Abstract
Within a Medecins Sans Frontieres's nutrition programme in Kamrangirchar slum, Dhaka, Bangladesh this study was conducted to assess the acceptability of a peanut‐based ready‐to‐use therapeutic food (RUTF) – Plumpy'nut® (PPN) among malnourished pregnant and lactating women (PLW). This was a cross‐sectional survey using semi‐structure questionnaire that included all PLW admitted in the nutrition programme, who were either malnourished or at risk of malnutrition and who had received PPN for at least 4 weeks. A total of 248 women were interviewed of whom 99.6% were at risk of malnutrition. Overall, 212 (85%) perceived a therapeutic benefit. Despite this finding, 193 (78%) women found PPN unacceptable, of whom 12 (5%) completely rejected it after 4 weeks of intake. Reasons for unacceptability included undesirable taste (60%) and unwelcome smell (43%) – more than half of the latter was due to the peanut‐based smell. Overall, 39% attributed side effects to PPN intake including nausea, vomiting, diarrhoea, abdominal distension and pain. Nearly 80% of women felt a need to improve PPN – 82% desiring a change in taste and 48% desiring a change in smell. Overall, only 146 (59%) understood the illustrated instructions on the package. Despite a perceived beneficial therapeutic effect, only two in 10 women found PPN acceptable for nutritional rehabilitation. We urge nutritional agencies and manufacturers to intensify their efforts towards developing more RUTF alternatives that have improved palatability and smell for adults and that have adequate therapeutic contents for treating malnourished PLW in Bangladesh.
Keywords: Plumpy'nut, RUTF, acceptability, pregnant and lactating women, Bangladesh
Introduction
Malnutrition prevalence among pregnant and lactating women (PLW) in Bangladesh is one of the highest in the world (WHO 2007a). The demographic health survey in 2007 showed that 30% of women in child‐bearing age (15–45 years) were undernourished (body mass index < 18.5) (NIPORT 2009). Maternal malnutrition adversely affects the health of the mother and newborn and is associated with intrauterine growth retardation and low birthweight (Black et al. 2008; Elshibly & Schmalisch 2008).
Reliance on the use of ready‐to‐use therapeutic food (RUTF) has been a key element of community‐based management approaches of uncomplicated acute malnutrition among children and adults (WHO 2007b; UNHCR 2009). One of the commonly used RUTF in Africa is Plumpy'nut® (PPN; Nutriset, Malaunay, France). It is a peanut‐based paste with milk powder, sugar, vegetables oil, minerals and vitamins. The product does not require cooking or dilution with water and is thus practical (Sandige et al. 2004). It is a microbiological safe product and can be kept under routine household conditions and without refrigeration for up to 24 months from the date of manufacture (Nutriset 2012).
Medecins Sans Frontieres (MSF) implemented a PPN‐based nutrition programme for malnourished PLW in Kamrangirchar slum setting in Dhaka, Bangladesh. During implementation, many women complained of the taste and peanut‐associated smell of PPN. The programme also experienced a high loss‐to‐follow‐up rate (25–30%) and a high non‐respondent rate (32–35%) despite women being on PPN for a period up to 5 months. It was felt that these issues might be related to intolerance of and poor acceptability of PPN, and the study was therefore conducted to assess acceptability and tolerance of PPN among PLW in Kamrangirchar slum in Bangladesh.
Key messages
Despite a perceived therapeutic benefit of peanut‐based ready‐to‐use therapeutic food (Plumpy'nut) among malnourished pregnant and lactating women (PLW), eight out of every 10 women receiving it for nutritional rehabilitation in a slum setting in Bangladesh found problems related to its acceptability.
We urge nutritional agencies and therapeutic food manufacturers to intensify their effort towards developing more ready‐to‐use therapeutic food alternatives that has improved palatability and smell for adults and that contains the adequate therapeutic contents for treating malnourished PLW in Bangladesh.
Methods
Design
This was a cross‐sectional survey using a semi‐structured questionnaire.
Study setting and study population
The study was conducted between May and July 2011 in Kamrangirchar, an urban slum setting in Dhaka, Bangladesh. The slum has an estimated population of 400 000 inhabitants living within an area of 3.1 km2. It is designated as an ‘informal setting’ and all health services are outsourced to non‐governmental organisations. MSF health services in Kamrangirchar were provided through two primary health care (PHC) clinics. The nutrition programme for PLW started in August 2010. The study included all PLW who were either malnourished or at risk of malnutrition, and who had received PPN for at least 4 weeks at the time of the study. These individuals were identified using the programme's database.
