Abstract
The objective of this study was to assess the degree of concordance between two popular classification systems [the Centers for Disease Control and Prevention (CDC)‐2000 and the Institute of Medicine (IOM)‐2009] used to categorise the nutritional status of pregnant adolescents. This cross‐sectional study involved 327 pregnant adolescents (10–19 years) booking for antenatal care at a single public maternity in São Paulo, Brazil. Participants were classified into one of four categories, by both systems according to their pre‐pregnancy body mass index and age. The CDC‐2000 system classified significantly fewer pregnant adolescents as underweight (3.7% vs. 12.5%, P < 0.0001) and significantly more adolescents as normal‐weight (86.8% vs. 75.6%, P = 0.0003) than the IOM‐2009 system. The distribution of the adolescents in the two systems differed significantly. The global rate of discordance was 13.5%. The overall concordance between the two systems was marginally good (K = 0.63), being moderate for younger (<16 years) adolescents (K = 0.52). Approximately one in every seven pregnant adolescent would be classified in a non‐corresponding category if the IOM‐2009 classification was used instead of the CDC‐2000 classification. The IOM‐2009 nutritional classification, which does not take into account age and gender, tends to overestimate the proportion of underweight adolescents, especially in the younger‐age group. The use of this classification system can lead to recommendations of higher gestational weight gain in a substantial proportion of pregnant adolescents, which could predispose to post‐partum weight retention and future obesity.
Keywords: nutrition assessment, pregnancy in adolescence, classification, body mass index, ideal body weight, prenatal nutritional physiological phenomena
Introduction
Maternal nutritional status is a key factor for a healthy pregnancy. Women who enter pregnancy with excess adiposity or underweight are at higher risk than normal‐weight women for several complications such as pre‐eclampsia, gestational diabetes, preterm birth and having a macrosomic or low‐birthweight infant (O'Brien et al. 2003; Torloni et al. 2009a,b; McDonald et al. 2010). Similarly, both excessive and insufficient gestational weight gain (GWG) are also associated with adverse pregnancy outcomes and are important determinants of birthweight (Abrams et al. 2000; Abrams & Laros 1986; Crane et al. 2009; Edwards et al. 1996; Rode et al. 2007).
Based on the premise that fetal growth is determined by a woman's initial body mass index (BMI, kg m−2) as well as her GWG, in 1990 the Institute of Medicine (IOM) issued specific recommendations for assessment of the nutritional status of pregnant women and appropriate weight gain during pregnancy (Institute of Medicine 1990). These original IOM guidelines recommended specific weekly and total GWG, based on the classification of women at the beginning of pregnancy into one of four BMI categories: low (<19.8 kg m−2), average (19.8–26.0 kg m−2), high (26.1–29.0 kg m−2) and obese (>29.0 kg m−2). In 2009, the IOM revised these guidelines (Institute of Medicine 2009) and adopted the BMI cut‐offs proposed by the World Health Organization (WHO), which are widely used worldwide: <18.5, 18.5–24.9, 25–29.9 and ≥30 kg m−2 (Table 1) (World Health Organization 1998). However, the adequacy of this classification for pregnant adolescents has been questioned. Despite acknowledging that its guidelines were developed for adults, the IOM states that pregnant adolescents should be classified and follow the same GWG recommendations as adult women. Those contrary to the use of IOM guidelines for adolescent pregnancies argue that there are the large differences in percentage of body fat in the same BMI category, depending on the adolescent's age and degree of sexual maturity (Daniels et al. 1997). On the other hand, a single BMI categorisation system to classify all pregnant women, regardless of their age, aggregates simplicity and ease of use, which are important factors in the implementation of any guideline (Francke et al. 2008).
Table 1.
Terms, definitions and equivalence of the categories proposed by the CDC‐2000, IOM‐1990 and IOM‐2009 for pre‐pregnancy nutritional assessment
| Categories | CDC‐2000 (percentile*) | IOM‐1990 (BMI, kg m−2) | IOM‐2009 (BMI, kg m−2) |
|---|---|---|---|
| 1 | Underweight (<5th) | Low (<19.8) | Underweight (<18.5) |
| 2 | Healthy‐weight (5th–<85th) | Average (19.8–26.0) | Normal (18.5–24.9) |
| 3 | Overweight (85th–<95th) | High (>26.0–29.0) | Overweight (25–29.0) |
| 4 | Obese (≥95th) | Obese (>29.0) | Obese (≥30) |
BMI, body mass index; CDC, Centers for Disease Control and Prevention; IOM, Institute of Medicine.*Percentile: age and gender specific BMI growth curves percentiles for children and adolescents from 2 to 20 years.
