Abstract
Breastfeeding is the most advantageous feeding option for infants, and epidemiological studies provide evidence for its promotion. The objective of this review was to comprehensively delineate the barriers and facilitators of exclusive breastfeeding of infants aged 0–6 months old by mothers in developing countries. A search of CINAHL, MEDLINE and PsycINFO was carried out to retrieve studies from January 2001 to January 2014. Using our inclusion criteria, we selected studies that described barriers and facilitators of exclusive breastfeeding. Qualitative and quantitative studies were considered. Twenty‐five studies involving 11 025 participants from 19 countries were included. Barriers and facilitators of exclusive/full breastfeeding were identified, analysed tabulated and summarised in this review. Maternal employment was the most frequently cited barrier to exclusive breastfeeding. Maternal perceptions of insufficient breast milk supply was pervasive among studies while medical barriers related to illness of mothers and/or infants as well as breast problems, rather than health care providers. Socio‐cultural factors such as maternal and significant other's beliefs about infant nutrition also often constitute strong barriers to exclusive breastfeeding. Despite these barriers, mothers in developing countries often possess certain personal characteristics and develop strategic plans to enhance their success at breastfeeding. Health care providers should be informed about the determinants of exclusive breastfeeding and provide practical anticipatory guidance targeted at overcoming these barriers. In so doing, health care providers in developing countries can contribute to improving maternal and child health outcomes.
Keywords: breastfeeding, exclusive breastfeeding, breastfeeding support, barriers, facilitators, developing countries
Introduction
Breastfeeding: public health significance
Breast milk is recognised to be the optimal feeding option for infants (Arthur & Richard 2012; Kramer & Kakuma 2012), and epidemiological studies provide evidence for its promotion, protection and support, especially as it relates to timely initiation and exclusivity. Breastfeeding is considered critical for sustaining the health and well‐being of newborns and infants (Howie et al. 1990; Arifeen et al. 2001; Ip et al. 2007; Kramer & Kakuma 2012). Besides being a source of adequate nutrition for the breastfed infant, it provides clear short‐term benefits by reducing mortality and morbidity from infectious diseases (Arifeen et al. 2001; Kramer & Kakuma 2012). Breastfed infants are also reported to present lower morbidity from allergic diseases (Burr et al. 1993), as well as reduced risk of sudden infant death syndrome (Ford et al. 1993). The long‐term protective effects of breastfeeding against non‐communicable diseases (Kwan et al. 2004; Sadauskaite‐Kuehne et al. 2004; Horta et al. 2007; Ip et al. 2007) have also been reported. Collective evidence from longitudinal studies (Horwood & Fergusson 1998; Anderson et al. 1999), randomised controlled trial (RCT) (Kramer 2010), clinical trials (Morley et al. 1988; Lucas et al. 1992) and neuro‐developmental research (Lanting & Boersma 1996; Morley 1996) all demonstrate the long‐term effect of breastfeeding on improvement of individual cognitive ability and educational achievement, with greater effects often seen with exclusivity and increased duration (Kramer 2010).
Although substantial progress has been recorded in reductions in child deaths worldwide, suboptimal breastfeeding continues to be a leading cause of disease burden and risk factor for child mortality in developing regions of the world (Lim et al. 2013). Thus, based upon evidence for improved maternal, child and population‐level health outcomes, current international opinion recommends that infants be exclusively breastfed for the first 6 months of life followed by the introduction of age appropriate nutritionally adequate and safe complementary foods with continued breastfeeding until 2 years of age or beyond (Kramer et al. 2003; World Health Organization & UNICEF 2003). Also, given the recognition of breastfeeding promotion as the single most cost‐effective child health intervention (Adam et al. 2005; Darmstadt et al. 2005), many national and international programmes and policies have been introduced to improve breastfeeding practices. However, at the level of the individual, a mother's decision on breastfeeding is influenced by a complex combination of traits and behaviours in different contexts. An understanding of these factors has been considered important in providing support to mothers and has been reviewed in several studies (Dennis 2002; Johnston & Esposito 2007; Labbok & Taylor 2008; Whalen & Cramton 2010; McAndrew et al. 2012). Dennis (2002) examined factors influencing breastfeeding initiation and duration among mothers in developed countries under the domains of personal and intrapersonal characteristics, hospital policies and intrapartum experiences, sources of support and breastfeeding interventions and concluded on the need for complementation of professional services with peer support. Additional recommendations include the need for maternal and child health service providers to educate themselves regarding predictors of and barriers to optimal breastfeeding so they can support mothers to meet their personal goals and expert recommendation for breastfeeding practice (Whalen & Cramton 2010).
Comparatively, fewer studies have been conducted in developing countries to identify the barriers to breastfeeding exclusivity among mothers while available evidence has not been systematically synthesised. This necessitates a review of literature examining factors that contribute to or serve as barriers to a mother's success in breastfeeding. Furthermore, health care professionals and policy makers would be informed on how best to support mothers and enhance the success of breastfeeding promotion interventions in developing countries. This review was conducted to comprehensively delineate factors that facilitate or act as barriers to exclusive breastfeeding (EBF) of infants aged 0–6 months among mothers in developing countries.
Key messages
Breastfeeding practices among mothers in developing counties are influenced by a variety of socio‐demographic, socio‐cultural and health‐related factors.
It is imperative that health care providers and policy makers in developing countries understand these factors and provide specific guidance and policies to protect and promote early and exclusive breastfeeding.
Tailoring interventions to support high‐risk groups (such as older mothers and women in employment) is likely to enhance the effectiveness of breastfeeding promotion interventions.
Research examining the impact of preconception and early prenatal breastfeeding plan as well as maternal self‐confidence on breastfeeding duration and exclusivity is needed in developing countries.
Methods
This review included any relevant studies published between January 2001, when the global breastfeeding recommendations were last revised, and January 2014. Quantitative and qualitative primary studies that focused on factors influencing EBF during the first 6 months of life were included. Studies were excluded if they were based entirely on secondary data or examined breastfeeding determinants too broadly, covering age range from 6 to 24 months. Participants included pregnant women and mothers of infants aged between 0 and 6 months.
Search strategy
A search strategy was developed to identify studies relevant to the review objective using the following keywords: ‘breastfeeding’, ‘exclusive breastfeeding’, ‘factor(s)’, ‘determinant(s)’, ‘constraint(s)’, ‘facilitator(s)’, ‘practice’. The electronic search terms were used one by one and/or in combination, were repeatedly refined in response to the emerging data and modified as appropriate for different databases while maintaining the terms central to the search. An example of a full search strategy is shown in Supporting Information http://onlinelibrary.wiley.com/doi/10.1111/mcn.12180/suppinfo. Using the optimised search terms, the following databases were searched: CINAHL, MEDLINE and PsycINFO retrieving 1302 articles. Following removal of duplicates and title screening based upon inclusion criteria, 272 potentially relevant titles were retrieved. Fifty‐seven of these were selected for full‐text screening. An additional 19 references were identified from the reference list of these 57 articles and reports for full‐text screening. Twenty‐five articles met the final criteria for inclusion (see Fig. 1).
Figure 1.
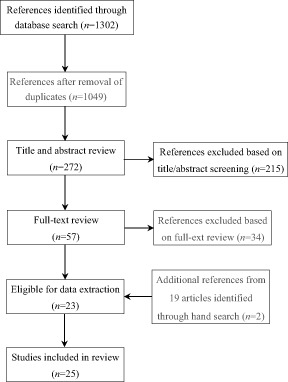
Flowchart showing identification of studies.
Study selection and eligibility criteria
Studies included in this review were restricted to (1) studies published in English from 2001 to 2014; (2) original research articles with primary data considering early infancy (0–6 months); and (3) studies conducted in developing countries.
Studies carried out primarily among HIV populations were excluded. Also, unpublished doctoral dissertations, reports and other reviews were not included. The World Bank list of economies was used to classify developing countries (World Bank 2014). Breastfeeding practices considered in this review were EBF, where the infant receives only breast milk allowing no other liquids or solids, and full breastfeeding (fBF), whereby the infant receives only breast milk without supplementation with non‐human milk (Labbok & Krasovec 1990).
Data extraction and quality appraisal
All identified studies were independently assessed by two authors for relevance based upon the objective of the review. This process was carried out using the study titles and abstracts (full text for those without an abstract) (see Fig. 1). Discrepancies were resolved through discussion and consensus. Studies that failed to meet the inclusion criteria were excluded. Data extraction from the final sample of articles was then conducted using a pre‐established data extraction form. For each study, the data extraction process identified the study design, geographic location, participants breastfeeding practice measured, facilitators of and barriers to EBF or fBF. Enabling factors and barriers to optimal breastfeeding were then grouped into thematic categories and presented as a narrative summary. The Critical Appraisal Skills Programme system of appraisal was adopted to appraise the methods, credibility and relevance of the diverse literature being considered for inclusion (Singh 2013).
Data synthesis
As the identified studies used different approaches in quantitative and qualitative research and methods, both textual narrative and thematic analyses were performed. For the quantitative studies, a textual narrative analysis was provided with study characteristics, and key findings and conclusions of individual studies were summarised in Table 1. Thematic synthesis of data was performed for the qualitative studies as described by Thomas & Harden (2008). Data from qualitative studies are presented under identified themes in Table 2.
Table 1.
