurance system based on highly interrelated specific actions at the facility and community level.
Adherence to the BFHI Ten Steps has a positive impact on short‐term, medium‐term and longer‐term BF outcomes.
There is a dose–response relationship between the number of BFHI steps women are exposed to and the likelihood of improved breastfeeding outcomes.
Community support (step 10) is key for sustaining the short‐term breastfeeding benefits obtained from the BFHI steps requiring implementation only at the maternity ward.
Avoiding in‐hospital supplementation appears to be a key step for breastfeeding success, perhaps reflecting adequate implementation of the rest of Ten Steps.
Objectives
The primary aim of this review was to examine the impact of the BFHI package on breastfeeding and child health outcomes worldwide and in the United States. This is relevant because previous reviews have focused largely on the impact of individual BFHI steps (Perez‐Escamilla et al., 1994; WHO 1998; Dyson et al., 2005; Jaafar et al., 2011; Jaafar et al., 2012; Moore et al., 2012). Because the United States is in the midst of major policy decisions regarding future strategies and investments in breastfeeding protection, promotion and support (National Academies of Sciences, Engineering, and Medicine, 2015), findings specific to the United States are also examined.
Methods
The specific research questions were designed, and the literature search was conducted using the PICOS (Participants, Interventions, Comparators, Outcomes, Study Design) model for evidenced‐based medical research (Table 2; Liberati et al., 2009).
Table 2.
PICOS model for evidence‐based medical research questions. Baby‐Friendly Hospital Initiative systematic review
| Population |
|---|
| Women who deliver a healthy, full‐term infant in a hospital or birthing centre. |
| Intervention |
| Research question: Is there an impact of BFHI on breastfeeding and infant health outcomes globally and in the USA? |
| Comparison |
| Women not exposed to the Ten Steps; degree of exposure to the Ten Steps. |
| Outcomes |
| Exclusive breastfeeding at discharge through 6 months post‐partum. Any breastfeeding at discharge through 12 months post‐partum. Onset of lactation. Infant health outcomes: gastrointestinal infection, upper and lower respiratory tract infection, otitis media, allergies, asthma, obesity and intelligence. |
| Study designs |
| Randomized controlled trials quasi‐experimental designs (with or without a parallel reference group), prospective studies cross‐sectional studies |
Eligibility criteria
The specific inclusion and exclusion criteria are listed in Table 3. In brief, observational, quasi‐experimental and experimental studies of both primiparous and multiparous women were included if they assessed BF outcomes and/or infant health outcomes for healthy, term infants born in facilities designated as baby friendly or implementing at least three or all of the BFHI steps but not designated as baby friendly. Studies that assessed the impact of community‐based initiatives connected to BFHs were also included (i.e. Baby‐friendly Primary Care Units and referral to home‐based peer counselling at discharge from BFH).
Table 3.
Study inclusion and exclusion criteria. Baby‐Friendly Hospital Initiative systematic review
| Inclusion criteria |
|---|
| Studies that |
| 1. Assessed breastfeeding outcomes for women who delivered a healthy term infant in a baby friendly‐designated hospital or birthing centre |
| 2. Assessed breastfeeding outcomes for women who were exposed to a combination of at least three BFHI steps |
| 3. Assessed breastfeeding outcomes for women who were exposed to Baby Friendly Community initiatives or community support linked to a baby friendly hospital |
| 4. Assessed infant health outcomes for women who delivered a healthy term infant in a Baby Friendly‐designated hospital or birthing centre |
| 5. Assessed infant health outcomes for women who were exposed to a combination of BFHI steps |
| 6. Assessed infant health outcomes for women who were exposed to Baby Friendly Community initiatives or community support linked to a Baby Friendly hospital |
| 7. Study conducted in low‐income, middle‐income and high‐income countries |
| Exclusion criteria |
| Studies that |
| 1. Had an ecological design |
| 2. Included women who delivered a preterm/sick infant |
| 3. Included women who were HIV positive |
| 4. Included women who delivered at home |
| 5. Included women and infants with breastfeeding contraindications |
| 6. Were published in languages other than English, Spanish or Portuguese |
Information sources
MEDLINE, EMBASE, Global Health, CINAHL, PUBMED and Web of Science were searched from their dates of inception to December 2012. Hand searches were conducted of the bibliographies of each of the manuscripts considered eligible for the study as well as of relevant background articles.
Search strategy
Literature searches were conducted by two of the authors (JM and RPE). Databases were searched using different combinations of the terms ‘baby friendly’, ‘Ten Steps’ and ‘hospital practices’ as text words. The Medical Subject Heading (MeSH) term ‘breastfeeding’ was exploded (i.e. expanded to include all sub‐terms) and combined with the text word searches to obtain the final set of articles (i.e. infant health outcomes were extracted from the literature identified through this search approach). Infant health outcomes examined were gastrointestinal infection, upper and lower respiratory tract infection, otitis media, allergies, asthma, obesity and intelligence.
Study selection
All records were imported into EndNote X6. Duplicates were removed, followed by a review of titles and abstracts. Once articles were removed based on titles and abstracts, a full text review was conducted of the remaining articles.
Data collection process
Structured forms were developed to extract key information from each article including study design, outcomes and results. Data extraction was carried out by the first author (RPE).
Quality assessment
The quality of the studies was assessed using a modified version of the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology (Table 4; Guyatt et al., 2011). Studies were classified as being of either high, moderate, low or very low quality, taking into account the study design and key design features including sample size, exposure and outcome measures, random allocation procedures (when applicable), inclusion of control or reference group and statistical analyses. RCTs were initially considered to be of high quality and quasi‐experimental studies of medium quality but could be downgraded based on study design limitations. Prospective studies were considered to be of moderate quality but could be downgraded or upgraded up to moderate quality. Cross‐sectional and retrospective studies were considered to be of low quality but could be downgraded or upgraded. Quality assessment was performed by two authors (RPE and SSP) based on independent rankings and a consensus process.
Table 4.
Summary of study quality by outcome, study design and location. Baby‐Friendly Hospital Initiative systematic review.
| Outcome | Study design | Quality | Global | USA |
|---|---|---|---|---|
| Breastfeeding | Cross‐sectional/retrospective | Very low | Narchi et al. (2009) | Dabritz et al. (2009) |
| Shilpa et al. (2009) | ||||
| Vieira et al. (2006) | Declercq et al. (2009) | |||
| Ojofeitimi et al. (2000) | ||||
| Bartington et al. (2006) | Rosenberg et al. (2008) | |||
| Weng et al. (2003) | ||||
| Rivera‐Lugo et al. (2007) | ||||
| Silva et al. (2008) | ||||
| Low | Sampaio et al. (2011) | Merewood et al. (2005) | ||
| Venancio et al. (2002) | ||||
| Broadfoot et al. (2005) | ||||
| Helsing et al. (2002) | ||||
| Mydlilova et al. (2009) | ||||
| Moderate | De Oliveira et al. (2003) | — | ||
| Merten et al. (2005) | ||||
| Venancio et al. (2012) | ||||
| Prospective | Very Low | Chien et al. (2007) | — | |
| Giovannini et al. (2005) | ||||
| Dulon et al. (2003) | ||||
| Low | Pincombe et al. (2008) | Kuan et al. (1999) | ||
| Tarrant et al. (2011) | Murray et al. (2007) | |||
| Nickel et al. (2012) | ||||
| Moderate | — | DiGirolamo et al. (2001) | ||
| DiGirolamo et al. (2008) | ||||
| Perrine et al. (2012) | ||||
| Quasi‐experimental without parallel comparison group | Very Low | Caldeira and Goncalves (2007) | — | |
| Bosnjak et al. (2004) | ||||
| Coutinho et al. (2005b) | ||||
| Duyan Camurdan et al. (2007) | ||||
| Dasgupta et al. (1997) | ||||
| Low | Braun et al. (2003) | Wright et al. (1996) | ||
| Cattaneo and Buzzetti (2001) | Philipp et al. (2001) | |||
| Garcia‐de‐Leon‐Gonzalez et al. (2011) | Philipp et al. (2003) | |||
| Ingram et al. (2011) | ||||
| Zakarija‐Grkovic et al. (2012) | ||||
| Moderate | Valdes et al. (1993) | — | ||
| Quasi‐experimental with parallel comparison group | Very Low | Martens (2000) | — | |
| Low | Abolyan (2006) | — | ||
| Gau (2004) | ||||
| Moderate | Lutter et al. (1997) | — | ||
| RCT | High | Kramer et al. (2001) | — | |
| Coutinho et al. (2005a) | ||||
| Taddei et al. (2000) | ||||
| Child health | RCT | Moderate | Kramer et al. (2007c) | — |
| High | Kramer et al. (2001) | — | ||
| Kramer et al. (2002) | ||||
| Kramer et al. (2007a) | ||||
| Kramer et al. (2007b) | ||||
| Kramer et al. (2008a) | ||||
| Kramer et al. (2008b) |
Results
Results are presented below by geographic location (global vs. United States only) and by study design. From the 834 records originally identified, 58 articles were included in the final review (Fig. 1). Data extracted for each study are presented in WebAppendix Tables 1, 2, 3, 4 in Supporting Information.
