Abstract
Breastfeeding is widely endorsed as the optimal strategy for feeding newborns and young infants, as well as improving child survival and achieving Millennium Development Goal 4. Exclusive breastfeeding (EBF) for the first 6 months of life is rarely practised in South Africa. Following the 2010 World Health Organization (WHO) infant feeding recommendations (EBF for HIV‐positive mothers with maternal or infant antiretroviral treatment), South Africa adopted breastfeeding promotion as a National Infant Feeding Strategy and removed free formula milk from the Prevention of Mother‐to‐Child Transmission of HIV programme. This study aimed to explore the perceptions of mothers and household members at community level regarding the value they placed on formula feeding and circumstances that drive the practice in a peri‐urban community. We conducted in‐depth interviews with HIV‐positive and HIV‐negative mothers in a community‐randomised trial (Good Start III). Focus group discussions were held with grandmothers, fathers and teenage mothers. Data were analysed using thematic analysis. The following themes were identified; inadequate involvement of teenage mothers; grandmothers who become replacement mothers; fear of failing to practise EBF for 6 months; partners as formula providers and costly formula milk leading to risky feeding practices. The new South African Infant Feeding Strategy needs to address the gaps in key health messages and develop community‐orientated programmes with a focus on teenage mothers. These should encourage the involvement of grandmothers and fathers in decision‐making about infant feeding so that they can support EBF for optimal child survival.
Keywords: formula feeding, community perceptions, HIV, qualitative research, focus group discussion, social circumstances
Introduction
Breastfeeding is widely endorsed as the optimal strategy for feeding newborns and young infants; as well as a key strategy for improving child survival and achieving Millennium Development Goal 4 (WHO Collaborative Study Team 2000; Black et al. 2003; Stein & Kuhn 2009). Breast milk plays a major role in child growth and development, decreasing the risk of acute and chronic diseases, including diarrhoea and respiratory tract infections during infancy (Birch et al. 1993; Dewey et al. 1995).
Exclusive breastfeeding (EBF) for the first 6 months of life is rarely practised in South Africa (Tylleskar et al. 2011; Goga et al. 2012), even though the country has high rates (75–97%) of breastfeeding initiation (Ghuman et al. 2009). The South African Demographic and Health Surveys of 1998 and 2003 show that only 10% and 12%, respectively, of infants aged 0–3 months were exclusively breastfed. EBF was even lower in 4–6‐month‐old infants, at 1% and 2%, respectively (National Department of Health South Africa 1998, 2003).
In South Africa, the most common infant feeding practice is mixed feeding (Coutsoudis 2000; Doherty et al. 2006b), which carries the highest risk of exposing infants to HIV, as well as to the risk of diarrhoea and malnutrition. A cluster‐randomised trial to promote EBF in three South African communities found that while peer support doubled the frequency of EBF at 12 weeks of age (Tylleskar et al. 2011), this was from a low base (6–10%), and by this age, 20% of HIV‐negative women who had initiated breastfeeding had stopped breastfeeding and were giving formula milk (Doherty et al. 2012). This finding raises questions about the broader social constructs that promote formula feeding in South Africa, particularly in HIV‐negative women who had no access to free infant formula from health facilities.
Following the 2010 WHO infant feeding recommendations for HIV‐positive mothers to exclusively breastfeed with antiretroviral treatment for mothers or prophylaxis for infants, South Africa adopted breastfeeding promotion as the National Infant Feeding Strategy (National Department of Health South Africa 2011b, 2012). A decision was also taken to remove free formula milk from the Prevention of Mother‐to‐Child Transmission of HIV (PMTCT) programme. This change in policy created an opportunity to support all mothers to breastfeed their infants regardless of their HIV status. However, reversing years of formula feeding necessitates understanding the value mothers, household members and the community place on formula feeding and the circumstances that drive the practice. Strategies could then be developed to empower mothers and their households to commit to breastfeeding. The aim of this study was to explore mothers' and household members' perceptions, understanding of and the value they place on formula feeding, and the factors that drive it.
Key messages
In a South African disadvantaged peri‐urban setting with a high HIV prevalence, mothers transferred the motherhood role to their mothers and grandmothers while partners provided inadequate financial support leading to risky mixed formula feeding.
Teenage mothers rarely breastfed their infants due to perceived constraints such as embarrassment, loss of freedom and sagging breasts, which they associated with unattractive physical appearance and loss of boyfriends.
