Abstract
The increase in overweight and obesity among women is a growing concern, and reproduction is associated with persistent weight gain. We have shown that dietary behavioural modification treatment, with or without exercise, results in weight loss and maintenance of weight loss. The aim of this study was to provide an explanatory model of how overweight and obese women achieve weight loss during, and after, participating in a post‐partum diet and/or exercise intervention. Using Grounded Theory, we performed and analysed 29 interviews with 21 women in a 12‐week Swedish post‐partum lifestyle intervention with a 9‐month follow‐up. Interviews were made after the intervention and at the 9‐month follow‐up. To overcome initial barriers to weight loss, the women needed a ‘Catalytic Interaction’ (CI) from the care provider. It depended on individualised, concrete, specific and useful information, and an emotional bond through joint commitment, trust and accountability. Weight loss was underpinned by gradual introduction of conventional health behaviours. However, the implementation depended on the experience of the core category process ‘Transformative Lifestyle Change’ (TLC). This developed through a transformative process of reciprocal changes in cognitions, emotions, body, environment, behaviours and perceived self. Women accomplishing the stages of the TLC process were successful in weight loss, in contrast to those who did not. The TLC process, dependent on initiation through CI, led to implementation and integration of recognised health behaviours, resulting in sustainable weight loss. The TLC model, including the CI construct and definition of barriers, facilitators and strategies provides an explanatory model of this process.
Keywords: behaviour change, exercise, Grounded Theory, diet, obesity/overweight, weight management
Background
The past decade's epidemic increase of overweight and obesity among women of childbearing age is of growing concern in relation to maternal and child health (Socialstyrelsen 2005; Siega‐Riz & Laraia 2006; ‘Health Survey for England 2007’, National Statistics 2008). Childbearing is associated with persistent weight gain due to gestational weight gain and post‐partum weight retention, which may exacerbate overweight and associated conditions for women entering pregnancy overweight (Harris & Ellison 1997; Gunderson & Abrams 2000; Abrams et al. 2013). Weight retention leading to or increasing overweight or obesity after pregnancy increases the risk of gestational diabetes, short duration of or failure to initiate breastfeeding, as well as complications during subsequent pregnancies (Linne et al. 2002; Amir & Donath 2007; Institute of Medicine/National Research Council 2009). For women with multiple pregnancies, the consequences of overweight or obesity and associated conditions may be intensified with each subsequent pregnancy (Gore et al. 2003). Weight gain also increases future risk of cardiovascular disease, type 2 diabetes and cancer (Rooney & Schauberger 2002). However, these risks are significantly reduced if women return to their pre‐pregnancy weight by 6 months post‐partum (Rooney & Schauberger 2002).
Many women wish to lose weight in the post‐partum period and experience increased motivation from becoming a parent (Bastian et al. 2010). At the time of commencing our trial, only three randomised, controlled trials to evaluate lifestyle intervention for weight loss among breastfeeding women had been conducted. A systematic review of this evidence suggested that the combination of dietary restrictions and exercise is preferable to reach short‐term weight loss (Amorim et al. 2007). However, the longer term effects of these interventions are unknown among post‐partum women. Since then additional trials have been published finding a 16‐week diet and exercise intervention to result in weight loss among overweight and obese women, whereas a longer 9‐month diet and exercise trial did not lead to weight loss (Østbye et al. 2009; Colleran & Lovelady 2012). Thus the data are still inconclusive. The inconsistency indicates that a deeper understanding of the processes involved is warranted.
Achieving weight loss goals, satisfaction with achieved weight, vigilance in weight control, coping and problem‐solving skills as well as self‐efficacy may be important determinants of weight control (Byrne 2002; Byrne et al. 2003). Furthermore, successful weight loss maintenance among women has been conceptualised as a shift in identity (Epiphaniou & Ogden 2010). The shift in identity is characterised by emergence of a positive self‐image, internalising structured and healthy yet flexible dietary habits which lead to feelings of satisfaction instead of deprivation or constriction, and finding new strategies to keep up motivation. A study of behavioural aspects of weight maintenance and relapse among American women indicated that developing individual strategies as opposed to following a set programme, monitoring weight, eating a healthy diet, having a greater ability to cope with problems and social support were common to those maintaining weight (Kayman et al. 1990). Furthermore, guided by Newman's theory of health as expanding consciousness, weight loss and maintenance among women were understood as change from low self‐confidence and vulnerability, to increased self‐awareness, confidence, self‐esteem and personal integration and control (Berry 2004). However, there is a lack of understanding of how post‐partum women can successfully lose weight and maintain weight loss. A qualitative study exploring experiences of a weight loss intervention among post‐partum women described reasons for declining to participate in a weight loss intervention, and concluded that post‐partum women face difficult and complex challenges to prioritising their health and weight management (Carter‐Edwards et al. 2009). Thus, special consideration must be taken to this. Unfortunately, that intervention did not result in weight loss. However, we have recently shown that dietary behavioural modification treatment, with or without exercise, results in weight loss and maintenance of weight loss (Bertz et al. 2012). The aim of this study is to provide an explanatory model of how overweight and obese women achieve weight loss during, and after, participating in a post‐partum diet and exercise intervention. As quantitative evidence is accumulating, stating that post‐partum weight loss can be achieved through lifestyle intervention, qualitative data are also needed to underpin clinical decisions and design of interventions.
Key messages
This article provides an explanatory model of weight loss and maintenance among overweight and obese post‐partum women, and introduces two theoretical constructs to conceptualise the main findings; Transformative Lifestyle Change and Catalytic Interaction.
Longer term weight loss was understood as integration of recognised health behaviours through a transformative process of rewarding reciprocal changes in cognitions, emotions, body, behaviours and perceived self (the Transformative Lifestyle Change).
Initiation of lifestyle changes was understood as dependent on an energising mixture of personalised and useful information and follow‐up, relevant at both cognitive and emotional levels (the Catalytic Interaction).
Methods
Study design
We were guided by Grounded Theory (Glaser & Strauss 1967; Corbin & Strauss 2008). The Grounded Theory method is a systematic research methodology involving the discovery of theory through the analysis of data. It is useful in the analysis of areas where little is previously known. In Grounded Theory methodology data are used to generate a theory or model on a certain social situation/process and to discover the main area of concern in that situation/process, from the perspective of the participants. Thus Grounded Theory was chosen, firstly because little is known about the subject area. Following from that, the aim was to generate an explanatory model rather than a description or an analysis using existing theories. And finally, the area involves social processes including the woman and the health care provider/child/partner/other significant others and the social situations encountered.
