Abstract
The Haitian National Nutrition Policy identifies the promotion of optimal complementary feeding (CF) practices as a priority action to prevent childhood malnutrition. We analysed data from the nationally representative 2005–2006 Haiti Demographic Health Survey using the World Health Organization 2008 infant and young child feeding indicators to describe feeding practices among children aged 6–23 months and thus inform policy and programme planning. Multivariate regression analyses were used to identify the determinants of CF practices and to examine their association with child growth outcomes. Overall, 87.3% of 6–8‐month‐olds received soft, solid or semi‐solid foods in the previous 24 h. Minimum dietary diversity (MDD), minimum meal frequency (MMF) and minimum acceptable diet (MAD) were achieved in 29.2%, 45.3% and 17.1% of children aged 6–23 months, respectively. Non‐breastfed children were more likely to achieve MDD than breastfed children of the same age (37.3% vs. 25.8%; P < 0.001). The proportion of children achieving MMF varied significantly by age (P < 0.001). Children with overweight mothers were more likely to achieve MDD, MMF and MAD [odds ratio (OR) 2.08, P = 0.012; OR 1.81, P = 0.02; and OR 2.4, P = 0.01, respectively] than children of normal weight mothers. Odds of achieving MDD and MMF increased with household wealth. Among mothers with secondary or more education, achieving MDD or MAD was significantly associated with lower mean weight‐for‐age z‐score and height‐for‐age z‐score (P‐value <0.05 for infants and young child feeding indicator × maternal education interaction). CF practices were mostly inadequate and contributed to growth faltering among Haitian children 6–23 months old.
Keywords: complementary feeding, infant and child nutrition, child growth, health policy, low‐income countries
Introduction
To promote optimal child growth and development, the World Health Organization (WHO) recommends exclusive breastfeeding (EBF) for the first 6 months of life followed by continued breastfeeding and gradual introduction of appropriate and safe complementary foods until age 23 months (UNICEF et al. 2010). Specific recommendations for complementary feeding (CF) practices include feeding a variety of developmentally appropriate nutrient‐dense foods at age‐appropriate frequency depending on the breastfeeding status of the child (Dewey 2003; World Health Organization 2005). Providing education around these improved infants and young child feeding (IYCF) practices with or without food supplements is an effective strategy for reducing the risk of stunting and improving developmental outcomes among children in low‐income countries (Bhutta et al. 2008).
In 2007, the WHO released a series of indicators to assess whether specific recommended CF practices, including adequate dietary diversity and appropriate frequency of feeding, are being implemented by caregivers at the population level (Daelmans et al. 2009; World Health Organization 2010). Recent analyses have applied the WHO IYCF indicator definitions to nationally representative Demographic and Health Survey (DHS) data from countries in Asia and sub‐Saharan Africa. The analyses examine the determinants of IYCF practices (Hazir et al. 2012; Joshi et al. 2012; Senarath & Dibley 2012; Senarath et al. 2012a,b) and the relationship between IYCF indicators and child growth (Marriott et al. 2010, 2012; Disha et al. 2012; Zongrone et al. 2012). To date, no one has examined these indicators in the Latin American and Caribbean (LAC) region.
Haiti has the highest rates of childhood underweight and wasting in the LAC region, and one‐third of Haitian children less than 5 years of age are stunted (Lutter & Chaparro 2008). The Haitian National Nutrition Policy identifies the promotion of optimal CF practices starting at age 6 months as a priority action for the prevention of childhood malnutrition (Ministère de la Santé Publique et de la Population 2012). While scale‐up of IYCF interventions is high priority, there are limited available data to identify specific target populations and guide the development of context‐specific strategies including behaviour change messages, particularly in urban environments (Ruel et al. 2004; Menon et al. 2005; World Bank 2010). The objectives of this analysis are to describe the prevalence and determinants of WHO‐recommended feeding practices among Haitian children aged 6–23 months and to describe the relationship between these feeding practices and child growth outcomes using the 2005–2006 Haiti DHS (HDHS).
Key messages
The majority (>50%) of Haitian children aged 6–23 months do not meet the World Health Organization recommendations for dietary diversity and feeding frequency. Interventions should encourage caregivers to feed a greater variety of foods to younger children and increase frequency among older children in this age group.
The dietary patterns of Haitian children aged 6–23 months differ by department. Children in the Ouest department, including metropolitan Port‐au‐Prince, were least likely to meet the minimum dietary diversity recommendation.
Dietary diversity is associated with lower weight‐for‐age z‐score and height‐for‐age z‐score among Haitian children with mothers with secondary or more education, but not among those with less education.
Materials and methods
Study design
This secondary analysis uses data from the 2005–2006 HDHS that included a cross‐sectional nationally representative sample of 9998 households in all 10 departments of Haiti. The survey used a two‐stage cluster sampling design. Information was collected on households, women and men of reproductive age, and children under the age of 5 within the households. Informed consent was obtained from all survey participants prior to data collection. Response rate was 99.6%. More information about survey design, data collection and data management is available in the 2005–2006 HDHS final report (Cayemittes et al. 2007). Permission to use the data was obtained from ICF International (Calverton, MD, USA).
We used data on 1701 children aged 6–23 months living with the respondent at the time of the survey.
Data collection
Feeding indicators
We used the updated WHO IYCF indicators (World Health Organization 2010) in our analyses. Four indicators were calculated with some modifications as explained below due to limitations in data available in the 2005–2006 HDHS.
Introduction of solid, semi‐solid or soft foods
Proportion of children aged 6–8 months who received solid, semi‐solid or soft foods in the previous 24 h.
Minimum dietary diversity (MDD)
Proportion of breastfed and non‐breastfed children aged 6–23 months who received foods from four or more out of seven food groups in the previous 24 h. The seven food groups defined by the WHO guidelines included grains, roots and tubers, legumes and nuts, dairy products (milk, infant formula, yogurt, cheese), flesh foods (meat, liver or organ meats, fish, poultry), eggs, vitamin A‐rich fruits and vegetables, and other fruits and vegetables. There was no minimum quantity of food required to be counted as meeting the food group.
Minimum meal frequency (MMF)
Proportion of breastfed and non‐breastfed children aged 6–23 months who received solid, semi‐solid or soft foods at least the minimum number of times in the previous 24 h. For breastfed children, the minimum number of times for children aged 6–8 months was two or more, and for aged 9–23 months was three or more. For non‐breastfed children, the minimum number of times was four or more, but for non‐breastfed children milk feeds were counted in addition to solid, semi‐solid or soft foods. The HDHS data set includes milk as a yes/no variable but does not include the number of milk feeds per day. It was not possible to calculate the MMF indicator for 86 out of 430 non‐breastfed children for whom, after considering the number of times solid, semi‐solid and soft foods were fed and whether any milk was given, required information about the specific number of milk feeds in order to determine whether or not they met the MMF criteria. We excluded these 86 children from multivariate analyses after running sensitivity analyses based on multiple assumption scenarios.
Minimum acceptable diet (MAD)
Proportion of breastfed children aged 6–23 months who achieved both MDD and MMF in the previous 24 h. Proportion of non‐breastfed children who received two or more milk feeds and four or more out of six food groups (milk product group excluded) and met the MMF criteria in the previous 24 h. Given that the HDHS data set does not include the number of milk feeds per day, it was not possible to calculate this indicator for any non‐breastfed children who received milk. Multivariate analysis was therefore restricted to breastfed children only.
In addition to the WHO indicators described above, we calculated a continuous dietary diversity score ranging from 0 to 7 based on the total number of WHO‐defined food groups received in the previous 24 h.
