Abstract
The specific role of weight change in the first weeks of gestation in fetal growth has not been fully explored in humans. Our aims were to investigate: (1) the specific association between weight change in the first trimester of pregnancy (WCT1) and size at birth in term pregnancies; and (2) the role of placental weight in this relationship. From 2002 women included in the French EDEN study, 1744 mother–child pairs reached term, had pre‐pregnancy weight available and at least five measures of weight in pregnancy. We extrapolated women's weight at each week of gestation with a three‐degree polynomial model and estimated weight change during each trimester of gestation. We used a multivariate linear model to investigate the associations between WCT1 and birth size after taking into account potential confounders (age, parity, BMI, tobacco use, educational level, length of gestation, newborn gender, weight change after the first trimester and centre of study). Then, we performed path analysis to investigate whether the relation between WCT1 and birth size could be mediated by placental weight. After taking into account weight gain in later gestation, WCT1 was positively associated with birthweight. Results of path analysis showed that there was no direct association between WCT1 and birth size, but that this association was mediated by placental weight. Weight change during the first weeks of pregnancy may impact on fetal growth independently of weight change later in pregnancy through its effects on placental growth and function.
Keywords: weight gain, pregnancy, birth, fetal growth, women's weight, placental development
Introduction
Maternal pre‐pregnancy body mass index (BMI) is strongly and positively associated with birthweight after accounting for gestational age (Kramer et al. 2002). When BMI before pregnancy is taken into account, maternal weight gain during pregnancy has an independent positive effect on birthweight (Kinnunen et al. 2003; Kari et al. 2007; Heude et al. 2012). High maternal pre‐pregnancy BMI is associated with lower weight gain during pregnancy, which may, in part, be due to medical advice but may also indicate a regulation of gestational weight gain based on maternal fat stores at the start of pregnancy (Heude et al. 2012). Maternal weight gain in early pregnancy is explained mainly by an expansion of both plasma volume and of fat stores to sustain fetal perfusion and nutrition throughout pregnancy (Naeye & Tafari 1985; Bernstein et al. 2001). Maternal weight gain later in pregnancy is more influenced by fetal and placental weight increase and fluid retention. Therefore, maternal weight gain in the first trimester of pregnancy may have a specific effect on fetal growth. Few studies have focused on the pattern of weight gain during pregnancy, in relation to pregnancy outcomes. Abrahams & Selvin reported that each kilogram of maternal weight gain during the first and second trimesters was associated with an increase in birthweight (Abrams & Selvin 1995). Neufeld et al. showed that maternal weight change from the first to the second trimester (between the third and sixth months) was strongly associated with birth length, but not weight change between the sixth and ninth months, and concluded that mid‐gestation may be a sensitive period for linear fetal growth (Neufeld et al. 2004).
Maternal weight change early in pregnancy may influence fetal growth through various mechanisms: quantitative and qualitative difference in energy intake and therefore an availability of nutrients for fetal and placental growth (Rosso 1980; Abrams & Selvin 1995); plasma volume expansion and fat storage in early pregnancy (Naeye & Tafari 1985). On the other hand, obesity and vomiting in early pregnancy appear to be specifically related to maternal weight change in early pregnancy.
The aim of this study was to investigate the specific relationship between maternal weight change in the first trimester of pregnancy and fetal growth and birth size, and to test whether this association could be mediated by placental growth.
Key messages
-
•
Women's weight change in early pregnancy is less explained by fetal and placental weights than their weight change in later pregnancy.
-
•
Maternal weight change in early pregnancy is mainly explained by plasma volume expansion and fat storage to sustain fetal nutrition.
-
•
Weight change in the first semester appears to be related to fetal growth through its influence in placental growth and function.
-
•
Weight change in early pregnancy may be taken into account in fetal growth monitoring, especially in women with BMI below 25 kg m−2.
Methods
Participants
Data were collected for mother–child pairs enrolled in the ongoing EDEN mother–child cohort (study of pre‐ and early post‐natal determinants of child development and health), from University Hospitals in Nancy and Poitiers, France (Drouillet et al. 2008). Women attending their first prenatal visit before 24 weeks of gestation at these two maternity departments were invited to participate in this study. Enrolment in the study started in February and September 2003 in Poitiers and Nancy, respectively, and lasted 27 months in each centre. Exclusion criteria were multiple pregnancies, known pre‐gestational diabetes, plans to move outside the region in the next 3 years, and lack of ability to speak and read French. Among eligible women, 55% (2002 women) accepted to participate (1034 women in Nancy and 968 in Poitiers). The women and their offspring are being followed up for over 5 years.
Written consent was obtained for the mother and for her offspring after delivery. The EDEN study has been approved by the ethics committee (Comité Consultatif pour la Protection des personnes dans la Recherche Biomédicale) of Kremlin Bicêtre Hospital and by the Commission Nationale de l'Informatique et des Libertés.
Data collection
The mother's pre‐pregnancy weight and educational level were obtained by interview at inclusion. At 24–28 weeks of gestation, they answered a self‐administered questionnaire and a clinical examination was performed by midwife research assistants. Maternal height was measured with a wall Seca 2006 stadiometer (Seca, Hamburg, Germany) to the nearest 0.2 cm. Also, during this clinical examination, women were weighed with an electronic scale Terraillon SL 351 (Hanson Ltd, Hemel Hempstead, UK). Measures of fetal anthropometry [head circumference (HC), abdominal circumference (AC), biparietal diameter (BD) and femoral length (FL)] were obtained from routine ultrasound of pregnancy monitoring at about 22 weeks, and 32 weeks of amenorrhea.