Study characteristics and summary of findings from included quantitative studies
| No | Study (year), location | Participants (n) | Design/data synthesis | Main barriers /facilitators | Summary | Authors conclusion |
|---|---|---|---|---|---|---|
| 1. | Abuidhail et al. (2014), Jordan | Post‐partum mother and infant pairs (n = 600) | Longitudinal prospective design. Reported percentages of particular responses. | Barriers: Infant hungry after BF (53%), subsequent pregnancy (27.4%), breast problems (25.5%) | The main barriers to EBF were infants feel hungry after breastfeeding, short periods between pregnancies and breast problems | Post‐partum mothers initiated EBF practice within the first hour of birth but practice declined gradually as the infant grew up within the first 6 months |
| 2. | Agbo et al. (2013), Nigeria | Married female residents doctors (n = 47) | Descriptive cross‐sectional study. Reported percentages of particular responses. |
Barriers: Return to work (61.1%), inadequate lactation and return to work (22.2%), other family demands (5.6%) Facilitators: Family support and longer maternity leave (25.5%), early closure from work (17.0%), perceived benefit to child (10.6%) crèche at work place (6.4%), exemption from calls (4.3%) |
Resumption of work was the main barrier to exclusive breastfeeding. Longer maternity leave and provision of crèches at work places were regarded as potential motivators of EBF | Conducive atmosphere should be created at the work place to encourage the female health care professional to practise EBF on their children as they encourage other mothers to do same |
| 3. | Agnarsson et al. (2001)*, Tanzania | Mothers with infants <7 months old (n = 108) | Household survey. Percentages of responses were reported. | Barriers: Perceived insufficient breast milk, child crying due to insatiety | The main reasons for non‐exclusive breastfeeding were the mothers belief of breast milk insufficiency and child crying because it was not satisfied with mother's milk | The average duration of EBF, although far below recommended levels, is higher than is found in most studies in Africa and Tanzania |
| 4. | Agunbiade & Ogunleye (2012)*, Nigeria | BF mothers with child between age 3 months and 1 year (n = 200) | Complementary mixed qualitative and quantitative method design. Reported percentages of particular responses | Barriers: Baby hungry after feeding (29%), maternal health problems (27%), fear of infant addiction to breast milk (26%), breast pains (25%), pressure from mother‐in‐law (25%), return to work/business (24%) | Major constraints to exclusive breastfeeding were the perception that babies continued to be hungry | BF mothers are faced with multiple challenges as they strive to practice EBF. Scaling up of EBF among mothers requires concerted multi‐level efforts |
| 5. | Al‐Sahab et al. (2008), Lebanon | First Year of Life Follow‐up study birth cohort aged 0–2 months followed up for first year of life (n = 1320) |
Prospective cohort study. ORs were presented. |
Barriers: Maternal employment [non‐working mothers 2.38 times (CI 1.56–3.36) more likely to fBF], paediatrician being male (mothers seeing female paediatrician fBF 1.49 times more likely to fBF) Facilitators: Multiparity (one child OR = 1.90; CI 1.23–2.93) or (two children OR = 2.26; CI 1.40–3.65), younger maternal age (being ≤25) (OR = 2.5; CI 1.46–4.37), early discharge (OR = 1.68; CI 1.14–2.48), religion being Muslim (OR = 1.88; CI 1.27–2.78) |
Significant predictors of fBF at 4 months included maternal age, working status and sex of paediatrician | Breastfeeding rates have been explained by maternal factors such as age, parity religion and health‐care‐related factors such as early discharge and sex of paediatrician. This constitutes the basis for designing interventions. |
| 6. | Arusei et al. (2011), Kenya | Mother–infant pair attending maternal and child health clinic (n = 151) | Longitudinal study. Percentages of particular responses and ORs were presented. | Barriers: Maternal belief that water aids digestion (38%), insufficient breast milk (25%), advice from relatives/friends (18%), acclimatisation (22%), work resumption (13%). Mother's lack of knowledge on infant feeding recommendations (OR = 9.19; CI, 1.72–49.23), late BF initiation (OR = 8.19; CI, 1.34–58.93) | There was a sharp decline in EBF rates from 40.4% at 6 weeks to 9.9% at 10 weeks. Maternal beliefs about infant feeding and PIM were main reasons for EBF cessation. | There is a need to accelerate awareness of optimum infant feeding recommendations and augment the rigorous practice of the WHO ten steps to successful BF |
| 7. | Barennes et al. (2012), Laos | Mothers with infants <24 months old (n = 1057) | Randomised multi‐stage sampling survey. Percentages of particular responses and ORs were presented. | Barriers: Ethnic majority (Lao Loum) mothers of ethnic majority (OR = 1.8 CI, 1.2–2.8) with higher living standards (mothers living in concrete houses (OR = 1.6 CI, 1.1–2.5) more likely to use BMS prior to 6 months. Lack of colostrum use (OR = 0.6 CI, 0.4–1.0). | Lao Loum mothers with better living conditions were more likely to us BMS before 6 months while mothers who fed colostrum at birth and those unemployed living in rural areas were less likely to consider the use of BMS | In Laos, mothers with the highest socio‐economic status are showing a tendency to give up BF |
| Bashour et al. (2008), Syria | Post‐partum mothers (n = 876) | Randomised controlled trial. Percentages of observed outcomes. | Facilitators: Early post‐partum home visit (28.5% and 30% in intervention groups | A significantly higher proportion of mothers in intervention arms reported practicing EBF compared to the non‐intervention group | Post‐partum home visits significantly increased exclusive breastfeeding while other outcomes did not change | |
| Chandrashekhar et al. (2007), Nepal | Mothers who delivered within the previous 2 months (n = 385) | Cross sectional. Percentages of responses and ORs presented. |
Barriers: Caesarean section delivery [mothers with vaginal delivery more likely to EBF (OR 7.6, CI 1.7–34.1)] Facilitators: Friend's feeding practice (mothers more likely to EBF if friend did (OR 2.2, CI, 1.1–4.5)], colostrum use [more likely to EBF if colostrum was first meal (OR 27.2, CI, 12.6–58.7)] |
Friends' feeding practices, type of delivery and baby's first feed were the factors influencing EBF practice | Practices such as pre‐lacteal feeds and premature introduction of complementary feeds are of great concern in this urban population | |
| Dearden et al. (2002)*, Viet Nam | Mothers of infants less than 6 months old in northern Viet Nam (n = 120) | Cross sectional. Responses categorised according to outcome and barrier using pre‐established format. |
Barriers: Work outside home, poor maternal diet, belief that mother ate something unsuitable of mother's body does not supportive of EBF Facilitators: Perceptions of sufficient BM to feed infant, belief that BM is nutritious, encouragement by commune HW |
The risk of not exclusively breastfeeding was greatest for women who returned to work | Strategies such as improving knowledge about the introduction of water and semi‐solids, addressing perceptions of milk insufficiency and presenting mothers with options for EBF even when they work outside home can be implemented to increase EBF practice in rural work environments | |
| do Nascimento et al. (2010), Brazil | Caregivers of children <1 year (n = 1470) | Cross‐sectional population survey. PRs for factors associated with non‐EBF. | Barriers: Pacifier use (PR = 1.69, CI, 1.37–2.09), lower maternal education (PR = 1.59, CI, 1.10–2.29) | Factors associated with interruption of EBF for infants up to 6 months old were higher infant age, pacifier use and lower maternal education | In developing countries, specific strategies must be created for the delivery of information about breastfeeding and the effects of pacifier use especially for less educated women | |
| Hruschka et al. (2003), Guatemala | Mothers of infants aged 0–6 months (n = 328) | Prospective cohort study. HR was presented. | Barriers: Delayed onset of lactation (HR = 4.87, CI, 2.29–10.36), caesarean birth (HR = 1.72, CI, 1.06–2.78) | Mothers who experienced delayed OL had greater risk of ending fBF and the relationship between delayed OL and fBF was mediated partly by pre‐onset supplementation | Mothers who experience delayed OL are less likely to continue fBF in the first 6 months | |
| Kakute et al. (2005), Cameroon | Actively breastfeeding mothers (n = 320) | Survey questionnaire. Percentages of particular responses. | Barriers: Family/community pressure (42.5%), baby not satisfied with BM (20%), mother exhausted from field work (8.4%), no help for daily work (7.2%) | All women surveyed ceased EBF prior to 6 months. Mothers' decisions were influenced mainly by cultural factors. | Women identified various cultural beliefs that constitute barriers to EBF. Health education efforts should focus not only on promoting EBF, but on changing knowledge and attitudes of the communities. | |
| Karacam (2008), Turkey | Mothers with babies aged 0–4 months old (n = 514) | Cross sectional. Percentages of particular responses and ORs. |
Barriers: Frequent crying of baby (OR = 1.69, CI, 1.13–2.53) Facilitators: Maternal employment reduced likelihood of ending EBF (OR = 0.49, CI, 0.29–0.83) |
Risk of use of complementary foods was increased by excessive crying of the baby while a mother being employed considerably reduced the likelihood of giving complementary food | Midwives and nurses can encourage EBF behaviour by providing focused education and counselling to women whose babies cry frequently | |
| Nawaz et al. (2009), Pakistan | Children under 6 month of age (n = 305) | Cross sectional. Percentages of particular responses were presented. | Barriers: Perceptions of insufficient BM (45.9%), maternal employment (18.4%), maternal sickness (13.11%), congenital/acquired disease of child (17.04), subsequent pregnancy (3.61%) | Main causes of non‐breastfeeding included mother's perception of having insufficient milk. Other causes included maternal employment, morbidity in mother and infant and subsequent pregnancy. | Main causes of non‐breastfeeding of infants <6 months are perceptions of having insufficient milk, working women and twin babies. | |
| Okafor et al. (2013), Nigeria | Women whose child was < = 2 years old (n = 600) | Community‐based, cross‐sectional. Percentages of particular responses and ORs. | Barriers: Older maternal age, nulliparity or having > = 5 children, lower maternal education, lack of formal ANC attendance, lack of institutional delivery | Mothers with no formal education were at higher risk of not practising EBF while formal antenatal care and institutional delivery increased the practice of EBF for 6 months | Promotion of good health‐seeking behaviour, maternal education and family planning are recommended to improve mothers breastfeeding practice and infant nutrition | |
| Perera et al. (2012), Sri Lanka | A birth cohort (n = 500) | Prospective observational study. Percentages of particular responses | Barriers: Maternal anxiety of inadequate BM, inadequate weight gain, return to work, older maternal age | The main reason for stopping EBF was concerns regarding weight gain and mothers return to work | Mothers resuming work and concerns regarding adequacy of breast milk were the major reasons to cease EBF | |