Figure 1.
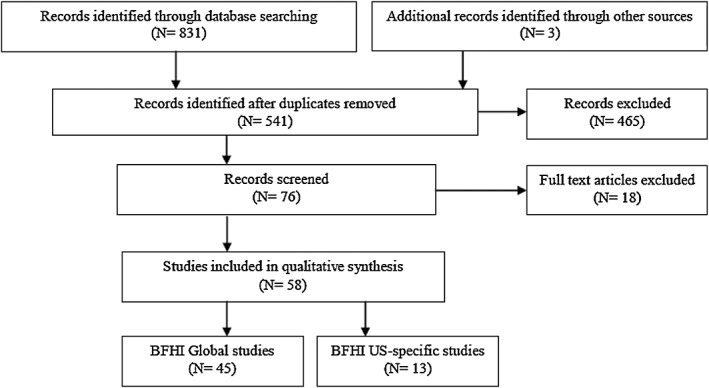
Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) flow diagram. BHFI, Baby‐friendly Hospital Initiative.
Randomized controlled trials
Study quality
Nine of the 58 articles identified were derived from three RCTs conducted in Belarus and Brazil. The Promotion of Breastfeeding Trial (PROBIT) was rated as high quality for all outcomes (Kramer et al., 2001; Kramer et al., 2002; Kramer et al., 2007a; Kramer et al., 2007b; Kramer et al., 2008a; Kramer et al., 2008b) except oral health as there was a high degree of measurement clustering by polyclinic (Kramer et al., 2007c). The two Brazilian studies were of medium (Taddei et al., 2000) and high (Coutinho et al., 2005a) quality.
Studies' description and findings
The large‐scale clustered RCT PROBIT found that the implementation of the Ten Steps had a positive impact on exclusive breastfeeding (EBF) and any breastfeeding (ABF) duration and a significant decrease in the incidence of gastrointestinal infections and atopic eczema at 1 year of age (Kramer et al., 2001). However, the intervention did not have an impact on respiratory tract infections (Kramer et al., 2001), infant weight outcomes or head circumference at 12 months (Kramer et al., 2002). PROBIT's 6.5‐year pp follow‐up study found a positive intervention effect on children's IQ and academic performance (Kramer et al., 2008a) but not on anthropometry or blood pressure outcomes (Kramer et al., 2007b), asthma and allergy risk (Kramer et al., 2007a), dental health (Kramer et al., 2007c), child behaviour or maternal adjustment (Kramer et al., 2008b). Interestingly, PROBIT had a positive impact on the likelihood that the mother would breastfeed her subsequent child for at least 3 months (Kramer et al., 2008b).
The RCT conducted by Coutinho et al. in Brazil found that strengthening step 10 by adding home peer counselling had a significant positive impact of the intervention on the prevalence of EBF and ABF among 0‐ to 6‐month‐old infants (Coutinho et al., 2005a). Taddei et al. did not find an impact of BFHI on ABF duration among Brazilian women delivering in eight hospitals that were randomly assigned to Ten Steps training or to continue the standard of care (Taddei et al., 2000).
Experimental evidence conclusions
High‐quality RCTs indicate that BFHI implementation leads to improvements in EBF and ABF and health benefits among infants and school‐aged children. Long‐term sustainability of breastfeeding improvements is likely to rely on the strong implementation of step 10. This is based on three important findings: (1) the success of PROBIT and the fact that the trial involved strong implementation of BF promotion and support by trained polyclinic personnel; (2) the findings from Coutinho et al. (2005a) regarding the addition of home peer counselling to step 10; and (3) the lack of BF benefits shown in an RCT with weak step 10 implementation (Taddei et al., 2000).
Quasi‐experimental
Eighteen quasi‐experimental studies conducted in Brazil, Canada, Chile, Croatia, India, Italy, Russia, Spain, Taiwan, Turkey, United States and the UK have examined the association between BFHI and BF outcomes.
Quasi‐experimental with parallel comparison group
Study quality
Four quasi‐experimental studies conducted in Brazil (Lutter et al., 1997), Canada (Martens, 2000), Russia (Abolyan, 2006) and Taiwan (Gau, 2004) included a parallel comparison group. The quality of these studies was very low (Martens, 2000), low (Gau, 2004; Abolyan, 2006) and moderate (Lutter et al., 1997).
Studies' description and findings
In Taiwan, delivering in BFHs was associated with higher BF initiation and a higher prevalence of EBF and ABF across time (Gau, 2004). In a Canadian hospital serving a predominantly aboriginal population, in‐hospital EBF rates increased significantly after exposure to a brief in‐service BFHI maternity staff training (Martens, 2000). Women delivering in a BFH in Santos, Brazil with strong step 10 implementation had significantly higher EBF duration compared with their counterparts delivering in a hospital with partial implementation of the Ten Steps that did not include step 10 (Lutter et al., 1997). Russian women giving birth in four certified BFHs had better in‐hospital BF behaviours (earlier BF initiation and higher EBF prevalence at hospital discharge) than their counterparts delivering in non‐certified hospitals (Abolyan, 2006).
Pre‐post BFHI implementation without parallel comparison group
Study quality
Fourteen pre–post studies without a parallel comparison group were conducted in Brazil, Chile, Croatia, India, Italy, Spain, Turkey, UK and the United States. Five studies were of very low quality (Dasgupta et al., 1997; Bosnjak et al., 2004; Coutinho et al., 2005b; Caldeira & Goncalves, 2007; Duyan Camurdan et al., 2007), eight of low quality (Wright et al., 1996; Cattaneo & Buzzetti, 2001; Philipp et al., 2001; Braun et al., 2003; Philipp et al., 2003; Garcia‐de‐Leon‐Gonzalez et al., 2011; Ingram et al., 2011; Zakarija‐Grkovic et al., 2012) and one of moderate quality (Valdes et al., 1993).
Studies' description and findings
A Brazilian study found that a 18‐h BFHI training of maternity staff led to improvements in adherence to some of the Ten Steps (early skin‐to‐skin contact, BF positioning support and not offering supplements or pacifiers) and to EBF (Coutinho et al., 2005b). However, EBF rates remained very low suggesting the need to strengthen step 10 (Coutinho et al., 2005b). A study conducted in Brazil found a positive adjusted association of BFHI implementation in one hospital with EBF duration and breastfeeding continuation at 4 months pp (Braun et al., 2003). Another Brazilian study with a pre/post cross‐sectional design also found a positive association of BFHI with increased EBF, full breastfeeding (FBF) and ABF duration (Caldeira & Goncalves, 2007).