Setting
Women participating in a randomised controlled trial of lifestyle intervention set in an urban area in southern Sweden were recruited to this qualitative study. The aim of the trial was to evaluate the effect of a 12‐week dietary and/or physical exercise intervention on weight and body composition and weight maintenance at the end of the intervention (12 weeks) and at 9 months after the intervention (1‐year follow‐up), in overweight and obese post‐partum women. Recruitment in cooperation with 15 antenatal care clinics, representative of the city's socioeconomic diversity took place between 2007 and 2010.
In Sweden, parents can use 480 days of paid parental leave per child, of which most can be divided freely between the parents until the year the child starts school. Most women take full‐time leave during the first months after delivery, whereas after 1 year most are no longer on leave. The cost is shared by the state and the employer (‘The Swedish Social Insurance Agency’ 2010).
Brief description of the intervention study
In total, 68 healthy women who were overweight or obese [body mass index (BMI) 25–35 kg m−2] before pregnancy and intending to breastfeed exclusively for the first 6 months were included. The women were randomised to four intervention groups: Dietary behaviour modification group (D group), Physical exercise behaviour modification group (E group), Combined dietary plus physical exercise behaviour modification group (DE group) or Control group (C group).
Two treatments were provided: D treatment and E treatment. For the women receiving the D treatment (D and DE groups), a dietician provided an individually tailored intervention based on the woman's 4‐day weighed food diary, meeting the current Nordic Nutrition Recommendations (Nordic Council of Ministers 2004). The goal of the intervention was outcome specific: to reduce weight by 0.5 kg week−1 (but not exceed 1 kg week−1) to a total of 6 kg weight loss. The women were provided with electronic scales for self‐monitoring of body weight. For the women receiving the E treatment (E and DE groups), a physiotherapist provided an individually tailored exercise intervention based on the woman's fitness level. The women were provided with a heart rate monitor for self‐monitoring. The goal of the intervention was behavioural; to complete a 45 min brisk walk 4 days week−1 at levels representing 60–70% of the maximum heart rate, referred to as ‘pulse zone walks’. The DE group received both the D and E treatments in their entirety.
The trial methods and quantitative results have been presented elsewhere (Bertz et al. 2012). In short, we demonstrated that dietary treatment was (1) sufficient to provide a significant and clinically meaningful weight loss of ∼10%, and that (2) the weight loss was sustained 9 months after the treatment ended (P < 0.001 at both time points). However, exercise treatment alone did not increase total energy expenditure or weight loss. Combined treatment did not yield significant weight or body composition changes beyond those of dietary treatment alone.
Qualitative data collection
Women from D, E and DE intervention groups and also C group were interviewed using an interview guide with open‐ended questions. The interviews were digitally recorded and transcribed verbatim. A pilot interview was performed and thereafter the interview guide was constructed. The interview guide was revised continuously in line with issues emerging in data analysis in accordance with Grounded Theory. The main focus was: ‘What are your experiences from making diet and/or exercise changes in the context of the intervention?’ Follow‐up questions were posed and recurrent interviews were carried out in which women were asked about their experiences of maintaining lifestyle changes.
Starting in October 2008, women finishing either the 12‐week intervention or the 1‐year follow‐up were invited to be interviewed. All invited women accepted within 2 weeks (n = 21). In total, 29 interviews were conducted with; 11 women at post‐intervention only, 10 at 1‐year follow‐up only, and eight on both occasions (Table 1). To start data collection, the first eight women in D, E and DE groups that were scheduled for either 12‐week or 1‐year measurements were invited for initial interviews. Thereafter theoretical sampling was initiated. A total of 15 interviews were conducted following successful weight loss or maintenance (four in D, three in E, eight in DE), whereas 14 were conducted following unsuccessful weight loss or maintenance (three in D, five in E, four in DE, two in C), to achieve saturation regarding both outcomes. Women achieving and sustaining a weight loss of 6 kg or more were considered successful in accordance with the intervention trial goals, based on weight loss recommendations for post‐partum women (Institute of Medicine/National Research Council 2009). Because of the theoretical sampling procedure not all women were interviewed at both time points, but were selected to add to or saturate the emerging theory. Two women from C group were invited for interviews as negative cases (Corbin & Strauss 2008). The interviewed women's baseline BMI ranged from 26 to 34 kg m−2, and age from 26 to 40 years. The interviews were conducted in privacy in the women's homes. For women who were interviewed twice, the follow‐up interview 1 year later was conducted by phone. The first interviews were approximately 45 min in length, and the follow‐up interviews lasted between 20 and 35 min. Additionally, e‐mails from the women expressing thoughts on their experiences of diet and/or exercise changes were used as data sources. Finally, memos often including quotes from the participants were written by the researchers during the intervention to aid data collection and analysis.
Table 1.
Sampling order, group allocation, interview time points and weight among study women (qualitative substudy)
| Sampling order | Intervention group allocation | Baseline weight (kg) | Baseline BMI (kg m−2) | Post‐intervention weight change (kg) | Post‐intervention interview | 1‐year follow‐up weight change (kg) | 1‐year follow‐up interview |
|---|---|---|---|---|---|---|---|
| 1 | Exercise | 87 | 29 | −3 | −12 | ×* | |
| 2 | Diet + Exercise | 92 | 34 | −4 | × | −5 | |
| 3 | Diet + Exercise | 70 | 26 | −3 | × | −4 | |
| 4 | Diet | 100 | 32 | −12 | * | −9 | ×* |
| 5 | Diet | 84 | 34 | −2 | × | −4 | × |
| 6 | Exercise | 99 | 36 | −1 | × | −3 | × |
| 7 | Exercise | 89 | 27 | −7 | * | −7 | ×* |
| 8 | Diet | 86 | 27 | −6 | ×* | −1 | |
| 9 | Diet + Exercise | 83 | 30 | −12 | ×* | −16 | ×* |
| 10 | Diet | 77 | 28 | −6 | * | −10 | ×* |
| 11 | Diet + Exercise | 87 | 27 | −7 | * | −6 | ×* |
| 12 | Diet + Exercise | 82 | 33 | −2 | × | −5 | × |
| 13 | Diet | 80 | 32 | −5 | × | −13 | ×* |
| 14 | Exercise | 92 | 34 | −5 | × | 0 | × |
| 15 | Diet + Exercise | 90 | 28 | −6 | ×* | −6 | ×* |
| 16 | Diet + Exercise | 90 | 30 | −11 | ×* | −25 | ×* |
| 17 | Diet + Exercise | 88 | 31 | −7 | ×* | 1 | |
| 18 | Exercise | 99 | 33 | −3 | −9 | ×* | |
| 19 | Control | 88 | 30 | 0 | −2 | × | |
| 20 | Exercise | 85 | 29 | 4 | −1 | × | |
| 21 | Control | 90 | 33 | 2 | −4 | × |
× Interview performed.