| Santo et al. (2007), Brazil | Post‐partum mother and infant pairs (n = 220) | Prospective cohort study. Percentages of particular responses and HR. | Barriers: Adolescent mother (HR = 1.48, CI, 1.01–2.17), <6 ANC visits (HR = 1.60, CI, 1.10–2.33), pacifier use (HR = 1.53, CI, 1.12–2.11), poor latch‐on (HR = 1.29, CI, 1.06–1.58) | Factors associated with EBF cessation prior to 6 months were adolescent mother, <6 prenatal visits, pacifier use within the first month and poor latch‐on parameters | Activities to promote EBF should be intensified for adolescent mothers and for those whose prenatal care is less than ideal reinforcing the ill effects of pacifier used. Mothers also need appropriate instruction on correct breastfeeding techniques. | |
| Sasaki et al. (2010), Cambodia | Mothers with infants aged from 6 to 24 months (n = 312) | Cross‐sectional study. Percentages of particular responses and ORs. | Barriers: Maternal occupation (OR = 4.71, CI, 2.77–8.01), lack of paternal attendance at breastfeeding classes (OR = 1.93, CI, 1.13–3.28), lack of a maternal antenatal EBF plan (OR = 10.01, CI, 3.68–27.24) | Risk factors for EBF cessation included the lack of a maternal antenatal EBF plan, maternal employment and lack of paternal attendance at breastfeeding classes | It is important to educate mothers on the significance of EBF so that they will develop the intention and plan to practise EBF. Paternal involvement in breastfeeding classes may help complement breastfeeding practices | |
| Tamiru et al. (2013)*, Ethiopia | Mothers with infants aged <6 months (n = 384) | Community‐based cross‐sectional study. Percentages of particular responses and ORs. |
Barriers: Maternal beliefs that: complementary food provides more nutrients than BM (41.88%), additional food protected baby from evil eyes/stomach ache (15.7%), breasts too small (3.1%). Mothers perception that complementary food is necessary for normal growth (AOR = 4.24, CI, 2.33–7.71) Facilitators: Early BF initiation (AOR = 0.52, CI, 0.32–0.84), maternal knowledge of EBF duration (AOR = 0.43, CI, 0.06–0.99), maternal preference for BM (AOR = 0.15, CI, 0.05–0.45) |
Majority of mothers introduced complementary foods early due to perceptions of breast milk insufficiency and influences from social beliefs. Early initiation of breastfeeding and maternal attitude about dietary importance of breast milk were supportive factors for breastfeeding. | Factors contributing to early introduction of complementary foods need to be taken into account while designing intervention strategies for breastfeeding | |
| Ulak et al. (2012), Nepal | Mothers with infants aged <6 months (n = 325) | Cross‐sectional survey. Percentages of particular responses and ORs. |
Barriers: Insufficient BM (51.4%), baby crying/hungry (29.2%), work outside home (16.3%) mothers illness (3.1%). Living in joint families (84% vs. 64%, P < 0.001) Facilitators: Knowledge of EBF recommendation (OR = 0.6, CI, 0.4–0.9), infant not hospitalised (OR = 2.7, CI, 1.0–7.4) |
The main reason for non‐exclusive breastfeeding was insufficient breast milk. Enabling factors for EBF included mothers' knowledge on recommended duration of EBF and not living in joint families. | Continuation of EBF until 6 months was not common despite initiation of breastfeeding. Very few mothers received information on BF duration during antenatal visit indicating a need for counseling on EBF. | |
| Vaahtera et al. (2001), Malawi | Mothers with infants aged <6 months (n = 760) | Prospective cohort study. Associations between predictor variables and duration of EBF. | Barriers: Lower maternal education, higher number of children <15 years old | Better adherence to infant feeding recommendations was associated with increased education, lower parity and other socio‐economic factors | EBF is uncommon and complementary foods were introduces to infants early among rural families. Education and family planning may improve adherence to infant feeding recommendations in the population. |
ANC, antenatal care; AOR, adjusted odds ratio; BF, breastfeeding; 95% CI, 95% confidence interval; BMS, breast milk substitutes; EBF, exclusive breastfeeding; fBF, full breastfeeding; HR, hazards ratio; HW, health worker; OR, odds ratio; PIM, perceptions of insufficient breast milk; PR, prevalence ratio; WHO, World Health Organization.
*Studies utilising mixed qualitative and quantitative methods.
Table 2.
Study characteristics and summary of findings from included qualitative studies
| Author (year), location | Participants (n) | Data collection /synthesis | Main barriers/facilitators | Key findings | Authors conclusion |
|---|---|---|---|---|---|
| Agnarsson et al. (2001)*, Tanzania | Mothers with infants <7 months old, elderly women, TBAs and health care providers (nurses/midwives, medical doctor, nurse tutor) | Key informant interviews and focus group discussions using semi‐structured questions | Barriers: Cultural beliefs about BM (‘bad breast milk’), belief that colostrum is bad, old milk | Health care providers displayed an understanding of infant feeding recommendations while mothers, grandmothers and TBAs reported traditional practices preventing early initiation of BF and exclusivity | Divergent views were expressed about infant feeding practices among health care providers and mothers, grandmothers and TBAs |
| Agunbiade & Ogunleye (2012)*, Nigeria | Nurses (n = 10), mothers practising EBF (n = 11), grandmothers (n = 10) | In‐depth structured interviews and focus group discussions. Notes and audiotapes were transcribed translated and coded based on major themes. | Barriers: Health‐related problems, refusal of BM by infant, inadequate maternal nutrition, lactation problems, inadequate support from husband and conflicting opinions on infant feeding practices from the significant other | Poor feeding, inadequate support from husband and conflicting positions on infant feeding practices from the significant others were dominant constraints to the practice of EBF | BF mothers are faced with multiple challenges as they strive to practise EBF. Policies aimed at improving EBF uptake should also incorporate significant others in the process. |
| Dearden et al. (2002)*, Viet Nam | Mothers of infants <6 months old, husbands, parents and parents‐in‐law | Focus groups. Interviews were tape recorded, data were transcribed, translated and categorised according to outcome and barrier. |
Barriers: Work outside home, poor maternal diet, mother eats something unsuitable, mothers body does not support EBF Facilitators: Belief that BM is sufficient to feed infant, BM is nutritious, encouragement by commune health workers |
Work outside home and poor maternal diets were key barriers to giving only BM | Strategies addressing perceptions of milk insufficiency and presenting mothers with options for EBF even when they work outside home can be implemented to increase EBF practice in rural work environments |
| Shao Mlay et al. (2004), Tanzania | BF working mothers of babies <7 months old (n = 6) | Participants were interviewed individually until a repeat pattern of information was heard. Data were analysed and organised under specific properties of the central categories. |
Barriers: Maternal employment, lack of workplace flexibility, no on‐site child care, lack of expressing/BF rooms and short maternity leave at most workplaces Facilitators: Women's assigned value of BM, previous experience and knowledge of EBF, maternal determination and resilience, |
Women in employment face major constraints and often lack the support to put EBF knowledge to practise. Despite the social constraints against EBF, some women made personal adjustments to help overcome these constraints. | Public health officials educated women on the advantages of EBF in terms of their babies' health and their own but women were left to their own devises when it came to solving the practical problems of BF at the same time as holding down a full‐time job |
| Nabulsi (2011), Lebanon | Post‐partum women with healthy live term newborns (n = 36) | Focus group discussions and serial follow‐up in‐depth interviews. Interviews were tape recorded and transcribed. Major and minor themes were generated. |
Barriers: Perceptions of insufficient BM, fear of weight gain or breast sagging, breast pains, sleep deprivation, exhaustion and maternal employment Facilitators: Maternal positive attitude towards BF, determination, family support |
Themes generated revealed both positive and negative perceptions of BF. Women who breastfeed were determined to succeed and overcome barriers relying mostly on family support and proper time management. | Increasing awareness of future mothers about BF difficulties along with the benefits to children, mothers and society at large may further promote BF, and improve exclusivity and continuation rates in Lebanon |
| Otoo et al. (2009), Ghana | BF mothers with at least one child <4 months old (n = 35) | Focus group discussions. Tape‐recorded discussions were transcribed, coded and grouped to form major themes. |
Barriers: Maternal employment, breast and nipple problems, perceived BM insufficiency, pressure from family and inability to breastfeed outside home Facilitators: Mothers prior experience with non‐exclusively breastfed infant, belief that BM is best, convenient and available at no cost |
Participants understood that EBF is the superior infant feeding method but still believed that water can be given if clean. | Addressing the concerns expressed in this study can be used to enhance EBF promotion in this region |
| Tamiru et al. (2013)*, Ethiopia | Key informants (n = 15) | In‐depth interviews. Audio‐taped data were transcribed and categorised to generate themes. |
Barriers: Cultural beliefs about infant feeding, e.g. belief that complementary food protects infant from evil eyes, perceptions of insufficient BM Facilitators: Mothers knowledge of the benefits of BF |
Mothers who had basic knowledge about dietary importance of BM as well as maternal exposure to BF education had greater role in enhancing optimal infant feeding practices | Factors contributing to early introduction of complementary foods need to be taken into account while designing intervention strategies for BF |
BF, breastfeeding; BM, breast milk; EBF, exclusive breastfeeding; TBA, traditional birth attendant. *Studies utilising mixed qualitative and quantitative methods.
Results
Twenty‐five studies involving 11 025 participants were selected for inclusion in the review. The studies represented a wide variety of countries and designs. Nineteen countries were represented with the majority located in Africa (10 countries) followed by the Middle East (5 counties), South/South East Asia (7 countries) and the Latin Americas (3 countries). Almost all studies were observational employing diverse methodologies. Fourteen studies were cross sectional and seven were prospective cohort studies. Three qualitative studies used in‐depth interviews and focus group discussions and one RCT was included. Four of the studies with cross‐sectional designs used mixed qualitative and quantitative methods. The data extraction process identified 17 enabling factors from 14 studies categorised into three domains and 22 barriers for optimal breastfeeding from 25 studies grouped into four broad domains (Table 3).