In a hospital in India, women delivering vaginally or via caesarean section 6 months after BFHI certification began breastfeeding earlier compared with women who delivered 6 months before the hospital was certified as baby friendly (Dasgupta et al., 1997). The study, however, did not document pre–post group equivalence and did not adjust findings for potential confounders. A study conducted in eight Italian hospitals distributed across two regions found a positive association between BFHI implementation, EBF at hospital discharge, EBF at 3 months and ABF at 6 months (Cattaneo & Buzzetti, 2001). A medical records study conducted in one Turkish hospital covering the first 24 months pp found that BFHI implementation was associated with a 1.5 times increase in breastfeeding duration, but there was no association with EBF across time pp (Duyan Camurdan et al., 2007). In agreement with this study, a maternity records study conducted in one hospital in Spain found that the median breastfeeding duration increased progressively across time after BFHI programme implementation (Garcia‐de‐Leon‐Gonzalez et al., 2011).
A UK study involving Baby Friendly Initiative training of home‐visiting staff in a primary care trust found that the likelihood of breastfeeding initiation and ABF at 8 weeks pp was significantly higher in the year following (vs. 2 years before) implementation of the intervention (Ingram et al., 2011). Chilean women attending a post‐natal outpatient BF support clinic linked with a BFH who delivered after BFHI implementation had higher in‐hospital EBF and FBF rates at 6 months and a lower likelihood of weaning from the breast by 6 months compared with their counterparts delivering before BFHI implementation. Women delivering post‐BFHI implementation were also more likely to remain amenorrheic at 6 months pp (Valdes et al., 1993).
A study conducted in Arizona, USA, found that BFHI implementation was associated with greater likelihood of breastfeeding initiation within 1 h of birth and lower likelihood of in‐hospital formula supplementation (Wright et al., 1996). In this study, after adjusting for potential confounders, breastfeeding duration was longer among those not receiving in‐hospital supplementation, not given formula discharge/coupons and rooming‐in >60% of time. A study conducted in Boston, USA (Philipp et al., 2001) found that in‐hospital BF outcomes improved in a maternity hospital after implementation of BFHI and these improvements remained in place 2 years post‐accreditation (Philipp et al., 2003).
A national study conducted in Croatia found that ABF rates improved from pre to post BFHI implementation, and ABF rates increased even further after community‐based support groups were introduced as part of the national breastfeeding programme strategy (Bosnjak et al., 2004). A more recent study conducted in a maternity ward in Croatia that assessed BFHI steps 4 to 9 found that exposing maternity staff to the 20‐h UNICEF/WHO BFHI training led to greater adherence to some steps 4 (early contact), 7 (rooming‐in) and 8 (BF on demand) (Zakarija‐Grkovic et al., 2012). The intervention increased EBF during the first 48 h after birth but was not associated with longer‐term benefits in breastfeeding outcomes. This was not surprising as post‐training, 79% of infants were still receiving in‐hospital supplementation.
Quasi‐experimental evidence conclusions
Consistent but limited quality quasi‐experimental studies suggest that BFHI is associated with improved in‐hospital and post‐discharge BF outcomes. Because studies were collected in 12 different countries, these findings strengthen the external validity of the high‐quality RCTs reported previously. Consistent but limited quality quasi‐experimental studies suggest that step 10 needs to be well implemented for BFHI to have longer‐term impacts on breastfeeding outcomes (Lutter et al., 1997; Coutinho et al., 2005b).
Observational
Prospective
Study quality
Eleven of the studies identified in this systematic review were prospective. Six were conducted in the United States and one each in Taiwan, Italy, Germany, Australia and Hong Kong. Three studies were classified as being of very low quality (Dulon et al., 2003; Giovannini et al., 2005; Chien et al., 2007), five of low quality (Kuan et al., 1999; Murray et al., 2007; Pincombe et al., 2008; Tarrant et al., 2011 Nickel et al., 2012) and three of medium quality (DiGirolamo et al., 2001; DiGirolamo et al., 2008; Perrine et al., 2012).
Studies' description and findings
Maternal rating of in‐hospital breastfeeding support experience was positively associated with meeting prenatal‐intended breastfeeding duration in the United States (Kuan et al., 1999). In a sub‐sample of women who received breastfeeding support at home from a visiting nurse, both the rating of breastfeeding support experience in the maternity ward and at home were associated with breastfeeding success (Kuan et al., 1999). The US Infant Feeding Practices Study (IFPS I) found an inverse dose–response association between the number of BFHI steps that women were exposed to and the likelihood of stopping BF by 6 weeks pp (DiGirolamo et al., 2001). Multivariate analyses also documented that, of the five BFHI steps women were asked to recall, initiating BF >1 h pp and in‐hospital formula supplementation were the strongest risk factors for stopping BF by 6 weeks pp. A replication study conducted by the same group with IFPS II confirmed these findings with data collected 11 years later (DiGirolamo et al., 2008). Another IFPS II analysis also found a dose–response relationship between exposure to the six BFHI steps as recalled by mothers and median BF duration (Nickel et al., 2012). Lack of exposure to steps 6, 4 and 9 together or 8 and 9 together was associated with the greatest decrease in BF duration. Another US study examining the six BFH practices recalled by participants in the IFPS II found that women whose infants were not provided with in‐hospital formula supplementation were more likely to meet their prenatal EBF duration intention (Perrine et al., 2012).
A prospective Italian study found that lack of exposure to steps 6 (in‐hospital supplementation), 7 (rooming‐in) or 8 (BF on demand) increased the odds of practising predominant breastfeeding (vs. EBF) in the maternity ward and that in‐hospital predominant breastfeeding (vs. EBF) was associated with shorter FBF duration (Giovannini et al., 2005). A German study found that women delivering in hospitals with a high (vs. low) breastfeeding promotion Ten Steps index were more likely to breastfeed at 4 months pp (Dulon et al., 2003). A mailed questionnaire study conducted in Colorado, USA, found that five out of nine breastfeeding practices examined (breastfeeding within 1 h pp, no infant feeding supplements, rooming‐in, no pacifier and pp phone contact) were associated with an increased likelihood of breastfeeding at 8 weeks (Murray et al., 2007). Women exposed to these five hospital practices had longer breastfeeding durations after adjusting for socio‐economic status. Hong Kong women exposed to six of the Ten Steps, as documented in their hospital records, were three times more likely than those exposed to none or only one of the steps to breastfeed for more than 8 weeks pp after adjusting for confounders (Tarrant et al., 2011). Multivariate analyses also showed that feeding only breast milk in the maternity ward and providing information on breastfeeding support after hospital discharge were the only steps that independently predicted longer breastfeeding duration. An Australian study with primiparous women found that breastfeeding on demand was the only practice, out of six, associated with increased breastfeeding duration (Pincombe et al., 2008).
Summary of prospective evidence
Consistent but limited evidence suggests that exposure to BFH step(s) is associated with improved BF outcomes. There is a dose–response synergistic association between the number of steps women recall being exposed to and improved BF outcomes. Findings support that even a partial implementation of steps (vs. all or none approach) improves breastfeeding outcomes. Consistent with one quasi‐experimental study, four studies found lack of compliance with step 6 to be a risk factor for poor breastfeeding outcomes.