Growth outcomes
Weight‐for‐age (WAZ), height‐for‐age (HAZ) and weight‐for‐height (WHZ) z‐scores were calculated using the WHO Child Growth Standards Macro for Statistical Package for the Social Sciences (spss; WHO Multicentre Growth Reference Study Group 2006).
Other biological, household and environmental characteristics
Several biological factors are known determinants of post‐natal growth including child age, multiple vs. single birth, child sex and maternal body mass index (BMI; normal 18.5–24.9 kg m−2, underweight <18.5 kg m−2, overweight ≥25.0 kg m−2).
Variables were selected to represent access to health care during two different periods: pregnancy and early childhood. There are multiple pathways through which access to antenatal care (ANC) might impact IYCF practices and post‐natal growth. Infant feeding counselling and other ANC services may influence breastfeeding initiation and duration (Vieira et al. 2010; Agho et al. 2011). Multiple micronutrient supplementation during pregnancy has been associated with birth size (Shah & Ohlsson 2009), which, in turn, is associated with growth across childhood (Adair 2007). Based on WHO Focused ANC guidelines (World Health Organization 2002), we classified children born to mothers who reported four or more ANC visits vs. zero to three visits.
Access to health care at least once during early childhood was assessed by whether the mother reported currently having a Ministry of Public Health and Population (MOPHP) child health card. Per MOPHP protocols, all children aged 0–59 months who access health care in Haiti should receive a ‘road‐to‐health’ card and participate in routine growth monitoring and infant feeding counselling by community or clinic‐based staff. Children of mothers who reported a lost card or never having received a card were classified as not having a health card.
Other risk factors and potential confounders included in the analysis were maternal education (none, primary, secondary or higher), current maternal employment (yes, no), residence (urban, rural) and department (Nord‐Ouest, Nippes, Sud‐Est, Nord, Nord‐Est, Artibonite, Centre, Sud, Grand‐Anse and Ouest, which includes metropolitan Port‐au‐Prince). Department is the term used for the country's major administrative units. For multivariate growth analysis, low maternal education was classified as primary or less, and high maternal education was secondary or more.
The standard DHS wealth variable was also included in the analysis. It was calculated by factor analysis based on household size, water source, type of toilet, primary cooking method, materials used in housing construction and ownership of household assets. More information on construction of the DHS wealth index can be found elsewhere (Rutstein et al. 2004).
Data analysis
All statistical analyses were performed using spss software version 19 (IBM Corp., Armonk, NY, USA). We used the spss 19 Complex Sample module to account for the two‐stage cluster sampling design of the HDHS survey. Probability weights were applied to all analyses to account oversampling and undersampling of certain groups to produce a nationally representative sample. All sample sizes reported are estimated using these weights. Unadjusted prevalence estimates were compared across categories using Pearson's chi‐square. Means were compared across categories using analysis of variance. Multiple logistic regression was used to identify predictors of MDD, MMF and MAD. Logistic regression results are presented as ORs with 95% confidence interval (CI) and P‐values. We used multiple linear regression to assess the relationship between the WHO ICYF indicators (MDD, MMF, MAD) and achieved growth z‐score (WAZ, HAZ, WHZ) after adjusting for the other covariates in the model. Results are presented as β parameter estimates with 95% CI and P‐values. Observations with missing data for any of the predictors were excluded for each regression analysis. In particular, maternal BMI and maternal education were available for fewer children than other variables. Values presented in the text are means or percentages with 95% CI. For all analyses, significance was accepted at a P < 0.05 level and all tests were two‐sided.
Results
Characteristics of the sample
Table 1 describes the general characteristics of the sample (N = 1701). Child and household variables were generally as expected, with equal numbers of male and female children and a low prevalence of multiple births. Eighty‐five per cent of children had a health card, suggesting they had seen a health provider at least once since birth.
Table 1.
Characteristics of children aged 6–23 months who live with mother, HDHS 2005–2006 (N = 1701)
| N | % | 95% CI | ||
|---|---|---|---|---|
| Child characteristics | ||||
| Sex | ||||
| Female | 855 | 50.3 | 47.6 | 53.0 |
| Male | 846 | 49.7 | 47.0 | 52.4 |
| Age group | ||||
| 6–8 months | 299 | 17.6 | 15.2 | 20.2 |
| 9–11 months | 274 | 16.1 | 14.1 | 18.3 |
| 12–17 months | 608 | 35.7 | 32.9 | 38.7 |
| 18–23 months | 520 | 30.6 | 28.0 | 33.3 |
| Type of birth | ||||
| Multiple | 38 | 2.2 | 1.4 | 3.6 |
| Single | 1663 | 97.8 | 96.4 | 98.6 |
| Maternal characteristics | ||||
| Maternal BMI | ||||
| Underweight | 109 | 13.2 | 10.6 | 16.4 |
| Overweight | 147 | 18.0 | 14.6 | 21.9 |
| Normal | 564 | 68.8 | 64.3 | 72.9 |
| Maternal education | ||||
| No school | 243 | 29.4 | 25.3 | 34.0 |
| Primary | 361 | 43.8 | 39.1 | 48.5 |
| Secondary+ | 221 | 26.8 | 22.9 | 31.1 |
| Mother currently employed | ||||
| Yes | 844 | 49.8 | 46.6 | 53.1 |
| No | 850 | 50.2 | 46.9 | 53.4 |
| Household characteristics | ||||
| Wealth quintile | ||||
| Lowest | 410 | 24.1 | 20.5 | 28.1 |
| Second | 359 | 21.1 | 18.2 | 24.4 |
| Middle | 326 | 19.1 | 16.5 | 22.2 |
| Fourth | 356 | 20.9 | 17.8 | 24.5 |
| Highest | 250 | 14.7 | 12.1 | 17.7 |
| Residence | ||||
| Urban | 580 | 34.1 | 30.9 | 37.4 |
| Rural | 1121 | 65.9 | 62.6 | 69.1 |
| Department | ||||
| Nord‐Ouest | 107 | 6.3 | 5.1 | 7.8 |
| Nippes | 45 | 2.7 | 2.1 | 3.4 |
| Sud‐Est | 105 | 6.2 | 4.9 | 7.8 |
| Nord | 164 | 9.6 | 8.0 | 11.5 |
| Nord‐Est | 63 | 3.7 | 3.0 | 4.5 |
| Artibonite | 309 | 18.1 | 15.4 | 21.2 |
| Centre | 193 | 11.4 | 8.9 | 14.4 |
| Sud | 100 | 5.9 | 4.7 | 7.4 |
| Grand‐Anse | 73 | 4.3 | 3.2 | 5.7 |
| Ouest (including PAP) | 542 | 31.8 | 28.6 | 35.3 |
| Access to health care | ||||
| Currently has child health card | ||||
| Yes | 1457 | 85.6 | 82.2 | 88.5 |
| No | 244 | 14.4 | 11.5 | 17.8 |
| Mother antenatal visit | ||||
| 4+ | 827 | 50.8 | 47.4 | 54.3 |
| 0–3 times | 799 | 49.2 | 45.7 | 52.6 |
BMI, body mass index; CI, confidence interval; HDHS, Haiti Demographic and Health Survey; PAP, Port‐au‐Prince.
Prevalence of maternal overweight (18.0%) was higher than underweight (13.2%). The majority of mothers had a normal BMI (68.8%). More than two‐thirds of mothers had at least some primary education and half of mothers identified themselves as unemployed at the time of the survey. Half of the mothers completed at least four ANC visits during their last pregnancy.
Fewer children in our sample were in the highest wealth category (14.7%) compared with the others. Approximately one‐third of the sample lived in the Ouest department, which includes metropolitan Port‐au‐Prince. Two‐thirds of the overall sample was rural.
