Abstract
Good nutrition in the early years of life is vitally important for a child's development, growth and health. Children's diets in the United Kingdom are known to be poor, particularly among socially disadvantaged groups, and there is a need for timely and appropriate interventions that support parents to improve the diets of young children. The Medical Research Council has highlighted the importance of conducting developmental and exploratory research prior to undertaking full‐scale trials to evaluate complex interventions, but have provided very limited detailed guidance on the conduct of these initial phases of research. This paper describes the initial developmental stage and the conduct of an exploratory randomised controlled trial undertaken to determine the feasibility and acceptability of a family‐centred early years' nutrition intervention. Choosing Healthy Eating when Really Young (CHERRY) is a programme for families with children aged 18 months to 5 years, delivered in children's centres in one urban (Islington) and one rural (Cornwall) location in the United Kingdom. In the development stage, a mixed‐methods approach was used to investigate the nature of the problem and options for support. A detailed review of the evidence informed the theoretical basis of the study and the creation of a logic model. In the feasibility and pilot testing stage of the exploratory trial, 16 children's centres, with a sample of 394 families were recruited onto the study. We hope that the methodology, which we present in this paper, will inform and assist other researchers in conducting community‐based, exploratory nutrition research in early years settings.
Keywords: nutrition intervention, early years, community‐based research, exploratory randomised controlled trial
Background
A healthy diet in childhood is essential for both short‐term and future health as dietary habits established in early life persist into adulthood (Skinner et al. 2002; Nicklaus et al. 2005). A substantial body of evidence indicates that a healthy diet has multiple health benefits in childhood and beyond including lower blood pressure (Moore et al. 2005), greater bone mass (Tylavsky et al. 2004) and protection against certain cancers (Maynard et al. 2003). In addition, poor dietary habits are a major determinant of childhood overweight and obesity, which currently affects 22.6% of 4–5‐year‐olds and 33.4% of 10–11‐year‐olds in the United Kingdom and by 2050, this proportion is predicted to rise further (Foresight 2007; The NHS Information Centre 2011). Excess consumption of non‐milk extrinsic sugars (NMES) is associated with dental caries, a common but preventable childhood disease (World Health Organization 2003). Nutrition across the life course is also an important contributing factor to inequalities in health (James et al. 1997).
Currently, only one in five 5–15‐year‐olds in the United Kingdom are consuming the recommended five portions of fruits and vegetables daily, with average consumption of approximately three servings per day (The NHS Information Centre 2010). A recent cohort study in London with a sample of 384 families found that 15.9% of 18‐month‐olds ate no fruit and 8.4% ate no vegetables over a 3‐day period (Holmes et al. 2008). The most recent UK National Diet and Nutrition Survey found that children aged 1.5–3 years were not meeting the recommended minimum amounts of fruit and vegetables, and exceeding the recommended amount of NMES (Bates et al. 2012). There is a strong relationship between socio‐economic deprivation and diet quality: socially deprived groups consume significantly more NMES and lower amounts of fresh fruit and vegetables, and have a higher prevalence of obesity and dental caries (Watt & Sheiham 1999; Gregory et al. 2000; Nelson et al. 2007).
Young children's eating habits are influenced by a multitude of biological, psychological, behavioural, social, community and environmental factors. Changing eating behaviours is therefore a complex challenge which requires more than simply providing educational support (National Institute for Health and Clinical Excellence 2008; Lawrence & Barker 2009). Recent guidance from The National Institute for Health and Clinical Excellence (NICE) on improving nutrition in low‐income mothers and their children highlighted the paucity of high‐quality interventions and stressed the importance of taking a ‘whole settings approach’ to healthy eating (National Institute for Health and Clinical Excellence 2008). The Marmot Review has highlighted the importance of focusing on the early years sector as a key strategy to combat health inequalities (Marmot 2010). Reaching the families most in need of help can, however, be extremely challenging, but children's centres, which have been designed to offer a range of childcare, education, health and family support services and are situated in the most deprived areas across England, are an ideal setting in which to promote health.
Interventions, which aim to tackle such complex and persistent problems, require careful planning, development and evaluation. The Medical Research Council (MRC) framework for developing and evaluating complex interventions highlights the importance of undertaking detailed preparatory investigations of the problem to be addressed and careful piloting and development of the intervention, prior to undertaking a full‐scale intervention (Medical Research Council 2008). However, very few papers have provided a detailed account of the conduct and methodology of exploratory trials (Michie et al. 2011). The aim of this paper is to describe the methodological development of a nutrition intervention delivered in children's centres and the assessment of its feasibility and acceptability via an exploratory randomised controlled trial. As there is a paucity of papers describing the development, testing and nature of early years' community‐based nutrition interventions, it is hoped that this paper will assist researchers and early years practitioners in developing future interventions in this important area of public health.
Key messages
The early years sector is a key area in which to combat health inequalities such as poor diet, a problem that is known to persist into later life.
Interventions, which aim to tackle health inequalities, require careful planning, development and evaluation, yet little guidance is available on practically how to do this
This paper has described in detail the methodology employed in the initial developmental and exploratory stages of evaluating an early years' nutrition intervention. The insights gained from this research will be used to inform the design and delivery of future large‐scale randomised controlled trials to address this important public health issue.
Methodology
Study population
Cornwall (rural study location) and Islington (urban study location) were chosen to represent a diverse range of low‐income communities across England. In 2007, the Borough of Islington in inner London and was ranked the sixth most deprived district out of a total of 354 boroughs across England. Cornwall has a history of disadvantage arising from its geographical location (an isolated county in South West England) and the decline of traditional industries (mining, fishing, agriculture, textiles). Its most deprived district, Penwith, was ranked the 21st most deprived district in England in 2007 (Department for Communities and Local Government 2007).