The new South African Infant Feeding Strategy needs to develop community‐orientated programmes that encourage the involvement of grandmothers and partners in decision‐making on infant feeding, so that they can support breastfeeding.
Subjects and methods
Setting
This qualitative study was a sub‐study of a randomised controlled trial known as Good Start III, (ISRCTN41046462), which was implemented in a township on the periphery of Durban, KwaZulu‐Natal province between 2008 and 2011. The township has an estimated population of 1 million people. HIV prevalence is estimated at 41% among women attending antenatal public health facilities (National Department of Health South Africa 2011a). The goal of the trial was to develop, evaluate and cost an integrated and scaleable package delivered in households by community health workers, targeting pregnant and post‐natal women and their newborns to provide essential maternal/newborn care, as well as support for access to PMTCT (Tomlinson et al. 2011).
Design
We used a qualitative study design, including focus group discussions (FGDs) and in‐depth interviews. The interview guide and FGDs sought responses to the following key questions: (1) What motivates mothers to use formula milk? (2) How does formula get into the households? (3) What are your views of mothers who formula feed? Two data collection methods were used because while infant feeding is personal, it is also embedded in the culture and social norms of the community, and hence group discussions were deemed a suitable forum to explore these norms. The FGDs and in‐depth interviews were conducted by two experienced interviewers/FGD facilitators, fluent in isiZulu and English.
Participants
We purposively selected 11 HIV‐positive mothers and 9 HIV‐negative mothers from the larger trial who indicated that they were formula feeding their infants under‐6 months of age. Interviewers telephonically contacted 20 grandmothers and 20 fathers related to the said HIV‐negative and HIV‐positive mothers. Out of these 20 grandmothers and 20 fathers, we selected the first 14 of each group who agreed to participate in FGDs (i.e. seven for HIV‐exposed, seven for non‐HIV‐exposed grandchildren and babies, respectively). The majority of mothers (19 out of 20), who participated in the in‐depth interviews, were 20 years old or above. However, 842 out of 3653 (23%) women who participated in the Good Start III trial were aged between 16 and 19 years and 3194 (87%) were single. To address this difference, we purposively selected 14 teenage mothers aged between 16 and 19 years who reported formula feeding their infants less than 6 months of age (Fig. 1). One father and one teenage mother declined to participate on the day of the FGDs.
Figure 1.
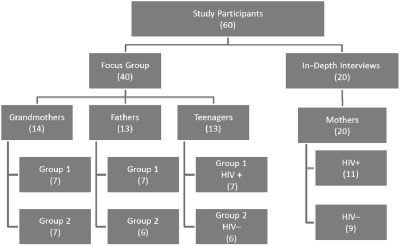
Participants' profile.
Data collection
Interviewers explained the purpose of the study during the recruitment process to each of the participant mothers, fathers and grandmothers. All interviews and FGDs were carried out at Prince Mshiyeni Memorial Hospital, from March to May 2011. The first author, who is not conversant with the isiZulu language, attended all interviews and FGDs as an observer and gained insight into the interviews and FGDs through the body language and other non‐verbal cues. Interviews lasted from 50 to 90 min and FGDs lasted from 90 to 180 min.
Ethical considerations
We obtained Ethical approval (10/09/29) from the University of the Western Cape Research and Ethics Committee and acquired signed informed consent from all participants. In order to preserve anonymity, codes were used to identify individuals in FGDs and in‐depth interviews. For the in‐depth interviews, the code denoted the participant's identification letters, the HIV status and age in years. For the FGDs, the code denoted the category of the group, the number, the identification letter for the individual in the group and the age in years. For the teenage mother's individual codes, age and HIV status were used to identify each participant and group.
Results of the study will be communicated to the community through meetings organised by the Community Health Committees.
Data analysis
Thematic analysis as described by Braun and Clarke (Braun & Clarke 2006) was used to analyse the data. The transcripts were coded, collated and grouped into themes. Data analysis was a continuous process. After each interview or FGD, the interviewers met with the first author to reflect on the findings. Gaps and new emerging questions were included in subsequent interviews and FGDs.
The voice‐recorded interviews and FGDs were transcribed verbatim and translated into English. Both the isiZulu and English versions were read several times by the interviewers/FGD facilitators and PI to ensure that the content was retained after translation. TD also read several of the transcripts to confirm the identified themes.
Trustworthiness
Multiple strategies were used to ensure trustworthiness of the research findings. Firstly, triangulation of the results from in‐depth interviews and FGDs were used to compare findings across data collection methods. In addition, four different groups of participants were included (mothers, fathers, grandmothers and teenage mothers) and information was compared across these four groups. Finally, the first author and TD identified themes independently.