Feeding practices
Time of introduction of soft, solid or semi‐solid foods
There were 87.3% of the 6–8‐month–olds who received soft, solid or semi‐solid foods in the previous 24 h. The total number of children in 6–8 months age group in the sample was too small to examine this outcome by department.
Minimum dietary diversity
Overall, 29.2% of children aged 6–23 months achieved MDD. Non‐breastfed children aged 6–23 months were more likely to achieve minimum diversity than breastfed children of the same age (37.3% vs. 25.8%; P < 0.001). This is consistent with the fact that breast milk was not counted as a food group, but other milk products more commonly given to non‐breastfed children were counted as a unique group. Among breastfed children, the proportion of children achieving MDD increased significantly with age (12.9% 6–8 months, 24.7% 9–11 months, 31.5% 12–17 months, 32.4% 18–23 months; P < 0.001) (Table 2). In contrast, the proportion of non‐breastfed children achieving MDD decreased with age. This is possibly explained by the small number of non‐breastfed children in younger age groups (Table 2). Children in the Artibonite department were most likely to achieve MDD (41.1%), whereas only 19.3% of children in Sud‐Est achieved this indicator (Table 3).
Table 2.
Proportion of children achieving WHO IYCF indicator by age group and breastfeeding status among children aged 6–23 months living with mother, HDHS 2005–2006
| 6–8 months | 9–11 months | 12–17 months | 18–23 months | Total | P‐value | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | |||||||
| Minimum dietary diversity | |||||||||||||||||||||
| Breastfed | 290 | 12.9 | 9.0 | 18.1 | 243 | 24.7 | 19.1 | 31.4 | 461 | 31.5 | 26.0 | 37.6 | 207 | 32.4 | 25.2 | 40.5 | 1201 | 25.8 | 22.7 | 29.2 | <0.001 |
| Non‐breastfed | 4 | 88.4 | 51.1 | 98.2 | 24 | 47.6 | 27.0 | 69.0 | 130 | 34.1 | 25.2 | 44.4 | 304 | 37.2 | 30.0 | 45.1 | 462 | 37.3 | 31.4 | 43.6 | 0.014 |
| Combined | 297 | 13.7 | 9.8 | 18.8 | 272 | 28.1 | 22.1 | 35.1 | 600 | 32.4 | 27.2 | 38.1 | 518 | 35.1 | 29.4 | 41.2 | 1687 | 29.2 | 26.1 | 32.6 | <0.001 |
| Minimum meal frequency | |||||||||||||||||||||
| Breastfed | 288 | 70.4 | 63.1 | 76.7 | 241 | 35.2 | 28.1 | 43.1 | 456 | 41.5 | 35.1 | 48.1 | 204 | 39.1 | 31.4 | 47.4 | 1189 | 46.8 | 43.0 | 50.7 | <0.001 |
| Non‐breastfed | 3 | 87.8 | 36.5 | 98.9 | 12 | 77.3 | 43.4 | 93.8 | 101 | 47.9 | 34.1 | 62.1 | 230 | 34.1 | 25.6 | 43.8 | 346 | 40.1 | 32.8 | 47.9 | 0.014 |
| Combined | 291 | 70.6 | 63.3 | 76.9 | 252 | 37.2 | 30.0 | 45.0 | 557 | 42.6 | 37.0 | 48.5 | 434 | 36.5 | 30.1 | 43.3 | 1534 | 45.3 | 41.6 | 49.0 | <0.001 |
| Minimum acceptable diet | |||||||||||||||||||||
| Breastfed | 286 | 12.2 | 8.4 | 17.5 | 241 | 12.4 | 8.3 | 18.2 | 456 | 19.6 | 14.9 | 25.2 | 204 | 23.9 | 17.1 | 32.3 | 1187 | 17.1 | 14.3 | 20.3 | 0.011 |
CI, confidence interval; HDHS, Haiti Demographic and Health Survey; WHO, World Health Organization; IYCF, infant and young child feeding.
Table 3.
Proportion of children achieving WHO IYCF indicator by department among breastfed and non‐breastfed children 6–23 months living with mother, HDHS 2005–2006
| Indicator | Age group | Nord‐Ouest | Nippes | Sud‐Est | Nord | Nord‐Est | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | |||||||
| Minimum diet diversity | 6–23 | 107 | 24.9 | 16.4 | 36.1 | 45 | 21.0 | 13.8 | 30.7 | 105 | 19.3 | 13.2 | 27.3 | 163 | 28.0 | 19.6 | 38.2 | 62 | 29.9 | 23.5 | 37.2 |
| Minimum meal frequency | 6–23 | 97 | 28.6 | 20.5 | 38.3 | 43 | 40.1 | 28.7 | 52.6 | 100 | 33.2 | 25.2 | 42.3 | 148 | 40.5 | 30.8 | 50.9 | 57 | 34.0 | 27.5 | 41.3 |
| Minimum acceptable diet † | 6–23 | 77 | 14.0 | 8.9 | 21.2 | 34 | 9.7 | 4.1 | 21.2 | 79 | 8.3 | 4.4 | 15.4 | 117 | 17.1 | 10.7 | 26.3 | 48 | 11.2 | 6.5 | 18.6 |
| Indicator | Age group | Artibonite | Centre | Sud | Grand‐Anse | Ouest (including PAP) | Total | P‐value | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | N | % | 95% CI | |||||||||
| Minimum diet diversity | 6–23 | 307 | 41.1 | 31.1 | 51.9 | 190 | 30.0 | 22.9 | 38.3 | 100 | 36.9 | 28.5 | 46.2 | 73 | 21.4 | 14.7 | 29.9 | 533 | 25.6 | 20.2 | 31.9 | 1686 | 29.2 | 26.1 | 32.6 | 0.004 |
| Minimum meal frequency | 6–23 | 285 | 53.3 | 41.1 | 65.1 | 183 | 45.5 | 36.3 | 55.0 | 89 | 41.6 | 30.3 | 53.9 | 68 | 30.4 | 22.8 | 39.2 | 465 | 52.7 | 45.8 | 59.5 | 1534 | 45.3 | 41.6 | 49.0 | 0.002 |
| Minimum acceptable diet † | 6–23 | 201 | 28.9 | 19.1 | 41.2 | 143 | 19.4 | 12.8 | 28.4 | 77 | 19.7 | 12.7 | 29.1 | 59 | 13.8 | 8.0 | 23.0 | 351 | 13.6 | 9.3 | 19.4 | 1187 | 17.1 | 14.3 | 20.3 | 0.003 |
CI, confidence interval; HDHS, Haiti Demographic and Health Survey; WHO, World Health Organization; IYCF, infant and young child feeding. †Breastfed children only.
Table 4 presents foods fed in the previous 24 h by age category. The mean number of food groups consumed increased from 2.08 in 6–8‐month group to 3.04 at 18–23‐month group (P < 0.001). Grains, roots and tubers were the most common group fed across all age groups followed by legumes and nuts. A much larger proportion of children who consumed legumes consumed beans and peas (49.7%) compared with nuts (3.1%). Consumption of dairy products did not vary by age. Milk products (33.6%) were more commonly fed to 6–23‐month‐olds than infant formula (7.2%) or other dairy products such as cheese or yogurt (7.2%). Overall, 37.0% of children aged 6–23 months received a non‐dairy animal source food (flesh food or eggs) in the previous 24 h. The most common sources were beef, pork or lamb (14.9%), and fish (12.9%). Consumption of eggs was low across 6–23‐months‐olds (8.0%) and did not increase significantly with age. Consumption of vitamin A‐rich fruits and vegetables increased with age. Dark green leafy vegetables were more commonly fed than yellow‐orange vegetables (4.4%) or vitamin A‐rich fruits (22.8%). There were significant differences in consumption of legumes and nuts, dairy products, flesh foods, vitamin A‐rich fruits and vegetables, and other fruits and vegetables by department (Fig. 1). Consumption of legumes and nuts (63.8%), flesh foods (42.7%) and vitamin A‐rich fruits and vegetables (45.8%) were all highest in the Artibonite compared with the other nine departments. Consumption of other fruits and vegetables was highest in Centre (49.1%) and lowest in the Sud‐Est (15.6%).