Study design
As outlined by the MRC guidance, complex interventions involve four key stages: theoretical development and modelling, feasibility/piloting, evaluation and finally, implementation (Medical Research Council 2008). This paper describes details of the first two stages of the MRC framework, namely, the development and feasibility/piloting of the early years' nutrition intervention.
The initial development stage is crucial in identifying the evidence base and appropriate theory for the intervention. At this stage, gaining a detailed understanding of the nature of the problem to be addressed is also fundamentally important. The next stage involves feasibility and pilot testing of the intervention. Undertaking an exploratory randomised controlled trial is considered best practice to assess the acceptability and feasibility of the intervention, test recruitment and retention rates, determine intra‐cluster correlation coefficients and effect estimates. This is important to inform sample size calculations for future definitive trials designed to assess the effectiveness and cost‐effectiveness of a full‐scale intervention. The final phase focuses on the subsequent implementation of the intervention in terms of assessing the dissemination and longer term follow‐up.
The MRC guidance on conducting exploratory trials is rather vague and general in nature and provides very limited detailed methodological guidance (Michie et al. 2005; Medical Research Council 2008). Within public health nutrition research, and specifically community‐based interventions targeting pre‐school children, very few papers provide details of the methodological development of the intervention. A comprehensive step‐by‐step account of the methodology employed in this study is therefore presented (Fig. 1).
Figure 1.
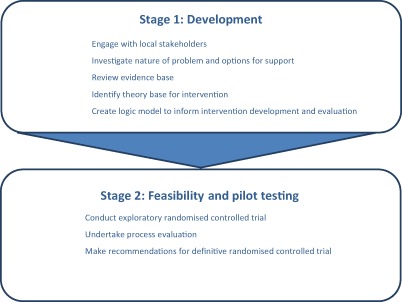
Flow chart of methodology employed in CHERRY.
Stage 1: development
Ethics approval
Prior to commencing the study, full ethics approval was received from Camden and Islington Community Research Ethics Committee (09/H0722/56).
Engagement with local stakeholders
A key practical measure in the development of any community‐based intervention is engagement with local stakeholders to understand the local context and to consult on the nature of the proposed intervention. Members of the study team in both study sites (Islington and Cornwall) visited a wide range of key local stakeholders based in local authorities, community health services and voluntary sector organisations. In particular, a major effort was made to engage with children's centre staff in both areas to understand more fully what was currently happening in terms of nutritional support provided and the potential for developing a new intervention. Local steering groups comprising representatives of the different sectors were formed in both areas to provide an ongoing consultation forum during the development and implementation stages of the study.
Understanding the nature of the problem and options for support
A mixed‐methods approach using both qualitative and quantitative techniques was used to explore with parents/guardians and children's centre staff factors influencing young children's diets, barriers to change and options for developing a supportive intervention. Initially, separate focus groups with parents/guardians and staff were conducted in both areas (Hayter et al. 2012). A questionnaire survey was conducted with heads of all children's centres in both locations as well as over 260 parents/guardians using opportunistically selected children's centres to inform the development of the intervention (Ohly et al. 2012). A short self‐administered questionnaire was also used to gather information from children's centre managers on food‐related activities taking place, options for staff training and nature of food policies operating in each centre.
The detailed results from this preliminary work have been published elsewhere (Hayter et al. 2012; Ohly et al. 2012) but in summary the main insights gained to inform the development of the intervention were:
-
Acknowledgement of the wide range of factors influencing parental feeding practices including:
Affordability of food,
Time constraints in hectic family life,
Availability of foods and influence of food marketing and advertising,
Family influences and challenges to parental wishes and
Familiarity of food to children and the difficulties of dealing with fussy eating.
-
Key implications for development of intervention were:
Recognition that complex and varied influences on food practices require multifaceted support. Information leaflets alone would not be sufficient to address problems identified.
Need to understand importance of family and social influences within family structures.
Strong support expressed from both parents and staff for the development of a new tailored intervention in children's centres.
Necessity of practical support that engages with parents and equips them with the necessary knowledge, skills and self‐confidence and moves beyond narrow provision of information alone.
Need to include support on dealing with fussy eating and managing on a tight budget.
Very few differences were evident on support required in urban and rural settings – core programme therefore applicable in both areas.
Identifying the evidence base
A detailed and comprehensive review of the relevant UK and international nutrition, health promotion and behaviour change literature was undertaken to assess the evidence base for the intervention. Particular focus was placed upon interventions targeting pre‐school children and those delivered in early years settings. Both systematic reviews (n = 6) and empirical studies (n = 20) were included in the review. In addition, a review was also undertaken of studies, which had assessed the factors influencing dietary patterns of families with pre‐school children and barriers preventing the adoption of recommended feeding practices.
The review highlighted the paucity of well‐designed community‐based early years' nutrition interventions but usefully highlighted the importance of the following issues:
Methodological limitations of literature included poor designs, small and mostly unrepresentative study samples and poor evaluation with limited follow‐up data. Need for more robust dietary assessment pre‐ and post‐intervention.
Limited inclusion of lower income populations.
Most successful studies achieved increases in fruit consumption and used a variety of approaches including parental support.
Encouraging results also from repeat exposure studies tackling fussy eating habits.
Few UK studies published.
Very limited focus on intervention to reduce sugary drinks or snack consumption.