Results
Sample description
The majority of the mothers in the in‐depth interviews were aged 20–25 years and 35% had a high school education. Five (38%) had completed high school, four (30%) were in tertiary institutions, three (23%) were still in high school and one had dropped out.
The majority of the fathers were aged between 24–30 years, 61% had a high school education and 60% were employed. The majority of grandmothers were aged between 50 and 59 and 77% had completed some high school. The majority of the mothers lived with their mothers and/or grandmothers. In addition, some of the teenage mothers had mothers who had been teenage mothers as well.
Themes
The analysis identified five primary themes related to social circumstances that drive formula feeding: inadequate involvement among young teenage mothers; grandmothers becoming replacement mothers; fear of failing to practise EBF for 6 months; partners as formula providers and costly formula milk leading to risky practices.
Inadequate involvement among teenage mothers
Teenage mothers' uneasiness to take on a mother's role was identified across all groups. One teenage mother confirmed that she did not spend any time with her baby. She did not know how her baby was fed or bathed and believed that care of the baby was her mother's responsibility. However, even those who spent some time with their babies tended to depend on their own mothers to raise their babies: particularly those who were still schooling.
‘I agree with other grandmothers, they do not want to breastfeed because they do not have love for their babies, although they continue having them when they are not ready to have them.’ (GMFGIF59)
‘… formula feeding is a good thing. … I was going to be stuck with my baby … I am studying I managed to continue with my school. …’ (TFG‐F19)
‘I stayed for one month then I went to school but I usually come on week‐ends or if I don't have money I come on month end’ (TFG+18)
Teenage mothers perceived breastfeeding as a constraint to their freedom that impinged on their physical appearance. Regardless of their HIV status, they associated breastfeeding with losing weight, sagging or shrinking breasts, leading to an unattractive physical appearance. They associated breastfeeding with unfashionable clothing and complained of a foul smell from clothes stained with breast milk. They were worried that they could lose their boyfriends or fail to find new ones. Resuming pre‐pregnancy lifestyles was a major priority, which led to breastfeeding avoidance. These dilemmas of being mothers but at the same time wanting to maintain a teenage lifestyle were characterised by ‘partying’ and transferring the motherhood role to their own mothers or grandmothers. All groups indicated that peer pressure lead to avoidance of breastfeeding:
‘… the second week after delivery the mother does not want to breastfeed, once she is visited by her friends they go to night clubs and you can see that the mother does not have time to breastfeed her baby the baby is yours.’ (GMFG1B48)
‘friends who do not have children are the most influential in making the wrong decisions … when the mother of your baby is pregnant some movements are cut off, and these friends are the ones who advise her not to breastfeed because she will forfeit her freedom.’ (FFG2D30)
Grandmothers becoming replacement mothers
Grandmothers described facing a triple burden. They struggled with accepting the pregnancies of their young daughters, they used their meagre pension grants to buy formula for their grandchildren, and, they took on the role of raising their grandchildren to adulthood. The tension between mothers and their daughters or granddaughters was described as disappearing when the new baby arrived. Grandmothers were extremely emotional when narrating their experiences, but at the same time they accepted their replacement mother role:
‘A grandchild becomes your own baby, therefore everything that concerns him becomes your responsibility and you cannot run away from this, no matter how annoyed you were about your daughter. When the baby arrives you forget all the negative issues. … the person who is always there ensures that the milk is there … we as grandmothers we buy the milk …’ (GMFG1D57)
‘Oh she plays a role of being a mother because she is the one who bathes her and formula feeds her … she sleeps with my mother. … in most cases she is like a mother to her’ (ZK+31)
Fear of failing to practise EBF for 6 months
Mothers were aware of the risk of HIV infection if they were unable to breastfeed their babies exclusively. However, many of them had not disclosed their HIV status to their boyfriends or mothers. A few, who had disclosed their status, feared that in their absence, the grandmothers could have fed their babies formula milk or solids, which could have resulted in the baby being infected due to the mixed feeding. Due to this hesitation, they chose formula feeding. HIV‐negative mothers who were constantly worried that they may actually be HIV positive due to their powerlessness to negotiate condom use and or having multiple sexual partners adopted the same practice:
‘Some get tested at the clinic and they are told that they are infected (HIV positive) but they do not disclose their status at home. Then they prefer formula because even if the baby can be given water or other things, it will not be infected if it is formula fed.’ (GMFG1G58)