The same research assistants performed a second clinical examination, on average 2 days after delivery. The mother's weight was measured with the same protocol as earlier. The newborn were weighed using an electronic Seca scales (Seca 737 in Nancy and Seca 335 in Poitiers) and birth length was measured with a wooden somatometre (Testut, Béthune, France).
Additional data were extracted from the maternity records: mother's weight measured and reported by clinicians at each prenatal visit (eight measures on average), parity and placental weight at birth. Placental weight was systematically recorded in Poitiers centre, whereas in Nancy it tended to be more recorded in case of Caesarean. Data on frequent vomiting in early pregnancy were obtained by questionnaire at recruitment. Data on cigarette use before pregnancy were obtained by questionnaire at 24–28 weeks of gestation and those for cigarette use during the third trimester of gestation were obtained by questionnaire in the post‐partum period.
Generated variables
Maternal education was categorised in three levels: ‘Before admission at university’; ‘Admission at university’; and ‘≥2 years after admission at university’. We defined three categories of cigarette smoking: ‘never’ for women who did not smoke both before and during pregnancy; ‘before pregnancy only’ for women who smoked before but not during pregnancy; and ‘in pregnancy’ for women who declared smoking during pregnancy. We estimated fetal weight (EFW) during the second and third trimesters of gestation using the Hadlock formula based on four measures: HC, AC, BD and FL (Hadlock et al. 1985). Fetal growth between the second and the third trimesters of pregnancy was estimated by calculating the EFW in the third trimester minus EFW in the second trimester. Also, fetal growth between 6 months and delivery was calculated as birthweight minus EFW at 6 months. Large‐for‐gestational age (LGA) and small‐for‐gestational age (SGA) were defined as birthweights over the 90th percentile and below the 10th percentile, respectively, of French gestational age‐ and gender‐specific reference curves (Mamelle et al. 1996). The newborn's ponderal index was computed as birthweight (kg) divided by birth length (m) cubed. Pre‐pregnancy BMI was calculated as reported weight before pregnancy divided by height (m) squared. BMI categories were defined as thin (BMI < 18.5 kg m−2), normal (BMI between 18.5 and 25 kg m−2), overweight (BMI between 25 and 30 kg m−2) and obese (BMI ≥ 30 kg m−2).
Population selection
From the 2002 mothers included in the EDEN study, we excluded 142 mother–child pairs with fewer than five measures of maternal weight during pregnancy. Among the mothers with at least five measures of weight during pregnancy, we excluded 14 whose weight before pregnancy was missing. From the remaining mothers, we excluded from this analysis the 102 with preterm births, as weight change in the first trimester was not related to prematurity, and preterm babies may have experienced specific situations which would have affected their growth in utero. Analyses were performed for 1744 mother–child pairs.
Estimation of weight change
In the EDEN study, measures of women's weight through pregnancy were not obtained at the same gestational ages. Therefore, we would have many missing values if we studied weight change at a given period during pregnancy. The important number of measures of women's weight at different times during pregnancy (eight measures on average) allowed us to have a precise estimation of women's weight at each week of gestation.
Maternal weight at each week of gestation was estimated using a third‐degree polynomial model, which included a subject random effect on the intercept, slope and curvature, and is based on women's weights measured during prenatal visits. When compared, the observed weight before pregnancy (mean ± standard deviation = 62.2 ± 12.8, which was not included in the model) and the predicted weight (mean ± standard deviation = 62.3 ± 12.7) were highly correlated (r = 0.99). Thereafter, we computed weight change at each trimester of pregnancy: for the first trimester (WCT1), predicted weight at 14 completed weeks minus predicted weight at the start of gestation; for the second trimester (WCT2), predicted weight at 28 completed weeks minus predicted weight at 14 weeks; and for the third trimester (WCT3), predicted weight at delivery (adjusted for gestational age) minus predicted weight at 28 weeks.
Statistical analysis
Characteristics of the mother and their newborns are described by means ± standard deviations and percentages (n). The evolution of the average weight of mothers during gestation was modelled within BMI strata. Associations between WCT1 and maternal characteristics (age, BMI, cigarette smoking, parity, education, frequent vomiting in early pregnancy and recruitment centre) were estimated with a linear regression model.
The associations between WCT1 and fetal growth and birth size were analysed in three steps. Firstly, the associations between WCT1 and fetal growth, birthweight, placental weight and birth length were analysed by linear models, with adjustment for recruitment centre, maternal age, education, pre‐pregnancy BMI and maternal height, and additional adjustment for gestational age (gestational age at ultrasound for the EFW at the second and third trimesters), cigarette smoking, parity and the newborn's gender. The relations between WCT1 and SGA, and LGA were analysed with a logistic model with the same adjustments as before, except for gestational age and newborn's gender.
In the second step, we adjusted for WCT2 and WCT3 to investigate whether the observed associations were independent of weight gain in later gestation.