Cross‐sectional/retrospective
Study quality
Twenty cross‐sectional/retrospective studies were identified. Seven were conducted in Brazil, four in the United States and one each in Scotland, the UK, Russia, Puerto Rico, the Czech Republic, India, Nigeria, Switzerland and Taiwan. Eleven studies were classified as being of very low quality (Ojofeitimi et al., 2000; Weng et al., 2003; Bartington et al., 2006; Vieira et al., 2006; Rivera‐Lugo et al., 2007; Rosenberg et al., 2008; Silva et al., 2008; Dabritz et al., 2009; Declercq et al., 2009; Narchi et al., 2009; Shilpa et al., 2009), six of low quality (Helsing et al., 2002; Venancio et al., 2002; Broadfoot et al., 2005; Merewood et al., 2005; Mydlilova et al., 2009; Sampaio et al., 2011) and three of moderate quality (de Oliveira et al., 2003; Merten et al., 2005; Venancio et al., 2012).
Studies' description and findings
A retrospective study that interviewed women at 9 months pp found that UK women delivering at BFH units were more likely to initiate breastfeeding but were not more likely to continue breastfeeding by 1 month pp (Bartington et al., 2006). Consistent with RCT findings (Coutinho et al., 2005a), this study suggested that step 10 was weak and would need to be strengthened to increase BF duration. A Scottish study that reviewed clinical screening records from 33 maternity wards found that the prevalence of breastfeeding at 7 days pp was higher among women delivering in hospitals certified as baby friendly vs. not certified (Broadfoot et al., 2005). A retrospective study conducted in California, USA, found that among women with 6‐ to 8‐month‐old infants who had returned to work, ‘almost’ EBF at 6 months (defined as breast milk as the sole source of milk allowing for occasional intake of other water‐based fluids) was positively associated with in‐hospital EBF, and receipt of a phone number from staff for pp BF support, and inversely associated with receipt of hospital discharge packs (Dabritz et al., 2009).
Brazilian mothers with <6‐month‐old infants attending Primary Health Care Units (PHCUs) with fair baby friendly performance, as determined by a 10‐item baby friendly primary health care unit score, had higher EBF rates compared with their counterparts attending PHCUs with poor baby friendly performance (de Oliveira et al., 2003).
Russian women delivering in a BFH had a higher likelihood of initiating breastfeeding earlier and a lower likelihood of the infant receiving infant formula supplements (Helsing et al., 2002). A national retrospective phone and internet survey found that US women delivering in hospitals that followed six to seven steps (vs. none to one) were more likely to meet their late pregnancy EBF intentions (Declercq et al., 2009). Among primiparae, the specific steps associated with meeting prenatal EBF intentions were as follows: help with breastfeeding initiation, no in‐hospital formula/water supplementation, community resources and no pacifiers. Among multiparae, the corresponding steps were as follows: no in‐hospital formula/water supplementation and breastfeeding on demand.
A study conducted in Puerto Rico found that maternal perception of compliance with the Ten Steps was positively associated with a higher likelihood of in‐hospital FBF (vs. partial BF) (Rivera‐Lugo et al., 2007). A US study that reviewed medical records or birth certificate data from 28 hospitals that had received the BFHI accreditation in 2001 and had retained it by 2003 found that the in‐hospital rates of BF initiation and EBF were higher compared with national data (Merewood et al., 2005). A national Swiss cross‐sectional study that interviewed women who had given birth within 9 months preceding the survey documented that delivering in a BFH was associated with longer EBF, FBF and ABF duration (Merten et al., 2005). The steps associated with longer ABF duration in multivariate analyses were rooming‐in, first BF within 1 h pp, BF on demand and no pacifier use.
A national cross‐sectional chart review conducted in the Czech Republic found higher likelihood of EBF at the time of hospital discharge in BFH vs. non‐BFH hospitals (Mydlilova et al., 2009). A small retrospective cohort study from Brazil that recruited women who attended all breastfeeding education sessions offered at a primary health care centre found that EBF between 60 and 180 days pp was more likely among women that gave birth in BFH vs. non‐BFH (Narchi et al., 2009). In that study, rooming‐in was associated with an increased likelihood of EBF. Giving birth in a BFH in Nigeria was associated with higher likelihood of having initiated breastfeeding within 30 min pp and of EBF at the time of the survey (Ojofeitimi et al., 2000).
A cross‐sectional review of metabolic screening forms conducted in Oregon, USA, among women delivering in 57 hospitals found that a higher (vs. lower) Ten Steps adherence score was associated with higher likelihood of BF at 2 days and 2 weeks pp (Rosenberg et al., 2008). In this study, the only individual step associated with breastfeeding success was the hospital having a written breastfeeding policy. This step may be a proxy for better adherence to Ten Steps as strong collinearity was found among individual steps. A cross‐sectional Brazilian study that interviewed women with infants <5‐month‐old attending five community centres found that those delivering in BFHs (vs. non‐BFHs) had longer breastfeeding duration (Sampaio et al., 2011). A very low quality retrospective study conducted in India found no differences in prelacteal feedings or EBF among women who gave birth in a BFH vs. in non‐BFHs (Shilpa et al., 2009).
A cross‐sectional Brazilian study with mothers of infants <1‐year old attending immunization clinics found that birth in a BFH was associated with a higher prevalence of EBF among infants <4 months and ABF among infants <1 year (Venancio et al., 2002). Consistent with these findings, a more recent national immunization campaign Brazilian survey found that being born in a BFH was associated with timely breastfeeding initiation and longer EBF duration (Venancio et al., 2012). A retrospective study conducted in Brazil also targeting women with infants <1‐year old attending immunization clinics documented that women who delivered in BFHs were less likely to self report having had experienced mastitis (Vieira et al., 2006). A study from Pelotas, Brazil, found that infants born in a BFH were more likely to be doing EBF at 1 month pp compared with their counterparts born in non‐BFHs, although this association was only marginally significant (Silva et al., 2008). Findings from a cross‐sectional Taiwanese study indicate that women delivering in BFHs had higher rates of EBF and ABF both in the hospital and at 1 month pp (Weng et al., 2003).
Cross‐sectional/retrospective evidence conclusions
Consistent but limited quality evidence from 19 out of 20 cross‐sectional/retrospective studies suggests that infants born in BFHs (vs. non BFHs) are more likely to be exclusively breastfed and to be breastfed for longer. Evidence from one medium quality study (de Oliveira et al., 2003) suggests that Baby Friendly Primary Health Care Units are likely to increase the chances of EBF. Study findings were subsequently confirmed by an RCT in the same population (Coutinho et al., 2005a).
United States results
Thirteen out of the 58 studies that met the inclusion criteria of this systematic review were conducted in the United States (Wright et al., 1996; Kuan et al., 1999; DiGirolamo et al., 2001; Philipp et al., 2001; Philipp et al., 2003; Merewood et al., 2005; Murray et al., 2007; DiGirolamo et al., 2008; Rosenberg et al., 2008 Dabritz et al., 2009; Declercq et al., 2009; Nickel et al., 2012; Perrine et al., 2012). None of the studies were RCTs and thus none were classified as high quality (Table 4). Nevertheless all studies support the acceleration of the implementation of the Baby Friendly Initiative nationwide. No studies conducted in the United States examined the impact of BFHI on child health outcomes.
Conclusion
The global evidence consistently supports the conclusion that adherence to the BFHI Ten Steps has a positive impact on short‐term, medium‐term and longer‐term BF outcomes across geographies. Of the 58 studies that met the systematic review criteria, 55 support this relationship, and none suggest a negative impact of BFHI on BF outcomes. The vast majority of the research identified and reviewed herein is observational in nature given the moral and ethical considerations inherent in randomly assigning infants to breastfeed or not. Per the study quality definitions then, most of the evidence could not be ranked as high quality. However, we found that the observational evidence fully supports the experimental (e.g. randomization to the Ten Steps) and quasi‐experimental findings reviewed. Our findings are in full agreement with a previous review supporting the implementation of ‘structured programmes’ to improve breastfeeding initiation as well as duration of any BF and EBF (Beake et al., 2012). The authors of that review defined a ‘structured programme’ as ‘a multifaceted approach to support breastfeeding that targeted change at organizational, service delivery and individual behaviour levels, for example, implementation of the 10 steps of the BFHI’ (Beake et al., 2012).