Selecting a theory base for the intervention
It is now increasingly recommended, not only by the MRC 2008 guidance, but also by other reports that theory should be used in the design and evaluation of public health interventions (Medical Research Council 2000, 2008; National Institute for Health and Clinical Excellence 2007). It is argued that an intervention based on relevant theory rather than just a pragmatic approach is more likely to be effective (Medical Research Council 2008). Theory should also be used to provide a rationale for how an intervention will achieve the desired changes. In the context of this study, two levels of change were anticipated (at the individual and also institutional level, i.e. the children's centres) requiring a wider theoretical perspective.
However, despite this growing emphasis on the use of theory in developing interventions, there is little practical guidance on just how to select an appropriate theory (Michie et al. 2005). For instance, the MRC recommends using an appropriate theory with little explanation of what this means (Medical Research Council 2008); NICE similarly recommends choosing a ‘relevant behavioural model’ (with a further complication here in that the terms theory and model are sometimes used inter‐changeably; National Institute for Health and Clinical Excellence 2007). The philosopher John Dewey in a classic seminal paper noted back in 1916, the means by which particular theories are selected and used, often remains in the ‘twilight zone of enquiry’ (Dewey 1916). We therefore wished to formulate an explicit and transparent procedure by which we carried out the identification of appropriate theories to inform the development of the early years' nutrition intervention.
Information gathered from the earlier stages of the study provided useful background to inform the selection of the theory base. In particular, critically reviewing recent systematic reviews of the behaviour change literature helped to identify common findings on the theoretical basis of interventions. From this, we then put together a composite approach drawing on Carpiano and Daley's (Carpiano & Daley 2006) recommendations in using and building theory in the context of public health, supplemented by guidance from NICE (National Institute for Health and Clinical Excellence 2007) and the GSR review (Darnton 2008), both of which set out a structured approach to developing interventions for behaviour change. Carpiano and Daley outline a three‐stage approach to using theory that we then followed with modification:
-
Define a conceptual framework to identify the variables and the broad relations between them that account for the phenomenon of interest.
This is equivalent to the NICE guidance and the ANGELO (Analysis Grid for Elements Linked to Obesity) approach that involves mapping the problem or issue to be assessed and where the best options for intervention might lie (Swinburn et al. 1999; National Institute for Health and Clinical Excellence 2007).
-
Select and define relevant theories to provide a more dense and coherent set of relationships between the key variables of interest.
To do this and to identify specific causal factors, the baseline qualitative and quantitative data were used to identify the key influencing factors and also those that could be addressed in the context of intervention.
-
Finally, develop a logic model that is more specific still and that predicates specific assumptions about a limited set of outcomes.
We set about designing a logic model in relation to the study outcomes (see Fig. 2).
Figure 2.
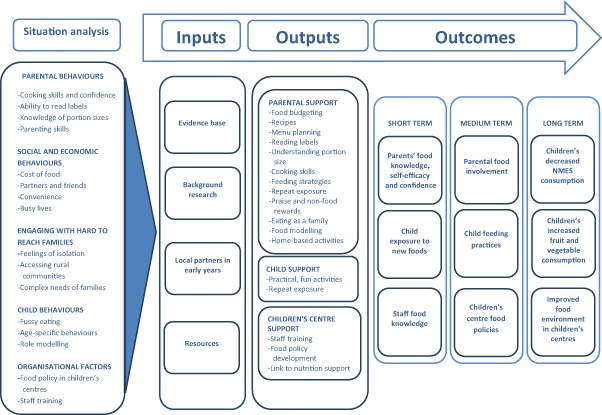
Logic model for the development of CHERRY.
Lastly, based upon the essential criteria of relevance and effectiveness (Taylor et al. 2006), we selected two theories: the social cognitive theory (Bandura 1986) to inform the individual behaviour change components of the intervention and the stage theory of organisational change for the institutional element (Kaluzny & Hernandez 1988). The social cognitive theory highlights the importance of self‐efficacy in behaviour change. The qualitative data collected in the focus groups stressed that parents were largely well informed on dietary recommendations but often lacked the skills and confidence to adopt practically these measures in their busy and hectic lives (Hayter et al. 2012). The stage theory of organisational change, based on Rogers' theory of innovation (Rogers 1983), describes how organisations pass through a series of steps in the process of implementing innovation and change. Again, both the qualitative and quantitative data collected from children's centre staff highlighted the importance of policy guidance, staff training and engagement with parents as key issues in promoting change in nutrition practices within the children's centres (Hayter et al. 2012; Ohly et al. 2012).
Development of a logic model to inform the intervention
The final step in the development phase was the creation of a logic model, based upon the data and knowledge gathered in the previous steps, which diagrammatically mapped out the inputs, outputs and expected outcomes for the planned intervention (McLaughlin & Jordan 1999). Figure 2 presents a summary of the key elements of the logic model.
Stage 2: feasibility and pilot testing
The methodology adopted in the exploratory randomised controlled trial used to assess the feasibility, acceptability and effect size of the early years' nutrition intervention (Choosing Healthy Eating when Really Young; CHERRY) will now be described.
Study setting: children's centres
Children's centres provided the setting for recruitment of families and delivery of the intervention. Children's centres are government‐funded early years organisations where children under five and their families can receive integrated services and support, such as access to health and parenting services, advice and information on health, training and return to work, and in some areas high‐quality early years child care (Department for Education 2012).
Selection of children's centres
Children's centres in both study locations were randomly selected to participate in the study. Initially, 64 centres in total were approached with 38 agreeing to participate. More children's centres were selected in Cornwall to represent its larger geographical area and population size; in Islington, six children's centres were simply randomly selected from a list of those centres who expressed an interest in participating in the study (9 out of 16). In Cornwall, the random selection was stratified by geographical location and deprivation to ensure representativeness of the county. Ten children's centres were selected from those who expressed an interest in participating in the study (30 out of 33). The 16 selected children's centres were then randomly assigned to intervention or control group. Three intervention and three control centres in Islington, and five intervention and five control centres in Cornwall.
