Abstract
Intimate partner violence (IPV) is widespread; yet research is thin and equivocal regarding its potential adverse effects on infant feeding practices. With a national sample of 3552 mothers and infants aged 180 days or younger from the 2005–2006 National Family Health Survey for India, we used logistic regression to estimate the unadjusted and adjusted associations of maternal reported lifetime exposure to any IPV and to physical or sexual IPV with feeding practices at birth and in the prior 24 h. Compared with their unexposed counterparts, mothers exposed to any IPV and to any physical or sexual IPV had higher adjusted odds of giving their infant liquids [aOR 1.32, 95% confidence interval (CI) 1.04–1.66; aOR 1.37, 95% CI 1.08–1.75, respectively], and thus lower adjusted odds of exclusively breastfeeding their infant in the prior 24 h (aOR 0.78, 95% CI 0.62–0.98; aOR 0.74, 95% CI 0.58–0.95). Mothers exposed to physical or sexual IPV also had higher adjusted odds of feeding their infant solids in the prior 24 h (aOR 1.50, 95% CI 1.01–2.23). Exposure to IPV was not significantly associated with breastfeeding immediately after birth or with bottle feeding in the prior 24 h. Perinatal screening for IPV, and addressing IPV and feeding practices in exposed mothers, may improve maternal health and infant nutrition in similar settings.
Keywords: India, intimate partner violence (IPV), maternal and child health, infant feeding practices, breastfeeding, complementary feeding
Introduction
Intimate partner violence (IPV), or ‘victim/perpetrator relationships among current or former intimate partners’ (Saltzman et al. 2002), is widespread. Across diverse settings, 15–71% of ever‐partnered women have reported lifetime physical and/or sexual IPV (Ellsberg et al. 2008), and the risk of exposure is higher during and after pregnancy (Devries et al. 2010). In India, 34% of all women 15–49 years have reported some exposure to violence since age 15, two in five ever‐married women 15–49 years have reported some form of IPV (psychological, physical or sexual IPV hereafter referred to as any IPV), and the reported prevalence of any lifetime IPV varies by state, from 7% in Himachal Pradesh to 61% in Bihar [International Institute for Population Sciences (IIPS) & Macro International (MI), 2007a].
The early initiation of breastfeeding (within one hour of birth) and exclusive breastfeeding until 6 months of age are aspects of optimal breastfeeding practices [United Nations Children's Fund (UNICEF) & World Health Organization (WHO) 2003]. An estimated 1.4 million deaths to infants in poorer countries could be averted with optimal breastfeeding (Lauer et al. 2006); yet levels of early initiation and exclusive breastfeeding remain low in many countries (Black et al. 2008). In India, in 2005–2006, almost all children 0–5 years were ever breastfed (96%), but only 25% were breastfed within 1 h of birth, and this percentage varied widely across states (4–66%) (IIPS & MI 2007a). Also, less than half (46%) of infants 0–5 months and only 28% of those 4–6 months were exclusively breastfed (IIPS & MI 2007a).
In diverse settings, maternal reported exposure to IPV has been linked with poor outcomes related to child survival, health, and nutrition (Yount et al. 2011).1 Breastfeeding and complementary feeding practices are important potential links in the relationship between maternal exposure to IPV and these outcomes in children. Yet the possible effects of maternal exposure to IPV on infant feeding practices are understudied, and the limited available evidence is mixed (Yount et al. 2011).2
Scholars have proposed two competing hypotheses to explain the relationship between maternal exposure to IPV and breastfeeding. The deficit hypothesis suggests that mothers exposed to (especially physical or sexual) IPV may have behavioural or physiological difficulties with breastfeeding (Kendall‐Tackett 2007). Behaviourally, an IPV‐exposed mother may attach distressing sexual meanings to breastfeeding and the breasts (Klingelhafer 2007), engage in negative coping behaviours that are associated with the cessation of breastfeeding (Bailey & Daugherty 2007), or may be physically injured, anxious or depressed, all of which may impair her ability to breastfeed her infant (Yount et al. 2011). The compensatory hypothesis suggests that mothers exposed to IPV may be more sensitive to their child's needs and exhibit certain positive parenting behaviours, including more optimal infant feeding practices by mothers who know the recommended guidelines; however, feeding an infant foods too early may also be a compensatory response to IPV exposure, especially if certain foods are scarce and valued or if early complementary feeding is seen as beneficial. Compensatory parenting, such as becoming a more effective and responsive mother, has been observed in some mothers exposed to IPV who have preschool‐aged and younger children (Levendosky et al. 2003).
The evidence base for the association between IPV and breastfeeding practices in India is particularly limited. A cross‐sectional study of 600 mother–infant (3–5 months old) dyads in rural Andhra Pradesh, India did not detect a significant association between maternal report of physical IPV and exclusive breastfeeding; however, the results suggested that mothers with greater financial autonomy were more likely to breastfeed exclusively, and their greater decision‐making power was positively associated with infant nutritional outcomes, including weight‐for‐age z‐score (WAZ) and weight‐for‐length z‐score (WLZ) (Shroff et al. 2011). Although there is limited evidence on the relationship between IPV exposure and breastfeeding practices in India, maternal exposure to IPV has been associated with poorer nutritional outcomes, including wasting and stunting in children 12–35 months (Ackerson & Subramanian 2008), a higher risk of neonatal, perinatal and child mortality (below age five) (Ackerson & Subramanian 2009; Koenig et al. 2010), and lower rates of child immunization (Sabarwal et al. 2012). Exposure to IPV has also been shown to be negatively associated with maternal health, prenatal care and mental health in India (Kumar et al. 2005; Ackerson & Subramanian 2008; Koski et al. 2011; Mahapatro et al. 2011).