Nutritional management of malnourished PLW
The management of PLW was centred around a community‐based approach (WHO 2007b). Screening of PLW was done door‐to‐door in the community by a team of community health workers and in the PHCs screening was offered to all PLW who presented with their infants to receive preventive or curative care. PLW were admitted to the nutrition programme if they were found with severe acute malnutrition (SAM) [mid‐upper arm circumference (MUAC) <170 mm or the presence of severe nutritional oedema ≥ grade three] or were at risk of malnutrition (MUAC < 210 mm). Based on the measured MUAC threshold, PPN daily dose was prescribed (one to three packs per day) for 2–5 months. Along with the nutritional support, PLW were offered antenatal and postnatal care.
Nutritional follow‐up assessments were done monthly within the community. Women who recorded complete rejection of PPN were switched to another RUTF (BP100 – high‐energy biscuit bars). Women were discharged from the programme when they attained a MUAC > 220 mm, oedema < grade two and were assessed as being of good clinical status for at least two consecutive visits. PLW who did not recover after receiving PPN for 5 months were switched to multiple micronutrient powder (MNP) supplement.
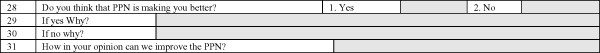
PPN acceptability survey
A semi‐structured questionnaire was used to gather socio‐demographic information, perceptions of PPN (taste, smell, consistency, colour, side effects), packaging, consumption of PPN (accepted readily, forced to ingest it, rejected completely), general appreciation of PPN and suggestions to improve it. The questionnaire included open‐ and closed‐ended questions (‘Yes’ or ‘No’ and several answers questions; Annex 1).
Three female interviewers who spoke the local language conducted the interviews using a pre‐tested questionnaire. The interviewers received training on the study approach and were independent from regular programme staff to limit responder bias. Independent home visits were arranged to conduct the interviews.
PPN was considered acceptable if PLW did not perceive problems of undesirable taste, smell, colour, consistency or side effects at any time during the course of intake. Unacceptability was defined if PLW (1) perceived any of the previously mentioned problems; (2) felt that they were being forced to take PPN; or (3) completely rejected PPN after 4 weeks of intake.
This study protocol was approved by the MSF Ethics Review Board, Geneva, Switzerland and The Union Ethics Advisory Group, Paris, France. Written informed consent was sought and obtained from all participants.
Statistical analysis
The data obtained from the semi‐structured interview were coded, and Epi Info 6.04d (CDC, Atlanta, GA, USA) was used for data entry and analysis.
Results
Characteristics of the study population
A total of 248 women [median age 20 years, inter‐quartile range (IQR) 18–24] were interviewed. The majority (99.6%) were at risk of malnutrition on admission with a median MUAC 202 mm (IQR 196–206). Overall, 161 (65%) women were pregnant and 87 (35%) were lactating. Most (99%) were married and 95% were housewives, while the remainder were daily workers. Mean household income per day was US$ 3.00 [standard deviation (SD) 2.95]. Nearly 30% were illiterate while the remainder had a mean of 4 years education (SD 3.24). The overall median period of PPN intake was 16 weeks (IQR 10–20). At interview, 134 (54%) women were receiving PPN, 101 (41%) were switched to MNP and 13 (5%) to BP100.
Overall acceptability of PPN
Fifty‐five (22%) women accepted PPN completely. The remaining 193 (78%) found PPN unacceptable, of whom 12 (5%) completely rejected PPN after 4 weeks of intake. The remaining 181 (73%) found PPN unacceptable because of undesirable taste, unwelcome smell or attributed side effects and stated that they forced themselves to take PPN.
Overall, 149 (60%) women found the PPN taste unacceptable while 107 (43%) found the smell unwelcome – more than half complaining of the peanut‐based smell (Table 1). In an attempt to compensate for the unacceptable taste and smell, 133 (54%) mixed PPN with water and seven (3%) mixed it with other food such as chapatti and rice.
Table 1.
Perception of Plumpy'nut acceptability among pregnant and lactating women in Kamrangirchar slum, Dhaka, Bangladesh
| Variable | n (%) |
|---|---|
| Total | 248 |
| Taste | |
| Acceptable | 99 (40) |
| Unacceptable | 149 (60) |
| Too sweet | 76 |
| Too salty | 68 |
| Unfamiliar taste | 5 |
| Smell | |
| Acceptable | 141 (57) |
| Unacceptable | 107 (43) |
| Strong smell of peanut | 62 |
| Medicine like smell | 27 |
| Unfamiliar smell | 18 |
| Consistency | |
| Acceptable | 217 (87) |
| Unacceptable | 31 (13) |
| Sticky | 27 |
| Oily | 4 |
| Colour | |
| Acceptable | 238 (96) |
| Unacceptable (ugly colour) | 10 (4) |
A total of 97 (39%) women reported at least one side effect attributed to PPN, which included nausea (27%), vomiting (19%), diarrhoea (8%), abdominal distension (7%) and abdominal pain (3%). Most of the reported side effects were higher among pregnant than lactating women (Table 2).