*Successful according to short‐ and/or long‐term intervention weight loss goal.
Data analysis
The analysis started with open coding using NVivo 8.0 software (QSR International Pty Ltd, Doncaster, Vic., Australia). The interviews were read and coded line by line or paragraph by paragraph. The process of coding continued until categories emerged, and properties and dimensions were identified (Glaser & Strauss 1967; Corbin & Strauss 2008). These were thoroughly discussed by the whole team. During axial coding, linking categories, general patterns and similarities and differences were continuously sought by constant comparisons within and between codes and categories. In the analysis process, statements from interviewed women were also considered in relation to success of weight loss/management. Memos were written throughout the process to aid the concurrent data collection and analysis. Selective coding was used in rereading the material to make sure as many aspects as possible related to the categories were identified. High replication of data within emerging categories and verification of actions, incidents and strategies by several participants indicated saturation (Corbin & Strauss 2008).
To improve trustworthiness, all interviews were conducted by a research group member who was not associated with the intervention. Triangulation took place during the data analysis, with researchers representing both the insider perspective (nutrition science) and the outsider perspective (caring science), and data‐checks with quantitative outcomes. Also, the different backgrounds of the research group members brought different perspectives into the analysis process. In addition, every fifth interview was coded individually by two researchers, and thereafter any differences were negotiated. Using NVivo allowed all authors to access data and coding schemes, ensuring transparency throughout the process. The study was approved by the Regional Ethics Board in Gothenburg, Sweden.
Findings
Overall model
An explanatory model illustrating the process of achieving and maintaining weight loss during and after a diet and/or exercise intervention in the post‐partum period is presented in Fig. 1. The model represents the Transformative Lifestyle Change (TLC) that captures the categories and interactions that emerged, representing the women's experiences. A trajectory (circular arrow) holds seven action‐stages (boxes) defined by the central action of each stage (from seizing the convergence of facilitating factors to adaptive transposing), beginning and ending with two opposite lifestyle states respectively marking the initialisation and exit of the TLC process (discontentedly lacking lifestyle control and lifestyle managing) defined by the central experience of each (block‐arrows), and interaction (thin arrows) with the intervention (circle) through Catalytic Interaction (CI). The core category TLC (in italics) develops as a result of the progression along the action stage trajectory. The dashed arrow depicts possible reverse movement between action‐stages. Below, the conceptual model is described in detail (categories in bold italics, substantive codes in italics).
Figure 1.
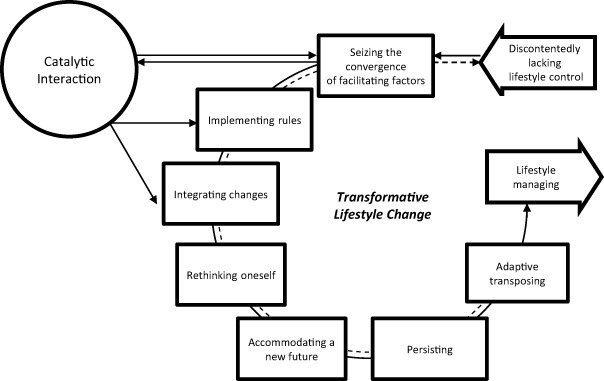
Conceptual model of the Transformative Lifestyle Change process of achieving and maintaining weight loss, aided by a diet and/or exercise intervention in the postpartum period.
Core category
Transformative Lifestyle Change
TLC explains the main issue of the participants; how to achieve sustainable weight loss, and how they tried to solve this issue. The TLC construct describes the multileveled and intertwined changes that led to weight management; changing women from discontentedly lacking lifestyle control to become lifestyle managing. The construct is composed of ‘transformative’ and ‘lifestyle change’, to conceptualise how lifestyle changes produced significant and deeply rooted changes in the self and life among these women. The transformative change was initially catalysed by the intervention through an external impetus; the CI which facilitated the implementation of the initial cognitive, emotional and behavioural changes. Thereafter, the TLC was driven by a self‐reinforcing interplay between step wise behavioural changes and the effects of these changes. The effects of the behavioural changes were the rewarding and sought after bodily changes of decreased weight and improved well‐being. The experience of a successful outcome following behavioural changes increased mental energy and motivation, improved self‐image, and led to alignment of inner, previously conflicting, rational and emotional drivers. This created positive feedback that supported further change and persistence, and over time established cognitive and emotional changes, i.e. a change in the perceived self, needed to maintain the new weight and lifestyle. Women accomplishing the stages of the TLC process were successful in weight loss, in contrast to those who did not. The process began and ended in a ‘normal life’ state (i.e. working/studying, not in active lifestyle treatment), after the trajectory had progressed forth and then back again over a state‐of‐mind cycle in which focus was put on the actions of change, outweighing many concerns of normal life for a limited time. The environment became subject to concrete changes, mainly to hinder the negative influence of an obesogenic environment by changes in the day‐to‐day practical and social environment, and the broader life context was approached with new insights and an attitude that made it more manageable.
Initial lifestyle state
Discontentedly lacking lifestyle control
Before joining the intervention, these women perceived themselves as lacking lifestyle control, self‐control and the ability to maintain a healthy weight. The major barrier was (1) stress, but also (2) social norms and (3) lack of structure or discipline, or (4) lack of sufficient motivation were perceived to maintain weight problems through a lifestyle they could not control, nor were satisfied with. These were also barriers to lifestyle change during the intervention.
Discontentedly lacking lifestyle control decreased motivation and negatively affected self‐image by maintaining an inner conflict; by giving in to the ‘path of least resistance’1 despite ‘knowing better’. ‘I work so much, it becomes like a vicious circle, my energy just runs short all the time, because you don't have the energy to just keep going, and then it's easy to go for bad solutions’ (DE, 9, Successful 2.
Catalytic interaction
The ‘energising’ interaction between health care provider and patient was the key to successful initiation of change. It depended on individualised, concrete, specific and useful information, and an emotional bond through joint commitment, trust and accountability. These aspects are covered in the three distinct subcategories Spark, Direction, and Pressure and Praise.