Table 3.
Summary of barriers and facilitators of exclusive/full breastfeeding in infants aged 0–6 months
| Barriers | n | Facilitators | n |
|---|---|---|---|
| Socio‐demographic factors | Social support | ||
| Maternal employment | 16 | Family support | 2 |
| Maternal age | 4 | Friends breastfeeding pattern | 1 |
| Maternal education | 4 | Nuclear family structure | 1 |
| Parity | 3 | Workplace flexibility and support | 2 |
| Religion | 1 | Medical and health care/nutrition | |
| Medical and health‐care‐related factors | Naturalness and perceived benefits to the child (nutritional and health) | 3 | |
| Perceptions of insufficient or lack of breast milk | 12 | Early post‐partum discharge | 2 |
| Maternal/infant morbidity/mortality and lactation problems | 9 | Paediatrician being female | 1 |
| Twin delivery | 2 | Early post‐partum home visiting/encouragement from health workers | 2 |
| Caesarean section | 2 | Early initiation of breastfeeding and colostrum use | 5 |
| Subsequent pregnancy | 2 | ANC attendance and institutional delivery | 2 |
| Lack of ANC attendance and EBF plan | 3 | Maternal knowledge of EBF duration | 3 |
| Poor maternal nutrition | 3 | Rooming in | 1 |
| Other infant‐related factors | 3 | Psychological and other maternal factors | |
| Socio‐cultural factors | Mothers will and resilience | 2 | |
| Other family demands/lack of support | 4 | Perceived joyful and connecting experience | 1 |
| Maternal beliefs about breastfeeding and infant nutrition | 5 | Maternal food preference | 1 |
| Relative's advice (pressure)/peer pressure | 5 | Convenient for mother | 1 |
| Acclimate infant to other foods | 2 | Breastfeeding on demand and night feeding | 1 |
| Cultural practices | 3 | ||
| Concerns about body image | 4 | ||
| Environmental factors | |||
| Lack of social infrastructure and amenities | 4 | ||
| Breast milk substitute and pacifier use | 2 |
ANC, antenatal care; EBF, exclusive breastfeeding; n, number of sources citing factor.
Predictors of exclusive breastfeeding
Socio‐demographic factors
Empirical evidence from both qualitative and quantitative studies reveals that maternal characteristics, such as age, educational level, employment, parity, family type, religion, place of residence and living standard, all act to influence a mother's infant feeding practice. Sixteen of the 25 studies found being in formal employment or being engaged in work outside home (Dearden et al. 2002; Shao Mlay et al. 2004; Kakute et al. 2005; Al‐Sahab et al. 2008; Karacam 2008; Otoo et al. 2009; Sasaki et al. 2010; Arusei et al. 2011; Nabulsi 2011; Agunbiade & Ogunleye 2012; Barennes et al. 2012; Perera et al. 2012; Ulak et al. 2012; Agbo et al. 2013; Tamiru et al. 2013) to be strongly associated with EBF (Table 3). A cross‐sectional survey to determine actual EBF rates in a cohort of Sri Lankan infants aged less than 6 months old showed that mother starting work was a reason to stop EBF as early as 2 months of infant age (Perera et al. 2012). Similarly, women in rural Vietnam who had returned to work post‐partum found to be more likely than mothers who had not to fail to exclusively breastfeed (Dearden et al. 2002). In‐depth interviews with mothers in Ghana (Otoo et al. 2009) and Tanzania (Shao Mlay et al. 2004) also identified maternal employment as an important barrier to EBF, resulting either from short maternity leaves or lack of on‐site feeding locations. However, in contrast to these reports, one study conducted among Turkish women found maternal employment to be positively associated with EBF (Karacam 2008). Four studies showed that adolescent mothers aged <20 years old (Santo et al. 2007) or mothers who are ≥35 years old (Al‐Sahab et al. 2008; Perera et al. 2012; Okafor et al. 2013) are less likely to breastfeed their babies exclusively compared with other mothers. While more studies found that lower maternal education was a risk factor for non‐exclusive breastfeeding (Vaahtera et al. 2001; do Nascimento et al. 2010; Okafor et al. 2013), Barennes et al. (2012) reported the opposite in their study. Reports on associations between parity and EBF were inconsistent. Other factors found to be associated with EBF practice include family type (Ulak et al. 2012), religion (Al‐Sahab et al. 2008), place of residence and living standard (Vaahtera et al. 2001; Barennes et al. 2012). One study conducted in Nepal reported that living in joint families is negatively associated with exclusive or predominant breastfeeding for up to 4 months (Ulak et al. 2012). Regarding standard of living of mothers, while Barennes et al. (2012) found that living in urban areas, with good sanitary conditions, increased the risk of using breast milk substitutes prior to 6 months in Laos, another study in Malawi found better adherence to infant feeding recommendations among mothers with higher living standards (Vaahtera et al. 2001).
Medical and health‐care‐related factors
Perceptions of breast milk (in)sufficiency
Thirteen studies reported on mother's perception of the adequacy of breast milk in satisfying the energy and nutritional demands of their infants (Agnarsson et al. 2001; Dearden et al. 2002; Kakute et al. 2005; Karacam 2008; Nawaz et al. 2009; Otoo et al. 2009; Arusei et al. 2011; Nabulsi 2011; Agunbiade & Ogunleye 2012; Perera et al. 2012; Ulak et al. 2012; Tamiru et al. 2013; Abuidhail et al. 2014). In 11 studies, mothers stopped practising EBF due to perceptions of insufficient breast milk (Agnarsson et al. 2001; Kakute et al. 2005; Nawaz et al. 2009; Otoo et al. 2009; Arusei et al. 2011; Nabulsi 2011; Perera et al. 2012; Ulak et al. 2012; Agbo et al. 2013; Abuidhail et al. 2014), lactational problems (Agunbiade & Ogunleye 2012) or excessive crying of the infant (Agnarsson et al. 2001). One study found a significant association between frequent crying of an infant and increased use of complementary foods (Karacam 2008). In contrast, Dearden et al. (2002) reported that women who felt that they had sufficient milk for their infants were significantly more likely to exclusively breastfeed their infants.
Maternal and infant morbidity
Maternal and/or infant morbidities were a major barrier to EBF in nine studies (Agnarsson et al. 2001; Nawaz et al. 2009; Otoo et al. 2009; Arusei et al. 2011; Nabulsi 2011; Agunbiade & Ogunleye 2012; Perera et al. 2012; Ulak et al. 2012; Abuidhail et al. 2014). Five of these studies were carried out in African countries and reported morbid conditions including infant colic (Arusei et al. 2011), maternal sickness (Agnarsson et al. 2001; Kakute et al. 2005; Otoo et al. 2009; Agunbiade & Ogunleye 2012) and breast problems such as breast/nipple infections (Kakute et al. 2005), breast abscesses, swelling and pain (Otoo et al. 2009; Agunbiade & Ogunleye 2012) as reasons for discontinuing EBF. Two separate studies in Lebanon and Jordan involving post‐partum mother–infant cohorts that were followed up from birth reported maternal illness (Abuidhail et al. 2014) and negative breastfeeding experiences (painful and tiring) as main barriers to EBF (Nabulsi 2011), while in Pakistan, mothers with chronic disease conditions or those having infants with congenital or acquired diseases were less likely to breastfeed exclusively (Nawaz et al. 2009). Other reported factors that act as barriers to EBF include subsequent pregnancy (Abuidhail et al. 2014), mode of delivery being Caesarean section (Chandrashekhar et al. 2007), mother feeling tired post‐partum (Agnarsson et al. 2001) and inadequate weight gain by infant (Perera et al. 2012).
Timely initiation of breastfeeding
Five studies were identified that reported on the association between the timing of breastfeeding initiation, colostrum use and EBF. Two of the studies showed that mothers who initiated breastfeeding within the first hour of delivery were significantly less likely to introduce complementary foods prior to 6 months (Arusei et al. 2011; Tamiru et al. 2013). Similarly, mothers in Nepal (Chandrashekhar et al. 2007) and Laos (Barennes et al. 2012) who fed colostrum to their infants as the first meal were more likely than others to practise EBF. On the contrary, mothers of infants from four Guatemala communities reporting delayed onset of lactation (described in this study as lactation >3 days post‐partum) were significantly at a greater risk of ending fBF than did mothers experiencing normal lactation (Hruschka et al. 2003).
Antenatal attendance, EBF recommendation knowledge and plan
Early cessation of EBF was found to be significantly associated with fewer (<6) maternal antenatal visits (Santo et al. 2007) or non‐attendance of formal antenatal clinics at a health facility (Okafor et al. 2013). Interestingly in a Cambodian study, Sasaki et al. (2010) provided evidence to show that lack of paternal attendance at prenatal breastfeeding classes and the lack of maternal antenatal EBF plan are also important barriers to breastfeeding exclusivity during the first 6 months of life. However, three studies showed that mothers who reported that they knew the WHO recommendations on early infant feeding were significantly more likely to practise EBF than others who did not know (Arusei et al. 2011; Ulak et al. 2012; Tamiru et al. 2013).
Health‐care‐related and other factors
Several studies reported on influence of health‐care‐related factors on EBF practice. In particular, women who had institutional deliveries in Nigeria (Okafor et al. 2013) and those who had nurses, midwives or doctors in attendance at delivery in a Vietnamese study (Dearden et al. 2002) were significantly more likely to exclusively breastfeed their infants. According to this study, mothers who practised EBF also indicated that community health workers influenced their decision to exclusively breastfeed (Dearden et al. 2002). A similar finding was reported in an RCT carried out in Syria to assess the impact of community‐based post‐natal home visit intervention on maternal and child health outcomes, whereby post‐partum home visits significantly increased EBF among mothers (Bashour et al. 2008). Also, mothers in Lebanon who were discharged early, within 48 h of delivery, were reported to be more likely to be breastfeeding at 1 month compared with those discharged late. In the same study, paediatrician's gender was found to be a significant predictor of breastfeeding, whereby paediatricians being male was an important barrier to EBF at 4 months (Al‐Sahab et al. 2008).