Observational studies suggest that there is a dose–response relationship between the number of BFHI steps women are exposed to and the likelihood of improved BF outcomes. The high‐quality PROBIT RCT conducted in Belarus also supports a positive impact of BFHI on some but not all infant and child health outcomes examined. Unfortunately, there were no additional moderate or high‐quality studies examining these relationships. It is noteworthy that with the exception of one study examining the association between BFHI and mastitis (Vieira et al., 2006) and one study examining lactational amenorrhea (Valdes et al., 1993), studies did not report maternal health outcomes.
All of the United States BFHI evidence comes from observational studies, the vast majority of which are of very low or low quality. Although there is consistent empirical evidence that BFHI has led to improvements in breastfeeding outcomes in the very short and short terms, its impact on BF outcomes in the long term remains unclear. Stronger study designs (e.g. RCTs and/or quasi‐experimental with a baseline equivalent parallel reference group) need to be implemented in the United States to better understand the impact of the BFHI on BF and child health outcomes. The external validity of BFHI studies conducted abroad to the United States is indeed limited because of the major differences in social, cultural and regulatory environments that influence breastfeeding behaviours (Giovannini et al., 2005; Perez‐Escamilla, 2012; Perez‐Escamilla & Chapman, 2012).
An important finding from this systematic review is that community support (step 10) appears to be key for long‐term sustainability of the short‐term breastfeeding gains obtained as a result of BFHI efforts focusing solely in maternity facilities. The PROBIT trial, for example, focused not only on the maternity hospitals but also on the polyclinics proving post‐natal paediatric care. The RCT by Coutinho in Brazil (Coutinho et al., 2005a) found that adequate implementation of step 10 (defined as home visits by peer counsellors) is needed for long‐term impacts on ABF and EBF. Also in Brazil, De Oliveira et al. (2003) documented that greater adherence to Primary Health Care Unit Baby Friendly steps was associated with improved EBF and ABF rates during the first 6 months pp. Additional quasi‐experimental and observational studies also provide indirect evidence in support of this finding (i.e. low ABF rates in the short term in the absence of a well‐implemented step 10) (de Oliveira et al., 2003; Silva et al., 2008; Coutinho et al., 2005b; Lutter et al., 1997). The central importance of step 10 calls for increasing investments on structured programmes at the community level such as the Baby Friendly Primary Health Care initiative from Brazil (de Oliveira et al., 2003) and the Supplemental Nutrition Program for Women, Infants and Children (WIC) breastfeeding peer counselling programme in the United States [National Academies of Sciences, Engineering, and Medicine (2015)].
Findings from studies measuring degree of exposure to the Ten Steps are encouraging but need to be interpreted with caution because of possible maternal recall (e.g. successful BF women may be more likely to recall having received in‐hospital BF support) or indication (women receiving help on BF may have been those experiencing BF difficulties) biases.
Even though this systematic review excluded studies focusing on a single BFHI step, several articles (Chien et al., 2007; DiGirolamo et al., 2001; DiGirolamo et al., 2008; Giovannini et al., 2005; Tarrant et al., 2011; Zakarija‐Grkovic et al., 2012) reported that lack of adherence to step 6 (in‐hospital supplementation) was a major risk factor for poor BF outcomes. However, it is not possible to conclude that step 6 regardless of how the remaining steps are implemented should be the sole focus of BF promotion and support in maternity wards. Step 6 is indeed likely to be a reflection of adequate implementation of steps 1 thru 9 because each of the Ten Steps is indeed highly interconnected with the others, structurally and physiologically, and the steps are statistically correlated with each other (Merewood et al., 2005, UNICEF/WHO 2009, Wright et al., 1996).
Breastfeeding is a behaviour that is influenced by a multitude of internal and external motivational factors. It is recommended that future research takes into account psychosocial constructs that can help to explain these motivational influences and simultaneously fill the knowledge void between intentions and behaviours in healthy lifestyles research (Perez‐Escamilla, 2012; Perez‐Escamilla & Chapman, 2012; Schwarzer, 2008; Venancio et al., 2012).
A limitation of our review is that we were unable to compare the impact of partial vs. full implementation of the Ten Steps. We did not undertake this comparison because there was a high degree of variability in terms of which combinations of steps were implemented across studies and also because recall studies can only probe for those steps that mothers can be expected to remember (i.e. steps 3 thru 10) but not others [step 1 (written policy), step 2 (training of health facility staff)]. A second limitation of our systematic review is that it examined primiparous and multiparous women together, however, both groups of women have different BF protection, promotion and support needs. It was not possible to analyse the differential impact of BFHI based on parity as most studies included both groups of women and did not report the findings by parity. In spite of this limitation, our findings have strong policy implications for the general population of women and infants (see Key messages box). This review strongly supports additional investments in the expansion and financing of quality implementation of BFHI globally. Although there may be other structured approaches to protection, promotion and support of breastfeeding that may be as efficacious as the BFHI, the global political commitment to the BFHI makes it an obvious structured evidence‐based approach to pursue.
Source of funding
This systematic review was funded by the CDC, USA.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
RPE was responsible for conception of study. RPE and JM designed the review strategy and conducted electronic searches. RPE and SSP extracted studies' data and assessed quality of studies. RPE drafted initial version of manuscript. All co‐authors participated in manuscript preparation and critically reviewed all sections of the text. Final approval of the version to be published was given by RPE and JM.
Supporting information
Supporting Information
Supporting Information
Supporting Information
Acknowledgements
We would like to thank Dr Donna J. Chapman (Springfield College, Massachusetts), Rosie Li (Centers for Disease Control and Prevention (CDC), USA), Cria Perrin (CDC), Kelley Scanlon (CDC) and Larry Grummer‐Strawn (World Health Organization, Geneva; formerly at CDC) for their thoughtful input on previous versions of this systematic review.
Pérez‐Escamilla, R. , Martinez, J. L. , and Segura‐Pérez, S. (2016) Impact of the Baby‐friendly Hospital Initiative on breastfeeding and child health outcomes: a systematic review. Maternal & Child Nutrition, 12: 402–417. doi: 10.1111/mcn.12294.