Partners as formula providers
Mothers as well as the grandmothers expected the fathers to provide formula for their babies. The fathers' view on formula feeding and the reliability of their income did not alter this expectation in anyway. Several grandmothers lamented that some of the fathers had neglected this responsibility or only buy token formula milk sufficient for 3 days. Partners complained about struggling to get money to buy formula and being instructed to buy certain brands. Some fathers indicated that they were coerced to buy formula milk even though they would have preferred their babies to be breastfed:
‘… We are really suffering from buying formula … they know that if they breastfeed they have to spend more time at home … they can prepare the formula, leave the baby … and visit another boyfriend. …’ (FFG2A40)
‘He asked me what I will feed our baby and I said formula milk. He said if it was up to him he would have breastfed our baby, I asked why, he said breastfed baby do not get sick easily. I said a person who is breastfeeding becomes thin … so it is better to formula feed.’ (TFG‐D19)
Mothers viewed provision of formula milk by their partners as an important way of caring for the babies and keeping in contact with the fathers. However, in instances where fathers failed to provide formula milk, mothers sued for child maintenance. Mothers who were neglected by their partners indicated that formula feeding was better than breastfeeding because if they felt that they could no longer cope with the child‐care demands, they could send the babies to their partners' or their paternal grandmothers' homes, thus trying to make the fathers accountable:
‘… it is better to formula feed so that if the baby's father is giving you problems you can ‘dump’ the baby on him … fathers send their babies to rural areas to stay with their mothers.’ (TM+24)
‘I was abused when I was pregnant, I decided to formula feed. … I was angry because he was having affairs with other women. … I wanted him to know how difficult it is to take care of a baby. …’ (TM‐28)
Costly formula milk leads to risky feeding practices
Formula milk was expensive for most households. Some mothers supplemented their infant's child support grant with older children's support grants to augment formula provided by their partners. In an attempt to reduce the costs, grandmothers prepared diluted formula milk, so that a tin of formula lasted longer and fathers often bought other cheaper baby foods to replace formula milk:
‘… we do not put the correct amounts … those struggling to make ends meet … try to save the milk by reducing the quantities instead of putting the correct measurements … babies get diarrhoea. All these formula rationing, causes the baby to be weak.’ (GMF1G250)
‘My grandmother refused buying formula … she told me about my father and aunts that she breastfed them, I told her about the diseases, on her pension grant collection day she gave out money to buy formula.’ (FFG1B30)
When households completely ran out of formula milk and other commercial baby foods, they fed their babies porridge (mahewu), water, sugar water, rooibos tea or ijuba (local brew) until they could afford to buy more formula milk:
‘Others resort to black tea with only sugar added. Some use ‘mahewu’ and those who drink alcohol feed ‘ijuba’ to the babies …’ (GMF2GF58)
Discussion
To our knowledge, this is the first qualitative study that explores the social circumstances that drive formula feeding in a disadvantaged peri‐urban community in South Africa. We found that the community's awareness of breastfeeding benefits was not sufficient to motivate the mothers to breastfeed. Several underlying social factors appeared to outweigh these benefits with the result that formula feeding became the preferred infant feeding choice.
Teenagers account for a substantial number of mothers in South Africa. In the Good Start III study, teenage mothers made up 23% of the study sample. Other studies from South Africa have shown that by the age of 19, more than 30% of teenagers have given birth at least once (Kaufman et al. 2001; Varga & Brookes 2008), and teenage births make up half of all first births (Gustafsson & Worku 2007). Although unmarried daughters may be severely reprimanded for becoming pregnant, once a baby is born, it is generally welcomed into the household, and the girl usually returns to school (Preston‐Whyte et al. 1990). The South African Constitution and Schools Act of 1996 (Government of the Republic of South Africa 1996a,b) makes provision for pregnant girls to access education. The 2007 Department of Education guidelines (National Department of Education South Africa 2007) advocates for the right of pregnant girls to remain in school but suggests up to a 2‐year waiting period before girls can return to school in the interest of the rights of the child. However, girls return to school based on the households' circumstances and many do not want to miss a year of school. In our study, some girls returned to schooling as early as 1 month after delivery, and for them, this justified formula feeding. Promoting breastfeeding to teenage mothers will entail revision of the current policies, for example by allowing at least 6 months exemption from school. In addition, school curricula need to include information on the rights of infants to optimum nutrition, obligations and responsibilities of parents.