Spark
To these well‐educated women, all with internet access, any information was accessible at any time. Also, most were motivated to weight loss and considered themselves well informed regarding official diet and exercise recommendations. Still, this was not enough to achieve weight loss. To act on the information provided during treatment it had to be perceived as (1) personally relevant, (2) applicable, (3) emotionally convincing (to outweigh conflicting interests), (4) ‘eye‐opening’ or positively surprising, and (5) delivered in a credible way. The spark to create an energising sense of increased motivation and self‐belief thus came from the feeling that the information provided was different from what they already knew or had access to, that it would make a difference to act on it, and that they could be successful in acting on it. Regarding diet, this came from writing and discussing the food diary, and through outcome‐quantification i.e. being informed in exact numbers about the total and per week weight loss that concrete changes in accordance with the intervention would lead to. With exercise, it came from information on ‘fat‐burning’ during walking in the specified heart rate zone. The spark was strengthened by (6) professional credibility from the dietitian and physiotherapist, and (7) advanced medical technology. Among those not successful, lack of spark was one reason. ‘I made it the full first week but … it [limiting the sweets] felt really ridiculous so I [gave up], and then I had blown it.’ (D, 5, Unsuccessful)
Direction
The intervention programme provided direction on how to channel motivation. (1) Following a plan was motivating in itself, and further facilitated change by minimising ambiguity. (2) A specified attractive goal (weight or exercise level) broken down into weekly (3) subgoals made the goal feel desired, real and within reach.
(4) Gradual introduction of (5) clearly specified changes was seen as crucial to reducing the barriers to change, as opposed to general lifestyle advice and quick‐fix approaches. Many women had experiences with the latter, and became surprised with how effective simple and small changes were, and how easy they were to make. For the changes to come into effect, the direction given had to be clear yet flexible, and adaptable to all situations in the woman's normal life.
Pressure and praise
The intervention provided pressure (in vivo code) to ‘deliver results’ regarding goals of the intervention, by (1) being monitored and (2) feeling accountable, through the biweekly cellphone text message follow‐ups and the trial measurements. This was in line with the women's rational goals, and necessary to overcome ‘emotional discomfort’, take actions and keep motivated. ‘You really do it when someone is watching you’ (D, 4, Successful). Many women felt more motivated and more satisfied with their results when they were pushed to lose weight, while simultaneously restricted not to lose too much too fast. ‘I didn't experience that the main focus was weight loss, but rather that it should not go too fast. Thus my expectations became more patient, in some way I was continuously satisfied with a small weight loss’ (D, from memo, Successful).
(3) Encouragement and (4) praise from the intervention staff increased both persistence and compliance by increasing motivation and perceived resourcefulness. Being told ‘you can make it’, ‘keep up the good work’ and ‘you are doing great’ made a real difference. The women felt that the intervention staff personally and genuinely believed in them and their ability to succeed.
Trajectory of action stages
Seizing the convergence of facilitating factors
These women sought for a suitable time in life to make lifestyle changes to lose weight. Motivation to weight loss was a pressing sense of need for improved health and well‐being, and to some extent appearance. In addition, parenthood produced a strong responsibility for maintaining health and serving as a role model. During pregnancy and in the early post‐partum period, they experienced increased motivation, and decided to make use of the perceived freedom of parental leave. Among some women increasing age and number of children were additionally motivating factors. Many were unsure about how and where to find support for weight management until presented with the opportunity to join the clinical trial. All women figured that participation in the study would provide a much needed (1) push in the right direction to overcome inertia. Viewing the trial as attractive in terms of sophistication, credibility and scope led to the decision to join the trial. Thus, the tipping point to take action was the (2) accumulated personal motivation coupled with the (3) increased motivation because of the child, and the (4) recognition of important contextual facilitators. Among women who did not succeed in weight loss during the trial, these motivating factors were not sufficiently relevant or recognised at that time, but were thought of as possible problems in the future. ‘Now I don't have any problems, but if it keeps up it will get harder I guess when the weight goes up’ (DE, 2, Unsuccessful). ‘I feel I don't have any problems with my weight, except appearance‐wise’ (D, 4, Unsuccessful).
Implementing rules
During the process of implementing concrete changes, four of the key strategies provided by the intervention were (1) perceived (as) rules. These were ‘candy only once a week’, ‘the plate model’ (i.e. half the plate covered by vegetables) in D groups, ‘optimal exercise level’ (exercise at 60–70% of maximum heart rate) and ‘four exercise sessions per week’ in E groups. The women put much effort into implementing them. Many experienced that ‘the trick’ or key to weight loss was to stay strict regarding the ‘candy‐rule’. Adhering to these strategies did not, and was not expected to, ‘come naturally’; instead they had to be (2) consciously enforced. Making lifestyle changes by exerting willpower and self‐control was perceived to require much mental energy. However, the perceived effort was reduced with the (3) simplicity of rules, as opposed to constantly reasoning with one self or others about what to do.
Integrating changes
Integration of lifestyle changes (the rules and other parts of the treatment programme) into the individual life circumstances, ‘making it work’, was needed to create relevant and sustainable change. The strategies were: (1) Planning of exercise sessions and writing daily or weekly menus and grocery lists was used to gain control. ‘I think it's a way of life; instead of exercising when you get the time, you make sure to book it in your schedule’ (E, 7, Successful). ‘I make a menu for four to five days, and also add what kind of vegetables to have, and try to have it at home too’ (D, 13, Successful). Parts of life that women could not plan themselves, such as social events, were fine‐tuned with (2) a conscious approach, particularly regarding type and amount of food when eating away from home. (3) Strategic daily‐life‐environment adjustments were made to underpin the new way of life; access to exercise irrespective of the weather by joining a gym or acquiring home‐exercise equipment, keeping healthy foods and ready‐to‐eat vegetables at all times, keeping the home free of candy during weekdays, including throwing away the kids’ left‐over candy. (4) Involving the partner was important to get support and avoid conflicts in lifestyle choices. (5) Regularity in eating habits became a cornerstone for maintaining both desired food choices and weight. This demanded planning and led to portion size control through avoidance of ‘crashing’ and subsequent uncontrollable ‘urges’. Also, (6) new self‐monitoring routines were established. Monitoring and logging weight and exercise results was considered a way to keep control, to increase motivation, and serve as action‐triggers for other health behaviours. ‘The thing is that I have the scales, and I still weigh myself three times a week, it's really good because I still have control. I have bought my own small scales and keep the same statistics as I did during the intervention.’ (DE, 15, Successful)
Among those who did not succeed in weight loss, attempts at integration were often hindered by social/contextual factors; lack of good available options, perceived social norms, but also lack of planning resulting in ‘convenience‐solutions’. ‘It went really fine at first, but then … I was away from home a lot, I felt I couldn't control what food I got. And there was a lot of coffee with pastries offered by people all the time. I didn't have much, but I have a hard time saying no’ (DE, 12, Unsuccessful).