In this analysis, we use logistic regression to assess the unadjusted and adjusted associations of maternal reported lifetime exposure to either any IPV or to physical or sexual IPV with the timing of breastfeeding initiation, exclusive breastfeeding in the prior 24 h, and complementary feeding in the prior 24 h in 3552 dyads of mothers and infants ≤180 days who took part in the cross‐sectional 2005–2006 National Family Health Survey (NFHS‐3) (IIPS & MI 2007a). Given the available evidence from India linking IPV exposure with poor childhood nutrition as well as maternal autonomy with adherence to recommended breastfeeding practices, we expect to find that maternal exposure to IPV is associated with sub‐optimal infant feeding practices, consistent with the deficit hypothesis.
Key messages
Intimate partner violence (IPV) is common, but its potential adverse effects on infant feeding practices are understudied.
We assessed associations of lifetime IPV with infant feeding practices in 3552 mother–infant (≤180 days old) dyads in India.
Compared to their counterparts, mothers exposed to any IPV and to any physical–sexual IPV had higher adjusted odds of non‐exclusive breastfeeding.
Addressing IPV and its after‐effects in the perinatal period may improve infant feeding, growth and development in India and similar settings.
Materials and methods
Sample and data
The data for this study come from the 2005–2006 National Family Health Survey for India (IIPS & MI 2007a), a cross‐sectional household survey. Designed to be nationally representative with a stratified, multi‐stage probability sample design, the survey was conducted from November 2005 to August 2006. A total of 124 385 never‐ and ever‐married women 15–49 years (95% of all eligible women) received a Women's Questionnaire, which among other questions, included a birth history and detailed questions about the health, care and feeding practices of children born in the prior 5 years (IIPS & MI 2007b). Of these respondents, 83 703 (69 704 ever‐married and 13 999 never‐married women) were selected randomly to receive an IPV module, a shortened adaptation of the Revised Conflict Tactics Scale (CTS2) (Straus 1990). This module included questions about violence since age 15 for never‐ and ever‐married women, as well as questions about lifetime and prior‐year violence perpetrated by the current or most recent husband for ever‐married women.
The unit of analysis for this study is the mother‐infant dyad. To be included in the final sample, infants had to be 180 days old or younger at the time of the mother's interview, the mother had to be selected for and must have completed the IPV module, and all data on infant feeding practices and IPV had to be non‐missing. Of 256 782 total mother–child dyads documented in the birth histories, 5183 mother–infant dyads were potentially eligible for inclusion in our final sample based on the age of the infant at the time of interview (Fig. 1). Of these dyads, 3790 mothers had been selected for the IPV module, but 28 of these mothers were not interviewed because of a lack of privacy or other, unrecorded reasons. Excluding another 210 mothers with missing data on infant feeding practices or IPV yielded a final sample of 3552 mother–infant dyads.
Figure 1.
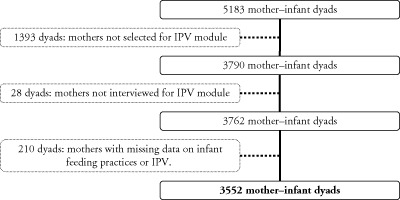
Selection of mother–infant dyads for analysis, 2005–2006 National Family Health Survey. IPV, intimate partner violence.
Compared with mothers included in the analysis, mothers who were selected for the IPV module but were excluded from this analysis because of missing data (n = 238) were more likely to have bottle‐fed their infant (41% vs. 12%, P < 0.001) and to have fed their infant liquids (91% vs. 55%, P < 0.001) or solids (52% vs. 7%, P < 0.001) in the prior 24 h. Thus, excluded mothers were less likely than included mothers to have exclusively breastfed their infant (4% vs. 45%, P < 0.001). Although the two groups did not differ on any of the covariates included in the analysis, women who had been excluded from the analysis were marginally more likely to report any physical or sexual IPV (46% vs. 36%, P = 0.058). Forty‐four mothers had missing covariate data on religion (n = 6), completed grades of schooling (n = 1), or the gap between the mother's and her husband's completed grades (n = 38). To retain these observations in the analysis, we imputed the mean value for grades of schooling and the modal value for categorical variables (i.e. religion, gap between mother's and her husband's completed grades) based on the sample with values for these variables.
Outcomes
Two of five binary outcomes measured whether (= 1) or not (= 0) the infant was breastfed: within 1 hour after birth and exclusively (without any other food, liquid, or solid) in the prior 24 h. Three complementary feeding outcomes, which are not recommended for infants this age, measured whether (= 1) or not (= 0), the infant in the prior 24 h: drank from a bottle with a nipple, ate solid or semi‐solid foods (including any meat, eggs or organs; nuts; food made from grains, roots, beans, peas or lentils; fruits or vegetables; milk products), and drank liquids other than breast milk (including plain water; tea or coffee; tinned, powdered, or fresh milk; baby formula; baby cereal; porridge or gruel).
Exposures
Two measures for exposure to IPV captured whether (= 1) or not (= 0) the mother reported any lifetime exposure to: (1) any (psychological, physical, or sexual) IPV or (2) physical or sexual IPV. These measures were constructed from separate questions about lifetime exposure to specific forms of physical IPV (slapped her; twisted her arm or pulled her hair; pushed, shook or threw something at her; punched her with his fist or with something that could hurt; kicked, dragged or beat her up; tried to choke or burn her on purpose; or threatened to attack her with a knife, gun or any other weapon), specific forms of sexual IPV (physically forced to have sexual intercourse or to perform any sexual acts), and specific forms of psychological IPV (humiliated her in front of others; threatened to hurt or harm her or someone close to her; or insulted or tried to make her feel badly about herself). We used lifetime reported IPV as the exposure rather than specifying a time frame because any such exposure has been linked with long‐term detrimental health outcomes for women and children (Yount et al. 2011).