Table 2.
Perception of attributed side effects to Plumpy'nut intake among pregnant and lactating women in Kamrangirchar, Dhaka, Bangladesh
| Side effects* | Pregnant (n‐%) | Lactating (n‐%) |
|---|---|---|
| Total (n) | 161 | 87 |
| Nausea | 45 (28) | 23 (26) |
| Vomiting | 37 (23) | 11 (13) |
| Diarrhoea | 15 (9) | 4 (5) |
| Abdominal distension | 14 (9) | 2 (2) |
| Abdominal pain | 3 (2) | 4 (5) |
*More than one response by the same responder.
Despite the mentioned limitations in PPN acceptability, 212 (85%) women perceived PPN to be beneficial as a therapeutic product for improving general health. As quoted by one interviewed women ‘Before I took PPN, I used to feel weak and dizzy, now I have the strength to walk and work at home’. The majority said ‘I feel better’ and reported weight gain. Some reported specific perceived health benefits such as ‘My child is getting more breast milk’ and ‘PPN has reduced my fatigue and weakness’.
PPN packaging
The majority (99%) of women found PPN package easy to open. Overall, 146 (59%) understood the illustrated instructions on the package, 81 (33%) found the instructions inconspicuous and 21 (8%) said they were illiterate.
Suggestions for improving the acceptability of PPN
Table 3 shows PLW suggestions to improve PPN acceptability. The majority (79%) felt that the overall PPN acceptability should be improved – 82% of them desired a change in taste and 48% desired a change in smell.
Table 3.
Suggestions of the pregnant and lactating women to improve PPN acceptability, in Kamrangirchar Slum, Dhaka, Bangladesh (n‐248)
| Variable | Total (n‐%) |
|---|---|
| PPN needs to be improved | 196 (79) |
| PPN characters that need improvement* (n‐196) | |
| Taste | 160 (82) |
| Make it less sweet | 75 |
| Make it less salty | 64 |
| Add a flavour | 21 |
| Smell | 94 (48) |
| Add a new smell | 76 |
| Reduce the peanut smell | 18 |
| Consistency | 42 (21) |
| Make it more liquid | 13 |
| Make it more solid (like biscuit) | 14 |
| Make it less oily | 15 |
| Colour | 7 (4) |
| Change colour | 7 |
*More than one response by the same participant.
PPN, Plumpy'nut.
Discussion
This study shows that despite a perceived therapeutic benefit, eight of every 10 PLW receiving PPN for nutritional rehabilitation in a slum setting in Bangladesh found problems related to RUTF acceptability. The strengths of this study are: – (i) this is one of the first studies from a South Asian context assessing the acceptability of PPN among PLW, which is widely promoted as a nutritional rehabilitation product; (ii) the assessment was conducted within the framework of a routine nutritional programme; and (iii) all women eligible to participate accepted to be interviewed. This study also addresses malnutrition among PLW – a vulnerable priority group for achieving the Millennium Development Goals four and five (UN 2005). An important limitation of the study is that women who were lost‐to‐follow‐up could not be included because of the practical difficulties of tracing a generally mobile and migrant slum population. Assessing PLW adherence to PPN intake was also not in the scope of our study and will require further research.
The findings of this study raise a number of important considerations related to PPN acceptability. First, the fact that 60% of women found the taste of this ‘food product’ unacceptable is concerning. A considerable proportion also complained of its peanut‐based smell. Although peanuts are part of the staple diet in Africa, acceptability of peanut‐based RUTF in the few published studies has been variable. There was good acceptability in PLW in Ghana (Adu‐Afarwuah et al. 2011), but this was poor among malnourished HIV‐infected adults in Kenya (Dibari et al. 2011). In Bangladesh, lentils constitute the main ‘pulse’ in the basic daily diet. Although peanuts are available in the local markets and are inexpensive, they are not used routinely as part of a Bangladeshi diet (Wollinka et al. 1997). The use of peanut as a core constituent in PPN needs to be re‐examined as undesirable taste and smell of any RUTF is likely to adversely influence acceptability and adherence, which eventually impact nutritional outcomes. Second, 40% of women reported attributed side effects to PPN intake, and these were higher among pregnant than lactating women. However, there is no evidence to substantiate the direct relation between PPN and reported side effects, and this issue thus merits further assessment and research. Third, 40% of women found the illustrations on the package inconspicuous and incomprehensible, which highlights the need to find more suitable ways of communicating the ‘instructions for use’ in such communities.