Rethinking oneself
Successively (1) the self‐image changed, women recognised that they could be normal weight, and also greater confidence in weight and lifestyle control emerged as traits of the new self‐image. ‘I can do it, I'm like that’ (D, from memo, Successful). Also (2) shifts in perspectives were noted; changes in food‐preferences and experiences of what and how much food or exercise that was needed to sustain well‐being. ‘It was a great aha‐experience. I figured out how I personally should do things. Before, I always thought I had to go flat out, or I might as well not bother, but not anymore’ (D, 13, Successful).
Accommodating a new future
After implementation and integration of changes in a ‘here and now’ fashion; cognitive and emotional room had to be created to (1) accept a future involving a new lifestyle and (2) plan for the changes to last. To achieve this, many women set long‐term weight goals. Three major long‐term, personal weight goals were represented; return to weight before children, BMI below 25 kg m−2, and weight stability after reaching the intervention weight loss goal. These are likely goals that represent the women's perception of long‐term weight control success. For some this was an ambitious goal representing substantive additional weight loss, whereas others were already successful in this regard. In relation to the trial weight loss goal, most women perceived this to represent success if it also met the major personal goal of their preference. Some women also planned for running longer races, a few even a half‐marathon. Ambitious goal‐setting increased motivation by adding continued outcome‐hopes and pressure.
Persisting
Being (1) steadfast and committed, ‘stubborn’ in staying with one's plan was seen as a crucial factor in lifestyle management, particularly after the intervention. However, this depended on (2) the conviction that a successful and attractive outcome was attainable. Not being, or being able to be, persistent was among all women regarded as a crucial reason for not achieving successful weight management. Inner conflicts were constant barriers to persistence. The main inner conflict stood between being short‐sighted and choosing instant gratification (e.g. the rewarding or comforting pleasure of old habits) vs. the rationally desired long‐term goals with greater rewards (i.e. losing weight and feeling good about oneself). ‘It [weight loss] felt so very good, that's why I don't understand myself, why I eat these unhealthy foods, since I know that I lose weight if I look after myself’ (DE, 17, Unsuccessful).
(3) Accepting and constructively dealing with temporary setbacks increased persistence, as opposed to employing an all or nothing mentality which only worsened the setback. Experiencing setbacks was common, and part of a trial and error exploration of how to maintain lifestyle changes. ‘Well, I was under those seven kilos. And then came this damned vacation, and I gained two kilos, but I've lost them again’ (DE, 15, Successful). To get back on track after relapses, the strategies of the intervention were reemployed. To persist in emerging changes was difficult at times, and the shift in daily life routines that came with holidays was problematic to many. ‘In the beginning I succeeded, but then summer came, I shouldn't blame that but it was really hard and I ate, like my “old food‐life”, so I tried a week again and did well for a few days, but fell into old patterns again’ (DE, 2, Unsuccessful). Support that extended the intervention, mainly in the form of pressure, was desired as a means to maintain the initiated changes by increasing persistence. After the intervention some women recognised a (4) need for continued support, and acquired such. These forms of support ranged from forming an exercise group among friends or joining a gym, to joining Weight Watchers or hiring a coach.
Adaptive transposing
The end of parental leave required adaptive transposing of acquired lifestyle behaviours due to the shift in environment when returning to ‘normal life’ of work or education. ‘You start making changes in this little bubble, and then you have to expand it’ (D, from memo, Successful). Strategies of integration and maintenance of lifestyle changes acquired during parental leave were reemployed in an environment‐specific manner.
To manage inappropriate food choices at work (1) pro‐active strategies were to start bringing a lunch‐box, or choose a restaurant with healthy food options. ‘I take a lunch‐box to work, and cook the food at home, usually with low‐fat products and good foods’ (D, 13, Successful). Also, (2) re‐active strategies, such as rule‐based restrictions or ‘conscious choices’ of the available foods were made. ‘Previously I used to eat a full portion at the diner, but now I take a little more than half, I have realized that it's way too much for me with one full serving’ (DE, 9, Successful). Physical activity was mainly integrated as a means of transport to and from work, in the form of walking or bicycling. ‘I bought a bike, so now I take it to and from work. Regardless of the weather’ (E, 18, Successful).
Among some women no adaptive transposing took place, and the return to work disintegrated emerging lifestyle changes. Mainly stress, but also ambiguity regarding concrete strategies and perceived social norms were reasons for this. For several initially successful women this was the ‘critical point’ beyond which some did not manage to maintain weight loss and lifestyle changes. For a few, this turned into a negative feedback loop which brought them back to discontentedly lacking lifestyle control, whereas most women maintained motivation and self‐belief and were determined to carry on towards their goals.
Lifestyle state outcome
Lifestyle managing
Being lifestyle managing was the outcome of TLC, representing the ability to (1) control the self and (2) to control relevant circumstances of life to the extent that sustainable weight management was possible. (3) Cognitive and emotional internalisation of lifestyle changes were achieved when new behaviours were considered to have little or no impact on the perceived levels of mental energy required to maintain them. ‘Not having to think about it’ was used to describe how these behaviours were not cognitively demanding, and did not evoke any inner conflict. New lifestyle strategies were implemented and integrated, and many (4) inner conflicts were resolved as emotion and rationality were increasingly aligned. An (5) automatic or habitual execution of acquired new behaviours, efficiently maintained the new lifestyle. ‘Now I have the exercise that I didn't have before, and I'm prudent with my diet, without really having to think about it’ (D, 13, Successful). To be lifestyle managing built on internalisation of the main qualities sought by the women for weight control: motivation, confidence, new perspectives on healthier eating and exercise habits, a self‐verified and individualised toolbox of lifestyle strategies and skills applicable in the normal environment and perceived control. ‘Participating in the study has changed me. I thought before that I was the kind who couldn't get slim, but today I realize that it is quite easy to influence, with the right diet. It is not about “all my slim friends can eat much more” and “I gain so easily”. Also, I'm more satisfied with my body today. I have better control over my eating. It doesn't feel so chaotic and unmanageable; rather I know exactly how to eat to manage my weight, and how I eat if I gain weight. I have always enjoyed good food, and I do that today too, but I don't have to eat loads of the good food.’ (DE, 9, Successful)
Discussion
Two new constructs emerged in this study; TLC and CI, which we believe are valuable in explaining successful weight loss treatment. To overcome initial barriers to weight loss, the women needed treatment to provide a CI. It depended on the health care provider delivering individualised, concrete, specific and useful information, and an emotional bond through joint commitment, trust and accountability. Weight loss was underpinned by gradual introduction of new health behaviours; reducing sweets, consuming low fat/low sugar foods, increasing fruits and vegetables, regular meals, regular exercise, self‐weighing, planning of meals and exercise, and walking or bicycling for transport. Not all women used all the above strategies, however, dietary changes were essential to achieve weight loss. TLC developed through, and reinforced continuous, implementation of new behaviours. This led to fundamental changes in the women's attitudes and emotions. The nine stages of the TLC led to habituating the new behaviours and to gaining lifestyle control. Women accomplishing the stages of the TLC process were successful in weight loss, in contrast to those who did not. This stresses and defines key aspects of the health care provider – patient relationship, and the implementation of particular health behaviours. Our findings indicate that TLC, through CI, is a useful conceptualisation of successful weight loss and weight loss maintenance among overweight and obese women who seek weight loss support during the post‐partum period.