Other factors reported to serve as barriers to EBF include delivery of twins (Kakute et al. 2005; Nawaz et al. 2009), improper latch‐on techniques (Santo et al. 2007), inadequate infant weight gain (Perera et al. 2012) and refusal of breast milk by some children (Agunbiade & Ogunleye 2012).
Socio‐cultural factors
Availability of social support and other family demands
Several studies reported the availability of a support system to be a facilitator of EBF and the absence thereof as a barrier. In four of the studies employing qualitative methods to explore facilitators and barriers to EBF, lack of support from significant family members and/or lack of social support was a commonly recurring theme. Two separate studies showed that mothers in Ghana and Nigeria considered lack of support from their partners' important factors, leading to discontinuation of EBF (Otoo et al. 2009; Agunbiade & Ogunleye 2012). Similarly, Shao Mlay et al. (2004) emphasised how lack of support brought about by gender roles constitutes important stressors on breastfeeding mothers. In the same study carried out among women in employment in Tanzania, it was found that women were often left to their own devices when it came to solving practical problems of breastfeeding in both the home and the workplace (Shao Mlay et al. 2004). On the other hand, in the study by Nabulsi (2011), mothers reported family support of a breastfeeding mother to be a cultural expectation, which served as an important facilitator of EBF.
Cultural influences and beliefs about breastfeeding and infant nutrition
Five studies described the role of maternal beliefs about infant nutrition on breastfeeding. Some mothers were found to discontinue (or not practise) EBF due to cultural beliefs or family traditions (Otoo et al. 2009; Tamiru et al. 2013). In other studies, mothers reported offering foods other than breast milk to their infants because they believed water‐based drinks aided digestion (Arusei et al. 2011) and to acclimate the infant to other foods (Otoo et al. 2009; Agunbiade & Ogunleye 2012). Agunbiade & Ogunleye (2012), Kakute et al. (2005), and Otoo et al. (2009) all reported family and community pressure as a major reason for discontinuation for EBF in different African communities. Conversely, a study carried out in Nepal showed that feeding practices of friends influenced the mothers decision to breastfeed exclusively, whereby mothers whose friends practised EBF were more likely to breastfeed their baby exclusively (Chandrashekhar et al. 2007). Other facilitators of EBF reported in two studies include maternal determination and resilience that came from knowledge of the benefits of breastfeeding (Shao Mlay et al. 2004; Nabulsi 2011) and mothers' perception of breastfeeding as a natural, joyful and connecting experience for both mother and child (Nabulsi 2011).
Concerns about changes in body image
According to four studies, perceptions of body image and unwanted body changes were another reason why some mothers may refuse to breastfeed their babies at all. Negative effects of breastfeeding on body image described in these studies include changes in breast shape and sagging (Otoo et al. 2009; Nabulsi 2011; Agunbiade & Ogunleye 2012) and weight gain (Nabulsi 2011). On the other hand, Tamiru et al. (2013) reported that some mothers failed to breastfeed due to concerns that their breast was too small.
Environmental and other factors
Other factors identified by several studies to serve as barriers to EBF include fear of contamination if breast milk was expressed due to non‐availability of steady supply of electricity to refrigerate the breast milk (Dearden et al. 2002; Agbo et al. 2013) and unavailability of hygienic and convenient feeding locations (Shao Mlay et al. 2004; Otoo et al. 2009). Findings from two studies conducted in Brazil also showed that pacifier use was associated with EBF discontinuation in infants less than 6 months old (Santo et al. 2007; do Nascimento et al. 2010).
Discussion
Studies aiming to identify factors associated with and influencing infant feeding practices are of great public health significance given the importance of EBF and the unacceptably low rates of this infant feeding pattern across the developing world. To this end, we sought to provide a narrative presentation of evidence of the barriers and facilitators of EBF in infants under 6 months old born to mothers in developing countries. Twenty‐five studies were included, presenting data from a number of counties across three continents. All of the evidence was collected from primary research of varying methodologies and quality. The lack of consistency in breastfeeding definitions, the wide variety of methodologies and the outcome measures make comparison of findings from individual studies difficult. Although this review summarised the findings in separate broad categories, most of the reviewed studies reported on a combination of factors. Our findings suggest that EBF is determined by a combination of these factors, either facilitating or inhibiting a woman's ability to exclusively breastfeed for 6 months.
Factors that act as barriers to exclusive breastfeeding
Much of the evidence from the included studies revealed that mothers engaged in formal or informal income‐generating activities outside home, who were less educated or older, were less likely to practise EBF according to WHO recommendations. The single deterrent of EBF with the most empirical support was maternal employment, highlighting the difficulties mothers working outside home face with regard to breastfeeding, wherein majority of the included studies showed that a woman's return to work was predictive of EBF cessation. This observation might be further exacerbated by the short maternity leave for women in formal employment in some of the countries represented (International Labor Organization 1998) and emphasises maternity leave duration as crucial for prolonging EBF. With more female labour force participation across many regions of the world (United Nations 2010), maternal employment rates are also likely to increase. As demonstrated in a study by Baker & Milligan (2008), maternity protection legislation allows women to breastfeed without having to choose between work and the best nutrition for their infant. Evidence using longitudinal data shows that longer maternity leave increased the likelihood of mothers attaining the recommendation of 6 months EBF in Canada (Baker & Milligan 2008). However, such effect may not be applicable in situations where women are mostly employed in the informal sector. This is particularly important in the context of developing countries given that mothers with lower education are more likely than better educated mothers to be in informal employment. They are also less likely to know the benefits of EBF, making them more at risk of EBF cessation. It is therefore necessary that an inter‐sectorial and comprehensive approach is employed by countries to reduce the adverse socio‐economic impact of maternity on women and their households through capacity building, policies and programmes in support of women's social and economic empowerment. For example, evidence demonstrates the impact of coupling health education with microfinance on improving health outcome in areas including maternal and child health, child nutrition and breastfeeding (Pronyk et al. 2007; Leatherman et al. 2012). Furthermore, maternity leave and workplace protection for breastfeeding mothers need to involve government authorities enforcing labour laws in private and public sectors. Regarding maternal age, the findings of this review differ from reports from the United States (Whalen & Cramton 2010; Jones et al. 2011), England (Oakley et al. 2013) and Australia (Fisher et al. 2013) where higher maternal age is shown to be associated with increased odds of EBF. Our review showed that older mothers had lower EBF rates compared with younger non‐adolescent mothers. This may be due to higher employment rates, maternal fatigue and difficulty in combining demands of work, domestic responsibilities and breastfeeding among older mothers. Similar to findings in the United States (Whalen & Cramton 2010), a few studies showed that mothers who are primiparous and with no prior experience of breastfeeding were less likely to exclusively breastfeed, while women with at least one child had a higher likelihood of practising EBF. However, the presence of other children (Perera et al. 2012; Okafor et al. 2013), employment (Shao Mlay et al. 2004; Al‐Sahab et al. 2008; Agbo et al. 2013) and the lack of support (Shao Mlay et al. 2004) may be responsible for early discontinuation of EBF for parity higher than two. Although health care providers cannot impact a mother's parity, they may be able to improve EBF success by identifying and educating these high‐risk groups on practical ways of establishing breastfeeding and time management.
Among medical and health‐care‐related factors, the influential nature of perceived insufficient breast milk (PIM) was pervasive across the studies with women in most of the studies citing PIM to be a major barrier to EBF (Nawaz et al. 2009; Arusei et al. 2011; Barennes et al. 2012; Perera et al. 2012; Ulak et al. 2012; Agbo et al. 2013). In several of these studies, infants crying after feeds were regarded as infant insatiety cues, and thus, the primary indicator of breast milk inadequacy. However, without consideration of other factors, it remains unclear if maternal perception of inadequate breast milk is accurate. An integrative review of literature on PIM by Gatti (2008) also concluded on the need for determining the relationship between perceived and actual breast milk supply. This would allow for health worker training to provide maternal education about PIM and maternal behaviours that influence milk supply. Given that a mother's view of infant insatiety with breastfeeding is related to perceptions of milk supply, addressing PIM would require emphasis on breastfeeding counselling during the antenatal period. It is also necessary to educate women about proper breastfeeding techniques address cultural beliefs about lactation and provide anticipatory guidance on overcoming other common problems mothers may encounter during breastfeeding. Also important is the in‐hospital practice and the early post‐partum period, which are critical to the development of PIM and other lactation problems (Gatti 2008). However, in settings where the rate of health facility delivery is low, community‐based support for breastfeeding mothers through home visits by trained health workers or other support group activities during the post‐partum period would be important.
While in many studies, mothers were reported to acknowledge the benefits of EBF, they were also constrained by various social and cultural barriers. However, there is ample evidence on the effectiveness of support interventions in improving breastfeeding outcomes (Hannula et al. 2008; Renfrew et al. 2012). Although a majority of the studies reporting these barriers are from cultures where breastfeeding is a normative expectation, women still experience lack of support due not only to unavailability of proper infrastructure as elucidated in three studies (Shao Mlay et al. 2004; Otoo et al. 2009; Agbo et al. 2013), but often caused by gender roles (Shao Mlay et al. 2004; Agunbiade & Ogunleye 2012) and the influence of significant family members possibly in an attempt to carry‐on age long traditions and customs.
Interestingly, a number of studies (Otoo et al. 2009; Nabulsi 2011; Agunbiade & Ogunleye 2012) revealed that a concern over body image is a reason why many mothers determine not to breastfeed at all or fail to breastfeed their infants exclusively. While this notion is widely disputed among paediatricians and lactation experts, the perceived negative impact of breastfeeding on breast appearance has been cited elsewhere (Foster et al. 1996; Barnes et al. 1997). As with breasts appearance, past studies have also shown that the odds of intending to breast feed as early as during the infant's first week was significantly higher (odds ratio = 1.25, 95% confidence interval 1.09–1.42) for women who had no concern over their body image than for those with body image disturbances (Barnes et al. 1997). Given the above, while educational programmes often focus on the health benefits of breastfeeding for mother and child, attention needs to shift to the decision‐making processes that mothers go through in making their infant feeding choices including the effect body image has on optimal infant feeding.