In summary, the findings of this study indicate a need for possible ‘ways forward’ in better adapting (or replacing) RUTF used in contexts such as Kamrangirchar slum. As PPN is a product designed for malnourished children, the ideal would be the development of a RUTF that is adapted to adult's expressed palatability preferences and based on locally available pulses. Local recipes based on pulses (e.g. rice and lentils) such as the Khichuri exist in Bangladesh, and two studies have shown that it is effective in preventing malnutrition among children and in increasing body weight of adult women (Roy et al. 2007, 2008). However, the nutritional contents of such recipes need to be carefully assessed for their potential use for therapeutic rehabilitation in PLW. There are other RUTF alternatives that are based on local staples such as sesame and chickpeas (Valid Nutrition 2013), which were well accepted and effective among malnourished HIV‐positive adults in Malawi (Bahwere et al. 2009). However, the accessibility of these alternatives may not be the same as PPN, and there is still a need to continue supporting the use of the latter in this setting.
In conclusion, we urge nutritional agencies and therapeutic food manufacturers to intensify their effort towards developing more RUTF alternatives with improved palatability and smell for adults and with adequate therapeutic contents for treating malnourished PLW in Bangladesh.
Source of funding
The study was funded by Medecins Sans Frontieres – Brussels Operational Centre and the Ministry of Foreign Affairs, Luxembourg.
Conflicts of interest
The authors declare that they have no conflicts of interest. This study protocol was approved by the MSF Ethics Review Board, Geneva, Switzerland and The Union Ethics Advisory Group, Paris, France.
Contribution
EA, RZ, PD and PA conceptualised the study and all authors contributed to its improvement. EA, ZS and TA implemented the study. Data analysis was done by EA and RZ and all co‐authors contributed to its improvement. The first draft of the manuscript was written by EA and RZ and was critically reviewed by all co‐authors. EA and RZ handled the repeated revisions. All authors accepted the final version.
Acknowledgements
We thank MSF team working in Kamrangirchar for their support to implement the study. We are particularly grateful to the interviewers for their effort and the PLW who accepted participating in the survey.
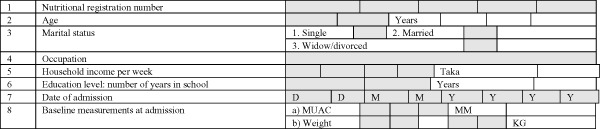
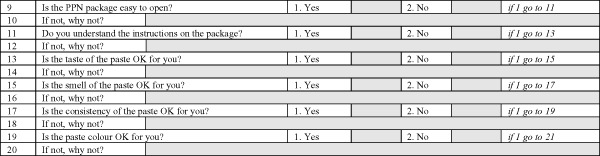
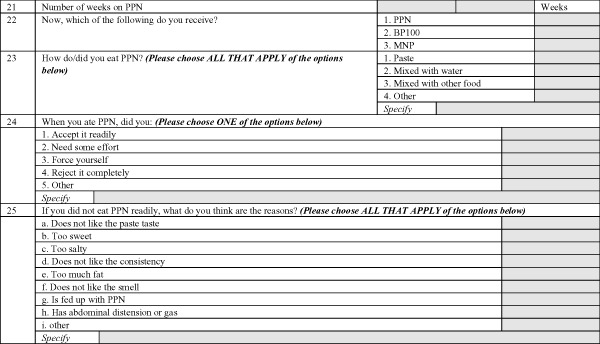
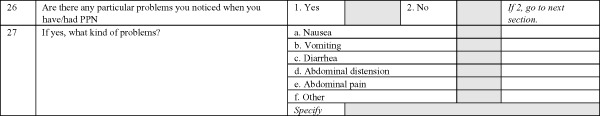
Annex: Plumpy'nut (PPN) acceptability questionnaire among pregnant and lactating women (PLW)
Section 1: demographic information
Section 2: perception of PPN acceptability
Section 3: feeding with PPN
Section 4: side effects of PPN
Section 5: general appreciation of PPN
Ali, E. , Zachariah, R. , Shams, Z. , Manzi, M. , Akter, T. , Alders, P. , Allaouna, M. , Delchevalerie, P. , and Harries, Anthony. D. (2015) Peanut‐based ready‐to‐use therapeutic food: how acceptable and tolerated is it among malnourished pregnant and lactating women in Bangladesh?. Matern Child Nutr, 11: 1028–1035. doi: 10.1111/mcn.12050.