Ever since 2000, the Centers for Disease Control and Prevention (CDC) recommends that BMI categorisation of individuals between 2 and 20 years of age should be based on a series of percentile curves especially developed for their age and gender (Table 1) (Centers for Disease Control and Prevention 2000). Previous studies have compared the categorisation and GWG recommendations for pregnant adolescents classified according to the IOM‐1990 and CDC‐2000 guidelines and reported that the former tended to increase the prevalence of underweight adolescents, when compared with the CDC‐2000 system (Groth 2007; Fernandez et al. 2008). Therefore, adolescents of the same height and weight at the beginning of pregnancy would be classified in non‐corresponding categories and receive different GWG recommendations, depending on whether the IOM‐1990 or CDC‐2000 guideline is adopted.
As previously mentioned, the IOM modified its BMI cut‐offs in 2009. However, to the best of our knowledge, there have been no previous publications specifically designed to compare the degree of concordance between the two systems (CDC‐2000 vs. IOM‐2009) in the classification of the nutritional status of pregnant adolescents. If there is a good degree of agreement between the new IOM‐2009 and CDC‐2000 guidelines, then GWG recommendations would be similar and either system could be used, depending on the preferences of the health professionals caring for the pregnant adolescent.
The controversies and paucity of studies surrounding this important topic motivated us to perform this study. Our main objective was to assess the degree of concordance between the CDC‐2000 and the new IOM‐2009 guidelines to categorise the nutritional status of pregnant adolescents.
Key messages
The overall concordance between the two nutritional classification systems was marginally good.
The Institute of Medicine (IOM)‐2009 classification, which does not take into account age and gender, tends to overestimate the proportion of underweight adolescents, especially among younger girls.
The use of the IOM‐2009 system would lead to inappropriate gestational weight gain (GWG) recommendations in approximately one in every seven pregnant adolescents, most of which would be counselled to gain more weight.
The use of the IOM‐2009 classification will lead to recommendations of higher GWG in pregnant adolescents, potentially increasing the risks of post‐partum weight retention and future obesity.
Material and methods
This cross‐sectional study analysed the records of all adolescents (10–19 years) booked for antenatal care at a single institution, the Amparo Maternal Maternity, located in São Paulo, Brazil, between January 2005 and December 2009. This free, public, catholic maternity serves a low‐income population in the southern part of the largest city of Brazil. Antenatal care at Amparo is provided by a team of obstetricians and nurses. At the time of the study, initial maternal BMI was routinely calculated and recorded at the first antenatal care visit of all patients, based on their measured height and self‐reported usual pre‐pregnancy weight. At each subsequent visit, all patients were weighed and counselled about appropriate GWG according to their specific initial BMI category, based on the recommendations of the IOM‐1990 guidelines, which were in use at the time of the study.
The records of all nulliparae 10–19 years of age booking for antenatal care with a live singleton pregnancy during the study period were eligible for inclusion. Records with illegible or missing essential information (age, pre‐pregnancy weight or measured height) were excluded. All included adolescents were classified by the investigators according to their initial BMI into one of four categories, according to the IOM‐2009 recommendations (Institute of Medicine 2009) (Table 1). Based on their age, measured height and pre‐pregnancy weight, each adolescent was also categorised by the investigators into one of four nutritional classes based on the CDC‐2000 growth curves (Centers for Disease Control and Prevention 2000) (Table 1).
We present the distribution of the adolescents in the four categories of each classification as percentages and 95% confidence interval (CI) and the proportion of discordance between the two nutritional assessment systems. In this study, ‘discordance’ was defined as the inclusion of the same adolescent in two non‐equivalent categories by the two classification systems, while ‘agreement’ was defined as the inclusion of the same adolescent in equivalent categories by the two systems. For example, if an adolescent's characteristics (age, height and pre‐pregnancy weight) led us to classify her in CDC‐2000 category 2 (healthy‐weight) and in category 1 of the IOM‐2009 system (underweight), this would be a case of discordance. We calculated the percentage of discordance comparing the proportion of adolescents included in each CDC‐2000 category with the proportion of adolescents included in the equivalent IOM‐2009 category. A subgroup analysis was performed to assess the percentage of discordance in younger (<16 years) and older (16–19 years) adolescents.