Table 4.
Food groups † and food types fed in the previous 24 h among children aged 6–23 months living with caregiver, HDHS 2005–2006
| Group | Foods included | 6–8 months | 9–11 months | 12–17 months | 18–23 months | Total (6–23 months) | P‐value | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | ||||||||
| Group 1: grains, roots and tubers | 73.1 | 66.6 | 78.7 | 90.5 | 85.7 | 93.8 | 91.4 | 88.5 | 93.6 | 90.2 | 87.0 | 92.8 | 87.7 | 85.5 | 89.5 | <0.001 | |
| Cereals | Baby cereal | 12.8 | 8.7 | 18.3 | 12.6 | 7.5 | 20.3 | 11.3 | 8.2 | 15.6 | 10.4 | 7.7 | 13.9 | 11.5 | 9.3 | 14.1 | 0.83 |
| Porridge | Porridge of gruel | 34.4 | 28.5 | 40.9 | 44.2 | 37.1 | 51.6 | 33.0 | 28.4 | 38.1 | 28.9 | 24.4 | 33.9 | 33.8 | 30.7 | 37.1 | 0.003 |
| Grains | Bread, noodles other made from grains | 45.2 | 37.8 | 52.8 | 65.3 | 58.0 | 71.9 | 74.2 | 69.4 | 78.4 | 72.9 | 68.0 | 77.3 | 67.3 | 64.0 | 70.3 | <0.001 |
| Tubers | Potatoes, cassava or other tubers | 8.0 | 5.0 | 12.5 | 11.3 | 8.0 | 15.8 | 17.7 | 14.4 | 21.6 | 17.3 | 13.4 | 22.0 | 14.8 | 12.6 | 17.4 | 0.001 |
| Group 2: legumes and nuts | 27.6 | 22.0 | 34.0 | 52.6 | 45.8 | 59.2 | 52.9 | 47.9 | 57.9 | 61.5 | 56.4 | 66.4 | 51.0 | 47.7 | 54.3 | <0.001 | |
| Legumes | Beans, peas, lentils | 26.5 | 21.1 | 32.8 | 51.2 | 44.3 | 58.0 | 51.1 | 46.0 | 56.1 | 60.5 | 55.4 | 65.4 | 49.7 | 46.3 | 53.1 | <0.001 |
| Nuts | Any type of nuts | 1.7 | 0.6 | 4.6 | 2.1 | 0.8 | 5.7 | 4.0 | 2.3 | 6.8 | 3.5 | 1.9 | 6.3 | 3.1 | 2.2 | 4.5 | 0.40 |
| Group 3: dairy products | 41.7 | 34.4 | 49.4 | 41.9 | 34.5 | 49.7 | 36.5 | 31.9 | 41.4 | 35.2 | 29.4 | 41.4 | 37.9 | 34.6 | 41.3 | 0.32 | |
| Milk | Tinned, powdered or fresh animal milk | 37.7 | 30.3 | 45.7 | 37.4 | 30.0 | 45.4 | 32.2 | 27.4 | 37.4 | 30.8 | 25.4 | 36.9 | 33.6 | 30.3 | 37.0 | 0.32 |
| Infant formula | Infant/baby formula | 7.0 | 3.9 | 12.3 | 7.2 | 4.4 | 11.5 | 8.9 | 6.4 | 12.2 | 5.4 | 3.4 | 8.5 | 7.2 | 5.7 | 9.1 | 0.36 |
| Milk products | Cheese, yogurt, other milk products | 7.9 | 4.7 | 12.9 | 11.6 | 6.2 | 20.7 | 7.3 | 4.9 | 10.7 | 4.4 | 2.8 | 7.0 | 7.2 | 5.5 | 9.4 | 0.077 |
| Group 4: flesh foods | 14.2 | 9.9 | 20.1 | 27.0 | 21.0 | 34.0 | 37.7 | 32.2 | 43.5 | 38.3 | 32.2 | 44.8 | 32.1 | 28.5 | 35.9 | <0.001 | |
| Meat | Meat (beef, pork, lamb, etc.) | 6.3 | 3.7 | 10.5 | 13.6 | 9.2 | 19.6 | 16.0 | 12.4 | 20.5 | 19.0 | 14.3 | 24.8 | 14.9 | 12.4 | 17.8 | 0.002 |
| Liver | Liver, heart, other organs | 1.8 | 0.6 | 5.2 | 2.3 | 0.9 | 5.6 | 4.3 | 2.6 | 6.8 | 3.8 | 2.0 | 7.0 | 3.3 | 2.4 | 4.7 | 0.39 |
| Fish | Fish or shellfish | 7.6 | 4.9 | 11.8 | 9.8 | 6.5 | 14.4 | 16.7 | 13.1 | 21.1 | 13.1 | 10.0 | 16.9 | 12.9 | 10.8 | 15.3 | 0.003 |
| Chicken | Chicken, other poultries | 1.0 | 0.3 | 3.6 | 5.8 | 2.8 | 11.5 | 6.0 | 4.2 | 8.6 | 6.0 | 4.2 | 8.6 | 5.2 | 3.7 | 7.2 | 0.081 |
| Group 5: eggs | 6.3 | 3.5 | 11.3 | 9.2 | 6.1 | 13.6 | 8.9 | 6.6 | 12.0 | 7.1 | 5.0 | 10.1 | 8.0 | 6.6 | 9.6 | 0.56 | |
| Group 6: vitamin A‐rich fruits and vegetables | 22.8 | 17.4 | 29.1 | 32.5 | 26.3 | 39.5 | 36.3 | 31.1 | 41.8 | 39.0 | 33.7 | 44.7 | 34.1 | 30.7 | 37.7 | 0.001 | |
| Vitamin A‐rich fruits | Mangoes, papayas, others | 4.0 | 1.9 | 8.5 | 4.8 | 2.4 | 9.2 | 4.7 | 3.0 | 7.3 | 3.9 | 2.3 | 6.6 | 4.4 | 3.1 | 6.0 | 0.94 |
| Yellow‐orange vegetables | Pumpkin, carrots, squash | 9.9 | 5.9 | 16.0 | 17.5 | 12.3 | 24.4 | 16.4 | 12.9 | 20.5 | 17.9 | 14.3 | 22.1 | 15.9 | 13.6 | 18.4 | 0.11 |
| Dark green leafy | Spinach, kale, watercress | 12.8 | 9.0 | 17.7 | 20.4 | 15.3 | 26.5 | 25.0 | 20.4 | 30.1 | 27.3 | 22.4 | 32.8 | 22.8 | 19.9 | 26.0 | <0.001 |
| Group 7: other fruits and vegetables | 23.6 | 17.7 | 30.9 | 23.6 | 17.7 | 30.9 | 33.0 | 27.7 | 38.8 | 32.8 | 27.4 | 38.8 | 30.0 | 26.7 | 33.6 | 0.062 | |
| Mean dietary diversity score ‡ | 2.08 | 1.91 | 2.26 | 2.79 | 2.60 | 2.99 | 2.96 | 2.78 | 3.13 | 3.04 | 2.86 | 3.21 | 2.80 | 2.69 | 2.91 | <0.001 | |
CI, confidence interval; HDHS, Haiti Demographic and Health Survey. † N for food groups analysis: 299 (6–8 months), 274 (9–11 months), 608 (12–17 months), 520 (18–23 months), 1701 (6–23 months). ‡ N for mean diet diversity score: 297 (6–8 months), 272 (9–11 months), 600 (12–17 months), 518 (18–23 months), 1686 (6–23 months).