Sample size
For exploratory trials, it is inappropriate to undertake a detailed power calculation; one of the main purposes behind conducting a pilot study is to assess practicality and acceptability of the trial methods and to provide an effect size and intra cluster correlation coefficient to inform power calculations for a future definitive trial (Medical Research Council 2008). However, based upon pragmatic considerations, it was estimated that in each children's centre (n = 16), there would be approximately 40 possible participants. Assuming 60% of parents invited to participate accepted the offer, and that at the 6 months follow‐up there would be a 75% retention rate, this would give a final sample of 288). This target sample is very similar to a successful primary care nutrition intervention which had a sample size of 258 families at follow‐up (129 per arm; Ashfield‐Watt 2007). That trial was designed to have at least 80% power at the 5% significance level, in order to detect an increase of 0.7 portions of fruit and vegetables per day (standard deviation 2.0).
Recruitment of subjects
Parents were recruited into the study over five recruitment waves between September 2010 and November 2011. Parents were eligible for inclusion if they had at least one child aged between 18 months and 5 years at the time of recruitment. For parents with more than one child in this age range, the youngest child was chosen for assessment. Parents were excluded from participation if their child had a diagnosed medical condition, which affected their diet, for example food allergies or diabetes, and if they were not able to communicate effectively in English.
Parents were recruited using a variety of different approaches to maximise uptake. Researchers provided induction sessions at the children's centres, during which they explained the project fully and asked staff to identify suitable families. Local health visiting teams and other outreach staff were also asked to refer families to the study. Researchers regularly attended outreach sessions at children's centres and other local childcare settings (such as community groups, primary schools and private nurseries) to meet suitable families. The researcher gave a brief explanation of the study, assessed eligibility and invited parents to take part. Eligible parents registered their details and were then followed up with a telephone call from the research team to arrange their initial home visit.
In addition to face‐to‐face recruitment, adverts were also placed in local newspapers, and schools, libraries and doctors' surgeries were asked to display recruitment posters. Fliers were distributed by post to families who were registered with children's centres. Social networking sites were also used to increase awareness of the project.
Finally, communication technology was also used as a recruitment tool. Adverts for the project included a ‘short‐code’, a 5‐digit number to which parents could text ‘CHERRY’ to register their interest. They immediately received an automated acknowledgement message. All participants who registered their interest by this method were telephoned by the research team within 24 h in order to explain the intervention more fully and assess their eligibility to participate. All parents that took part were offered a £10 high street voucher and a cook book developed for families with young children on completing the follow‐up assessment after 6 months.
Development of the intervention
The CHERRY programme was developed by the research team between June 2009 and August 2010 based upon the data gathered in the initial stage of the study. It was a family‐centred nutrition intervention delivered in selected children's centres across Islington and Cornwall. The programme focused on healthy eating for under‐fives and their families and involved a mixture of learning, discussion and practical ‘cook and eat’ activities. The training of children's centre staff and support with developing food policies in centres was also a key component of the intervention.
Informed by the earlier stages of the study, and in particular the qualitative and quantitative data gathered from parents (Hayter et al. 2012; Ohly et al. 2012), the focus of CHERRY was on making simple changes to improve the food that young children and their families eat. Specifically, it aimed to increase fruit and vegetables and to decrease the amount of sugary drinks and snacks consumed by young children. It also aimed to help parents gain confidence around food, increase their food involvement and their own consumption of fruit and vegetables.
Delivery of the intervention
CHERRY was delivered by trained tutors to eight groups of families in Islington and 12 groups in Cornwall between October 2010 and November 2011, with an average of eight (and between 5–12) families attending each group. Tutors were selected according to their ability to successfully deliver the CHERRY programme; they were then trained to deliver the programme during a 1‐day intensive training course, which all tutors attended. The research team monitored the tutors for consistency and quality of delivery by attending sessions at random throughout the course of the project. At each session, a member of staff from the children's centre (and/or sometimes one of the research team) was present to provide support to the tutor as required. The delivery was standardised as much as practically possible between groups; however, there were some differences depending on the needs of each group, for example, the recipes prepared and the focus of discussions.
The intervention group participants attended four sessions (one each week) over 4 weeks. Each session lasted 2 h. The first hour of each session involved parents discussing and learning about a variety of aspects of healthy eating while the children attended a free crèche in the adjacent room (the crèche activities were not considered part of CHERRY and were not monitored). The second hour involved parents and children together for a more practical, ‘hands on’ cook and eat session involving basic food preparation and tasting. Each session began with a recap from the previous week and finished with parents being given a ‘CHERRY at home’ activity to complete before the following week's session; these were both designed to consolidate parents' learning. The intervention group also received SMS reminders via mobile phones between sessions; SMSs included the main messages of the CHERRY programme, as well as reminders to attend each session. Table 1 outlines the content of the course in more detail.
Table 1.