To get an estimate, with a 95% CI and a sample error of 5%, the calculated sample size was 246 individuals. The chi‐squared and Fisher's exact tests were used to compare categorical variables. Kappa coefficients were used to analyse the agreement between the two nutritional classification systems. Concordance was graded as excellent (0.81–1.00), good (0.61–0.80), moderate (0.41–0.60), low (0.21–0.40) and poor (<0.20) following the recommendations of Altman for Kappa coefficients (Altman 1991). Bowker's symmetry test (Bowker 1948), a generalisation of the McNemar's test for analyses of categorical variables with three or more classes, was also used to compare concordance of the two classifications. Significance was established at P < 0.05. The software Statistical Analysis System version 8.02 (SAS Institute Inc., Cary, NC, USA) was used for statistical analyses.
The study was approved by the Institutional Review Boards of São Paulo Federal University and Amparo Maternal Maternity. All patients booking for antenatal care gave written informed consent authorising use of their data for this study.
Results
During the study period, 575 adolescents booked for antenatal care, 446 of which were nulliparae. A total of 119 did not fulfil the selection criteria and were excluded, 327 were included in the final analyses. The main reasons for the 119 exclusions were lack or illegible information on pre‐pregnancy weight (63) or height (57) or exact age (21); several records lacked two or more of these data. The other main characteristics of the excluded adolescents did not differ significantly from the included participants, presented on Table 2.
Table 2.
Characteristics of 327 adolescents booked for antenatal care at Amparo Maternal Maternity, São Paulo (2005–2009)
| Characteristic | Value |
|---|---|
| Age, years | |
| Range | 12–19 |
| Mean (SD) | 17.3 (1.5) |
| <16 | 47 (14.4) |
| Currently in school | 87 (26.6) |
| <8 years education | 198 (60.7) |
| Currently employed | 77 (23.6) |
| Age at menarche, years | |
| Range | 7–17 |
| Mean (SD) | 12.1 (1.6) |
| Age at first sexual intercourse, years | |
| Range | 9–19 |
| Mean (SD) | 15.0 (1.7) |
SD, standard deviation. All values expressed as N (%) unless otherwise stated.
The proportion of adolescents classified as low‐weight (category 1) was significantly lower when the CDC‐2000 system was used: 3.7% (95% CI 1.9–6.3) vs. 12.5% (95% CI 9.2–16.6), P < 0.0001 (Fig. 1). Most of the adolescents were classified as average‐weight (category 2), regardless of the system used. However, the proportion of participants in this category was significantly higher when the CDC‐2000 was used: 86.8% (95% CI 82.7–90.3) vs. 75.6% (95% CI 70.5–80.1), P = 0.0003. The proportion of overweight adolescents (category 3) was similar in both systems: 8.6% (95% CI 5.8–12.2) vs. 10.7% (95% CI 7.6–14.6) for CDC‐2000 and IOM‐2009, respectively, P = 0.427. Finally, the proportion of adolescents classified as obese (category 4) was very low and did not differ significantly between the two systems (0.9%, 95% CI 0.2–2.9 and 1.2%, 95% CI 0.4–3.3, for CDC‐2000 and IOM‐2009, respectively, P = 0.99). Figure 2 presents the distribution the 327 adolescents according to their age and pre‐pregnancy BMI categorisation using the two different systems. The proportion of the 280 older adolescents (16–19 years) categorised as underweight was approximately three times lower when the CDC classification was used instead of the IOM‐2009 classification: 3.9% (95% CI 2.0–6.9) vs. 12.1% (95% CI 8.6–16.6), respectively, P = 0.0005 (Table 3). A significantly higher proportion of the older adolescents was categorised as normal‐weight when the CDC‐2000 system was used than when the IOM‐2009 system was used: 87.5% (95% CI 83.1–91.2) vs. 75.4% (95% CI 69.8–80.3), CDC vs. IOM, respectively, P = 0.0003. The proportion of older adolescents in the overweight and obese categories was similar in the two systems: 11.1% (95% CI 7.8–15.5) vs. 7.5% (95% CI 4.8–11.4) (P = 0.190) in the IOM‐2009 and CDC‐2000 systems category 3, and 1.4% (95% CI 0.5–3.9) vs. 1.1% (95% CI 0.3–3.4) in the IOM‐2009 and CDC‐2000 systems category 4 (P = 1.00).