References
- Abolyan L.V. (2006) The breastfeeding support and promotion in Baby‐Friendly Maternity Hospitals and not‐as‐yet Baby‐Friendly Hospitals in Russia. Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine 1 (2), 71–8. [DOI] [PubMed] [Google Scholar]
- Bartington S., Griffiths L. J., Tate A. R., Dezateux C. & Millennium Cohort Study Health, G. (2006) Are breastfeeding rates higher among mothers delivering in Baby Friendly accredited maternity units in the UK? International Journal of Epidemiology, 35(5), 1178–86. [DOI] [PubMed] [Google Scholar]
- Beake S., Pellowe C., Dykes F., Schmied V. & Bick D. (2012) A systematic review of structured compared with non‐structured breastfeeding programmes to support the initiation and duration of exclusive and any breastfeeding in acute and primary health care settings. Maternal & Child Nutrition 2, 141–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosnjak A.P., Batinica M., Hegedus‐Jungvirth M., Grguric J. & Bozikov J. (2004) The effect of baby friendly hospital initiative and postnatal support on breastfeeding rates – Croatian experience. Collegium Antropologicum 28 (1), 235–43. [PubMed] [Google Scholar]
- Bowatte G., Tham R., Allen K.J., Tan D.J., Lau M., Dai X. et al. (2015) Breastfeeding and childhood acute otitis media: a systematic review and meta‐analysis. Acta Paediatrica. Supplementum 104 (467), 85–95. [DOI] [PubMed] [Google Scholar]
- Braun M.L., Giugliani E.R., Soares M.E., Giugliani C., de Oliveira A.P. & Danelon C.M. (2003) Evaluation of the impact of the baby‐friendly hospital initiative on rates of breastfeeding. American Journal of Public Health 93 (8), 1277–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broadfoot M., Britten J., Tappin D.M. & MacKenzie J.M. (2005) The Baby Friendly Hospital Initiative and breast feeding rates in Scotland. Archives of Disease in Childhood. Fetal and Neonatal Edition 90 (2), F114–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldeira A.P. & Goncalves E. (2007) Assessment of the impact of implementing the Baby‐Friendly Hospital Initiative. Jornal de Pediatria 83 (2), 127–32. [DOI] [PubMed] [Google Scholar]
- Cattaneo A. & Buzzetti R. (2001) Effect on rates of breast feeding of training for the baby friendly hospital initiative. BMJ 323 (7325), 1358–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chien L.Y., Tai C.J., Chu K.H., Ko Y.L. & Chiu Y.C. (2007) The number of Baby Friendly hospital practices experienced by mothers is positively associated with breastfeeding: a questionnaire survey. International Journal of Nursing Studies 44 (7), 1138–46. [DOI] [PubMed] [Google Scholar]
- Chowdhury R., Sinha B., Sankar M.J., Taneja S., Bhandari N., Rollins N. et al. (2015) Breastfeeding and maternal health outcomes: a systematic review and meta‐analysis. Acta Paediatrica. Supplementum 104 (467), 96–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coutinho S.B., de Lira P.I., de Carvalho Lima M. & Ashworth A. (2005a) Comparison of the effect of two systems for the promotion of exclusive breastfeeding. Lancet 366 (9491), 1094–100. [DOI] [PubMed] [Google Scholar]
- Coutinho S.B., Lima Mde C., Ashworth A. & Lira P.I. (2005b) The impact of training based on the Baby‐Friendly Hospital Initiative on breastfeeding practices in the Northeast of Brazil. Jornal de Pediatria 81 (6), 471–7. [DOI] [PubMed] [Google Scholar]
- Dabritz H.A., Hinton B.G. & Babb J. (2009) Evaluation of lactation support in the workplace or school environment on 6‐month breastfeeding outcomes in Yolo County, California. Journal of Human Lactation 25 (2), 182–93. [DOI] [PubMed] [Google Scholar]
- Dasgupta A., Bhattacharya S., Das M., Chowdhury K.M. & Saha S. (1997) Breast feeding practices in a teaching hospital of Calcutta before and after the adoption of BFHI (Baby Friendly Hospital Initiative). Journal of the Indian Medical Association 95 (6), 169–71. [PubMed] [Google Scholar]
- de Oliveira M.I., Camacho L.A. & Tedstone A.E. (2003) A method for the evaluation of primary health care units' practice in the promotion, protection, and support of breastfeeding: results from the state of Rio de Janeiro, Brazil. Journal of Human Lactation 19 (4), 365–73. [DOI] [PubMed] [Google Scholar]
- Declercq E., Labbok M.H., Sakala C. & O'Hara M. (2009) Hospital practices and women's likelihood of fulfilling their intention to exclusively breastfeed. American Journal of Public Health 99 (5), 929–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiGirolamo A.M., Grummer‐Strawn L.M. & Fein S. (2001) Maternity care practices: implications for breastfeeding. Birth‐Issues in Perinatal Care 28 (2), 94–100. [DOI] [PubMed] [Google Scholar]
- DiGirolamo A.M., Grummer‐Strawn L.M. & Fein S.B. (2008) Effect of maternity‐care practices on breastfeeding. Pediatrics 122 (Suppl 2), S43–9. [DOI] [PubMed] [Google Scholar]
- Dulon M., Kersting M. & Bender R. (2003) Breastfeeding promotion in non‐UNICEF‐certified hospitals and long‐term breastfeeding success in Germany. Acta Paediatrica 92 (6), 653–8. [DOI] [PubMed] [Google Scholar]
- Duyan Camurdan A., Ozkan S., Yuksel D., Pasli F., Sahin F. & Beyazova U. (2007) The effect of the baby‐friendly hospital initiative on long‐term breast feeding. International Journal of Clinical Practice 61 (8), 1251–5. [DOI] [PubMed] [Google Scholar]
- Dyson L., McCormick F. & Renfrew M.J. (2005) Interventions for promoting the initiation of breastfeeding. Cochrane Database of Systematic Reviews 2 (2), 1–10 [DOI] [PubMed] [Google Scholar]
- Garcia‐de‐Leon‐Gonzalez R., Oliver‐Roig A., Hernandez‐Martinez M., Mercader‐Rodriguez B., Munoz‐Soler V., Maestre‐Martinez M.I. et al. (2011) Becoming baby‐friendly in Spain: a quality‐improvement process. Acta Paediatrica 100 (3), 445–50. [DOI] [PubMed] [Google Scholar]
- Gau M.L. (2004) Evaluation of a lactation intervention program to encourage breastfeeding: a longitudinal study. International Journal of Nursing Studies 41 (4), 425–35. [DOI] [PubMed] [Google Scholar]
- Giovannini M., Riva E., Banderali G., Salvioni M., Radaelli G. & Agostoni C. (2005) Exclusive versus predominant breastfeeding in Italian maternity wards and feeding practices through the first year of life. Journal of Human Lactation 21 (3), 259–65. [DOI] [PubMed] [Google Scholar]
- Guyatt G.H., Oxman A.D., Vist G., Kunz R., Brozek J., Alonso‐Coello P. et al. (2011) GRADE guidelines: 4. Rating the quality of evidence—study limitations (risk of bias). Journal of Clinical Epidemiology 64 (4), 407–415. [DOI] [PubMed] [Google Scholar]
- Helsing E., Chalmers B.E., Dinekina T.J. & Kondakova N.I. (2002) Breastfeeding, baby friendliness and birth in transition in North Western Russia: a study of women's perceptions of the care they receive when giving birth in six maternity homes in the cities of Archangelsk and Murmansk, 1999. Acta Paediatrica 91 (5), 578–83. [DOI] [PubMed] [Google Scholar]
- Horta B.L., Loret de Mola C. & Victora C.G. (2015a) Long‐term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta‐analysis. Acta Paediatrica. Supplementum 104 (467), 30–7. [DOI] [PubMed] [Google Scholar]