CHERRY programme outline
| Session | Theory | Cook and eat | ‘CHERRY at home’ | Learning outcomes |
|---|---|---|---|---|
|
Week 1 Family‐friendly food |
|
A tasting session including a wide variety of fresh, tinned and dried fruits and vegetables, to introduce the idea of children trying new foods | Goal setting: Parents choose a healthy eating goal for the child, themselves or the whole family to do over the week |
|
|
Week 2 Introducing new foods (‘fussy eating’) |
|
An introduction to preparing easy meals, which are quick to make and well‐balanced. | Introducing new foods with the Tiny Tastes™ chart |
|
|
Week 3 Healthy snacks and drinks for children |
|
How to make healthy versions of common snack foods, to be eaten as part of a ‘mini‐meal’. |
Have a go at introducing new healthy snacks and drinks at home Continue using the Tiny Tastes™ chart |
To encourage parents to provide healthier snacks and drinks (with a focus on fruit and vegetables and reducing sugar)
|
|
Week 4 Healthy eating and food shopping on a budget |
|
Preparation of recipes that are appropriate for a low budget: a whole meal (main course and dessert) | To continue to put into practice the CHERRY principles at home |
|
Other intervention components
A major limitation of many interventions is the failure to focus on improving the social environment, which has a profound influence in supporting and maintaining individual behaviour change (National Institute for Health and Clinical Excellence 2007). Therefore, the intervention comprised not only individually focused nutrition support, but also encompassed activities directed at developing the capacity of the children's centre to promote and maintain healthy nutritional practices. In the intervention centres, a staff training session was offered to all staff working in the centres. The training session covered various aspects of healthy eating and nutrition for early years and included an introduction and overview of the CHERRY programme. Each training session was tailored to the needs of the staff, as identified by heads of each intervention centre. Intervention centres were also given support and advice to revise and develop their centre's food policies in order to support healthy eating practices and procedures.
Control group
The children's centres randomised to the control group did not receive any of the components of the CHERRY programme. During the study period, the control centres agreed not to implement any new nutritional interventions but continued with existing support. On final completion of the study, the CHERRY resources were disseminated to control centres and other early years settings interested in nutrition.
Outcome measures
Primary outcomes
The primary outcome was the child's fruit and vegetable consumption at home (portions per day). This was defined as the total weight (grams) of fruit and vegetables consumed, the number of different types of fruit and vegetables consumed, and the actual types of fruit and vegetables consumed. The number of portions per day was calculated based on guidance that one child's portion weighs 40 g (Nelson et al. 1997).
Secondary outcomes
The secondary outcome was the child's soft drink consumption. This was defined as the total quantity (mL) of soft drinks consumed; the number of occasions soft drinks were consumed; the types of soft drinks consumed; the quantity (mL) of each type. Sugary drinks and artificially sweetened drinks were considered separately.
Additional outcomes
An additional outcome was the child's consumption of sugary foods. This was defined as the number of occasions sugary snacks were consumed (snacks defined as food eaten more than 30 min after a meal); the types of sugary snacks consumed; the number of sugary snacks in each category.
Additional outcomes related to the parent's diet were consistent with the child's outcomes, namely, the consumption of fruit and vegetables, soft drinks and sugary foods. These were defined as the total weight (grams) of fruit and vegetables consumed and the number of portions per day, calculated based on guidance that one adult's portion weighs 80 g (National Health Service 2011); the number of different types of fruit and vegetables consumed; the types and quantities (mL) of soft drinks consumed; the number of portions of sugary foods consumed (based on standard portions, e.g. one slice of cake, one standard size chocolate bar, two biscuits, etc.).
Other parental outcomes thought to influence the way parents feed their young children and therefore potential intermediate outcomes for the intervention included food knowledge, food confidence, nutrition self‐efficacy, food involvement and parental stress; parental perception of child food fussiness was also included.
Measurement methods
Baseline assessment for the intervention groups was completed 2–4 weeks (depending on school holidays) before the families started attending the CHERRY sessions. While the intervention group was attending CHERRY, baseline assessment for the control group was completed. This was done in five phases between October 2010 and November 2011. Follow‐up assessment was completed 6 months after the families finished attending the CHERRY sessions (intervention groups) or 6 months after baseline (control groups). This was also done in five phases between June 2011 and June 2012.
At each time point, the data collection involved one home visit and three telephone calls. When it was not possible to arrange a home visit, the researchers either arranged to meet the parent somewhere more convenient (for example, their local children's centre) or completed the data collection by phone after sending parents the relevant paperwork.
Data collection methods
24‐h recalls
The child's diet was assessed using the multiple‐pass 24‐h recall method. As the children concerned were under 5 years of age, the parents completed the interviews on their behalf. They were asked by the researcher exactly what their child ate and drank the previous day. The standard protocol from the Low Income Diet and Nutrition Survey (LIDNS) was followed, which specifies four 24‐h dietary recalls on random days (including at least one weekend day) within a 10‐day period (Nelson et al. 2007). The LIDNS team compared the effectiveness and acceptability of four dietary survey methods (multiple‐pass 24‐h recall, food checklist and semi‐weighed method and 4‐day weighed inventory) and concluded that four multiple‐pass 24‐h recalls were the best method for measuring diet in low‐income households (Holmes et al. 2008).
In the present study, a portion size booklet was compiled using photographs provided by the Caroline Walker Trust, illustrating recommended portion sizes for pre‐school children. Parents were also asked to describe portion sizes using household measures or actual measures where possible. On days when children had been cared for by someone else, parents were asked in advance to find out as much detail as possible about what the child consumed.
During the home visits (one at baseline and one at follow‐up), parents were asked to respond to the first 24‐h recall interview of four. After this, as the interview style was familiar to the parent, phone calls were arranged to complete the remaining three 24‐h dietary recalls.