Integration with health behaviour theories
Initiating change
Several health behaviour theories; the Health Belief Model, (Rosenstock et al. 1988), the Theory of Planned Behaviour, (Ajzen 1991), Social Cognitive Theory (SCT) (Rosenstock et al. 1988) and the Transtheoretical Model (TTM), (Prochaska & Norcross 2001) share core concepts with our newly identified category TLC. Although there are differences among these theories, it is noteworthy that some concepts are very similar (Bandura 2004). These are motivation to make health issues relevant, the perception of a health problem or threat, and the perception that action can be taken to solve this problem. Also, prominent in several of these theories are versions of the concepts self‐efficacy and outcome‐expectancies (Bandura 2004), which also emerged in our model as central to engaging in and maintaining lifestyle changes.
To generate and sustain a high level of motivation and compliance it appears beneficial if the health care provider utilises an intervention plan that corresponds to the three CI‐concepts (1) spark, (2) direction, and (3) pressure and praise, as these emerged in our study as most associated with successful change. CI integrates well with the working alliance construct (Brodin 1979), which includes three components: (1) the agreement between therapist and client about the goals of intervention, (2) the agreement about the therapy tasks needed to accomplish those goals, and (3) the emotional bond developed between therapist and client that allow the client to make therapeutic progress. Almost all women stated that they needed ‘pressure’ to get the extra energy or motivation needed to overcome many barriers to change. They used the specific word ‘pressure’ frequently. When analysed in context it mainly alluded to accountability. This is in contrast to the common notion that external pressure may obstruct change. However, the women referred to this feeling of pressure as supporting their rational and freely chosen goals, not a pressure to act against their will.
Maintaining change
Like TTM, our model is dynamic and predicts that adoption of health behaviours consists of several stages. We also suggest that the stages leading to lifestyle change include pre‐action contemplations, followed by actions of increasingly internalised behaviour changes towards self‐directed and sustainable weight maintenance. However, our model is more segmented, comprising seven distinct ‘action‐stages’.
We identified the adaptive transposing stage that emerged as highly relevant to post‐partum women. This highlights the importance of assessing the behaviour/environment‐interaction, particularly in transition periods. The transformation from ‘discontentedly lacking lifestyle control’ to ‘lifestyle managing’ also represents a shift from externality to internality in agreement with the locus of control theory (Rotter 1966). This was seen as a shift among the women from feeeling ther weight and lifestyle to be determined by outside factors to gaining the ability to control relevant aspects of their life themselves.
Integration with psychological behaviour change theories
Resisting temptations, regulating negative feelings and coping with stress require self‐control. After a few self‐control expending efforts, following attempts at self‐control are more likely to fail. Continuous self‐control efforts also decline over time. However, behaviours that do not require self‐control do not expend nor require self‐control strength (Muraven & Baumeister 2000). This supports how TLC, through producing new automatic behaviours and a self‐image aligned with new lifestyle, leads to behaviours more likely to endure because these behaviours are changed from self‐control strength taxing towards evoking no or few inner conflicts. Furthermore, self‐control strength is like a muscle; not only can it be exhausted but it can also be exercised (Muraven & Baumeister 2000). Repeated practice and rest over time can improve self‐control strength. By gradual introduction of both magnitude and complexity of self‐control demanding actions among the women such an exercise effect may have occurred.
Cognitive dissonance theory states that inconsistency among cognitions lead to a psychological tension with drive‐like properties to reduce this tension, e.g. by changing attitude towards a behaviour (Festinger 1962). During the intervention, repetition of new behaviours may have caused a change in attitude towards these behaviours thus resolving the cognitive dissonance that was generated. While women were initially driven by both initial motivation and pressure, these behaviours were likely to lead to changes in attitude, which later underpinned the change process through reduction of resistance to the new lifestyle.
Finally, the TLC can also be integrated with findings in theory of habit. Wood et al. found that individuals engaged in habitual behaviour are likely to think about issues unrelated to the behaviour, whereas during non‐habitual behaviour thoughts corresponding to the behaviour occur. During habitual behaviour actions are thus thought not to depend on conscious guidance (Wood et al. 2002). This is in agreement with the experience among the women of ‘not having to think about it’ when new behaviours had become automatic or habitual, as conceptualised in the lifestyle‐managing stage.
Integration with qualitative and quantitative research
In line with previous findings, for these women initial motivation to change was health, appearance and well‐being (Kwan 2009), and more post‐partum‐specific; responsibility for the child. Weight loss and weight maintenance may be understood as implementing healthy eating habits, underpinned by a shift in behaviours and identity, leading to increased control, resourcefulness, flexibility and self‐efficacy (Kayman et al. 1990; Berry 2004; Epiphaniou & Ogden 2010; Hindle & Carpenter 2011). By using positive deviance to determine successful weight‐control practices, themes in the areas of (1) nutrition, (2) physical activity, (3) restraint, (4) self‐monitoring, and (5) motivation were found by Stuckey et al. (2011). Practices in these areas were identified also in our analysis. In line with this, successful women strove to adhere to dietary and exercise behaviours in line with current recommendations (Nordic Council of Ministers 2004), which is similar to habits of other successful weight loss maintainers found in the National Weight Control Registry (Klem et al. 1997; Phelan et al. 2006).