Covariates
Covariates considered for analysis were those that may confound the relationships of interest given their associations with both IPV and infant feeding practices. These covariates included the child's gender (Mahapatro et al. 2011), child's age in months (IIPS & MI 2007a), maternal age in years (Kishor & Johnson 2004), parity excluding the index infant (Phillips et al. 2011), mother's completed grades of schooling (Ackerson et al. 2008), the difference in completed grades between the mother and her husband (mother fewer, mother and husband the same number, mother more) (Ackerson et al. 2008), mother's relationship to the head of household (wife, daughter, daughter‐in‐law, other) (Raj et al. 2011), religion (Hindu, Muslim, Other) (IIPS & MI 2007a), household wealth quintile (poorest, poor, middle, rich, richest) (IIPS & MI 2007a), urban vs. rural residence (Kishor & Johnson 2004; Senarath et al. 2010) and region (North, Northeast, East, Central, South, West) (IIPS & MI 2007a). The household wealth quintile was constructed from the score estimated from a principal components analysis of 33 items capturing ownership of a list of assets, amenities of the dwelling, and members' possession of a bank or post office account (IIPS & MI 2007a).
Analyses
Relative frequencies were calculated for all outcomes, exposure variables and covariates. Either Rao–Scott chi‐square tests or t‐tests of association, adjusting for the complex survey design, were estimated between the five feeding outcomes and exposures and between the covariates and exposures. Logistic regression then was used to assess the associations of maternal exposure to IPV and infant feeding practices. For each of the five feeding outcomes, we estimated two unadjusted logistic regression models to assess the relationship of each feeding practice with exposure to either any IPV (vs. never any IPV) or any physical or sexual IPV (vs. never physical or sexual IPV). We then estimated the same set of models adjusting for the covariates listed earlier. In sensitivity tests, we tested the inclusion of two additional covariates representing exposure to other types of violence: (1) physical violence by a parent since age 15 (slapped, kicked or anything else to hurt you physically); and (2) forced to have sexual intercourse or perform other sexual acts in either childhood or adulthood by someone other than a husband. Analyses were conducted in STATA 12.0, and standard errors were adjusted for the stratified, multistage, cluster sample design using the svy and subpop commands in STATA 12.0 and the IPV weights available in the NFHS‐3 (StataCorp 2011). Results are presented as odds ratios and 95% confidence intervals. Significant (P ≤ 0.05) and marginally significant (P ≤ 0.10) odds ratios with common patterns are discussed.
Results
Sample characteristics
On average, mothers were 24.4 years old and had 1.7 ever‐born children, excluding the index infant (Table 1). Mothers had completed a mean 4.4 grades of schooling, half had less schooling than their husband (52%), and 17% had more schooling than their husband. A majority was Hindu (79%), about one‐fourth was living in urban areas (24%) and more than half was living in the Central (31%) and Eastern (24%) regions of India. Over one‐third (39%) of mothers reported ever being exposed to any IPV, and 36% reported ever being exposed to physical or sexual IPV (Table 1). Thus, the mothers reporting any IPV and reporting physical or sexual IPV were largely overlapping. Mothers most often reported ever experiencing physical IPV (34%), followed by psychological (16%) and then sexual (12%) IPV (not shown in Table 1). Of women reporting exposure to any IPV, 74% reported experiencing such violence in the prior year, while 72% of women reporting ever exposure to physical or sexual IPV reported such violence occurring in the prior year (not shown in Table 1).
Table 1.
Descriptive analyses of maternal exposure to IPV and covariates, 3552 mother–infant dyads in India*
| Covariates | Any type of IPV † | Physical or sexual IPV | Total | ||||
|---|---|---|---|---|---|---|---|
| Never (61.1%) | Ever (38.9%) | P‐value ‡ | Never (63.8%) | Ever (36.2%) | P‐value ‡ | ||
| Urban (%) | 28.6 | 17.2 | 0.00 | 28.2 | 17.0 | 0.00 | 24.2 |
| Wealth index (%) | |||||||
| Poorest | 19.0 | 34.0 | 0.00 | 19.0 | 35.1 | 0.00 | 24.8 |
| Poorer | 19.8 | 26.9 | 20.1 | 26.9 | 22.6 | ||
| Middle | 20.4 | 19.9 | 20.3 | 19.9 | 20.2 | ||
| Richer | 21.2 | 14.3 | 21.0 | 14.0 | 18.5 | ||
| Richest | 19.7 | 4.9 | 19.5 | 4.1 | 13.9 | ||
| Parity exclusive of index child (SD) | 1.3 (1.7) | 2.3 (2.0) | 0.00 | 1.4 (1.7) | 2.4 (2.1) | 0.00 | 1.7 (1.9) |