Parental questionnaire
Parents were also asked to complete a short questionnaire during the home visits (one at baseline and one at follow‐up). The questionnaire was developed using validated items from existing measures wherever possible. The questionnaire was piloted to assess its acceptability and feasibility with parents in Cornwall (n = 14) and Islington (n = 6) and was modified accordingly. The questionnaire included sections covering core demographic details, parents' diet over the previous 24 h, food knowledge (Ashfield‐Watt 2007), food confidence (Watt et al. 2006; Wrieden et al. 2007; Barton et al. 2011), nutrition self‐efficacy (Schwarzer & Renner 2009), food involvement (Bell & Marshall 2003; Barker 2008), parenting stress (Abidin 1995) and finally a measure of the child's food fussiness (Wardle et al. 2001).
Process evaluation
As highlighted by the MRC guidance (Medical Research Council 2008), an essential component of an exploratory randomised controlled trial is the process evaluation to assess how the intervention was delivered, the process of implementation and its acceptability to key stakeholders. Process evaluation data were collected through a variety of ways: during the delivery of the CHERRY sessions in the intervention children's centres, participants and the CHERRY tutors were asked to give their feedback at the end of each session. Reunion sessions were held at the children's centres 3 months after the intervention, when parents had the opportunity to provide more detailed qualitative feedback in a focus group setting. Parents from the intervention group were also asked their views of the intervention in the 6‐month follow‐up questionnaire.
In addition, semi‐structured telephone interviews (n = 11) were conducted with a purposively selected sample of individuals from both Islington and Cornwall including CHERRY trainers, parents who attended CHERRY, children's centre staff and the main researchers involved in collecting data and supporting the study. These interviews explored views on the nature of the intervention, its delivery and its potential impact. Discussions also focused on what were considered the positive features of the intervention, as well any problems that occurred. Finally, recommendations on how to improve and develop the intervention were considered.
Outcome data analysis
The data analysis consisted of the following steps: descriptive analyses were used to describe the social and demographic characteristics of study participants and their families, as well as food consumption characteristics of the participants. Independent t‐tests (or non‐parametric equivalent methods) were used to assess difference in primary outcome (fruit and vegetables consumption measured in g day−1) between the intervention and control groups at baseline. Similar analysis was conducted for other secondary, continuous outcomes such as child's consumption of sugary drinks measured in mL day−1. Paired t‐tests (or non‐parametric equivalents) were used to assess changes in outcomes from baseline to follow‐up. Longitudinal data were analysed using multilevel regression techniques taking into account potential clustering of individuals within children's centres and the repeated nature of the data (for each individual, up to four dietary recalls were available both at baseline and at 6 months). Potential confounding factors were included in multivariable analysis, as were the stratifying variables. Effect modifiers such as gender and geographical location (Islington/Cornwall) were also tested in regression models. For non‐continuous secondary outcomes, logistic regression was used in the appropriate steps of the analysis.
Discussion
The diets of pre‐school children in the United Kingdom are a major cause for concern. Dietary practices are influenced by a complex array of individual, social and environmental factors. Interventions to promote healthier dietary practices need to be multifaceted in nature as simple educational approaches alone will have minimal long‐term impact and fail to address health inequalities (National Institute for Health and Clinical Excellence 2007). Recent reviews of the nutrition and public health literature have highlighted a paucity of well‐designed interventions to tackle this problem (National Institute for Health and Clinical Excellence 2008). In the absence of high‐quality research, there is a temptation to rush into undertaking ambitious large‐scale intervention trials. However, the implementation and evaluation of complex interventions needs to be informed by detailed developmental and exploratory work (Medical Research Council 2008). This paper has outlined the methodology employed in the developmental and exploratory phases of an early years' nutrition intervention delivered in children's centres across Islington and Cornwall.
A lengthy, detailed and rigorous process was undertaken to explore carefully the nature of the nutrition intervention needed, as well as testing the newly developed intervention through an exploratory randomised controlled trial. Engagement with local stakeholders and the collection of both qualitative and quantitative data from parents and children's centre staff was immensely informative in understanding the dietary problems and challenges parents and staff faced. Particular attention was also placed in carefully selecting the most appropriate theory base for the intervention. Findings from systematic reviews of the nutrition and behaviour change literature were also very informative in guiding the selection of the intervention theoretical models and in designing the intervention programme. Particular emphasis was placed upon the development of self‐efficacy through practical skills development and confidence building.
Conducting the exploratory trial has provided very valuable insights into the feasibility and acceptability of the nutrition intervention and its evaluation. Our focus group and questionnaire data from parents and children centre staff clearly demonstrated that nutrition in early years is considered an important issue where more support is needed (Hayter et al. 2012; Ohly et al. 2012). Our diverse range of recruitment methods were very successful in attracting participants into the trial (n = 394) and a 77% retention rate (n = 304) at 6 months follow‐up is very good for a community‐based sample. It was interesting that a much higher retention rate (85%) was achieved for the control group compared with those in the intervention arm (70%). The process evaluation indicated that the intervention was highly praised by most participants as being informative, practical and tailored to their particular needs. Although the parental component of the intervention has been shown to be acceptable, plans to develop and implement food policies in the centres have not progressed as hoped. This was partly due to the major differences in how centres were organised in the two study areas. In Cornwall, centres tended to be much smaller and more informal organisations less amenable to developing food policies. In Islington where more progress was made in this area, concerns were expressed by staff that the adoption of food polices might deter lower income families from using the drop in services at the centres. More research is needed on the adoption and evaluation of local food policies in early years settings. Due to limited funding and the inability to provide comprehensive interpretation services, it was not possible to include potential participants who were not able to communicate effectively in English. Particularly for inner city locations with marked population diversity, further research is also needed on the most effective ways of engaging with these communities and in developing culturally appropriate early years' nutrition interventions.