Factors supportive of exclusive breastfeeding
Social relationships and support from family and friends are important determinants of successful breastfeeding. Although breastfeeding practice is influenced by a wide range of factors, our review found that support from family members (Nabulsi 2011) and presence of a friend who breastfed a child (Chandrashekhar et al. 2007) are important determinants of EBF in different populations. Several reviews have also provided supportive evidence on the role of family and friends in breastfeeding success (Johnston & Esposito 2007; Whalen & Cramton 2010), even among working mothers (Johnston & Esposito 2007). For example, in their review, Johnston and Esposito reported on the role of a supportive partner, family members and friends in ensuring continued breastfeeding during employment for mothers in the United States (Johnston & Esposito 2007). This support may be from interactions with persons such as family members and close friends or individuals in everyday life. Hospital practices such as rooming‐in and early discharge (Al‐Sahab et al. 2008) were also found to be supportive of EBF. Prior studies have also shown that maintaining mother–infant closeness improved breastfeeding and other outcomes up to 1 year later compared with separation of mother and infant (Perez‐Escamilla et al. 1992; Bystrova et al. 2009). However, opinions on the effect of early discharge on breastfeeding outcome are mixed (Waldenström et al. 1987; Winterburn & Fraser 2000; Heck et al. 2003; Cambonie et al. 2010) with some studies reporting improved breastfeeding outcomes (Margolis & Schwartz 2000; Yanicki et al. 2002). Further, this review highlighted the importance of community‐based post‐natal home visits in promoting and improving EBF rates (Dearden et al. 2002; Bashour et al. 2008). In many developing countries where a large proportion of deliveries take place at home, and with restricted access to health care facilities (Montagu et al. 2011), home visits by trained health workers is particularly important to empower mothers to initiate and establish breastfeeding. Interestingly, Al‐Sahab et al. (2008) in their study also revealed the positive impact of female paediatricians on EBF rates in Lebanon. A systematic review by Roter & Hall (2004) showed that female physicians offer more positive, emotional focused talk with psychosocial questioning and counselling. Besides this attribute, they may also encourage and support mothers by reflecting on their personal experiences. Therefore, research is needed into care‐seeking behaviour of mothers in the early post‐partum period in order to promote health system capacity building supportive of breastfeeding. It may also become necessary to integrate self‐efficacy enhancing strategies into health care services in developing countries in order to improve mothers' confidence in their ability to breastfeed and to preserve it even in the event that she encounters any difficulties.
Comparison with studies from developed countries
EBF continues to be recognised as the optimal mode of nutrition for infants globally. It is against this backdrop that several developed countries have set goals to support, protect and promote breastfeeding among mothers (U.S. Department of Health and Human Services 2013; Ministry of Health, Labour and Welfare 2013; Australian Government Department of Health and Ageing 2009). Despite these efforts, however, many mothers still fail to meet their desired breastfeeding goals for various reasons. Certain maternal characteristics have been reported to be risk factors for EBF cessation often as early as 1‐month post‐partum. An extensive literature review on achieving EBF in the United States broadly categorised obstacles and constraints specific to EBF practice to include factors relating to health care system and providers, social, economic and political influences as well as media and marketing practices (Labbok & Taylor 2008). Unlike the observation from studies in developing countries, medical constraints that mothers in developed countries face relate more to problems from health systems rather than directly to the mother's health (Whalen & Cramton 2010; Oakley et al. 2013). However, lactational problems and perceptions of breast milk insufficiency are common barriers to successful breastfeeding among mothers in both developed and developing countries. While health behaviours such as smoking and overnutrition among mothers in developed countries have been reported to reduce the likelihood of EBF practice (Labbok & Taylor 2008; Whalen & Cramton 2010; Oakley et al. 2013), none of the studies included in the current review reported on maternal smoking while concerns of body image was related more with breasts appearance (Otoo et al. 2009; Nabulsi 2011; Agunbiade & Ogunleye 2012). This may be due to the fact that in many developing countries (especially in Africa and Middle East), there is an overall veneration of larger body size for women (Holdsworth et al. 2004; Rguibi & Belahsen 2006; Ettarh et al. 2014). From a public health perspective, these differences present opportunities for interventions promoting positive health behaviours among pregnant and breastfeeding women. It is also recommended that health care workers employ a proactive approach of routinely educating pregnant women on the benefits of positive health behaviours while highlighting the disadvantages of risky health behaviours for maternal, child and population health. Similar to reports from developing countries, numerous studies also showed that positive maternal attitudinal and intrapersonal characteristics predicted higher rates of EBF (Dennis 2002; Johnston & Esposito 2007; Labbok & Taylor 2008; Whalen & Cramton 2010). A striking difference between studies from both regions was the influence of prenatal infant feeding intention on EBF rates. A consistent association between an early prenatal breastfeeding intention and improved breastfeeding outcomes has been shown among mothers in several developed countries (Dennis 2002; Labbok & Taylor 2008; Inoue et al. 2012; McAndrew et al. 2012), a relationship that has not been explored sufficiently in many developing countries.
Public health implications
Optimal breastfeeding of infants has the greatest potential to improve child health outcomes and reduce child health inequality. However, EBF rates must be high especially in high burden countries for the gains to be realised. To achieve this, it is imperative that health care providers understand the context‐specific factors that influence a mother's ability to breastfeed successfully. Although it may be difficult to directly impact certain socio‐demographic, medical and socio‐cultural barriers to EBF, knowing these barriers and other reasons why women fail to practise EBF would assist health care providers in targeting anticipatory guidance during antenatal clinics and post‐partum follow‐up visits. Breastfeeding counselling and promotion can be carried out prior to and/or early in pregnancy to promote a positive attitude and commitment to breastfeeding. Also, antenatal clinics should be packaged to deliver standardised, practical and consistent messages about the practice and benefits of EBF. Encouraging close family members to attend antenatal clinics would also help elicit support and dispel certain myths around infant feeding. Additionally, health care providers should educate working mothers on coping strategies and assist them to develop a strategic plan for breastfeeding after returning to work. They also could introduce peer‐information sharing as part of communal antenatal clinics in areas where this is practised where pregnant women can learn from the experiences of others who have been successful at breastfeeding. On a broader scale, public health authorities need to engage with relevant government sectors and policy makers to suggest labour law revisions, and enforce policies to allow working mothers from both the formal and the informal sectors to breastfeed in the workplace. Achieving the breastfeeding recommendation for optimal child growth and development might also require legislation to lengthen maternity leave to 6 months as recently passed in Vietnam. Additionally, local authorities should educate and encourage employers on the need to implement policies supportive of breastfeeding, such as on‐site child care facilities, paid breaks for breastfeeding, provision of nursing rooms at work places, flexible working schedule and policies that exempt breastfeeding mothers from duties requiring prolonged separation from their babies.
Opportunities for further research
This systematic review identifies barriers and facilitators of EBF across individual, socio‐cultural and medical environments. Important issues such as maternal characteristics, social relationships and environmental factors are major determinants of breastfeeding success. Further research could elaborate on how these characteristics and under what conditions they influence breastfeeding success. At the individual level, research could be performed to estimate the impact of preconception and early prenatal EBF plan on breastfeeding duration and exclusivity. Using validated tools, research might also explore the effect of maternal self‐confidence on optimal breastfeeding practices and perceived milk insufficiency.
Limitations
This review contains only primary research published from 2001 to 2014 among non‐HIV‐infected populations living in developing countries. Including populations with HIV would enrich the findings of this review by reflecting the mother's views of constraints arising from social factors, cultural norms, and medical and health care needs. The wide variation in the study methods and the types of study designs in the included studies precluded the possibility of conducting meta‐analysis. A meta‐analysis involving studies with prospective cohort design may further provide evidence into how much each factor contributes to EBF practice. Also, research conducted using secondary data would have provided a more in‐depth and statistically relevant summary covering a broader range of breastfeeding outcomes. Finally, studies published prior to 2001 would provide an expanded perspective of the multifactorial determinants of breastfeeding.
Conclusion
Although breastfeeding is universally practised in many developing countries, rates and duration of practice of EBF are unacceptably low due to difficulties that many mothers face. A review of past studies also makes potential areas of interventions and gaps in research apparent. Studies have revealed socio‐demographic, medical, psychosocial, cultural and environmental determinants of optimal breastfeeding practice. Health care providers should be informed about these determinants and provide specific and practical guidance targeted at overcoming these barriers. In so doing, health care providers in developing countries can make significant contribution to the improvement of maternal and child health outcomes.
Source of funding
This review received no specific funding from any agency.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
OOB and SS conceptualised the review. OOB and AD conducted the search, study selection and data extraction. All authors were involved with the interpretation of the findings. OOB wrote the manuscript with input from AA, EO, KMA and SS.
Supporting information
Table S1. Example of full search strategy for MEDLINE and PsycINFO.
Acknowledgement
We thank Sarah Krull Abe for editorial review of the manuscript.
Balogun, O. O. , Dagvadorj, A. , Anigo, K. M. , Ota, E. , and Sasaki, S. (2015) Factors influencing breastfeeding exclusivity during the first 6 months of life in developing countries: a quantitative and qualitative systematic review. Matern Child Nutr, 11: 433–451. doi: 10.1111/mcn.12180.