- Horta B.L., Loret de Mola C. & Victora C.G. (2015b) Breastfeeding and intelligence: a systematic review and meta‐analysis. Acta Paediatrica. Supplementum 104 (467), 14–9. [DOI] [PubMed] [Google Scholar]
- Ingram J., Johnson D. & Condon L. (2011) The effects of Baby Friendly Initiative training on breastfeeding rates and the breastfeeding attitudes, knowledge and self‐efficacy of community health‐care staff. Primary Health Care Research & Development 12 (3), 266–75. [DOI] [PubMed] [Google Scholar]
- Jaafar S. H., Jahanfar S., Angolkar M. & Ho J. J. (2011) Pacifier Use Versus no Pacifier use in Breastfeeding Term Infants for Increasing Duration of Breastfeeding. Cochrane Database Syst Rev 2011 Mar 16 (3), CD007202. [DOI] [PubMed] [Google Scholar]
- Jaafar S.H., Lee K.S. & Ho J.J. (2012) Separate care for new mother and infant versus rooming‐in for increasing the duration of breastfeeding. Cochrane Database of Systematic Reviews Sep 12 9, CD006641. [DOI] [PubMed] [Google Scholar]
- Kramer M.S., Aboud F., Mironova E., Vanilovich I., Platt R.W., Matush L. et al.Promotion of Breastfeeding Intervention Trial Study, G (2008a) Breastfeeding and child cognitive development: new evidence from a large randomized trial. Archives of General Psychiatry 65 (5), 578–84. [DOI] [PubMed] [Google Scholar]
- Kramer M.S., Chalmers B., Hodnett E.D., Sevkovskaya Z., Dzikovich I., Shapiro S. et al. (2001) Promotion of Breastfeeding Intervention Trial (PROBIT): a randomized trial in the Republic of Belarus. JAMA 285 (4), 413–20. [DOI] [PubMed] [Google Scholar]
- Kramer M.S., Fombonne E., Igumnov S., Vanilovich I., Matush L., Mironova E. et al.Promotion of Breastfeeding Intervention Trial Study, G (2008b) Effects of prolonged and exclusive breastfeeding on child behavior and maternal adjustment: evidence from a large, randomized trial. Pediatrics 121 (3), e435–40. [DOI] [PubMed] [Google Scholar]
- Kramer M. S., Guo T., Platt R. W., Shapiro S., Collet J. P., Chalmers B., Hodnett E., Sevkovskaya Z., Dzikovich I., Vanilovich I. & Group P. S. (2002) Breastfeeding and infant growth: biology or bias? Pediatrics 110(2 Pt 1), 343–7. [DOI] [PubMed] [Google Scholar]
- Kramer M.S., Matush L., Vanilovich I., Platt R., Bogdanovich N., Sevkovskaya Z. et al.Promotion of Breastfeeding Intervention Trial Study, G (2007a) Effect of prolonged and exclusive breast feeding on risk of allergy and asthma: cluster randomised trial. BMJ 335 (7624), 815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer M.S., Matush L., Vanilovich I., Platt R.W., Bogdanovich N., Sevkovskaya Z. et al. (2007b) Effects of prolonged and exclusive breastfeeding on child height, weight, adiposity, and blood pressure at age 6.5 y: evidence from a large randomized trial. American Journal of Clinical Nutrition 86 (6), 1717–21. [DOI] [PubMed] [Google Scholar]
- Kramer M.S., Vanilovich I., Matush L., Bogdanovich N., Zhang X., Shishko G. et al. (2007c) The effect of prolonged and exclusive breast‐feeding on dental caries in early school‐age children. New evidence from a large randomized trial. Caries Research 41 (6), 484–8. [DOI] [PubMed] [Google Scholar]
- Kuan L.W., Britto M., Decolongon J., Schoettker P.J., Atherton H.D. & Kotagal U.R. (1999) Health system factors contributing to breastfeeding success. Pediatrics 104 (3), e28. [DOI] [PubMed] [Google Scholar]
- Kyenkya‐Isabirye M. (1992) UNICEF launches the Baby‐Friendly Hospital Initiative. MCN: American Journal of Maternal Child Nursing 17 (4), 177–9. [DOI] [PubMed] [Google Scholar]
- Labbok M.H. (2012) Global baby‐friendly hospital initiative monitoring data: update and discussion. Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine 7, 210–22. [DOI] [PubMed] [Google Scholar]
- Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P. et al. (2009) The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate health care interventions: explanation and elaboration. Annals of Internal Medicine 151 (4), W‐65–W‐94. [DOI] [PubMed] [Google Scholar]
- Lutter C.K., Perez‐Escamilla R., Segall A., Sanghvi T., Teruya K. & Wickham C. (1997) The effectiveness of a hospital‐based program to promote exclusive breast‐feeding among low‐income women in Brazil. American Journal of Public Health 87 (4), 659–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens P.J. (2000) Does breastfeeding education affect nursing staff beliefs, exclusive breastfeeding rates, and Baby‐Friendly Hospital Initiative compliance? The experience of a small, rural Canadian hospital. Journal of Human Lactation 16 (4), 309–18. [DOI] [PubMed] [Google Scholar]
- Merewood A., Mehta S.D., Chamberlain L.B., Philipp B.L. & Bauchner H. (2005) Breastfeeding rates in US Baby‐Friendly hospitals: results of a national survey. Pediatrics 116 (3), 628–634. [DOI] [PubMed] [Google Scholar]
- Merten S., Dratva J. & Ackermann‐Liebrich U. (2005) Do baby‐friendly hospitals influence breastfeeding duration on a national level? Pediatrics 116 (5), e702–8. [DOI] [PubMed] [Google Scholar]
- Moore E.R., Anderson G.C., Bergman N. & Dowswell T. (2012) Early skin‐to‐skin contact for mothers and their healthy newborn infants. Cochrane Database of Systematic Reviews May 16 5, CD003519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray E.K., Ricketts S. & Dellaport J. (2007) Hospital practices that increase breastfeeding duration: results from a population‐based study. Birth 34 (3), 202–11. [DOI] [PubMed] [Google Scholar]
- Mydlilova A., Sipek A. & Vignerova J. (2009) Breastfeeding rates in baby‐friendly and non‐baby‐friendly hospitals in the Czech Republic from 2000 to 2006. Journal of Human Lactation 25 (1), 73–8. [DOI] [PubMed] [Google Scholar]
- Narchi N.Z., Fernandes R.A., Dias Lde A. & Novais D.H. (2009) Variables that influence the maintenance of exclusive breastfeeding. Revista Da Escola de Enfermagem Da Usp 43 (1), 87–94. [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine (2015) Review of WIC Food Packages: Proposed Framework for Revisions: Interim Report. The National Academies Press: Washington, DC: Chapter 7.. [PubMed] [Google Scholar]
- Naylor A.J. (2001) Baby‐Friendly Hospital Initiative. Protecting, promoting, and supporting breastfeeding in the twenty‐first century. Pediatric Clinics of North America 48 (2), 475–83. [DOI] [PubMed] [Google Scholar]
- Nickel N.C., Labbok M.H., Hudgens M.G. & Daniels J.L. (2012) The extent that noncompliance with the ten steps to successful breastfeeding influences breastfeeding duration. Journal of Human Lactation 29 (1), 59–70. [DOI] [PubMed] [Google Scholar]
- Ojofeitimi E.O., Esimai O.A., Owolabi O.O., Oluwabusi O.O.F. & Olanuga T.O. (2000) Breast feeding practices in urban and rural health centres: impact of baby friendly hospital initiative in Ile‐Ife, Nigeria. Nutrition & Health 14 (2), 119–25. [DOI] [PubMed] [Google Scholar]
- Peres K.G., Cascaes A.M., Nascimento G.G. & Victora C.G. (2015) Effect of breastfeeding on malocclusions: a systematic review and meta‐analysis. Acta Paediatrica. Supplementum 104 (467), 54–61. [DOI] [PubMed] [Google Scholar]
- Perez‐Escamilla R. (2012) Breastfeeding social marketing: lessons learned from USDA's “Loving Support” campaign. Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine 7 (5), 358–63. [DOI] [PubMed] [Google Scholar]