In the final step, we selected the 1304 mother–child pairs for whom placental weight was available. Placental weight at delivery was considered to be a marker of placental growth and function. As used before in the EDEN study, we adopted path analysis to investigate whether a causal relationship between WCT1 and birth size (birthweight and length) was mediated by the placenta (Regnault et al. 2011). Figure 1 displays the model we postulated for birthweight. A single‐headed arrow represents the direct effect of one variable on another, with a relation defined by a linear equation. We postulated that WCT1 might influence birthweight through placental function. In path models, a given variable can be an explanatory variable in one equation and an outcome in the other. The assumption of normality is required for all variables that are influenced by at least one variable (Loehlin 2004). Variables included in the model were pre‐adjusted for variables that were significantly related to them, when considered in multivariable models (see legend of Fig. 1). Path analyses allow an estimation of the indirect effects of a variable on an outcome (effects that are mediated by other variables) (Loehlin 2004).
Figure 1.
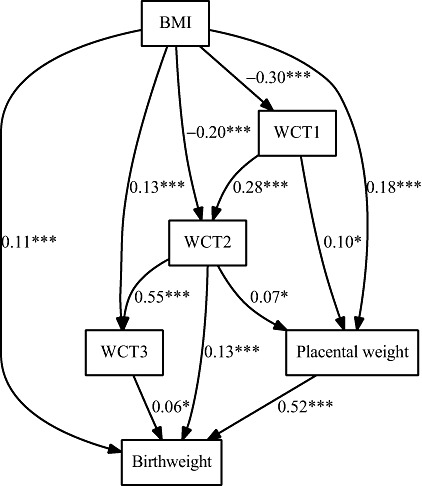
Path diagram depicting the relations between pre‐pregnancy body mass index, weight changes in pregnancy, placental weight and birthweight. P‐value codes: ***<0.0001, **0.0001–0.001, *0.001–0.05. Variables in the model were pre‐adjusted for characteristics which remained significantly associated with them when included in multivariate linear model among recruitment centre, maternal age, education, maternal height, gestational age, cigarette smoking, parity and newborn's gender. BMI, body mass index; WCT1, WCT2 and WCT3, weight changes in the first, the second and the third trimesters.
The conditions of validity of the path model were verified with some usual criteria: the hierarchical chi‐square test (P‐value > 0.05), the goodness‐of‐fit index (GFI between 0.95 and 1), the adjusted GFI (AGFI between 0.95 and 1) and the root mean square error of approximation (<0.05) (Loehlin 2004).
The different paths in the model (representing the relations between the different variables) can be associated with standardised partial correlation coefficients that are interpreted as coefficients of correlation between two variables when all the other variables are held constant.
The same approach was used to assess the potential mediation of the placenta in the association between WCT1 and birth length. We assessed whether the relations were different by recruitment centre, newborn gender, parity, BMI and cigarette smoking, and vomiting in early pregnancy. We also investigated if gestational diabetes and gestational hypertension modified our results.
For sensitivity analyses, we have done the same investigations in subjects from Poitiers centre only where placental weight was systematically recorded.
All analyses used SAS software (version 9.2, Cary, NC, USA). In particular, the TCALIS procedure was used for path analysis.
Results
In the first step of our analysis, we excluded women with less than five measures of weight during pregnancy. When we compared women who were included vs. those who were excluded in term births, those who were included declared less tobacco use before and during pregnancy (P = 0.006) and had a higher study level (P = 0.02).
In the second step, we excluded mother–child pairs whose placental weight at delivery was not available. About 94% of women from Poitiers centre had a measure of placental weight vs. 43% for those from Nancy centre. In term births, women without a measure placental weight were more frequently diagnosed for gestational hypertension and had a higher study level. Birthweight and birth length were higher in those whose placental weight was measured (http://onlinelibrary.wiley.com/10.1111/j.1740-8709.2012.00423.x/suppinfo). These differences were due to differences in these characteristics between study centres. Women from Nancy were more frequently diagnosed for gestational hypertension (5.6% vs. 2.8%, P = 0.005) and had a higher educational level (P < 0.0001), whereas offspring's mean birthweight and height were higher in Poitiers centre (P = 0.007).
The mean weight gain of mothers in the first trimester was 3.3 kg and they gained 13.6 kg on average during pregnancy (Table 1). The proportion of women with frequent vomiting in early pregnancy was 23.6%. Figure 2 illustrates a sigmoid curve for weight during pregnancy. Thin and normal weight women gained more weight during pregnancy. WCT1 was positively associated with maternal age, whereas there was a negative association with maternal pre‐pregnancy BMI (Table 2). Women from the Poitiers centre gained more weight in the first trimester than those from Nancy. Women who smoked before pregnancy only and those who were still smoking during pregnancy gained more weight in the first trimester. Educational level was negatively associated with WCT1. Frequent vomiting in early pregnancy was associated with a lower WCT1 (Table 2).
Table 1.