| Mother's completed grades of schooling (SD) | 5.5 (5.1) | 2.8 (3.7) | 0.00 | 5.4 (5.1) | 2.7 (3.7) | 0.00 | 4.4 (4.8) |
| Difference in completed grades between mother and her husband (%) | |||||||
| Mother fewer grades | 53.0 | 50.6 | 0.00 | 53.4 | 49.6 | 0.00 | 52.0 |
| Same | 28.2 | 36.3 | 28.2 | 36.9 | 31.3 | ||
| Mother more grades | 18.8 | 13.2 | 18.4 | 13.5 | 16.6 | ||
| Relationship to household head | |||||||
| Wife | 37.9 | 49.8 | 0.00 | 38.0 | 50.5 | 0.00 | 42.5 |
| Daughter | 20.9 | 14.9 | 21.3 | 13.7 | 18.5 | ||
| Daughter‐in‐law | 30.1 | 25.3 | 29.9 | 25.4 | 28.2 | ||
| Other | 11.2 | 9.9 | 10.8 | 10.5 | 10.7 | ||
| Maternal age, years (SD) | 24.0 (4.9) | 25.1 (5.2) | 0.00 | 24.0 (4.9) | 25.2 (5.3) | 0.00 | 24.4 (5.1) |
| Child's age, months (SD) | 3.0 (1.7) | 3.1 (1.6) | 0.13 | 3.0 (1.7) | 3.1 (1.6) | 0.27 | 3.0 (1.7) |
| Female child (%) | 49.1 | 54.1 | 0.06 | 49.0 | 54.5 | 0.04 | 51.0 |
| Religion (%) | |||||||
| Hindu | 78.5 | 80.6 | 0.04 | 78.9 | 80.0 | 0.05 | 79.3 |
| Muslim | 16.0 | 16.5 | 15.7 | 17.1 | 16.2 | ||
| Other | 5.5 | 2.9 | 5.4 | 3.0 | 4.5 | ||
| Region (%) | |||||||
| North | 15.2 | 12.4 | 0.00 | 15.2 | 12.2 | 0.00 | 14.1 |
| Central | 27.4 | 36.2 | 28.0 | 35.9 | 30.8 | ||
| East | 19.3 | 31.3 | 19.2 | 32.4 | 24.0 | ||
| Northeast | 4.0 | 4.4 | 3.9 | 4.5 | 4.1 | ||
| South | 18.2 | 8.6 | 18.0 | 8.3 | 14.5 | ||
| West | 15.8 | 7.2 | 15.7 | 6.6 | 12.4 | ||
IPV, intimate partner violence. *Weighted values are shown. †Psychological, physical or sexual IPV. ‡Comparison between ever and never exposed to IPV, adjusted for sample design, Rao–Scott χ2 tests for categorical variables and t‐tests for interval variables. Boldface indicates significant results (P < 0.05), italics indicate marginally significant results (P < 0.10).
Compared with their unexposed counterparts, women exposed to any IPV were less often living in an urban area (17% vs. 29%), were more often in the lowest two wealth quintiles (61% vs. 39%), had higher parity excluding the index infant (2.3 vs. 1.3 children), had fewer completed grades (2.8 vs. 5.5 grades), less often had more schooling than their husband (13% vs. 19%), more often were the wife of the household head (50% vs. 38%), were older (25 vs. 24 years), more often had a female infant (54% vs. 49%), more often self‐identified as Hindu (81% vs. 79%) and more often lived in the Central and Eastern regions of India (68% vs. 47%). Similar differences were observed in the characteristics of women exposed to physical or sexual IPV in comparison to those unexposed.
Around 33% of mothers breastfed within 1 h of birth, and this percentage was lower among mothers who were exposed to IPV than among those who were unexposed (29% vs. 35%, Table 2). The practice of bottle feeding with a nipple in the prior 24 h did not differ by IPV exposure status (12%). More than half of all mothers fed their infant other liquids in the prior 24 h (55%), and mothers exposed to any IPV and to any physical or sexual IPV engaged in this practice marginally more often than their counterparts (57% vs. 53% and 58% vs. 53%, respectively). Few mothers (7%) fed their infant solid foods in the prior 24 h, and this practice did not differ significantly by exposure to IPV (Table 2). Around 45% of mothers reported exclusively breastfeeding their infant in the prior 24 h, and this percentage was marginally lower among mothers exposed to physical or sexual IPV than their counterparts (42% vs. 47%). Almost all infants were being breastfed at the time of the survey (99%) (not shown in Table 2).
Table 2.
Descriptive analyses of maternal exposure to IPV and infant feeding practices, 3552 mother‐infant dyads in India*
| Outcomes | Any type of IPV † | Any physical or sexual IPV | Total | ||||
|---|---|---|---|---|---|---|---|
| Never (61.1%) | Ever (38.9%) | Rao–Scott χ2 P‐value ‡ | Never (63.8%) | Ever (36.2%) | Rao–Scott χ2 P‐value ‡ | ||
| Breastfed immediately after birth (within 1 h) (%) | 34.6 | 29.4 | 0.03 | 34.5 | 29.2 | 0.03 | 32.6 |
| Drank from a bottle with a nipple in the past 24 h (%) | 12.2 | 12.0 | 0.88 | 11.9 | 12.5 | 0.73 | 12.1 |
| Fed liquids in the prior 24 h (%) | 53.0 | 57.4 | 0.09 | 52.9 | 57.8 | 0.07 | 54.7 |
| Fed solids in the prior 24 h (%) | 6.6 | 7.4 | 0.48 | 6.4 | 7.8 | 0.22 | 6.9 |
| Exclusively breastfed in the prior 24 h (%) | 46.4 | 42.3 | 0.11 | 46.5 | 41.9 | 0.09 | 44.8 |
IPV, intimate partner violence. *Weighted values are shown. †Psychological, physical or sexual IPV. ‡Comparison between ever and never experiencing IPV, adjusted for sample design. Boldface indicates significant results (P < 0.05), italics indicate marginally significant results (P < 0.10).