The quest for freedom was another factor that drove formula feeding in this peri‐urban context. Formula feeding removed the barriers to meeting friends, boyfriends or finding new boyfriends as well as frequenting entertainment establishments. Nelson and Sethi reported that teenage mothers in Canada were unlikely to initiate or continue breastfeeding due to lifestyle restrictions and loss of freedom associated with breastfeeding (Nelson & Sethi 2005).
Fear of losing weight, sagging breasts, breast leakages, breast milk‐stained clothes and the ‘foul’ smell of breast milk were the physical factors that teenage mothers wanted to avoid in order to convince their boyfriends and peers that little had changed in their lives. Similar findings have been reported from United Kingdom and Lebanon (Barnes et al. 1997; Nabulsi 2011). Parenting during the teenage years is complex, as developmentally, the ‘tasks of adolescence’ have not been completed, and these are compromised by additional demands of motherhood (Mercer 1980). However, several studies have identified key support strategies, including emotional, esteem, informational and network support that can be used to encourage teenage mothers to breastfeed. (Dykes et al. 2003; Quinlivan et al. 2003; Lavender & Wood 2005). In addition, the teenagers' mothers' continuous support was found to be crucial in assisting the teenager mothers in decision with regard to making infant feeding choices. (Dykes et al. 2003). These studies provide a springboard for designing targeted and culturally appropriate programmes for teenage mothers.
HIV‐positive mothers feared failing to practise EBF because many had not disclosed their HIV status for fear of being stigmatised. Others who had disclosed their status mistrusted their grandmothers to adhere to their choices. Studies have shown that going against community norms of feeding prompts questions about mothers' HIV status, unwanted disclosure and fear of stigma from partner's family and community (Perez et al. 2004; Doherty et al. 2006a). Fear expressed by these women was probably a reflection of what they had experienced or observed in their households and neighbourhoods. Disclosure in South Africa is a major challenge in HIV‐positive mothers and particularly those living in extended families due to fear of confidentiality breaches, unequal gender relations and intergenerational power relations (Brookes et al. 2004; Varga et al. 2006). Years of promoting formula feeding in an attempt to prevent MTCT of HIV by health workers have further eroded the confidence of women to breastfeed (Buskens & Jaffe 2008; Desclaux & Alfieri 2009; Koricho et al. 2010). Promotion of breastfeeding and practising EBF will only be possible if mothers feel supported by their families to disclose their HIV status. There is a need to craft community‐orientated stigma reduction programmes for PMTCT of HIV services.
In many African countries, grandmothers often make critical decisions about early child feeding practices particularly for first‐time mothers (Aubel et al. 2004; Bezner Kerr et al. 2008; Arts et al. 2011; Aubel 2012). What was novel in our study was the total transfer of the mother's role to the grandmothers. There was a perception that teenage mothers were incapable of looking after their infants; therefore, they were marginalised in their infants' feeding and care. The current model of infant feeding counselling by health care workers is directed at mothers and excludes grandmothers and fathers who often provide crucial support for infant feeding. Grandmothers may not be aware of the new infant feeding recommendation and may have based the infant feeding plan on their own experiences or traditional community norms. Data from Mozambique and Senegal have shown how grandmothers can be key players in supporting appropriate child care, including optimal infant feeding even in the context of HIV, if they are well informed and trained. In rural Ethiopia, maternal grandmothers have been credited with supporting infant nutrition and improving child survival (Aubel et al. 2004; Gibson & Mace 2005; Arts et al. 2011).
In our study, breastfeeding seemed to be the preferred infant feeding method by the majority of the fathers, but they ended up supporting formula feeding. The provision of formula milk by men was a reflection of the community's perception of their role. Data from high‐income countries have shown how fathers can have an important influence on infant feeding particularly on decision‐making whether to formula or breastfeed (Freed et al. 1992; Giugliani et al. 1994; Arora et al. 2000).
Currently, there are no strategies in South Africa for provision of regular support when breastfeeding becomes a challenge. Studies from the United Kingdom indicate that more of the same strategies that do not engage crucial family members including grandmothers in supporting breastfeeding are likely to fail (Ingram et al. 2003; Hoddinott et al. 2012). In the South African context, programmes geared to engage grandmothers and fathers in a dialogue to renegotiate infant feeding practices and strengthen commitment of household members, particularly grandmothers to support EBF, are crucial. It is crucial not only to communicate clear breastfeeding messages but also to reiterate why EBF is desirable after years of promoting formula feeding. This will be particularly important among significant others, especially grandmothers and fathers, who are presently supporting formula feeding.