Figure 1.
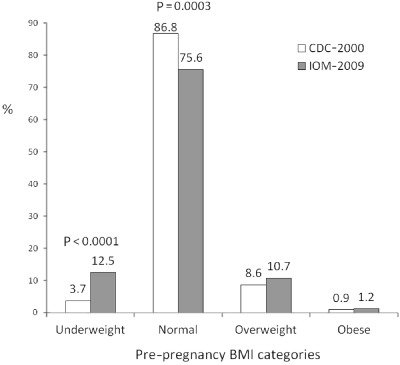
Classification of the nutritional status of 327 adolescents according to the CDC‐2000 and IOM‐2009 systems. IOM categories: 1, underweight: <18.5 kg m−2; 2, normal: 18.5–24.9 kg m−2; 3, overweight: 25.0–29.9 kg m−2; 4, obese: ≥30 kg m−2. CDC categories: 1, underweight: BMI <5th percentile for gender and age; 2, healthy‐weight (normal): BMI 5th–<85th percentile; 3, at‐risk for overweight (overweight) 85th–<95th percentile; 4, overweight (obese) ≥95th percentile for gender and age. Bowker's symmetry test P < 0.001, overall K = 0.632. BMI, body mass index; CDC, Centers for Disease Control and Prevention; IOM, Institute of Medicine.
Figure 2.
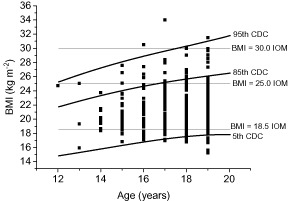
Distribution of 327 adolescents, according to age and pre‐pregnancy body mass index, using the Centers for Disease Control and Prevention (CDC)‐2000 and Institute of Medicine (IOM)‐2009 classification systems.
Table 3.
Classification of 327 pregnant adolescents according to two nutritional assessment systems
| Classifications | Adolescents | |||
|---|---|---|---|---|
| CDC‐2000* | IOM‐2009 † | All | <16 years | 16–19 years |
| (n = 327) | (n = 47) | (n = 280) | ||
| N (%) ‡ | N (%) ‡ | N (%) ‡ | ||
| Underweight (n = 12) | Underweight (C) | 12 (100.0) | 1 (100.0) | 11 (100.0) |
| Normal (I) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Overweight (I) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Obese (I) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Healthy‐weight (n = 284) | Underweight (I) | 29 (10.2) | 6 (15.4) | 23 (9.4) |
| Normal (C) | 244 (85.9) | 33 (84.6) | 211 (86.1) | |
| Overweight (I) | 11 (3.9) | 0 (0.0) | 11 (4.5) | |
| Obese (I) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Overweight (n = 28) | Underweight (I) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Normal (I) | 3 (10.7) | 3 (42.9) | 0 (0.0) | |
| Overweight (C) | 24 (85.7) | 4 (57.1) | 20 (95.2) | |
| Obese (I) | 1 (3.6) | 0 (0.0) | 1 (4.8) | |
| Obese (n = 3) | Underweight (I) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Normal (I) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Overweight (I) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Obese (C) | 3 (100.0) | 0 (0.0) | 3 (100.0) | |
| P values | <0.001 § | 0.046 ¶ | <0.001** | |
C, concordant: adolescents classified in equivalent categories by both systems (CDC‐2000 and IOM‐2009); I, incorrect: adolescents classified in different categories by each system. CDC, Centers for Disease Control and Prevention; CI, confidence interval; IOM, Institute of Medicine. *CDC: underweight: <5th percentile; normal: ≥5th percentile and <85th percentile; excess weight: ≥85th percentile and <95th percentile; obese: ≥95th percentile for maternal age. †IOM (kg m−2): underweight: <18.5; normal: 18.5–24.9; overweight: 25.0–29.9; obese: ≥30. ‡Percents calculated over the total of that column. §Symmetry test: P < 0.001 – K: 0.632; 95% CI: 0.532–0.732. ¶Symmetry test: P = 0.046 – K: 0.520; 95% CI: 0.247–0.792. **Symmetry test: P < 0.001 – K: 0.651; 95% CI: 0.545–0.757.