Figure 1.
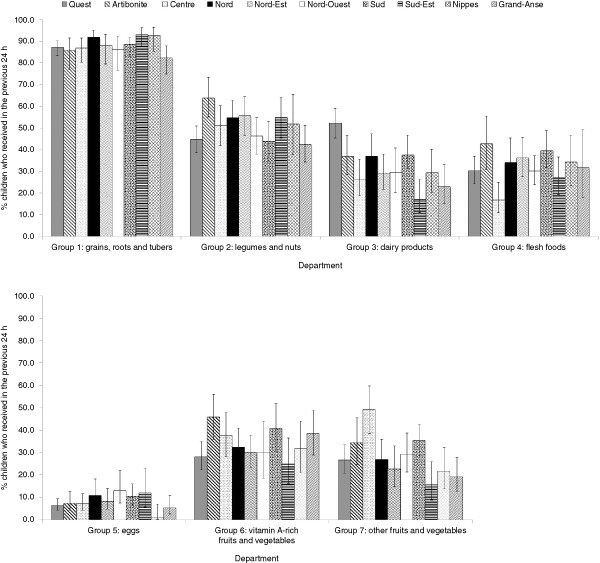
Proportion of children aged 6–23 months and living with mother who received specified food groups in the previous 24 h by department, Haiti Demographic and Health Survey 2005–2006.
In multivariate analysis, the most salient predictor of MDD was department (Table 5). Odds of achieving MDD in all nine departments were compared relative to Ouest, which includes metropolitan Port‐au‐Prince. Highest OR were in Centre (OR 8.54; P < 0.001), Sud (OR 4.72; P = 0.004), Artibonite (OR 3.77; P < 0.001) and Nord (OR 3.11; P = 0.001). Children in the youngest age group (6–8 months) were less likely to achieve MDD compared with children aged 18–23 months (OR 0.38; P = 0.007), which is consistent with 6–8 months being a transitional feeding time. Odds of achieving MDD increased with higher wealth quintile. Children with overweight mothers were more likely to achieve MDD compared with children of normal weight mothers (OR 2.08; P = 0.012). Unexpectedly, children of underweight mothers were also more likely to achieve MDD than normal weight mothers, but the OR was not statistically significant (OR 1.49; P = 0.24).
Table 5.
Determinants of minimum dietary diversity, minimum meal frequency and minimum acceptable diet among children aged 6–23 months who live with mother, HDHS 2005–2006
| Minimum dietary diversity (N = 774) | Minimum meal frequency (N = 745) | Minimum acceptable diet (N = 592) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | OR | 95% CI | P‐value | N | OR | 95% CI | P‐value | N | OR | 95% CI | P‐value | |||||
| Intercept | 0.087 | 0.55 | ||||||||||||||
| Residence | Urban | 278 | 0.71 | 0.40 | 1.26 | 0.24 | 256 | 0.95 | 0.52 | 1.74 | 0.87 | 197 | 0.64 | 0.31 | 1.32 | 0.23 |
| Rural | 496 | 490 | 396 | |||||||||||||
| Department | Nord‐Ouest | 46 | 2.88 | 1.16 | 7.18 | 0.023 | 45 | 0.66 | 0.33 | 1.34 | 0.25 | 35 | 1.84 | 0.51 | 6.62 | 0.35 |
| Nippes | 21 | 2.34 | 0.91 | 5.97 | 0.076 | 20 | 1.25 | 0.55 | 2.86 | 0.60 | 16 | 1.95 | 0.43 | 8.87 | 0.39 | |
| Sud‐Est | 44 | 1.55 | 0.65 | 3.71 | 0.33 | 42 | 0.82 | 0.29 | 2.34 | 0.71 | 34 | 0.44 | 0.03 | 5.76 | 0.53 | |
| Nord | 90 | 3.11 | 1.62 | 5.99 | 0.001 | 85 | 0.78 | 0.37 | 1.63 | 0.51 | 65 | 2.80 | 0.78 | 10.04 | 0.11 | |
| Nord‐Est | 31 | 2.16 | 1.02 | 4.55 | 0.044 | 30 | 0.68 | 0.30 | 1.53 | 0.35 | 26 | 1.15 | 0.27 | 4.86 | 0.84 | |
| Artibonite | 125 | 3.77 | 1.89 | 7.51 | <0.001 | 123 | 1.65 | 0.78 | 3.50 | 0.19 | 90 | 3.75 | 1.25 | 11.26 | 0.019 | |
| Centre | 80 | 8.54 | 4.02 | 18.13 | <0.001 | 84 | 2.40 | 1.14 | 5.07 | 0.022 | 65 | 11.60 | 3.54 | 38.00 | <0.001 | |
| Sud | 50 | 4.72 | 1.65 | 13.50 | 0.004 | 46 | 1.09 | 0.46 | 2.61 | 0.84 | 41 | 3.50 | 0.95 | 12.92 | 0.060 | |
| Grand‐Anse | 35 | 2.57 | 0.92 | 7.16 | 0.072 | 34 | 0.36 | 0.16 | 0.78 | 0.01 | 31 | 2.50 | 0.62 | 10.04 | 0.19 | |
| Ouest | 250 | 236 | 189 | |||||||||||||
| Sex | Female | 388 | 0.99 | 0.66 | 1.50 | 0.98 | 379 | 0.86 | 0.57 | 1.29 | 0.46 | 299 | 0.66 | 0.37 | 1.17 | 0.16 |
| Male | 385 | 366 | 293 | |||||||||||||
| Birth type | Multiple | 9 | 0.00 | 0.00 | 0.00 | <0.001 | 9 | 1.73 | 0.54 | 5.52 | 0.35 | 6 | 0.00 | 0.00 | 0.00 | <0.001 |
| Single | 765 | 736 | 586 | |||||||||||||
| Age group | 6–8 | 123 | 0.38 | 0.19 | 0.76 | 0.007 | 125 | 4.97 | 2.45 | 10.07 | <0.001 | 121 | 0.32 | 0.13 | 0.81 | 0.016 |
| 9–11 | 135 | 0.73 | 0.36 | 1.45 | 0.36 | 133 | 0.74 | 0.38 | 1.44 | 0.38 | 129 | 0.35 | 0.13 | 0.95 | 0.039 | |
| 12–17 | 305 | 0.79 | 0.47 | 1.35 | 0.40 | 293 | 0.87 | 0.50 | 1.52 | 0.63 | 241 | 0.41 | 0.19 | 0.88 | 0.023 | |
| 18–23 | 211 | 195 | 101 | |||||||||||||
| Wealth | Lowest | 123 | 0.22 | 0.08 | 0.61 | 0.004 | 172 | 0.31 | 0.13 | 0.74 | 0.008 | 140 | 0.25 | 0.06 | 1.06 | 0.061 |
| Second | 135 | 0.31 | 0.13 | 0.73 | 0.008 | 183 | 0.45 | 0.19 | 1.06 | 0.068 | 147 | 0.34 | 0.09 | 1.28 | 0.11 | |
| Middle | 305 | 0.53 | 0.23 | 1.21 | 0.13 | 124 | 0.61 | 0.28 | 1.33 | 0.22 | 99 | 0.90 | 0.29 | 2.76 | 0.86 | |
| Fourth | 211 | 0.80 | 0.41 | 1.56 | 0.50 | 157 | 0.44 | 0.22 | 0.89 | 0.022 | 123 | 0.64 | 0.25 | 1.66 | 0.36 | |
| Highest | 120 | 109 | 83 | |||||||||||||
| Mother's BMI | Underweight | 100 | 1.49 | 0.77 | 2.88 | 0.24 | 101 | 0.92 | 0.50 | 1.68 | 0.78 | 90 | 0.99 | 0.43 | 2.28 | 0.98 |
| Overweight | 136 | 2.08 | 1.18 | 3.66 | 0.012 | 127 | 1.81 | 1.07 | 3.04 | 0.026 | 104 | 2.40 | 1.23 | 4.69 | 0.010 | |
| Normal | 538 | 517 | 398 | |||||||||||||
| Mother's education | No school | 229 | 0.85 | 0.44 | 1.67 | 0.64 | 228 | 0.35 | 0.18 | 0.71 | 0.003 | 184 | 0.53 | 0.21 | 1.32 | 0.18 |
| Primary | 339 | 0.92 | 0.55 | 1.54 | 0.75 | 330 | 0.55 | 0.31 | 0.96 | 0.034 | 272 | 0.95 | 0.47 | 1.92 | 0.89 | |
| Secondary+ | 206 | 187 | 136 | |||||||||||||
| Mother currently working | Yes | 406 | 1.14 | 0.74 | 1.75 | 0.554 | 393 | 1.03 | 0.68 | 1.55 | 0.880 | 309 | 0.70 | 0.37 | 1.32 | 0.272 |
| No | 367 | 352 | 284 | |||||||||||||
| Child has health card | Yes | 666 | 1.20 | 0.68 | 2.11 | 0.528 | 640 | 1.06 | 0.57 | 1.98 | 0.857 | 501 | 1.83 | 0.73 | 4.55 | 0.195 |
| No | 108 | 105 | 91 | |||||||||||||