Characteristics, mean ± standard deviation or % (frequency) of mothers and newborn
| n | Mean ± SD | |
|---|---|---|
| Age (years) | 1744 | 29.0 ± 4.9 |
| Height (cm) | 1726 | 163.5 ± 6.1 |
| Pre‐pregnancy weight (kg) | 1744 | 62.2 ± 12.8 |
| Body mass index (kg m−2) | 1726 | 23.2 ± 4.6 |
| Pregnancy weight gain (kg) | 1717 | 13.6 ± 4.7 |
| Weight gain in the first trimester (kg) | 1744 | 3.30 ± 2.48 |
| Weight gain in the second trimester (kg) | 1744 | 6.8 ± 2.1 |
| Weight gain in the third trimester (kg) | 1744 | 4.5 ± 2.3 |
| Frequent vomiting in early pregnancy [% (n)] | 1724 | 23.6 (406) |
| Educational level [% (n)] | 1720 | |
| 1 (Before admission at university) | 28.2 (485) | |
| 2 (admission at university) | 17.9 (308) | |
| 3 (≥2 years after admission at university) | 53.9 (927) | |
| Cigarette smoking [% (n)] | 1725 | |
| Never | 62.8 (1084) | |
| Before pregnancy only | 20.8 (358) | |
| During pregnancy | 16.4 (283) | |
| Recruitment centre [% (n)] | 1744 | |
| Poitiers | 48.5 (846) | |
| Nancy | 51.5 (898) | |
| Parity [%(n)] | 1744 | |
| 0 | 32.2 (562) | |
| 1 | 33.8 (590) | |
| ≥2 | 33.9 (592) | |
| Gestational age (weeks) | 1744 | 39.5 ± 1.2 |
| Birthweight (g) | 1740 | 3340 ± 438 |
| Birth length (cm) | 1715 | 49.8 ± 2.1 |
| Small‐for‐gestational age [% (n)] | 1740 | 7.9 (139) |
| Large‐for‐gestational age [% (n)] | 1740 | 8.6 (149) |
SD, standard deviation.
Figure 2.

The average weight of mothers during gestation, within body mass index strata.
Table 2.
Mother's weight gain (kg) during the first trimester of pregnancy according to her characteristics, estimated by linear regression models
| Parameter | Beta ± SE* | P‐value |
|---|---|---|
| Age (years) | 0.04 ± 0.01 | 0.005 |
| Body mass index (kg m−2) | −0.16 ± 0.01 | <.0001 |
| Cigarette smoking | <0.0001 | |
| Never | −0.76 ± 0.16 | |
| Before pregnancy only | 0.12 ± 0.19 | |
| During pregnancy | Reference | |
| Parity | 0.34 | |
| 0 | −0.13 ± 0.16 | |
| 1 | −0.21 ± 0.14 | |
| ≥2 | Reference | |
| Educational level | <0.0001 | |
| 1 (before admission at university) | 0.72 ± 0.14 | |
| 2 (admission at university) | 0.30 ± 0.16 | |
| Reference | ||
| Vomiting in early pregnancy | 0.0008 | |
| Not frequent | 0.45 ± 0.13 | |
| Frequent | Reference | |
| Recruitment centre | 0.002 | |
| Poitiers | 0.36 ± 0.11 | |
| Nancy | Reference | |
SE, standard error.
When adjusted for maternal and pregnancy characteristics (recruitment centre, maternal age, educational, pre‐pregnancy BMI, maternal height, gestational age, cigarette smoking, parity and newborn's gender), WCT1 was positively associated with fetal growth (EFW at second and third trimester, and change in EFW from second to third trimester, change in EFW between third trimester and delivery and placental weight) (Table 3). Furthermore, WCT1 was positively associated with birthweight, birth length and risk of LGA, with a negative relation with risk of SGA. These associations remained significant when further adjusted for WCT2 and WCT3 (Table 3).
Table 3.
Newborn characteristics for a 1‐kg change in weight during the first trimester of pregnancy (WCT1), before and after adjustment for weight change in the second and third trimesters of pregnancy (WCT2 and WCT3). Results are from separate linear and logistic models
| Before adjustment for WCT2 and WCT3 | Further adjustment for WCT2 and WCT3 | |||
|---|---|---|---|---|
| Beta ± SE | P‐value | Beta ± SE | P‐value | |
| Estimated fetal weight at 20–24 weeks (g) | 1.26 ± 0.64 | 0.05 | 1.47 ± 0.65 | 0.02 |
| Change in estimated fetal weight from 20–24 to 30–34 (g) | 9.53 ± 2.66 | 0.0003 | 7.86 ± 2.72 | 0.004 |
| Estimated fetal weight at 30–34 weeks (g) | 12.78 ± 2.57 | <0.0001 | 11.24 ± 2.63 | <0.0001 |
| Change in estimated fetal weight from 30–34 weeks to birth (g) | 11.17 ± 4.10 | 0.006 | 6.07 ± 4.16 | 0.14 |
| Birthweight (g) | 24.19 ± 3.98 | <0.0001 | 17.74 ± 4.02 | <0.0001 |
| Birth length (cm) | 0.09 ± 0.02 | <0.0001 | 0.07 ± 0.02 | 0.0001 |
| Ponderal index* (kg m−3) | 0.05 ± 0.028 | 0.07 | 0.03 ± 0.03 | 0.31 |
| Placental weight (g) | 5.30 ± 1.40 | 0.0001 | 4.76 ± 1.45 | 0.001 |
| Odds ratio (95% CI) | P‐value | Odds ratio (95% CI) | P‐value | |
| Small‐for‐gestational age | 0.86 (0.79–0.94) | 0.0004 | 0.90 (0.82–0.97) | 0.005 |
| Large‐for‐gestational age | 1.13 (1.06−1.21) | 0.0005 | 1.10 (1.03−1.19) | 0.008 |
SE, standard error. *Ponderal index = birthweight (kg)/birth length (cm)3. Adjustment for recruitment centre, maternal age, education, pre‐pregnancy body mass index, maternal height, gestational age, cigarette smoking, parity and newborn's gender.