Regression results
Compared with their counterparts, mothers exposed to any IPV and to physical or sexual IPV had lower unadjusted odds of breastfeeding immediately after birth (ORs = 0.79 and 0.78 respectively, P = 0.026) and marginally higher unadjusted odds of feeding liquids in the prior 24 h (ORs = 1.19 and 1.22, P ≤ 0.088) (Table 3). Mothers exposed to physical or sexual IPV had marginally lower unadjusted odds of exclusively breastfeeding in the prior 24 h (OR = 0.83, P = 0.090) (Table 3).
Table 3.
Associations of maternal reported exposure to IPV with infant feeding practices, 3552 mother–infant dyads in India*
| Outcomes | Unadjusted | Adjusted † | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P‐value ‡ | OR | 95% CI | P‐value ‡ | |
| Ever any IPV = 1 (ref: never any IPV = 0) | ||||||
| Breastfed immediately after birth (within 1 h) | 0.79 | (0.63, 0.97) | 0.026 | 1.04 | (0.82, 1.33) | 0.717 |
| Drank from a bottle with a nipple in the past 24 h | 0.98 | (0.70, 1.36) | 0.884 | 1.18 | (0.83, 1.67) | 0.367 |
| Fed liquids in the prior 24 h | 1.19 | (0.97, 1.46) | 0.088 | 1.32 | (1.04, 1.66) | 0.021 |
| Fed solids in the prior 24 h | 1.13 | (0.80, 1.60) | 0.484 | 1.31 | (0.89, 1.94) | 0.176 |
| Exclusively breastfed in the prior 24 h | 0.85 | (0.69, 1.04) | 0.114 | 0.78 | (0.62, 0.98) | 0.034 |
| Ever any physical or sexual IPV = 1 (ref: never physical or sexual IPV = 0) | ||||||
| Breastfed immediately after birth (within 1 h) | 0.78 | (0.63, 0.97) | 0.026 | 1.04 | (0.82, 1.32) | 0.756 |
| Drank from a bottle with a nipple in the past 24 h | 1.06 | (0.76, 1.49) | 0.727 | 1.33 | (0.93, 1.91) | 0.121 |
| Fed liquids in the prior 24 h | 1.22 | (0.98, 1.51) | 0.072 | 1.37 | (1.08, 1.75) | 0.011 |
| Fed solids in the prior 24 h | 1.24 | (0.88, 1.76) | 0.222 | 1.50 | (1.01, 2.23) | 0.046 |
| Exclusively breastfed in the prior 24 h | 0.83 | (0.67, 1.03) | 0.090 | 0.74 | (0.58, 0.95) | 0.017 |
IPV, intimate partner violence; OR, odds ratio; CI, confidence intervals. *Models are adjusted for the stratified, cluster sample design. †Covariates include urban/rural residence; household wealth quintile; maternal age in years; child's age in months; parity exclusive of index child; mother's completed grades of schooling; the difference in completed grades between the mother and her husband; mother's relationship to household head; gender of child; maternal religion; and region of residence. ‡Boldface indicates significant results (P < 0.05), italics indicate marginally significant results (P < 0.10).
In general, the relationships of exposure to IPV and feeding practices became stronger with adjustment for covariates. Compared with their unexposed counterparts, mothers exposed to any IPV and to physical or sexual IPV, respectively, had lower adjusted odds of exclusively breastfeeding their infant (aORs = 0.78 and 0.74 respectively, P ≤ 0.034), as well as higher adjusted odds of giving their infant liquids (aORs = 1.32 and 1.37 respectively, P ≤ 0.021). Mothers exposed to physical or sexual IPV also had higher adjusted odds than their counterparts of feeding their infant solids (aOR = 1.50, P = 0.046) in this period. The adjusted odds of breastfeeding immediately after birth and of bottle feeding did not differ with exposure to either measure of IPV.
Computing the average marginal effect (AME) of exposure to any IPV on the probability of feeding an infant liquids suggests that exposure to any IPV increases the probability of feeding liquids by 5.6 percentage points (predicted probability of feeding liquids 58.1% for those exposed vs. 52.5% for those unexposed); whereas exposure to physical or sexual IPV increases the probability of feeding liquids by 6.4 percentage points (58.7% for those exposed vs. 52.3% for those unexposed).3 In comparison, the AME of exposure to any IPV on the probability of feeding solids is 1.6 percentage points (7.9% for those exposed vs. 6.3% for those unexposed), and the AME of exposure to physical or sexual IPV on feeding solids is 2.4 percentage points (8.5% for those exposed vs. 6.1% for those unexposed). Thus, exposure to IPV is associated with an increased risk of engaging in non‐exclusive breastfeeding, mainly as a result of feeding infants liquids because few women reported feeding infants solid foods in the prior 24 h (6.9%).
We tested the sensitivity of our results to the inclusion of other indicators of physical violence: exposure to physical violence by parents after age 15 and forced sexual acts by someone other than a husband in either childhood or adulthood (results available upon request). Very few mothers in the sample reported exposure to forced sexual acts by someone other than a husband (<1%), and a small number reported exposure to physical violence at the hands of a parent after age 15 (4%). In general, the inclusion of these covariates did not substantially alter the estimated association of exposure to any IPV or to physical or sexual IPV with breastfeeding outcomes. Although some models indicated a significant association between exposure to forced sexual acts by someone other than a husband and negative breastfeeding behaviours, these results should be interpreted cautiously as few women reported exposure to this type of violence.