South Africa could also draw on Brazil's success story, where promotion of breastfeeding through social mobilisation, including media campaigns, breastfeeding‐friendly policies and human resources training have lead to increased rates of EBF (Rea 2003).
Limitations
We explored community perceptions and understanding of mothers, grandmothers and fathers of the value they place on formula milk and circumstances that drive formula feeding in a peri‐urban community; rural dwellers may have differing views. Our sample, typical of qualitative research, was small; however, the setting, a township settlement on the outskirts of a major city, is typical of many settings in South Africa and neighbouring countries and these findings may be applicable to these similar high HIV prevalence settings.
Conclusions
The new South African Infant Feeding Strategy needs to address the gaps in key health messages and develop community‐orientated programmes with a focus on teenage mothers. These should encourage the involvement of grandmothers and fathers in decision‐making about infant feeding so that they can support breastfeeding for optimal child survival.
Sources of funding
University of Western Cape, National Research Foundation grant and the Swedish Research Council (Links programme) supported this work.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
PI participated in the conceptualisation of the study, collection, analysis & interpretation of the data, as well as writing and reviewing the manuscript. DJ, MT and LP were involved in conceptualisation of the study as well as writing and reviewing of the manuscript. TD participated in the conceptualisation of the study, analysis and interpretation of the data, as well as writing and reviewing the manuscript. DS was involved in writing and reviewing the manuscript. All authors approved the final version of the paper.
Acknowledgements
We thank all of the participants for giving of their time for these interviews and discussions.
The authors would like to acknowledge the support of Ms Vuyolwethu Magasana and Ms Sandile Madinane in data collection, and Mrs Sithembiso Mkwananzi for research administration. MT, TD and DJ are supported by the National Research Foundation, South Africa.
References
- Arora S., McJunkin C., Wehrer J. & Kuhn P. (2000) Major factors influencing breastfeeding rates: mother's perception of father's attitude and milk supply. Pediatrics 106, E67. [DOI] [PubMed] [Google Scholar]
- Arts M., Geelhoed D., De Schacht C., Prosser W., Alons C. & Pedro A. (2011) Knowledge, beliefs, and practices regarding exclusive breastfeeding of infants younger than 6 months in Mozambique: a qualitative study. Journal of Human Lactation: Official Journal of International Lactation Consultant Association 27, 25–32; quiz 63–25. [DOI] [PubMed] [Google Scholar]
- Aubel J. (2012) The role and influence of grandmothers on child nutrition: culturally designated advisors and caregivers. Maternal & Child Nutrition 8, 19–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aubel J., Toure I. & Diagne M. (2004) Senegalese grandmothers promote improved maternal and child nutrition practices: the guardians of tradition are not averse to change. Social Science & Medicine 59, 945–959. [DOI] [PubMed] [Google Scholar]
- Barnes J., Stein A., Smith T. & Pollock J.I. (1997) Extreme attitudes to body shape, social and psychological factors and a reluctance to breast feed. ALSPAC Study Team. Avon Longitudinal Study of Pregnancy and Childhood. Journal of the Royal Society of Medicine 90, 551–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bezner Kerr R., Dakishoni L., Shumba L., Msachi R. & Chirwa M. (2008) ‘We grandmothers know plenty’: breastfeeding, complementary feeding and the multifaceted role of grandmothers in Malawi. Social Science & Medicine 66, 1095–1105. [DOI] [PubMed] [Google Scholar]
- Birch E., Birch D., Hoffman D., Hale L., Everett M. & Uauy R. (1993) Breast‐feeding and optimal visual development. Journal of Pediatric Ophthalmology and Strabismus 30, 33–38. [DOI] [PubMed] [Google Scholar]
- Black R.E., Morris S.S. & Bryce J. (2003) Where and why are 10 million children dying every year? The Lancet 361, 2226–2234. [DOI] [PubMed] [Google Scholar]
- Braun V. & Clarke V. (2006) Using thematic analysis in psychology. Qualitative Research in Psychology 3, 77–101. [Google Scholar]
- Brookes H.B., Govender L., Makhura T., Moalusi C. & Varga C. (2004) Social and Community Factors Affecting PMTCT Program Efficacy and Implementation in Limpopo Province . Final study report submitted to UNICEF South Africa. Human Sciences Research Council, Durban.