Figure 1 displays the path diagram depicting the direct associations between pre‐pregnancy BMI, WCT1, WCT2, WCT3 and placental weight and their direct association with birthweight. The total, direct and indirect associations are reported in Table 4.
Table 4.
Total, direct and indirect associations of maternal anthropometry and placental weight on birthweight
| Total | Direct | Indirect | ||
|---|---|---|---|---|
| Pre‐pregnancy body mass index | Standardised beta | 0.14 | 0.11 | 0.03 |
| Standard error | 0.03 | 0.02 | 0.02 | |
| P‐value | <0.0001 | <0.0001 | 0.11 | |
| Weight change in the first trimester | Standardised beta | 0.10 | 0 | 0.10 |
| Standard error | 0.02 | 0.02 | ||
| P‐value | <0.0001 | <0.0001 | ||
| Weight change in the second trimester | Standardised beta | 0.20 | 0.13 | 0.08 |
| Standard error | 0.03 | 0.03 | 0.02 | |
| P‐value | <0.0001 | 0 | 0.002 | |
| Weight change in the third trimester | Standardised beta | 0.06 | 0.06 | 0 |
| Standard error | 0.03 | 0.03 | ||
| P‐value | 0.03 | 0.03 | ||
| Placental weight | Standardised beta | 0.52 | 0.52 | 0 |
| Standard error | 0.02 | 0.02 | ||
| P‐value | <0.0001 | <0.0001 |
Standardised betas are interpretable as correlation coefficients.
Results of path analysis showed that pre‐pregnancy BMI was negatively associated with WCT1 (r = −0.30) and WCT2 (r = −0.20), while it was positively associated with WCT3 (r = 0.13, P < 0.0001). According to the postulated path diagram, pre‐pregnancy BMI was also independently associated with placental weight (r = 0.18) and birthweight (r = 0.11, P < 0.0001).
WCT1 was not independently associated with birthweight, but a significant indirect association was found (r = 0.10, P < 0.0001) (Table 4). WCT1 was directly associated with placental weight (r = 0.10, P = 0.002), which, in turn, was independently associated with birthweight (r = 0.52). There was a direct association between WCT1 and WCT2 (r = 0.28), which was independently associated with birthweight (r = 0.13, P < 0.0001) and had a small direct association with placental weight (r = 0.07, P = 0.03).
There was only a weak association between WCT3 and birthweight (r = 0.06, P = 0.03). As there was no direct association between WCT3 and placental weight, this path was removed from the model.
The associations with birth length in place of birthweight were similar to that observed for birthweight (Fig. 1 and http://onlinelibrary.wiley.com/10.1111/j.1740-8709.2012.00423.x/suppinfo). However, a small independent association between WCT1 and birth length was observed (r = 0.07, P = 0.01).
In summary, WCT1 influenced birthweight and birth length mainly through its effects on placental weight and WCT2.
Further adjustment for gestational diabetes and gestational hypertension did not change the association between WCT1 and newborn anthropometry. When the same analyses were restricted to Poitiers centre where placental weight was systematically measured for sensitivity analyses, the same results were observed.
Discussion
Weight change in the first trimester was associated with fetal growth and birth size even when weight changes in later gestation were taken into account. Results of path analysis showed that the relation between weight change in the first trimester and birth size was, in part, mediated by placental weight at birth, which we used as a proxy of placental growth and function. As women in our study centres appeared to be quite different and that placental weight was systematically recorded in Poitiers centre but not in Nancy, we restricted our analysis to women in Poitiers centre and observed similar results. No difference in weight gain during the first trimester was observed between women who had a measure of placental weight (3.3 g) and those without a measure of placental weight (3.2 kg, P = 0.7).
Weights at each week of gestation were estimated based on measures of weight during pregnancy (eight on average). Previous studies used piecewise linear regression models to estimate weight change at each trimester of pregnancy from measured weights during pregnancy (Abrams et al. 1995; Carmichael et al. 1997). In our study, a polynomial model and three degrees was adequate, as the quadratic term was not significant. The important number of measures of women's weight (eight measures on average) at different moments of pregnancy in the EDEN study allowed a precise estimation of women's weight at each week of gestation. To verify that our model gave good estimations of women's weights during pregnancy, we compared women's reported pre‐pregnancy weight (mean = 62.2 kg ± 12.8 kg, which was not included in our model) with women's pre‐pregnancy weight obtained with the model (mean = 62.3 kg ± 12.7). These two measures were comparable and highly correlated (r = 0.99). The same verification was done with women's weight measured between 24 and 28 weeks (25th week on average) and women's weight at 25 weeks of gestation obtained with our model. The two measures were also comparable and highly correlated. Thereafter, we added women's weight measured between 24 and 28 weeks of gestation to our model to reduce the number of women with less than five measures of weight in our sample.
In this study, weight change in the first trimester is considered as an indicator of women's nutritional status in early pregnancy. One may argue that, due to physiological changes in early pregnancy, weight change in the first trimester of pregnancy may not fully reflect the women's nutritional status. However, the physiological changes in early pregnancy are related to women's nutrition status. The choice of the first trimester as a limit of the early pregnancy period may be found arbitrary. However, it is more common to adopt the limits of different trimesters as different stages of pregnancy. Also, it would have been interesting to have a longitudinal model of repeated measurements of fetal biometry, but since we had only two fetal measurements during pregnancy, this was not possible in this study. The use of birthweight minus EFW at sixth month of pregnancy as an indicator of fetal growth may be weakened by the fact that the error of measurement of birthweight may be different from the error of measurement of fetal size by ultrasound (errors related to the use of ultrasound).