Discussion
IPV is a global problem that adversely affects maternal and child health. This paper examined the unadjusted and adjusted associations of maternal exposure to IPV with infant feeding practices, an important topic given high rates of IPV, sub‐optimal feeding practices, and scant and equivocal findings regarding their potential links. This analysis extends the evidence base in several ways. First, we focus on the case of India, a diverse country in which one‐third of the world's malnourished children live (You et al. 2011). Second, we leverage a large, nationally representative sample of mother–infant dyads, which addresses the small sample sizes of most prior studies. Third, we examine two measures for lifetime exposure to IPV, a global measure capturing any prior physical, sexual or psychological IPV, and a specific measure capturing any prior physical or sexual IPV. Our specification of global and specific forms of IPV addresses the tendency of prior research to not state the form of IPV under study or to focus only on physical or sexual forms (Yount et al. 2011). Finally, we consider multiple feeding practices, including ones previously studied (the initiation of breastfeeding) and others never studied, such as the timing of initiation, exclusive breastfeeding and multiple (non‐recommended) complementary feeding practices (Yount et al. 2011).
On the one hand, the combined lower adjusted odds of exclusive breastfeeding among mothers exposed to IPV and their higher adjusted odds of providing other liquids or foods are consistent with the deficit hypothesis. Following this interpretation, mothers exposed to IPV may be less able physiologically or behaviourally to breastfeed exclusively and so rely on complementary foods to nourish their infants. On the other hand, these results could also be viewed as consistent with the compensatory hypothesis if women exposed to IPV are unaware of the guidelines for infant feeding and tend to feed their children complementary foods that are scarce or valued in the local context. Yet additional analyses showed that mothers exposed to IPV were not more likely to feed their infant potentially valued foods, such as baby food (results available upon request). Thus, collectively, our results corroborate a deficit model for the effects of maternal exposure to IPV on infant feeding practices and highlight the potentially important intergenerational effects of IPV at a critical stage of early childhood, with potential long‐term effects on the well‐being of exposed children, their families and the larger society.
Notably, our reliance on cross‐sectional retrospective maternal reports of IPV and infant feeding practices precludes causal inferences. Still, most adjusted associations were highly significant and persisted despite potential selection and response effects that would likely bias associations towards the null. Specifically, women who were excluded from the analysis because of missing data on IPV or breastfeeding behaviours were more likely to engage in non‐recommended breastfeeding practices and were marginally more likely to be exposed to physical or sexual IPV. These patterns, and the possible nondisclosure of exposure to IPV by some mothers in the analysis, suggest that our estimates may reflect lower bounds for the effects of maternal exposure to IPV and engagement in non‐recommended infant feeding practices.
Because the NFHS‐3 collected data on exclusive breastfeeding using a 24 h recall, we were unable to determine the association between IPV exposure and engagement in exclusive breastfeeding for the full first 6 months of life or between IPV exposure and the precise timing of the introduction of non‐recommended foods. The reliability of the measure of exclusive breastfeeding was improved by the inclusion of a detailed foods list in the NFHS‐3; nevertheless, greater insights into the relationship between maternal exposure to IPV and infant feeding practices could be gained by collecting more detailed measures for the consumption of breast milk, other liquids and solid foods in the prior 24 h, and by using calendar methods to identify the duration of exclusive breastfeeding and the timing of the first introduction of other liquids and solid foods. Longitudinal studies of IPV‐exposed and unexposed mother–infant pairs in which biomarkers of maternal and infant stress, breast milk volume, and breast‐milk composition are collected with observations and reports of maternal and infant behaviour would clarify biological and behavioural causal pathways, mothers' rationales for selected feeding practices, and the role of infant feeding as a mediator between IPV and child growth (Yount et al. 2011).
Other relationships that warrant study are those between maternal exposure to IPV, their autonomy and feeding practices. In India, a husband's controlling behaviour has been strongly associated with his perpetration of IPV (Dalal & Lindqvist 2012), and enhanced maternal autonomy in decision‐making may be positively associated with infant feeding practices in rural areas (Shroff et al. 2011). This pathway may be relevant in parts of India and other South, East and Southeast Asian settings, where more rigid forms of patriarchy persist (Kandiyoti 1988). Although India is a large and diverse country in which the population of malnourished children reflects a high percentage of the malnourished children globally, similar research is needed to corroborate or refute our findings in other contexts.
Optimal infant feeding practices help to ensure appropriate nutrition in early life, which is essential for healthy growth and development (Kramer & Kakuma 2004). This research underscores the intergenerational consequences of maternal exposure to IPV and suggests a programmatic need to screen perinatally for IPV in poor settings to identify mothers at higher risk of non‐exclusive breastfeeding, as well as non‐recommended complementary feeding practices. Support to mothers should include not only the promotion of optimal feeding practices (UNICEF & WHO 2003), but also efforts to mitigate IPV and the physiological stress that may ensue from exposure (Woods et al. 2005). Success in these efforts would enhance maternal–infant interactions in ways that would further support optimal infant feeding practices.
Source of funding
None.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
KMY initiated the idea for this research as part of her research programme on the intergenerational effects of intimate partner violence. SZ‐B and KL prepared the data and conducted the statistical analysis. All authors contributed to the study design and writing of the manuscript. All authors read and approved the final version.
Acknowledgements
This paper is based on the Masters of Public Health thesis that Ms. Kayla Lavilla completed while she was a graduate student working under the direction of the corresponding author in the Hubert Department of Global Health at the Rollins School of Public Health, Emory University.