- Perez‐Escamilla R. & Chapman D.J. (2012) Breastfeeding protection, promotion, and support in the United States: a time to nudge, a time to measure. Journal of Human Lactation 28 (2), 118–21. [DOI] [PubMed] [Google Scholar]
- Perez‐Escamilla R., Pollitt E., Lönnerdal B. & Dewey K.G. (1994) Infant feeding policies in maternity wards and their effect on breast‐feeding success: an analytical overview. American Journal of Public Health 84 (1), 89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrine C.G., Scanlon K.S., Li R., Odom E. & Grummer‐Strawn L.M. (2012) Baby‐Friendly hospital practices and meeting exclusive breastfeeding intention. Pediatrics 130 (1), 54–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philipp B.L., Malone K.L., Cimo S. & Merewood A. (2003) Sustained breastfeeding rates at a US baby‐friendly hospital. Pediatrics 112 (3 Pt 1), e234–6. [DOI] [PubMed] [Google Scholar]
- Philipp B.L., Merewood A., Miller L.W., Chawla N., Murphy‐Smith M.M., Gomes J.S. et al. (2001) Baby‐friendly hospital initiative improves breastfeeding initiation rates in a US hospital setting. Pediatrics 108 (3), 677–81. [DOI] [PubMed] [Google Scholar]
- Pincombe J., Baghurst P., Antoniou G., Peat B., Henderson A. & Reddin E. (2008) Baby Friendly Hospital Initiative practices and breast feeding duration in a cohort of first‐time mothers in Adelaide. Australia. Midwifery. 24 (1), 55–61. [DOI] [PubMed] [Google Scholar]
- Rivera‐Lugo M., Parrilla‐Rodriguez A.M., Davila‐Torres R.R., Albizu‐Garcia C. & Rios‐Motta R. (2007) Full breastfeeding during the postpartum hospitalization and mothers' report regarding baby friendly practices. Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine 2 (1), 19–26. [DOI] [PubMed] [Google Scholar]
- Rosenberg K.D., Stull J.D., Adler M.R., Kasehagen L.J. & Crivelli‐Kovach A. (2008) Impact of hospital policies on breastfeeding outcomes. Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine 3 (2), 110–6. [DOI] [PubMed] [Google Scholar]
- Sampaio P.F., Moraes C.L., Reichenheim M.E., Oliveira A.S. & Lobato G. (2011) Birth in Baby‐Friendly Hospitals in Rio de Janeiro, Brazil: a protective factor for breastfeeding? Cadernos de Saúde Pública 27 (7), 1349–61. [DOI] [PubMed] [Google Scholar]
- Sankar M.J., Sinha B., Chowdhury R., Bhandari N., Taneja S., Martines J. et al. (2015) Optimal breastfeeding practices and infant and child mortality: a systematic review and meta‐analysis. Acta Paediatrica. Supplementum 104 (467), 3–13. [DOI] [PubMed] [Google Scholar]
- Schwarzer R. (2008) Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Applied Psychology: An International Review 57 (1), 1–29. [Google Scholar]
- Shilpa L., Prakash A. & Rao S. (2009) BFHI in a tertiary care hospital: does being Baby friendly affect lactation success? Indian Journal of Pediatrics 76 (6), 655–7. [DOI] [PubMed] [Google Scholar]
- Silva M.B.d., Albernaz E.P., Mascarenhas M.L.W. & Silveira R.B.d. (2008) Influence of breastfeeding support on the exclusive breastfeeding of babies in the first month of life and born in the city of Pelotas, State of Rio Grande do Sul, Brazil. Revista Brasileira de Saude Materno Infantil 8 (3), 275–284. [Google Scholar]
- Taddei J.A., Westphal M.F., Venancio S., Bogus C. & Souza S. (2000) Breastfeeding training for health professionals and resultant changes in breastfeeding duration. Sao Paulo Medical Journal = Revista Paulista de Medicina 118 (6), 185–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarrant M., Wu K.M., Fong D.Y., Lee I.L., Wong E.M., Sham A. et al. (2011) Impact of baby‐friendly hospital practices on breastfeeding in Hong Kong. Birth 38 (3), 238–45. [DOI] [PubMed] [Google Scholar]
- Tham R., Bowatte G., Dharmage S.C., Tan D.J., Lau M., Dai X. et al. (2015) Breastfeeding and the risk of dental caries: a systematic review and meta‐analysis. Acta Paediatrica. Supplementum 104 (467), 62–84. [DOI] [PubMed] [Google Scholar]
- UNICEF/WHO . (2009) Baby‐Friendly Hospital Initiative: revised, Updated and Expanded for Integrated Care. Available at: http://whqlibdoc.who.int/publications/2009/9789241594967_eng.pdf (Accessed 23 August 2013). [PubMed]
- Baby Friendly USA . (2010) Guidelines and evaluation criteria for facilities seeking baby‐friendly designation Available at: http://www.babyfriendlyusa.org/get-started/the-guidelines-evaluation-criteria (Accessed 23 August 2013).
- Baby Friendly USA . (2012) Find Facilities, Available at: http://www.babyfriendlyusa.org/find-facilities. (Accessed 23 August 2013). [Google Scholar]
- Valdes V., Perez A., Labbok M., Pugin E., Zambrano I. & Catalan S. (1993) The impact of a hospital and clinic‐based breastfeeding promotion programme in a middle class urban environment. Journal of Tropical Pediatrics 39 (3), 142–51. [DOI] [PubMed] [Google Scholar]
- Venancio S.I., Escuder M.M., Kitoko P., Rea M.F. & Monteiro C.A. (2002) Frequency and determinants of breastfeeding in the State of Sao Paulo, Brazil. Revista de Saúde Pública 36 (3), 313–8. [DOI] [PubMed] [Google Scholar]
- Venancio S.I., Saldiva S.R., Escuder M.M. & Giugliani E.R. (2012) The Baby‐Friendly Hospital Initiative shows positive effects on breastfeeding indicators in Brazil. Journal of Epidemiology & Community Health 66 (10), 914–8. [DOI] [PubMed] [Google Scholar]
- Vieira G.O., Silva L.R., Mendes C.M. & Vieira Tde O. (2006) Lactational mastitis and Baby‐Friendly Hospital Initiative, Feira de Santana, Bahia, Brazil. Cadernos de Saúde Pública 22 (6), 1193–200. [DOI] [PubMed] [Google Scholar]
- Weng D.R., Hsu C.S., Gau M.L., Chen C.H. & Li C.Y. (2003) Analysis of the outcomes at baby‐friendly hospitals: appraisal in Taiwan. Kaohsiung Journal of Medical Sciences 19 (1), 19–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . (1989) The Ten Steps to Successful Breastfeeding Protecting, Promoting and Supporting Breast‐feeding: The Special Role of Maternity Services. Geneva, Switzerland: World Health Organization; Available at: http://whqlibdoc.who.int/publications/9241561300.pdf (Accessed 23 August 2013). [Google Scholar]
- WHO . (1998) Evidence for the ten steps to successful breastfeeding. Availble at: http://whqlibdoc.who.int/publications/2004/9241591544_eng.pdf (Accessed 23 August 2013).
- WHO . (2002) Infant and young child nutrition: global strategy on infant and young child feeding. Geneva, Switzerland: Available at: http://apps.who.int/gb/archive/pdf_files/WHA55/ea5515.pdf?ua=1 (Accessed 1 December, 2015) [Google Scholar]
- WHO/UNICEF . (2003) Global strategy for infant and young child feeding. Available at: http://www.who.int/maternal_child_adolescent/documents/9241562218/en/index.html (Accessed 23 August 2013).
- Wright A., Rice S. & Wells S. (1996) Changing hospital practices to increase the duration of breastfeeding. Pediatrics 97 (5), 669–75. [PubMed] [Google Scholar]
- Zakarija‐Grkovic I., Segvic O., Bozinovic T., Cuze A., Lozancic T., Vuckovic A. et al. (2012) Hospital practices and breastfeeding rates before and after the UNICEF/WHO 20‐h course for maternity staff. Journal of Human Lactation 28 (3), 389–99. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information
Supporting Information
Supporting Information