The BMI distribution of the 47 younger adolescents (<16 years) followed a similar pattern. The proportion of younger adolescents classified as underweight was almost seven times higher when the IOM‐2009 instead of the CDC‐2000 system was used (14.9%, 95% CI 6.7–28.9 vs. 2.1%, 95% CI 0.1–12.7, respectively, P = 0.059). There was a higher prevalence of young normal‐weight participants when the CDC‐2000 classification was used (83.0%, 95% CI 69.2–92.4) than when the IOM‐2009 system was used (76.6%, 95% CI 62.0–87.7) although this difference was not statistically significant (P = 0.608). The proportion of younger adolescents categorised as overweight was two times higher when the CDC system was used, although this difference was not significant (14.9%, 95% CI 6.7–28.9 vs. 8.5%,95% CI 2.8–21.3 for CDC and IOM, respectively, P = 0.523). None of the younger adolescents was classified in the highest BMI category (Table 3).
The global rate of discordance between the two classification systems was 13.5% (95% CI 9.9–17.6), which means that 44 of the 327 adolescents would be classified in non‐equivalent BMI categories in the two systems. Almost all of these cases (40/44) occurred in the normal‐weight CDC‐2000 system: 10.2% (n = 29) of the 284 adolescents classified as normal‐weight by the CDC would be considered underweight by the IOM‐2009 system and another 3.9% (n = 11) would be classified as pre‐obese by the IOM‐2009 (Table 3). The other four cases of discordance occurred in the third CDC category: out of the 28 adolescents classified as overweight by this system, three (10.7%) would be classified as normal‐weight and one (3.0%) as obese by the IOM‐2009 system. There was 100% agreement between the two systems in the classification of adolescents in the first (underweight) and last (obese) categories, using the CDC‐2000 as reference. However, these two categories together represented only 5% of the total number of adolescents enrolled in this study.
According to the Kappa test, the overall concordance between the two nutritional assessment systems was marginally good (K = 0.63, 95% CI 0.53–0.73), being moderate for the younger adolescents (K = 0.52, 95% CI 0.25–0.79). There was a higher global rate of discordance in the younger adolescents than in the older adolescents: 19.2% (95% CI 9.1–33.3) vs. 12.5% (95% CI 8.8–16.9), P = 0.246. According to the symmetry test, the proportions obtained by the two systems differed significantly (P < 0.001), indicating that the IOM‐2009 classification tended to overestimate the proportion of underweight adolescents (Table 3), a tendency observed for younger as well as older adolescents.
Discussion
The global rate of discordance between the two nutritional classification systems (IOM‐2009 and CDC‐2000) was 13.5% (ranging from 10% to 18%) in this group of Brazilian primiparous adolescents. The rate of discordance was somewhat higher in younger than in older adolescents (19.2% vs. 12.5%). Despite the marginally good overall rate of agreement between the two systems (K = 0.63), the symmetry test detected significant differences in the distribution of the adolescents in the two systems. Compared with the CDC‐2000 BMI‐for‐age system, the IOM‐2009 nutritional classification tended to overestimate the proportion of underweight adolescents, regardless of their age group.
Using the CDC‐2000 system as reference, there was an excellent degree of concordance (almost 100%) between the two systems in the classification of adolescents in the two extremes of the nutritional classification (categories 1 and 4, i.e. underweight and obese). However, the vast majority (95.4%) of our sample fell into the middle categories (normal or overweight). Therefore, the clinical significance of this concordance is questionable as these extreme categories represent such a small part of the total sample.