References
- Abuidhail J., Al‐Modallal H., Yousif R. & Almresi N. (2014) Exclusive breast feeding (EBF) in Jordan: prevalence, duration, practices, and barriers. Midwifery 30, 331–337. [DOI] [PubMed] [Google Scholar]
- Adam T., Lim S.S., Mehta S., Bhutta Z.A., Fogstad H., Mathai M. et al (2005) Cost effectiveness analysis of strategies for maternal and neonatal health in developing countries. BMJ (Clinical Research Ed.) 331, 1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agbo H.A., Envuladu E.A., Adams H.S., Inalegwu E., Okoh E., Agba A. et al (2013) Barriers and facilitators to the practice of exclusive breast feeding among working class mothers: a study of female resident doctors in tertiary health institutions in Plateau State. E3 Journal of Medical Research 2, 112–116. [Google Scholar]
- Agnarsson I., Mpello A., Gunnlaugsson G., Hofvander Y. & Greiner T. (2001) Infant feeding practices during the first six months of life in a rural area in Tanzania. East African Medical Journal 78, 9–13. [DOI] [PubMed] [Google Scholar]
- Agunbiade O.M. & Ogunleye O.V. (2012) Constraints to exclusive breastfeeding practice among breastfeeding mothers in Southwest Nigeria: implications for scaling up. International Breastfeeding Journal 7, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al‐Sahab B., Tamim H., Mumtaz G., Khawaja M., Khogali M., Afifi R. et al (2008) Predictors of breast‐feeding in a developing country: results of a prospective cohort study. Public Health Nutrition 11, 1350–1356. [DOI] [PubMed] [Google Scholar]
- Anderson J.W., Johnstone B.M. & Remley D.T. (1999) Breast‐feeding and cognitive development: a meta‐analysis. The American Journal of Clinical Nutrition 70, 525–535. [DOI] [PubMed] [Google Scholar]
- Arifeen S., Black R.E., Antelman G., Baqui A., Caulfield L. & Becker S. (2001) Exclusive breastfeeding reduces acute respiratory infection and diarrhea deaths among infants in Dhaka slums. Pediatrics 108, e67. [DOI] [PubMed] [Google Scholar]
- Arthur E.I. & Richard S.J. (2012) Breastfeeding and the use of human milk. Pediatrics 129, e827–e841. [DOI] [PubMed] [Google Scholar]
- Arusei R.J., Ettyang G.A. & Esamai F. (2011) Feeding patterns and growth of term infants in Eldoret, Kenya. Food and Nutrition Bulletin 32, 307–314. [DOI] [PubMed] [Google Scholar]
- Australian Government Department of Health and Ageing (2009) Australian Health Ministers' Conference 2009, The Australian National Breastfeeding Strategy 2010–2015. Australian Government Department of Health and Ageing: Canberra, Australia. Available at: http://www.health.gov.au/internet/main/publishing.nsf/Content/6FD59347DD67ED8FCA257BF0001CFD1E/$File/Breastfeeding_strat1015.pdf
- Baker M. & Milligan K. (2008) Maternal employment, breastfeeding, and health: evidence from maternity leave mandates. Journal of Health Economics 27, 871–887. [DOI] [PubMed] [Google Scholar]
- Barennes H., Empis G., Quang T.D., Sengkhamyong K., Phasavath P., Harimanana A. et al (2012) Breast‐milk substitutes: a new old‐threat for breastfeeding policy in developing countries. A case study in a traditionally high breastfeeding country. PLoS ONE 7, e30634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes J., Stein A., Smith T. & Pollock J. (1997) Extreme attitudes to body shape, social and psychological factors and a reluctance to breast feed. Journal of the Royal Society of Medicine 90, 551–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashour H.N., Kharouf M.H., Abdulsalam A.A., El Asmar K., Tabbaa M.A. & Cheikha S.A. (2008) Effect of postnatal home visits on maternal/infant outcomes in Syria: a randomized controlled trial. Public Health Nursing 25, 115–125. [DOI] [PubMed] [Google Scholar]
- Burr M.L., Limb E.S., Maguire M.J., Amarah L., Eldridge B.A., Layzell J.C. et al (1993) Infant feeding, wheezing, and allergy: a prospective study. Archives of Disease in Childhood 68, 724–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bystrova K., Ivanova V., Edhborg M., Matthiesen A.S., Ransjö‐Arvidson A.B., Mukhamedrakhimov R. et al (2009) Early contact versus separation: effects on mother–infant interaction one year later. Birth (Berkeley, Calif.) 36, 97–109. [DOI] [PubMed] [Google Scholar]
- Cambonie G., Rey V., Sabarros S., Baum T.P., Fournier‐Favre S., Mazurier E. et al (2010) Early postpartum discharge and breastfeeding: an observational study from France. Pediatrics International 52, 180–186. [DOI] [PubMed] [Google Scholar]
- Chandrashekhar T., Joshi H., Binu V., Shankar P., Rana M. & Ramachandran U. (2007) Breast‐feeding initiation and determinants of exclusive breast‐feeding – a questionnaire survey in an urban population of western Nepal. Public Health Nutrition 10, 192–197. [DOI] [PubMed] [Google Scholar]
- Darmstadt G.L., Bhutta Z.A., Cousens S., Adam T., Walker N. & De Bernis L. (2005) Evidence‐based, cost‐effective interventions: how many newborn babies can we save? The Lancet 365, 977–988. [DOI] [PubMed] [Google Scholar]
- Dearden K.A., Quan L.N., Do M., Marsh D.R., Pachón H., Schroeder D.G. et al (2002) Work outside the home is the primary barrier to exclusive breastfeeding in rural Viet Nam: insights from mothers who exclusively breastfed and worked. Food and Nutrition Bulletin 23, 99–106. [PubMed] [Google Scholar]
- Dennis C.L. (2002) Breastfeeding initiation and duration: a 1990–2000 literature review. Journal of Obstetric, Gynecologic, and Neonatal Nursing: JOGNN/NAACOG 31, 12–32. [DOI] [PubMed] [Google Scholar]
- Ettarh R., Van De Vijver S., Oti S. & Kyobutungi C. (2014) Overweight, obesity, and perception of body image among slum residents in Nairobi, Kenya, 2008–2009. Preventing Chronic Disease 11, E212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher J., Hammarberg K., Wynter K., McBain J., Gibson F., Boivin J. et al (2013) Assisted conception, maternal age and breastfeeding: an Australian cohort study. Acta Paediatrica 102, 970–976. [DOI] [PubMed] [Google Scholar]
- Ford R.P., Taylor B.J., Mitchell E.A., Enright S.A., Stewart A.W., Becroft D.M. et al (1993) Breastfeeding and the risk of sudden infant death syndrome. International Journal of Epidemiology 22, 885–890. [DOI] [PubMed] [Google Scholar]
- Foster S.F., Slade P. & Wilson K. (1996) Body image, maternal fetal attachment, and breast feeding. Journal of Psychosomatic Research 41, 181–184. [DOI] [PubMed] [Google Scholar]
- Gatti L. (2008) Maternal perceptions of insufficient milk supply in breastfeeding. Journal of Nursing Scholarship 40, 355–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannula L., Kaunonen M. & Tarkka M.T. (2008) A systematic review of professional support interventions for breastfeeding. Journal of Clinical Nursing 17, 1132–1143. [DOI] [PubMed] [Google Scholar]
- Heck K.E., Schoendorf K.C., Chávez G.F. & Braveman P. (2003) Does postpartum length of stay affect breastfeeding duration? A population‐based study. Birth (Berkeley, Calif.) 30, 153–159. [DOI] [PubMed] [Google Scholar]
- Holdsworth M., Gartner A., Landais E., Maire B. & Delpeuch F. (2004) Perceptions of healthy and desirable body size in urban Senegalese women. International Journal of Obesity and Related Metabolic Disorders: Journal of the International Association for the Study of Obesity 28, 1561–1568. [DOI] [PubMed] [Google Scholar]
- Horta B.L., Bahl R., Martines J.C. & Victora C.G. (2007). Evidence on the long‐term effects of breastfeeding: Systematic reviews and meta‐analyses. WHO: Geneva Switzerland. [Google Scholar]
- Horwood L.J. & Fergusson D.M. (1998) Breastfeeding and later cognitive and academic outcomes. Pediatrics 101, e9. [DOI] [PubMed] [Google Scholar]
- Howie P.W., Forsyth J.S., Ogston S.A., Clark A. & Florey C.D. (1990) Protective effect of breast feeding against infection. The BMJ 300, 11–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hruschka D.J., Sellen D.W., Stein A.D. & Martorell R. (2003) Delayed onset of lactation and risk of ending full breast‐feeding early in rural Guatemala. The Journal of Nutrition 133, 2592–2599. [DOI] [PubMed] [Google Scholar]
- Inoue M., Binns C.W., Otsuka K., Jimba M. & Matsubara M. (2012) Infant feeding practices and breastfeeding duration in Japan: a review. International Breastfeeding Journal 7, 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Labor Organization (1998) More than 120 Nations Provide Paid Maternity Leave ILO. Available at: http://www.ilo.org/global/about-the-ilo/newsroom/news/WCMS_008009/lang-en/index.htm (Accessed 15 May 2014).
- Ip S., Chung M., Raman G., Chew P., Magula N., Devine D. et al (2007) Breastfeeding and maternal and infant health outcomes in developed countries. Evidence Report/Technology Assessment 153, 1–186. [PMC free article] [PubMed] [Google Scholar]
- Johnston M.L. & Esposito N. (2007) Barriers and facilitators for breastfeeding among working women in the United States. Journal of Obstetric, Gynecologic, and Neonatal Nursing: JOGNN/NAACOG 36, 9–20. [DOI] [PubMed] [Google Scholar]
- Jones J.R., Kogan M.D., Singh G.K., Dee D.L. & Grummer‐Strawn L.M. (2011) Factors associated with exclusive breastfeeding in the United States. Pediatrics 128, 1117–1125. [DOI] [PubMed] [Google Scholar]
- Kakute P.N., Ngum J., Mitchell P., Kroll K.A., Forgwei G.W., Ngwang L.K. et al (2005) Cultural barriers to exclusive breastfeeding by mothers in a rural area of Cameroon, Africa. Journal of Midwifery & Women's Health 50, 324–328. [DOI] [PubMed] [Google Scholar]
- Karacam Z. (2008) Factors affecting exclusive breastfeeding of healthy babies aged zero to four months: a community‐based study of Turkish women. Journal of Clinical Nursing 17, 341–349. [DOI] [PubMed] [Google Scholar]
- Kramer M.S. (2010) ‘Breast is best’: the evidence. Early Human Development 86, 729–732. [DOI] [PubMed] [Google Scholar]
- Kramer M.S. & Kakuma R. (2012) Optimal duration of exclusive breastfeeding. Cochrane Database of Systematic Reviews (8), CD003517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer M.S., Guo T., Platt R.W., Sevkovskaya Z., Dzikovich I., Collet J.‐P. et al (2003) Infant growth and health outcomes associated with 3 compared with 6 mo of exclusive breastfeeding. The American Journal of Clinical Nutrition 78, 291–295. [DOI] [PubMed] [Google Scholar]
- Kwan M.L., Buffler P.A., Abrams B. & Kiley V.A. (2004) Breastfeeding and the risk of childhood leukemia: a meta‐analysis. Public Health Reports 119, 521–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labbok M. & Krasovec K. (1990) Toward consistency in breastfeeding definitions. Studies in Family Planning 21, 226–230. [PubMed] [Google Scholar]
- Labbok M.H. & Taylor E. (2008) Achieving Exclusive Breastfeeding in the United States: Findings and Recommendations. Washington, DC.