The relation between WCT1 and birthweight and birth length may be explained by several mechanisms: an adequate placental development, which, in turn, influences fetal growth; fat storage in early pregnancy and its later release for fetal growth; and an availability of macronutrients and micronutrients for early fetal growth.
The mother provides oxygen, nutrients, hormones and antibodies to the fetus via the placenta, and the end products of fetal metabolism are removed via the placenta. Placental weight at delivery is positively correlated with the newborn's weight, but the maximal growth of the placenta precedes that of the fetus. Its growth rate is initially greater than that of the fetus (Thame et al. 2004). A small placenta usually alters fetal growth (Belkacemi et al. 2010). Maternal nutrition is associated with placental weight (Belkacemi et al. 2010), and a reduction in maternal nutrition in early pregnancy may alter placental growth and birthweight. In our study, maternal weight gain (used as a proxy of nutritional state) in the first trimester influenced placental weight at delivery. Thame et al. found that placental volume at 14 weeks of gestation and the rate of placental growth between 17 weeks and 20 weeks were significantly associated with fetal measurement at 35 weeks, even when placental volume at 24 weeks was added to the model (Thame et al. 2004). The rapid growth of the placenta early in pregnancy is important to supply nutrients necessary for fetal growth. All these findings confirm the hypothesis that placental volume and placental growth are influenced by maternal nutrition in early pregnancy and, in turn, also contribute to fetal growth.
Plasma volume expansion in early pregnancy was identified as an important factor of weight gain in early pregnancy and particularly necessary for fetal growth. Abrahams et al. suggested that a low plasma volume expansion might limit uteroplacental flow, reducing the transfer of nutrients to support fetal growth (Abrams & Selvin 1995).
Neufeld et al. reported that weight change between the third and sixth month of gestation had a positive effect on linear fetal growth and not weight change from 6 to 9 months of gestation (Neufeld et al. 2004). In our study, we found an effect of WCT1 on birth length independently of placental weight, suggesting that the influence of weight change in early pregnancy on birth length may begin early in the first 3 months, but this independent effect of WCT1 on birth length was small. Weight change in the first trimester may reflect energy intake at this stage of pregnancy and therefore correspond to an availability of nutrients that supply fetal growth even in the earliest stage of the first trimester, before the contact between the embryo and maternal blood via the placenta (Burton et al. 2007). It has been suggested that endometrial‐decidual glands are sources of nutrients for the embryo; the endometrium contains large accumulations of glycogen that are greatest close to the materno–fetal interface (Burton et al. 2007). The endometrial‐decidual glands have also been identified as a source of growth factors such as the epidermal growth factor (Hempstock et al. 2004; Burton et al. 2007) which stimulates cytotrophoblast cell proliferation, which represents the materno–fetal interface during early pregnancy (Hamilton & Boyd 1960).
Studies suggested that weight change in the first trimester may influence fetal growth through fat storage in early pregnancy. There is a specific pattern of fat deposition during pregnancy (Taggart et al. 1967). Starting from early pregnancy, fat appears to be deposited preferentially over the hips, back and upper thighs. Fat stored in early pregnancy is released for fetal growth as pregnancy advances (Naeye & Tafari 1985).
Studies reported that total pregnancy weight gain is negatively associated with pre‐pregnancy BMI (Diouf et al. 2011). To our knowledge, the pattern of weight gain (through the trimesters of pregnancy) in association with pre‐pregnancy BMI has not been reported before. We found that pre‐pregnancy BMI was negatively associated with weight gain in the first and second trimesters of pregnancy, but it was positively associated with weight gain in the third trimester. Weight change in the first trimester seemed to be a result of physiologic adaptations to the mother's periconceptional fat. The lower weight gain during the first trimester in mothers with higher BMI did not impact on fetal growth. Women's with higher BMI have sufficient nutrient availability to support fetal and placental growth. BMI before pregnancy had significant independent effects on the newborn and placental weights (Kramer et al. 2002).
An excessive weight gain during pregnancy is associated with adverse pregnancy outcomes (Caesarean sections, gestational hypertension and macrosomia) (Crane et al. 2009). Conversely, women who gained less than the recommended weight gain have higher risks of pre‐eclampsia, Caesarean sections, macrosomia and low birthweight (Langford et al. 2011). In this study, we found that weight change in the first trimester of pregnancy was associated with fetal growth and risk of LGA. We did not find any association between weight change in the first trimester of pregnancy and adverse pregnancy outcomes such as gestational diabetes, gestational hypertension or risk of Caesarean sections. If these results are confirmed, the monitoring of weight change in early pregnancy may be considered by clinicians as an important factor in the management of fetal growth without threatened effect on women's health.
In this study, we found that frequent vomiting in early pregnancy was associated with poor weight gain in the first trimester. Other studies also reported that vomiting in early pregnancy is associated with weight loss in early pregnancy (Kinnunen et al. 2003; Kari et al. 2007; Heude et al. 2012). When compared to infants of mothers who gained weight in early pregnancy, infants of mothers who lost weight in early pregnancy were found to more often have poor fetal growth and to be SGA (Niebyl 2010). In our study, we did not find a statistically significant relationship between weight loss in the first 3 months of gestation and risk of SGA.