Based on our results, the use of the IOM‐2009 system would lead to inappropriate GWG recommendations in approximately one in every seven pregnant adolescents (13.4%), most of which would be counselled to gain more weight than recommended during pregnancy. For example, 10.2% of the healthy‐weight adolescents (according to the CDC‐2000 system) and 10.7% of those at risk of overweight would be encouraged to gain more weight during pregnancy if the IOM‐2009 system was used, because they would be classified as underweight or normal‐weight, respectively, by this second system (Institute of Medicine 2009). The benefits of high GWG in adolescents are questionable and previous studies suggest that rapid weight gain during pregnancy is one of the main contributing factors to post‐partum weight retention (Stevens‐Simon et al. 1992; Scholl & Hediger 1995).
Extrapolating our findings to larger populations, the use of the IOM‐2009 system to classify the nutritional status of adolescents booking for antenatal care would lead to misclassification of a large number of normal‐weight adolescents as being underweight, especially in the youngest age groups. Consequently, if the IOM‐2009 system was used, many more adolescents would be encouraged to increase their GWG, which could expose them to risks for adverse maternal and perinatal outcomes associated with excessive GWG, as well as increase their post‐partum weight retention and consequently increase their probability of developing obesity and its long‐term consequences (Mamun et al. 2010). As BMI programming seems to take place during the growth phase of an individual, the prevention of overweight during adolescence is considered one of the best ways to reduce morbidity and mortality of adults (Must et al. 1992). Therefore, misclassification of the nutritional status of pregnant adolescents and ensuing excessive GWG could, in theory, have serious long‐term public health implications.
To the best of our knowledge, this is the first study to compare the revised IOM‐2009 nutritional classification system based on the WHO classification and the CDC‐2000 system for assessment of pregnant adolescents. In 2008, Fernandez et al. used a large database of deliveries in New York (1999–2000) and reported that approximately one in every four adolescent would be classified in a non‐corresponding category if the IOM‐1990 classification, the recommended system at the time, was used instead of the CDC‐2000 classification. More specifically, if the IOM‐1990 system was used, 20.7% of all adolescents in that study would be labelled as underweight, compared with only 4.7% if the CDC‐2000 system was used (Fernandez et al. 2008). Similarly, Groth compared the distribution of 347 African American pregnant American adolescents and reported that the percentage of teenagers classified as underweight was significantly higher when the IOM‐1990 instead of the CDC‐2000 was used (28% vs. 2%, P < 0.001) (Groth 2007). However, both of these studies were referring to the IOM‐1990 categories and therefore cannot be compared with our data.
Our finding of a somewhat better degree of agreement between the two systems may in part be explained by the change in the BMI cut‐offs proposed by the IOM‐2009 revision. By lowering the cut‐off for the lowest category from 19.8 to 18.5, the new IOM‐2009 recommendations reduced the number of adolescents (and adult women) classified as underweight, when compared with the 1990 recommendations. Despite this improvement, our findings indicate that the IOM‐2009 system continues to overestimate the proportion of underweight adolescents in comparison with the CDC‐2000 system, which uses different BMI cut‐offs calculated according to gender and age.
In a recent publication, which aimed to assess the GWG distributions of healthy adolescents with optimal birth outcomes compared with the current IOM‐2009 recommendations, Fernandez et al. used both systems to classify their population, in order to avoid possible misclassification. Although the focus of their study was not the concordance of the two classifications, they mention that if they had used the IOM‐2009 classification, 7.2% of their healthy‐weight adolescents would have been misclassified as underweight and 5.8% as overweight (Fernandez et al. 2011).
A limitation of this study was the small number of younger adolescents, which reduced the power to detect differences between the two systems in this age group. Another potential weakness was the use of self‐reported maternal weight for pre‐pregnancy BMI calculations. Although women tend to be imprecise when reporting their usual weight, mean variations between self‐reported and measured values are small (Engstrom et al. 2003) and may be influenced by biotype (Brunner‐Huber 2007) and ethnicity (Gillum & Sempos 2005). The original 1990 GWG ranges recommended by the IOM guidelines were drawn from a US sample based on self‐reported weight. The validity of self‐reported weight has been extensively studied in different countries, including Brazil. The existing evidence indicates that it is an appropriate method to obtain BMI estimations in this specific population (Stewart 1982; Schmidt et al. 1993; Fonseca et al. 2004). The alternative to using self‐reported data would be to calculate initial maternal BMI using weight measured at the first antenatal care visit. However, this option does not ensure accuracy especially when the first visit does not occur in the first weeks of pregnancy, a common situation especially among adolescents of low socio‐economic status.