The Active Mothers Postpartum (AMP) behavioural intervention trial to enhance weight loss in post‐partum women who were overweight or obese prior to pregnancy provided a multicomponent intervention based on SCT, TTM and motivational models (Østbye et al. 2009). However, the 12‐month intervention did not lead to weight loss. At least four clear differences between the AMP design and our trial were experienced as important to the outcome by the interviewed women in our trial: (1) individual personalised counselling; (2) meticulous and/or objective measurements; (3) flexibility in appointments and communication through the individualised approach and (4) self‐monitoring in combination with follow‐up cellphone text messaging. Also, the setting of the AMP trial, as well as diverse ethnicity and socioeconomic characteristics in the study populations differed from our trial.
Stages of change (TTM) have been investigated cross‐sectionally among post‐partum women participating in a weight management programme. The pro‐to‐con ratio was highest in the action stage for losing weight, avoiding high‐fat foods, and exercising three times per week. A lower ratio was found during the maintenance stage (Krummel et al. 2004). In accordance with our model, this poses a threat to long‐term weight loss, and must be compensated for by a shift in attitudes, underpinned by suitable strategies for changes to endure.
Limitations and strengths
The study concerns a specific population for whom the results are highly relevant. However, it was conducted among Swedish women, predominantly married or cohabitating and well educated. This may limit the transferability of results. In addition, Swedish parental leave is long and highly reimbursed by international comparison, which may benefit interventions initiated during this window of opportunity. If so, this is an important health argument for a generous parental leave policy. The study sample was fairly small, although within the range appropriate for generating a substantive theory (Corbin & Strauss 2008). However in order to develop a formal theory the findings require confirmation and may in accordance with Grounded Theory methodology also undergo modification. High trustworthiness was achieved through the research group composition, full participation among respondents, repeated interviews, interviews being done during active participation in the intervention study and in parallel with analysis, and use of multiple data sources (Corbin & Strauss 2008). Further research should include a more diverse population from different treatment programmes, and also regarding ethnicity and socioeconomic status. Also, the model generated here should be systematically evaluated in the clinical setting.
Conclusion
In this article, we present new knowledge regarding the process of achieving weight loss and maintenance in a post‐partum treatment context, including the role of the heath care provider. The explanatory model developed here may be used to assist a health care provider in understanding treatment barriers and facilitators, and their occurrence along the course of a post‐partum weight loss treatment. The categories, and their underpinning substantive codes, provide concrete elements to consider in weight loss treatment. Among the women participating in this study, a successful outcome understood as TLC through CI depended not only on a temporary combination of willpower and support, but also on the development of reciprocal changes in cognitions, emotions, body, environment, behaviour and perceived self, which jointly reduced the barriers to a new lifestyle. This highlights the multidimensional complexity of lifestyle treatment for overweight and obesity, and also adds new knowledge in this area of research and treatment.
Source of funding
The Swedish Research Council (Project grant: K2009‐70X‐21091‐01‐3) and the Swedish Council for Working Life and Social Research (Project grant: 2006‐0339 and Project grant: 2007‐1958).
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
AW, FB and CSL conceptualized and designed the study. CSL conducted interviews. FB, CSL and AW interpreted the data and were involved in the critical revision of manuscript. FB wrote the paper and had primary responsibility for final content. All authors read and approved the final manuscript.
Acknowledgement
We thank all participating women for their invaluable contributions to the study, and we acknowledge Dr Monica Hunsberger for her thoughtful comments and help.
Bertz, F. , Sparud‐Lundin, C. , and Winkvist, A. (2015) Transformative Lifestyle Change: key to sustainable weight loss among women in a post‐partum diet and exercise intervention. Matern Child Nutr, 11: 631–645. doi: 10.1111/mcn.12103.
Trial registration number: NCT01343238.
Footnotes
Single or few‐word quote from interview or memo is in‐vivo code or same wording used by multiple women.
Identifier for quote. D denotes Diet group, E denotes Exercise group, DE denotes Diet and Exercise group, C denotes Control group. Number indicates individual according to sampling order. From memo indicates memo‐note from women not interviewed. Successful or Unsuccessful indicates whether the person reached the intervention weight loss goal.
References
- Abrams B., Heggeseth B., Rehkopf D. & Davis E. (2013) Parity and body mass index in US women: a prospective 25‐year study. Obesity (Silver Spring, Md.) 21, 1514–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajzen I. (1991) The theory of planned behavior. Organizational Behavior and Human Decision Processes 50 (2), 179–211. [Google Scholar]
- Amir L.H. & Donath S. (2007) A systematic review of maternal obesity and breastfeeding intention, initiation and duration. BMC Pregnancy and Childbirth 7 (9), 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amorim A.R., Linne Y.M. & Lourenco P.M. (2007) Diet or exercise, or both, for weight reduction in women after childbirth. Cochrane Database of Systematic Reviews (3), CD005627. [DOI] [PubMed] [Google Scholar]
- Bandura A. (2004) Health promotion by social cognitive means. Health Education & Behavior 31 (2), 143–164. [DOI] [PubMed] [Google Scholar]
- Bastian L.A., Pathiraja V.C., Krause K., Namenek Brouwer R.J., Swamy G.K., Lovelady C.A. et al (2010) Multiparity is associated with high motivation to change diet among overweight and obese postpartum women. Women's Health Issues 20 (2), 133–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry D. (2004) An emerging model of behavior change in women maintaining weight loss. Nursing Science Quarterly 17 (3), 242–252. [DOI] [PubMed] [Google Scholar]