| Mother ANC visits | 4+ | 398 | 1.88 | 1.17 | 3.00 | 0.009 | 377 | 1.19 | 0.75 | 1.88 | 0.455 | 300 | 1.77 | 0.92 | 3.40 | 0.087 |
| 0–3 times | 375 | 369 | 292 | |||||||||||||
| Currently breastfeeding | Yes | 591 | 0.65 | 0.38 | 1.11 | 0.118 | 594 | 1.51 | 0.83 | 2.75 | 0.177 | 592 | ||||
| No | 182 | 151 | 0 | |||||||||||||
ANC, antenatal care; BMI, body mass index; CI, confidence interval; HDHS, Haiti Demographic and Health Survey; OR, odds ratio.
Minimum meal frequency
Overall, a larger proportion of children achieved MMF (45.3%) compared with MDD (29.2%). The proportion of children achieving MMF varied significantly by age (P < 0.001; Table 2) and department (P < 0.002; Table 3). Controlling for other variables in the model, the most salient determinant of achieving MMF was age. Children in the 6–8 months age group were much more likely to achieve MMF than older children (OR 4.97; P < 0.001) possibly because the threshold number of feeding episodes to achieve MMF among breastfed children is lower for this age group. Living in Centre (OR 2.40; P = 0.022) or Grand‐Anse (OR 0.36; P = 0.002) compared with Ouest was associated with MMF in opposing directions. Odds of achieving MMF increased with household wealth and maternal education. Children of overweight mothers were more likely to meet MMF (OR 1.81; P = 0.026; Table 5).
Minimum acceptable diet
MAD is a function of both MDD and MMF and so it is consistent that the overall proportion of breastfed children achieving this indicator (17.1%) is lower than for either of the contributing indicators. The proportion of children achieving MAD increased with age (P = 0.011) and varied by department (P = 0.003). Proportion was much higher in the Artibonite (28.9%) compared with other departments and lowest in the Sud‐Est (8.3%; Tables 2 and 3). As with MDD, both department and age were key determinants of MAD in multivariate analysis (Table 5). Children in Centre department had much higher odds of achieving MAD compared with Ouest (OR 11.6; P < 0.001), and odds were also significantly higher in the Artibonite but not to the same magnitude (OR 3.75; P = 0.019). Children in youngest age groups were almost 70% less likely to meet MAD than children in 18–23‐month age range (6–8 months OR 0.32, P = 0.016; 9–11 months OR 0.35, P = 0.039). Maternal BMI was also a statistically significant determinant after controlling for other variables in the model. Children with an overweight mother were more likely to meet the MAD indicator compared with children of mothers with a normal BMI (OR 2.4; P = 0.01).
Feeding indicators and growth
Table 6 presents a summary of multiple linear regression models testing the main and interaction effects of the three key IYCF indicators (MDD, MMF and MAD) and maternal education level on child anthropometry. Results show a statistically significant negative relationship between achieving MDD or MAD, and mean WAZ and HAZ indicators among children of mothers with secondary or more education.
Table 6.
Summary of results from multiple linear regression models between IYCF indicators, maternal education and mean anthropometric outcomes among children aged 6–23 months, HDHS 2005–2006
| Main effect for IYCF indicator § | Main effect for maternal education ¶ | Interaction (IYCF Indicator × Mat Ed) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | B | 95% CI | P‐value | B | 95% CI | P‐value | P‐value | |||
| WAZ | ||||||||||
| Minimum dietary diversity † | 753 | −0.397 | −0.752 | −0.043 | 0.028 | −0.478 | −0.806 | −0.151 | 0.004 | 0.012 |
| Minimum meal frequency † | 726 | 0.026 | −0.437 | 0.489 | 0.91 | −0.204 | −0.625 | 0.216 | 0.34 | 0.58 |
| Minimum acceptable diet ‡ | 578 | −0.624 | −1.274 | 0.027 | 0.06 | −0.351 | −0.683 | −0.018 | 0.039 | 0.058 |
| HAZ | ||||||||||
| Minimum dietary diversity † | 753 | −0.595 | −1.009 | −0.181 | 0.005 | −0.626 | −0.976 | −0.275 | 0.001 | 0.001 |
| Minimum meal frequency † | 726 | 0.352 | −0.103 | 0.807 | 0.13 | −0.027 | −0.422 | 0.368 | 0.89 | 0.047 |
| Minimum acceptable diet ‡ | 578 | −0.642 | −1.117 | −0.167 | 0.008 | −0.369 | −0.687 | −0.052 | 0.023 | 0.016 |
| WHZ | ||||||||||
| Minimum dietary diversity † | 753 | −0.126 | −0.565 | 0.313 | 0.57 | −0.221 | −0.57 | 0.128 | 0.21 | 0.55 |
| Minimum meal frequency † | 726 | −0.214 | −0.759 | 0.331 | 0.44 | −0.273 | −0.739 | 0.192 | 0.25 | 0.56 |
| Minimum acceptable diet ‡ | 578 | −0.408 | −1.316 | 0.501 | 0.38 | −0.224 | −0.616 | 0.169 | 0.26 | 0.30 |
HAZ, height‐for‐age z‐score; HDHS, Haiti Demographic and Health Survey; IYCF, improved infants and young child feeding; WAZ, weight‐for‐age z‐score; WHZ, weight‐for‐height z‐score. †Models also adjusted for child sex, age group, birth type, mother's body mass index (BMI), wealth, residence, department, mother's antenatal visit, current breastfeeding status. ‡Models also adjusted for child sex, age group, birth type, mother's BMI, wealth, residence, department, mother's antenatal visit. §Main effect B estimate is for children who achieved indicator relative to children who did not achieve indicator. ¶Main effect B estimate is for children of mothers with none or primary education compared with secondary or more education.