Another valuable insight gained from the exploratory trial has been the ability to assess the acceptability of the evaluation methods used. The baseline and follow‐up parental interviews and 24‐h recalls, although time consuming, have proved an acceptable and suitable means of collecting the data. In the process evaluation, very few participants complained about the time or difficulty completing the evaluation measures. This confirms the work undertaken by the LIDNS team that the 24‐h recalls were an appropriate method for assessing diet in low‐income populations (Holmes et al. 2008).
In conclusion, the methodology employed in this study has provided a wide range of invaluable insights into the development and testing of an early years' community‐based nutrition intervention. The developmental and exploratory stages are of fundamental importance in developing, implementing and evaluating a complex intervention.
Source of funding
This work was commissioned by the Food Standards Agency in 2009 and supported by the Department of Health (UK) from 2010.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
RW, AD, HP, HC, LM, CP, PMc and GR designed and wrote the original study proposal. RW, AH, HO, GR, HC, LC, CP, PMc and AD developed the nutrition intervention programme and AH and HO carried out the majority of the data collection. RW, AH, HO, GR, LC and HP significantly contributed to writing this paper. HC and LM critically revised the draft manuscript. All authors read and approved the final version of the manuscript.
Acknowledgements
We would like to thank all the parents who gave up their time to take part in the study and the volunteers who kindly helped out with data collection. We would also like to thank Ashley Ecker for her support in recruiting parents, and collecting and entering data. Thanks are also due to the project steering group and the funding body, the Department of Health.
This article is published with the permission of the Controller of HMSO and the Queen's Printer for Scotland.
References
- Abidin R. (1995) Parenting Stress Index: Professional Manual, 3rd edn Psychological Assessment Resources Inc: Odessa. [Google Scholar]
- Ashfield‐Watt P.A.L. (2007) Effect of a pilot community intervention on fruit and vegetable intakes: use of FACET (Five‐a‐day Community Evaluation Tool). Public Health Nutrition 10, 671–680. [DOI] [PubMed] [Google Scholar]
- Bandura A. (1986) Social Foundation of Thought and Action: A Social Cognitive Theory. Prentice‐Hall: New York. [Google Scholar]
- Barker M. (2008) Constraints on food choices of women in the UK with lower educational attainment. Public Health Nutrition 11, 464–468. [DOI] [PubMed] [Google Scholar]
- Barton K.L., Wrieden W.L. & Anderson A.S. (2011) Validity and reliability of a short questionnaire for assessing the impact of cooking skills interventions. Journal of Human Nutrition and Dietetics 24, 588–595. [DOI] [PubMed] [Google Scholar]
- Bates B., Lennox A., Prentice A., Bates C. & Swann G. (2012) National Diet and Nutrition Survey. Headline Results from Years 1, 2 and 3 (Combined) of the Rolling Programme (2008/2009–2010/11) . In: Department of Health, editor. Food Standards Agency.
- Bell R. & Marshall D. (2003) The construct of food involvement in behavioral research: scale development and validation. Appetite 40, 235–244. [DOI] [PubMed] [Google Scholar]
- Carpiano R.M. & Daley D.M. (2006) A guide and glossary on post‐positivist theory building for population health. Journal of Epidemiology and Community Health. 60, 564–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darnton A. (2008) GSR Behaviour Change Knowledge Review . HM Treasury, Government Social Research Unit.
- Department for Communities and Local Government (2007) The English Indices of Deprivation. London: Department for Communities and Local Government. [Google Scholar]
- Department for Education (2012) The ‘Core Purpose’ of Sure Start Children's Centres . Available at: http://media.education.gov.uk/assets/files/pdf/s/sure%20start%20childrens%20centres%20core%20purpose.pdf (Accessed 1 October 2012).
- Dewey J. (1916) Democracy and Education. Macmillan: New York. [Google Scholar]
- Foresight (2007) Tackling Obesities: Future Choices – Building the Obesity System Map . Government Office for Science.
- Gregory J.R., Lowe S., Bates C.J., Prentice A., Jackson L.V., Smithers G. et al (2000) National Diet and Nutrition Survey: Children Aged 4–18 Years. HMSO: London. [Google Scholar]
- Hayter A.K.M., Draper A.K., Ohly H.R., Rees G.A., Pettinger C., McGlone P. et al (2012) A qualitative study exploring parental accounts of feeding pre‐school children in two low‐income populations in the UK. Maternal and Child Nutrition. doi: 10.1111/mcn.12017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes B., Dick K. & Nelson M. (2008) A Comparison of Four Dietary Assessment Methods in Materially Deprived Households in England. Public Health Nutrition 11, 444–456. [DOI] [PubMed] [Google Scholar]
- James W.P., Nelson M., Ralph A. & Leather S. (1997) Socioeconomic determinants of health. The contribution of nutrition to inequalities in health. British Medical Journal 314, 1545–1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaluzny A.D. & Hernandez S.R. (1988) Organisation change and innovation In: Health Care Management: A Text in Organisation Theory and Behaviour (eds Shortell S.M. & Kaluzny A.D.), 2nd edn, pp 379–417. Wiley: New : York. [Google Scholar]
- Lawrence W. & Barker M. (2009) A review of factors affecting the food choices of disadvantaged women. Proceedings of the Nutrition Society 68, 189–194. [DOI] [PubMed] [Google Scholar]
- Marmot M. (2010) Fair Society, Healthy Lives (The Marmot Review): A Strategic Review of Health Inequalities in England. UCL Institute of Health Equity: London. [Google Scholar]
- Maynard M., Gunnell D., Emmett P., Frankel S. & Davey Smith G. (2003) Fruit, vegetables, and antioxidants in childhood and risk of adult cancer: the Boyd Orr cohort. Journal of Epidemiology and Community Health 57, 218–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin J.A. & Jordan G.B. (1999) Logic models: a tool for telling your program's performance story. Evaluation and Programme Planning 22, 65–72. [Google Scholar]
- Medical Research Council (2000) A Framework for the Development and Evaluation of RCTs for Complex Interventions to Improve Health. Medical Research Council: London. [Google Scholar]
- Medical Research Council (2008) Developing and Evaluating Complex Interventions: New Guidance. Medical Research Council: London. [Google Scholar]
- Michie S., Johnston M., Abraham C., Lawton R., Parker D. & Walker A. (2005) Making psychological theory useful for implementing evidence based practice: a consensus approach. Quality and Safety of Health Care 14, 26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S., van Stralen M.M. & West R. (2011) The behaviour change wheel: a new method for characterising anddesigning behaviour change interventions. Implementation Science 6, 42–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore L.L., Singer M.R., Bradlee M.L., Djousse L., Proctor M.H., Cupples L.A. et al (2005) Intake of fruits, vegetables, and dairy products in early childhood and subsequent blood pressure change. Epidemiology 16, 4–11. [DOI] [PubMed] [Google Scholar]
- National Health Service (2011) 5 A Day Portion Sizes . Available at: http://www.nhs.uk/Livewell/5ADAY/Documents/Downloads/5ADAY_portion_guide.pdf (Accessed 15 May 2013).