Zureick‐Brown, S. , Lavilla, K. , and Yount, K. M. (2015) Intimate partner violence and infant feeding practices in India: a cross‐sectional study. Matern Child Nutr, 11: 792–802. doi: 10.1111/mcn.12057.
Footnotes
Data on exposure to IPV for the literature cited here typically comes from women's self‐report as does the data on IPV used in the analysis presented in this paper. Hereafter, ‘reported exposure’ is implied in all references to IPV exposure.
In an extensive review of the literature, Yount et al. (2011) identified only eight studies that have assessed maternal exposure to IPV and infant feeding practices, of which most (six) were based on cross‐sectional designs and small, purposive samples. Two case studies, from Australia and Brazil, revealed mixed experiences of breastfeeding in mothers exposed to IPV (Heads 2007; Lourenço & Deslandes 2008). One cross‐sectional, facility‐based study in Hong Kong suggested that exposure to IPV in pregnancy was negatively associated with the initiation of breastfeeding (Lau & Chan 2007); whereas a small, cross‐sectional, facility‐based study in the United States found no association between exposure to physical or sexual IPV and either the initiation or duration of breastfeeding (Bullock et al. 2001). Using data from a large (n = 118 579) cross‐sectional study of women participating in the Pregnancy Risk Assessment Monitoring System in the United States, Silverman et al. (2006) found that women exposed to IPV in pregnancy were less likely than unexposed women to initiate breastfeeding and were more likely to cease breastfeeding (at 4 weeks after birth); however, these relationships were not statistically significant after adjusting for smoking status and demographic measures. In one prospective cohort study, maternal exposure to IPV was negatively associated with engagement in any breastfeeding 6 weeks after birth, but information about IPV was not systematically collected, and potential confounders were not controlled (Acheson 1995).
The average marginal effect is calculated by computing the marginal effect for each respondent [i.e. the difference in predicted probabilities of engaging in a particular infant feeding practice assuming the individual reported exposure to IPV (= 1) vs. did not report exposure to IPV (= 0)] and averaging these marginal effects across the sample.
References
- Acheson L. (1995) Family violence and breast‐feeding. Archives of Family Medicine 4, 650–652. [DOI] [PubMed] [Google Scholar]
- Ackerson L.K. & Subramanian S.V. (2008) Domestic violence and chronic malnutrition among women and children in India. American Journal of Epidemiology 167, 1188–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ackerson L.K. & Subramanian S.V. (2009) Intimate partner violence and death among infants and children in India. Pediatrics 124, e878–e889. [DOI] [PubMed] [Google Scholar]
- Ackerson L.K., Kawachi I., Barbeau E.M. & Subramanian S.V. (2008) Effects of individual and proximate educational context on intimate partner violence: a population‐based study of women in India. American Journal of Public Health 98, 507–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey B.A. & Daugherty R.A. (2007) Intimate partner violence during pregnancy: incidence and associated health behaviors in a rural population. Maternal and Child Health Journal 11, 495–503. [DOI] [PubMed] [Google Scholar]
- Black R.E., Allen L.H., Bhutta Z.A., Caulfield L.E., de Onis M., Ezzati M. et al (2008) Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 371, 243–260. [DOI] [PubMed] [Google Scholar]
- Bullock L.F., Libbus M.K. & Sable M.R. (2001) Battering and breastfeeding in a WIC population. The Canadian Journal of Nursing Research 32, 43–56. [PubMed] [Google Scholar]
- Dalal K. & Lindqvist K. (2012) A national study of the prevalence and correlates of domestic violence among women in India. Asia‐Pacific Journal of Public Health 24, 265–277. [DOI] [PubMed] [Google Scholar]
- Devries K.M., Kishor S., Johnson H., Stockl H., Bacchus L.J., Garcia‐Moreno C. et al (2010) Intimate partner violence during pregnancy: analysis of prevalence data from 19 countries. Reproductive Health Matters 18, 158–170. [DOI] [PubMed] [Google Scholar]
- Ellsberg M., Jansen H.A., Heise L., Watts C.H. & Garcia‐Moreno C. (2008) Intimate partner violence and women's physical and mental health in the WHO multi‐country study on women's health and domestic violence: an observational study. Lancet 371, 1165–1172. [DOI] [PubMed] [Google Scholar]
- Heads J. (2007) Letter to the editor. Journal of Human Lactation 23, 313. [DOI] [PubMed] [Google Scholar]
- International Institute for Population Sciences (IIPS) & Macro International (MI) (2007a) National Family Health Survey (NFHS‐3), 2005–06: India: Volume I. IIPS: Mumbai. [Google Scholar]
- International Institute for Population Sciences (IIPS) & Macro International (MI) (2007b) National Family Health Survey (NFHS‐3), 2005–06: India: Volume II. IIPS: Mumbai. [Google Scholar]
- Kandiyoti D. (1988) Bargaining with patriarchy. Gender and Society 2, 274–290. [Google Scholar]
- Kendall‐Tackett K.A. (2007) Violence against women and the perinatal period: the impact of lifetime violence and abuse on pregnancy, postpartum, and breastfeeding. Trauma, Violence and Abuse 8, 344–353. [DOI] [PubMed] [Google Scholar]
- Kishor S. & Johnson K. (2004) Profiling Domestic Violence – A Multi‐Country Study. ORC Macro: Calverton, MD. [Google Scholar]