References
- Adu‐Afarwuah S., Lartey A., Zeilani M. & Dewey K.G. (2011) Acceptability of lipid‐based nutrient supplements (LNS) among Ghanaian infants and pregnant or lactating women. Maternal & Child Nutrition 7, 344–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahwere P., Sadler K. & Collins S. (2009) Acceptability and effectiveness of chickpea sesame‐based ready‐to‐use therapeutic food in malnourished HIV‐positive adults. Patient Preference and Adherence 3, 67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black R.E., Allen L.H., Bhutta Z.A., Caulfield L.E., de Onis M., Ezzati M. et al (2008) Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 371, 243–260. [DOI] [PubMed] [Google Scholar]
- Dibari F., Bahwere P., Le Galla I., Guerrero S., Mwaniki D. & Seal A. (2011) A qualitative investigation of adherence to nutritional therapy in malnourished adult AIDS patients in Kenya. Public Health Nutrition 15, 316–311. [DOI] [PubMed] [Google Scholar]
- Elshibly E.M. & Schmalisch G. (2008) The effect of maternal anthropometric characteristics and social factors on gestational age and birth weight in Sudanese newborn infants. BMC Public Health 8, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Population Research and Training (2009) Bangladesh Demographic and Health Survey 2007. NIPORT: Dhaka, Maryland, USA. Available at: http://www.measuredhs.com/pubs/pdf/FR207/FR207%5BApril-10-2009%5D.pdf28
- Nutriset (2012) Plumpy'Nut®: Ready‐to‐Use Therapeutic Food (RUTF). Available at: http://www.nutriset.fr/en/product-range/produit-par-produit/plumpy-nut-ready-to-use-therapeutic-food-rutf.html (Accessed June 2012).
- Roy S.K., Jolly S.P., Shafique S., Fuchs G.J., Mahmud Z., Chakraborty B. et al (2007) Prevention of malnutrition among young children in rural Bangladesh by a food‐health‐care educational intervention: a randomized, controlled trial. Food Nutrition Bulletin 28, 375–383. [DOI] [PubMed] [Google Scholar]
- Roy S.K., Bilkes F., Islam K., Ara G., Tanner P., Wosk I. et al (2008) Impact of pilot project of Rural Maintenance Programme (RMP) on destitute women: CARE Bangladesh. Food Nutrition Bulletin 29, 67–75. [DOI] [PubMed] [Google Scholar]
- Sandige H., Ndekha M.J., Briend A., Ashorn P. & Manary M.J. (2004) Home‐based treatment of malnourished Malawian children with locally produced or imported ready‐to‐use food. Journal of Pediatric Gastroenterology Nutrition 39, 141–146. [DOI] [PubMed] [Google Scholar]
- United Nations (2005) The Millennium Development Goals Report. Available at: http://unstats.un.org/unsd/mi/pdf/MDG%20Book.pdf (Accessed April 2012).
- United Nations High Commissioner for Refugees (2009) Guidelines for Selective Feeding: The Management of Malnutrition in Emergencies. UNHCR: Geneva, Switzerland. Available at: http://www.ennonline.net/pool/files/ife/wfp-unhcr-sfp-guidelines.pdf (Accessed March 2012).
- Valid Nutrition (2013) Ready to Use Foods: Local Production. Available at: http://www.validnutrition.org/ready-to-use-food/production (Accessed February 2013).
- Wollinka O., Keeley E., Barton R. Burkhalter B.R. & Bashir N. (1997) Hearth Nutrition Model: Applications in Haiti, Vietnam, and Bangladesh. World Relief Corporation & BASICS Project: Arlington, USA. Available at: http://pdf.usaid.gov/pdf_docs/PNACA868.pdf (Accessed February 2013).
- World Health Organization (2007a) WHO Bangladesh Country Cooperation Strategy 2008–2013. WHO: New Delhi: Available at: http://www.ennonline.net/pool/files/ife/wfp-unhcr-sfp-guidelines.pdf (Accessed March 2012). [Google Scholar]
- World Health Organization (2007b) Community‐Based Management of Severe Acute Malnutrition: A Joint Statement by the World health Organization, the World Food Programme, the United Nations, System Standing Committee on Nutrition and the United Nations Children's Fund. WHO: Geneva, Switzerland. Available at: http://www.who.int/nutrition/topics/Statement_community_based_man_sev_acute_mal_eng.pdf5 (Accessed February 2012).