- National Institute for Health and Clinical Excellence (2007) Behaviour Change at Population, Community and Individual Levels, Public Health Guidance 06. National Institute for Health and Clinical Excellence: London. [Google Scholar]
- National Institute for Health and Clinical Excellence (2008) Improving the Nutrition of Pregnant and Breastfeeding Mothers and Children in Low‐Income Households, Public Health Guidance 11. National Institute for Health and Clinical Excellence: London. [Google Scholar]
- Nelson M., Atkinson M. & Meyer J. (1997) Food Portion Sizes: A Photographic Atlas. Ministry of Agriculture, Fisheries and Food: London. [Google Scholar]
- Nelson M., Erens B., Bates B., Church S. & Boshier T. (2007) Low Income Diet and Nutrition Survey: Appendices . In: Food Standards Agency, editor. Norwich.
- Nicklaus S., Boggio V., Chabanet C. & Issanchou S. (2005) A prospective study of food variety seeking in childhood, adolescence and early adult life. Appetite 44, 289–297. [DOI] [PubMed] [Google Scholar]
- Ohly H.R., Hayter A.K.M., Pettinger C., Pikhart H., Watt R.G. & Rees G.A. (2012) Developing a nutrition intervention in children's centres: exploring views of parents in rural/urban settings in the UK. Public Health Nutrition, 1–6. doi: 10.1017/S1368980012003977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers E. (1983) Diffusion of Innovations. 3rd edn, Free Press: New York. [Google Scholar]
- Schwarzer R. & Renner B. (2009) Health‐Specific Self‐Efficacy Scales. Freie Universität Berlin: Berlin. Contract No.: 30th April 2012. [Google Scholar]
- Skinner J.D., Carruth B.R., Bounds W., Ziegler P. & Reidy K. (2002) Do food‐related experiences in the first 2 years of life predict dietary variety in school‐aged children? Journal of Nutrition Education and Behavior 34, 310–315. [DOI] [PubMed] [Google Scholar]
- Swinburn B., Egger G. & Raza F. (1999) Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Preventitive Medicine 29 (6 Pt 1), 563–570. [DOI] [PubMed] [Google Scholar]
- Taylor D., Bury M., Campling N., Carter S., Garfied S., Newbould J. et al (2006) A Review of the Use of the Health Belief Model (HBM), the Theory of Reasoned Action (TRA), the Theory of Planned Behaviour (TPB) and The Trans‐Theoretical Model (TTM) to Study and Predict Health Related Behaviour Change : National Institute for Health and Clinical Excellence, Department of Health.
- The NHS Information Centre (2010) Health Survey for England 2010 . In: The Health and Social Care Information Centre.
- The NHS Information Centre (2011) National Child Measurement Programme: England, 2010/11 School Year . The Health and Social Care Information Centre.
- Tylavsky F.A., Holliday K., Danish R., Womack C., Norwood J. & Carbone L. (2004) Fruit and vegetable intakes are an independent predictor of bone size in early pubertal children. American Journal of Clinical Nutrition 79, 311–317. [DOI] [PubMed] [Google Scholar]
- Wardle J., Guthrie C.A., Sanderson S. & Rapoport L. (2001) Development of the children's eating behaviour questionnaire. Journal of Child Psychology and Psychiatry 42, 963–970. [DOI] [PubMed] [Google Scholar]
- Watt R., Dowler E., Hardy R., Kelly Y., McGlone P., Molloy B. et al (2006) Promoting Recommended Infant Feeding Practices in a Low‐Income Sample – Randomised Controlled Trial of A Peer Support Intervention. University College London Unit SSR: London. [Google Scholar]
- Watt R.G. & Sheiham A. (1999) Inequalities in oral health: a review of the evidence and recommendations for action. British Dental Journal 187, 6–12. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2003) Diet, nutrition and the prevention of chronic diseases . WHO Technical Report Series 916, Geneva. [PubMed]
- Wrieden W.L., Anderson A.S., Longbottom P.J., Valentine K., Stead M., Caraher M. et al (2007) The impact of a community‐based food skills intervention on cooking confidence, food preparation methods and dietary choices – an exploratory trial. Public Health Nutrition 10, 203–211. [DOI] [PubMed] [Google Scholar]