Our results show that, compared with the CDC‐2000 nutritional classification system (which takes into account maternal age and sexual maturity), the new BMI categories proposed by the IOM‐2009 revision continue to overestimate the proportion of underweight adolescents especially in the younger‐age group. Therefore, adoption of the IOM‐2009 system to categorise the nutritional status of pregnant adolescents will lead to recommendations of increased GWG for a large proportion of adolescents. This could have significant implications for pregnancy outcomes as well as long‐term consequences related to post‐partum weight retention and future obesity (Abrams & Laros 1986;Institute of Medicine 2009). Implications of these findings are especially relevant to developing countries and to lower‐income populations of developed countries, where adolescent pregnancies still represent a substantial proportion of all deliveries.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Sources of funding
None.
Contributions
JFAA, GMV, CAFG and IPCS participated in the design of the study. JFAA and GMV collected the data and analysed results. MRT and CAFG analysed and interpreted the data and wrote the initial draft of the paper. MF and IPCS assisted in the interpretation of the results. All authors collaborated in the preparation of the final paper and critically reviewed all sections of the text for important intellectual content.
References
- Abrams B., Altman S.L. & Pickett K.E. (2000) Pregnancy weight gain: still controversial. The American Journal of Clinical Nutrition 71 (5 Suppl.), 1233S–1241S. [DOI] [PubMed] [Google Scholar]
- Abrams B.F. & Laros R.K. Jr (1986) Prepregnancy weight, weight gain, and birth weight. American Journal of Obstetrics and Gynecology 154, 503–509. [DOI] [PubMed] [Google Scholar]
- Altman D.G. (1991) Practical Statistics for Medical Research. 1st edn, Chapman & Hall: London. [Google Scholar]
- Bowker A.H. (1948) A test for symmetry in contingency tables. Journal of the American Statistical Association 43, 572–574. [DOI] [PubMed] [Google Scholar]
- Brunner‐Huber L.R. (2007) Validity of self‐reported height and weight in women of reproductive age. Maternal and Child Health Journal 11, 137–144. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2000) Pediatric Growth Charts [Online]. Available at: http://www.cdc.gov/growthcharts/ (Accessed 12 December 2010).
- Crane J.M., White J., Murphy P., Burrage L. & Hutchens D. (2009) The effect of gestational weight gain by body mass index on maternal and neonatal outcomes. Journal of Obstetrics and Gynaecology Canada 31, 28–35. [DOI] [PubMed] [Google Scholar]
- Daniels S.R., Khoury P.R. & Morrison J.A. (1997) The utility of body mass index as a measure of body fatness in children and adolescents: differences by race and gender. Pediatrics 99, 804–807. [DOI] [PubMed] [Google Scholar]
- Edwards L.E., Hellerstedt W.L., Alton I.R., Story M. & Himes J.H. (1996) Pregnancy complications and birth outcomes in obese and normal‐weight women: effects of gestational weight change. Obstetrics and Gynecology 87, 389–394. [DOI] [PubMed] [Google Scholar]
- Engstrom J.L., Paterson S.A., Doherty A., Trabulsi M. & Speer K.L. (2003) Accuracy of self‐reported height and weight in women: an integrative review of the literature. Journal of Midwifery & Women's Health 48, 338–345. [DOI] [PubMed] [Google Scholar]
- Fernandez I.D., Olson C.M. & De Ver D.T. (2008) Discordance in the assessment of prepregnancy weight status of adolescents: a comparison between the Centers for Disease Control and Prevention sex‐ and age‐specific body mass index classification and the Institute of Medicine‐based classification used for maternal weight gain guidelines. Journal of the American Dietetic Association 108, 998–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez I.D., Hoffmire C.A. & Olson C.M. (2011) Gestational weight gain in adolescents: a comparison to the new Institute of Medicine recommendations. Journal of Pediatric and Adolescent Gynecology 24, 368–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fonseca M.J., Faerstein E., Chor D. & Lopes C.S. (2004) [Validity of self‐reported weight and height and the body mass index within the ‘Pro‐saude’ study]. Revista de Saude Publica 38, 392–398. [DOI] [PubMed] [Google Scholar]