Discussion
CF practices were generally not adequate among Haitian children aged 6–23 months. While the proportion of Haitian children aged 6–8 months meeting the introduction of solid, semi‐solid or soft foods indicator was acceptable (>80%), the low EBF rate among 0–5‐month‐olds (41%) in Haiti suggests that many of these children may have received these foods before 6 months of age, which hinders EBF recommendations (Cayemittes et al. 2007; UNICEF et al. 2010). The proportion of children meeting MDD, MMF and MAD indicators in Haiti was consistent with reports from DHS analyses in low‐income countries in sub‐Saharan Africa and South Asia (Marriott et al. 2010; Disha et al. 2012; Senarath et al. 2012a). Less than one‐third of Haitian children aged 6–23 months met the MDD indicator compared with 7.1% in Ethiopia and 37.4% in Zambia (Disha et al. 2012). Among four South Asian countries, Senarath et al. (2012a) reported the range of 15.2% (in India) to 71.1% (in Sri Lanka) meeting MDD.
In our Haiti analysis, 45.3% of children met MMF indicator, a lower proportion than 4 of 6 South Asian countries (Marriott et al. 2010; Senarath et al. 2012a) and 8 of 10 sub‐Saharan African countries (Marriott et al. 2010; Disha et al. 2012). The proportion of children aged 6–23 months meeting MMF in these contexts ranged from 41.5% in India to 88.3% in Sri Lanka (Senarath et al. 2012a). In Haiti as well as the sub‐Saharan Africa and Asia analyses, the composite MAD indicator appears to be driven by the lower rates of MDD rather than MMF (Marriott et al. 2010; Disha et al. 2012; Senarath et al. 2012a).
Many of our findings related to predictors of MDD, MMF and MAD in Haiti including household wealth, maternal education, maternal BMI and access to ANC were consistent with previous reports from low‐income countries (Marriott et al. 2010; Disha et al. 2012; Senarath et al. 2012a). Therefore, we will focus our discussion on several findings that have important implications for policy and programmes in Haiti.
First, department was the most salient predictor of MDD in the multivariate analysis that underscores geographic disparities in food availability and IYCF practices and the need for geographically targeted interventions. Compared with Ouest, residence in any of the other nine departments was associated with higher odds of meeting MDD, although differences were not statistically significant for three departments (Nippes, Sud‐Est, Grand‐Anse). Ouest includes the Port‐au‐Prince metropolitan area that encompasses more than one‐third of Haiti's population. While urban populations have access to lower cost imported foods including rice, beans, maize and dairy (United States Agency for International Development 2012), they may have less access to flesh foods, eggs, fruits and vegetables produced in rural communities.
The higher odds of achieving MDD and MMF in Centre and Artibonite was unexpected given that these departments have the highest reported rates of underweight and stunting in the country (Cayemittes et al. 2007), and are classified as being the most vulnerable to food insecurity (United States Agency for International Development 2012). One plausible explanation is the presence of large‐scale IYCF education and food distribution programmes in those regions during the period of the DHS survey. The World Vision Haiti programme in Centre and parts of the Artibonite specifically promoted CF practices related to improved dietary diversity and frequency of feeding and provided household food rations to children in this age group. Effectiveness studies demonstrated the impact of this programme on feeding practices (Ruel et al. 2004, 2008).
Second, reported food group patterns may have implications for micronutrient status. Although readily available in Haiti, the consumption of vitamin A‐rich fruits and vegetables in general, and mangos and papayas in particular, was low across all age groups. Reports from field‐based programmes suggest that certain varieties of mangos and greens are not culturally regarded as high value and generally not consumed despite being freely available at little or no cost. Targeted promotion and social marketing efforts could potentially address some of these barriers.
Animal source foods also provide highly bioavailable forms of several key micronutrients. According to our analysis, almost one‐third of children aged 6–23 months consumed some form of flesh food in the previous 24 h. However, given that meat and seafood are frequently used in very small quantities to flavour Haitian stews and other mixed foods, it is difficult to assess the potential nutritional benefit of these foods without a measure of the quantity consumed. Egg consumption was rare across all age groups and departments. This may be attributable to their relatively high cost and a common belief in Haiti that eggs cause dental decay in young children (Loechl et al. 2005).
In the HDHS 2005–2006, consumption of nuts among 6–23‐month‐old children was rare. More recently, the use of peanut‐based foods for nutritional rehabilitation and preventative supplementation has been scaled up across the country (World Food Program 2010). Future dietary surveys will show whether this influx of peanut‐based products has influenced the overall intake patterns in this age group.
Third, overall, measures of dietary diversity (mean diversity score and MDD) increased with age, whereas the proportion of Haitian children reaching MMF varied with age. This pattern was also seen in South Asia and sub‐Saharan Africa (Marriott et al. 2010; Disha et al. 2012; Senarath et al. 2012a). While some of these differences may be a function of the indicator definition as described above, they underscore the importance of targeting age‐specific messages to introduce a greater variety of foods to younger children and focus on increasing frequency of feeding with older children.
Finally, the finding that meeting MDD and MAD was associated with lower mean HAZ and WHZ among children with mothers with secondary or more education was unexpected, and the magnitude of the effect was large. Other studies using MDD and MAD (Marriott et al. 2012), as well as other dietary diversity measure, (Ruel & Menon 2002) indicators, have found a positive growth association only among higher educated women. It is not clear why meeting the MDD and MAD criteria is associated with poorer growth outcomes among Haitian children with more educated mothers and it warrants further investigation.
Primary limitations of this study are the cross‐sectional survey design and use of 24‐h recalls data to assess feeding practices. The recall approach is subject to respondent bias. Multiple testing may have increased the likelihood of a type 1 error. Also, we were limited in the application of the indicators among non‐breastfed children who are disproportionally represented in older age groups. Furthermore, it is important to point out that we excluded observations with missing data from our regression analyses. BMI data were available for less than half of all women aged 15–49 years in the HDHS (Cayemittes et al. 2007) and, in turn, limited the total number of observations included in the regression analyses. Some caution should be exercised in interpreting regression results.
Source of funding
The financial support for the study was provided by UNICEF Haiti under the agreement SSA/HTIA/2011/000026830‐0. The views expressed in this publication do not necessarily reflect those of the UNICEF.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
RH designed the study, conducted the analysis, obtained the literature, interpreted the results and wrote the manuscript. INT, MAA, JPM and RJS generated the concept of the study, and reviewed and revised the manuscript.
Acknowledgements
The authors would like to thank Jing Yang of the Cornell Statistical Consulting Unit for assistance with preparing the data sets and creating variables. We also thank Laura Santacrosse for her assistance in identifying supporting literature.
Heidkamp, R. A. , Ayoya, M. A. , Teta, I. N. , Stoltzfus, R. J. , and Marhone, J. P. (2015) Complementary feeding practices and child growth outcomes in Haiti: an analysis of data from Demographic and Health Surveys. Matern Child Nutr, 11: 815–828. doi: 10.1111/mcn.12090.
References
- Adair L.S. (2007) Size at birth and growth trajectories to young adulthood. American Journal of Human Biology 19, 327–337. [DOI] [PubMed] [Google Scholar]
- Agho K.E., Dibley M.J., Odiase J.I. & Ogbonmwan S.M. (2011) Determinants of exclusive breastfeeding in Nigeria. BMC Pregnancy Childbirth 11, 2 Available at: http://www.biomedcentral.com/content/pdf/1471-2393-11-2.pdf (Accessed 25 February 2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhutta Z.A., Ahmed T., Black R.E., Cousens S., Dewey K., Giugliani E. et al (2008) What works? Interventions for maternal and child undernutrition and survival. Lancet 371, 417–440. [DOI] [PubMed] [Google Scholar]
- Cayemittes M., Placide M.F., Mariko S., Barrere B., Severe B. & Alexandre C. (2007) Enquête mortalité, morbidité et utilisation des services (EMMUS‐IV): Haïti, 2005–2006. Ministere de la Sante Publique et de la Population, Institut Haïtien de l'Enfance, Macro International: Calverton, MD.