Conclusion
Weight change during the first weeks of pregnancy seems to impact on fetal growth, independently of later weight changes during pregnancy. Weight change in early pregnancy and placental growth appeared as two related indicators of adequate adaptation to pregnancy to support fetal growth. Weight change in early pregnancy may participate in fetal growth and placental function.
Sources of funding
The EDEN Study is funded by grants from the Foundation for Medical Research, the French Ministry of Research: the Institut Fédératif de Recherche program, the Institut National de la Santé et de la Recherche Médicale Human Nutrition National Research Program, and the Diabetes National Research Program (via a collaboration with the French Association for Diabetes Research), the French Ministry of Health Perinatality Program, the French Agency for Environment Security, the French National Institute for Population Health Surveillance, the Paris–Sud University, the French National Institute for Health Education, Nestlé, the National Education Health Insurance (MGEN), the French Speaking Association for the Study of Diabetes and Metabolism, the National Agency for Research (non‐thematic programme), and the National Institute for Research in Public Health (TGIR health cohort 2008 programme).
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
All authors participated in the design and/or analysis and interpretation of the data and revision of the manuscript. ID conducted the statistical analyses, reviewed the literature and prepared the manuscript. JB and OM supervised the statistical analyses, the study design and manuscript preparation. AF, MK, MAC and BH designed the EDEN study, helped design the study's analytical strategy and revised the manuscript.
Supporting information
Fig. S1. Path diagram depicting the relations between pre‐pregnancy BMI, weight changes in pregnancy, placental weight and birth length. P‐value codes: ***<0.0001, **0.0001–0.001, *0.001–0.05. BMI, body mass index; WCT1, WCT2 and WCT3, weight changes in the first, the second and the third trimesters. Variables in the model were pre‐adjusted for characteristics which remained significantly associated with them when included in multivariate linear model among: recruitment centre, maternal age, education, maternal height, gestational age, cigarette smoking, parity, newborn gender.
Table S1. Comparison of women and their newborn for women whose placental weight was available vs. those for whom placental weight was not available: mean ± standard deviation or % (frequency).
Table S2. Total, direct and indirect effects of maternal anthropometry and placental weight on birth length.
Acknowledgement
We thank Beverley Balkau who reviewed the manuscript for content and language.
Constitution of the EDEN Mother–Child Cohort Study Group: M.A. Charles, M. de Agostini, A. Forhan, B. Heude, P. Ducimetière, M. Kaminski, M.J. Saurel‐Cubizolles, P. Dargent, X. Fritel, B. Larroque, N. Lelong, L. Marchand, C. Nabet, I. Annesi‐Maesano, R. Slama, V. Goua, G. Magnin, R. Hankard, O. Thiebaugeorges, M. Schweitzer, B. Foliguet and N. Job‐Spira.
References
- Abrams B. & Selvin S. ( 1995. ) Maternal weight gain pattern and birth weight . Obstetrics & Gynecology 86 , 163 – 169 . [DOI] [PubMed] [Google Scholar]
- Abrams B. , Carmichael S. & Selvin S. ( 1995. ) Factors associated with the pattern of maternal weight gain during pregnancy . Obstetrics & Gynecology 86 , 170 – 176 . [DOI] [PubMed] [Google Scholar]
- Belkacemi L. , Nelson D.M. , Desai M. & Ross M.G. ( 2010. ) Maternal undernutrition influences placental‐fetal development . Biology of Reproduction 83 , 325 – 331 . [DOI] [PubMed] [Google Scholar]
- Bernstein I.M. , Ziegler W. & Badger G.J. ( 2001. ) Plasma volume expansion in early pregnancy . Obstetrics & Gynecology 97 , 669 – 672 . [DOI] [PubMed] [Google Scholar]
- Burton G.J. , Jauniaux E. & Charnock‐Jones D.S. ( 2007. ) Human early placental development: potential roles of the endometrial glands . Placenta 28 ( Suppl. A ), S64 – S69 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmichael S. , Abrams B. & Selvin S. ( 1997. ) The pattern of maternal weight gain in women with good pregnancy outcomes . American Journal of Public Health 87 , 1984 – 1988 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane J.M. , White J. , Murphy P. , Burrage L. & Hutchens D. ( 2009. ) The effect of gestational weight gain by body mass index on maternal and neonatal outcomes . Journal of Obstetrics and Gynaecology Canada 31 , 28 – 35 . [DOI] [PubMed] [Google Scholar]
- Diouf I. , Charles M.A. , Blondel B. , Heude B. & Kaminski M. ( 2011. ) Discordant time trends in maternal body size and offspring birthweight of term deliveries in France between 1972 and 2003: data from the French National Perinatal Surveys . Paediatric and Perinatal Epidemiology 25 , 210 – 217 . [DOI] [PubMed] [Google Scholar]