- Buskens I. & Jaffe A. (2008) Demotivating infant feeding counselling encounters in southern Africa: do counsellors need more or different training? AIDS Care 20, 337–345. [DOI] [PubMed] [Google Scholar]
- Coutsoudis A. (2000) Influence of infant feeding patterns on early mother‐to‐child transmission of HIV‐1 in Durban, South Africa. Annals of the New York Academy of Sciences 918, 136–144. [DOI] [PubMed] [Google Scholar]
- Desclaux A. & Alfieri C. (2009) Counseling and choosing between infant‐feeding options: overall limits and local interpretations by health care providers and women living with HIV in resource‐poor countries (Burkina Faso, Cambodia, Cameroon). Social Science & Medicine (1982) 69, 821–829. [DOI] [PubMed] [Google Scholar]
- Dewey K.G., Heinig M.J. & Nommsen‐Rivers L.A. (1995) Differences in morbidity between breast‐fed and formula‐fed infants. The Journal of Pediatrics 126, 696–702. [DOI] [PubMed] [Google Scholar]
- Doherty T., Chopra M., Nkonki L., Jackson D. & Greiner T. (2006a) Effect of the HIV epidemic on infant feeding in South Africa: ‘When they see me coming with the tins they laugh at me’. Bulletin of the World Health Organization 84, 90–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doherty T., Chopra M., Nkonki L., Jackson D. & Persson L.A. (2006b) A longitudinal qualitative study of infant‐feeding decision making and practices among HIV‐positive women in South Africa. The Journal of Nutrition 136, 2421–2426. [DOI] [PubMed] [Google Scholar]
- Doherty T., Sanders D., Jackson D., Swanevelder S., Lombard C., Zembe W. et al (2012) Early cessation of breastfeeding amongst women in South Africa: an area needing urgent attention to improve child health. BMC Pediatrics 12, 105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dykes F., Moran V.H., Burt S. & Edwards J. (2003) Adolescent mothers and breastfeeding: experiences and support needs – an exploratory study. Journal of Human Lactation: Official Journal of International Lactation Consultant Association 19, 391–401. [DOI] [PubMed] [Google Scholar]
- Freed G.L., Fraley J.K. & Schanler R.J. (1992) Attitudes of expectant fathers regarding breast‐feeding. Pediatrics 90, 224–227. [PubMed] [Google Scholar]
- Ghuman M., Salooje H. & Morris G. (2009) Infant feeding practices in a high HIV prevalence rural district in KwaZulu‐Natal, South Africa. South African Journal of Clinical Nutrition 22, 74–79. [Google Scholar]
- Gibson A.M. & Mace R. (2005) Helpful grandmothers in rural Ethiopia: a study of the effect of kin on child survival and growth. Evolution and Human Behavior 26, 469–482. [Google Scholar]
- Giugliani E.R., Bronner Y., Caiaffa W.T., Vogelhut J., Witter F.R. & Perman J.A. (1994) Are fathers prepared to encourage their partners to breast feed? A study about fathers' knowledge of breast feeding. Acta Paediatrica 83, 1127–1131. [DOI] [PubMed] [Google Scholar]
- Goga A.E., Doherty T., Jackson D.J., Sanders D., Colvin M., Chopra M. et al (2012) Infant feeding practices at routine PMTCT sites, South Africa: results of a prospective observational study amongst HIV exposed and unexposed infants – birth to 9 months. International Breastfeeding Journal 7, 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of the Republic of South Africa (1996a) No. 84 of 1996: South African Schools Act, 1996.
- Government of the Republic of South Africa (1996b) Statutes of the Republic of South Africa‐Constitutional Law ‐Constitution of the Republic of South Africa No. 108 of 1996.