- Klingelhafer S.K. (2007) Sexual abuse and breastfeeding. Journal of Human Lactation 23, 194–197. [DOI] [PubMed] [Google Scholar]
- Koenig M.A., Stephenson R., Acharya R., Barrick L., Ahmed S. & Hindin M. (2010) Domestic violence and early childhood mortality in rural India: evidence fromprospective data. International Journal of Epidemiology 39, 825–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koski A.D., Stephenson R. & Koenig M.R. (2011) Physical violence by partner during pregnancy and use of prenatal care in rural India. Journal of Health, Population, and Nutrition 29, 245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer M.S. & Kakuma R. (2004) The optimal duration of exclusive breastfeeding: a systematic review. Advances in Experimental Medicine and Biology 554, 63–77. [DOI] [PubMed] [Google Scholar]
- Kumar S., Jeyaseelan L., Suresh S. & Ahuja R.C. (2005) Domestic violence and its mental health correlates in Indian women. The British Journal of Psychiatry 187, 62–67. [DOI] [PubMed] [Google Scholar]
- Lau Y. & Chan K.S. (2007) Influence of intimate partner violence during pregnancy and early postpartum depressive symptoms on breastfeeding among Chinese women in Hong Kong. Journal of Midwifery & Women's Health 52, E15–E20. [DOI] [PubMed] [Google Scholar]
- Lauer J.A., Betran A.P., Barros A.J.D. & de Onis M. (2006) Deaths and years of life lost due to suboptimal breast‐feeding among children in the developing world: a global ecological risk assessment. Public Health Nutrition 9, 673–685. [DOI] [PubMed] [Google Scholar]
- Levendosky A.A., Huth‐Bocks A.C., Shapiro D.L. & Semel M.A. (2003) The impact of domestic violence on the maternal‐child relationship and preschool‐age children's functioning. Journal of Family Psychology 17, 275–287. [DOI] [PubMed] [Google Scholar]
- Lourenço M.A. & Deslandes S.F. (2008) Maternal care and breastfeeding experience of women suffering intimate partner violence. Revista de Saúde Pública 42, 615–621. [DOI] [PubMed] [Google Scholar]
- Mahapatro M., Gupta R.N., Gupta V. & Kundu A.S. (2011) Domestic violence during pregnancy in India. Journal of Interpersonal Violence 26, 2973–2990. [DOI] [PubMed] [Google Scholar]
- Phillips G., Brett K. & Mendola P. (2011) Previous breastfeeding practices and duration of exclusive breastfeeding in the United States. Maternal and Child Health Journal 15, 1210–1216. [DOI] [PubMed] [Google Scholar]
- Raj A., Sabarwal S., Decker M.R., Nair S., Jethva M., Krishnan S. et al (2011) Abuse from in‐laws during pregnancy and post‐partum: qualitative and quantitative findings from low‐income mothers of infants in Mumbai, India. Maternal and Child Health Journal 15, 700–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabarwal S., McCormick M.C., Silverman J.G. & Subramanian S.V. (2012) Association between maternal intimate partner violence victimization and childhood immunization in India. Journal of Tropical Pediatrics 58, 107–113. [DOI] [PubMed] [Google Scholar]
- Saltzman L.E., Fanslow J.L., McMahon P.M. & Shelley G.A. (2002) Intimate Partner Violence Surveillance: Uniform Definitions and Recommended Data Elements, Version 1.0. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control: Atlanta, GA. [Google Scholar]
- Senarath U., Dibley M.J., Godakandage S.S., Jayawickrama H., Wickramasinghe A. & Agho K.E. (2010) Determinants of infant and young child feeding practices in Sri Lanka: secondary data analysis of Demographic and Health Survey 2000. Food and Nutrition Bulletin 31, 352–365. [DOI] [PubMed] [Google Scholar]
- Shroff M.R., Griffiths P.L., Suchindran C., Nagalla B., Vazir S. & Bentley M.E. (2011) Does maternal autonomy influence feeding practices and infant growth in rural India? Social Science & Medicine 73, 447–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman J.G., Decker M.R., Reed E. & Raj A. (2006) Intimate partner violence around the time of pregnancy: association with breastfeeding behavior. Journal of Women's Health (Larchmont) 15, 934–940. [DOI] [PubMed] [Google Scholar]
- StataCorp (2011) Stata Statistical Software: Release 12. StataCorp LP: College Station, TX. [Google Scholar]
- Straus M.A. (1990) The Conflict Tactics Scale and its critics: An evaluation and new data on validity and reliability In: Physical Violence in American Families: Risk Factors and Adaptations to Violence in 8,145 Families (eds Straus M.A. & Gelles R.J., edited with the assistance of C. Smith), pp 49–73. Transaction Publishing: New Brunswick, NJ. [Google Scholar]
- United Nations Children's Fund (UNICEF) & World Health Organization (WHO) (2003) Global Strategy for Infant and Young Child Feeding. United Nations Children's Fund/World Health Organization: Geneva, Switzerland. [Google Scholar]
- Woods A.B., Page G.G., O'Campo P., Pugh L.C., Ford D. & Campbell J.C. (2005) The mediation effect of posttraumatic stress disorder symptoms on the relationship of intimate partner violence and IFN‐γ levels. American Journal of Community Psychology 36, 159–175. [DOI] [PubMed] [Google Scholar]
- You D., Jones G. & Wardlaw T. (2011) Levels & Trends in Child Mortality: Report 2011. United Nations Inter‐Agency Group for Child Mortality Estimation (IGME): New York. [Google Scholar]
- Yount K.M., DiGirolamo A.M. & Ramakrishnan U. (2011) Impacts of domestic violence on child growth and nutrition: a conceptual review of the pathways of influence. Social Science & Medicine 72, 1534–1554. [DOI] [PubMed] [Google Scholar]