- Francke A.L., de Smit M.C., Veer A.J. & Mistiaen P. (2008) Factors influencing the implementation of clinical guidelines for health care professionals: a systematic meta‐review. BMC Medical Informatics and Decision Making 8, 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillum R.F. & Sempos C.T. (2005) Ethnic variation in validity of classification of overweight and obesity using self‐reported weight and height in American women and men: the Third National Health and Nutrition Examination Survey. Nutrition Journal 4, 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groth S. (2007) Are the Institute of Medicine recommendations for gestational weight gain appropriate for adolescents?, Journal of Obstetric, Gynecologic, and Neonatal Nursing 36, 21–27. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (1990) Nutrition during Pregnancy. National Academies Press: Washington, DC. [Google Scholar]
- Institute of Medicine (2009) Weight Gain during Pregnancy: Reexamining the Guidelines. National Academies Press: Washington, DC. [PubMed] [Google Scholar]
- Mamun A.A., Kinarivala M., O'Callaghan M.J., Williams G.M., Najman J.M. & Callaway L.K. (2010) Associations of excess weight gain during pregnancy with long‐term maternal overweight and obesity: evidence from 21 y postpartum follow‐up. The American Journal of Clinical Nutrition 91, 1336–1341. [DOI] [PubMed] [Google Scholar]
- McDonald S.D., Han Z., Mulla S. & Beyene J. (2010) Overweight and obesity in mothers and risk of preterm birth and low birth weight infants: systematic review and meta‐analyses. British Medical Journal (Clinical Research Ed.) 341, c3428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Must A., Jacques P.F., Dallal G.E., Bajema C.J. & Dietz W.H. (1992) Long‐term morbidity and mortality of overweight adolescents. A follow‐up of the Harvard Growth Study of 1922 to 1935. The New England Journal of Medicine 327, 1350–1355. [DOI] [PubMed] [Google Scholar]
- O'Brien T.E., Ray J.G. & Chan W.S. (2003) Maternal body mass index and the risk of preeclampsia: a systematic overview. Epidemiology (Cambridge, Mass.) 14, 368–374. [DOI] [PubMed] [Google Scholar]
- Rode L., Hegaard H.K., Kjaergaard H., Moller L.F., Tabor A. & Ottesen B. (2007) Association between maternal weight gain and birth weight. Obstetrics and Gynecology 109, 1309–1315. [DOI] [PubMed] [Google Scholar]
- Schmidt M.I., Duncan B.B., Tavares M., Polanczyk C.A., Pellanda L. & Zimmer P.M. (1993) Validity of self‐reported weight – a study of urban Brazilian adults. Revista de Saude Publica 27, 271–276. [DOI] [PubMed] [Google Scholar]
- Scholl T.O. & Hediger M.L. (1995) Weight gain, nutrition, and pregnancy outcome: findings from the Camden study of teenage and minority gravidas. Seminars in Perinatology 19, 171–181. [DOI] [PubMed] [Google Scholar]
- Stevens‐Simon C., Roghmann K.J. & McAnarney E.R. (1992) Relationship of self‐reported prepregnant weight and weight gain during pregnancy to maternal body habitus and age. Journal of the American Dietetic Association 92, 85–87. [PubMed] [Google Scholar]
- Stewart A.L. (1982) The reliability and validity of self‐reported weight and height. Journal of Chronic Diseases 35, 295–309. [DOI] [PubMed] [Google Scholar]
- Torloni M.R., Betran A.P., Daher S., Widmer M., Dolan S.M., Menon R. et al (2009a) Maternal BMI and preterm birth: a systematic review of the literature with meta‐analysis. The Journal of Maternal‐Fetal & Neonatal Medicine 22, 957–970. [DOI] [PubMed] [Google Scholar]
- Torloni M.R., Betran A.P., Horta B.L., Nakamura M.U., Atallah A.N., Moron A.F. et al (2009b) Prepregnancy BMI and the risk of gestational diabetes: a systematic review of the literature with meta‐analysis. Obesity Reviews 10, 194–203. [DOI] [PubMed] [Google Scholar]
- World Health Organization (1998) Obesity: Preventing and Managing the Global Epidemic . Report of a WHO consultation on obesity; WHO/NVT/NCD/98.1. [PubMed]