- Daelmans B., Dewey K. & Arimond M. (2009) New and updated indicators for assessing infant and young child feeding. Food and Nutrition Bulletin 30, S256–S262. [DOI] [PubMed] [Google Scholar]
- Dewey K. (2003) Guiding Principles for Complementary Feeding of the Breastfed Child. Pan American Health Organization: Washington, DC. [Google Scholar]
- Disha A., Rawat R., Subandoro A. & Menon P. (2012) Infant and young child feeding (IYCF) practices in Ethiopia and Zambia and their association with child nutrition: analysis of Demographic and Health Survey data. African Journal of Food, Agriculture, Nutrition and Development 12 Available at: http://www.ajfand.net/Volume12/No2/Disha11320.pdf (Accessed 25 February 2013). [Google Scholar]
- Hazir T., Senarath U., Agho K., Akram D.S., Kazmi N., Abbasi S. et al (2012) Determinants of inappropriate timing of introducing solid, semi‐solid or soft food to infants in Pakistan: secondary data analysis of Demographic and Health Survey 2006–2007. Maternal & Child Nutrition 8 (Suppl. 1), 78–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi N., Agho K.E., Dibley M.J., Senarath U. & Tiwari K. (2012) Determinants of inappropriate complementary feeding practices in young children in Nepal: secondary data analysis of Demographic and Health Survey 2006. Maternal & Child Nutrition 8 (Suppl. 1), 45–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loechl C., Menon P., Ruel M.T., & Pelto G. (2005) A Qualitative Study of the Patterns of Infant Feeding and Care in the Hinche Area of Plateau Central, Haiti. A report submitted to the Food and Nutrition Technical Assistance Project, Academy for Educational Development, Washington, DC.
- Lutter C.K. & Chaparro C.M. (2008) Malnutrition in Infants and Young Children in Latin America and the Caribbean: Achieving the Millennium Development Goals. Pan American Health Organization: Washington, DC. [Google Scholar]
- Marriott B.P., White A.J., Hadden L., Davies J.C. & Wallingford J.C. (2010) How well are infant and young child World Health Organization (WHO) feeding indicators associated with growth outcomes? An example from Cambodia. Maternal & Child Nutrition 6, 358–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marriott B.P., White A., Hadden L., Davies J.C. & Wallingford J.C. (2012) World Health Organization (WHO) infant and young child feeding indicators: associations with growth measures in 14 low‐income countries. Maternal & Child Nutrition 8, 354–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon P., Ruel M.T., Loechl C. & Pelto G. (2005) From research to program design: use of formative research in Haiti to develop a behavior change communication program to prevent malnutrition. Food and Nutrition Bulletin 26, 241–242. [DOI] [PubMed] [Google Scholar]
- Ministère de la Santé Publique et de la Population Unité de Coordination du Programme National d'Alimentation et de Nutrition (2012) Politique Nationale de Nutrition. Ministère de la Santé Publique et de la Population: Port‐au‐Prince, Haiti. [Google Scholar]
- Ruel M.T. & Menon P. (2002) Child feeding practices are associated with child nutritional status in Latin America:innovative uses of the demographic and health surveys. The Journal of Nutrition 132, 1180–1187. [DOI] [PubMed] [Google Scholar]
- Ruel M.T., Menon P., Loechl C. & Pelto G. (2004) Donated fortified cereal blends improve the nutrient density of traditional complementary foods in Haiti, but iron and zinc gaps remain for infants. Food and Nutrition Bulletin 25, 361–376. [DOI] [PubMed] [Google Scholar]
- Ruel M.T., Menon P., Habicht J.P., Loechl C., Bergeron G., Pelto G. et al (2008) Age‐based preventive targeting of food assistance and behaviour change and communication for reduction of childhood undernutrition in Haiti: a cluster randomised trial. Lancet 371, 588–595. [DOI] [PubMed] [Google Scholar]
- Rutstein S.O., Johnson K. & ORC Macro, MEASURE/DHS+ (PROGRAMME) (2004) The DHS wealth index. ORC Macro, MEASURE DHS+: Calverton, MD.
- Senarath U. & Dibley M.J. (2012) Complementary feeding practices in South Asia: analyses of recent national survey data by the South Asia Infant Feeding Research Network. Maternal & Child Nutrition 8 (Suppl. 1), 5–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senarath U., Agho K.E., Akram D.E., Godakandage S.S., Hazir T., Jayawickrama H. et al (2012a) Comparisons of complementary feeding indicators and associated factors in children aged 6–23 months across five South Asian countries. Maternal & Child Nutrition 8 (Suppl. 1), 89–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senarath U., Siriwardena I., Godakandage S.S., Jayawickrama H., Fernando D.N. & Dibley M.J. (2012b) Determinants of breastfeeding practices: an analysis of the Sri Lanka Demographic and Health Survey 2006–2007. Maternal & Child Nutrition 8, 315–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah P.S. & Ohlsson A. (2009) Effects of prenatal multimicronutrient supplementation on pregnancy outcomes: a meta‐analysis. Canadian Medical Association Journal 180, E99–E108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF, WHO, UNESCO, UNFPA, UNDP, UNAIDS, WFP & World Bank (2010) Facts for Life, 4th edn UNICEF: New York. [Google Scholar]
- United States Agency for International Development (2012) Famine Early Warning System Network Haiti Price Bulletin: July 2012.
- Vieira T.O., Vieira G.O., Giugliani E.R., Mendes C.M., Martins C.C. & Silva L.R. (2010) Determinants of breastfeeding initiation within the first hour of life in a Brazilian population: cross‐sectional study. BMC Public Health 10, 760 Available at: http://www.biomedcentral.com/content/pdf/1471-2458-10-760.pdf (Accessed 25 February 2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Multicentre Growth Reference Study Group (2006) WHO Child Growth Standards: Length/Height‐for‐Age, Weight‐for‐Age, Weight‐for‐Length, Weight‐for‐Height and Body Mass Index‐for‐Age: Methods and Development. WHO: Geneva. [Google Scholar]
- World Bank (2010) Promoting Nutrition Security in Haiti: An Assessment of Pre‐ and Post‐Earthquake Conditions and Recommendations for the Way Forward. World Bank: Washington, DC. [Google Scholar]
- World Food Program (2010) The Right Nutrition – A Key Priority After Haiti Earthquake Available at: http://www.wfp.org/aid-professionals/blog/right-nutrition-key-priority-after-earthquake-haiti (Accessed 25 February 2013).
- World Health Organization (2002) WHO Antenatal Care Randomized Trial: Manual For The Implementation Of The New Model. WHO: Geneva. [Google Scholar]
- World Health Organization (2005) Guiding Principles for Feeding Non‐Breastfed Children 6–24 Months of Age. World Health Organization: Geneva. [Google Scholar]
- World Health Organization (2010) Indicators for Assessing Infant and Young Child Feeding Practices Part 2: Measurement. World Health Organization: Geneva. [Google Scholar]
- Zongrone A., Winskell K. & Menon P. (2012) Infant and young child feeding practices and child undernutrition in Bangladesh: insights from nationally representative data. Public Health Nutrition 15, 1697–1704. [DOI] [PubMed] [Google Scholar]