- Drouillet P. , Forhan A. , De Lauzon‐Guillain B. , Thiebaugeorges O. , Goua V. , Magnin G. et al . ( 2008. ) Maternal fatty acid intake and fetal growth: evidence for an association in overweight women. The ‘EDEN mother‐child’ cohort (study of pre‐ and early postnatal determinants of the child's development and health) . The British Journal of Nutrition 101 , 1 – 9 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadlock F.P. , Harrist R.B. , Sharman R.S. , Deter R.L. & Park S.K. ( 1985. ) Estimation of fetal weight with the use of head, body, and femur measurements – a prospective study . American Journal of Obstetrics and Gynecology 151 , 333 – 337 . [DOI] [PubMed] [Google Scholar]
- Hamilton W.J. & Boyd J.D. ( 1960. ) Development of the human placenta in the first three months of gestation . Journal of Anatomy 94 , 297 – 328 . [PMC free article] [PubMed] [Google Scholar]
- Hempstock J. , Cindrova‐Davies T. , Jauniaux E. & Burton G.J. ( 2004. ) Endometrial glands as a source of nutrients, growth factors and cytokines during the first trimester of human pregnancy: a morphological and immunohistochemical study . Reproductive Biology and Endocrinology 2 , 58 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heude B. , Thiebaugeorges O. , Goua V. , Forhan A. , Kaminski M. , Foliguet B. et al . ( 2012. ) Pre‐pregnancy body mass index and weight gain during pregnancy: relations with gestational diabetes and hypertension, and birth outcomes . Maternal and Child Health Journal 16 , 355 – 363 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kari Y.L. , Rössner S. & Neovius M. ( 2007. ) Maternal predictors of birthweight: the importance of weight gain during pregnancy . Obesity Research & Clinical Practice 1 , 243 – 252 . [DOI] [PubMed] [Google Scholar]
- Kinnunen T.I. , Luoto R. , Gissler M. & Hemminki E. ( 2003. ) Pregnancy weight gain from 1960s to 2000 in Finland . International Journal of Obesity and Related Metabolic Disorders 27 , 1572 – 1577 . [DOI] [PubMed] [Google Scholar]
- Kramer M.S. , Morin I. , Yang H. , Platt R.W. , Usher R. , McNamara H. et al . ( 2002. ) Why are babies getting bigger? Temporal trends in fetal growth and its determinants . The Journal of Pediatrics 141 , 538 – 542 . [DOI] [PubMed] [Google Scholar]
- Langford A. , Joshu C. , Chang J.J. , Myles T. & Leet T. ( 2011. ) Does gestational weight gain affect the risk of adverse maternal and infant outcomes in overweight women? Maternal and Child Health Journal 7 , 860 – 865 . [DOI] [PubMed] [Google Scholar]
- Loehlin J.C. ( 2004. ) Latent variable models: An introduction to factor, path, and structural equation analysis . Laurence Erlbaum Associates, Inc. : Mahwah, NJ . [Google Scholar]
- Mamelle N. , Munoz F. & Grandjean H. ( 1996. ) [Fetal growth from the AUDIPOG study. I. Establishment of reference curves] . Journal de Gynecologie, Obstetrique et Biologie de la Reproduction 25 , 61 – 70 . [PubMed] [Google Scholar]
- Naeye R.L. & Tafari N. ( 1985. ) Biologic bases for international fetal growth curves . Acta Paediatrica Scandinavica. Supplement 319 , 164 – 169 . [DOI] [PubMed] [Google Scholar]
- Neufeld L.M. , Haas J.D. , Grajeda R. & Martorell R. ( 2004. ) Changes in maternal weight from the first to second trimester of pregnancy are associated with fetal growth and infant length at birth . The American Journal of Clinical Nutrition 79 , 646 – 652 . [DOI] [PubMed] [Google Scholar]
- Niebyl J.R. ( 2010. ) Clinical practice. Nausea and vomiting in pregnancy . The New England Journal of Medicine 363 , 1544 – 1550 . [DOI] [PubMed] [Google Scholar]
- Regnault N. , Botton J. , Heude B. , Forhan A. , Hankard R. , Foliguet B. et al . ( 2011. ) Higher cord C‐peptide concentrations are associated with slower growth rate in the 1st year of life in girls but not in boys . Diabetes 60 , 2152 – 2159 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosso P. ( 1980. ) Placental growth, development, and function in relation to maternal nutrition . Federation Proceedings 39 , 250 – 254 . [PubMed] [Google Scholar]
- Taggart N.R. , Holliday R.M. , Billewicz W.Z. , Hytten F.E. & Thomson A.M. ( 1967. ) Changes in skinfolds during pregnancy . The British Journal of Nutrition 21 , 439 – 451 . [DOI] [PubMed] [Google Scholar]
- Thame M. , Osmond C. , Bennett F. , Wilks R. & Forrester T. ( 2004. ) Fetal growth is directly related to maternal anthropometry and placental volume . European Journal of Clinical Nutrition 58 , 894 – 900 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig. S1. Path diagram depicting the relations between pre‐pregnancy BMI, weight changes in pregnancy, placental weight and birth length. P‐value codes: ***<0.0001, **0.0001–0.001, *0.001–0.05. BMI, body mass index; WCT1, WCT2 and WCT3, weight changes in the first, the second and the third trimesters. Variables in the model were pre‐adjusted for characteristics which remained significantly associated with them when included in multivariate linear model among: recruitment centre, maternal age, education, maternal height, gestational age, cigarette smoking, parity, newborn gender.
Table S1. Comparison of women and their newborn for women whose placental weight was available vs. those for whom placental weight was not available: mean ± standard deviation or % (frequency).
Table S2. Total, direct and indirect effects of maternal anthropometry and placental weight on birth length.