- Bertz F., Brekke H.K., Ellegård L., Rasmussen K.M., Wennergren M. & Winkvist A. (2012) Diet and exercise weight loss trial in lactating overweight and obese women. American Journal of Clinical Nutrition 96, 698–705. [DOI] [PubMed] [Google Scholar]
- Brodin E.S. (1979) The generalizability of the psychoanalytic concept of te working alliance. Psychotherapy: Theory, Research and Practice 16, 252–260. [Google Scholar]
- Byrne S. (2002) Psychological aspects of weight maintenance and relapse in obesity. Journal of Psychosomatic Research 53, 1029–1036. [DOI] [PubMed] [Google Scholar]
- Byrne S., Cooper Z. & Fairburn C. (2003) Weight maintenance and relapse in obesity: a qualitative study. International Journal of Obesity 27, 955–962. [DOI] [PubMed] [Google Scholar]
- Carter‐Edwards L., Østbye T., Bastian L.A., Yarnall K.S., Krause K.M. & Simmons T.J. (2009) Barriers to adopting a healthy lifestyle: insight from postpartum women. BMC Research Notes 2, 161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colleran H.L. & Lovelady C.A. (2012) Use of MyPyramid Menu Planner for Moms in a weight‐loss intervention during lactation. Journal of the Academy of Nutrition and Dietetics 112 (4), 553–558. [DOI] [PubMed] [Google Scholar]
- Corbin J. & Strauss A. (eds) (2008) Basics of Qualitatative Research, 3rd edn Sage Publications: Thousand Oaks, CA. [Google Scholar]
- Epiphaniou E. & Ogden J. (2010) Successful weight loss maintenance and a shift in identity from restriction to a new liberated self. Journal of Health Psychology 15 (6), 887–896. [DOI] [PubMed] [Google Scholar]
- Festinger L. (1962) Cognitive dissonance. Scientific American 207, 93–102. [DOI] [PubMed] [Google Scholar]
- Glaser B.G. & Strauss A.L. (eds) (1967) The Discovery of Grounded Theory, Strategies for Qualitative Research. Aldine Transaction: New Brunswick, NJ. [Google Scholar]
- Gore S.A., Brown D.M. & West D.S. (2003) The role of postpartum weight retention in obesity among women: a review of the evidence. Annals of Behavioral Medicine 26 (2), 149–159. [DOI] [PubMed] [Google Scholar]
- Gunderson E.P. & Abrams B. (2000) Epidemiology of gestational weight gain and body weight changes after pregnancy. Epidemiologic Reviews 22 (2), 261–274. [DOI] [PubMed] [Google Scholar]
- Harris H.E. & Ellison G.T. (1997) Do the changes in energy balance that occur during pregnancy predispose parous women to obesity? Nutrition Research Reviews 10, 57–81. [DOI] [PubMed] [Google Scholar]
- Hindle L. & Carpenter C. (2011) An exploration of the experiences and perceptions of people who have maintained weight loss. Journal of Human Nutrition and Dietetics 24 (4), 342–350. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine/National Research Council (2009) Weight Gain during Pregnancy: Reexamining the Guidelines. National Academy Press: Washington, DC. [PubMed] [Google Scholar]
- Kayman S., Bruvold W. & Stern J.S. (1990) Maintenance and relapse after weight loss in women: behavioral aspects. The American Journal of Clinical Nutrition 52 (5), 800–807. [DOI] [PubMed] [Google Scholar]
- Klem M.L., Wing R.R., McGuire M.T., Seagle H.M. & Hill J.O. (1997) A descriptive study of individuals successful at long‐term maintenance of substantial weight loss. The American Journal of Clinical Nutrition 66 (2), 239–246. [DOI] [PubMed] [Google Scholar]
- Krummel D.A., Semmens E., Boury J., Gordon P.M. & Larkin K.T. (2004) Stages of change for weight management in postpartum women. Journal of the American Dietetic Association 104 (7), 1102–1108. [DOI] [PubMed] [Google Scholar]
- Kwan S. (2009) Competing motivational discourses for weight loss: means to ends and the nexus of beauty and health. Qualitative Health Research 19 (9), 1223–1233. [DOI] [PubMed] [Google Scholar]
- Linne Y., Barkeling B. & Rössner S. (2002) Natural course of gestational diabetes mellitus: long term follow up of women in the SPAWN study. BJOG 109 (11), 1227–1231. [DOI] [PubMed] [Google Scholar]
- Muraven M. & Baumeister R.F. (2000) Self‐regulation and depletion of limited resources: does self‐control resemble a muscle? Psychological Bulletin 126 (2), 247–259. [DOI] [PubMed] [Google Scholar]
- National Statistics (2008) Health Survey for England 2007 Available at: https://catalogue.ic.nhs.uk/publications/public-health/surveys/heal-surv-late-tren-eng-2007/heal-surv-late-tren-eng-2007-rep-v1.pdf
- Nordic Council of Ministers (2004) Nordic Nutrition Recommendations 2004. Integrating Nutrition and Physical Activity. Norden: Copenhagen. [Google Scholar]
- Østbye T., Krause K.M., Lovelady C.A., Morey M.C., Bastian L.A., Peterson B.L. et al (2009) Active Mothers Postpartum: a randomized controlled weight‐loss intervention trial. American Journal of Preventive Medicine 37 (3), 173–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan S., Wyatt H.R., Hill J.O. & Wing R.R. (2006) Are the eating and exercise habits of successful weight losers changing? Obesity (Silver Spring, Md.) 14 (4), 710–716. [DOI] [PubMed] [Google Scholar]
- Prochaska J.O. & Norcross J.C. (2001) Stages of change. Psychotherapy 38 (4), 443–448. [Google Scholar]
- Rooney B.L. & Schauberger C.W. (2002) Excess pregnancy weight gain and long‐term obesity: one decade later. Obstetrics and Gynecology 100 (2), 245–252. [DOI] [PubMed] [Google Scholar]
- Rosenstock I.M., Strecher V.J. & Becker M.H. (1988) Social learning theory and the Health Belief Model. Health Education Quarterly 15 (2), 175–183. [DOI] [PubMed] [Google Scholar]
- Rotter J.B. (1966) Generalized Expectancies for Internal versus External Control of Reinforcement. American Psychological Association: Washington. [PubMed] [Google Scholar]
- Siega‐Riz A.M. & Laraia B. (2006) The implications of maternal overweight and obesity on the course of pregnancy and birth outcomes. Maternal and Child Health Journal 10 (5 Suppl.), S153–S156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Socialstyrelsen (2005) Folkhälsorapporten 2005. Socialstyrelsen. Stockholm.
- Stuckey H.L., Boan J., Kraschnewski J.L., Miller‐Day M., Lehman E.B. & Sciamanna C.N. (2011) Using positive deviance for determining successful weight‐control practices. Qualitative Health Research 21 (4), 563–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Swedish Social Insurance Agency (2010) Parental Benefit Available at: https://www.forsakringskassan.se/wps/wcm/connect/28f32b72-c3fd-43a9-9c33-038fdad53c00/foraldrapenning_eng.pdf?MOD=AJPERES
- Wood W., Quinn J.M. & Kashy D.A. (2002) Habits in everyday life: thought, emotion and action. Journal of Personality and Social Psychology 83 (6), 1281–1297. [PubMed] [Google Scholar]