- Gustafsson S. & Worku S. (2007) Teenage Motherhood and Long‐run Outcomes in South Africa. Tinbergen Institute Discussion Paper. Tinbergen Institute: Amsterdam. [Google Scholar]
- Hoddinott P., Craig L.C., Britten J. & McInnes R.M. (2012) A serial qualitative interview study of infant feeding experiences: idealism meets realism. BMJ Open 2, e000504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingram J., Johnson D. & Hamid N. (2003) South Asian grandmothers' influence on breast feeding in Bristol. Midwifery 19, 318–327. [DOI] [PubMed] [Google Scholar]
- Kaufman C.E., de Wet T. & Stadler J. (2001) Adolescent pregnancy and parenthood in South Africa. Studies in Family Planning 32, 147–160. [DOI] [PubMed] [Google Scholar]
- Koricho A.T., Moland K.M. & Blystad A. (2010) Poisonous milk and sinful mothers: the changing meaning of breastfeeding in the wake of the HIV epidemic in Addis Ababa, Ethiopia. International Breastfeeding Journal 5, 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavender T. & Wood L. (2005) Supporting teenage mothers with breastfeeding guardians. British Journal of Midwifery 13, 354–359. [Google Scholar]
- Mercer R.T. (1980) Teenage motherhood: the first year. Part i: the teenage mother's views and responses part ii: how the infants fared. Journal of Obstetric, Gynecologic, & Neonatal Nursing 9, 16–27. [DOI] [PubMed] [Google Scholar]
- Nabulsi M. (2011) Why are breastfeeding rates low in Lebanon? A qualitative study. BMC Pediatrics 11, 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Department of Education South Africa (2007) Measures for the Prevention and Management of Learner Pregnancy.
- National Department of Health South Africa (1998) South African Demographic and Health Survey (SADHS).
- National Department of Health South Africa (2003) The South African Demographic and Health Survey (SADHS) 2003 Preliminary Report.
- National Department of Health South Africa (2011a) The 2010 National Antenatal Sentinel & Syphillis Prevalence Survey in South Africa.
- National Department of Health South Africa (2011b) Government Adopts Breastfeeding‐Only Infant Feeding Strategy: Distribution of Breast Milk Substitute through Health Facilities to be Discontinued.
- National Department of Health South Africa (2012) Strategic Plan for Maternal, Newborn, Child and Women's Health (MNCWH) and Nutrition in South Africa.
- Nelson A. & Sethi S. (2005) The breastfeeding experiences of Canadian teenage mothers. Journal of Obstetric, Gynecologic & Neonatal Nursing 34, 615–624. [DOI] [PubMed] [Google Scholar]
- Perez F., Mukotekwa T., Miller A., Orne‐Gliemann J., Glenshaw M., Chitsike I. et al (2004) Implementing a rural programme of prevention of mother‐to‐child transmission of HIV in Zimbabwe: first 18 months of experience. Tropical Medicine & International Health 9, 774–783. [DOI] [PubMed] [Google Scholar]
- Preston‐Whyte E., Zondi M., Mavundla G. & Gumede H. (1990) Teenage pregnancy, whose problem? Realities and prospects for action in KwaZulu/Natal. Southern African Journal of Demography = Suidelike Afrikaanse tydskrif vir demografie 3, 11–20. [PubMed] [Google Scholar]
- Quinlivan J.A., Box H. & Evans S.F. (2003) Postnatal home visits in teenage mothers: a randomised controlled trial. The Lancet 361, 893–900. [DOI] [PubMed] [Google Scholar]
- Rea M.F. (2003) A review of breastfeeding in Brazil and how the country has reached ten months' breastfeeding duration. Cad Saude Publica 19 (Suppl. 1), S37–S45. [DOI] [PubMed] [Google Scholar]
- Stein Z. & Kuhn L. (2009) Breast feeding: a time to craft new policies. Journal of Public Health Policy 30, 300–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlinson M., Doherty T., Jackson D., Lawn J.E., Ijumba P., Colvin M. et al (2011) An effectiveness study of an integrated, community‐based package for maternal, newborn, child and HIV care in South Africa: study protocol for a randomized controlled trial. Trials 12, 236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tylleskar T., Jackson D., Meda N., Engebretsen I.M., Chopra M., Diallo A.H. et al (2011) Exclusive breastfeeding promotion by peer counsellors in sub‐Saharan Africa (PROMISE‐EBF): a cluster‐randomised trial. The Lancet 378, 420–427. [DOI] [PubMed] [Google Scholar]
- Varga C. & Brookes H. (2008) Factors influencing teen mothers' enrollment and participation in prevention of mother‐to‐child HIV transmission services in Limpopo Province, South Africa. Qualitative Health Research 18, 786–802. [DOI] [PubMed] [Google Scholar]
- Varga C.A., Sherman G.G. & Jones S.A. (2006) HIV‐disclosure in the context of vertical transmission: HIV‐positive mothers in Johannesburg, South Africa. AIDS Care 18, 952–960. [DOI] [PubMed] [Google Scholar]
- WHO Collaborative Study Team (2000) Effect of breastfeeding on infant and child mortality due to infectious diseases in less developed countries: a pooled analysis. The Lancet 355, 451–455. [PubMed] [Google Scholar]