- Lanting C.I. & Boersma E.R. (1996) Lipids in infant nutrition and their impact on later development. Current Opinion in Lipidology 7, 43–47. [DOI] [PubMed] [Google Scholar]
- Leatherman S., Metcalfe M., Geissler K. & Dunford C. (2012) Integrating microfinance and health strategies: examining the evidence to inform policy and practice. Health Policy and Planning 27, 85–101. [DOI] [PubMed] [Google Scholar]
- Lim S.S., Vos T., Flaxman A.D., Danaei G., Shibuya K., Adair‐Rohani H. et al (2013) A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet 380, 2224–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas A., Morley R., Cole T., Lister G. & Leeson‐Payne C. (1992) Breast milk and subsequent intelligence quotient in children born preterm. The Lancet 339, 261–264. [DOI] [PubMed] [Google Scholar]
- Margolis L.H. & Schwartz J.B. (2000) The relationship between the timing of maternal postpartum hospital discharge and breastfeeding. Journal of Human Lactation 16, 121–128. [DOI] [PubMed] [Google Scholar]
- McAndrew F., Thompson J., Fellows L., Large A., Speed M. & Renfrew M.J. (2012) Infant feeding survey 2010. Health and Social Care Information Centre: Leeds.
- Montagu D., Yamey G., Visconti A., Harding A. & Yoong J. (2011) Where do poor women in developing countries give birth? A multi‐country analysis of demographic and health survey data. PLoS ONE 6, e17155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morley R. (1996) Diet in infancy and development outcome. Seminars in Neonatology 1, 27–34. [Google Scholar]
- Morley R., Cole T., Powell R. & Lucas A. (1988) Mother's choice to provide breast milk and developmental outcome. Archives of Disease in Childhood 63, 1382–1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nabulsi M. (2011) Why are breastfeeding rates low in Lebanon? a qualitative study. BMC Pediatrics 11, 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- do Nascimento M.B.R., Reis M.A.M., Franco S.C., Issler H., Ferraro A.A. & Grisi S.J.F. (2010) Exclusive breastfeeding in southern Brazil: prevalence and associated factors. Breastfeeding Medicine 5, 79–85. [DOI] [PubMed] [Google Scholar]
- Nawaz R., Ur Rehman S., Nawaz S. & Mohammad T. (2009) Factors causing non‐breastfeeding in children under six months of age in district Nowshera, Pakistan. Journal of Ayub Medical College, Abbottabad: JAMC 21, 93–95. [PubMed] [Google Scholar]
- Oakley L.L., Renfrew M.J., Kurinczuk J.J. & Quigley M.A. (2013) Factors associated with breastfeeding in England: an analysis by primary care trust. BMJ Open 3, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okafor I., Olatona F. & Olufemi O. (2013) Breastfeeding practices of mothers of young children in Lagos, Nigeria. Nigerian Journal of Paediatrics 41, 43–47. [Google Scholar]
- Otoo G.E., Lartey A.A. & Pérez‐Escamilla R. (2009) Perceived incentives and barriers to exclusive breastfeeding among periurban Ghanaian women. Journal of Human Lactation 25, 34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perera P.J., Ranathunga N., Fernando M.P., Sampath W. & Samaranayake G.B. (2012) Actual exclusive breastfeeding rates and determinants among a cohort of children living in Gampaha district Sri Lanka: a prospective observational study. International Breastfeeding Journal 7, 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez‐Escamilla R., Segura‐Millán S., Pollitt E. & Dewey K.G. (1992) Effect of the maternity ward system on the lactation success of low‐income urban Mexican women. Early Human Development 31, 25–40. [DOI] [PubMed] [Google Scholar]
- Ministry of Health, Labour and Welfare (2013) Promotion Committee of the ‘Healthy Families (Sukoyaka Oyako) 21’ Project Dietary Guidelines for Pregnant and Lactating Women Ministry of Health, Labour and Welfare: Tokyo (in Japanese). Available at: http://www.mhlw.go.jp/stf/houdou/0000030389.html
- Pronyk P.M., Hargreaves J.R. & Morduch J. (2007) Microfinance programs and better health: prospects for sub‐Saharan Africa. JAMA: The Journal of the American Medical Association 298, 1925–1927. [DOI] [PubMed] [Google Scholar]
- Renfrew M.J., McCormick F.M., Wade A., Quinn B. & Dowswell T. (2012) Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database of Systematic Reviews (5), CD001141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rguibi M. & Belahsen R. (2006) Body size preferences and sociocultural influences on attitudes towards obesity among Moroccan Sahraoui women. Body Image 3, 395–400. [DOI] [PubMed] [Google Scholar]
- Roter D.L. & Hall J.A. (2004) Physician gender and patient‐centered communication: a critical review of empirical research. Annual Review of Public Health 25, 497–519. [DOI] [PubMed] [Google Scholar]
- Sadauskaite‐Kuehne V., Ludvigsson J., Padaiga Z., Jasinskiene E. & Samuelsson U. (2004) Longer breastfeeding is an independent protective factor against development of type 1 diabetes mellitus in childhood. Diabetes/Metabolism Research and Reviews 20, 150–157. [DOI] [PubMed] [Google Scholar]
- Santo L.C.D.E., De Oliveira L.D. & Giugliani E.R.J. (2007) Factors associated with low incidence of exclusive breastfeeding for the first 6 months. Birth (Berkeley, Calif.) 34, 212–219. [DOI] [PubMed] [Google Scholar]
- Sasaki Y., Ali M., Kakimoto K., Saroeun O., Kanal K. & Kuroiwa C. (2010) Predictors of exclusive breast‐feeding in early infancy: a survey report from Phnom Penh, Cambodia. Journal of Pediatric Nursing 25, 463–469. [DOI] [PubMed] [Google Scholar]
- Shao Mlay R., Keddy B. & Noerager Stern P. (2004) Demands out of context: Tanzanian women combining exclusive breastfeeding with employment. Health Care for Women International 25, 242–254. [DOI] [PubMed] [Google Scholar]
- Singh J. (2013) Critical appraisal skills programme. Journal of Pharmacology & Pharmacotherapeutics 4, 76–77. [Google Scholar]
- Tamiru D., Aragu D. & Belachew T. (2013) Survey on the introduction of complementary foods to infants within the first six months and associated factors in rural communities of Jimma Arjo. International Journal of Food Sciences and Nutrition 2, 77–84. [Google Scholar]
- Thomas J. & Harden A. (2008) Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Medical Research Methodology 8, 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulak M., Chandyo R.K., Mellander L., Shrestha P.S. & Strand T.A. (2012) Infant feeding practices in Bhaktapur, Nepal: a cross‐sectional, health facility based survey. International Breastfeeding Journal 7, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations (2010) The World's Women 2010: Trends and Statistics. United Nations: New York. [Google Scholar]
- U.S. Department of Health and Human Services (2013) Healthy People 2020 Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=26 (Accessed 28 July 2014).
- Vaahtera M., Kulmala T., Hietanen A., Ndekha M., Cullinan T., Salin M.L. et al (2001) Breastfeeding and complementary feeding practices in rural Malawi. Acta Paediatrica (Oslo, Norway: 1992) 90, 328–332. [PubMed] [Google Scholar]
- Waldenström U., Sundelin C. & Lindmark G. (1987) Early and late discharge after hospital birth: breastfeeding. Acta Paediatrica 76, 727–732. [DOI] [PubMed] [Google Scholar]
- Whalen B. & Cramton R. (2010) Overcoming barriers to breastfeeding continuation and exclusivity. Current Opinion in Pediatrics 22, 655–663. [DOI] [PubMed] [Google Scholar]
- Winterburn S. & Fraser R. (2000) Does the duration of postnatal stay influence breast‐feeding rates at one month in women giving birth for the first time? A randomized control trial. Journal of Advanced Nursing 32, 1152–1157. [DOI] [PubMed] [Google Scholar]
- World Bank (2014) World Bank List of Economies 2014 World Bank. Available at: http://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=0CBwQFjAA&url=http%3A%2F%2Fsiteresources.worldbank.org%2FDATASTATISTICS2FResources2FCLASS.XLS&ei=Cce0U9y5LsK78gWY4YCoCQ&usg=AFQjCNHWuLdkFELyg0PTXBHupLnCGsB91Q&bvm=bv.70138588,d.dGc (Accessed 30 June 2014).
- World Health Organization & UNICEF (2003) Global strategy for infant and young child feeding. WHO: Geneva, Switzerland.
- Yanicki S., Hasselback P., Sandilands M. & Jensen‐Ross C. (2002) The safety of Canadian early discharge guidelines: effects of discharge timing on readmission in the first year post‐discharge and exclusive breastfeeding to four months. Canadian Journal of Public Health = Revue Canadienne de Sante'e Publique 93, 26–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Example of full search strategy for MEDLINE and PsycINFO.


